Abstract
Enhanced Recovery After Surgery (ERAS) protocols have substantially proven their merit in diminishing recuperation durations and mitigating postoperative adverse events in geriatric populations undergoing colorectal cancer procedures. Despite this, the pivotal aspect of postoperative pain control has not garnered the commensurate attention it deserves. Typically, employing a multimodal analgesia regimen that weaves together nonsteroidal anti-inflammatory drugs, opioids, local anesthetics, and nerve blocks stands paramount in curtailing surgical complications and facilitating reduced convalescence within hospital confines. Nevertheless, this integrative pain strategy is not devoid of pitfalls; the specter of organ dysfunction looms over the geriatric cohort, rooted in the abuse of analgesics or the complex interplay of polypharmacy. Revolutionary research is delving into alternative delivery and release modalities, seeking to allay the inadvertent consequences of analgesia and thereby potentially elevating postoperative outcomes for the elderly post-colorectal cancer surgery populace. This review examines the dual aspects of multimodal analgesia regimens by comparing their established benefits with potential limitations and offers insight into the evolving strategies of drug administration and release.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inadequate pain control post-colorectal surgery in elderly patients can lead to significant negative outcomes, highlighting the imperative for improved analgesic strategies tailored to this vulnerable demographic to avert complications such as increased hospital stays and the potential for chronic pain development. |
The extensive discussion on the pros and cons of various analgesics and pain relief techniques within traditional multimodal analgesia emphasizes its crucial role in elderly colorectal surgery patients. While this approach is essential to minimizing surgical complications and enhancing recovery, it requires nuanced consideration of each patient’s specific needs and vulnerabilities. |
The potential for adverse effects, particularly with polypharmacy and the individual's physiological changes due to aging, necessitates a judicious use of drugs and techniques to prevent unnecessary complications. |
Progress in pain management has seen the exploration of novel methodologies like controlled drug release systems, including hydrogels and nanoparticles. These advancements aim to refine pain relief strategies and minimize side effects, presenting a significant potential to enhance postoperative care. |
The integration of these innovative systems with traditional multimodal analgesia approaches could represent a breakthrough in overcoming the limitations currently faced in effectively managing pain among elderly colorectal surgery patients. |
Introduction
Colorectal cancer ranks as the third most common malignancy and stands as the second leading cause of cancer-induced fatalities; notably, over half of those diagnosed are aged 65 or above [1, 2]. For these senior patients, surgical intervention is considered the cornerstone of treatment [3]. ERAS encapsulates a collection of optimized perioperative care protocols founded on solid medical research, aimed at reducing convalescence periods and diminishing the incidence of postoperative complications [4]. Studies validating its effectiveness span diverse demographics, with a particular focus on the older demographic undergoing colorectal procedures [5,6,7]. However, inadequate postoperative analgesia can have detrimental ramifications, including prolonged hospitalization [8], an array of complications such as nausea, vomiting, bowel obstruction, anastomotic failures, urinary retention, and respiratory infections [9], as well as a heightened likelihood of hospital readmission [10]. Delivering effective postoperative analgesia for elderly colorectal cancer patients is a significant enhancer of the ERAS protocol.
A principal component of ERAS is multimodal analgesia, an approach that employs a variety of analgesic modalities and medications concomitantly to mitigate pain [11]. This multipronged strategy, which includes nerve blocks, local anesthetics, analgesics, and sedative medications, is designed to maximize pain relief through the synergistic effects between disparate analgesic techniques and holdings, curb the potential for adverse reactions via reduced dosing, and abate the risk of opioid dependence by minimizing opioid utilization during the perioperative phase. Nevertheless, the widespread use of multiple drug therapies and the potential for inappropriately prescribed medications can lead to grave consequences for the elderly [12]. An association between excessive polypharmacy and adverse health outcomes, including a statistically significant correlation with poorer up-to-5-year overall survival, has been observed in older individuals with colorectal cancer [13]. Age-associated polypharmacy is further complicated by drug–drug interactions, toxicity, confusion, amongst other challenges, particularly in the geriatric population that often contends with reduced hepatic and renal function [14].
Innovations in analgesic delivery, employing various materials, show promise in ameliorating some of the limitations associated with multimodal analgesia in postoperative care for the elderly after colorectal surgeries. This review article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. In the following discussion, we aim to critically appraise the pros and cons of multimodal analgesia strategies for older postoperative colorectal cancer patients and explore the burgeoning potential of novel analgesic delivery systems designed to enhance multimodal analgesia's efficacy.
The Heavy Burden of Poor Pain Control After Colorectal Surgery in Elderly Patients
Post-surgical pain, particularly acute within the first 24 h, is a common occurrence that disproportionately affects elderly patients [15, 16]. This pain extends beyond the immediate physical discomfort, stirring negative emotional experiences and potentially heightening the risk of post-surgical complications in those undergoing colorectal procedures [9, 17]. Unchecked, this postoperative pain may evolve into a chronic state, presenting a persistent challenge [18]. The intricacies of managing postoperative pain in elderly patients are intensified by a myriad of factors such as age-related physiological shifts, comorbidity-induced changes, and intricate interactions between illnesses and drugs, as well as between various drugs themselves [19]. Notably, a retrospective study indicated a direct link between moderate-to-severe postoperative pain and the occurrence of anastomotic leakage (AL)—a complication that can precipitate additional surgery [20]. AL ranks among the more serious outcomes of colorectal surgery, typically resulting in extended hospitalizations, increased readmissions, and escalated healthcare costs [21]. The severity of AL also bears a tangible association with increased mortality in the geriatric demographic, emphasizing the critical need for robust pain management protocols [22]. The repercussions of inadequate pain control are not limited to AL; issues like intestinal blockages and urinary retention compound hospital durations and financial strains [9, 23, 24]. Moreover, the repercussions of severe post-surgical complications can revisit patients in the form of pain episodes a month or even a year following their operations [25]. This pattern of recurrent pain not only places an immense burden on patients but also significantly diminishes their quality of life.
Hence, it is paramount that the pain experienced by elderly patients post-colorectal surgery is afforded significant clinical attention and management. The ensuing discourse aims to meticulously outline the analgesic medications and techniques employed to alleviate pain in this vulnerable patient group following their surgical interventions.
Opioids for Analgesia
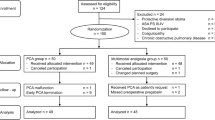
Opioid analgesics primarily interact with opioid receptors located in the peripheral and central nervous systems, including μ, κ, and δ receptors. Through the activation of intracellular G proteins and/or GPCR kinases (GRK) alongside β-arrestins, these medications trigger neuronal hyperpolarization and inhibit the emission of pronociceptive neurotransmitters. This process effectively reduces the propagation of pain signals and facilitates analgesia [26]. Serving as a fundamental component for the treatment of moderate-to-severe pain, opioids are also integral to the World Health Organization’s (WHO) three-step ladder for cancer pain management [27]. However, the deployment of opioid analgesics is not without its set of challenges [28,29,30]. Their interaction with non-target receptors can potentially lead to issues such as addiction and misuse [31,32,33,34]. Their interaction with non-target receptors can potentially lead to issues such as addiction and misuse [28]. The utilization of opioids around the time of colorectal surgery has been associated with a notable frequency of adverse reactions, prolonging hospital stays, escalating expenses, and heightening the risk of postoperative readmission [35,36,37,38]. This consideration is especially crucial in surgeries performed on the aging population afflicted with colorectal cancer. It has been illustrated that among elderly female patients undergoing elective open colectomy, minimizing routine oral opioid consumption is strongly linked to reduced hospitalization durations [39]. Decreasing the dosage of opioids for elderly patients undergoing colorectal surgery not only can lower the rate of adverse reactions but also can diminish the risk of cognitive impairments [40]. Remarkably, studies have illuminated the possibility of conducting opioid-free analgesia within this patient group, despite some limitations such as the singular focus of the institutions involved [41, 42].
Within specific analgesic frameworks, colorectal surgeries can be executed without relying on opioids. While the analgesic efficacy of opioids is well documented, their application in aiding the rapid recovery of elderly colorectal cancer patients necessitates a thorough evaluation of their potential adverse reactions and misuse risks. With meticulous management, opioids can indeed contribute positively to surgical outcomes. Nonetheless, in addressing the specialized needs of the elderly patient demographic, a delicate equilibrium between the benefits and risks of analgesic options must be meticulously maintained to ensure both effective pain control and minimizing the likelihood of adverse outcomes.
Analgesic Drug
Nonsteroidal Anti-Inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) act by impeding the synthesis of prostaglandins through the inhibition of cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) enzymes, bestowing them with their noted anti-inflammatory and analgesic properties [43]. These agents are championed as a facet of multimodal analgesia after colorectal surgery, credited for their capacity to diminish opioid consumption [44, 45]. Research further suggests that NSAIDs may facilitate expedited bowel recovery, minimize postoperative complications, and consequently abbreviate hospital stays following colorectal operations [46,47,48]. Yet, the contention persists regarding the potential of NSAID administration during the perioperative period to precipitate anastomotic leakage (AL) [49,50,51,52]. Delving into this debate, a recent prospective multicenter cohort study involving elderly colorectal surgery patients determined that NSAID usage did not influence the incidence of postoperative AL [53]. Theoretically, COX-1 is instrumental in the synthesis of prostaglandins that confer protective benefits to the platelets and the gastrointestinal tract, whereas COX-2 is implicated in the elicitation of inflammatory and pain symptoms [43]. Non-selective NSAIDs inhibit COX-1 or COX-2 to varying degrees. Hence, selective COX-2 inhibitors might exert a milder impact on AL compared to their non-selective counterparts due to their targeted inhibition [54]. Notably, observational data suggest that ketorolac, when employed perioperatively, does not materially correlate with augmented AL occurrence post-colorectal surgery. Conversely, the use of diclofenac may be associated with an increased likelihood of such postoperative complications [54,55,56,57]. Furthermore, NSAIDs have been associated with adverse cardiovascular outcomes, including acute myocardial infarction and dose-related heart failure [58,59,60].
In synthesis, NSAIDs possess a vital role within the multimodal analgesia framework, especially for elderly patients undergoing colorectal surgeries, given their efficacy in reducing opioid consumption and providing postoperative pain control. Nevertheless, a diligent consideration of the potential risks attributed to NSAID administration is imperative, with AL standing as a quintessential concern in the postoperative panorama of the elderly cohort undergoing colorectal surgeries. The majority of extant investigations elucidating the relationship between NSAIDs and AL are observational in nature, lending themselves to potential selection bias and confounding variables, thereby begetting conclusions of questionable robustness. Consequently, there is a pressing demand for more rigorous randomized controlled trials to discern the precise nexus between NSAID categories, dosage regimens, and the balance of benefits against adverse sequelae in the elderly post-colorectal surgery patient population.
Acetaminophen
Acetaminophen, by metabolizing into N-acylphenolamine (AM404) and acting on the transient receptor potential vanilloid 1 (TRPV1) as well as cannabinoid 1 receptors, facilitates analgesic effects [61]. Its minimal suppression of cyclooxygenase (COX) enzymes coupled with an absence of significant gastrointestinal and renal side effects renders acetaminophen as a preferred, first-line analgesic, particularly favorable for patients ineligible for NSAIDs and the geriatric population [62]. Research evidence underscores acetaminophen's efficacy in providing substantial pain relief, curbing opioid requirements, shortening hospitalization, mitigating instances of intestinal obstruction, and fostering a quicker restoration of intestinal functions amidst colorectal surgical procedures [63]. Notably, intravenous administration of acetaminophen in the early postoperative phases post colorectal surgery may pivotally bolster patient recovery compared to its oral counterpart [64]. Nevertheless, contrasting views emerge from a recent retrospective study that challenges the assertion of acetaminophen’s role in diminishing hospital stays or opioid usage substantially during colorectal surgical interventions [65]. In the realm of postoperative analgesia, acetaminophen, devoid of an anti-inflammatory capacity, is often paired with NSAIDs to expedite patient convalescence following colorectal surgeries [66]. This combination, however, must be prescribed with vigilance due to the potential augmented risk of gastrointestinal bleeding, especially in elderly patients [67]. Predominantly liver-metabolized, acetaminophen, while generally safe within therapeutic parameters, harbors the sinister potential of eliciting grave hepatotoxicity and inducing acute liver failure in scenarios of compromised hepatic function—owing to malnutrition, age-related physiological downturns, or multiple comorbidities [68]. In circumstances of overdose, the strategic administration of activated charcoal to attenuate paracetamol absorption, supplemented by acetylcysteine, can be instrumental in averting hepatic cellular injury [69].
In brief, the judicious use of acetaminophen in elderly colorectal surgical patients bearing normal liver functionality could be supportive of their recovery trajectory. Its application during the perioperative phase demands cautious consideration for individuals with weakened or malfunctioning livers. Considering the scarcity of research specifically focusing on the effectiveness of acetaminophen for the elderly undergoing colorectal surgeries, further empirical investigation is necessitated to underpin its utility.
Lidocaine
Lidocaine is a widely utilized amide local anesthetic, known for impeding the generation and propagation of action potentials by the reversible blockade of voltage-gated sodium channels, thereby manifesting analgesic and anti-inflammatory properties [70]. Research indicates that intravenous (IV) administration of lidocaine in the context of both laparoscopic and open colorectal surgeries during the perioperative phase contributes to mitigated pain levels, reduced incidence of nausea and vomiting, abbreviated duration of ileus, decreased reliance on opioids, a shortened hospital stay, and expedited recovery of gastrointestinal tract function [71,72,73,74,75]. Specifically, in elderly patient populations who have undergone laparoscopic colorectal surgeries, the application of IV lidocaine has been associated with enhanced gastrointestinal recuperation and a concurrent reduction in opioid consumption [76]. However, the implementation of IV lidocaine as a standard aspect of perioperative care in colorectal surgery proceedings is subject to ongoing debate, owing much to the disparity of the study designs referenced in pertinent meta-analyses. These variations encompass differing lidocaine doses and administration duration, along with inconsistent perioperative management protocols and research goals. One meta-analysis revealed no apparent benefits of IV lidocaine in improving outcomes after laparoscopic colectomy [77]. Conversely, another meta-analysis drawing from randomized controlled trials posited that a minimum of 24-h postoperative IV lidocaine infusion is requisite to proffer effective analgesia and reduce the length of hospitalization [78]. Intriguingly, there is evidence to suggest that lidocaine might exert anti-tumoral activity, promoting apoptosis and curtailing the proliferation of colorectal cancer cells, while concurrently furnishing effective analgesia during colorectal interventions [79]. Given that lidocaine undergoes hepatic biotransformation and the elderly frequently present with concurrent illnesses or diminished hepatic function, it is plausible for IV lidocaine to provoke systemic toxicity with potential ramifications on the central nervous system (manifesting as somnolence, seizures) and the cardiovascular system (including arrhythmias, cardiac arrest) [70, 80].
To summarize, IV lidocaine holds promise for the enhancement of postoperative pain management in the elderly demographic undergoing colorectal surgeries. However, the precise optimal dosing and length of lidocaine therapy under diverse perioperative protocols remain indeterminate. There is a pressing need for more expansive and stringent multicenter randomized controlled trials to thoroughly assess the safety profiles and effectiveness of lidocaine. When considering treatment for senior patients, prefacing a lower initial dose and titrating the infusion rate conservatively is advisable. Throughout the administration of IV lidocaine, vigilant monitoring of vital signs such as blood pressure, an ECG, and the availability of emergency equipment are of paramount importance for ensuring patient safety.
α2 Adrenergic Agonists
Α2 adrenergic agonists mitigate pain by inhibiting neural signals within the spinal cord and reducing neurotransmitter release in the brain, effectively regulating both peripheral and central pain pathways [81]. Among these, clonidine and dexmedetomidine have shown promising results for postoperative pain control in colorectal surgery, presenting a viable alternative to opioid analgesics.
Dexmedetomidine, administered intravenously, has demonstrated capabilities in lowering resting pain scores, enhancing parasympathetic activity, and mitigating inflammatory responses, thus fostering gastrointestinal recovery after colorectal surgery [82,83,84,85]. Specifically for elderly patients, dexmedetomidine has been associated with a lower risk of postoperative delirium, spotlighting its potential for safer post-surgical recovery within this demographic [86,87,88]. Nevertheless, caution is warranted regarding its dosage, as excessive levels were found to augment risks of hypotension and bradycardia and delay emergence from anesthesia [89,90,91]. Clonidine, commonly administered via epidural or intrathecal routes, also delivers analgesic benefits [92]. It has demonstrated efficacy in lessening systemic inflammation during colorectal surgeries and providing pain relief [93, 94]. Nonetheless, due to its broader action spectrum, clonidine may heighten hypotension risk compared to dexmedetomidine [95]. Intriguingly, evidence suggests a correlation between clonidine usage and increased opioid consumption in colorectal surgery patients—a point of concern considering the adverse outcomes associated with elevated opioid use [96]. These findings underscore the nuanced balance required in managing postoperative pain. While alpha-2 adrenergic agonists provide valuable tools within the arsenal of multimodal analgesia, their optimal dosing and impact on postoperative recovery merit further research.
Gabapentinoids
Gabapentinoids, a class of antiepileptic medications that includes gabapentin and pregabalin, exert analgesic effects by interacting with the α2δ subunit of voltage-dependent calcium channels, resulting in the attenuation of calcium influx, decremented release of excitatory neurotransmitters, and inhibition of spinal sensitization [97]. Central to their established use is the role they play as a first-line treatment for adult neuropathic pain [98]. Concurrently, gabapentinoids have gained favor in multimodal analgesic strategies for their role in substantially diminishing opioid requirements in the perioperative milieu of colorectal surgeries [44, 66, 99]. The preoperative administration of gabapentinoids has been endorsed for its efficacy in forestalling postoperative nausea and vomiting [100, 101]. Nonetheless, it warrants acknowledgment that, particularly within the elderly patient population who may have additional health conditions, gabapentinoids have been implicated in escalating the incidence of postoperative delirium, profound sedation, respiratory depression, and complications when used in conjunction with novel antipsychotic medications [102,103,104]. Retrospective analysis of elective colorectal surgical cases has demonstrated that while gabapentinoid usage marginally decreased the requirement for intravenous morphine equivalents on the day of surgery, it paradoxically elevated the necessity for noninvasive ventilation and the employment of naloxone to remediate opioid-induced respiratory depression and sedation [105]. The American Geriatrics Society's Beers Criteria flags gabapentin as a medication that holds potential inappropriateness for geriatric use [106].
Consequently, the incorporation of gabapentinoids in perioperative pain management for the elderly is subjected to debate and calls for a reassessment of its routine prophylactic employment. The diversity inherent in colorectal surgical practices underscores the challenge of ascertaining an optimal dose and usage duration for gabapentinoids that strikes a balance between reducing opioid consumption and circumventing adverse effects. In clinical scenarios, the imperative evaluation of patient-specific factors, such as age, underlying medical conditions, and concurrent medication regimens, must complement the comprehensive assessment of the benefits and potential risks, thereby enabling the crafting of individualized, judicious care plans.
The employment of conventional analgesic modalities for postoperative pain relief in senior individuals after colorectal surgical procedures offers a host of potential advantages that are not insignificant. These benefits span the spectrum from diminishing the need for opioids—a measure that can significantly mitigate the risks associated with opioid use—to alleviating the typical discomforts of postoperative nausea and vomiting. They also promote more expedient gastrointestinal recuperation and may contribute to a reduced length of hospital recuperation time. Nonetheless, the selection of analgesics within this demographic must be approached with deliberate prudence. Geriatric patients frequently present with a tangle of polypharmacy and associated health complications. It is essential, therefore, to navigate these complexities with care to minimize the possibility of adverse drug-disease interactions. Of note, the pool of clinical data pertaining to elderly patients who have undergone colorectal surgery is oftentimes limited to a narrow scope of medications or classes thereof. There is, therefore, a pressing necessity for the inception and completion of more targeted clinical trials. Such research endeavors can serve as a beacon, offering broader references and spawning a wider array of analgesic options tailor-made for this vulnerable segment of the population. The subsequent Table 1 encapsulates an overview that distills the purported merits and potential limitations of various analgesic agents earmarked for postoperative pain management in the context of colorectal surgery among the elderly.
Analgesic Technique
Epidural Analgesia
Epidural analgesia, a technique involving the administration of analgesic agents (typically low doses of local anesthetics and opioids) into the epidural space, effectively blocks the transmission of pain signals to the cerebral cortex, thereby inducing analgesia. This procedure poses an array of benefits when applied to postoperative pain management in colorectal surgeries. According to certain research findings, epidural analgesia may not only enhance overall survival rates but also exhibit no significant correlation with increased instances of cancer recurrence [107, 108]. Recognized as the standard bearer for postoperative pain relief following open colorectal surgery, epidural analgesia is lauded for ensuring comprehensive pain control, facilitating gastrointestinal recovery, and reducing complications related to pulmonary functions as well as curtailing the length of hospital stays [44, 109,110,111]. Conversely, the deployment of epidural analgesia in the context of laparoscopic colorectal procedures is a subject of debate—while deemed a safe practice, it has been associated with a spike in hospital costs, extended durations of hospital admission, and a higher prevalence of urinary tract infections and incidents of hypotension [112,113,114,115]. In stark contrast, a multivariate analysis delving into the contributions of epidural analgesia to the convalescence process following colorectal surgeries suggested that, for open procedures, epidural analgesia might amplify occurrences of bowel obstruction and extend hospitalization periods, yet it appears to exert no discernible impact on the recovery trajectory of laparoscopic interventions [116]. These mixed findings cast a modicum of doubt regarding the role of epidural analgesia in promoting the rehabilitation of patients who have undergone colorectal surgeries [116, 117]. Despite its established place as a cornerstone in pain management strategies, epidural analgesia is not devoid of risks; potential significant adverse events include the formation of epidural hematomas, permanent nerve damage, and instances of cardiac arrest precipitated by accidental intravascular injection of analgesic medications [118]. Notably, research focusing specifically on the utility of epidural analgesia in geriatric colorectal surgery patients is limited, with most existing studies not making explicit age-based distinctions. Due to physiological shifts that occur with aging (such as the reduction of myelinated nerve fibers and the compromised functionality of the liver and kidneys) the elderly population may exhibit heightened sensitivity to local anesthetics and experience prolongation in drug half-lives.
To encapsulate, while epidural analgesia is deemed potentially advantageous for those recovering from open colorectal surgeries, its advisability for laparoscopic surgeries remains questionable, particularly when alternative analgesic options, like the transversus abdominis plane block, are accessible [119]. Consequently, there is an imperative need for additional research dedicated to the application of epidural analgesia in the senior cohort undergoing colorectal surgery, to furnish robust, high-quality evidence that can guide clinical practice.
Intrathecal Analgesia
Intrathecal analgesia, which involves the administration of analgesics such as morphine or diacetylmorphine directly into the subarachnoid space, is designed to target the spinal cord sites directly and inhibit the transmission of pain signals to the cerebral cortex, resulting in effective pain relief. Clinical studies have attested to its ability to provide superior analgesia, reduce dependency on opioids, and subsequently improve prognostic outcomes for patients who have undergone colorectal surgeries [120,121,122,123]. This technique is particularly beneficial in the context of laparoscopic colorectal surgeries, where it has been shown to efficiently attenuate visceral pain better than ultrasound or laparoscopy-guided transversus abdominis plane (TAP) blocks, without concomitantly escalating postoperative complications such as ileus or prolonged hospitalization [124,125,126]. Moreover, when compared with epidural analgesia, intrathecal analgesia has been linked with a faster resumption of normal activities and shorter postoperative hospital stays following laparoscopic colorectal procedures [127, 128]. Pertinent findings from a retrospective examination of 233 elderly patients undergoing pancreaticoduodenectomy revealed a reduction in overall opioid consumption, decreased hospital stay lengths, and enhanced functional recovery associated with the use of intrathecal analgesia [129]. Despite these promising outcomes, the field lacks a consensus regarding the optimal dosage of analgesic drugs required to maximize the efficacy of intrathecal analgesia [130]. Although intrathecal analgesia serves as a powerful pain management tool, practitioners must be mindful of the increased risk of side effects such as somnolence, respiratory depression, and pruritus [131, 132]. Specific drugs, like nalbuphine, have been identified to counteract the pruritus induced by intrathecal administration in cases such as labor pain relief [133].
To encapsulate, intrathecal analgesia represents an effective method for controlling pain during laparoscopic colorectal procedures, but evidence to support its use in open colorectal surgeries remains sparse. Given that respiratory depression constitutes a potentially fatal side effect of intrathecal analgesia, stringent monitoring is imperative during its application. The current body of research underscores the necessity for further high-caliber studies focusing on intrathecal analgesia within the elderly patient demographic undergoing colorectal surgery. Such research is crucial for elucidating the relationship between the types of analgesic drugs employed and patient outcomes, as well as determining the most appropriate drug dosages.
Transverse Abdominal Plane Block
The transversus abdominis plane (TAP) block is a regional analgesia technique that delivers local anesthetics between the internal oblique and transversus abdominis muscles, effectively targeting the sensory nerves emanating from the lower thoracic (T6) and the first lumbar (L1) nerves. This provides analgesia to the anterolateral abdominal wall's skin, muscles, and parietal peritoneum [134]. Moreover, it can be divided into three types according to different methods of operation. Traditional blind puncture TAP block is primarily based on the triangle of petit positioning. However, there are some operation-related risks, such as inadvertent vascular injection of local anesthetics, visceral injury, or temporary femoral nerve paralysis. These risks are particularly accentuated in patients with physiological variations such as the elderly, who may possess a reduced muscle mass, or in obese patients with deeper tissue layers complicating the identification of the correct puncture site [135]. The advent of ultrasound-guided TAP blocks has elevated the safety and efficacy of this technique, though the diffusion and consequent analgesic efficacy of local anesthetics can vary based on the injectate’s site and the employed method [136]. During the early postoperative period following colorectal surgery, laparoscopic-guided TAP blocks have shown superiority over ultrasound-guided approaches in terms of pain control and opioid-sparing effects, notwithstanding a scarcity of noninferiority research due to the exclusive performance of the procedure by surgeons [137,138,139,140]. Numerous studies have demonstrated that TAP blocks analgesia after laparoscopic colorectal surgery, lowers the requirement for opioids, speeds up gastrointestinal healing, and shortens hospital stays [141,142,143,144,145]. Acknowledging its benefits, the TAP block has been embraced as a component of multimodal analgesia during laparoscopic surgeries in the Guidelines for Perioperative Care in Elective Colorectal Surgery [44].
Moreover, compared to epidural analgesia, TAP blocks have demonstrated comparable analgesic efficacy and are associated with reduced postoperative nausea, vomiting, ileus, and paresthesia in patients undergoing laparoscopic colorectal surgery [146]. To surpass the transitory nature of a single bupivacaine injection, continuous TAP block with catheter placement or the use of liposome-encapsulated bupivacaine can prolong analgesia, a strategy that has matched the efficacy of epidural analgesia in open colorectal surgery according to cohort studies [147]. Some investigations have found perioperative pain control with liposomal bupivacaine in TAP blocks to be as effective as epidural analgesia regardless of the surgical approach, with potential additional benefits for patient recovery [119, 137, 148]. However, debates persist concerning the cost-effectiveness of liposomal bupivacaine compared to traditional formulations [149, 150].
Overall, TAP blocks offer a safe and effective analgesic strategy suitable for laparoscopic colorectal surgeries, and may serve as a viable option to epidural analgesia, particularly when traditional routes are contraindicated or undesirable. It is essential, however, to recognize that TAP blocks are not typically indicated for deep visceral pain management. Although current evidence substantiates the efficacy of TAP blocks, additional studies tailored to the needs of elderly patients and comprehensive comparisons with epidural analgesia, specifically in the context of open colorectal surgeries, are warranted to optimize postoperative pain relief strategies and fortify the evidence base.
Wound Infiltration
Wound infiltration analgesia (WI) is an approach that administers local anesthetic directly to the site of incision, effectively blocking the voltage-gated sodium channels on the cell membranes of peripheral nerve fibers, thereby preventing the initiation and transmission of pain signals. It may involve either a single injection of a local anesthetic at the end of the procedure or a continuous infusion via a catheter placed prior to the closing of the incision. Efficacy of WI in colorectal surgery is well documented, with reduced opioid requirements, shortened hospital stays, and enhanced postoperative recovery among its noted benefits [121, 151, 152]. WI has been observed to offer an analgesic effect and facilitate postoperative recovery comparable to that of a TAP block in the context of laparoscopic colorectal procedures. Its greater safety profile, ease of administration, and cost-effectiveness potentially render it a preferred option [153, 154]. Research, including a prospective study, has indicated that a combination of TAP block and WI can achieve exceptional pain control while diminishing the need for opioid analgesics, mitigating postoperative nausea, and promoting faster bowel recovery in comparison to the use of WI alone [155]. However, recent findings also suggest that the addition of a TAP block to WI may not significantly further the cause of analgesia and improved prognosis [156, 157]. In cases of open colorectal surgery, WI has been found to be less effective than epidural analgesia in terms of analgesic impact and functional recovery, though it is associated with a lower risk of adverse events such as hypotension [110, 158]. Enhancements in the duration and quality of WI analgesia can be achieved by incorporating adjuvants such as nalbuphine or ketorolac [159]. Notably, while WI carries a risk for wound infection and other potential complications like systemic toxicity from the local anesthetic (particularly if used concurrently with TAP block), or bruising and hematoma from vascular perforation, such incidences are generally rare [160].
WI has been proven to augment analgesia and decrease reliance on opioids during both laparoscopic and open colorectal surgeries. However, when employed in isolation for open colorectal surgery, WI does not cater to all pain requirements since effects are mostly localized to the incision area. Hence, its integration with other analgesic techniques or agents should be considered. Owing to its simplicity and safety, WI may be deemed a first-line choice for laparoscopic colorectal surgeries, yet there is a pressing need for more dedicated research to elucidate its efficacy specifically within the older patient demographic to establish clear evidence-based guidelines.
Acupuncture Analgesia
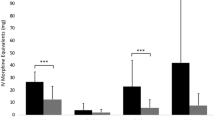
Acupuncture analgesia operates by activating the endogenous opioid peptide system, which affects the body's pain regulation systems by altering the processing and perception of harmful stimuli at different levels of the central nervous system [161]. In the practice of electroacupuncture, following the insertion of acupuncture needles, an electroacupuncture device is connected to transmit electrical currents through the needles. Transcutaneous electrical acupoint stimulation (TEAS), on the other hand, does not involve needle insertion, but instead currents are delivered to the acupoints via surface electrodes similar to transcutaneous electrical nerve stimulation (TENS) [162]. Numerous studies have demonstrated that electroacupuncture can reduce the duration of postoperative ileus, ambulation time, and demand for postoperative analgesia in patients undergoing laparoscopic surgery for colorectal cancer [163,164,165,166]. Likewise, perioperative TEAS has been shown to facilitate postoperative recovery of gastrointestinal function, decrease the incidence of postoperative gastrointestinal dysfunctions (PGD) and postoperative nausea and vomiting (PONV), as well as reduce postoperative pain scores and the length of hospital stays [163,164,165,169]. A randomized controlled trial investigating the effects of TEAS at the ST36 acupoint on recovery after laparoscopic colorectal cancer surgery found that TEAS promoted gastrointestinal recovery and reduced pain intensity within 48 h post-surgery, addressing early postoperative analgesic needs [170]. Intriguingly, TEAS has been found to lower the incidence of perioperative neurocognitive disorders (PND) when used adjunctively with elderly patients [171]. Acupuncture analgesia, integrating Eastern and Western medical practices, offers a safe, effective, and new approach for managing pain in colorectal surgery patients. When considering the multitude of benefits attributed to TENS, it appears to hold significant potential as an auxiliary and complementary therapy for postoperative pain. However, due to the lack of standardized settings for acupuncture stimulation frequency, duration, and strength, and the lack of flexibility in selecting acupoints for different surgeries, it remains challenging to ascertain the most suitable methods for specific patient groups to reduce pain scores and intravenous analgesic consumption. In addition, there is a scarcity of literature directly comparing different acupuncture techniques in postoperative pain management. Currently, acupuncture is an intriguing adjunctive tool for acute pain management. Continuous research on a broader patient population may further clarify the role of acupuncture in the alleviation of postoperative pain, potentially enriching analgesic care strategies for colorectal surgery patients, particularly the elderly.
Indeed, the intricacies of postoperative analgesia for laparoscopic and open colorectal surgeries warrant multifaceted consideration, as the appropriate strategies differ markedly between the two. For laparoscopic colorectal resections, modalities such as TAP blocks or WI stand out for their safety and efficacy, albeit with the noteworthy limitation of not addressing visceral pain. Contrarily, the use of epidural analgesia is often linked to higher hospitalization costs, longer stays, and a greater incidence of urinary tract infections and hypotension. In the realm of open colorectal surgeries, epidural analgesia and intrathecal morphine manifest as superior alternatives, providing optimal pain relief while also aiding in the recuperative process of gastrointestinal functions and potentially reducing hospitalization duration. The TAP block, particularly when enhanced with catheter insertion or liposomal bupivacaine, presents itself as a valuable substitute for postoperative pain control if epidural or intrathecal analgesia is not viable.
Notwithstanding the choice of analgesic technique, each carries its set of challenges. In the elderly, the practicality of various analgesic interventions may be hindered due to weakening organ function, comorbid chronic ailments, and the intricacies of polypharmacy. There is an evident need for more extensive research devoted to the application and interplay of different postoperative analgesia strategies in the elderly population undergoing colorectal surgery to solidify the evidence base and refine analgesic protocols.
Possibility and Prospect of Combining Novel Materials with Multimodal Analgesia
Traditional approaches to medication administration often necessitate high dosages or frequent dosing to achieve therapeutic levels in the bloodstream, which can lead to an escalation of adverse effects and potential toxicity [172, 173]. This is particularly relevant in the management of postoperative pain in the elderly, where physiological alterations such as diminished hepatic and renal functions preclude the straightforward escalation of dosage or repetition of administration. Targeting these challenges, there has been a significant stride in the development of controlled drug delivery systems. These novel systems are engineered to precisely regulate the distribution of drugs, thereby mitigating the incidence of side effects and optimizing therapeutic efficacy [174]. Among these innovations, hydrogels and nanoparticles have garnered attention as the most extensively researched carriers for the delivery of analgesic agents.
Hydrogels
Adjustable degradability and the protective capacity against drug degradation render hydrogels an efficient medium for both temporal and spatial control of analgesic release. The unique properties of hydrogels, especially those formed from biopolymers such as alginate, collagen, and chitosan, make them highly suitable for drug delivery in elderly patients undergoing colorectal surgery [175,176,177]. These wound-healing hydrogels can doubly function as carriers for analgesics, potentially synergizing the wound-healing and analgesic properties. The characteristic features of hydrogels make them an attractive prospect for sustained drug release as part of a multimodal approach to pain management postoperatively [178].
The concept of using hydrogels to deliver analgesics dates back to 1985 when studies like that of Westerling et al. noted that rectal administration of morphine within hydrogels produced higher plasma concentrations without marked side effects, suggesting enhanced and prolonged absorption of the drug [179]. Subsequent research on pediatric ENT surgery patients found that although hydrogels could reduce certain side effects such as nausea and dry mouth, they provided less analgesia than intramuscular injections [180]. These initial findings demonstrated potential in reducing opioid-related adverse effects but at some cost to analgesic effectiveness.
With the evolution of the multimodal approach to postoperative rehabilitation [181], the enhancement of perioperative care pathways has advanced significantly, culminating in the versatile multimodal analgesic techniques of today [182, 183]. Compared to the previous methods, there are many new ways to reduce opioid usage by using hydrogel without decreasing the analgesic effect. There are many new options for what drugs to load and how to load them.
NSAIDs are a commonly used medicine in multi-mode analgesia with a wide receptors distribution, which results in a high adverse effect. Hydrogel-based localized sustained release can potentially mitigate these risks. For instance, ketorolac, an effective NSAID for postoperative pain control, is limited in use due to its short duration and systemic side effects [184]. Wu et al.'s development of a ketorolac-eluting hydrogel demonstrated elevated local tissue levels of the drug with fewer systemic effects in animal models [185]. Additionally, NSAIDs can be incorporated into pH-sensitive hydrogels optimized for colon-targeted drug delivery, reducing upper gastrointestinal side effects and enhancing bioavailability [186]. This form of targeted therapy aligns with enhanced recovery after surgery principles but requires further validation for its impact on the rehabilitation of elderly postoperative patients.
The extended release of local anesthetics using injectable hydrogels has also been extensively explored. Addressing the rapid release issue of water-soluble drugs, novel formulations like the self-assembly amphiphilic peptide designed by Peng et al. enable the sustained release of charged lidocaine molecules through controlled biomineralization [187]. Chen et al.'s "sequentially releasing" method further innovates pain management by combining clonidine and ropivacaine in a composite hydrogel to prolong the analgesic effect at the target site [188].
The hydrogel platform's potential extends beyond conventional anesthetics and NSAIDs. Novel applications include dexmedetomidine delivery, hydrogel-based microneedle devices, and polyherbal extracts, each presenting precise analgesic modalities [189,190,191]. Beyond pain relief, hydrogels also assist in wound healing and provide antibacterial, anti-inflammatory, and pro-repair benefits that aid in reducing the transition from acute to chronic pain—an invaluable feature in multimodal pain management strategies [18, 192, 193].
Nanoparticle
Nanoparticles have emerged as promising carriers for conventional drugs, effectively addressing pharmacokinetic limitations observed in long-term drug delivery studies. Their usage in the delivery of local anesthetics has been particularly emphasized due to their excellent biocompatibility, biodegradability, and adaptability. These attributes have led to successful applications in postoperative pain management, yielding significant analgesic effects with minimized side effects [194].
A novel approach in this domain involves a layer-by-layer structure for achieving prolonged anesthetic effects. This technique entails loading lidocaine into core–shell nanostructured lipid nanoparticles, which are subsequently coated with chitosan (CS) and hyaluronic acid (HA) to facilitate topical analgesia. This innovative drug delivery system aims to surmount the intestinal epithelium's barrier function, offering an anesthesia solution characterized by sustained release behavior across the intestinal barrier [195, 196]. When integrated with sequential release mechanisms and multimodal analgesia strategies, this approach holds potential to significantly enhance treatment outcomes for elderly colorectal cancer patients.
Poly (lactic-co-glycolic acid) (PLGA), endorsed by the FDA for various therapeutic interventions, stands out for its outstanding biocompatibility and mechanical properties [197]. Investigations by Moraes et al. into ropivacaine-loaded PLGA nanospheres delineated that such a delivery system could markedly attenuate the toxicity usually associated with ropivacaine formulations. The implementation of PLGA microspheres proposes a biocompatible strategy capable of extending the effective duration of local anesthetics [198].
The integration of local anesthetic agents with nanoparticles paves the way for responsive and controlled drug release mechanisms. Gao et al.'s design of hollow mesoporous organosilica nanoparticles (HMONs)-based platforms exemplifies this concept. These platforms can be activated by acidity or ultrasonic irradiation to dispense the drug, providing a controlled and extended analgesic effect [199].
Similar to hydrogels, nanoparticles could be engineered for responsive release and multi-layered structures, offering the distinct advantage of enhancing the oral bioavailability of drugs [200]. The core principle of multimodal analgesia—utilizing a combination of analgesic drugs and methods with diverse mechanisms of action—aims at maximizing synergistic analgesic benefits while minimizing the adverse effects of individual drugs. Nanoparticles' versatility in oral administration and the capacity for modification further support the potential for an improved multimodal analgesic approach.
Despite these advancements, the journey towards integrating regulated drug delivery systems into multimodal analgesia faces substantial hurdles, including nano-toxicity, immunogenicity, preservation of structural stability, scalability, restricted shelf-life stability, complexities in delivery system design, elevated production costs, challenges in reproducibility, and the difficulty of detecting drug plasma levels compared to traditional methods. These obstacles warrant diligent investigation as the field continues to evolve.
Conclusions
The landscape of surgical treatment for elderly patients with colorectal cancer has evolved considerably, with the implementation of enhanced recovery after surgery (ERAS) protocols becoming increasingly predominant. Effective postoperative analgesia emerges as a vital component of recovery, particularly for the elderly demographic. However, the distinct physiological characteristics of this age group, coupled with the intricacies of pain management, can render some standard multimodal analgesia techniques less feasible due to pre-existing chronic conditions and extensive polypharmacy. The specificity required in the pain management approaches for postoperative colorectal surgery in elderly patients necessitates a more targeted focus in clinical research. This calls for comprehensive multicenter clinical trials aimed at delivering higher-quality evidence tailored to the requirements of both open and laparoscopic surgeries within this population. Discussions surrounding the selection of analgesics, determination of safe dosages, and a balanced evaluation of the risks and rewards associated with various analgesic methodologies for the elderly necessitate ongoing exploration and refinement.
Innovative biomaterials, when synergized with conventional multimodal analgesics, hold exciting potential to broaden the scope of multimodal analgesia. By offering superior postoperative relief and mitigating the complexities of disease–drug and drug–drug interactions pervasive among the elderly, these novel materials stand to significantly contribute to the enhancement of patient outcomes. However, before their widespread adoption, critical factors such as biocompatibility, biodegradability, and the economics of production must be thoroughly vetted.
In any case, bridging cutting-edge biomaterials with established analgesic drugs and techniques heralds a promising frontier for future research, potentially revolutionizing the way postoperative pain is managed.
Data Availability
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
References
Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145–64.
Turri G, Caliskan G, Conti C, et al. Impact of age and comorbidities on short- and long-term outcomes of patients undergoing surgery for colorectal cancer. Front Oncol. 2022;12: 959650.
Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017;152(3):292–8.
Coeckelberghs E, Vanhaecht K, Seys D, et al. A breakthrough improvement collaborative significantly reduces hospital stay after elective colectomy for cancer across a healthcare system. Ann Surg. 2022;276(5):890–6.
Tan JKH, Ang JJ, Chan DKH. Enhanced recovery program versus conventional care after colorectal surgery in the geriatric population: a systematic review and meta-analysis. Surg Endosc. 2021;35(6):3166–74.
Ripollés-Melchor J, Ramírez-Rodríguez JM, Casans-Francés R, et al. Association between use of enhanced recovery after surgery protocol and postoperative complications in colorectal surgery: the postoperative outcomes within enhanced recovery after surgery protocol (POWER) study. JAMA Surg. 2019;154(8):725–36.
Martínez-Escribano C, Moreno FA, Pérez-López M, et al. Malnutrition and increased risk of adverse outcomes in elderly patients undergoing elective colorectal cancer surgery: a case-control study nested in a cohort. Nutrients. 2022;14(1):207.
van Boekel RLM, Warlé MC, Nielen RGC, et al. Relationship between postoperative pain and overall 30-day complications in a broad surgical population: an observational study. Ann Surg. 2019;269(5):856–65.
Hernandez-Boussard T, Graham LA, Desai K, et al. The fifth vital sign: postoperative pain predicts 30-day readmissions and subsequent emergency department visits. Ann Surg. 2017;266(3):516–24.
Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152(7):691–7.
Tian F, Chen Z, Wu J. Prevalence of polypharmacy and potentially inappropriate medications use in elderly Chinese patients: a systematic review and meta-analysis. Front Pharmacol. 2022;13: 862561.
Chen L-J, Nguyen TNM, Chang-Claude J, et al. Association of polypharmacy with colorectal cancer survival among older patients. Oncologist. 2021;26(12):e2170–80.
Hoel RW, Giddings Connolly RM, Takahashi PY. Polypharmacy management in older patients. Mayo Clin Proc. 2021;96(1):242–56.
Willingham MD, Vila MR, Ben Abdallah A, et al. Factors contributing to lingering pain after surgery: the role of patient expectations. Anesthesiology. 2021;134(6):915–24.
Walker EMK, Bell M, Cook TM, et al. Patient reported outcome of adult perioperative anaesthesia in the United Kingdom: a cross-sectional observational study. Br J Anaesth. 2016;117(6):758–66.
Regenbogen SE, Mullard AJ, Peters N, et al. Hospital analgesia practices and patient-reported pain after colorectal resection. Ann Surg. 2016;264(6):1044–50.
Glare P, Aubrey KR, Myles PS. Transition from acute to chronic pain after surgery [J]. Lancet. 2019;393(10180):1537–46.
Falzone E, Hoffmann C, Keita H. Postoperative analgesia in elderly patients. Drugs Aging. 2013;30(2):81–90.
Boström P, Svensson J, Brorsson C, et al. Early postoperative pain as a marker of anastomotic leakage in colorectal cancer surgery. Int J Colorectal Dis. 2021;36(9):1955–63.
Lee SW, Gregory D, Cool CL. Clinical and economic burden of colorectal and bariatric anastomotic leaks. Surg Endosc. 2020;34(10):4374–81.
Boström P, Haapamäki MM, Rutegård J, et al. Population-based cohort study of the impact on postoperative mortality of anastomotic leakage after anterior resection for rectal cancer. BJS Open. 2019;3(1):106–11.
Kang CY, Chaudhry OO, Halabi WJ, et al. Risk factors for postoperative urinary tract infection and urinary retention in patients undergoing surgery for colorectal cancer. Am Surg. 2012;78(10):1100–4.
Tevis SE, Carchman EH, Foley EF, et al. Postoperative ileus-more than just prolonged length of stay? J Gastrointest Surg. 2015;19(9):1684–90.
Hanley C, Ladha KS, Clarke HA, et al. Association of postoperative complications with persistent post-surgical pain: a multicentre prospective cohort study. Br J Anaesth. 2022;128(2):311–20.
Che T, Roth BL. Molecular basis of opioid receptor signaling. Cell. 2023;186(24):5203–19.
Forbes K. Pain in patients with cancer: the World Health Organization analgesic ladder and beyond. Clin Oncol (R Coll Radiol). 2011;23(6):379–80.
Fiore JF, El-Kefraoui C, Chay M-A, et al. Opioid versus opioid-free analgesia after surgical discharge: a systematic review and meta-analysis of randomised trials. Lancet. 2022;399(10343):2280–93.
TASMAN Collaborative. Impact of opioid-free analgesia on pain severity and patient satisfaction after discharge from surgery: multispecialty, prospective cohort study in 25 countries. Br J Surg. 2024;111(1):znad421.
Wei Q, Li M, Du Q, et al. Association between opioids use and risk of multiple cancers: a two-sample Mendelian randomization study. J Anest Transl Med. 2024;3(1):1–9.
Mazzeo F, Meccariello R, Guatteo E. Molecular and epigenetic aspects of opioid receptors in drug addiction and pain management in sport. Int J Mol Sci. 2023;24(9):31.
Cuitavi J, Torres-Pérez JV, Lorente JD, et al. Crosstalk between mu-opioid receptors and neuroinflammation: Consequences for drug addiction and pain. Neurosci Biobehav Rev. 2023;145:105011.
Zhang J-J, Song C-G, Dai J-M, et al. Mechanism of opioid addiction and its intervention therapy: focusing on the reward circuitry and mu-opioid receptor. MedComm. 2022;3(3):e148.
Listos J, Łupina M, Talarek S, et al. The mechanisms involved in morphine addiction: an overview. Int J Mol Sci. 2019;20(17):4302.
Homsi J, Brovman EY, Rao N, et al. The association between potential opioid-related adverse drug events and outcomes in colorectal surgery. J Laparoendosc Adv Surg Tech A. 2019;29(11):1436–45.
Cortez AR, Freeman CM, Levinsky NC, et al. The impact of preoperative opioid use on outcomes after elective colorectal surgery: a propensity-matched comparison study. Surgery. 2019;166(4):632–8.
Jackson NA, Gan T, Davenport DL, et al. Preoperative opioid, sedative, and antidepressant use is associated with increased postoperative hospital costs in colorectal surgery. Surg Endosc. 2021;35(10):5599–606.
Hassinger TE, Krebs ED, Turrentine FE, et al. Preoperative opioid use is associated with increased risk of postoperative complications within a colorectal-enhanced recovery protocol. Surg Endosc. 2021;35(5):2067–74.
Ahmed J, Lim M, Khan S, et al. Predictors of length of stay in patients having elective colorectal surgery within an enhanced recovery protocol. Int J Surg. 2010;8(8):628–32.
Sun XJ, Feng TC, Wang YM, et al. The effect of the enhanced recovery after surgery protocol and the reduced use of opioids on postoperative outcomes in elderly patients with colorectal cancer. Eur Rev Med Pharmacol Sci. 2023;27(20):10053–60.
Lohsiriwat V. Opioid-free analgesia: is it achievable in open colorectal surgery without neuraxial block? Minerva Surg. 2022;77(6):573–81.
Yap R, Nassif G, Hwang G, et al. Achieving opioid-free major colorectal surgery: is it possible? Dig Surg. 2020;37(5):376–82.
Cashman JN. The mechanisms of action of NSAIDs in analgesia. Drugs. 1996;52(Suppl 5):13–23.
Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg. 2019;43(3):659–95.
Maund E, McDaid C, Rice S, et al. Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs for the reduction in morphine-related side-effects after major surgery: a systematic review [J]. Br J Anaesth. 2011;106(3):292–7.
Milne TGE, Jaung R, O’Grady G, et al. Nonsteroidal anti-inflammatory drugs reduce the time to recovery of gut function after elective colorectal surgery: a systematic review and meta-analysis [J]. Colorectal Dis. 2018;20(8):O190–8.
Chapman SJ, Garner JJ, Drake TM, et al. Systematic review and meta-analysis of nonsteroidal anti-inflammatory drugs to improve GI recovery after colorectal surgery. Dis Colon Rectum. 2019;62(2):248–56.
Brolet EA, Joris JL, Monseur JJ, et al. Impact of non-steroidal anti-inflammatory drugs on the efficiency of enhanced recovery programmes after colorectal surgery: a retrospective study of the GRACE database. Anaesth Crit Care Pain Med. 2021;40(3): 100880.
Arron MNN, Lier EJ, de Wilt JHW, et al. Postoperative administration of non-steroidal anti-inflammatory drugs in colorectal cancer surgery does not increase anastomotic leak rate; a systematic review and meta-analysis. Eur J Surg Oncol. 2020;46(12):2167–73.
Kastora SL, Osborne LL, Jardine R, et al. Non-steroidal anti-inflammatory agents and anastomotic leak rates across colorectal cancer operations and anastomotic sites: a systematic review and meta-analysis of anastomosis specific leak rate and confounding factors. Eur J Surg Oncol. 2021;47(11):2841–8.
Grahn O, Lundin M, Chapman SJ, et al. Postoperative nonsteroidal anti-inflammatory drugs in relation to recurrence, survival and anastomotic leakage after surgery for colorectal cancer. Colorectal Dis. 2022;24(8):933–42.
Chien-Ying Wu, Cheng K-C, Chen Y-J, et al. Risk of NSAID-associated anastomosis leakage after colorectal surgery: a large-scale retrospective study using propensity score matching. Int J Colorectal Dis. 2022;37(5):1189–97.
Sun L, Feng Y. Safety and efficacy of non-steroidal anti-inflammatory drugs to reduce ileus after colorectal surgery. Br J Surg. 2020;107(2):e161–9.
Modasi A, Pace D, Godwin M, et al. NSAID administration post colorectal surgery increases anastomotic leak rate: systematic review/meta-analysis. Surg Endosc. 2019;33(3):879–85.
Klein M, Gogenur I, Rosenberg J. Postoperative use of non-steroidal anti-inflammatory drugs in patients with anastomotic leakage requiring reoperation after colorectal resection: cohort study based on prospective data. BMJ. 2012;345:e6166.
Saleh F, Jackson TD, Ambrosini L, et al. Perioperative nonselective non-steroidal anti-inflammatory drugs are not associated with anastomotic leakage after colorectal surgery. J Gastrointest Surg. 2014;18(8):1398–404.
Hawkins AT, McEvoy MD, Wanderer JP, et al. Ketorolac use and anastomotic leak in elective colorectal surgery: a detailed analysis. Dis Colon Rectum. 2018;61(12):1426–34.
Bell S, Rennie T, Marwick CA, et al. Effects of peri-operative nonsteroidal anti-inflammatory drugs on post-operative kidney function for adults with normal kidney function. Cochrane Database Syst Rev. 2018;11(11):CD011274.
Arfè A, Scotti L, Varas-Lorenzo C, et al. Non-steroidal anti-inflammatory drugs and risk of heart failure in four European countries: nested case-control study. BMJ. 2016;354:i4857.
STARSurg Collaborative. Perioperative nonsteroidal anti-inflammatory drugs (NSAID) administration and acute kidney injury (AKI) in major gastrointestinal surgery: a prospective, multicenter, propensity matched cohort study. Ann Surg. 2022;275(5):904–910.
Ohashi N, Kohno T. Analgesic effect of acetaminophen: a review of known and novel mechanisms of action. Front Pharmacol. 2020;11: 580289.
Freo U, Ruocco C, Valerio A, et al. Paracetamol: A review of guideline recommendations. J Clin Med. 2021;10(15):3420.
Aryaie AH, Lalezari S, Sergent WK, et al. Decreased opioid consumption and enhance recovery with the addition of IV Acetaminophen in colorectal patients: a prospective, multi-institutional, randomized, double-blinded, placebo-controlled study (DOCIVA study). Surg Endosc. 2018;32(8):3432–3438.
Marcotte JH, Patel KM, Gaughan JP, et al. Oral Versus Intravenous acetaminophen within an enhanced recovery after surgery protocol in colorectal surgery. Pain Phys. 2020;23(1):57–64.
Rizk E, Haas EM, Swan JT. Opioid-sparing effect of liposomal bupivacaine and intravenous acetaminophen in colorectal surgery. J Surg Res. 2021;259:230–41.
Helander EM, Webb MP, Bias M, et al. A comparison of multimodal analgesic approaches in institutional enhanced recovery after surgery protocols for colorectal surgery: pharmacological agents. J Laparoendosc Adv Surg Techn Part A. 2017;27(9):903–8.
Rahme E, Barkun A, Nedjar H, et al. Hospitalizations for upper and lower GI events associated with traditional NSAIDs and acetaminophen among the elderly in Quebec, Canada. Am J Gastroenterol. 2008;103(4):872–82.
Jaeschke H. Acetaminophen: dose-dependent drug hepatotoxicity and acute liver failure in patients. Dig Dis. 2015;33(4):464–71.
Chiew AL, Gluud C, Brok J, et al. Interventions for paracetamol (acetaminophen) overdose. Cochrane Database Syst Rev. 2018;2(2):C003328.
Hermanns H, Hollmann MW, Stevens MF, et al. Molecular mechanisms of action of systemic lidocaine in acute and chronic pain: a narrative review. Br J Anaesth. 2019;123(3):335–49.
Rollins KE, Javanmard-Emamghissi H, Scott MJ, et al. The impact of peri-operative intravenous lidocaine on postoperative outcome after elective colorectal surgery: a meta-analysis of randomised controlled trials. Eur J Anaesthesiol. 2020;37(8):659–70.
Wei S, Yu-Han Z, Wei-Wei J, et al. The effects of intravenous lidocaine on wound pain and gastrointestinal function recovery after laparoscopic colorectal surgery. Int Wound J. 2020;17(2):351–62.
Chen P-C, Lai C-H, Fang C-J, et al. Intravenous infusion of lidocaine for bowel function recovery after major colorectal surgery: a critical appraisal through updated meta-analysis, trial sequential analysis, certainty of evidence, and meta-regression. Front Med (Lausanne). 2021;8:759215.
Chapman SJ, Pericleous A, Downey C, et al. Postoperative ileus following major colorectal surgery. Br J Surg. 2018;105(7):797–810.
Cooke C, Kennedy ED, Foo I, et al. Meta-analysis of the effect of perioperative intravenous lidocaine on return of gastrointestinal function after colorectal surgery. Tech Coloproctol. 2019;23(1):15–24.
Qin P, Wei K, Yang Q, et al. Effect of lidocaine or dexmedetomidine on postoperative recovery in elder patients undergoing colorectal surgery. Minerva Anestesiol. 2023;89(5):405–414.
Sarakatsianou C, Perivoliotis K, Tzovaras G, et al. Efficacy of intravenous use of lidocaine in postoperative pain management after laparoscopic colorectal surgery: a meta-analysis and meta-regression of RCTs. In Vivo. 2021;35(6):3413–21.
Yang W, Yan S, Yu F, et al. Appropriate duration of perioperative intravenous administration of lidocaine to provide satisfactory analgesia for adult patients undergoing colorectal surgery: a meta-analysis of randomized controlled trials. Anesth Analg. 2023;136(3):494–506.
Qu X, Yang L, Shi Q, et al. Lidocaine inhibits proliferation and induces apoptosis in colorectal cancer cells by upregulating mir-520a-3p and targeting EGFR. Pathol Res Pract. 2018;214(12):1974–9.
Waldinger R, Weinberg G, Gitman M. Local anesthetic toxicity in the geriatric population. Drugs Aging. 2020;37(1):1–9.
Bonnet F. Mechanisms of the analgesic effect of alpha 2 adrenergic agonists. Cah Anesthesiol. 1994;42(6):723–5.
Lee JE, Park HJ, Chung YJ, et al. Analgesic effect of dexmedetomidine in colorectal cancer patients undergoing laparoscopic surgery. Saudi Med J. 2022;43(10):1096–102.
Cheung CW, Qiu Q, Ying ACL, et al. The effects of intra-operative dexmedetomidine on postoperative pain, side-effects and recovery in colorectal surgery. Anaesthesia. 2014;69(11):1214–21.
He G-Z, Bu N, Li Y-J, et al. Extra loading dose of dexmedetomidine enhances intestinal function recovery after colorectal resection: a retrospective cohort study. Front Pharmacol. 2022;13:806950.
Sun W, Li F, Wang X, et al. Effects of dexmedetomidine on patients undergoing laparoscopic surgery for colorectal cancer. J Surg Res. 2021;267:687–94.
Chen H, Li F. Effect of dexmedetomidine with different anesthetic dosage on neurocognitive function in elderly patients after operation based on neural network model. World Neurosurg. 2020;138:688–95.
Zhang J, Liu G, Zhang F, et al. Analysis of postoperative cognitive dysfunction and influencing factors of dexmedetomidine anesthesia in elderly patients with colorectal cancer. Oncol Lett. 2019;18(3):3058–64.
He Y, Cheng J, Qin H, et al. Effects of dexmedetomidine on perioperative brain protection in elderly frail patients. J Anesth Transl Med. 2023;2(3):29–33.
Sui X, Wang Y, Jin M, et al. The effects of dexmedetomidine for patient-controlled analgesia on postoperative sleep quality and gastrointestinal motility function after surgery: a prospective, randomized, double-blind, and controlled trial. Front Pharmacol. 2022;13: 990358.
Zhang Y, Xing Z, Xu Y, et al. Effects of different doses of dexmedetomidine on cognitive dysfunction in elderly patients early after laparoscopic surgery for colorectal cancer. Nan Fang Yi Ke Da Xue Xue Bao. 2014;34(5):743–6.
Xiao Y, Tang L, Chen N. The effects of dexmedetomidine on postoperative sleep in elderly patients: a systematic review and meta-analysis. J Anesth Transl Med. 2023;2(3):11–20.
Persec J, Persec Z, Buković D, et al. Effects of clonidine preemptive analgesia on acute postoperative pain in abdominal surgery. Coll Antropol. 2007;31(4):1071–5.
Wu C-T, Jao S-W, Borel CO, et al. The effect of epidural clonidine on perioperative cytokine response, postoperative pain, and bowel function in patients undergoing colorectal surgery. Anesth Analg. 2004;99(2):502.
Persec J, Persec Z, Husedzinovic I. Postoperative pain and systemic inflammatory stress response after preoperative analgesia with clonidine or levobupivacaine: a randomized controlled trial. Wien Klin Wochenschr. 2009;121(17–18):558–63.
Blaudszun G, Lysakowski C, Elia N, et al. Effect of perioperative systemic α2 agonists on postoperative morphine consumption and pain intensity: systematic review and meta-analysis of randomized controlled trials. Anesthesiology. 2012;116(6):1312–22.
Gedda C, Nygren J, Garpenbeck A, et al. Multimodal analgesia bundle and postoperative opioid use among patients undergoing colorectal surgery. JAMA Netw Open. 2023;6(9): e2332408.
Kremer M, Salvat E, Muller A, et al. Antidepressants and gabapentinoids in neuropathic pain: mechanistic insights. Neuroscience. 2016;338:183–206.
Finnerup NB, Attal N, Haroutounian S, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162–73.
Mujukian A, Truong A, Tran H, et al. A standardized multimodal analgesia protocol reduces perioperative opioid use in minimally invasive colorectal surgery. J Gastroint Surg Off J Soc Surg Aliment Tract. 2020;24(10):2286–94.
Grant MC, Lee H, Page AJ, et al. The effect of preoperative gabapentin on postoperative nausea and vomiting: a meta-analysis. Anesth Analg. 2016;122(4):976–85.
Grant MC, Betz M, Hulse M, et al. The effect of preoperative pregabalin on postoperative nausea and vomiting: a meta-analysis. Anesth Analg. 2016;123(5):1100–7.
Cavalcante AN, Sprung J, Schroeder DR, et al. Multimodal analgesic therapy with gabapentin and its association with postoperative respiratory depression. Anesth Analg. 2017;125(1):141–6.
Deljou A, Hedrick SJ, Portner ER, et al. Pattern of perioperative gabapentinoid use and risk for postoperative naloxone administration. Br J Anaesth. 2018;120(4):798–806.
Park CM, Inouye SK, Marcantonio ER, et al. Perioperative Gabapentin use and in-hospital adverse clinical events among older adults after major surgery. JAMA Intern Med. 2022;182(11):1117–27.
Ohnuma T, Krishnamoorthy V, Ellis AR, et al. Association ’between gabapentinoids on the day of colorectal surgery and adverse postoperative respiratory outcomes. Ann Surg. 2019;270(6):e65–7.
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674–694.
Vogelaar FJ, Abegg R, van der Linden JC, et al. Epidural analgesia associated with better survival in colon cancer. Int J Colorectal Dis. 2015;30(8):1103–7.
Hasselager RP, Hallas J, Gögenur I. Epidural Analgesia and recurrence after colorectal cancer surgery: a Danish retrospective registry-based cohort study. Anesthesiology. 2022;136(3):459–71.
Warschkow R, Steffen T, Lüthi A, et al. Epidural analgesia in open resection of colorectal cancer: is there a clinical benefit? A retrospective study on 1,470 patients [J]. J Gastrointest Surg. 2011;15(8):1386–93.
Jouve P, Bazin J-E, Petit A, et al. Epidural versus continuous preperitoneal analgesia during fast-track open colorectal surgery: a randomized controlled trial. Anesthesiology. 2013;118(3):622–30.
Guay J, Nishimori M, Kopp S. Epidural local anaesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting and pain after abdominal surgery. Cochrane Database Syst Rev. 2016;7(7):CD001893.
Halabi WJ, Kang CY, Nguyen VQ, et al. Epidural analgesia in laparoscopic colorectal surgery: a nationwide analysis of use and outcomes. JAMA Surg. 2014;149(2):130–6.
Hübner M, Blanc C, Roulin D, et al. Randomized clinical trial on epidural versus patient-controlled analgesia for laparoscopic colorectal surgery within an enhanced recovery pathway. Ann Surg. 2015;261(4):648–53.
Perivoliotis K, Sarakatsianou C, Georgopoulou S, et al. Thoracic epidural analgesia (TEA) versus patient-controlled analgesia (PCA) in laparoscopic colectomy: a systematic review and meta-analysis. Int J Colorectal Dis. 2019;34(1):27–38.
Hanna MH, Jafari MD, Jafari F, et al. Randomized clinical trial of epidural compared with conventional analgesia after minimally invasive colorectal surgery. J Am Coll Surg. 2017;225(5):622–30.
Al-Mazrou AM, Kiely JM, Kiran RP. Epidural analgesia in the era of enhanced recovery: time to rethink its use? Surg Endosc. 2019;33(7):2197–205.
Rosen DR, Wolfe RC, Damle A, et al. Thoracic epidural analgesia: does it enhance recovery? Dis Colon Rectum. 2018;61(12):1403–9.
Von Hösslin T, Imboden P, Lüthi A, et al. Adverse events of postoperative thoracic epidural analgesia: A retrospective analysis of 7273 cases in a tertiary care teaching hospital. Eur J Anaesthesiol. 2016;33(10):708–14.
Torgeson M, Kileny J, Pfeifer C, et al. Conventional epidural vs transversus abdominis plane block with liposomal bupivacaine: a randomized trial in colorectal surgery. J Am Coll Surg. 2018;227(1):78–83.
Merchea A, Lovely JK, Jacob AK, et al. Efficacy and outcomes of intrathecal analgesia as part of an enhanced recovery pathway in colon and rectal surgical patients. Surg Res Pract. 2018;2018:8174579.
Helander EM, Webb MP, Bias M, et al. Use of regional anesthesia techniques: analysis of institutional enhanced recovery after surgery protocols for colorectal surgery. J Laparoendosc Adv Surg Tech A. 2017;27(9):898–902.
El-Boghdadly K, Jack JM, Heaney A, et al. Role of regional anesthesia and analgesia in enhanced recovery after colorectal surgery: a systematic review of randomized controlled trials. Reg Anesth Pain Med. 2022;47(5):282–92.
Brown L, Gray M, Griffiths B, et al. A multicentre, prospective, observational cohort study of variation in practice in perioperative analgesia strategies in elective laparoscopic colorectal surgery (the LapCoGesic study). Ann R Coll Surg Engl. 2020;102(1):28–35.
Colibaseanu DT, Osagiede O, Merchea A, et al. Randomized clinical trial of liposomal bupivacaine transverse abdominis plane block versus intrathecal analgesia in colorectal surgery. Br J Surg. 2019;106(6):692–9.
Calini G, Abd El Aziz MA, Solafah A, et al. Laparoscopic transversus abdominis plane block versus intrathecal analgesia in robotic colorectal surgery. Br J Surg. 2021;108(11):e369–70.
Han S-R, Lee CS, Bae JH, et al. The additional analgesic effects of transverse abdominis plane block in patients receiving low-dose intrathecal morphine for minimally invasive colorectal surgery: a randomized, single-blinded study. Ann Surg Treat Res. 2021;101(4):221–30.
Levy BF, Scott MJ, Fawcett W, et al. Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. Br J Surg. 2011;98(8):1068–78.
Virlos I, Clements D, Beynon J, et al. Short-term outcomes with intrathecal versus epidural analgesia in laparoscopic colorectal surgery. Br J Surg. 2010;97(9):1401–6.
Burchard PR, Melucci AD, Lynch O, et al. Intrathecal morphine and effect on opioid consumption and functional recovery after pancreaticoduodenectomy. J Am Coll Surg. 2022;235(3):392–400.
Alderman J, Sharma A, Patel J, et al. Intrathecal diamorphine for perioperative analgesia during colorectal surgery: a cross-sectional survey of current UK practice. BMJ Open. 2022;12(8): e057407.
Koning MV, Reussien E, Vermeulen BAN, et al. Serious Adverse Events after a Single Shot of Intrathecal Morphine: A Case Series and Systematic Review [J]. Pain Res Manag. 2022;2022:4567192.
Meylan N, Elia N, Lysakowski C, et al. Benefit and risk of intrathecal morphine without local anaesthetic in patients undergoing major surgery: meta-analysis of randomized trials. Br J Anaesth. 2009;102(2):156–67.
Becker LM, Teunissen AJW, Koopman JSHA. Prevention and treatment of neuraxial morphine-induced pruritus: a scoping review. J Pain Res. 2022;15:1633–45.
Tsai H-C, Yoshida T, Chuang T-Y, et al. Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:8284363.
Jankovic Z, Ahmad N, Ravishankar N, et al. Transversus abdominis plane block: how safe is it? Anesth Analg. 2008;107(5):1758–9.
Carney J, Finnerty O, Rauf J, et al. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66(11):1023–30.
Hamid HKS, Marc-Hernández A, Saber AA. Transversus abdominis plane block versus thoracic epidural analgesia in colorectal surgery: a systematic review and meta-analysis. Langenbecks Arch Surg. 2021;406(2):273–82.
Wong DJ, Curran T, Poylin VY, et al. Surgeon-delivered laparoscopic transversus abdominis plane blocks are non-inferior to anesthesia-delivered ultrasound-guided transversus abdominis plane blocks: a blinded, randomized non-inferiority trial. Surg Endosc. 2020;34(7):3011–9.
Copperthwaite A, Sahebally SM, Raza ZM, et al. A meta-analysis of laparoscopic versus ultrasound-guided transversus abdominis plane block in laparoscopic colorectal surgery. Ir J Med Sci. 2023;192(2):795–803.
Hamid HK, Emile SH, Saber AA, et al. Laparoscopic-guided transversus abdominis plane block for postoperative pain management in minimally invasive surgery: systematic review and meta-analysis. J Am Coll Surg. 2020;231(3):376.
Xu YJ, Sun X, Jiang H, et al. Randomized clinical trial of continuous transversus abdominis plane block, epidural or patient-controlled analgesia for patients undergoing laparoscopic colorectal cancer surgery. Br J Surg. 2020;107(2):e133–41.
Zhao Y, Zhang H-Y, Yuan Z-Y, et al. Analgesic efficacy of postoperative bilateral, ultrasound-guided, posterior transversus abdominis plane block for laparoscopic colorectal cancer surgery: a randomized, prospective, controlled study. BMC Anesthesiol. 2021;21(1):107.
Hain E, Maggiori L, et al. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis. Colorectal Dis. 2018;20(4):279–87.
Viderman D, Aubakirova M, Abdildin YG. Transversus abdominis plane block in colorectal surgery: a meta-analysis. Front Med (Lausanne). 2021;8: 802039.
Liu K-Y, Lu Y-J, Lin Y-C, et al. Transversus abdominis plane block for laparoscopic colorectal surgery: A meta-analysis of randomised controlled trials. Int J Surg (London, England). 2022;104:106825.
Pirrera B, Alagna V, Lucchi A, et al. Transversus abdominis plane (TAP) block versus thoracic epidural analgesia (TEA) in laparoscopic colon surgery in the ERAS program. Surg Endosc. 2018;32(1):376–82.
Miller D, Andriakos P, Vanbacker J, et al. Comparison of transversus abdominis plane catheters with thoracic epidurals for cost and length of stay in open colorectal surgeries: a cohort study [J]. BMC Anesthesiol. 2021;21(1):137.
Felling DR, Jackson MW, Ferraro J, et al. Liposomal bupivacaine transversus abdominis plane block versus epidural analgesia in a colon and rectal surgery enhanced recovery pathway: a randomized clinical trial. Dis Colon Rectum. 2018;61(10):1196–204.
Chevrollier GS, Klinger AL, Green HJ, et al. Liposomal Bupivacaine Transversus Abdominis Plane Blocks in Laparoscopic Colorectal Resections: A Single-Institution Randomized Controlled Trial [J]. Dis Colon Rectum. 2023;66(2):322–30.
Guerra L, Philip S, Lax EA, et al. transversus abdominis plane blocks in laparoscopic colorectal surgery: better pain control and patient outcomes with liposomal bupivacaine than bupivacaine. Am Surg. 2019;85(9):1013–6.
Hamel J-F, Joris J, Slim K, et al. Transversus abdominis block or wound infiltration should be performed in colorectal surgery patients in an enhanced recovery setting: a propensity score analysis of a national database. J Gastrointest Surg. 2023;27(4):798–802.
Ventham NT, O’Neill S, Johns N, et al. Evaluation of novel local anesthetic wound infiltration techniques for postoperative pain following colorectal resection surgery: a meta-analysis. Dis Colon Rectum. 2014;57(2):237–50.
Ren L, Qin P, Min S, et al. Transversus abdominis plane block versus local wound infiltration for postoperative pain after laparoscopic colorectal cancer resection: a randomized, double-blinded study. J Gastrointest Surg. 2022;26(2):425–32.
Rashid A, Gorissen KJ, Ris F, et al. No benefit of ultrasound-guided transversus abdominis plane blocks over wound infiltration with local anaesthetic in elective laparoscopic colonic surgery: results of a double-blind randomized controlled trial. Colorectal Dis. 2017;19(7):681–9.
Pedrazzani C, Menestrina N, Moro M, et al. Local wound infiltration plus transversus abdominis plane (TAP) block versus local wound infiltration in laparoscopic colorectal surgery and ERAS program. Surg Endosc. 2016;30(11):5117–25.
Pedrazzani C, Park SY, Conti C, et al. Analgesic efficacy of pre-emptive local wound infiltration plus laparoscopic-assisted transversus abdominis plane block versus wound infiltration in patients undergoing laparoscopic colorectal resection: results from a randomized, multicenter, single-blind, non-inferiority trial. Surg Endosc. 2021;35(7):3329–38.
Pedrazzani C, Park SY, Scotton G, et al. Analgesic efficacy of preemptive local wound infiltration plus laparoscopic-assisted transversus abdominis plane block versus wound infiltration in patients undergoing laparoscopic colorectal resection: study protocol for a randomized, multicenter, single-blind, noninferiority trial. Trials. 2019;20(1):391.
Li H, Chen R, Yang Z, et al. Comparison of the postoperative effect between epidural anesthesia and continuous wound infiltration on patients with open surgeries: a meta-analysis. J Clin Anesth. 2018;51:20–31.
Ren Y-F, Fu X, Wang Y-T, et al. Nalbuphine versus ketorolac as an adjuvant to local wound infiltration anesthesia in open colorectal surgery: a prospective randomized controlled study. Pain Ther. 2021;10(1):551–65.
Stamenkovic DM, Bezmarevic M, Bojic S, et al. Updates on wound infiltration use for postoperative pain management: a narrative review. J Clin Med. 2021;10(20):4659.
Helms JM. An overview of medical acupuncture. Altern Ther Health Med. 1998;4(3):35–45.
Shah S, Godhardt L, Spofford C. Acupuncture and postoperative pain reduction [J]. Curr Pain Headache Rep. 2022;26(6):453–8.
Ng S S M, Leung W W, Mak T W C, et al. Electroacupuncture reduces duration of postoperative ileus after laparoscopic surgery for colorectal cancer [J]. Gastroenterology, 2013, 144(2).
Ng SSM, Leung WW, Hon SSF, et al. Electroacupuncture for ileus after laparoscopic colorectal surgery: a randomised sham-controlled study [J]. Hong Kong Med J. 2013;19(Suppl 9):33–5.
Wang Y, Yang J-W, Yan S-Y, et al. Electroacupuncture vs sham electroacupuncture in the treatment of postoperative ileus after laparoscopic surgery for colorectal cancer: a multicenter randomized clinical trial. JAMA Surg. 2023;158(1):20–7.
Chen H-T, Hung K-C, Huang Y-T, et al. Efficacy of electroacupuncture in improving postoperative ileus in patients receiving colorectal surgery: a systematic review and meta-analysis. Int J Surg. 2024;110(2):1113–25.
Li W-j, Gao C, An L-X, et al. Perioperative transcutaneous electrical acupoint stimulation for improving postoperative gastrointestinal function: a randomized controlled trial. J Integr Med. 2021;19(3):211–8.
Zhang B, Xu F, Hu P, et al. Needleless transcutaneous electrical acustimulation: a pilot study evaluating improvement in post-operative recovery. Am J Gastroenterol. 2018;113(7):1026–35.
Fu C, Wu T, Shu Q, et al. Acupuncture therapy on postoperative nausea and vomiting in abdominal operation: a Bayesian network meta analysis. Medicine (Baltimore). 2020;99(23): e20301.
Huang W, Long W, Xiao J, et al. Effect of electrically stimulating acupoint, Zusanli (ST 36), on patient’s recovery after laparoscopic colorectal cancer resection: a randomized controlled trial. J Tradit Chin Med. 2019;39(3):433–9.
Li S, Jiang H, Liu W, et al. Transcutaneous electrical acupoint stimulation for the prevention of perioperative neurocognitive disorders in geriatric patients: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2022;101(50): e32329.
Langer R. Drug delivery and targeting. Nature. 1998;392(6679 Suppl):149.
Liechty WB, Kryscio DR, Slaughter BV, et al. Polymers for drug delivery systems. Annu Rev Chem Biomol Eng. 2010;1:149–73.
Tibbitt MW, Dahlman JE, Langer R. Emerging frontiers in drug delivery. J Am Chem Soc. 2016;138(3):704–17.
Momoh FU, Boateng JS, Richardson SCW, et al. Development and functional characterization of alginate dressing as potential protein delivery system for wound healing. Int J Biol Macromol. 2015;81:137–50.
Pandit A, Ashar R, Feldman D. The effect of TGF-beta delivered through a collagen scaffold on wound healing. J Invest Surg. 1999;12(2):89.
Jayakumar R, Prabaharan M, Sudheesh Kumar PT, et al. Biomaterials based on chitin and chitosan in wound dressing applications. Biotechnol Adv. 2011;29(3):322–37.
Li J, Mooney DJ. Designing hydrogels for controlled drug delivery. Nat Rev Mater. 2016;1(12):16071.
Westerling D. Rectally administered morphine: plasma concentrations in children premedicated with morphine in hydrogel and in solution. Acta Anaesthesiol Scand. 1985;29(7):653–6.
Guldbrand P, Mellström A. Rectal versus intramuscular morphine-scopolamine as premedication in children. Acta Anaesthesiol Scand. 1995;39(2):224–7.
Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606–17.
Helander EM, Menard BL, Harmon CM, et al. Multimodal analgesia, current concepts, and acute pain considerations. Curr Pain Headache Rep. 2017;21(1):3.
Gelman D, Gelmanas A, Urbanaitė D, et al. Role of multimodal analgesia in the evolving enhanced recovery after surgery pathways. Medicina (Kaunas). 2018;54(2):20.
Olmedo MV, Gálvez R, Vallecillo M. Double-blind parallel comparison of multiple doses of ketorolac, ketoprofen and placebo administered orally to patients with postoperative dental pain. Pain. 2001;90(1–2):135–41.
Wu M-H, Shih M-H, Hsu W-B, et al. Evaluation of a novel biodegradable thermosensitive keto-hydrogel for improving postoperative pain in a rat model. PLoS ONE. 2017;12(10):e0186784.
Zia MA, Sohail M, Minhas MU, et al. HEMA based pH-sensitive semi IPN microgels for oral delivery; a rationale approach for ketoprofen. Drug Dev Ind Pharm. 2020;46(2):272–82.
Peng F, Liu J, Zhang Y, et al. Designer self-assembling peptide nanofibers induce biomineralization of lidocaine for slow-release and prolonged analgesia. Acta Biomater. 2022;146:66–79.
Chen S, Yao W, Wang H, et al. Injectable electrospun fiber-hydrogel composite sequentially releasing clonidine and ropivacaine for prolonged and walking regional analgesia. Theranostics. 2022;12(11):4904–21.
Zhang W, Xu W, Ning C, et al. Long-acting hydrogel/microsphere composite sequentially releases dexmedetomidine and bupivacaine for prolonged synergistic analgesia. Biomaterials. 2018;181:378–91.
Indermun S, Choonara YE, Kumar P, et al. In vitro and in vivo evaluation of a hydrogel-based microneedle device for transdermal electro-modulated analgesia. J Pharm Sci. 2017;106(4):1111–6.
Saher T, Manzoor R, Abbas K, et al. Analgesic and anti-inflammatory properties of two hydrogel formulations comprising polyherbal extract. J Pain Res. 2022;15:1203–19.
Ma Z, Song W, He Y, et al. Multilayer injectable hydrogel system sequentially delivers bioactive substances for each wound healing stage. ACS Appl Mater Interfaces. 2020;12(26):29787–806.
Hou Y, Li Y, Li Y, et al. Tuning water-resistant networks in mussel-inspired hydrogels for robust wet tissue and bioelectronic adhesion. ACS Nano. 2023;17(3):2745–60.
Tong YCI, Kaye AD, Urman RD. Liposomal bupivacaine and clinical outcomes. Best Pract Res Clin Anaesthesiol. 2014;28(1):15–27.
Zhang L, Wang J, Chi H, et al. Local anesthetic lidocaine delivery system: chitosan and hyaluronic acid-modified layer-by-layer lipid nanoparticles. Drug Deliv. 2016;23(9):3529–37.
Wang J, Zhang L, Chi H, et al. An alternative choice of lidocaine-loaded liposomes: lidocaine-loaded lipid-polymer hybrid nanoparticles for local anesthetic therapy. Drug Deliv. 2016;23(4):1254–60.
Makadia HK, Siegel SJ. Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers (Basel). 2011;3(3):1377–97.
Moraes CM, de Matos AP, de Lima R, et al. Initial development and characterization of PLGA nanospheres containing ropivacaine. J Biol Phys. 2007;33(5–6):455–61.
Gao X, Zhu P, Yu L, et al. Ultrasound/acidity-triggered and nanoparticle-enabled analgesia. Adv Healthc Mater. 2019;8(9): e1801350.
Liu L, Yao W, Xie X, et al. pH-sensitive dual drug loaded janus nanoparticles by oral delivery for multimodal analgesia. J Nanobiotechnol. 2021;19(1):235.
Funding
This work was supported by the National Key Research and Development Program of China (Grant No. 2018YFC2001802), National Natural Science Foundation of China (Grant No. 82071251), Open Foundation of Hubei Key Laboratory of Regenerative Medicine and Multi-disciplinary Translational Research (Grant No. 2022zsyx008), Program of the Scientific and Technological in Guiyang City (Grant No. Zhu Ke He [2020]-16–5), the Science and Technology Talents Growth Project in Education Department of Guizhou Province (Grant No. Qian Jiao He KY Zi [2021]4Y211). The Rapid Service Fee will be paid by the authors.
Author information
Authors and Affiliations
Contributions
Li Huang and Tianhao Zhang contributed substantially to the article concept and manuscript writing. Xiangdong Chen and Daan Fu revised and approved the final version before submission. All the listed authors have participated actively in the study and have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
All of the authors (Li Huang, Tianhao Zhang, Kaixin Wang, Bingcheng Chang, Daan Fu, Xiangdong Cheng) — declare that they have no competing interests.
Ethical Approval
This review article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Huang, L., Zhang, T., Wang, K. et al. Postoperative Multimodal Analgesia Strategy for Enhanced Recovery After Surgery in Elderly Colorectal Cancer Patients. Pain Ther 13, 745–766 (2024). https://doi.org/10.1007/s40122-024-00619-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-024-00619-0