Abstract
Background
We hypothesized that administration of IV acetaminophen alone would reduce the opioid consumption in post-operative colorectal surgery and reduce the side effects of narcotics.
Methods
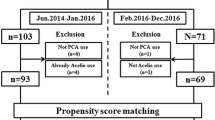
Patients were randomized to receive either IV acetaminophen or placebo in addition to opioid PCA. Primary endpoints evaluated were opioid consumption and pain visual analogue scale score (PVASS) during first 48 h post-operatively. Secondary endpoints evaluated were time of return of GI function (ROGIF), time to diet ordered (TTDO), length of hospital stay (LOHS), and occurrence of ileus.
Results
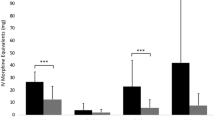
105 patients were enrolled and 97 remained in the study after exclusion (control group n = 50; study group n = 47). Mean ± SEs of opioid consumption in the study group was 21.5 ± 1.8 mg of morphine equivalent (ME) and 35.0 ± 3.3 mg ME at 24 and 48 h, respectively, versus 36.4 ± 4.1 mg ME and 59.7 ± 6.7 mg ME in the control group (p = 0.002 and 0.002). PVASS levels were lower in the study group at all intervals at 3, 8, 24, and 48 h (p = 0.02, 0.006, < 0.01, and 0.02). ROGIF, TTDO, and LOHS were also found to be lower in the study group (p ≤ 0.01, < 0.01, and 0.002). The rate of ileus was reduced by using IV acetaminophen (22% vs 2.1%; p = 0.004).
Conclusions
IV acetaminophen helps to reduce opioid consumption for patients undergoing colorectal surgery. Additionally, there appears to be a shortened length of hospital stay, better pain control, reduced time to return of bowel function, and lower rate of post-operative ileus in patients receiving IV acetaminophen.




Similar content being viewed by others
References
Bertolini A, Ferrari A, Ottani A, Guerzoni S, Tacchi R, Leone S (2006) Paracetamol: new vistas of an old drug. CNS Drug Rev 12(3–4):250–275
Gorocs TS, Lambert M, Rinne T, Krekler M, Modell S (2009) Efficacy and tolerability of ready-to-use intravenous paracetamol solution as monotherapy or as an adjunct analgesic therapy for postoperative pain in patients undergoing elective ambulatory surgery: open, prospective study. Int J Clin Pract 63(1):112–120
Yeh YC, Reddy P (2012) Clinical and economic evidence for intravenous acetaminophen. Pharmacotherapy 32(6):559–579
Arici S, Gurbet A, Turker G, Yavascaoglu B, Sahin S (2009) Preemptive analgesic effects of intravenous paracetamol in total abdominal hysterectomy. Agri 21(2):54–61
Cattabriga I, Pacini D, Lamazza G, Talarico F, Di Bartolomeo R, Grillone G et al (2007) Intravenous paracetamol as adjunctive treatment for postoperative pain after cardiac surgery: a double blind randomized controlled trial. Eur J Cardiothorac Surg 32(3):527–531
Eremenko AA, Kuslieva EV (2008) Analgesic and opioid-sparing effects of intravenous paracetamol in the early period after aortocoronary bypass surgery. Anesteziol Reanimatol 5(5):11–14
Moon YE, Lee YK, Lee J, Moon DE (2011) The effects of preoperative intravenous acetaminophen in patients undergoing abdominal hysterectomy. Arch Gynecol Obstet 284(6):1455–1460
Salihoglu Z, Yildirim M, Demiroluk S, Kaya G, Karatas A, Ertem M et al (2009) Evaluation of intravenous paracetamol administration on postoperative pain and recovery characteristics in patients undergoing laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 19(4):321–323
Toms L, McQuay HJ, Derry S, Moore RA (2008) Single dose oral paracetamol (acetaminophen) for postoperative pain in adults. Cochrane Database Syst Rev 8(4):CD004602
Tzortzopoulou A, McNicol ED, Cepeda MS, Francia MB, Farhat T, Schumann R (2011) Single dose intravenous propacetamol or intravenous paracetamol for postoperative pain. Cochrane Database Syst Rev 5(10):CD007126
Zafar N, Davies R, Greenslade GL, Dixon AR (2010) The evolution of analgesia in an ‘accelerated’ recovery programme for resectional laparoscopic colorectal surgery with anastomosis. Colorectal Dis 12(2):119–124
Jahr JS, Lee VK (2010) Intravenous acetaminophen. Anesthesiol Clin 28(4):619–645
Abramowicz M (ed) (2011) Intravenous acetaminophen (Ofirmev). Med Lett Drugs Ther 53(1362):26–28
Baley K, Michalov K, Kossick MA, McDowell M (2014 Feb) Intravenous acetaminophen and intravenous ketorolac for management of pediatric surgical pain: a literature review. AANA J 82(1):53–64
Barden J, Edwards J, Moore A, McQuay H (2004) Single dose oral paracetamol (acetaminophen) for postoperative pain. Cochrane Database Syst Rev 1(1):CD004602
Fayaz MK, Abel RJ, Pugh SC, Hall JE, Djaiani G, Mecklenburgh JS (2004) Opioid-sparing effects of diclofenac and paracetamol lead to improved outcomes after cardiac surgery. J Cardiothorac Vasc Anesth 18(6):742–747
Hernandez-Palazon J, Tortosa JA, Martinez-Lage JF, Perez-Flores D (2001) Intravenous administration of propacetamol reduces morphine consumption after spinal fusion surgery. Anesth Analg 92(6):1473–1476
Iorno V, Landi L, Di Pasquale R, Cicenia S, Moschini V (2013) Comparison of intravenous ketorolac with or without paracetamol in postoperative pain control following ambulatory surgery. Curr Med Res Opin 29(12):1685–1690
Olonisakin RP, Amanor-Boadu SD, Akinyemi AO (2012) Morphine-sparing effect of intravenous paracetamol for post operative pain management following gynaecological surgery. Afr J Med Med Sci 41(4):429–436
Pettersson PH, Jakobsson J, Owall A (2005) Intravenous acetaminophen reduced the use of opioids compared with oral administration after coronary artery bypass grafting. J Cardiothorac Vasc Anesth 19(3):306–309
Sinatra RS, Jahr JS, Reynolds LW, Viscusi ER, Groudine SB, Payen-Champenois C (2005) Efficacy and safety of single and repeated administration of 1 gram intravenous acetaminophen injection (paracetamol) for pain management after major orthopedic surgery. Anesthesiology 102(4):822–831
Wininger SJ, Miller H, Minkowitz HS, Royal MA, Ang RY, Breitmeyer JB et al (2010) A randomized, double-blind, placebo-controlled, multicenter, repeat-dose study of two intravenous acetaminophen dosing regimens for the treatment of pain after abdominal laparoscopic surgery. ClinTher 32(14):2348–2369
Joshi GP, Bonnet F, Kehlet H (2013) Evidence-based postoperative pain management after laparoscopic colorectal surgery. Colorectal Dis 15(2):146–155
Iyer S, Saunders WB, Stemkowski S (2009) Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm 15(6):485–494
Brett CN, Barnett SG, Pearson J (2012) Postoperative plasma paracetamol levels following oral or intravenous paracetamol administration: a double-blind randomised controlled trial. Anaesth Intensive Care 40(1):166–171
Bauer AJ, Sarr MG, Szurszewski JH (1991) Opioids inhibit neuromuscular transmission in circular muscle of human and baboon jejunum. Gastroenterology 202(4):970–976
van der Westhuizen J, Kuo PY, Reed PW, Holder K (2011) Randomised controlled trial comparing oral and intravenous paracetamol (acetaminophen) plasma levels when given as preoperative analgesia. Anaesth Intensive Care 39(2):242–246
HolmerPettersson P, Owall A, Jakobsson J (2004) Early bioavailability of paracetamol after oral or intravenous administration. Acta Anaesthesiol Scand 48(7):867–870
Acknowledgements
Contributors Recognition: Scott Hobler MD, Thomas L Husted MD, Shyam Allamaneni MD—Department of Surgery, The Jewish Hospital-Mercy Health, Cincinnati, OH, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Amir H. Aryaie, Sepehr Lalezari, Wallace K Sergent, Yana Puckett, Christopher Juergens, Craig Ratermann, and Cari Ogg have no conflicts of interest or financial ties to disclose.
Appendix A
Appendix A
Inclusion criteria
-
Patient undergoing colorectal operation (Hartmann’s procedure, sigmoidectomy, left hemicolectomy, right hemicolectomy, transverse colectomy, ileocecectomy, colo-colonic anastomosis, colorectal anastomosis, ileocolonic anastomosis, low anterior resection, or abdominoperineal resection)
-
Age range from 18 to 89 years old
-
Patient demonstrating that they understood the information on the consent form and providing signed, written informed consent before participation in the study.
Exclusion criteria
-
Patient younger than 18 years old or older than 89 years old
-
Patient or family unable to give consent
-
Patients who use opioids or tramadol daily for > 7 days before study medication administration (patient who, in the investigator’s opinion, had or was developing opioid tolerance)
-
Patients who had a chronic pain condition or any significant medical disease, laboratory abnormality, or condition that, in the investigator’s judgment, could have compromised the subject’s welfare, ability to communicate with the study staff, complete study activities, or otherwise restricted study participation
-
Patient who had hypersensitivity to opioids, acetaminophen, or the inactive ingredients of the study medication
-
Patients who had known or suspected history of alcohol or drug abuse or dependence within the previous 1 year
-
Patients who had impaired liver function
-
Patients who had fever within first 48 h post-operatively and required acetaminophen for fever reduction.
Rights and permissions
About this article
Cite this article
Aryaie, A.H., Lalezari, S., Sergent, W.K. et al. Decreased opioid consumption and enhance recovery with the addition of IV Acetaminophen in colorectal patients: a prospective, multi-institutional, randomized, double-blinded, placebo-controlled study (DOCIVA study). Surg Endosc 32, 3432–3438 (2018). https://doi.org/10.1007/s00464-018-6062-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6062-y