Abstract
Purpose
Surgery remains the mainstay of treatment for potentially curable colon cancer. Otherwise, the surgical stress response might increase the likelihood of cancer dissemination during and after cancer surgery. There is growing evidence that the type of anaesthesia during cancer surgery plays a role in the metastatic process. Therefore, we assessed if the method of anaesthesia is associated with long-term survival after colon cancer surgery.
Method
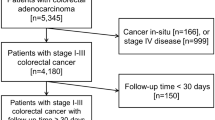
A retrospective single-centre study was conducted including 588 patients who underwent colorectal cancer surgery, TNM stage I–IV, in the Jeroen Bosch Hospital between 1995 and 2003. The Cox proportional hazard model was used for statistical analysis. Adjustments were made for age, sex, comorbidity, TNM stage, chemotherapy, emergency surgery status and year of incidence.
Results
Of the 588 primary colon cancer patients with a median age of 70 years, 399 (68 %) patients underwent colon surgery with epidural anaesthesia, whilst 189 (32 %) patients were operated without epidural anaesthesia. Five-year survival for patients not receiving epidural analgesia was 42 % versus 51 % for patients receiving epidural analgesia (p = 0.03). This effect remained after adjustment for relevant patient, tumour, and treatment characteristics (hazard ratio (HR) 1.30 (95 % confidence interval (CI) 1.05–1.59), p = 0.01). Subgroup analysis in patients of 80 years and older (n = 100) showed also a better overall survival after receiving epidural analgesia (HR 1.74 (95 % CI 1.11–2.72), p = 0.01).
Conclusion
Epidural analgesia during colon cancer surgery was associated with a better overall survival. Prospective trials evaluating the effects of locoregional analgesia on colon cancer recurrence are warranted.

Similar content being viewed by others
References
Paget S (1889) The distribution of secondary growths in cancer of the breast. Lancet 571–573
Denis MG, Lipart C, Leborgne J, LeHur PA, Galmiche JP, Denis M, Ruud E, Truchaud A, Lustenberger P (1997) Detection of disseminated tumor cells in peripheral blood of colorectal cancer patients. Int J Cancer 74:540–544
Shakhar G, Ben-Eliyahu S (2003) Potential prophylactic measures against postoperative immunosuppression: could they reduce recurrence rates in oncological patients? Ann Surg Oncol 10:972–992
Snyder GL, Greenberg S (2010) Effect of anaesthetic technique and other perioperative factors on cancer recurrence. Br J Anaesth 105:106–115
Ahlers O, Nachtigall I, Lenze J, Goldmann A, Schulte E, Hohne C, Fritz G, Keh D (2008) Intraoperative thoracic epidural anaesthesia attenuates stress-induced immunosuppression in patients undergoing major abdominal surgery. Br J Anaesth 101:781–787
Ben Eliyahu S (2002) The price of anticancer intervention. Does surgery promote metastasis? Lancet Oncol 3:578–579
Biki B, Mascha E, Moriarty DC, Fitzpatrick JM, Sessler DI, Buggy DJ (2008) Anesthetic technique for radical prostatectomy surgery affects cancer recurrence: a retrospective analysis. Anesthesiology 109:180–187
Exadaktylos AK, Buggy DJ, Moriarty DC, Mascha E, Sessler DI (2006) Can anesthetic technique for primary breast cancer surgery affect recurrence or metastasis? Anesthesiology 105:660–664
Tsui BC, Rashiq S, Schopflocher D, Murtha A, Broemling S, Pillay J, Finucane BT (2010) Epidural anesthesia and cancer recurrence rates after radical prostatectomy. Can J Anaesth 57:107–112
Lin L, Liu C, Tan H, Ouyang H, Zhang Y, Zeng W (2011) Anaesthetic technique may affect prognosis for ovarian serous adenocarcinoma: a retrospective analysis. Br J Anaesth 106:814–822
Christopherson R, James KE, Tableman M, Marshall P, Johnson FE (2008) Long-term survival after colon cancer surgery: a variation associated with choice of anesthesia. Anesth Analg 107:325–332
Gottschalk A, Ford JG, Regelin CC, You J, Mascha EJ, Sessler DI, Durieux ME, Nemergut EC (2010) Association between epidural analgesia and cancer recurrence after colorectal cancer surgery. Anesthesiology 113:27–34
Gupta A, Bjornsson A, Fredriksson M, Hallbook O, Eintrei C (2011) Reduction in mortality after epidural anaesthesia and analgesia in patients undergoing rectal but not colonic cancer surgery: a retrospective analysis of data from 655 patients in central Sweden. Br J Anaesth 107:164–170
Myles PS, Peyton P, Silbert B, Hunt J, Rigg JR, Sessler DI (2011) Perioperative epidural analgesia for major abdominal surgery for cancer and recurrence-free survival: randomised trial. BMJ 342:d1491
Wada H, Seki S, Takahashi T, Kawarabayashi N, Higuchi H, Habu Y, Sugahara S, Kazama T (2007) Combined spinal and general anesthesia attenuates liver metastasis by preserving TH1/TH2 cytokine balance. Anesthesiology 106:499–506
Bar-Yosef S, Melamed R, Page GG, Shakhar G, Shakhar K, Ben Eliyahu S (2001) Attenuation of the tumor-promoting effect of surgery by spinal blockade in rats. Anesthesiology 94:1066–1073
Ben Eliyahu S, Shakhar G, Rosenne E, Levinson Y, Beilin B (1999) Hypothermia in barbiturate-anesthetized rats suppresses natural killer cell activity and compromises resistance to tumor metastasis: a role for adrenergic mechanisms. Anesthesiology 91:732–740
O'Riain SC, Buggy DJ, Kerin MJ, Watson RW, Moriarty DC (2005) Inhibition of the stress response to breast cancer surgery by regional anesthesia and analgesia does not affect vascular endothelial growth factor and prostaglandin E2. Anesth Analg 100:244–249
Moller JF, Nikolajsen L, Rodt SA, Ronning H, Carlsson PS (2007) Thoracic paravertebral block for breast cancer surgery: a randomized double-blind study. Anesth Analg 105:1848–51, table
Yeager MP, Colacchio TA, Yu CT, Hildebrandt L, Howell AL, Weiss J, Guyre PM (1995) Morphine inhibits spontaneous and cytokine-enhanced natural killer cell cytotoxicity in volunteers. Anesthesiology 83:500–508
Gottschalk A, Sharma S, Ford J, Durieux ME, Tiouririne M (2010) Review article: the role of the perioperative period in recurrence after cancer surgery. Anesth Analg 110:1636–1643
Brittenden J, Heys SD, Ross J, Eremin O (1996) Natural killer cells and cancer. Cancer 77:1226–1243
Marret E, Remy C, Bonnet F (2007) Meta-analysis of epidural analgesia versus parenteral opioid analgesia after colorectal surgery. Br J Surg 94:665–673
Zafar N, Davies R, Greenslade GL, Dixon AR (2010) The evolution of analgesia in an 'accelerated' recovery programme for resectional laparoscopic colorectal surgery with anastomosis. Color Dis 12:119–124
Acknowledgments
The author wishes to thank Esther van den Broek, MSc, and Jorien M. Willems MD, PhD for their support with the statistical analysis and for critically reading the manuscript.
Conflict of interest
None declared.
Disclosures
None.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vogelaar, F.J., Abegg, R., van der Linden, J.C. et al. Epidural analgesia associated with better survival in colon cancer. Int J Colorectal Dis 30, 1103–1107 (2015). https://doi.org/10.1007/s00384-015-2224-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-015-2224-8



