Abstract
Background
The efficacy of transversus abdominis plane (TAP) block compared with thoracic epidural analgesia (TEA) in abdominal surgery has been controversial. We conducted this systematic review and meta-analysis to assess outcomes of TAP block and TEA in a procedure-specific manner in colorectal surgery.
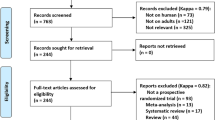
Methods
A systematic literature search of the PubMed, Embase, Cochrane Library, and Scopus databases was conducted through July 10, 2020, to identify randomized controlled trials (RCTs) comparing TAP block with TEA in colorectal surgery. Primary outcomes were pain scores at rest and movement at 24 h postoperatively. Secondary outcomes included postoperative pain scores at 0–2 and 48 h, opioid consumption, postoperative nausea and vomiting (PONV), functional recovery, hospital stay, and adverse events.
Results
Six RCTs with 568 patients were included. Methodological quality of these RCTs ranged from moderate to high. TAP block provided comparable pain control, lower 24 h and total opioid consumption, shorter time to ambulation and urinary catheter time, and lower incidence of sensory disturbance and postoperative hypotension compared with TEA. Meanwhile, the 48-h opioid consumption, PONV incidence, and hospital stay were similar between groups. When laparoscopic surgery was the only surgical approach employed, TAP block provided additional benefits of shorter time to first flatus and lower incidence of PONV compared with TEA.
Conclusions
Perhaps more germane to minimally invasive procedures, TAP block is equivalent to TEA in terms of postoperative pain control and provides better functional recovery with lower incidence of adverse events in patients undergoing colorectal surgery.



Similar content being viewed by others
References
Carmichael JC, Keller DS, Baldini G, Bordeianou L, Weiss E, Lee L, Boutros M, McClane J, Feldman LS, Steele SR (2017) Clinical practice guidelines for enhanced recovery after colon and rectal surgery from the American Society of Colon and Rectal Surgeons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis Colon Rectum 60:761–784. https://doi.org/10.1097/DCR.0000000000000883
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, Rockall TA, Young-Fadok TM, Hill AG, Soop M, de Boer HD, Urman RD, Chang GJ, Fichera A, Kessler H, Grass F, Whang EE, Fawcett WJ, Carli F, Lobo DN, Rollins KE, Balfour A, Baldini G, Riedel B, Ljungqvist O (2019) Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS) society recommendations: 2018. World J Surg 43:659–695. https://doi.org/10.1007/s00268-018-4844-y
Wick EC, Grant MC, Wu CL (2017) Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg 152:691–697. https://doi.org/10.1001/jamasurg.2017.0898
Werawatganon T, Charuluxanun S (2005) Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev 1:CD004088. https://doi.org/10.1002/14651858.CD004088.pub2
Joshi GP, Bonnet F, Kehlet H, PROSPECT collaboration (2013) Evidence-based postoperative pain management after laparoscopic colorectal surgery. Color Dis 15:146–155. https://doi.org/10.1111/j.1463-1318.2012.03062.x
Peltrini R, Cantoni V, Green R, Greco PA, Calabria M, Bucci L, Corcione F (2020) Efficacy of transversus abdominis plane (TAP) block in colorectal surgery: a systematic review and meta-analysis. Tech Coloproctol 24:787–802. https://doi.org/10.1007/s10151-020-02206-9
Qin C, Liu Y, Xiong J, Wang X, Dong Q, Su T, Liu J (2020) The analgesic efficacy compared ultrasound-guided continuous transverse abdominis plane block with epidural analgesia following abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol 20:52. https://doi.org/10.1186/s12871-020-00969-0
Desai N, El-Boghdadly K, Albrecht E (2020) Epidural vs. Transversus abdominis plane block for abdominal surgery - a systematic review, meta-analysis and trial sequential analysis. Anaesthesia. https://doi.org/10.1111/anae.15068
Baeriswyl M, Zeiter F, Piubellini D, Kirkham KR, Albrecht E (2018) The analgesic efficacy of transverse abdominis plane block versus epidural analgesia: a systematic review with meta-analysis. Medicine (Baltimore) 97:e11261. https://doi.org/10.1097/MD.0000000000011261
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Goossen K, Tenckhoff S, Probst P, Grummich K, Mihaljevic AL, Büchler MW, Diener MK (2018) Optimal literature search for systematic reviews in surgery. Langenbeck's Arch Surg 403:119–129. https://doi.org/10.1007/s00423-017-1646-x
Higgins JP, Green S (eds) Cochrane handbook for systematic reviews of interventions Version 5.1.0. [updated March 2011]. Available at: www.handbook.cochrane.org. Accessed July 12, 2020
Myles PS, Myles DB, Galagher W, Boyd D, Chew C, MacDonald N, Dennis A (2017) Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth 118:424–429. https://doi.org/10.1093/bja/aew466
Macintyre PE, Schug SA (2015) Pharmacology of opioids. In: Macintyre PE, Schug SA (eds) Acute pain management: a practical guide, 4th edn. CRC Press, Boca Raton, pp 29–51
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14:135. https://doi.org/10.1186/1471-2288-14-135
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Egger M, Davey SG, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple graphical test. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Niraj G, Kelkar A, Hart E, Horst C, Malik D, Yeow C, Singh B, Chaudhri S (2014) Comparison of analgesic efficacy of four-quadrant transversus abdominis plane (TAP) block and continuous posterior TAP analgesia with epidural analgesia in patients undergoing laparoscopic colorectal surgery: an open-label, randomized, non-inferiority trial. Anaesthesia 69:348–355. https://doi.org/10.1111/anae.12546
Qin CS, Lin YN, Liu JC (2016) Clinical study of ultrasound-guided continuous transversus abdominis plane block on the efficacy of postoperative analgesia in patients undergoing laparoscopic colorectal surgery. J Minim Invas Med 11:664–668. https://doi.org/10.11864/j.issn.1673.2016.05.02
Dai Y, Sun XD, Liu JC (2017) A comparative study of the analgesic effect of transverse abdominal block and thoracic epidural block after colorectal surgery. J Guangxi Med Univ 34:1213–1216. https://doi.org/10.16190/j.cnki.45-1211/r.2017.08.027
Xu YJ, Sun X, Jiang H, Yin YH, Weng ML, Sun ZR, Chen WK, Miao CH (2020) Randomized clinical trial of continuous transversus abdominis plane block, epidural or patient-controlled analgesia for patients undergoing laparoscopic colorectal cancer surgery. Br J Surg 107:e133–e141. https://doi.org/10.1002/bjs.11403
Torgeson M, Kileny J, Pfeifer C, Narkiewicz L, Obi S (2018) Conventional epidural vs transversus abdominis plane block with liposomal bupivacaine: a randomized trial in colorectal surgery. J Am Coll Surg 227:78–83. https://doi.org/10.1016/j.jamcollsurg.2018.04.021
Felling DR, Jackson MW, Ferraro J, Battaglia MA, Albright JJ, Wu J, Genord CK, Brockhaus KK, Bhave RA, McClure AM, Shanker BA, Cleary RK (2018) Liposomal bupivacaine transversus abdominis plane block versus epidural analgesia in a colon and rectal surgery enhanced recovery pathway: a randomized clinical trial. Dis Colon Rectum 61:1196–1204. https://doi.org/10.1097/DCR.0000000000001211
Park SY, Park JS, Choi GS, Kim HJ, Moon S (2017) Yeo J (2017) comparison of analgesic efficacy of laparoscope-assisted and ultrasound guided transversus abdominis plane block after laparoscopic colorectal operation: a randomized, single-blind, non-inferiority trial. J Am Coll Surg 225:403–410. https://doi.org/10.1016/j.jamcollsurg.2017.05.017
Jurt J, Hubner M, Pache B, Hahnloser D, Demartines N, Grass F (2018) Respiratory complications after colorectal surgery: avoidable or fate? World J Surg 42:2708–2714. https://doi.org/10.1007/s00268-018-4699-2
Hughes MJ, Harrison EM, Peel NJ, Stutchfield B, McNally S, Beattie C, Wigmore SJ (2015) Randomized clinical trial of perioperative nerve block and continuous local anaesthetic infiltration via wound catheter versus epidural analgesia in open liver resection (LIVER 2 trial). Br J Surg 102:1619–1628. https://doi.org/10.1002/bjs.9949
Revie EJ, McKeown DW, Wilson JA, Garden OJ, Wigmore SJ (2012) Randomized clinical trial of local infiltration plus patient controlled opiate analgesia vs. epidural analgesia following liver resection surgery. HPB (Oxford) 14:611–618. https://doi.org/10.1111/j.1477-2574.2012.00490.x
Shaker TM, Carroll JT, Chung MH, Koehler TJ, Lane BR, Wolf AM, Wright GP (2018) Efficacy and safety of transversus abdominis plane blocks versus thoracic epidural anesthesia in patients undergoing major abdominal oncologic resections: a prospective, randomized controlled trial. Am J Surg 215:498–501. https://doi.org/10.1016/j.amjsurg.2017.10.055
Yeap YL, Wolfe JW, Kroepfl E, Fridell J, Powelson JA (2020) Transversus abdominis plane (TAP) block for laparoscopic live donor nephrectomy: continuous catheter infusion provides no additional analgesic benefit over single-injection ropivacaine. Clin Transpl 34:e13861. https://doi.org/10.1111/ctr.13861
Choi YM, Byeon GJ, Park SJ, Ok YM, Shin SW, Yang K (2017) Postoperative analgesic efficacy of single-shot and continuous transversus abdominis plane block after laparoscopic cholecystectomy: a randomized controlled clinical trial. J Clin Anesth 39:146–151. https://doi.org/10.1016/j.jclinane.2017.03.050
Hutchins J, Delaney D, Vogel RI, Ghebre RG, Downs LS Jr, Carson L, Mullany S, Teoh D, Geller MA (2015) Ultrasound guided subcostal transversus abdominis plane (TAP) infiltration with liposomal bupivacaine for patients undergoing robotic assisted hysterectomy: a prospective randomized controlled study. Gynecol Oncol 138:609–613. https://doi.org/10.1016/j.ygyno.2015.06.008
Hutchins JL, Kesha R, Blanco F, Dunn T, Hochhalter R (2016) Ultrasound-guided subcostal transversus abdominis plane blocks with liposomal bupivacaine vs. non-liposomal bupivacaine for postoperative pain control after laparoscopic hand-assisted donor nephrectomy: a prospective randomised observer-blinded study. Anaesthesia 71:930–937. https://doi.org/10.1111/anae.13502
Wong KA, Cabrera AG, Argiroff AL, Pechman DM, Parides MK, Vazzana JT, Moran-Atkin EM, Choi JJ, Camacho DR (2020) Transversus abdominis plane block with liposomal bupivacaine and its effect on opiate use after weight loss surgery: a randomized controlled trial. Surg Obes Relat Dis 16:886–893. https://doi.org/10.1016/j.soard.2020.03.031
Hamid HKS, Emile SH, Saber AA, Ruiz-Tovar J, Minas V, Cataldo TE (2020) Laparoscopic-guided transversus abdominis plane block for postoperative pain management in minimally invasive surgery: a systematic review and meta-analysis. J Am Coll Surg 231:376–386.e15. https://doi.org/10.1016/j.jamcollsurg.2020.05.020
Babazade R, Saasouh W, Naylor AJ, Makarova N, Udeh CI, Turan A, Udeh BL (2019) The cost-effectiveness of epidural, patient-controlled intravenous opioid analgesia, or transversus abdominis plane infiltration with liposomal bupivacaine for postoperative pain management. J Clin Anesth 53:56–63. https://doi.org/10.1016/j.jclinane.2018.10.003
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Hytham Hamid, Artur Hernandez, and Alan Saber. The first draft of the manuscript was written by Hytham Hamid and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Ethical approval for this kind of studies (systematic review) was not required.
Informed consent
Informed consent is not required for this kind of studies (systematic review).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 187 kb).
Rights and permissions
About this article
Cite this article
Hamid, H.K.S., Marc-Hernández, A. & Saber, A.A. Transversus abdominis plane block versus thoracic epidural analgesia in colorectal surgery: a systematic review and meta-analysis. Langenbecks Arch Surg 406, 273–282 (2021). https://doi.org/10.1007/s00423-020-01995-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01995-9