Abstract
Background
Multimodal analgesia protocols are becoming a common part of enhanced recovery pathways after colorectal surgery. However, few protocols include a robust intraoperative component in addition to pre-operative and post-operative analgesics.
Method
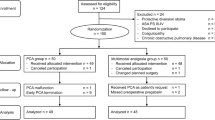
A prospective cohort study was performed in an urban teaching hospital in patients undergoing minimally invasive colorectal surgery before and after implementation of a multimodal analgesia protocol consisting of pre-operative (gabapentin, acetaminophen, celecoxib), intraoperative (lidocaine and magnesium infusions, ketorolac, transversus abdominis plane block), and post-operative (gabapentin, acetaminophen, celecoxib) opioid-sparing elements. The main outcome measure was use of morphine equivalents in the first 24-h post-operative period.
Results
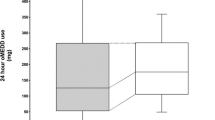
The study cohort (n = 71) included 41 patients before and 30 patients after implementation of a multimodal analgesia protocol. Mean age of the entire study cohort was 47 ± 19.7 years and 46% were male. Patients undergoing surgery post-multimodal analgesia vs. pre-multimodal analgesia had significantly lower use of IV morphine equivalents in first 24-h post-operative period (5.8 ± 6.4 mg vs. 22.8 ± 21.3 mg; p = 0.005) and first 48-h post-operative period (7.6 ± 9.4 mg vs. 42 ± 52.9 mg; p = 0.0008). This reduction in IV morphine equivalent use post-multimodal analgesia was coupled with improved pain scores in the post-operative period. Post-operative hospital length of stay, post-operative ileus, and overall complications were not significantly different between groups.
Conclusions
Multimodal analgesia incorporating pre-operative, intraoperative, and post-operative opioid-sparing agents is an effective method for reducing perioperative opioid utilization and pain after minimally invasive colorectal surgery.


Similar content being viewed by others
References
Carmichael JC, Keller DS, Baldini G, Bordeianou L, Weiss E, Lee L, Boutros M, McClane J, Feldman LS, Steele SR. (2017) Clinical practice guidelines for enhanced recovery after colon and rectal surgery from the American Society of Colon and Rectal Surgeons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis Colon Rectum. 60:761–784.
Wick EC, Grant MC, Wu CL. (2017) Postoperative multimodal analgesia pain management with an opioid analgesics and techniques: A review. JAMA Surg. 152:691–697.
Helander EM, Webb MP, Bias M, Whang EE, Kaye AD, Urman RD. (2017) A comparison of multimodal analgesic approaches in institutional enhanced recovery after surgery protocols for colorectal surgery: Pharmacological agents. J Laparoendosc Adv Surg Tech A. 9:903–908.
Joshi GP, Bonnet F, Kehlet H; PROSPECT collaboration. (2013) Evidence-based postoperative pain management after laparoscopic colorectal surgery. Colorectal Dis. 2:146–155.
Shaffer EE, Pham A, Woldman RL, Spiegelman A, Strassels SA Wan GJ. (2016) Estimating the effect of intravenous acetaminophen for postoperative pain management on length of stay in inpatient hospital costs. Advances in Therapy. 33:2211–2228.
Hickamn SR, Mathieson KM, Bradford LM, Garman CD, Gregg RW, Lukens DW. (2018) Randomized trial of oral versus intravenous acetaminophen for postoperative pain control. Am J Health Syst Pharm. 75:367–375.
Chen JY, Wu GJ, Mok MS, Chou YH, Sun WZ, Chen PL, Chan WS, Yien HW, Wen YR. (2005) Effect of adding ketorolac to intravenous morphine patient-controlled analgesia on bowel function in colorectal surgery patients—a prospective, randomized, double-blind study. Acta Anaesthesiol Scand. 49:546–551.
Arumugam S, Lau CS, Chamberlain RS. (2016) Use of preoperative gabapentin significantly reduces postoperative opioid consumption: a meta-analysis. J Pain Res. 9:631–640.
Yu N, Long X, Lujan-Hernandez JR, Succar J, Xin X, Wang X. (2014) Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 14:121.
Oh TK, Lee SJ, Do SH, Song IA. (2018) Transversus abdominis plane block using a short-acting anesthetic for postoperative pain after laparoscopic colorectal surgery: A systematic review and meta-analysis. Surg Endosc. 32(2):545–552.
Tikuisis R, Miliauskas P, Samalvicius NE, Zurauskas A, Samalavicius R, Zabulis V. (2014) Intravenous lidocaine for postoperative pain relief after hand-assisted laparoscopic colon surgery: A randomized, placebo-controlled trial. Tech Coloproctol. 18:373–380.
Herroeder S, Pecher S, Schonherr ME, Kaulitz G, Hahnenkamp K, Friess H, Bottiger BW, Bauer H, Dijkgraaf MG, Durieux ME, Hollmann MW. (2007) Systemic lidocaine shortens length of hospital stay after colorectal surgery: A double-blinded, randomized, placebo-controlled trial. Ann Surg. 246:192–200.
Shariat Mohararai R, Motalebi M, Najafi A, Zamani MM, Imani F, Etezadi F, Pourfakr P, Khajavi MR. (2013) Magnesium can decrease postoperative physiological ileus and postoperative pain in major non-laparoscopic gastrointestinal surgeries: A randomized controlled trial. Anesth Pain Med.4:e12750.
Abd-Elsalam KA, Fares KM, Mohamed MA, Mohamed MF, El-Rahman AMA, Tohamy MM. (2017) Efficacy of magnesium sulfate added to local anesthetic in a transversus abdominis plane block for analgesia following total abdominal hysterectomy: a randomized trial. Pain Physician. 20:641–647.
Atangana R, Ngowe Ngowe M, Binam F, Sossa MA. (2007) Morphine versus morphine-ketamine association in the management of postoperative pain in thoracic surgery. Acta Anaesthesiol Belg. 58:125–127.
Kim SH, Kim SI, Ok SY, Park SY, Kim MG, Lee SJ, Noh JI, Chun HR, Suh H. (2013) Opioid sparing effect of low dose ketamine in patients with intravenous patient-controleld analgesia using fentanyl after lumbar spinal fusion surgery. Korean J Anesthesiol. 64:524–528.
Thiele RH, Rea KM, Turrentine FE, Friel CM, Hassinger TE, McMurry TL, Goudreau BJ, Umapathi BA, Kron IL, Sawyer RG, Hedrick TL. (2015) Standardization of care: impact of an enhanced recovery protocol on length of stay complications, and direct costs after colorectal surgery. J Am Coll Surg. 220(4):430–43.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. (1973) Transection of the esophagus for bleeding esophageal varices. Br J Surg. 60(8):646–649.
Zaghiyan K, Mendelson B, Eng M, Ovsepyan G, Mirocha J, Fleshner P. (2018). Randomized clinical trial comparing laparoscopic vs. ultrasound-guided transversus abdominis plane block in minimally invasive colorectal surgery. Dis Colon Rectum. Nov 28 https://doi.org/10.1097/DCR.0000000000001292.
World Medical Association. (Accessed 2018) https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/. -General Assembly, Helsinki, Finland, June 1964.
CMS.Gov. (Accessed 2016) https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-Aug-2017.pdf. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (CDC) Compilation, Atlanta, GA.
Dindo D, Demartines N, Clavien PA. (2004) Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213.
Saleh F, Jackson TD, Ambrosini L, Gnanasegaramm JJ, Kwong J, Quereshy F, Okrainec A. (2014) Perioperative nonselective non-steroidal anti-inflammatory drugs are not associated with anastomotic leakage after colorectal surgery. J Gastrointest Surg. 8:1398–1404.
Lohsiriwat V. (2016) Opioid-sparing effect of selective cyclooxygenase-2 inhibitors on surgical outcomes after open colorectal surgery within an enhanced recovery after surgery protocol. World J Gastrointest Oncol. 8:543–549.
Hakkarainen TW, Steele SR, Bastaworous A, Dellinger EP, Farrokhi E, Farajah F, Florence M, Helton S, Horton S, Horton M, Pietro M, Varghese TK, Flum DR. (2015) Nonsteroidal anti-inflammatory drugs and the risk for anastomotic failure. JAMA Surg. 150:223–228.
Modasi A, Pace D, Godwin M, Smith C, Curtis B. (2018) NSAID administration post colorectal surgery increases anastomotic leak rate: A systematic analysis and meta-analysis. Surg Endosc. https://doi.org/10.1007/s00464-018-6355-1.
Ghuman A, Chan T, Karimuddin AA, Brown CJ, Raval MJ, Phang PT. (2015) Surgical site infection rates following implementation of a colorectal closure bundle in elective colorectal surgeries. Dis Colon Rectum. 58:1078–1082.
Naito M, Sato T, Nakamura T, Yamanashi T, Miura H, Tsutsui A, Watanabe M. (2017) Pain management using acetaminophen through postoperative course of laparoscopic colorectal surgery: A case matched control study. Ann Med Surg (Lond). 17:38–42.
Liska D, Bora Cengiz T, Novello M, Aiello A, Stocchi L, Hull TL, Steele Sr, Delaney CP, and Holubar SD. (2019) Do patients with inflammatory bowel disease benefit from an enhanced recovery pathway? Inflamm Bowel Dis. 2019 Aug 2. https://doi.org/10.1093/ibd/izz172.
Aryaie AH, Lalezari S, Sergent WK, Yana Puckett, Christopher Juergens, Craig Ratermann, Cari Ogg.(2018)Decreased opioid consumption and enhance recovery with the addition of IV acetaminophen in colorectal patients: A prospective, multi-institutional , randomized, double-blinded, placebo-controlled (DOCIVA Study). Surg Endosc. 32:3432–3438.
Fleet JL, Dixon SN, Kuwornu PJ, Dev VK, Montero-Odasso M, Burneo J, Garg Ax. (2018) Gabapentin dose and the 30-day risk of altered mental status in older adults: A retrospective population-based study. Plos One. 13: e0193134.
Maggiorgi L, Rullier E, Lefevre JH, Regimbeau JM, Berdah S, Karoui M Loriau J, Alves A, Vicaut E, Panis Y. (2017) Does a combination of laparoscopic approach and full fast track multimodal management decrease postoperative morbidity? A multicenter randomized controlled trial Ann Surg. 266:729–737.
Allen CA, Ivester JR Jr. (2018) Low-dose ketamine for postoperative pain management. J Perianesth Nurs. 33:389–398.
Murphy JD, Paskaradevan J, Eisler LL, Ouanes JP, Tomas VA, Freck EA, Wu CL. (2013) Analgesic efficacy of continuous intravenous magnesium infusion as an adjuvant to morphine for postoperative analgesia: A systematic review and meta-analysis. Middle East J Anaesthesiol. 22:11–20.
Albrecht E, Kirkham KR, Liu SS, Brull R. (2013) Peri-operative intravenous administration of magnesium sulphate and postoperative pain: a meta-analysis. Anaesthesia. 68:79–90.
Pedrazzani C, Menestrina N, Moro M, Brazzo G, Mantovani G, Polati E, Guglielmi A. (2016) Local wound infiltration plus transversus abdominis plane (TAP) block versus local wound infiltration in laparoscopic colorectal surgery and ERAS program. Surg Endosc. 30:5117–5125.
Kim AJ, Yong RJ, Urman RD. (2017) The role of transversus abdominis plane (TAP) blocks in enhanced recovery after surgery pathways for open and laparoscopic colorectal surgery. J Laparoendosc Adv Surg Tech A. 27:909–914.
Halabi WJ, Kang CY, Nguyen VQ, Carmichael JC, Mills S, Stamos MJ, Pigazzi A. (2014) Epidural analgesia in laparoscopic colorectal surgery: A nationwide analysis of use and outcomes. JAMA Surg. 149: 130–136.
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, Rockall TA, Young-Fadok TM, Hill AG, Soop M, De Boer D, Urman RD, Change GJ, Fichera A, Kessler H et al. (2019) Guidelines for perioperative care in elective colorectal surgery: Enhanced recovery after surgery (ERAS) society recommendations: 2018. World Journal of Surgery. 43(3): 659–695.
Alhashemi M, Fiore Jr. JF, Safa Nadia, Mahroos MA, Mata J, Pecorelli N, Baldini G, Dendukuri N, Stein BL, Liberman AS, Charlebois P, Carli F, and Feldman LS. Incidence and predictors of prolonged postoperative ileus after colorectal surgery in the context of an enhanced recovery pathway. (2019) Surgical Endoscopy. 22(7):2313–2322.
Brandstrup B, Svendsen PE, Rasmussen M, Belhage B, Rodt SA, Hansen B, Moller DR, Lundbech LB, Andersen N, Berg V, Thomassen N, Andersen ST, Simonsen L. (2012) Which goal for fluid therapy during colorectal surgery is followed by the best outcome: near-maximal stroke volume or zero fluid balance? Br J Anaesth. 109: 191–199.
Gomez-Izquierdo JC, Trainito A, Mirzakandov D, Stein BL, Liberman S, Charlebois P, Pecorelli N, Feldman L, Carli F, and Baldini G. (2017). Goal-directed fluid therapy does not reduce primary postoperative ileus after elective laparoscopic colorectal surgery: a randomized controlled trial. Anesthesiology. (127): 36-49.
Srinivasa S, Taylor MH, Singh PP, Yu TC, Soop M, and Hill AG. (2013). Randomized clinical trial of goal-directed fluid therapy within an enhanced recovery protocol for elective colectomy. Br J Surg. 100:66.
Rollins KE, Lobo DN (2016). Intraoperative goal-directed fluid therapy in elective major abdominal surgery: a meta-analysis of randomized controlled trials. Ann Surg. (263)465-476.
Author information
Authors and Affiliations
Contributions
(per the International Committee of Medical Journal Editors (ICMJE) guidelines)
Angela Mujukian
• Substantial contributions to acquisition, analysis, or interpretation of data
• Original drafting; revision for critically important intellectual content
• Final approval of the version to be published
• Accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Adam Truong
• Substantial contributions to acquisition, analysis, or interpretation of data
• Revision for critically important intellectual content
• Final approval of the version to be published
• Accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Hai Tran
• Substantial contributions to conception and design of the work
• Revision for critically important intellectual content
• Final approval of the version to be published
• Accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Rita Shane
• Substantial contributions to conception and design of the work
• Revision for critically important intellectual content
• Final approval of the version to be published
• Accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Phillip Fleshner
• Substantial contributions to conception and design of the work
• Revision for critically important intellectual content
• Final approval of the version to be published
• Accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Karen Zaghiyan
• Substantial contributions to conception and design of the work; acquisition, analysis or interpretation of data
• Drafting and revision for critically important intellectual content
• Final approval of the version to be published
• Accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Corresponding author
Ethics declarations
The study was conducted in accordance with the ethical principles stated in the Declaration of Helsinki20 and local regulations. All research-related activities were approved by the Cedars-Sinai Medical Center Institutional Review Board (nos. 46571 and 54607). Written informed consent was obtained from all participants.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mujukian, A., Truong, A., Tran, H. et al. A Standardized Multimodal Analgesia Protocol Reduces Perioperative Opioid Use in Minimally Invasive Colorectal Surgery. J Gastrointest Surg 24, 2286–2294 (2020). https://doi.org/10.1007/s11605-019-04385-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04385-9