Abstract
Cardiac arrest (CA) is a major cause of morbidity and mortality frequently associated with neurological and systemic involvement. Supportive therapeutic strategies such as mechanical ventilation, hemodynamic settings, and temperature management have been implemented in the last decade in post-CA patients, aiming at protecting both the brain and the lungs and preventing systemic complications. A lung-protective ventilator strategy is currently the standard of care among critically ill patients since it demonstrated beneficial effects on mortality, ventilator-free days, and other clinical outcomes. The role of protective and personalized mechanical ventilation setting in patients without acute respiratory distress syndrome and after CA is becoming more evident. The individual effect of different parameters of lung-protective ventilation, including mechanical power as well as the optimal oxygen and carbon dioxide targets, on clinical outcomes is a matter of debate in post-CA patients. The management of hemodynamics and temperature in post-CA patients represents critical steps for obtaining clinical improvement. The aim of this review is to summarize and discuss current evidence on how to optimize mechanical ventilation in post-CA patients. We will provide ten tips and key insights to apply a lung-protective ventilator strategy in post-CA patients, considering the interplay between the lungs and other systems and organs, including the brain.
Similar content being viewed by others
Background
Cardiac arrest (CA) is a major cause of morbidity and mortality with a high potential for detrimental systemic and cerebral complications [1]. Several therapeutic and supportive strategies have been implemented over the last years to optimize outcomes of post-CA patients, aiming at the improvement in neurological outcomes and survival [2, 3]. Among others, supportive strategies include appropriate settings of mechanical ventilation, aiming at optimizing gas exchange and limiting ventilator-induced lung injury (VILI), while avoiding systemic complications [3]. Mechanical ventilation should be targeted to limit hypoxemia and hyperoxemia and to maintain normal carbon dioxide levels [4,5,6,7,8], which are possible causes of secondary brain and reperfusion damage, lung damage, and poor survival [3, 9,10,11,12,13,14,15,16].
The literature in non-CA patients agrees on the importance of the use of lung-protective ventilator strategies (i.e., targeting at low tidal volume = VT of 6–8 ml/Kg predicted body weight (PBW), low plateau pressure = PPLAT < 20 cmH2O, driving pressure = ΔP < 13 cmH2O and low positive end-expiratory pressure (PEEP) < 7 cmH2O [5, 17,18,19,20,21,22,23,24,25,26,27] with some safety measures for patients with/or at risk of brain injury [28]. Recently, the concept of mechanical power (MP), the mechanical energy delivered per time by the ventilator on the respiratory system or the lung, has also been proposed as an important component of mechanical ventilation settings. High MP was found associated with worse outcomes in non-acute respiratory distress syndrome (ARDS) [29] and ARDS patients [30], but this effect has not been completely elucidated in post-CA patients [28]. Additionally, the optimal ventilatory targets, i.e., oxygen and carbon dioxide levels in post-CA patients, still deserve to be clarified [3]. This review aims at discussing the current advances in mechanical ventilation strategies in patients with the post-CA syndrome. We propose ten key rules for optimizing mechanical ventilation in patients after CA, considering the interplay between the lungs and other systems and organs, including the brain.
Rule one: tidal volume should be protective
VT represents one of the key parameters of lung-protective ventilator strategies. Low tidal volume (VT) in patients without ARDS (VT of 6–8 mL/kg PBW) resulted in no differences in ventilator-free days, intensive care unit (ICU), and hospital length of stay, 28-day and 90-day mortality in comparison with an intermediate VT strategy [21]. In the PRoVENT-iMiC study, Pisani et al. found no differences in VT between patients with higher or lower lung injury prediction score (around 8 mL/kg PBW) but lower values (around 7 mL/kg PBW) were applied in patients with ARDS [19]. A meta-analysis of 20 trials in critically ill patients without ARDS concluded that a strategy with lower VT was associated with less pulmonary infection, atelectasis, and mortality [31]. The guidelines of the European Society of Intensive Care Medicine (ESICM) and the European Resuscitation Council (ERC) provided some insights for mechanical ventilation (MV) in brain-injured and post-CA patients, suggesting applying a VT of 6–8 ml/kg PBW, but these recommendations were based on other populations and only small evidence in post-CA patients [32]. Few studies investigated the role of VT in CA patients. In an observational study, Sutherasan et al. reported the use of a median VT of 8.9 mL/kg PBW with a median PEEP of 3.5 cmH2O [18]. A VT higher than 10 mL/kg PBW was associated with ICU-acquired pneumonia [18]. In another study from Beitler et al., the use of lower VT was independently associated with favorable neurocognitive outcome, and ventilator-free days in a cohort of 256 post-CA patients [33]. A sub-analysis of the Target Temperature Management (TTM)1 trial reported a median VT of 7.7. mL/kg PBW (60% of patients were ventilated with a VT lower than 8 mL/kg PBW) and VT was not associated with mortality [26]. Evidence from a study including three different cohorts of patients with neurological diseases from distinct years (2004, 2010, and 2016) suggested an implementation over years of lung-protective ventilator strategies, especially regarding VT [34]. A very recent sub-study of the TTM2 trial including 1848 post-CA patients reported a median VT of 7 mL/kg PBW and a PEEP of 7 cmH2O without differences between survivors and non-survivors [28]. All these studies suggest a progressive reduction in VT over years which can be interpreted as an expression of increasingly application of lung-protective ventilator strategies in patients with CA. The association between lower VT and outcome is not consistent across studies, and no randomized controlled trials have been performed in the specific subgroup of patients [28]. Nevertheless, in other clinical settings, guidelines recommend using VT between 6 and 8 mL/kg PBW. Volume-controlled ventilation is currently more frequently used compared to pressure-controlled ventilation [18], but no data suggest any superiority between the different modes. The use of assisted ventilation, mainly pressure support ventilation (PSV), is increasingly used in patients after CA [18]. We suggest that in post-CA patients the VT should be set between 6 and 8 mL/kg PBW, in volume- or pressure-controlled ventilation but keeping in mind the interplay between VT and other parameters of MV (i.e., PPLAT, ΔP, PEEP, MP) as well as hemodynamics. Assisted ventilation may be used according to clinical conditions and the level of sedation of the patient.
Rule two: plateau pressure should be personalized
PPLAT is another important parameter of lung-protective ventilation, since it depends on the relationship between volume and compliance of the respiratory system in the absence of flow. Maintenance of PPLAT below 20 cmH2O is recommended in patients without ARDS to reduce mortality [23, 35]. The PREVENT trial in critically ill patients without ARDS reported lower PPLAT (PPLAT = 18 cmH2O) in the group at lower VT as compared to intermediate VT (PPLAT = 21 cmH2O), without significant differences in ventilator-free days, length of stay, complications, and mortality between the two groups [21]. The Relax trial found similar PPLAT between the group at lower PEEP = 5 cmH2O (19.9 cmH2O) and that at higher PEEP = 8 cmH2O (20 cmH2O), therefore suggesting that a lower PEEP strategy could preferable in patients without ARDS [22]. In a study in post-CA patients, PPLAT significantly differed among three cohorts of patients at different timeframes, with the highest value observed in the year 1998 and the lowest in 2010 (22.7 and 19.5 cmH2O, respectively), suggesting a progressive temporal change in ventilator setting in this population [18]; in addition, PPLAT higher than 17 cmH2O was found to be associated with ARDS development [18]. A very recent study in a cohort of patients post-CA suggested the adoption of PPLAT < 20 cmH2O [28]. As for VT, PPLAT should be set with the aim to reduce VILI, but most importantly should be considered within a personalized ventilatory strategy, accounting also for other ventilatory parameters which can be associated with mortality, including respiratory rate, driving pressure, and MP [28]. In the study by Robba et al., PPLAT was significantly associated with 6-month mortality [28]. The PPLAT of the respiratory system and transpulmonary pressure might differ in case of marked alterations of the chest wall elastance, as occurs in obesity. In obese patients or those with increased intra-abdominal pressure with PPLAT > 27 cmH2O, a simplified formula may help estimate the required correction of PPLAT: PPLAT target + (intra-abdominal pressure-13 cmH2O)/2 [36]. In mechanically ventilated non-obese patients, the average intra-abdominal pressure is 13 cmH2O and half of the intra-abdominal pressure is transmitted to the thoracic cavity [37]. We suggest that in post-CA patients the PPLAT should be kept equal or lower than 20 cmH2O and corrected for intra-abdominal pressure when clinically indicated.
Rule three: positive end-expiratory pressure should be low but enough
PEEP represents a key component of mechanical ventilation. Evidence agrees on that very low PEEP or zero PEEP can aggravate the risk of atelectasis and worsen lung damage [38]. The effects of higher PEEP on brain injury and intracranial pressure have been widely studied but still result a matter of debate [39]. High PEEP can increase intrathoracic pressure, potentially impairing left ventricle activity, decreasing the preload, afterload, and contractility, thus reducing venous return, which reflects on jugular veins acting as Starling resistors from intrathoracic pressure to the brain. Jugular veins present a valvular mechanism that limits the transmission of excessive intrathoracic pressure to the brain compartment. Indeed, it seems that if PEEP is lower than venous pressure, an excessive increase in pressure to the brain does not occur [40]. In the PRoVENT trial, when ΔP was included in the model, PEEP resulted associated with outcome [23]. In the Relax trial including critically ill patients with uninjured lungs, a lower PEEP strategy resulted in similar mortality and ventilator-free days than a higher PEEP strategy without the occurrence of severe hypoxemia [22]. The PRoVENT-iMiC observational study concluded that PEEP values were not associated with outcomes at multivariable analysis [19]. Few studies investigated the practice of the use of PEEP in post-CA population. Sutherasan et al. reported a mean PEEP value of 3.5 cmH2O in three cohorts of post-CA patients [18], while in a sub-analysis of the TTM1 trial, the mean PEEP was 6 cmH2O [26]. No randomized trials exist about PEEP in post-CA, but meta-analysis of trials in critically ill patients without ARDS confirmed that a higher PEEP strategy (5–30 cmH2O) was not associated with a better outcome, although it can decrease the incidence of ARDS and hypoxemia [41]. In this context, zero or very low PEEP levels should be avoided in the post-CA population to guarantee optimal oxygenation while limiting atelectasis or dynamic hyperinflation, hemodynamic derangement, impaired brain physiology, and other systemic complications [42, 43]. The most recent sub-analysis of the TTM2 trial in post-CA patients suggested that in this population, the application of a lung-protective ventilator strategy is even more common, including the use of a PEEP higher than in the past. In this study, a median value of 7 cmH2O of PEEP was used, but PEEP alone was not associated with patients’ outcomes, suggesting that a combination of ventilator parameters should be accounted for setting the ventilator in post-CA patients (i.e., ΔP which is a function of PPLAT and PEEP) [28]. We suggest that in post-CA patients a PEEP of 5 cmH2O should be initially used to reach a SatO2 at least above 92% and progressively increase in case of oxygen desaturation or worsening of respiratory mechanics.
Rule four: pay attention to the driving pressure!
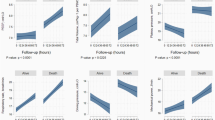
Driving pressure (ΔP) represents the distending pressure of the lungs, being the result of PPLAT minus PEEP, and representing the stress applied to the respiratory system. The VT changes differently affect the variation of ΔP (ΔΔP) and PPLAT, in relation to different static compliance of the respiratory system (Fig. 1). The PRoVENT study in patients without ARDS concluded that ΔP was not independently associated with in-hospital mortality, although ΔP value was available for 343 patients only [23]. In the PRoVENT-iMiC, median ΔP was similar in patients with or without lung injury but was higher in those with ARDS. At multivariable analysis, ΔP resulted not to be associated with outcome [19]. In post-CA patients, in a sub-analysis of the TTM1 trial, a median ΔP = 14.7 cmH2O was reported [18]. A ΔP < 13 cmH2O was suggested, since higher values are independently associated with higher mortality [21, 22, 28, 32]. In the study of Robba et al., ΔP was independently associated with mortality and poor neurological outcome. The formula of Costa et al., [(4 × ΔP) + respiratory rate], previously investigated in patients with ARDS, was recently applied by Robba et al. in a large cohort of post-CA patients, showing a stronger association with poor neurological outcome and mortality, when compared to MP alone [28]. This formula can easily guide ventilator settings at the bedside. Reducing VT to lower ΔP by 1 cmH2O is worthwhile only if the PaCO2 can be kept constant by increasing the respiratory rate by less than 4 breaths/min. Conversely, it may be worthwhile reducing the respiratory rate by four breaths if the increase in VT needed to maintain a constant PaCO2 results in an increase in ΔP less than 1 cmH2O. The variation of ΔP (ΔΔP) as a function of the variation of minute ventilation (ΔVE) at different static compliances of the respiratory system is depicted in Fig. 2. On the right side, the respiratory rate varies according to the ΔP, while in the left side, the respiratory rate is kept fixed at 10 breaths/min. We suggest in post-CA patients to maintain a ΔP < 13 cmH2O optimizing the VT for the respective compliance of the respiratory system.
Variation of tidal volume in function of variation of driving pressure. In this figure, we reported variation of ΔVT in function of the variation of ΔP (ΔΔP) at different static compliances of the respiratory system (20, 30, 40, 50, 60 mL/cmH2O). The respiratory rate varies according to the formula of Costa et al. Basal VT is assumed to be 7 ml/kg of predicted body weight (70 kg)
Variation of minute ventilation in function of variation of driving pressure. In this figure, the minute ventilation (VE) varies in function of the variation of driving pressure ΔP (ΔΔP) with (1) fixed respiratory rate to 10 breaths/min on the left, and (2) variable respiratory rate according to the formula by Costa et al. on the right. Basal VE is assumed to be 7 ml/kg of predicted body weight (70 kg) multiplied by 10 breaths/minute = 4.9 L/min
Rule five: respiratory rate should be targeted to pHa and PaCO2
Respiratory rate is one of the key variables of mechanical ventilation. Its contribution as harm during MV has been often underestimated. However, both respiratory rate per se and respiratory rate insensitivity (meaning as the ability of respiratory rate to control the minute ventilation) may become injurious during MV, thus promoting VILI, dynamic hyperinflation, and respiratory alkalosis [44]. Additionally, respiratory rate represents a major drive of chemical feedback such as arterial partial pressure of oxygen (PaO2), arterial partial pressure of carbon dioxide (PaCO2) and pHa. This assumes a pivotal relevance in patients who have/ or are at risk of brain injury such as post-CA patients, in order to modulate cerebral blood flow and vascular tone, as high PaCO2 can cause cerebrovascular vasodilation, and cerebral edema [45]. In normal conditions, when either volume or pressure increases, the respiratory rate decreases via the Hering–Breuer reflex [44]. The regulation of PaCO2 and oxygenation in post-CA population is challenging but deserves important attention in order to avoid secondary brain damage [28]. In a study by Harmon et al. respiratory rate, none of the other ventilation parameters was independently associated with 28-day mortality [26]. Similarly, in the study by Robba et al., the median respiratory rate was 17 breaths/min and resulted independently associated with 6 months of poor neurological outcome and mortality. As discussed above, respiratory rate should be adapted to ΔP and total mechanical power. We suggest that in post-CA patients, the respiratory rate should be kept in a range between 8 and 16 breaths/min.
Rule six: mechanical power is an attractive target, but with caution
MP is the product of mechanical energy and respiratory rate applied to the respiratory system or the lungs. MP accounts for several parameters of MV, and for this reason in the current years is gaining increased attention as a possible determinant of patient outcome [46]. In an observational cohort of critically ill patients without ARDS, MP resulted associated with in-hospital mortality, ICU mortality, 30-day mortality, ventilator-free days, ICU and hospital length of stay, with a consistent increase in the risk of death with MP higher than 17.0 J/min [47]. MP was even more strongly associated with mortality when it was normalized by body mass index [29]. The MP equation is made up of several parameters of lung-protective ventilation. The respective role of each individual ventilatory setting parameter within MP to determine effects on VILI and clinical outcomes is not clear. In a recent study of ARDS patients, Costa et al. [46] found that the impact of the ΔP on mortality was four times as large as that of the respiratory rate. This suggests that a reduction of 1 cmH2O in ΔP should be associated with a maximum increase in respiratory rate of 4 breaths/min, while a reduction of 3 cmH2O in ΔP to a maximum increase in respiratory rate of 12 breaths/min. However, these relationships might change at different levels of lung injury and respiratory or lung elastances. Previous studies on post-CA patients did not assess MP as a possible variable associated with outcome. In 2022, Robba et al. found that in post-CA patients, MP was independently associated with both 6 months of mortality and neurological outcome [28]. Figure 3 provides a theoretical analysis of five different respiratory system compliances (from 20 to 60 mL/cmH2O) during variations of ΔP (ΔΔP) in the function of variation of MP (ΔMP). In the right part of the graph, the formula of Costa et al. [(4 × ΔP) + respiratory rate] is adopted to see the variation of MP at different respiratory system compliances and maximum accepted different respiratory rates. In the left part of the graph, the respiratory rate is maintained constant to 10 breaths/minute while the respiratory system compliance is changing. Especially at lower respiratory system compliances, the change in MP is higher at the highest respiratory rate permitted by Costa et al. formula [(4 × ΔP) + respiratory rate]. This suggests that respiratory rate should be controlled within certain limits and play a relevant role to determine an excessive increase in MP, especially when the respiratory compliance is low. This formula can easily drive the MV setting at the bedside, when manipulating respiratory rate for keeping constant pHa (around 7.25) and PaCO2 [28]. In post-CA patients, only few of the parameters which constitute the MP formula were independently associated with poor outcome and VILI, while others were not (i.e., VT and PEEP) [28]. This suggests that caution is required to set the ventilator settings only on MP and conclusive evidence on its real clinical utility at the bedside is warranted especially in post-CA patients. As per evidence to date, if assessed at the bedside, we suggest that in post-CA patients MP should be targeted as lower than 17 J/min, taking into account ΔP and respiratory rate [28, 47]
Variation of mechanical power in function of variation of driving pressure. In this figure, the variation of mechanical power (ΔMP) in J/min changes in function of the variation of driving pressure ΔP (ΔΔP) with (1) fixed respiratory rate to 10 breaths/min on the left, and (2) variable respiratory rate according to the formula by Costa et al. on the right. The figure depicts the variation at different compliances of the respiratory system (20, 30, 40, 50, 60 mL/cmH2O). Basal MP is assumed to be calculated on a tidal volume (VT) of 7 ml/kg of predicted body weight (70 kg) and PEEP = 0 cmH2O, according to the formula of MP in pressure control ventilation = 0.098 × respiratory rate × VT × (PEEP + ΔP)
Rule seven: oxygenation should be accurately targeted to normoxia
Oxygenation is a key parameter to monitor in post-CA patients since this syndrome can activate different mechanisms such as reperfusion injury and oxidative stress, which can contribute to brain injury and neuronal damage [48]. Both hypoxemia and hyperoxemia are identified as possible detrimental stimuli on the outcome of critically ill patients. Hypoxemia in post-CA syndrome acts by altering the cerebral aerobic metabolism, which, if not restored, can lead to neuronal injury and cell death. Once the oxygen is restored after the return of spontaneous circulation, a possible reperfusion mechanism occurs, thus further accelerating neuronal death [3]. On the contrary, hyperoxemia may lead to the increased production of reactive oxygen species in the mitochondria and oxidative damage to the brain cells and seems to influence patients’ outcomes as well [3, 49]. The threshold responsible for hypoxic neuronal damages has yet to be defined, and, till now, it has been generally set at 60 mmHg [50,51,52,53]. Harmon et al. reported a liberal approach for oxygenation, thus the patients presenting with PaO2 up to 100 mmHg and with a high fraction of inspired oxygen levels. In non-survivors, oxygenation was lower [26]. However, other reports suggested that hypoxia can be detrimental also below 100 mmHg [18], while Ebner et al. suggested that either hypoxemia or hyperoxemia was not associated with outcome in post-CA patients, but recommended to titrate peripheral saturation of oxygen (SpO2) between 94 and 98% [5]. A very recent study demonstrated that a value of 60 mmHg could underestimate the risk of hypoxemia in the post-CA population as the best lower threshold associated with increased mortality was found at PaO2 of 69 mmHg, while the best upper threshold of PaO2 was 195 mmHg [54]. Regarding hyperoxia, a recent meta-analysis [55], showed that severe hyperoxemia (PaO2 > 300 mmHg) was associated with poor neurological outcome and mortality at follow-up in post-CA patients. In a study by Roberts et al., hyperoxemia with values > 300 mmHg was associated with poor outcome [56]. In the study of Robba et al., both hyperoxemia “per se” and the dose (AUC) of hyperoxemia over time were associated with mortality but not with poor neurological outcome. This suggests that the effect of hyperoxemia may depend on the duration of the exposure to high oxygen levels. In this study, the best upper threshold of PaO2 was > 195 mmHg. This is different from previous studies, but may explain why in previous studies a threshold of 300 mmHg was not associated with mortality or neurological outcome [57,58,59,60]. Current evidence also suggests that the “time passed” in one or another condition may play a key role in patient outcome, more than the single value per se, and that more attention should be paid to the titration of oxygen to lower levels than those applied in the past. The ICU-ROX trial confirmed no significant impact of conservative oxygen therapy (target peripheral saturation of oxygen = SpO2 > 90% and < 97%) as compared with usual oxygen therapy (SpO2 without upper limits but higher than 90%) on ventilator-free days [61]. Significant recommendations will come from the Mega-ROX trial (ANZCTRN 12620000391976) that will compare a liberal (SpO2 without upper limits, but > 90%) versus conservative (SpO2 91–94%) oxygen therapy in critically ill patients [62]. In a recent randomized controlled trial, targeting a restrictive (68–75 mmHg) versus a liberal (98–105 mmHg) oxygenation strategy in comatose patients after CA did not change the outcome (death, severe disability, and coma) [63]. While waiting for the results of ongoing clinical trials, according to the findings to date, a cutoff of PaO2 of 70–110 mmHg seems reasonable in this patient population.
Rule eight: carbon dioxide should be within normal ranges: so far
The role of carbon dioxide levels is frequently underestimated in post-CA patients. Hypercapnia and hypocapnia are detrimental to the brain physiology. An alteration of PaCO2 can widely affect the changes in intracellular pH and influence metabolic energy and oxygen demand also to the brain [3]. Hypocapnia is responsible for cerebral vasoconstriction and ischemic injury shifting to anaerobic metabolism and activating a systemic inflammatory response. On the other hand, hypercapnia can cause vasodilatation and promote a decrease in cerebral blood flow [3]. Although some researchers suggested the use of mild hypercapnia (PaCO2 50–55 mmHg) to improve cerebral oxygenation in comparison with normocapnia, elevated levels of PaCO2 can lead to lower pH and negatively influence outcome [64]. Therefore, changes in PaCO2 as well as mechanical ventilation during and after CA can affect carbon dioxide and pH levels and trigger dangerous pathways around pH, cellular demand, and catecholamine release [3], thus affecting the outcome. Ebner et al. [25] did not find any association between hypocapnia (< 34 mmHg) or hypercapnia (> 45 mmHg) and neurological outcome post-CA. While waiting for the results of the TAME randomized clinical trial (NCT03114033), the appropriate threshold to apply in post-CA patients is yet to be defined. According to the literature, a value of PaCO2 ranging between 35 and 50 mmHg seems to be preferable [3].
Rule nine: temperature can influence ventilatory function
The role of temperature management in post-CA patients is becoming increasingly clear, but its effect on the setting of the ventilatory parameter and gas exchange is still uncertain. Hypothermia at a targeted temperature of 33 °C did not confer a benefit as compared with a targeted temperature of 36 °C [65]. Targeted hypothermia at 33 °C followed by controlled rewarming did not reduce 6-month mortality as compared to targeted normothermia [66]. Temperature is a potential influencer of gas exchange, and the solubility of PaCO2 increases at lower temperatures. Indeed, blood gas analysis is commonly normalized to temperature, otherwise can report incorrect values. Similarly, in a small retrospective study, the PaCO2 decreased significantly more in the target temperature management group as compared with controls [67]. Regarding oxygen, a recent study found no significant differences in thresholds of oxygen related to the mortality between hypothermia and normothermia targets, thus suggesting that hypothermia does not improve oxygen tolerance [66]. The effect of temperature is relatively slight if dead space is not increased. These effects of temperature were investigated through the equation of alveolar dead space ventilation: (PaCO2 – end-tidal (et)CO2)/PaCO2, where temperature management at 33 °C resulted in lower etCO2 levels and higher alveolar dead space fraction compared to 36 °C with similar minute ventilation [26]. This effect can be explained by the lower pulmonary perfusion due to increased vasoconstriction, being also in accordance with the higher lactate levels at 33 °C compared to 36 °C [26]. In patients who remain comatose post-CA, the guidelines recommend continuous monitoring of core temperature and prevention of fever (defined as a temperature > 37.7 °C) for at least 72 h. Evidence is insufficient to recommend for or against temperature control at 32–36 °C or early cooling after CA [68].
Rule ten: hemodynamics should be maintained stable
Hemodynamics represents another important piece for optimization of MV. In post-CA patients, MV, fluids and vasopressor management, and temperature control can influence hemodynamics and outcome. Positive pressure ventilation can affect pulmonary blood flow and distribution, thus worsening cardiovascular function and gas exchange [69]. Indeed, the ventilator should be set to allow adequate expiratory time to limit the development of dynamic hyperinflation, and the effects of intrinsic PEEP and positive MV pressures to avoid cardiovascular collapse, especially in post-CA patients who frequently report altered cardiovascular function [69]. The administration of fluids to restore the end-diastolic volume can be considered in presence of PEEP if concomitant impaired left ventricular contractility and cardiac output occur. Vasopressors, inotropes, or inodilators such as epinephrine, dobutamine, or milrinone can be used to support cardiac output after the optimization of fluids and ventilator setting, but they can increase oxygen demand. [69]. A very recent trial suggested that targeting a mean arterial pressure of 63 mmHg or 77 mmHg in post-CA patients does not improve mortality or neurological outcome [70]. These results suggested adopting an individualized hemodynamic strategy. The temperature target can impact hemodynamics. Hypothermia at 33 °C, when compared to 36 °C, was associated with hemodynamic alterations (i.e., decreased heart rate, elevated lactate levels, and need for increased vasopressor support). Low mean arterial pressure and the need for high doses of vasopressors were independently associated with increased mortality in both groups [71]. A post hoc analysis of the TTM2 trial found that in post-CA patients with moderate vasopressor support on admission, hypothermia at 33 °C group increased non-neurological death. Indeed in the 33 °C group, hemodynamic instability and arrhythmias were more frequent [72]. In summary, patients with post-CA syndrome need to be strictly monitored for possible detrimental respiratory and cardiovascular interactions, thus accounting for targeted temperature management (around 36 °C) and personalized cardiovascular targets.
Future directions
The role of protective mechanical ventilation in post-CA patients is becoming even more clear. Figure 4 resumes the key rules for optimizing the setting of the ventilator in post-CA patients while accounting for lungs–heart and brain interactions. The PRoVENT-iMiC study showed that protective mechanical ventilation is easy to achieve following simple rules also in low- and middle-income countries where the resources are scarcer than high-income counties [19]. However, how to properly set the ventilator of a patient with post-CA syndrome as well as ARDS or other diseases needs education and training with specialized programs of intervention [73].
Ten key rules for optimizing ventilator setting in post-CA patients according to an organ protective mechanical ventilation strategy. VT = tidal volume, PBW = predicted body weight, PEEP = positive end-expiratory pressure, RR = respiratory rate, ΔP = driving pressure, MP = mechanical power, PaO2 = arterial partial pressure of oxygen, PaCO2 = arterial partial pressure of carbon dioxide, TTM = target temperature management, MAP = mean arterial pressure, CA, cardiac arrest
Conclusions
The role of protective and personalized mechanical ventilation setting in patients without ARDS and after CA is becoming more evident. Optimization of mechanical ventilation is cheap and may be adopted in high and middle-low economic income countries requiring only training and education. However, the individual role of each parameter of protective ventilation to minimize lung injury and their association with clinical major outcomes have not been completely elucidated in post-CA patients and deserve further research.
Availability of data and materials
Not applicable.
Abbreviations
- ΔP :
-
Driving pressure
- ARDS:
-
Acute respiratory distress syndrome
- CA:
-
Cardiac arrest
- ERC:
-
European Resuscitation Council
- ICU:
-
Intensive care unit
- MP:
-
Mechanical power
- MV:
-
Mechanical ventilation
- PaCO2 :
-
Arterial partial pressure of carbon dioxide
- PaO2 :
-
Arterial partial pressure of oxygen
- PBW:
-
Predicted body weight
- PEEP:
-
Positive end-expiratory pressure
- P PLAT :
-
Plateau pressure
- SpO2 :
-
Peripheral saturation of oxygen
- TTM:
-
Target temperature management
- V E :
-
Minute ventilation
- VILI:
-
Ventilator-induced lung injury
- V T :
-
Tidal volume
References
Eastwood GM, Tanaka A, Espinoza EDV, Peck L, Young H, Mårtensson J, et al. Conservative oxygen therapy in mechanically ventilated patients following cardiac arrest: a retrospective nested cohort study. Resuscitation. 2016;101:108–14.
Kim Y-M, Yim H-W, Jeong S-H, Lou KM, Callaway CW. Does therapeutic hypothermia benefit adult cardiac arrest patients presenting with non-shockable initial rhythms? A systematic review and meta-analysis of randomized and non-randomized studies. Resuscitation. 2012;83:188–96.
Robba C, Siwicka-Gieroba D, Sikter A, Battaglini D, Dąbrowski W, Schultz MJ, et al. Pathophysiology and clinical consequences of arterial blood gases and pH after cardiac arrest. Intensive Care Med Exp. 2020;8:19.
Newell C, Grier S, Soar J. Airway and ventilation management during cardiopulmonary resuscitation and after successful resuscitation. Crit Care. 2018;22:190.
Ebner F, Ullén S, Åneman A, Cronberg T, Mattsson N, Friberg H, et al. Associations between partial pressure of oxygen and neurological outcome in out-of-hospital cardiac arrest patients: an explorative analysis of a randomized trial. Crit Care. 2019;23:30.
Bellomo R, Bailey M, Eastwood GM, Nichol A, Pilcher D, Hart GK, et al. Arterial hyperoxia and in-hospital mortality after resuscitation from cardiac arrest. Crit Care. 2011;15:R90.
Wang C-H, Chang W-T, Huang C-H, Tsai M-S, Yu P-H, Wang A-Y, et al. The effect of hyperoxia on survival following adult cardiac arrest: a systematic review and meta-analysis of observational studies. Resuscitation. 2014;85:1142–8.
Vincent J-L, Taccone FS, He X. Harmful effects of hyperoxia in postcardiac arrest, sepsis, traumatic brain injury, or stroke: the importance of individualized oxygen therapy in critically ill patients. Can Respir J. 2017;2017:1–7.
Nolan JP, Neumar RW, Adrie C, Aibiki M, Berg RA, Böttiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. Resuscitation. 2008;79:350–79.
Sekhon MS, Ainslie PN, Griesdale DE. Clinical pathophysiology of hypoxic ischemic brain injury after cardiac arrest: a “two-hit” model. Crit Care. 2017;21:90.
Brueckl C, Kaestle S, Kerem A, Habazettl H, Krombach F, Kuppe H, et al. Hyperoxia-induced reactive oxygen species formation in pulmonary capillary endothelial cells in situ. Am J Respir Cell Mol Biol. 2006;34:453–63.
Brugniaux JV, Coombs GB, Barak OF, Dujic Z, Sekhon MS, Ainslie PN. Highs and lows of hyperoxia: physiological, performance, and clinical aspects. Am J Physiol Integr Comp Physiol. 2018;315:R1-27.
Farquhar H, Weatherall M, Wijesinghe M, Perrin K, Ranchord A, Simmonds M, et al. Systematic review of studies of the effect of hyperoxia on coronary blood flow. Am Heart J. 2009;158:371–7.
Cornet AD, Kooter AJ, Peters MJ, Smulders YM. The potential harm of oxygen therapy in medical emergencies. Crit Care. 2013;17:313.
Damiani E, Donati A, Girardis M. Oxygen in the critically ill. Curr Opin Anaesthesiol. 2018;31:129–35.
Crawford P, Good PA, Gutierrez E, Feinberg JH, Boehmer JP, Silber DH, et al. Effects of supplemental oxygen on forearm vasodilation in humans. J Appl Physiol. 1997;82:1601–6.
Sutherasan Y, Vargas M, Pelosi P. Protective mechanical ventilation in the non-injured lung: review and meta-analysis. Crit Care [Internet]. BioMed Central; 2014 [cited 2019 May 3];18:211. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24762100
Sutherasan Y, Peñuelas O, Muriel A, Vargas M, Frutos-Vivar F, Brunetti I, et al. Management and outcome of mechanically ventilated patients after cardiac arrest. Crit Care. 2015;19:215.
Pisani L, Algera AG, Serpa Neto A, Ahsan A, Beane A, Chittawatanarat K, et al. Epidemiological characteristics, ventilator management, and clinical outcome in patients receiving invasive ventilation in intensive care units from 10 Asian middle-income countries (PRoVENT-iMiC): an international, multicenter, prospective study. Am J Trop Med Hyg. 2021. https://doi.org/10.4269/ajtmh.20-1177.
Neto AS, Barbas CSV, Simonis FD, Artigas-Raventós A, Canet J, Determann RM, et al. Epidemiological characteristics, practice of ventilation, and clinical outcome in patients at risk of acute respiratory distress syndrome in intensive care units from 16 countries (PRoVENT): an international, multicentre, prospective study. Lancet Respir Med. 2016;4:882–93.
Simonis FD, Serpa Neto A, Binnekade JM, Braber A, Bruin KCM, Determann RM, et al. Effect of a low vs intermediate tidal volume strategy on ventilator-free days in intensive care unit patients without ARDS. JAMA. 2018;320:1872.
Algera AG, Pisani L, Serpa Neto A, den Boer SS, Bosch FFH, Bruin K, et al. Effect of a lower vs higher positive end-expiratory pressure strategy on ventilator-free days in ICU patients without ARDS: a randomized clinical trial. JAMA J Am Med Assoc. 2020;324:2509.
Simonis FD, Barbas CSV, Artigas-Raventós A, Canet J, Determann RM, Anstey J, et al. Potentially modifiable respiratory variables contributing to outcome in ICU patients without ARDS: a secondary analysis of PRoVENT. Ann Intensive Care. 2018;8:39.
Silva PL, Pelosi P, Rocco PRM. Optimal mechanical ventilation strategies to minimize ventilator-induced lung injury in non-injured and injured lungs. Expert Rev Respir Med. 2016;10:1243–5.
Ebner F, Harmon MBA, Aneman A, Cronberg T, Friberg H, Hassager C, et al. Carbon dioxide dynamics in relation to neurological outcome in resuscitated out-of-hospital cardiac arrest patients: an exploratory target temperature management trial substudy. Crit Care. 2018;22:196.
Harmon MBA, van Meenen DMP, van der Veen ALIP, Binnekade JM, Dankiewicz J, Ebner F, et al. Practice of mechanical ventilation in cardiac arrest patients and effects of targeted temperature management: a substudy of the targeted temperature management trial. Resuscitation. 2018;129:29–36.
Sutherasan Y, Raimondo P, Pelosi P. Ventilation and gas exchange management after cardiac arrest. Best Pract Res Clin Anaesthesiol. 2015;29:413–24.
Robba C, Badenes R, Battaglini D, Ball L, Brunetti I, Jakobsen JC, et al. Ventilatory settings in the initial 72 h and their association with outcome in out-of-hospital cardiac arrest patients: a preplanned secondary analysis of the targeted hypothermia versus targeted normothermia after out-of-hospital cardiac arrest (TTM2) tr. Intensive Care Med. 2022;online ahead of print.
Serpa Neto A, Deliberato RO, Johnson AE, Pollard TJ, Celi LA, Pelosi P, et al. Normalization of mechanical power to anthropometric indices: impact on its association with mortality in critically ill patients. Intensive Care Med. 2019;45:1835–7.
Chen L, Grieco DL, Beloncle F, Chen G-Q, Tiribelli N, Madotto F, et al. Partition of respiratory mechanics in patients with acute respiratory distress syndrome and association with outcome: a multicentre clinical study. Intensive Care Med. 2022;48:888–98.
Serpa Neto A, Cardoso SO, Manetta JA, Pereira VGM, Espósito DC, de Pasqualucci MOP, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome. JAMA. 2012;308:1651.
Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H, et al. European resuscitation council and European society of intensive care medicine guidelines 2021: post-resuscitation care. Intensive Care Med. 2021;47:369–421.
Beitler JR, Ghafouri TB, Jinadasa SP, Mueller A, Hsu L, Anderson RJ, et al. Favorable neurocognitive outcome with low tidal volume ventilation after cardiac arrest. Am J Respir Crit Care Med. 2017;195:1198–206.
Tejerina EE, Pelosi P, Robba C, Peñuelas O, Muriel A, Barrios D, et al. Evolution over time of ventilatory management and outcome of patients with neurologic disease. Crit Care Med. 2021;49:1095–106.
Pisani L, Algera AG, Neto AS, Azevedo L, Pham T, Paulus F, et al. Geoeconomic variations in epidemiology, ventilation management, and outcomes in invasively ventilated intensive care unit patients without acute respiratory distress syndrome: a pooled analysis of four observational studies. Lancet Glob Heal. 2022;10:e227–35.
Pelosi P, Ball L, Barbas CSV, Bellomo R, Burns KEA, Einav S, et al. Personalized mechanical ventilation in acute respiratory distress syndrome. Crit Care. 2021;25:250.
Regli A, Pelosi P, Malbrain MLNG. Ventilation in patients with intra-abdominal hypertension: what every critical care physician needs to know. Ann Intensive Care. 2019;9:52.
Farias LL, Faffe DS, Xisto DG, Santana MCE, Lassance R, Prota LFM, et al. Positive end-expiratory pressure prevents lung mechanical stress caused by recruitment/derecruitment. J Appl Physiol. 2005;98:53–61.
Robba C, Ball L, Nogas S, Battaglini D, Messina A, Brunetti I, et al. Effects of positive end-expiratory pressure on lung recruitment, respiratory mechanics and intracranial pressure in mechanically ventilated brain injured patients. Front Physiol. 2021;12: 711273.
Riforgiato C, Battaglini D, Robba C, Pelosi P. Mechanical ventilation—PEEP. Essentials evidence-based pract neuroanesthesia neurocritical care. Elsevier; 2022. p. 33–42.
Yi H, Li X, Mao Z, Liu C, Hu X, Song R, et al. Higher PEEP versus lower PEEP strategies for patients in ICU without acute respiratory distress syndrome: a systematic review and meta-analysis. J Crit Care. 2022;67:72–8.
Robba C, Poole D, McNett M, Asehnoune K, Bösel J, Bruder N, et al. Mechanical ventilation in patients with acute brain injury: recommendations of the European society of intensive care medicine consensus. Intensive Care Med. 2020;46:2397–410.
Algera AG, Pierrakos C, Botta M, Zimatore C, Pisani L, Tuinman P-R, et al. Myocardial function during ventilation with lower versus higher positive end-expiratory pressure in patients without ARDS. J Clin Med. 2022;11:2309.
Akoumianaki E, Vaporidi K, Georgopoulos D. The injurious effects of elevated or nonelevated respiratory rate during mechanical ventilation. Am J Respir Crit Care Med. 2019;199:149–57.
Heffner JE. Controlled hyperventilation in patients with intracranial hypertension. Arch Intern Med. 1983;143:765.
EL Costa V, Slutsky AS, Brochard LJ, Brower R, Serpa-Neto A, Cavalcanti AB, et al. Ventilatory variables and mechanical power in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2021;204:303–11.
Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44:1914–22.
Taran S, Pelosi P, Robba C. Optimizing oxygen delivery to the injured brain. Curr Opin Crit Care. 2022;28:145–56.
Ni Y-N, Wang Y-M, Liang B-M, Liang Z-A. The effect of hyperoxia on mortality in critically ill patients: a systematic review and meta analysis. BMC Pulm Med. 2019;19:53.
Shin HK, Dunn AK, Jones PB, Boas DA, Lo EH, Moskowitz MA, et al. Normobaric hyperoxia improves cerebral blood flow and oxygenation, and inhibits peri-infarct depolarizations in experimental focal ischaemia. Brain. 2007;130:1631–42.
Alternative Therapy Evaluation Committee for the Insurance Corporation of Brithish Columbia. A review of the scientific evidence on the treatment of traumatic brain injuries and strokes with hyperbaric oxygen. Brain Inj. 2003;17:225–36.
Rincon F, Mayer SA, Rivolta J, Stillman J, Boden-Albala B, Elkind MSV, et al. Impact of delayed transfer of critically ill stroke patients from the emergency department to the neuro-ICU. Neurocrit Care. 2010;13:75–81.
Le Gall JR. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA J Am Med Assoc. 1993;270:2957–63.
Robba C, Badenes R, Battaglini D, Ball L, Sanfilippo F, Brunetti I, et al. Oxygen targets and 6-month outcome after out of hospital cardiac arrest: a pre-planned sub-analysis of the targeted hypothermia versus targeted normothermia after out-of-hospital cardiac arrest (TTM2) trial. Crit Care. 2022;26:323.
La Via L, Astuto M, Bignami EG, Basalacchi D, Dezio V, Girardis M, et al. The effects of exposure to severe hyperoxemia on neurological outcome and mortality after cardiac arrest. Minerva Anestesiol. 2022;Online ahead of print.
Roberts BW, Kilgannon JH, Hunter BR, Puskarich MA, Pierce L, Donnino M, et al. Association between early hyperoxia exposure after resuscitation from cardiac arrest and neurological disability. Circulation. 2018;137:2114–24.
Johnson NJ, Dodampahala K, Rosselot B, Perman SM, Mikkelsen ME, Goyal M, et al. The association between arterial oxygen tension and neurological outcome after cardiac arrest. Ther Hypothermia Temp Manag. 2017;7:36–41.
Kim TJ, Kim J-M, Lee JS, Park S-H, Jeong H-B, Choi J-K, et al. Prognostication of neurological outcome after cardiac arrest using wavelet phase coherence analysis of cerebral oxygen. Resuscitation. 2020;150:41–9.
Ebner F, Riker RR, Haxhija Z, Seder DB, May TL, Ullén S, et al. The association of partial pressures of oxygen and carbon dioxide with neurological outcome after out-of-hospital cardiac arrest: an explorative international cardiac arrest registry 2.0 study. Scand J Trauma Resusc Emerg Med. 2020;28:67.
Peluso L, Belloni I, Calabró L, Dell’Anna AM, Nobile L, Creteur J, et al. Oxygen and carbon dioxide levels in patients after cardiac arrest. Resuscitation. 2020;150:1–7.
ICU-ROX Investigators and the Australian and New Zeland Intensive Care Society Clinical Trials Group. Conservative oxygen therapy during mechanical ventilation in the ICU. N Engl J Med. 2020;382:989–98.
Young PJ, Arabi YM, Bagshaw SM, Bellomo R, Fujii T, Haniffa R, et al. Protocol and statistical analysis plan for the mega randomised registry trial research program comparing conservative versus liberal oxygenation targets in adults receiving unplanned invasive mechanical ventilation in the ICU (Mega-ROX). Crit Care Resusc. 2022;24:137–49.
Schmidt H, Kjaergaard J, Hassager C, Mølstrøm S, Grand J, Borregaard B, et al. Oxygen targets in comatose survivors of cardiac arrest. N Engl J Med. 2022;Online ahead of print.
Tiruvoipati R, Pilcher D, Botha J, Buscher H, Simister R, Bailey M. Association of hypercapnia and hypercapnic acidosis with clinical outcomes in mechanically ventilated patients with cerebral injury. JAMA Neurol. 2018;75:818–26.
Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33 °C versus 36 °C after cardiac arrest. N Engl J Med. 2013;369:2197–206.
Dankiewicz J, Cronberg T, Lilja G, Jakobsen JC, Levin H, Ullén S, et al. Hypothermia versus normothermia after out-of-hospital cardiac arrest. N Engl J Med. 2021;384:2283–94.
Karnatovskaia LV, Festic E, Freeman WD, Lee AS. Effect of therapeutic hypothermia on gas exchange and respiratory mechanics: a retrospective cohort study. Ther Hypothermia Temp Manag. 2014;4:88–95.
Sandroni C, Nolan JP, Andersen LW, Böttiger BW, Cariou A, Cronberg T, et al. ERC-ESICM guidelines on temperature control after cardiac arrest in adults. Intensive Care Med. 2022;48:261–9.
Mahmood SS, Pinsky MR. Heart-lung interactions during mechanical ventilation: the basics. Ann Transl Med. 2018;6:349–349.
Kjaergaard J, Møller JE, Schmidt H, Grand J, Mølstrøm S, Borregaard B, et al. Blood-pressure targets in comatose survivors of cardiac arrest. N Engl J Med. 2022;online ahead of print.
Bro-Jeppesen J, Annborn M, Hassager C, Wise MP, Pelosi P, Nielsen N, et al. Hemodynamics and vasopressor support during targeted temperature management at 33 °C versus 36 °C after out-of-hospital cardiac arrest. Crit Care Med. 2015;43:318–27.
Düring J, Annborn M, Cariou A, Chew MS, Dankiewicz J, Friberg H, et al. Influence of temperature management at 33 °C versus normothermia on survival in patients with vasopressor support after out-of-hospital cardiac arrest: a post hoc analysis of the TTM-2 trial. Crit Care. 2022;26:231.
Battaglini D, Ionescu Maddalena A, Caporusso RR, Garofalo E, Bruni A, Bocci MG, et al. Acquisition of skills in critical emergency medicine: an experimental study on the SIAARTI Academy CREM experience. Minerva Anestesiol. 2021;87:1174–82.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
DB contributed to writing. PP and CR contributed to editing. All authors provided final approval of the version submitted. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Battaglini, D., Pelosi, P. & Robba, C. Ten rules for optimizing ventilatory settings and targets in post-cardiac arrest patients. Crit Care 26, 390 (2022). https://doi.org/10.1186/s13054-022-04268-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-022-04268-7