Abstract
Background
The majority of critically ill patients do not suffer from acute respiratory distress syndrome (ARDS). To improve the treatment of these patients, we aimed to identify potentially modifiable factors associated with outcome of these patients.
Methods
The PRoVENT was an international, multicenter, prospective cohort study of consecutive patients under invasive mechanical ventilatory support. A predefined secondary analysis was to examine factors associated with mortality. The primary endpoint was all-cause in-hospital mortality.
Results
935 Patients were included. In-hospital mortality was 21%. Compared to patients who died, patients who survived had a lower risk of ARDS according to the ‘Lung Injury Prediction Score’ and received lower maximum airway pressure (Pmax), driving pressure (ΔP), positive end-expiratory pressure, and FiO2 levels. Tidal volume size was similar between the groups. Higher Pmax was a potentially modifiable ventilatory variable associated with in-hospital mortality in multivariable analyses. ΔP was not independently associated with in-hospital mortality, but reliable values for ΔP were available for 343 patients only. Non-modifiable factors associated with in-hospital mortality were older age, presence of immunosuppression, higher non-pulmonary sequential organ failure assessment scores, lower pulse oximetry readings, higher heart rates, and functional dependence.
Conclusions
Higher Pmax was independently associated with higher in-hospital mortality in mechanically ventilated critically ill patients under mechanical ventilatory support for reasons other than ARDS.
Trial Registration ClinicalTrials.gov (NCT01868321).
Similar content being viewed by others
Introduction
Mechanical ventilation is a potentially life-saving intervention, though there is an increasing body of evidence for potential harm from this intervention in critically ill patients [1, 2]. Too high tidal volumes (VT) and airway pressures have been shown to be associated with worse outcomes in patients with acute respiratory distress syndrome (ARDS) [3, 4], and there is increasing evidence for the injurious effects of too high VT in ventilated patients without ARDS [5, 6]. While inadequately too low positive end-expiratory pressures (PEEP) have been demonstrated to worsen outcome of patients with ARDS, especially in moderate or severe cases [7], patients without ARDS likely do not benefit from higher PEEP [8]. More recently, a positive association between driving pressures (ΔP) and mortality was demonstrated in patients with ARDS [9], but it is unclear whether ΔP is associated with a worse outcome also in patients without ARDS.
Results from the ‘Large observational study to UNderstand the Global impact of Severe Acute respiratory FailurE’ (LUNG SAFE) [10], a prospective cohort study undertaken in 459 intensive care units (ICUs) in 50 countries, as well as the more recent ‘PRactice of VENTilation in patients without ARDS study’ (PRoVENT) [11], a prospective cohort study undertaken in 119 ICUs in 16 countries, convincingly showed that the practice of invasive mechanical ventilatory support in ICUs has changed remarkably over the recent years [10,11,12]. First, VT size decreased over time, not only in patients with ARDS [10, 12,13,14], but also in patients at risk of ARDS [11]. Presently, VT above 10 to 12 ml/kg predicted body weight (PBW) is seldom used. The median PEEP level that is set has increased over time in patients without ARDS [11, 13, 14]. In patients with ARDS, higher levels of PEEP usually are restricted to patients with more severe hypoxemia [7, 10, 15]. Both investigations, though, suggested there is still potential for improvement in ventilatory management in critically ill patients [10, 11], and one recently published secondary analysis of LUNG SAFE showed that lower PEEP, higher peak inspiratory (Ppeak), plateau (Pplat), ΔP, and increased respiratory rate represent potentially modifiable factors contributing to worse outcome in patients with ARDS [16].
The aim of the present study was to identify modifiable respiratory variables that could potentially change outcome in critically ill patients under invasive mechanical ventilatory support without ARDS. Specifically, we hypothesized that there are several modifiable respiratory variables associated with all-cause in-hospital mortality.
Methods
Study design
PRoVENT was an investigator-initiated international multicenter study; details of its methods have been published elsewhere [11, 17]. Details on study population and data collection are described in the supplement. PRoVENT was registered at Clinicaltrials.gov (NCT01868321).
Patients
Consecutive patients under invasive mechanical ventilatory support were eligible for participation if admitted in a predefined period lasting one week. Inclusion criteria were: (1) age ≥ 18 years and (2) under invasive mechanical ventilatory support, which could have been initiated outside the hospital, in the emergency room, in the normal ward or in the operating room, or start of invasive mechanical ventilatory support in the ICU, after admission. Patients in whom mechanical ventilatory support was started before the study recruitment week of PRoVENT, patients receiving only noninvasive mechanical ventilatory support or transferred from another hospital under invasive mechanical ventilatory support were excluded. Although data were also collected from patients who fulfilled the Berlin definition for ARDS [18] at start of ventilation, data of those patients were not used in the present analysis.
Definitions and calculations
The risk of death was derived from acute physiology and chronic health evaluation (APACHE) II scores [19] or simplified acute physiology score (SAPS) III [20].
Under the assumption that the maximum airway pressure (Pmax) during pressure-controlled assist modes of invasive mechanical ventilatory support is similar to Pplat during volume-controlled assist modes [21, 22], Pmax was defined as Pmax in pressure-controlled assist modes and plateau pressure in volume-controlled assist modes, when available. Also, ΔP was calculated by subtracting PEEP from Pmax during pressure-controlled and volume-controlled ventilation, respectively. This, however, was only done when set and measured respiratory rates were equal, indicating the absence of spontaneous breathing.
VT size was expressed as a volume normalized for predicted body weight (ml/kg PBW). The PBW of male patients was calculated as equal to 50 + 0.91(centimeters of height—152.4); that of female patients was calculated as equal to 45.5 + 0.91(centimeters of height—152.4) [23]. Dead space fraction was calculated as (partial pressure of carbon dioxide in arterial blood (PaCO2)–end-tidal carbon dioxide (etCO2))/PaCO2, and static compliance of the respiratory system as VT/ΔP. ‘Non-pulmonary’ sequential organ failure assessment (SOFA) was calculated by leaving out the pulmonary component and amending the denominator accordingly. The presence of acidosis was split into respiratory and metabolic acidosis to include separately in the univariate analysis, under the assumption that a respiratory acidosis could be modifiable by adjusting respiratory minute volume as opposed to metabolic acidosis. Immunosuppression was defined as the presence of human immunodeficiency virus or the use of chemotherapy, systemic steroids (> 1 mg/kg of prednisone or equivalent), or other immunosuppressive agents.
Outcomes
The primary outcome was all-cause in-hospital mortality, defined as mortality at hospital discharge, or at 90 days after start of invasive mechanical ventilatory support while still in hospital, whichever occurred first. The secondary outcome was ICU mortality, defined as mortality at ICU discharge or at 90 days after start of mechanical ventilatory support while still in ICU, whichever occurred first.
Statistical analysis
Daily-collected variables, including Pmax or Pplat, ΔP, PEEP, VT, oxygen fraction of inspired air (FiO2), respiratory rate, dead space fraction, and compliance, and blood gas analysis parameters such as partial pressure of oxygen in arterial blood (PaO2), PaCO2, pH, and bicarbonate level, were presented as medians with their interquartile ranges. Proportions were compared using Chi-square or Fisher’s exact tests, and continuous variables were compared using the t test or Wilcoxon rank sum test, as appropriate. Since the amount of missing data were low, no assumptions were made for missing data.
In all descriptive analyses, survivors were separated from non-survivors according to all-cause in-hospital mortality. In univariate analyses assessing the impact of ventilatory variables on outcome, relative risk (RR) of in-hospital mortality was estimated for patients dividing the study sample according to the median of Pmax (≤ 18 vs. > 18 cm H2O), ΔP (≤ 12 vs. > 12 cm H2O), PEEP (≤ 5 vs. > 5 cm H2O), and VT (≤ 7.9 vs. > 7.9 ml/kg PBW), as measured at the first day of ventilation. For this specific analysis, two separate groups were included: patients not at risk and patients at risk of ARDS according to the Lung Injury Prediction Score (LIPS), where a LIPS ≥ 4 was considered ‘at risk of ARDS’ and a LIPS < 4 ‘not at risk of ARDS.’
To identify potentially modifiable and non-modifiable factors contributing to hospital mortality, a multivariable model was built using demographic factors, comorbidities, illness severities, and respiratory and laboratorial variables at the first day of ventilation. Since Pmax and ΔP have a high collinearity, we chose to include only Pmax in the main model. We conducted multilevel analyses to adjust for clustering of the data. Therefore, a multilevel logistic regression was used to identify factors contributing to mortality by modeling it as the dependent variable. Variables were selected when the univariate analysis p value was< 0.2. Then, a multilevel multivariable logistic model was built with centers treated as random effect. The cluster effects induced by the structure of the data were taken into account through random effects. In the multivariable model, statistical significance was set at a p < 0.05. Results are shown as odds ratios (ORs) with 95% confidence intervals (CI).
The odds ratio for hospital mortality of Pmax was plotted in curves showing the odds ratios according to increases of one standard deviation of the Pmax. These curves were divided according to the risk of ARDS and adjusted for the variables included the final model and reported in Table 3. A similar curve was made using ICU mortality as outcome.
We performed a secondary analysis in which we replaced Pmax with ΔP in the multivariate model for in-hospital and ICU mortality. Since we lacked reliable values for ΔP for a large group of patients, this analysis had a much smaller sample size, increasing the risk of losing power to show an association between ΔP and in-hospital mortality. To test this, we performed one post hoc analysis in which we used Pmax instead of ΔP, but only for patients for whom we had a reliable ΔP.
Statistical significance was considered to be at two-sided p < 0.05. All analyses were performed with SPSS v.20 (IBM SPSS Statistics for Windows, Version 20·0. Armonk, NY: IBM Corp.), and R v.2·12·0 (http://www.r-project.org).
Results
Participating centers and patients
One hundred and nineteen ICUs from 16 countries in four continents enrolled 1021 patients under invasive mechanical ventilatory support. Excluding 86 patients who were admitted to ICU with ARDS, we analyzed the data from a total of 935 patients (Fig. 1). All-cause in-hospital mortality was 21% in all patients. Patients who survived had lower derived risk scores for mortality, were younger, and had lower SOFA scores; patients who died were more often functionally dependent and more often admitted for a medical condition or for emergency surgery (Table 1).
Ventilation characteristics
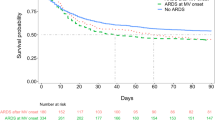
Patients who survived had a lower Pmax or Pplat, lower ΔP, lower PEEP, and lower FiO2 levels than patients who died, but a similar VT (Table 2). PaO2/FiO2, pulse oximetry, and arterial pH were higher and PaCO2 levels were lower in patients who survived (Table 2). The unadjusted impact of ventilatory parameters in the overall cohort and in each group of risk of ARDS is shown in Fig. 2. Mortality risk was similar in patients stratified according tidal volume and ΔP. In the overall cohort, patients receiving higher PEEP had higher risk of hospital mortality (Fig. 2). Patients ventilated with higher Pmax had a higher risk of hospital mortality in the overall cohort and in patients at risk of ARDS (Fig. 2).
Unadjusted relative risks of hospital mortality in the overall cohort and in patients at risk and not at risk of ARDS and according to the median of the: a Pmax; b PEEP; c ∆P; and d tidal volume. Abbreviations: Pmax: maximum airway pressure; PEEP: positive end-expiratory pressure; VT: tidal volume; ∆P: driving pressure; RR: relative risk; CI: confidence interval
Factors associated with in-hospital mortality
The results of the univariable analysis of factors associated with in-hospital mortality are provided in Additional file 1: Table S1. In multivariable analysis, Pmax was the only ventilatory variable associated with higher in-hospital mortality; in this analysis, the ΔP was excluded due to the collinearity with Pmax (Table 3). Non-modifiable factors associated with worse outcome were older age, presence of immunosuppression, higher non-pulmonary SOFA, lower pulse oximetry readings, higher heart rates, and functional dependency (Table 3).
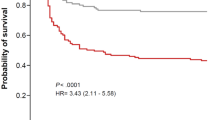
Figure 3 shows the odds ratio for hospital mortality per increase in one standard deviation in Pmax for patients not at risk of ARDS and patients at risk of ARDS and adjusted for the variables indicated in Table 3.
Odds ratio of hospital mortality according to increases in one standard deviation of Pmax and in the patients at risk and not at risk of ARDS. All curves are adjusted by the same set of variables described in Table 3
Factors associated with ICU mortality
Results of the univariable analysis of factors associated with ICU mortality are provided in Additional file 1: Table S2. After multivariable adjustments, Pmax was the only ventilatory variable associated with worse outcome (Additional file 1: Table S2); non-modifiable factors associated with worse outcome were history of COPD, presence of immunosuppression, higher non-pulmonary SOFA scores, and functional dependency.
Additional file 1: Figure S1 shows the odds ratio for ICU mortality per increase in one standard deviation in Pmax for patients not at risk of ARDS and patients at risk of ARDS and adjusted for the variables indicated in Additional file 1: Table S2.
Driving pressure
The analysis including ΔP was only possible in 343 patients for whom ΔP could be calculated in a reliable way. When considering ΔP instead of Pmax in the model, there was an association between ΔP and ICU (Additional file 1: Table S3), but not between ΔP and in-hospital mortality (Additional file 1: Table S4). The lack of an association between ΔP and in-hospital mortality could very well have been caused by the smaller sample size, since the post hoc analysis in which we used Pmax in the model, now using the same number of patients as done for the analysis including ΔP, also showed no association between Pmax and in-hospital mortality (Additional file 1: Table S5), while the association between Pmax and ICU mortality remained present (Additional file 1: Table S6).
Discussion
In the present study, older age, presence of immunosuppression, a more dependent premorbid condition, and severity of illness markers such as the pulse oximetry, the non-pulmonary SOFA score, and a higher heart rate were all independently associated with increased in-hospital mortality. In the present analysis, Pmax was the single ventilator factor associated with in-hospital mortality, suggesting this is the only potentially modifiable factor in these patients. Parts of our findings are in line with prior studies in this field. Older age is independently associated with worse outcome in patients with ARDS [16, 24, 25] and patients without ARDS [13], and also immunosuppression is a risk factor for mortality in our study and in trials that included patients with ARDS [16, 25]. Severity of illness factors associated with outcome was a higher heart rate and higher non-pulmonary SOFA score, consistent with previous studies in patients with [16, 25], as well as in patients without ARDS [13]. In addition to the results of the LUNG SAFE [16], we here show that, irrespective of the presence of ARDS, older patients, patients with immunosuppression, patients with high non-pulmonary SOFA score, and higher heart rate are at increased risk of worse outcomes. Ventilatory support with a higher Pmax was independently associated with both increased hospital mortality and ICU mortality. This finding is in accordance with previous studies where higher Pmax was associated with worse outcomes, for example increased risk of ventilator-induced lung injury (VILI) [26, 27], and increased mortality in patients without ARDS [13] and those with ARDS [16, 21, 28, 29].
ΔP was only associated with ICU mortality and not with in-hospital mortality. It should be recognized, though, that that analysis was only possible for 343 patients, and this smaller sample size may have reduced the power so that there was no association between ΔP and in-hospital mortality. This could also be concluded from the results of the post hoc analysis of Pmax, using the same smaller cohort of patients. Nevertheless, the finding that ΔP was not associated with in-hospital mortality is in line with a recently published investigation in a cohort of patients without ARDS [30]. In addition, the small range of tidal volumes used in this cohort also led to a small range of ΔP, which could blunt the effect of ΔP on mortality, which may be much subtler than is found in patients with ARDS [9]. Similar findings came from a recently published study that failed to find an association between ΔP and mortality, even though their results show a trend for higher mortality rates with each cm H2O increase of ΔP [30]. Yet the influence of ΔP on outcome is consistent with previous reports exposing the importance of ΔP on development of pulmonary complications also in patients without ARDS undergoing general anesthesia for surgery [31], and on ventilator-induced diaphragmatic injury in critically patients receiving mechanical ventilation [32]. Similarly, experimental studies suggested an association between higher ΔP and development of VILI. In studies considering patients with ARDS, ΔP was the ventilation variable that best stratified mortality risk, even in those undergoing ECMO for refractory hypoxemia [9, 16, 28, 33, 34].
While higher VT was related to worse outcomes in critically ill patients without ARDS [5, 6, 35], and with pulmonary complications in patients undergoing general anesthesia for surgery [36,37,38], in this analysis as well as the earlier reported primary analysis of PRoVENT [11], such an association was not found. The lack of a relationship between VT and outcome in the present study likely reflects the widespread adoption of lower VT ventilation, as VT in our cohort concentrated in a narrow range around a median of 7.9 ml/kg PBW. With less patients receiving ventilation with high VT, the association between VT and outcome was no longer present. This finding is in line with the abovementioned recently published investigation in a cohort of patients without ARDS [30]. We are awaiting the results from two randomized controlled trials (RCT) testing different VT in patients without ARDS [39, 40].
A higher PEEP level was not associated with outcome in our study, and this is similar to previous findings [8, 11, 41]. However, one small randomized controlled trial found that application of ‘prophylactic’ PEEP in non-hypoxemic ICU patients not only reduced the number of hypoxemic episodes, but also the incidence of ventilator-associated pneumonia [42]. Nevertheless, most trials performed so far that addressed the effects of PEEP on outcomes in ICU patients without ARDS were relatively small and mainly assessed other outcomes than mortality, for example development of pulmonary complications [8]. Well-designed RCT are needed to address the true impact of PEEP in ICU patients without ARDS.
We suggest that the risk of ARDS can act as an additive to ‘injurious’ ventilation, which can be explained by a smaller inspiratory capacity in these patients. When the inspiratory capacity is exceeded, stress failure occurs [43, 44]; thus, the level of a certain ventilation parameter could be well within the inspiratory capacity of a patient not at risk, while exceeding the smaller capacity of a patient at risk. These findings are particularly important since PRoVENT found differences between the ventilatory management of patients at risk and not at risk of ARDS [11]. While within the inspiratory capacity, the only independent variable for VILI is dynamic strain, i.e., VT, above the inspiratory capacity, the combination of all ventilation parameters can lead to VILI and worse outcome [43, 44].
The present analysis has several limitations. It is important to note that we classified pulse oximetry as non-modifiable; however, one could argue that this is modifiable through adjustment of FiO2. Also, although respiratory variables are potentially modifiable, adjustment of the ventilator can be influenced by certain non-modifiable factors that are present at the time of adjustment. For example, PEEP is affected by hypoxemia; some protocols allow higher plateau pressures in the presence of severe acidemia, and ΔP is directly influenced by changes in the respiratory system compliance. These interactions are complex, and ventilator settings may not always turn out to be modifiable when treating a patient. Another limitation is the use of maximal airway pressure in pressure-controlled mode as a surrogate for the plateau pressure to calculate ΔP, although this was only done when there was no proof of spontaneous breathing efforts to minimize erroneous measurements. Prospective trials are needed investigating specifically the directly measured pressures in the lung, including the transpulmonary driving pressure, to explore their effect on outcome in patients without ARDS.
By identifying potentially modifiable factors in care of ICU patients, we indicate what future implementation studies should focus on to actually prove benefit of the suggested strategies on outcome. The identification of non- or less-modifiable factors points out which patients are more vulnerable and potentially may benefit most from an early start of protective treatment strategies.
Conclusion
The present analysis of a large prospective observational study suggests that higher Pmax was a potentially modifiable factor associated with increased in-hospital mortality in critically ill patients without ARDS. Whether ΔP is also a potentially modifiable factor associated with increased in-hospital mortality needs further testing in larger patient cohorts.
Abbreviations
- APACHE:
-
acute physiology and chronic health evaluation
- ARDS:
-
acute respiratory distress syndrome
- ECMO:
-
extracorporeal membrane oxygenation
- etCO2 :
-
end-tidal carbon dioxide
- FiO2 :
-
fraction of inspired oxygen
- ICU:
-
intensive care unit
- LIPS:
-
Lung Injury Prediction Score
- PBW:
-
predicted body weight
- PaCO2 :
-
partial pressure of carbon dioxide (in arterial blood)
- PaO2 :
-
partial pressure of oxygen (in arterial blood)
- PEEP:
-
positive end-expiratory pressure
- P max :
-
maximum airway pressure
- P peak :
-
peak pressure
- P plat :
-
plateau pressure
- RCT:
-
randomized controlled trial
- SAPS:
-
simplified acute physiology score
- SOFA:
-
sequential organ failure assessment
- VILI:
-
ventilator-induced lung injury
- V T :
-
tidal volume
- ΔP :
-
driving pressure
References
Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369:2126–36.
Sutherasan Y, Vargas M, Pelosi P. Protective mechanical ventilation in the non-injured lung: review and meta-analysis. Crit Care. 2014;18:211.
Putensen C, Theuerkauf N, Zinserling J, et al. Meta-analysis: ventilation strategies and outcomes of the acute respiratory distress syndrome and acute lung injury. Ann Intern Med. 2009;151:566–76.
Burns KEA, Adhikari NKJ, Slutsky AS, et al. Pressure and volume limited ventilation for the ventilatory management of patients with acute lung injury: a systematic review and meta-analysis. PLoS ONE. 2011;6:e14623. https://doi.org/10.1371/journal.pone.0014623.
Serpa Neto A, Simonis FD, Barbas CSV, et al. Association between tidal volume size, duration of ventilation, and sedation needs in patients without acute respiratory distress syndrome: an individual patient data meta-analysis. Intensive Care Med. 2014;40:950–7.
Serpa Neto A, Simonis FD, Barbas CSV, et al. Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without acute respiratory distress syndrome. Crit Care Med. 2015;43:2155–63.
Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303:865–73.
Serpa Neto A, Filho RR, Cherpanath T, et al. Associations between positive end-expiratory pressure and outcome of patients without ARDS at onset of ventilation: a systematic review and meta-analysis of randomized controlled trials. Ann Intensive Care. 2016;6:109.
Amato MBP, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372:747–55. https://doi.org/10.1056/NEJMsa1410639.
Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800.
Serpa Neto A, Barbas CSV, Simonis FD, et al. Epidemiological characteristics, practice of ventilation, and clinical outcome in patients at risk of acute respiratory distress syndrome in intensive care units from 16 countries (PRoVENT): an international, multicentre, prospective study. Lancet Respir Med. 2016;4:882–93.
Thompson BT, Hayden D, Matthay MA, et al. Clinicians’ approaches to mechanical ventilation in acute lung injury and ARDS. Chest. 2001;120:1622–7. https://doi.org/10.1378/chest.120.5.1622.
Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation. JAMA. 2002;287:345–55.
Esteban A, Frutos-Vivar F, Muriel A, et al. Evolution of mortality over time in patients receiving mechanical ventilation. Am J Respir Crit Care Med. 2013;188:220–30.
Britos M, Smoot E, Liu KD, et al. The value of positive end-expiratory pressure and Fio2 criteria in the definition of the acute respiratory distress syndrome. Crit Care Med. 2011;39:2025–30.
Laffey JG, Bellani G, Pham T, et al. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: the LUNG SAFE study. Intensive Care Med. 2016. https://doi.org/10.1007/s00134-016-4571-5.
Serpa Neto A, Barbas CS, Artigas-Raventós A, et al. Rationale and study design of Provent-An international multicenter observational study on practice of ventilation in critically Ill patients without ARDS. J Clin Trials. 2013;3:2–7.
The ARDS Definition Task Force. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–33.
Zimmerman JE, Kramer AA, McNair DS, et al. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med. 2006;34:1297–310.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63.
Bos LD, Schouten LR, Cremer OL, et al. External validation of the APPS, a new and simple outcome prediction score in patients with the acute respiratory distress syndrome. Ann Intensive Care. 2016;6:89.
Chatburn RL, Volsko TA. Documentation issues for mechanical ventilation in pressure-control modes. Respir Care. 2010;55:1705–16.
Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342:1301–8.
Rubenfeld GD, Caldwell E, Peabody E, et al. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353:1685–93. https://doi.org/10.1056/NEJMoa050333.
Brun-Buisson C, Minelli C, Bertolini G, et al. Epidemiology and outcome of acute lung injury in European intensive care units Results from the ALIVE study. Intensive Care Med. 2004;30:51–61.
Dreyfuss D, Basset GUY, Soler P, et al. Intermittent Positive-Pressure Hyperventilation with High Inflation Pressures Produces Pulmonary Microvascular Injury in Rats. Am Rev Respir Dis. 1985;132:880–4.
Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis. 1974;110:556–65.
Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338:347–54.
Kregenow DA, Rubenfeld GD, Hudson LD, et al. Hypercapnic acidosis and mortality in acute lung injury. Crit Care Med. 2006;34:1–7.
Schmidt MFS, Amaral ACKB, Fan E, et al.: Driving pressure and hospital mortality in patients without ARDS: a cohort study. Chest 2017; 1–9.
Serpa Neto A, Hemmes SNT, Barbas CSV, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med. 2016;4:272–80.
Goligher EC, Fan E, Herridge MS, et al. Evolution of diaphragm thickness during mechanical ventilation. Impact of inspiratory effort. Am J Respir Crit Care Med. 2015;192:1080–8. https://doi.org/10.1164/rccm.201503-0620OC.
Estenssoro E, Dubin A, Laffaire E, et al. Incidence, clinical course, and outcome in 217 patients with acute respiratory distress syndrome. Crit Care Med. 2002;30:2450–6.
Serpa Neto A, Schmidt M, Azevedo LCP, et al. Associations between ventilator settings during extracorporeal membrane oxygenation for refractory hypoxemia and outcome in patients with acute respiratory distress syndrome: a pooled individual patient data analysis. Intensive Care Med. 2016;42:1672–84. https://doi.org/10.1007/s00134-016-4507-0.
Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA. 2012;308:1651–9.
Serpa Neto A, Hemmes SNT, Barbas CSV, et al. Incidence of mortality and morbidity related to postoperative lung injury in patients who have undergone abdominal or thoracic surgery: a systematic review and meta-analysis. Lancet Respir Med. 2014;2:1007–15.
Serpa Neto A, Hemmes SNT, Barbas CSV, et al. Protective versus conventional ventilation for surgery. Anesthesiology. 2015;123:66–78.
Futier E, Constantin J-M, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–37.
Simonis FD, Binnekade JM, Braber A, et al. PReVENT–protective ventilation in patients without ARDS at start of ventilation: study protocol for a randomized controlled trial. Trials. 2015;16:226.
Corporacion Parc Tauli: Corporacion Parc Tauli. Preventive Strategies in Acute Respiratory Distress Syndrome (ARDS) (EPALI). In: ClinicalTrials.gov NLM Identifier: NCT02070666.
PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology, Hemmes SNT, Gama de Abreu M, et al. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet (London, England). 2014;384:495–503.
Manzano F, Fernández-Mondéjar E, Colmenero M, et al. Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit Care Med. 2008;36:2225–31.
Protti A, Andreis DT, Milesi M, et al. Lung anatomy, energy load, and ventilator-induced lung injury. Intensive Care Med Exp. 2015;3:34.
Nieman GF, Satalin J, Andrews P, et al. Lung stress, strain, and energy load: engineering concepts to understand the mechanism of ventilator-induced lung injury (VILI). Intensive Care Med Exp. 2016;4:16.
Authors’ contributions
The members of the Steering Committee of the ‘PRactice of VENTilation in patients without ARDS study’ (PRoVENT) designed and overviewed conduct of the study and this secondary analysis. PRoVENT collaborators, consisting of National and Local Investigators, collected the data. The study report was written by the PRoVENT Writing Committee and revised by the PRoVENT Steering Committee. ASN and MJS had complete access to all study data and performed the analyses, with support from FDS, MGdA, and PP. FDS, ASN, MGdA, PP, and MJS made the final decision to submit the report for publication. ASN was the study coordinator. FDS, ASN, MGdA, PP, and MJS contributed equally to this secondary analysis of PRoVENT. All authors read and approved the final manuscript.
Acknowledgements
We are indebted to all participating research nurses, nurses, physicians, and our patients. Without this support, PRoVENT and its secondary analysis would have never have been successful.
PRoVENT: ‘PRactice of VENTilation in critically ill patients without ARDS at onset of ventilation study’ (https://sites.google.com/site/proventtrial/home).
PROVE Network: ‘PROtective VEntilation Network’ (http://www.provenet.eu). The PRoVENT Steering Committee members & Writing Committee members are listed below; Collaborators are listed in the Additional supplement.
Members of the PRoVENT Steering Committee
Ary Serpa Neto (Academic Medical Center, University of Amsterdam, Amsterdam, Netherlands; Hospital Israelita Albert Einstein, São Paulo, Brazil); Carmen SV Barbas (Hospital Israelita Albert Einstein, São Paulo, Brazil); Antonio Artigas-Raventós (Corporació Sanitaria i Universitaria Parc Taulí, Sabadell, Spain); Jaume Canet (Hospital Universitari Germans Trias I Pujol, Barcelona, Spain); Rogier M Determann (Academic Medical Center, University of Amsterdam, Amsterdam, Netherlands); Barry Dixon (St. Vincent’s Hospital, Melbourne, Australia); Goran Hedenstierna (Uppsala University, Uppsala, Sweden); Sabrine NT Hemmes (Academic Medical Center, University of Amsterdam, Amsterdam, Netherlands); Greet Hermans (University Hospital Leuven, Leuven, Belgium; KU Leuven, Leuven, Belgium); Michael Hiesmayr (Medical University Vienna, Vienna, Austria); Markus W Hollmann (Academic Medical Center, University of Amsterdam, Amsterdam, Netherlands); Samir Jaber (Saint Eloi University Hospital, Montpellier, France); Ignacio Martin-Loeches (Corporació Sanitaria i Universitaria Parc Taulí, Sabadell, Spain); Gary H Mills (Sheffield Teaching Hospital and University of Sheffield, Sheffield, UK); Rupert M Pearse (Queen Mary University of London, London, UK); Christian Putensen (University Hospital Bonn, Bonn, Germany); Werner Schmid (Medical University Vienna, Vienna, Austria); Paolo Severgnini (Insubria University, Varese, Italy); Roger Smith (St. Vincent’s Hospital, Melbourne, Australia); Tanja A Treschan (Düsseldorf University Hospital, Düsseldorf, Germany); Edda M Tschernko (Medical University Vienna, Vienna, Austria); Marcos F Vidal Melo (Massachusetts General Hospital, Harvard Medical School, Boston, USA); Hermann Wrigge (University of Leipzig, Leipzig, Germany); Marcelo Gama de Abreu (University Hospital Dresden, Technische Universität Dresden, Dresden, Germany); Paolo Pelosi (Ospedale Policlinico per la Oncologia, IRCCS per l’Oncologia, University of Genoa, Genoa, Italy); and Marcus J. Schultz (Academic Medical Center, University of Amsterdam, Amsterdam, Netherlands & Mahidol University, Bangkok, Thailand).
Members of the PRoVENT Writing Committee of this manuscript
Fabienne D. Simonis (Academic Medical Center, University of Amsterdam, Amsterdam, Netherlands); Ary Serpa Neto (Hospital Israelita Albert Einstein, São Paulo, Brazil); Marcelo Gama de Abreu (University Hospital Dresden, Technische Universität Dresden, Dresden, Germany); Paolo Pelosi (IRCCS AOU San Martino IST Hospital, University of Genoa, Genoa, Italy); Marcus J. Schultz (Academic Medical Center, University of Amsterdam, Amsterdam, Netherlands & Mahidol University, Bangkok, Thailand).
Competing interests
Rupert Pearse holds research grants and has given lectures and/or performed consultancy work for Nestle Health Sciences, Braun, Medtronic, Glaxo Smithkline, and Edwards Lifesciences and is a member of the associate editorial board of the British Journal of Anaesthesia. All other authors declared no conflicts of interest with respect to this analysis.
Availability of data and materials
Please contact corresponding author for data requests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
National coordinators of the PRoVENT study assisted local coordinators, who sought approval with their respective research ethics committees. If required, written informed consent was obtained from individual participants or their legal representative.
Funding
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional file
Additional file 1.
List of PRoVENT network collaborators. Table S1 Univariable analysis of factors associated with in-hospital mortality in patients without ARDS receiving mechanical ventilation. Table S2 Analysis of factors associated with ICU mortality in patients without ARDS receiving mechanical ventilation. Table S3 Analysis of factors associated with ICU mortality in patients without ARDS receiving mechanical ventilation considering driving pressure in the model instead of maximum airway pressure. Table S4 Analysis of factors associated with in-hospital mortality in patients without ARDS receiving mechanical ventilation considering driving pressure in the model instead of maximum airway pressure. Table S5 Analysis of factors associated with in-hospital mortality in patients without ARDS receiving mechanical ventilation considering maximum airway pressure in the subset of 343 patients in whom driving pressure could be reliably measured. Table S6 Analysis of factors associated with ICU mortality in patients without ARDS receiving mechanical ventilation considering maximum airway pressure in the subset of 343 patients in whom driving pressure could be reliably measured. Figure S1 Odds ratio of ICU mortality according to increases in one standard deviation of Pmax and in the patients at risk and not at risk of ARDS.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Simonis, F.D., Barbas, C.S.V., Artigas-Raventós, A. et al. Potentially modifiable respiratory variables contributing to outcome in ICU patients without ARDS: a secondary analysis of PRoVENT. Ann. Intensive Care 8, 39 (2018). https://doi.org/10.1186/s13613-018-0385-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-018-0385-7