Abstract
Background
We sought to determine the effect of emergency department length of stay (ED-LOS) on outcomes in stroke patients admitted to the Neurological Intensive Care Unit (NICU).
Methods
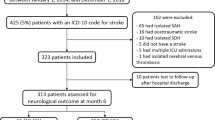
We collected data on all patients who presented to the ED at a single center from 1st February 2005 to 31st May 2007 with acute ischemic stroke (AIS), intracerebral hemorrhage (ICH), or transient ischemic attack (TIA) within 12 h of symptom onset. Data collected included demographics, admission/discharge National Institutes of Health Stroke Scale (NIHSS), discharge modified Rankin Score (mRS), and total ED length of stay. The effect of ED-LOS on discharge mRS, discharge NIHSS, and hospital LOS was assessed by logistic regression. Poor outcome was defined as mRS ≥4 at discharge.
Results
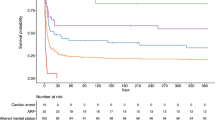
Of 519 patients presenting to the ED, 75 (15%) were critically ill and admitted to the NICU (mean age 65 ± 14 years, 31% men, and 37% Hispanic). Admission diagnosis included AIS (49%), ICH (47%), TIA (1%), and others (3%). Median ED-LOS was 5 h (IQR 3–8 h) and median hospital LOS was 7 days (IQR 3–15 days). In multivariate analysis, predictors of poor outcome included admission ICH (OR, 2.1; 95% CI, 1.1–4.3), NIHSS ≥6 (OR, 6.4; 95% CI, 2.3–17.9), and ED-LOS ≥5 h (OR, 3.8; 95% CI, 1.6–8.8). There was no association between ED-LOS and discharge NIHSS among survivors or total hospital LOS.
Conclusion
Among critically ill stroke patients, ED-LOS ≥5 h before transfer to the NICU is independently associated with poor outcome at hospital discharge.
Similar content being viewed by others
References
Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–83.
Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77.
Antman EM, Hand M, Armstrong PW, et al. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2008;51:210–47.
Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115:e478–534.
Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327.
Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med. 2001;29:635–40.
Mirski MA, Chang CW, Cowan R. Impact of a neuroscience intensive care unit on neurosurgical patient outcomes and cost of care: evidence-based support for an intensivist-directed specialty ICU model of care. J Neurosurg Anesthesiol. 2001;13:83–92.
Suarez JI, Zaidat OO, Suri MF, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med. 2004;32:2311–7.
Suarez JI. Outcome in neurocritical care: advances in monitoring and treatment and effect of a specialized neurocritical care team. Crit Care Med. 2006;34:S232–8.
Varelas PN, Eastwood D, Yun HJ, et al. Impact of a neurointensivist on outcomes in patients with head trauma treated in a neurosciences intensive care unit. J Neurosurg. 2006;104:713–9.
Fromm RE Jr, Gibbs LR, McCallum WG, et al. Critical care in the emergency department: a time-based study. Crit Care Med. 1993;21:970–6.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7.
Brott T, Adams HP Jr, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20:864–70.
Sacco RL, Boden-Albala B, Chen X, Lin IF, Kargman DE, Paik MC. Relationship of 6-month functional outcome and stroke severity: implications for acute stroke trials From the Northern Manhattan Stroke Study. Neurology. 1998;50:A327.
Dhamoon MS, Sciacca RR, Rundek T, Sacco RL, Elkind MS. Recurrent stroke and cardiac risks after first ischemic stroke: the Northern Manhattan Study. Neurology. 2006;66:641–6.
Laowattana S, Oppenheimer SM. Protective effects of beta-blockers in cerebrovascular disease. Neurology. 2007;68:509–14.
Elkind MS, Flint AC, Sciacca RR, Sacco RL. Lipid-lowering agent use at ischemic stroke onset is associated with decreased mortality. Neurology. 2005;65:253–8.
Saukkonen KA, Varpula M, Rasanen P, Roine RP, Voipio-Pulkki LM, Pettila V. The effect of emergency department delay on outcome in critically ill medical patients: evaluation using hospital mortality and quality of life at 6 months. J Intern Med. 2006;260:586–91.
Trzeciak S, Rivers EP. Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J. 2003;20:402–5.
Rincon F, Mayer SA. Neurocritical care: a distinct discipline? Curr Opin Crit Care. 2007;13:115–21.
Acknowledgments
This paper was supported by grants NINDS/NIH P50 NS049060 (SPOTRIAS). Dr. Rincon was a SPOTRIAS Fellow.
Conflict of interest statement
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rincon, F., Mayer, S.A., Rivolta, J. et al. Impact of Delayed Transfer of Critically Ill Stroke Patients from the Emergency Department to the Neuro-ICU. Neurocrit Care 13, 75–81 (2010). https://doi.org/10.1007/s12028-010-9347-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-010-9347-0