Abstract
Background
As the population ages, more older adults are presenting for surgery. Age-related declines in physiological reserve and functional capacity can result in frailty and poor outcomes after surgery. Hence, optimizing perioperative care in older patients is imperative. Enhanced Recovery After Surgery (ERAS) pathways and Minimally Invasive Surgery (MIS) may influence surgical outcomes, but current use and impact on older adults patients is unknown. The aim of this study was to provide evidence-based recommendations on perioperative care of older adults undergoing major abdominal surgery.
Methods
Expert consensus determined working definitions for key terms and metrics related to perioperative care. A systematic literature review and meta-analysis was performed using the PubMed, Embase, Cochrane Library, and Clinicaltrials.gov databases for 24 pre-defined key questions in the topic areas of prehabilitation, MIS, and ERAS in major abdominal surgery (colorectal, upper gastrointestinal (UGI), Hernia, and hepatopancreatic biliary (HPB)) to generate evidence-based recommendations following the GRADE methodology.
Result
Older adults were defined as 65 years and older. Over 20,000 articles were initially retrieved from search parameters. Evidence synthesis was performed across the three topic areas from 172 studies, with meta-analyses conducted for MIS and ERAS topics. The use of MIS and ERAS was recommended for older adult patients particularly when undergoing colorectal surgery. Expert opinion recommended prehabilitation, cessation of smoking and alcohol, and correction of anemia in all colorectal, UGI, Hernia, and HPB procedures in older adults. All recommendations were conditional, with low to very low certainty of evidence, with the exception of ERAS program in colorectal surgery.
Conclusions
MIS and ERAS are recommended in older adults undergoing major abdominal surgery, with evidence supporting use in colorectal surgery. Though expert opinion supported prehabilitation, there is insufficient evidence supporting use. This work has identified evidence gaps for further studies to optimize older adults undergoing major abdominal surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The global population is aging. The increases in the proportion of older adults and in life expectancy have led to a proportional increase in older patients presenting for surgery [1]. There is inherent decline in physiological reserve and functional capacity with age that increase the likelihood of older adults being frail; in turn, frailty is associated with poor outcomes, longer hospital lengths of stays (LOS), loss of independence, and a high risk of morbidity and mortality after surgery [2]. Frailty is associated with advanced age, but chronological age does not accurately predict surgical outcomes [3]. The complex relationship between biology, environment, and social support paired with variable adoption of Enhanced Recovery After Surgery (ERAS) protocols and Minimally Invasive Surgery (MIS) may more accurately influence surgical outcomes in the older adult. Thus, optimizing perioperative care in older adults undergoing major abdominal surgery is imperative.
Perioperative optimization initially centered on ERAS, multimodal pathways introduced in the 1990’s to hasten time to recovery after surgery [4]. Since their introduction, ERAS protocols have been adopted by most surgical service lines, with universal reductions in LOS, morbidity, and post-discharge nursing needs by 30–50%. Adding MIS to an ERAS protocol further optimizes clinical outcomes and the recovery benefit [5]. More recently, attention has focused on prehabilitation, where interventions work to improve functional capability prior to a surgical procedure [6]. There is data to support prehabilitation improving functional capacity both preoperatively and postoperatively [7]. The principles of ERAS and prehabilitation are particularly well-suited for older adult, who may run a higher risk of complications [8]. Despite growing awareness of ERAS and prehabilitation, there is variation in their use and no clear guidance on the optimal preoperative and postoperative optimization pathways [9]. There is also wide variations in the incidence of co-morbidities in this population, heterogeneity in how elderly are defined, contention on the specific elements and application of ERAS and prehabilitation programs, and the metrics for measuring success. Therefore, a consensus on recommendations and high-level evidence to guide the usage of ERAS, prehabilitation, and perioperative optimization in older adults undergoing major abdominal surgery is warranted.
The goal of this work was to provide evidence-based recommendations to optimize perioperative care in elderly patients undergoing major abdominal surgery.
Methods
Participants
A steering group comprised of 24 stakeholders with experience in evidence synthesis, guideline development methodology and perioperative optimization from the Society of American Gastrointestinal and Endoscopic Surgery (SAGES) and European Association of Endoscopic Surgery (EAES), a methodologist with expertise in guideline development (S.A.), a medical librarian (H.A.B.), and a SAGES Guidelines Committee Fellow (A.R.) was convened in September 2020. As the proposed target audience of this study is patients and their surgeons, this study followed a patient-centered perspective, and included a patient representative (D.K.) in all phases to guide patient preferences. All participants were well versed in ERAS and prehabilitation principles, with experience in the development and application appropriate to their respective role.
Time frame
The first online conference on October 24th, 2021, focused on team introductions, review of the process review, and expectations. An in-person consensus meeting was held in February 2022 at the EAES Winter Meeting, where articles and results of the systematic review explicitly created for the guideline and pertinent to a Key Question were provided to panel members for review. A consensus conference was held at the SAGES 2022 annual meeting, presenting an interim analysis of the systematic review. After presenting the data and audience discussion, participants voted on the proposed recommendations. The final voting meeting was held in June 2022. The panel subsequently convened for several virtual panel meetings between 2022 and 2023, where the literature search was updated, the GRADE evidence profile and summary of findings tables were reviewed, and the Evidence-to-Decision (EtD) tables and specific recommendations were generated. This was followed by critical review and revision by the authors and SAGES executive board review and approval in the latter part of 2023 and 2024.
Selection of key questions and outcomes of interest
Perioperative optimization of older adults undergoing major abdominal surgery was divided into four main topic areas: (i) definitions of key terms, application, and outcomes, (ii) preoperative optimization, (iii) MIS, and (iv) use of postoperative patient optimization and ERAS programs. For topic area i, an appraisal of terminology was performed, reviewing the literature and proposing sets of definitions. This was expanded to include all relevant nomenclature related to the topics, such as the definition, assessment and implications of frailty. Topic areas ii, iii, and iv were subdivided into PICO (Patient, Intervention, Comparator, Outcomes) pre-defined Key Questions (KQs). Each KQ was formulated, revised, and unanimously approved by the steering group. Each KQ stem was separately assessed in colorectal, upper gastrointestinal, hepatobiliary pancreatic and hernia surgery. Then, the panel determined which outcomes should be considered based on their clinical and lived experience, considering both the patient and surgeon perspective in decision making. The primary outcomes adopted were LOS, readmissions and early complications.
Data analysis
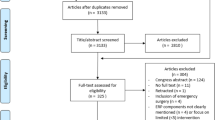
A systematic review and meta-analysis of articles collected from PubMed, Embase, Cochrane Library, and Clinicaltrials.gov databases was conducted and reported using PRISMA-S standards and written according to the SAGES Guidelines Committee’s standard operating procedure (Supplement 1) [10, 11]. For topic area i, the panel collectively selected the terminology that required refinement, and voted on working definitions of selected terminology, recommendations for application of each, and the outcomes for reporting results in studies focused on perioperative care of older adults. A modified Delphi method was used for consensus on agreement, with an agreement of 70% or more considered to reach consensus. For topic areas ii, iii, and iv, literature searches were conducted for each KQ individually, then consolidated under their overarching topic area. Identified studies were then reviewed by two independent reviewers to determine which areas were mapped into each KQ. The Covidence® platform (Veritas Health Ltd, Australia) [12] was used for title and abstract screening, followed by full-text review and data extraction for relevant papers. Two independent researchers assessed the eligibility of all studies, with a project lead (DK) resolving cases of disagreement. From the data extraction and Forest Plot results (generated using Cochrane RevMan [21]), evidence-based recommendations for each KQ were generated. Recommendations were graded using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach [13,14,15] and the GRADE guideline development tool [16]. Where applicable, the Appraisal of Guidelines Research & Evaluation tool (AGREE II) [17] and Essential Reporting Items for Practice Guidelines in Healthcare (RIGHT) checklist was used [18]. Cochrane Risk of Bias and Newcastle–Ottawa Scale tools were used to assess study quality. [19, 20]. For results with insufficient evidence, expert opinion from a consensus-based approach from the steering group was recorded.
Inclusion and exclusion criteria
Clinical studies in older adults (over 65 years) undergoing major abdominal surgery, defined as upper or lower gastrointestinal, hepatobiliary, or hernia, and describing preoperative optimization, use of minimally invasive approaches, postoperative optimization, and ERAS were included. The study designs considered were: randomized controlled trials; comparative non-randomized studies; prospective and retrospective case series (of more than 10 patients; and systematic review and meta-analysis. Articles were eligible for inclusion if published between January 1, 2000, to February 27, 2023. Articles were excluded if they were studies on children (under 18 years of age), narrative reviews, commentary or editorial formats, animal studies, or if published in non-English language.
Evidence appraisal
Methods outlined in the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach handbook [22] were used to appraise the available evidence. GRADEPro evidence tables were created from the groups’ data extraction and analysis. The highest level of data available was used for tables; less rigorous data addressing the same outcomes was not considered nor used in decision making. The group judged the certainty of evidence using the risk of bias across available studies, and the certainty of evidence was evaluated at the individual study level. If concerns arose in any of the risk of bias assessments certainty was downgraded [19]. Data were imported for each KQ into Evidence to Decision (EtD) tables (Supplement 4), which served as the framework through which recommendations were developed.
Development of recommendations
Outcomes from the Evidence to Decision (EtD) Tables were reviewed by the group as desirable or undesirable effects for the interventions [16]. The group then discussed the magnitude of desirable and undesirable effects, listed as anticipated absolute effects for the magnitude and 95% confidence interval (CI), the certainty of evidence, variation in values that may be assigned to outcomes, and the balance of these effects. Absolute percentage differences were calculated by the GRADEPro software based on the available data. The group voted on the overall certainty of evidence based on the risk of bias, inconsistency, indirectness, and imprecision of individual outcomes. After choosing whether the balance of these considerations favored the intervention, comparator, or combination, the panel discussed the acceptability and feasibility of this judgment.
For each decision, both the available evidence as well as pertinent additional considerations taken either from panel experience or interpretation of evidence were discussed. Based on the balance of effects and the acceptability and feasibility of a favored option, the panel voted on the final recommendation for that KQ. While serial voting was used to come to a consensus on individual components of the EtD, a supermajority (defined as ≥ 80% agreement), was used as the cut-off for consensus agreement. GRADE guidelines were followed to determine strong versus conditional recommendations. A strong recommendation occurred when the true effect was close to the estimated effect. If there was some uncertainty in the evidence, the strength of the final recommendation was downgraded as conditional. If there was no identified evidence for a KQ, an expert recommendation was stated based on the consensus of the experts within the steering group. Subgroups were addressed in the discussion for the justification for each recommendation and are specified for each KQ.
Guideline document review
All recommendations drafted were distributed to the full steering group for review and revision of the content, to ensure completeness, and accuracy. For external review, the manuscript was sent to the SAGES Guidelines Quality Assurance Task Force to minimize the introduction of bias in the recommendations. The final document was submitted to the SAGES Board for approval and published online (https://www.sages.org) for public comment an additional quality assurance.
Results
Evidence synthesis was conducted across the three subjects of prehabilitation, MIS, and ERAS, resulting in 20,106 total papers reviewed, with 10,901 unique items screened across the 24 KQs.
Terminology, recommendations for application, and outcomes
From the evidence synthesis, the group agreed on terminology that required standardization across the population level and perioperative periods (ERAS), then collectively voted on definitions and recommendations for their application in studies on older adults undergoing major abdominal surgery. All working definitions are seen in Table 1. In brief, any person aged 65 years or older meets the definition of “older adult”. “Older adult” in used in place of elderly per age inclusive language guidelines from the American Medical Association and Gerontological Society on Aging. Frailty was agreed as a state of increased vulnerability to stress from aging-associated decline in reserve and function across multiple physiologic systems. The panel agreed that any study on perioperative care of older adults should include one of the many available indices to measure frailty and assign a score to each patient, but could not reach consensus on any individual instrument. The panel recommended that frailty and comorbidity be separated and reported individually. The panel agreed that a risk score should be assessed for comorbidity burden and the name and score should be detailed, but there was no consensus on specific assessment tools.
Alcohol and smoking cessation were agreed upon as no consumption or any alcohol-containing beverage or nicotine-containing product for 4 weeks prior to surgery. Anemia in adults was agreed as a hemoglobin level less than 13 g/dL in men or less than 12 g/dL in women. The panel agreed that anemia should be included in any study reporting perioperative care in older adult population and corrected before any operation, but not on the timing, level to correct to, or the need to reassess. MIS was agreed to cover any laparoscopic, robotic, or assisted procedure; there was no agreement on including endoluminal procedures. The panel agreed that use of MIS versus open should be reported, and the type of MIS (laparoscopic or robotic or assisted) should be stated. Conversion to open was agreed as the inability to complete the dissection through an MIS approach, usually requiring an incision larger than that required to remove the specimen. If a conversion from MIS to open occurred, it should be clearly reported. Prehabilitation was agreed upon as the process that occurs between the time of diagnosis and the beginning of treatment, and includes physical, nutritional and psychological assessments to prepare a patient for the stress of surgery by improving their preoperative functional status. The panel agreed that a prehabilitation program should be implemented in elderly patients undergoing surgery but were not able to agree upon the timing or elements for a prehabilitation program from the literature. Prehabilitation was distinguished from ERAS—multimodal perioperative care pathways designed to achieve early recovery after major surgery by using evidence-based interventions—as ERAS protocols encompass components across the preoperative, intraoperative and postoperative periods and prehabilitation programs occur before surgery. There was a strong recommendation to adopt ERAS protocols in all elderly patients undergoing elective major abdominal surgery. The group recommended the specific elements used and compliance with ERAS protocol elements should be described. There was consensus that the outcomes that should be reported in perioperative care of older adults undergoing major abdominal surgery included: delirium; postoperative complications; LOS; and readmission. None of the screened articles investigated the effect of any of the above interventions on postoperative quality of life (QoL) in older adult, and given the heterogeneity of different QoL tools, the expert panel could not make a recommendation for including QoL. The quality of evidence and strength of the recommendations are seen in Table 2.
Key questions
With the terminology agreed upon, each KQ stem was for colorectal, upper gastrointestinal, hepatobiliary pancreatic and hernia surgery separately. Search strings and full PRIMSA flow diagrams for each KQ are seen in Supplement 2. Meta-analysis was only conducted in the topic areas of MIS and ERAS as there were not enough quality data in the prehabilitation section.
Prehabilitation (topic area ii, KQ1–KQ16)
Prehabilitation and preoperative sections (topic area ii, KQ 1–16) were addressed according to item-specific KQ. Literature search, review and synthesis was performed, resulting in 169 studies assessed at the full-text level. 144 were excluded and 9 items were duplicates leaving 16 unique studies across all KQs among which 5 RCT and 11 observational studies were found. Most studies were considered at low to moderate risk of bias by the reviewers, the main characteristics are summarized in Supplement 3 and underpinned the following weak recommendations.
KQ1: Should a prehabilitation (vs. no prehabilitation) program be used in elderly patients undergoing colorectal surgery?
Recommendation
The panel recommends that a prehabilitation program be used prior to colorectal surgery in elderly patients (Expert opinion based on low certainty of evidence).
Summary of evidence
70 studies were assessed at the full-text level and 16 were identified for KQ1. Of the 16, five were RCTs, eight retrospective papers and three prospective case–control studies. Ten studies involved patients undergoing colorectal surgery, while data about colorectal procedures were extracted from six other studies. Fifteen studies analyzed the 30-day complications, thirteen the LOS and six the 30-day readmission rates [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39].
Benefits of intervention
The analysis of 30-day complications showed better results in the prehabilitation group, including the 30-day postoperative LOS. However, the differences between the two groups were not statistically significant. Thirty-day readmission rates were analyzed by only six papers, showing no statistically significant differences between the two groups. [25, 28, 33, 35,36,37].
Harms and burdens
None of the analyzed outcomes showed undesirable effects for the intervention, which the panel considered critical.
Certainty in the evidence of effects
Low certainty of evidence was defined for all outcomes. Although the group considered the majority of included studies with low risk of bias and 5 RCTs have been included in the analysis, the heterogeneity among the included studies was very high. Similarly, the definition of elderly was heterogeneous, as well as definitions of prehabilitation programs. Finally, postoperative outcomes derived from colorectal procedures were merged with other types of surgical procedures in some included studies, thus the real results of the comparison between prehabilitation and no-prehabilitation program on postoperative outcomes are difficult to obtain.
Conclusions and research recommendations
Although there are limitations in the volume and strength of the current literature, the panel members agreed from the data and clinical experience that the application of a prehabilitation program can positively impact postoperative outcomes in elderly patients undergoing colorectal procedures, especially in terms of 30-day postoperative complications, LOS, and 30-day readmission rates.
KQ2: Should a prehabilitation (vs. no prehabilitation) program be used in elderly patients undergoing Upper GI surgery?
Recommendation
The panel recommends a prehabilitation program be used prior to Upper GI surgery in elderly patients (Expert opinion based on low certainty of evidence).
Summary of evidence
24 studies were assessed at the full-text level with three studies addressing this question. In two studies, upper GI surgery patients were included, but no data could be extracted on postoperative outcomes related specifically to the prehabilitation in older adults undergoing upper GI surgery [24, 34]. One prospective study specifically analyzed the adoption of a prehabilitation program in older adults undergoing upper GI surgery and was included in the final analysis [39].
Benefits of intervention
In the included study, the analysis of 30-day complications showed similar results between the two groups, while no data were reported in terms of LOS and 30-day readmissions.
Harms and burdens
The 30-day postoperative complications did not show undesirable effects for the intervention, which the panel considered critical.
Certainty in the evidence of effects
Low certainty of evidence was defined for the 30-day postoperative complications. The included study had a high risk of bias due to unpaired comparison between the groups.
Conclusions and research recommendations
Based on the data and clinical experience, the panel members recommend that a prehabilitation program be used before surgery to positively impact postoperative outcomes after upper GI surgery in older adults. Future research is needed to develop stronger evidence in this topic area.
KQ3: Should a prehabilitation (vs. no prehabilitation) program be used in elderly patients undergoing hepatobiliary pancreatic (HPB) surgery?
Recommendation
The panel cannot recommend that a prehabilitation program be used in elderly patients prior to HPB surgery (Expert opinion based on very low certainty of evidence).
Summary of evidence
28 studies were assessed at the full-text level. Three studies included patients who underwent HPB surgery [24, 33, 34]. Data on 30-day mortality, LOS and 30-day readmissions were retrieved, but results related specifically to the HPB surgery could not be extracted.
Benefits of intervention
There was no data on postoperative complications directly related to the HPB surgery that could be extracted from the included studies,
Certainty in the evidence of effects
Low certainty of evidence was defined for the analyzed outcomes. Despite the presence of an RCT, it was not possible to extract evidenced-based data related to HPB surgery.
Conclusions and research recommendations
There was no evidence to support a recommendation for prehabilitation, but from the clinical experience of the panel members, it was suggested that a prehabilitation program could positively impact postoperative complications in elderly patients undergoing HPB surgery. Further research is needed to develop evidence in this topic area.
KQ4: Should a prehabilitation (vs. no prehabilitation) program be used in elderly patients undergoing Hernia surgery?
Recommendation
The panel cannot recommend that a prehabilitation program be used in elderly patients prior to Hernia surgery (Expert opinion based on very low certainty of evidence).
Summary of evidence
16 studies were assessed at the full-text level. One study made it to extraction in this KQ [33], but no study met the inclusion criteria to be included in the final analysis.
Conclusions and research recommendations
There is no evidence in the literature to support a prehabilitation program in older adults undergoing hernia surgery, but from clinical experience the panel members suggested adoption of a prehabilitation program in older adults undergoing hernia surgery could lead to improved postoperative outcomes. Further research is needed to develop evidence in this topic area.
KQ5-8: Should perioperative optimization (vs. no optimization) of anemia be used in elderly patients undergoing major abdominal surgery (including Colorectal, Upper GI, Hernia, and HPB)?
Recommendation
The panel cannot recommend that anemia be corrected prior to Colorectal, Upper GI, Hernia, or HPB surgery in elderly patients (Expert opinion based on low certainty of evidence).
Summary of evidence
Only one prospective study was included in the analysis, involving 248 abdominal surgery patients. The patients were not matched, and the relevant outcomes were 30-day complications and LOS [29].
Benefits of intervention
The comparison between the two groups showed no significant difference in terms of 30-day postoperative complications or LOS.
Certainty in the evidence of effects
Low certainty of evidence based on a prospective study. The panel considered the sample small in size and the results preliminary.
Conclusions and research recommendations
There is no evidence in the literature reviewed to support correction of anemia in older adults undergoing colorectal, upper GI, hernia, or HPB surgery. Based on the panels experience, members suggest correcting anemia prior to major abdominal surgery in elderly patients. Further research is needed to develop evidence in this topic area.
KQ9-12 Should smoking cessation (vs. no smoking cessation) be applied in older adult patients undergoing Colorectal, Upper GI, Hernia, or HPB surgery?
Recommendation:
The panel cannot recommend perioperative smoking cessation prior to colorectal, Upper GI, Hernia, or HPB surgery in elderly patients (Expert opinion based on very low certainty of evidence).
Summary of evidence
Six studies were identified from the screening as eligible to be included in the analysis, but after the full-text review, no study met the inclusion criteria.
Conclusions and research recommendations
The effect of smoking cessation on outcomes after surgery is well accepted in general, but no study in the current perioperative literature focused on this aspect in older adults. While there is no evidence to support smoking cessation in older adults prior to colorectal, upper GI, hernia, or HPB surgery in elderly patients, the clinical experience of the panel members suggests preoperative smoking cessation 4 weeks before major abdominal surgery in older adults, and future research to develop evidence on this topic area.
KQ13-16: Should alcohol cessation (vs. no alcohol cessation) be applied in older adult patients undergoing Colorectal, Upper GI, Hernia, or HPB surgery?
Recommendation
The panel cannot recommend alcohol cessation in elderly patients undergoing Colorectal, Upper GI, Hernia, or HPB surgery (Expert opinion based on very low certainty of evidence).
Summary of evidence
No studies were identified regarding alcohol cessation or the comparison between alcohol cessation versus no alcohol cessation/ active alcohol consumption in elderly patients undergoing colorectal, upper GI, hernia, or HPB surgery.
Conclusions and research recommendations
It is generally accepted that alcohol cessation is associated with better outcomes after surgery than no alcohol cessation. However, there was no evidence found in the literature to support alcohol cessation in older adults prior to colorectal, upper GI, hernia, or HPB surgery over no alcohol cessation. It was noted that various definitions exist for alcohol excess, which risks heterogeneity. Based on the panel experience, members suggest stopping perioperative alcohol intake in elderly patients 4 weeks before undergoing major abdominal surgery, and future research to develop evidence on this topic area.
Role of MIS in older adults (topic area iii, KQ17-KQ20)
KQ17: Should MIS (vs open) Colorectal surgery be used in older adults?
Recommendation
The panel recommends MIS over open surgery in elderly patients undergoing Colorectal surgery (Conditional recommendation based on moderate certainty of evidence).
Summary of evidence
349 studies were assessed at the full-text level. 197 were extracted, and 82 included in the analysis. Among the 82 studies included in the systematic review and meta-analysis, 81, 72 and 7 observational studies were selected for the outcomes of 30-day complications, LOS and 30-day readmission, respectively [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121].
Benefits of intervention
The outcomes for MIS compared to open colorectal surgery were:
-
1.
30-day complications: (81 observational studies of 131,241 participants) absolute difference 101 fewer patients per 1000 (95% CI 121 fewer to 78 fewer) [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65, 67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121]
-
2.
Length of stay: (72 observational studies of 87,465 participants) mean difference 2.48 days fewer (95% CI 2.9 fewer to 2.05 fewer) [40,41,42,43,44,45,46,47,48, 51, 53,54,55,56,57,58,59,60,61,62, 64, 65, 67,68,69,70,71,72,73,74,75,76,77,78, 80,81,82, 84,85,86,87,88,89,90,91,92,93,94,95, 97,98,99,100,101,102,103,104, 106,107,108,109,110,111,112,113,114,115,116,117,118, 120, 121]
-
3.
30-day readmission: (7 observational studies of 16,075 participants) absolute difference 15 fewer patients per 1000 (95% CI 46 fewer to 36 more) [54, 66, 72, 82, 110, 111, 117]
The evidence is primarily based on short-term observational studies. However, the panel recognized the impact of the large number of studies and patients included (Supplement 5).
Harms and burdens
None of the outcomes showed undesirable effects for the intervention.
Certainty in the evidence of effects
The certainty of evidence was evaluated as moderate based on the outcomes of 30-day complications, LOS and 30-day readmission. These outcomes were limited by containing unmatched data and burdened by high heterogeneity (Supplement 4).
Decision criteria and additional considerations
While MIS is widely accepted as the gold standard for colorectal surgery, concerns remain about its use in older adult population, where cardiac and pulmonary comorbidities could affect ventilation, insufflation, and hemodynamic safety. The expert panel came to its opinion considering colorectal disease as a whole, without making distinctions on malignant or benign conditions or the location of the disease process in the lower GI tract.
Conclusions and research recommendations
From the data and clinical experience, the panel recommends MIS over open colorectal surgery in older adults. The choice for either approach should always be made on a patient-by-patient basis, considering specific comorbidities, expertise, and equipment availability.
KQ18: Should MIS (vs open) Upper GI surgery be used in older adults?
Recommendation
The panel recommends that elderly adults undergoing Upper GI surgery may benefit from MIS over open surgery (Conditional recommendation based on very low certainty of evidence).
Summary of evidence
251 studies were assessed at the full-text level. 99 were extracted. The analysis considered 18 observational studies for the outcome of 30-day complications, 14 observational studies for the outcome LOS and 2 observational studies for the outcome of 30-day readmission [122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139]. No RCT evidence met the inclusion criteria.
Benefits of intervention
Three outcomes were considered with desirable anticipated effects for MIS as compared to the open technique, including 30-day complications, LOS, and 30-day readmission. Overall, the panel evaluated these outcomes as critical.
-
1.
30-day complications: (18 observational studies with 10,431 participants) absolute difference 71 fewer patients per 1000 (95% CI 98 fewer to 40 fewer) [122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139]
-
2.
Length of stay: (14 observational studies with 4134 participants) mean difference 2.84 days fewer (95% CI 4.24 fewer to 1.45 fewer) [122, 123, 125,126,127, 129,130,131,132, 134,135,136, 138, 139]
-
3.
30-day readmission: (2 observational studies with 328 participants) absolute difference 47 fewer patients per 1000 (95% CI 66 fewer to 8 more) [123, 126]
Short-term observational studies were taken into consideration for the present evidence.
Harms and burdens
None of the outcomes showed undesirable effects for the intervention.
Certainty in the evidence of effects
The certainty of evidence was considered very low based on three selected outcomes (30-day complications, LOS and 30-day readmission). These outcomes were limited by unmatched data; interval estimates cross statistical and clinical significance (Supplement 4).
Decision criteria and additional considerations
The analysis focused on overall upper GI diseases, without any discrimination in terms of etiology (i.e., oncologic or functional) or localization along the upper gut, as most of the studies which met inclusion criteria focused on gastric rather than esophageal conditions. Moreover, the panel decided not to include bariatric-related gastric resection in this guideline, as it was already expanded on a previous review from the SAGES Guideline Committee [140].
Conclusions and research recommendations
From the literature and clinical experience, the panel recommends that MIS over open surgery be used in elderly patients undergoing upper GI surgery. Any further decision on which technique to be used should be made on a patient-centered basis, always considering specific comorbidities and conditions.
KQ19: Should MIS (vs open) HPB surgery be used in older adults?
Recommendation:
The panel recommends that elderly adults undergoing HPB surgery may benefit from MIS over open surgery (Conditional recommendation based on low certainty of evidence).
Summary of evidence
223 studies were assessed at the full-text level, including 8 that were added during the extraction process. 86 studies were extracted. Only observational evidence was found to meet the inclusion criteria for selected outcomes in 37 studies. The analysis considered 36 studies for the outcome of 30-day complications, 25 articles for the outcome LOS and 5 observational studies for the outcome of 30-day readmission [52, 124, 141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175]. No RCT evidence was included.
Benefits of intervention
Outcomes considered in this analysis showed desirable anticipated effects for MIS as compared to the open technique, listed as follows. Overall, the panel evaluated these outcomes as critical.
-
1.
30-day complications: (36 observational studies with 6222 participants) absolute difference 122 fewer patients per 1000 (95% CI 152 fewer to 88 fewer) [52, 124, 141,142,143,144,145, 147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175]
-
2.
Length of stay: (25 observational studies with 5862 participants) mean difference 3.85 days lower (95% CI 5.12 lower to 2.59 lower) [141,142,143,144,145,146,147,148,149,150,151,152,153, 156,157,158, 161,162,163, 166,167,168, 173,174,175]
-
3.
30-day readmission: (5 observational studies with 2180 participants) absolute difference 21 fewer patients per 1000 (95% CI 50 fewer to 21 more) [146, 161, 167, 168, 174]
Short-term observational studies were taken into consideration for the present evidence.
Harms and burdens
None of the outcomes showed undesirable effects for the intervention.
Certainty in the evidence of effects
Low certainty of evidence was considered for 30-day complications and LOS. Very low certainty of evidence was defined for 30-day readmission. The outcome of 30-day complications was marked by moderate heterogeneity. However, intervals are estimated beyond decision thresholds. 30-day readmissions interval estimates cross decision thresholds (Supplement 4).
Decision criteria and additional considerations
The analysis developed the Key Question of treating all HPB pathologies without distinction on the etiology or localization of disease, due to the minimal number of studies on this topic related to HPB disease. As most of the articles meeting inclusion criteria dealt with benign cholecystitis conditions, the panel unanimously voted to submit a single, comprehensive recommendation on the subject.
Conclusions and research recommendations
From the evidence and clinical experience, the panel recommends MIS over open surgery for elderly patients undergoing HPB surgery. The recommendation was defined as conditional due to low and very low certainty of evidence as well as for the intrinsic variety of the topics expanded on the present KQ. Further research is needed to develop evidence in this topic area beyond cholecystectomy for benign disease.
KQ20: Should MIS (vs open) Hernia surgery be used in older adults?
Recommendation
The panel recommends that elderly adults undergoing Hernia surgery may benefit from MIS over open surgery (Conditional recommendation based on very low certainty of evidence).
Summary of evidence
67 studies were assessed at the full-text level and 18 were extracted. The analysis considered 5 observational studies for the outcome of 30-day complications and 5 articles for the outcome LOS [176,177,178,179,180]. In this, four articles are unique and the Neupane study is listed twice under complications, once for inguinal and once for ventral hernia surgery. No study met the inclusion criteria for the outcome of 30-day readmission. No RCT evidence was included.
Benefits of intervention
The analysis showed desirable anticipated effects for MIS in hernia surgery as compared to the open technique. Overall, the panel evaluated these outcomes as critical.
-
1.
30-day complications: (5 observational studies with 29,285 participants, with the Neupane article is included once for inguinal and once for ventral surgery) absolute difference 30 fewer patients per 1000 (95% CI 58 fewer to 20 more) [176,177,178,179]
-
2.
Length of stay: (5 observational studies with 29,040 participants) mean difference 5.08 days fewer (95% CI 10.6 fewer to 0.44 more) [176,177,178,179,180]
Short-term observational studies were taken into consideration for the present evidence.
Harms and burdens
There were no outcomes with undesirable effects for the intervention. However, none of the included studies reported 30-day readmission rates, which was a critical outcome.
Certainty in the evidence of effects
Certainty of evidence was considered very low both for 30-day complications and LOS outcomes. The first was affected not only by a high risk of bias in 2 out of 3 studies but also from considerable heterogeneity and intervals estimates; the latter had a high or unclear risk of bias in 4 out of 5 articles, characterized by tremendous heterogeneity and intervals estimates. (Supplement 4).
Decision criteria and additional considerations
In the present analysis, overall hernia surgery was taken into consideration irrespective of the localization of the defect or the difference between primary or recurrent abdominal wall repair. None of the included studies considered the 30-day readmission rate, significantly restraining the strength of the recommendation.
Conclusions and research recommendations
Based on the evidence and clinical experience, the panel recommends MIS over open surgery for elderly adults undergoing hernia surgery. The recommendation was defined as conditional due to low and very low certainty of evidence. The decision on whether the MIS technique should be preferred over the traditional approach should always consider specific patients’ comorbidities and conditions. Further research is needed to develop evidence in this topic area.
Role of ERAS in older adults (topic area iv, KQ21-KQ24)
KQ21: Should ERAS (vs conventional care) be used in elderly patients undergoing Colorectal surgery?
Recommendation
The panel recommends that elderly adults undergoing Colorectal surgery benefit from ERAS programs over conventional care (Strong recommendation based on moderate certainty of evidence).
Summary of evidence
67 studies were assessed at the full-text level, 48 were extracted, and 9 were included in the analysis—one RCT [181] and 8 observational studies; no observational studies were found to meet the inclusion criteria. Literature research found no article considering the outcome of 30-day complications or LOS.
Benefits of intervention
The analysis showed both strong benefits and small undesirable effects for ERAS programs in colorectal surgery. Considering the panel’s wide experience with patients undergoing colorectal surgery, it was emphasized that the negative outcomes were largely limited in frequency.
-
1.
30-day complications: (1 RCT study with 150 participants) absolute difference 308 fewer patients per 1000 (95% CI 445 fewer to 144 fewer) [181]
-
2.
Length of stay: (1 RCT study with 150 participants) mean difference 2.25 days fewer (95% CI 3.52 fewer to 0.97 fewer) [181]
-
3.
30-day readmission: (1 RCT study with 150 participants) absolute difference 13 fewer patients per 1000 (95% CI 42 fewer to 163 more) [181]
Harms and burdens
The outcome considered showed some undesirable effects for the intervention, which the panel considered small in size.
-
1.
30-day readmission: (1 RCT study with 150 participants) absolute difference of 13 more patients per 1000 (95% CI 42 fewer to 163 more) [181]
Considering the results from the analysis, the panel pointed out the very small sample size and even smaller event rate in conjunction with a confidence interval that crosses multiple standards of clinical meaningfulness. However, the estimated effects of the evidence reviewed ranged from moderate benefits to minimal harms.
Certainty in the evidence of effects
Moderate certainty of evidence was defined for the outcome of 30-day complications. In this case, the number of events was below the threshold of 300. Hence the certainty was downgraded for imprecision. The panel assessed the certainty of evidence of the outcome LOS as moderate due to the high risk of bias of two trials and to the lack of reporting of LOS to follow-up, missingness, and planned statistical analysis. The readmission rate was considered with low certainty of evidence because of the aforementioned very small sample size and event rate. The panel evaluated all three selected outcomes as critical (Supplement 4).
Decision criteria and additional considerations
The item expanded on in this KQ was considered a priority by the panel, with a large desirable effect despite the analysis results. Undesirable effects were evaluated as small in size, even though the patients living far away from their hospital could be more affected by ERAS programs than those living closer. Nonetheless, any positive impact and undesirable anticipated effects should be considered for patients as part of shared decision making. In addition, readmission practices vary greatly from one country to another, possibly confounding the results. The panel determined that there was probably no important uncertainty or variability in how much people acknowledged the main outcome. The patient representative thought patients valued the complication outcomes highly.
Conclusions and research recommendations
Based on the evidence and clinical experience, use of an ERAS protocol was strongly recommended for older adults undergoing colorectal surgery. The panel considered the intervention was probably feasible to implement in 83% of cases. Issues restraining universal implementation of ERAS were lack of home support and transportation for patients living far away from the operative institution. The panel suggests more assistance at the institutional level including social support could address these limitations. Moreover, the panel agreed that more standardized data collection are needed to generate stronger evidence, such as multi-institutional studies and collaborative groups and registries for large, international studies.
KQ22: Should ERAS (vs conventional care) be used in elderly patients undergoing Upper GI surgery?
Recommendation
The panel recommends that the older adult population undergoing Upper GI surgery may benefit from either ERAS programs over conventional care (Conditional recommendation based on low certainty of evidence).
Summary of evidence
12 studies were assessed at the full-text level. Five were extracted. Only two RCTs were analyzed [182, 183], and no comparative observational studies were included. The outcome of 30-day complications, LOS and 30-day readmission were the only ones addressed in the present analysis.
Benefits of intervention
30-day complications and LOS outcomes showed desirable anticipated effects for ERAS over traditional care in patients undergoing upper GI surgery. Overall, the panel considered both outcomes as critical and small in size.
-
1.
30-day complications: (2 RCT studies with 299 participants) absolute difference 2 more patients per 1000 (95% CI 368 fewer to 342 fewer) [182, 183]
-
2.
Length of stay: (2 RCT studies with 299 participants) mean difference 0.83 days lower (95% CI 1.65 lower to 0.01 lower) [182, 183]
Complications were assumed to be trivial by the Expert Panel, but may change if additional data were available.
Harms and burdens
The outcome considered showed undesirable effects for the intervention, which the panel considered critical and small in size.
-
1.
30-day readmission: (2 RCT studies with 299 participants) absolute difference 69 more patients per 1000 (95% CI 6 more to 226 more) [182, 183]
Expert Panel highlights a small number of events and a confidence interval that crosses minimally important differences.
Certainty in the evidence of effects
Very low certainty of evidence was defined for the outcome of 30-day complications. Although one trial was methodologically acceptable, the other did not explain the randomization process properly. The intervention-control groups were not fully compared enough to derive the quality of the randomization process indirectly. The two studies included in the analysis of the outcome of 30-day complications had opposite findings, with one demonstrating fewer complications with ERAS and the other less with conventional care. This may be explained by the lack of definition of complications and unknown comparability between cohorts in the high risk of bias trial.
In addition to the small sample size and relatively small event size, there was a wide confidence interval with the estimated effects ranging from large benefit to large harm with ERAS. Concerning the LOS outcome, the small sample size increases the fragility of this outcome. Low certainty of evidence was considered for the outcomes of LOS and 30-day readmission. Selected articles reported the same issues on randomization mentioned above. In addition, a small sample size increased the fragility of the outcome of LOS. This, together with the small number of events and a confidence interval that crosses minimally important differences, burdened the outcome of 30-day readmission (Supplement 4).
Decision criteria and additional considerations
The panel saw the issue developed in the present KQ as a priority. A possibly important uncertainty or variability in how people value the main outcome was identified, and thus, possibly due to the long distance traveled by patients. In these cases, readmission and LOS may be more important than complications as they are very impactful to patients living far away from the hospital or operative institution.
Conclusions and research recommendations
The panel states that balance between desirable and undesirable effects does not favor the intervention or the comparison. The recommendation is based on a low certainty of evidence. Nonetheless, it was common among the panel members that the intervention was probably feasible to implement. This takes into account global considerations such as local culture, MIS technology, lack of follow-up due to long distances travelled by patients, and lack of social support. The advice is for a closer follow-up after discharge and implementation of institutional support. Concerning possible research priorities, more studies on ERAS implementation in resource-limited environments are needed, as well as multi-institutional RCT specifically looking at ERAS in upper GI surgery in elderly patients and prospective observational studies due to feasibility issues of conducting RCTs.
KQ23: Should ERAS (vs conventional care) be used in elderly patients undergoing HPB surgery?
Recommendation:
The panel recommends that the older adult population undergoing HPB surgery may benefit from an ERAS program over conventional care (Conditional recommendation based on a very low certainty of evidence).
Summary of evidence
17 studies were assessed at the full-text level. Five were extracted. Only two observational comparative studies addressing main outcomes were used for the final recommendation [184, 185]. No RCTs were included.
Benefits of intervention
All three main outcomes expressed desirable anticipated effects for ERAS over traditional care in patients undergoing upper HPB surgery. Overall, the panel considered all outcomes as critical and small in size.
-
1.
30-day complications: (2 observational studies with 265 participants) absolute difference 85 fewer patients per 1000 (95% CI 335 fewer to 343 more) [184, 185]
-
2.
Length of stay: (2 observational studies with 265 participants) mean difference 2.03 days lower (95% CI 5.01 lower to 0.95 higher) [184, 185]
-
3.
30-day readmission: (2 observational studies with 265 participants) absolute difference 29 fewer patients per 1000 (95% CI 68 fewer to 77 more) [184, 185]
Harms and burdens
There were no undesirable effects with ERAS for any critical outcomes.
Certainty in the evidence of effects
Very low certainty of evidence was assessed for all main outcomes. Both studies were judged to be of high risk of bias based on the Newcastle–Ottawa Scale, due to unclear descriptions of how patients were selected for either intervention and a lack of reporting on follow-up. Additionally, the two included studies had opposite findings, introducing considerable heterogeneity into the analysis (I2 84%). Lastly, small sample sizes and large confidence intervals increase the fragility, and thus imprecision of this outcome; indeed, the estimated effects range from large benefits to large harms (Supplement 4).
Decision criteria and additional considerations
The item addressed in the present KQ was considered a priority by the panel, with small desirable anticipated effects in favour of the intervention. The panel determined that there was possibly important uncertainty or variability in how much people acknowledged the main outcome.
Conclusions and research recommendations
The intervention probably favored the balance between desirable and undesirable effects. The recommendation was defined as conditional due to a very low certainty of evidence.
KQ24: Should ERAS (vs conventional care) be used in elderly patients undergoing hernia surgery?
Recommendation
The panel cannot recommend an ERAS programs over conventional care for elderly patients undergoing hernia surgery (Conditional recommendation based on the absence of evidence on this topic).
Summary of evidence
Five studies were assessed at full-text screening, none met the inclusion criteria. No observational studies or RCTs were found to meet the inclusion criteria on this topic.
Benefits of intervention
There were no desirable effects with ERAS for any critical outcomes due to a lack of evidence on the subject.
Harms and burdens
There were no undesirable effects with ERAS for any critical outcomes due to a lack of evidence on the subject.
Certainty in the evidence of effects
Literature research found no evidence on this topic (Supplement 4).
Decision criteria and additional considerations
Considering the complete absence of evidence on the matter, which was considered a priority by the Expert Panel, it feels like stating there was possibly important uncertainty or variability in how much people acknowledge the main outcome. Nonetheless, a common awareness emerged among the panel members regarding the possible gain from pushing for more ERAS surgical operations, which are already provided with effective, enhanced perioperative programs. Indeed, Nissen techniques and paraesophageal hernia (PEH) already have a low LOS. On the other hand, esophagectomy has limited and poor-quality data in elderly patients to draw any conclusion.
Conclusions and research recommendations
There is no evidence in the literature to support using an ERAS protocol over conventional care for elderly patients undergoing hernia surgery, but from clinical experience the panel members suggested that use of ERAS protocols in older adults undergoing hernia surgery could lead to improved postoperative outcomes. Further research is needed to develop evidence in this topic area.
Discussion
This collaborative SAGES-EAES Consensus addressed perioperative optimization in older adult patients. The main goal was to provide evidence-based recommendations for perioperative prehabilitation in the older adult population in order to standardize preoperative workup, implement patient’s physiological, functional and psychological status, and surgical treatment. Additionally, the vast expertise in perioperative management and MIS of the Expert Panel further enriched and drove the consensus discussion, especially in the topics with low level of evidence. What the panel found during this process was a lack of standard definitions for prehabilitation, ERAS, and their components, as well as a lack of strong evidence outside of clinical experience to support their use in the perioperative care of older adults undergoing major abdominal surgery.
In the current work, almost all of the given recommendations were conditional, based on low to very low certainty of evidence, with the exception of KQ21 dealing with ERAS programs in colorectal surgery. In many key questions, the panel could not provide an evidence-based recommendation due to lack of evidence, small sample size, or high risk of bias reported. In these cases, the panel made suggestions based on their clinical experience to provide guidance on the practical application of MIS, prehabilitation, and ERAS topics for practicing surgeons. With this approach, the panel reached consensus on providing conditional recommendations supporting the adoption of preoperative optimization among older adults across all specialities and the project achieved its objectives to inform the global perioperative community on perioperative care of older adults.
With the lack of standardized terms and evidence exposed, the project added additional value in providing universal definitions and recommendations for reporting on perioperative care components. These definitions can be applied in future studies to ensure investigators use common terminology and outcomes. Despite the wide acceptance of these concepts, gaps in the literature across surgical specialties in the risk stratification of comorbidity and frailty, the application of MIS, and the details for application of prehabilitation were also highlighted. This investigation can help guide future work for evidence-based clinical application of these perioperative care concepts in older adults.
Implementation
Given the diversity of the experts and stakeholders involved in this project representing European and North American practice, we believe that it is feasible to successfully implement these definitions, recommendations, and suggestions into clinical practice and that stakeholders will accept the recommendations. The primary considerations regarding the implementation of this Evidence-Based Recommendations and Expert Consensus include costs and support for developing prehabilitation and ERAS programs. Furthermore, some of the recommended techniques, such as MIS, require specialized knowledge and skills acquisition. Lastly, in order to achieve the full benefit of these recommendations, standardizing aspects of perioperative management in these specific groups of patients is required.
Limitations of this consensus
One of the main limitations of this Evidence-Based Recommendations and Expert Consensus is the low certainty of evidence for most of the key questions, except in appraisal the role of MIS in colorectal surgery. This project also did not address insurance coverage and cost analysis to society as it took a patient-centered perspective. In the development of the recommendations, we were not able to consider certain aspects of diversity, equity, and inclusion due to unavailability in the literature that was reviewed thus may limit their generalizability. Finally, these recommendations represent the current practice and the adoption and implementation of the recommendations will be regularly updated in the future with the needs for future studies to develop evidence proposed.
Conclusions
With the increasing life expectancy, perioperative optimization is essential as a risk mitigation toward achieving enhanced postoperative value among older adult patients. This collaborative Evidence-Based Recommendations and Expert Consensus provides a valuable tool to the perioperative community in standardizing definitions for perioperative care components and guiding the decision process concerning use of prehabilitation, ERAS, and MIS in elderly patients undergoing major abdominal surgery. These recommendations and suggestions can reduce inappropriate age-related inequity in access to surgical intervention and perioperative optimization.
Disclaimer
The Evidence-Based Recommendations and Expert Consensus are intended to provide the best available approach to medical conditions as established by a systematic review of available data and expert opinion. The suggested approach may not necessarily be the only acceptable given the complexity of the healthcare environment and the condition specifically treated. This Evidence-Based Recommendations and Expert Consensus is intended to be flexible, as the surgeon must always choose the best suited-to-patient approach and other clinical variables at the moment of decision. This Consensus applies to all appropriately credentialed physicians, regardless of specialty, and addresses the clinical situation in question. This work was developed under the auspices of SAGES and EAES, the Consensus and Guidelines committee, and approved by the Board of Governors. The recommendations of each Consensus undergo multidisciplinary review and are considered valid at the time of production based on the data available.
References
World Health Organization (2018) Ageing and health. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed 9 Dec 2019
Lin HS, Watts JN, Peel NM, Hubbard RE (2016) Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr 16:157
Kushner BS, Holden T, Han BJ, Hamilton J, Sehnert M, Holden SE (2022) Perioperative outcomes of the Geriatric Assessment and Medical Preoperative Screening (GrAMPS) program pilot for older hernia patients: does chronological age predict outcomes. Surg Endosc 36:5442–5450
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78:606–617
Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, Gerhards MF, van Wagensveld BA, van der Zaag ES, van Geloven AA, Sprangers MA, Cuesta MA, Bemelman WA et al (2011) Laparoscopy in combination with fast-track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 254:868–875
Carli F, Scheede-Bergdahl C (2015) Prehabilitation to enhance perioperative care. Anesthesiol Clin 33:17–33
Molenaar CJ, van Rooijen SJ, Fokkenrood HJ, Roumen RM, Janssen L, Slooter GD (2022) Prehabilitation versus no prehabilitation to improve functional capacity, reduce postoperative complications and improve quality of life in colorectal cancer surgery. Cochrane Database Syst Rev 5:CD013259
Ljungqvist O, Hubner M (2018) Enhanced recovery after surgery-ERAS-principles, practice and feasibility in the elderly. Aging Clin Exp Res 30:249–252
Luther A, Gabriel J, Watson RP, Francis NK (2018) The impact of total body prehabilitation on post-operative outcomes after major abdominal surgery: A systematic review. World J Surg 42:2781–2791
Rogers AT, Dirks R, Burt HA, Haggerty S, Kohn GP, Slater BJ, Walsh D, Stefanidis D, Pryor A (2021) Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) guidelines development: Standard operating procedure. Surg Endosc 35:2417–2427
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ et al (2021) PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev 10:39
Covidence (2022) Systematic review software. Veritas Health Innovation, Melbourne. http://www.covidence.org
Andrews JC, Schunemann HJ, Oxman AD, Pottie K, Meerpohl JJ, Coello PA, Rind D, Montori VM, Brito JP, Norris S, Elbarbary M, Post P, Nasser M, Shukla V, Jaeschke R, Brozek J, Djulbegovic B, Guyatt G (2013) GRADE guidelines: 15. Going from evidence to recommendation-determinants of a recommendation’s direction and strength. J Clin Epidemiol 66:726–735
Alonso-Coello P, Schunemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Rada G, Rosenbaum S, Morelli A, Guyatt GH, Oxman AD et al (2016) GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ 353:i2016
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, Treweek S, Mustafa RA, Vandvik PO, Meerpohl J, Guyatt GH, Schünemann HJ et al (2016) GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: clinical practice guidelines. BMJ 353:i2089
GRADEpro Guideline Development Tool (GDT) (2021) [Software]. McMaster University and Evidence Prime. http://gradepro.org.
Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, Fervers B, Graham ID, Grimshaw J, Hanna SE, Littlejohns P, Makarski J, Zitzelsberger L et al (2010) AGREE II: advancing guideline development, reporting and evaluation in health care. J Clin Epidemiol 63:1308–1311
Chen Y, Yang K, Marušic A, Qaseem A, Meerpohl JJ, Flottorp S, Akl EA, Schünemann HJ, Chan ES, Falck-Ytter Y, Ahmed F, Barber S, Chen C, Zhang M, Xu B, Tian J, Song F, Shang H, Tang K, Wang Q, Norris SL et al (2017) A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med 166:128–132
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2000) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute, Ottawa
Review Manager (RevMan) [computer program] (2014) Version 5.3. The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen
Schünemann HBJ, Brożek J, Guyatt G, Oxman A (2013) GRADE handbook for grading quality of evidence and strength of recommendations. http://guidelinedevelopment.org/handbook
Achilli P, Mazzola M, Bertoglio CL, Magistro C, Origi M, Carnevali P, Gervasi F, Mastellone C, Guanziroli N, Corradi E, Ferrari G (2020) Preoperative immunonutrition in frail patients with colorectal cancer: an intervention to improve postoperative outcomes. Int J Colorectal Dis 35:19–27
Barberan-Garcia A, Ubré M, Roca J, Lacy AM, Burgos F, Risco R, Momblán D, Balust J, Blanco I, Martínez-Pallí G (2018) Personalised prehabilitation in high-risk patients undergoing elective major abdominal surgery: a randomized blinded controlled trial. Ann Surg 267:50–56
Carli F, Bousquet-Dion G, Awasthi R, Elsherbini N, Liberman S, Boutros M, Stein B, Charlebois P, Ghitulescu G, Morin N, Jagoe T, Scheede-Bergdahl C, Minnella EM, Fiore JF Jr (2020) Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-day postoperative complications for frail patients undergoing resection of colorectal cancer: A randomized clinical trial. JAMA Surg 155:233–242. Erratum in: JAMA Surg. 2020 155:269
Chia CL, Mantoo SK, Tan KY (2016) ‘Start to finish trans-institutional transdisciplinary care’: a novel approach improves colorectal surgical results in frail elderly patients. Colorectal Dis 18:O43–O50
Indrakusuma R, Dunker MS, Peetoom JJ, Schreurs WH (2015) Evaluation of preoperative geriatric assessment of elderly patients with colorectal carcinoma: a retrospective study. Eur J Surg Oncol 41:21–27
Janssen TL, Steyerberg EW, Langenberg JCM, de Lepper C, Wielders D, Seerden TCJ, de Lange DC, Wijsman JH, Ho GH, Gobardhan PD, van Alphen R, van der Laan L (2019) Multimodal prehabilitation to reduce the incidence of delirium and other adverse events in elderly patients undergoing elective major abdominal surgery: an uncontrolled before-and-after study. PLoS ONE 14:e0218152
Janssen TL, Steyerberg EW, van Gammeren AJ, Ho GH, Gobardhan PD, van der Laan L (2021) Intravenous iron in a prehabilitation program for older surgical patients: prospective cohort study. J Surg Res 257:32–41
Janssen TL, Steyerberg EW, van Hoof-de LC, Seerden TCJ, de Lange DC, Wijsman JH, Ho GH, Gobardhan PD, van der Laan L (2020) Long-term outcomes of major abdominal surgery and postoperative delirium after multimodal prehabilitation of older patients. Surg Today 50:1461–1470
Karlsson E, Farahnak P, Franzén E, Nygren-Bonnier M, Dronkers J, van Meeteren N, Rydwik E (2019) Feasibility of preoperative supervised home-based exercise in older adults undergoing colorectal cancer surgery—a randomized controlled design. PLoS ONE 14:e0219158
Keeler BD, Simpson JA, Ng O, Padmanabhan H, Brookes MJ, Acheson AG et al (2017) Randomized clinical trial of preoperative oral versus intravenous iron in anaemic patients with colorectal cancer. Br J Surg 104:214–221
McDonald SR, Heflin MT, Whitson HE, Dalton TO, Lidsky ME, Liu P, Poer CM, Sloane R, Thacker JK, White HK, Yanamadala M, Lagoo-Deenadayalan SA (2018) Association of integrated care coordination with postsurgical outcomes in high-risk older adults: the Perioperative Optimization of Senior Health (POSH) initiative. JAMA Surg 153:454–462
Okazaki M, Matsukuma S, Suto R, Miyazaki K, Hidaka M, Matsuo M, Noshima S, Zempo N, Asahara T, Nomoto K (2013) Perioperative synbiotic therapy in elderly patients undergoing gastroenterological surgery: a prospective, randomized control trial. Nutrition 29:1224–1230
Ommundsen N, Wyller TB, Nesbakken A, Bakka AO, Jordhøy MS, Skovlund E, Rostoft S (2018) Preoperative geriatric assessment and tailored interventions in frail older patients with colorectal cancer: a randomized controlled trial. Colorectal Dis 20:16–25
Souwer ETD, Bastiaannet E, de Bruijn S, Breugom AJ, van den Bos F, Portielje JEA, Dekker JWT (2018) Comprehensive multidisciplinary care program for elderly colorectal cancer patients: “From prehabilitation to independence.” Eur J Surg Oncol 44:1894–1900
van der Vlies E, Smits AB, Los M, van Hengel M, Bos WJW, Dijksman LM, van Dongen EPA, Noordzij PG (2020) Implementation of a preoperative multidisciplinary team approach for frail colorectal cancer patients: Influence on patient selection, prehabilitation and outcome. J Geriatr Oncol 11:1237–1243
Watanabe T, Momosaki R, Suzuki S, Abo M (2020) Preoperative rehabilitation for patients undergoing colorectal cancer surgery: a retrospective cohort study. Support Care Cancer 28:2293–2297
Yamamoto K, Nagatsuma Y, Fukuda Y, Hirao M, Nishikawa K, Miyamoto A, Ikeda M, Nakamori S, Sekimoto M, Fujitani K, Tsujinaka T (2017) Effectiveness of a preoperative exercise and nutritional support program for elderly sarcopenic patients with gastric cancer. Gastric Cancer 20:913–918
Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, Ueno M, Yamaguchi T (2009) Short-term outcomes of laparoscopic rectal surgery for primary rectal cancer in elderly patients: is it safe and beneficial? J Gastrointest Surg 13:1614–1618
Allardyce RA, Bagshaw PF, Frampton CM, Frizelle FA, Hewett PJ, Rieger NA, Smith JS, Solomon MJ, Stevenson AR (2010) Australasian Laparoscopic Colon Cancer Study shows that elderly patients may benefit from lower postoperative complication rates following laparoscopic versus open resection. Br J Surg 97:86–91
Altuntas YE, Gezen C, Vural S, Okkabaz N, Kement M, Oncel M (2012) Laparoscopy for sigmoid colon and rectal cancers in septuagenarians: a retrospective, comparative study. Tech Coloproctol 16:213–219
Baek HN, Jung YH, Hwang YH (2011) Laparoscopic versus open appendectomy for appendicitis in elderly patients. J Korean Soc Coloproctol 27:241–245
Chang E, Chung PJ, Smith MC, Lee MJ, Gross DJ, Kao E, Sugiyama G (2019) Can the laparoscopic approach for adhesive small bowel obstruction be used in octogenarians? An observational study using ACS NSQIP. J Surg Res 233:345–350
Chen TC, Liang JT, Chang TC (2018) Should surgical treatment be provided to patients with colorectal cancer who are aged 90 years or older? J Gastrointest Surg 22:1958–1967
Chen Z, He X, Huang J, Zeng Y, Lian L, Wu X, Le J, Wang J, Lan P (2015) Short-term outcomes between laparoscopy-assisted and open colorectomy for colorectal cancer in elderly patients: a case-matched control study. Mol Clin Oncol 3(5):1155–1159
Chern YJ, Hung HY, You JF, Hsu YJ, Chiang JM, Hsieh PS, Tsai WS (2020) Advantage of laparoscopy surgery for elderly colorectal cancer patients without compromising oncologic outcome. BMC Surg 20:294
Chern YJ, Tsai WS, Hung HY, Chen JS, Tang R, Chiang JM, Yeh CY, You YT, Hsieh PS, Chiang SF, Lai CC, Lin GP, Hsu YR, You JF (2018) The dark side of laparoscopic surgery for colorectal cancer patients aged 75 years or older. Int J Colorectal Dis 33:1367–1371
Cheung HYS, Chung CC, Fung JTK, Wong JCH, Yau KKK, Li MKW (2007) Laparoscopic resection for colorectal cancer in octogenarians: Results in a decade. Dis Colon Rectum 50:1905–1910
Chung KC, Lee KC, Chen HH, Cheng KC, Wu KL, Song LC (2021) Differential short-term outcomes of laparoscopic resection in colon and rectal cancer patients aged 80 and older: an analysis of Nationwide Inpatient Sample. Surg Endosc 35:872–883
Clark CE 3rd, Jupiter DC, Thomas JS, Papaconstantinou HT (2012) Rectal prolapse in the elderly: trends in surgical management and outcomes from the American College of Surgeons National Surgical Quality Improvement Program database. J Am Coll Surg 215:709–714
Cocorullo G, Falco N, Tutino R, Fontana T, Scerrino G, Salamone G, Licari L, Gulotta G (2016) Open versus laparoscopic approach in the treatment of abdominal emergencies in elderly population. G Chir 37:108–112
Cummings LC, Delaney CP, Cooper GS (2012) Laparoscopic versus open colectomy for colon cancer in an older population: a cohort study. World J Surg Oncol 10:31
Daniel VT, Davids JS, Sturrock PR, Maykel JA, Phatak UR, Alavi K (2019) Getting to the bottom of treatment of rectal prolapse in the elderly: Analysis of the National Surgical Quality Improvement Program (NSQIP). Am J Surg 218:288–292
Dde’Angelis N, Abdalla S, Bianchi G, Memeo R, Charpy C, Petrucciani N, Sobhani I, Brunetti F (2018) Robotic versus laparoscopic colorectal cancer surgery in elderly patients: a propensity score match analysis. J Laparoendosc Adv Surg Tech A 28:1334–1345
Delgado S, Lacy AM, Garcia Valdecasas JC, Balague C, Pera M, Salvador L, Momblan D, Visa J (2000) Could age be an indication for laparoscopic colectomy in colorectal cancer? Surg Endosc 14:22–26
Devoto L, Celentano V, Cohen R, Khan J, Chand M (2017) Colorectal cancer surgery in the very elderly patient: a systematic review of laparoscopic versus open colorectal resection. Int J Colorectal Dis 32:1237–1242
Duan Y, Yang H, Yang Y, Wang G, Wang T, Chen Z, Gao X, Jiang T, Shi X (2018) Application of laparoscopy in acute appendicitis for the elderly: a single center experience. Biomed Res 29:1681–1684
Feng B, Zheng MH, Mao ZH, LiJ W, Lu AG, Wang ML, Hu WG, Dong F, Hu YY, Zang L, Li HW (2006) Clinical advantages of laparoscopic colorectal cancer surgery in the elderly. Aging Clin Exp Res 18:191–195
Frasson M, Braga M, Vignali A, Zuliani W, Di Carlo V (2008) Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 51:296–300
Fujii S, Ishibe A, Ota M, Yamagishi S, Watanabe K, Watanabe J, Kanazawa A, Ichikawa Y, Oba M, Morita S, Hashiguchi Y, Kunisaki C, Endo I (2014) Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients. Surg Endosc 28:466–476
Guida F, Clemente M, Valvano L, Napolitano C (2015) Laparoscopic or open hemicolectomy for elderly patients with right colon cancer? A retrospective analysis. G Chir 36:205–208
Hashida H, Mizuno R, Iwaki K, Kanbe H, Sumi T, Kawarabayashi T, Kondo M, Kobayashi H, Kaihara S (2020) Laparoscopic surgery for colorectal cancer in super-elderly patients: a single-center analysis. Surg Laparosc Endosc Percutan Tech 31:337–341
Hatakeyama T, Nakanishi M, Murayama Y, Komatsu S, Shiozaki A, Kuriu Y, Ikoma H, Ichikawa D, Fujiwara H, Okamoto K, Ochiai T, Kokuba Y, Otsuji E (2013) Laparoscopic resection for colorectal cancer improves short-term outcomes in very elderly colorectal cancer patients. Surg Laparosc Endosc Percutan Tech 23:532–535
Hinoi T, Kawaguchi Y, Hattori M, Okajima M, Ohdan H, Yamamoto S, Hasegawa H, Horie H, Murata K, Yamaguchi S, Sugihara K, Watanabe M (2015) Laparoscopic versus open surgery for colorectal cancer in elderly patients: a multicenter matched case-control study. Ann Surg Oncol 22:2040–2050
Horsey ML, Parascandola SA, Sparks AD, Hota S, Ng M, Obias V (2022) The impact of surgical approach on short- and long-term outcomes after rectal cancer resection in elderly patients: a national cancer database propensity score matched comparison of robotic, laparoscopic, and open approaches. Surg Endosc 36:1269–1277
Huang S, Li Z, Zou N, Dai T, Cao XL, Jia Z, Peng WP, Yang N, Jia RF, Zuo MZ (2021) Comparison of postoperative acute kidney injury between laparoscopic and laparotomy procedures in elderly patients undergoing colorectal surgery. Surg Laparosc Endosc Percutan Tech 31:160–164
Inoue K, Ueno T, Akishige N, Soeta T, Tsuchiya T, Nakayama S, Shima K, Goto S, Takahashi M, Naito H (2019) Short–term outcomes of laparoscopic colorectal cancer surgery in elderly patients: is it really safe in elderly patients with severe comorbidities? Int J Surg Open 17:27–32
Issa N, Grassi C, Melki Y, Powsner E, Dreznik Z (2011) Laparoscopic colectomy for carcinoma of the colon in octogenarians. J Gastrointest Surg 15:2011–2015
Jia RJ, Hou LY, Feng YZ, Li LF, Li MH, Zhang LB, Zhang HL (2015) Modified laparoscopic anterior resection of the rectum for rectal prolapse in elderly patients. World Chin J Digestol 23:2496–2500
Kannan U, Reddy VS, Mukerji AN, Parithivel VS, Shah AK, Gilchrist BF, Farkas DT (2015) Laparoscopic vs open partial colectomy in elderly patients: Insights from the American College of Surgeons—National Surgical Quality Improvement Program database. World J Gastroenterol 21:12843–12850
Keller DS, de Paula TR, Qiu J, Kiran RP (2021) The trends in adoption, outcomes, and costs of laparoscopic surgery for colorectal cancer in the elderly population. J Gastrointest Surg 25:766–774
Kennedy GD, Rajamanickam V, O’connor ES, Loconte NK, Foley EF, Leverson G, Heise CP (2011) Optimizing surgical care of colon cancer in the older adult population. Ann Surg 253:508–514
Koh FH, Wong J, Tan JK, Tan KK, Cheong WK, Lieske B (2015) Laparoscopic colorectal surgery is safe and benefits octogenarian patients with malignant disease: a matched case-control study comparing laparoscopic and open colorectal surgery. Int J Colorectal Dis 30:963–968
Kurian AA, Suryadevara S, Vaughn D, Zebley DM, Hofmann M, Kim S, Fassler SA (2010) Laparoscopic colectomy in octogenarians and nonagenarians: a preferable option to open surgery? J Surg Educ 67:161–166
Kye BH, Rookkachart T, Kim JH, Kim HJ, Lee YS, Lee IK, Kang WK, Cho HM, Oh ST (2019) Safety of laparoscopic oncologic resection in elderly patients with colorectal cancer: a multicenter retrospective study based on perioperative short-term outcomes. J Laparoendosc Adv Surg Tech A 29:1016–1022
Landi F, Vallribera F, Rivera JP, Bertoli P, Armengol M, Espín E (2016) Morbidity after laparoscopic and open rectal cancer surgery: a comparative analysis of morbidity in octogenarians and younger patients. Colorectal Dis 18:459–467
Law WL, Chu KW, Tung PH (2002) Laparoscopic colorectal resection: a safe option for elderly patients. J Am Coll Surg 195:768–773
Li Y, Wang S, Gao S, Yang C, Yang W, Guo S (2016) Laparoscopic colorectal resection versus open colorectal resection in octogenarians: a systematic review and meta-analysis of safety and efficacy. Tech Coloproctol 20:153–162
Lian L, Kalady M, Geisler D, Kiran RP (2010) Laparoscopic colectomy is safe and leads to a significantly shorter hospital stay for octogenarians. Surg Endosc 24:2039–2043
Matsuoka H, Maeda K, Hanai T, Sato H, Masumori K, Koide Y, Katsuno H, Endo T, Shiota M, Sugihara K (2018) Surgical management of colorectal cancer for the aging population—a survey by the Japanese Society for Cancer of Colon and Rectum. Asian J Surg 41:192–196
Miguchi M, Yoshimitsu M, Hakoda K, Omori I, Kohashi T, Hihara J, Ohdan H, Hirabayashi N (2018) Short-term outcomes of laparoscopic surgery in octogenarians with colorectal cancer: a single-institution analysis. Surg Today 48:292–299
Miguchi M, Yoshimitsu M, Shimomura M, Kohashi T, Egi H, Ohdan H, Hirabayashi N (2021) Long-term outcomes of laparoscopic surgery in elderly patients with colorectal cancer: a single institutional matched case-control study. Asian J Endosc Surg 14:200–206
Miyasaka Y, Mochidome N, Kobayashi K, Ryu S, Akashi Y, Miyoshi A (2014) Efficacy of laparoscopic resection in elderly patients with colorectal cancer. Surg Today 44:1834–1840
Moazzez A, Mason RJ, Katkhouda N (2013) Thirty-day outcomes of laparoscopic versus open appendectomy in elderly using ACS/NSQIP database. Surg Endosc 27:1061–1071
Moon SY, Kim S, Lee SY, Han EC, Kang SB, Jeong SY, Park KJ, Oh JH et al (2016) Laparoscopic surgery for patients with colorectal cancer produces better short-term outcomes with similar survival outcomes in elderly patients compared to open surgery. Cancer Med 5:1047–1054
Mukai T, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Ikeda A, Yamaguchi T (2014) Outcomes of laparoscopic surgery for colorectal cancer in oldest-old patients. Surg Laparosc Endosc Percutan Tech 24:366–369
Nakamura T, Sato T, Miura H, Ikeda A, Tsutsui A, Naito M, Ogura N, Watanabe M (2014) Feasibility and outcomes of surgical therapy in very elderly patients with colorectal cancer. Surg Laparosc Endosc Percutan Tech 24:85–88
Niitsu H, Hinoi T, Kawaguchi Y, Ohdan H, Hasegawa H, Suzuka I, Fukunaga Y, Yamaguchi T, Endo S, Tagami S, Idani H, Ichihara T, Watanabe K, Watanabe M et al (2016) Laparoscopic surgery for colorectal cancer is safe and has survival outcomes similar to those of open surgery in elderly patients with a poor performance status: subanalysis of a large multicenter case-control study in Japan. J Gastroenterol 51:43–54
Nishikawa T, Ishihara S, Hata K, Murono K, Yasuda K, Otani K, Tanaka T, Kiyomatsu T, Kawai K, Nozawa H, Yamaguchi H, Watanabe T (2016) Short-term outcomes of open versus laparoscopic surgery in elderly patients with colorectal cancer. Surg Endosc 30:5550–5557
Nishikawa T, Kawai K, Emoto S, Murono K, Hiyoshi M, Kaneko M, Sonoda H, Sasaki K, Shuno Y, Tanaka T, Hata K, Nozawa H (2019) The influence of pulmonary comorbidities on treatment choice and short-term surgical outcomes among elderly patients with colorectal cancer. Int J Colorectal Dis 34:1497–1501
Person B, Cera SM, Sands DR, Weiss EG, Vernava AM, Nogueras JJ, Wexner SD (2008) Do elderly patients benefit from laparoscopic colorectal surgery? Surg Endosc 22:401–405
Pinto RA, Ruiz D, Edden Y, Weiss EG, Nogueras JJ, Wexner SD (2011) How reliable is laparoscopic colorectal surgery compared with laparotomy for octogenarians? Surg Endosc 25:2692–2698
Richards CR, Steele SR, Lustik MB, Gillern SM, Lim RB, Brady JT, Althans AR, Schlussel AT (2019) Safe surgery in the elderly: a review of outcomes following robotic proctectomy from the Nationwide Inpatient Sample in a cross-sectional study. Ann Med Surg 44:39–45
Rinaldi L, Ouaissi M, Barabino G, Loundou A, Clavel L, Sielezneff I, Roblin X, Porcheron J, Williet N, Fuks D, Gayet B, Phelip JM (2017) Laparoscopy could be the best approach to treat colorectal cancer in selected patients aged over 80 years: outcomes from a multicenter study. Dig Liver Dis 49:84–90
Scarpa M, Di Cristofaro L, Cortinovis M, Pinto E, Massa M, Alfieri R, Cagol M, Saadeh L, Costa A, Castoro C, Bassi N, Ruffolo C (2013) Minimally invasive surgery for colorectal cancer: quality of life and satisfaction with care in elderly patients. Surg Endosc 27:2911–2920
She WH, Poon JT, Fan JK, Lo OS, Law WL (2013) Outcome of laparoscopic colectomy for cancer in elderly patients. Surg Endosc 27:308–312
Shigeta K, Baba H, Yamafuji K, Asami A, Takeshima K, Nagasaki K, Okamoto N, Murata T, Arai S, Kubochi K, Kitagawa Y (2016) Effects of laparoscopic surgery on the patterns of death in elderly colorectal cancer patients: competing risk analysis compared with open surgery. Surg Today 46:422–429
Sklow B, Read T, Birnbaum E, Fry R, Fleshman J (2003) Age and type of procedure influence the choice of patients for laparoscopic colectomy. Surg Endosc 17:923–929
Sotirova I, Gklavas A, Nastos C, Micha G, Dafnios N, Dellaportas D, Theodosopoulos T (2020) Comparison of the laparoscopic versus open surgery in patients aged over 75 years old with colorectal cancer. Short- and Mid-term outcomes J BUON 25:2186–2191
Stocchi L, Nelson H, Young-Fadok TM, Larson DR, Ilstrup DM (2000) Safety and advantages of laparoscopic vs open colectomy in the elderly: matched-control study. Dis Colon Rectum 43:326–332
Tan WS, Chew MH, Lim IA, Ng KH, Tang CL, Eu KW (2012) Evaluation of laparoscopic versus open colorectal surgery in elderly patients more than 70 years old: an evaluation of 727 patients. Int J Colorectal Dis 27:773–780
Tei M, Ikeda M, Haraguchi N, Takemasa I, Mizushima T, Ishii H, Yamamoto H, Sekimoto M, Doki Y, Mori M (2010) Risk factors for postoperative delirium in elderly patients with colorectal cancer. Surg Endosc 24:2135–2139
Tomimaru Y, Ide Y, Murata K (2011) Outcome of laparoscopic surgery for colon cancer in elderly patients. Asian J Endosc Surg 4:1–6
Tominaga T, Takeshita H, Arai J, Takagi K, Kunizaki M, To K, Abo T, Hidaka S, Nanashima A, Nagayasu T, Sawai T (2015) Short-term outcomes of laparoscopic surgery for colorectal cancer in oldest-old patients. Dig Surg 32:32–38
Troian M, Bellio G, Pasquali A, de Manzini N (2018) Laparoscopic vs open approach for pT3/pT4 colorectal cancer in the elderly: ten-year experience in a single center. Minerva Chir 73:20–28
Tuech JJ, Pessaux P, Rouge C, Regenet N, Bergamaschi R, Arnaud JP (2000) Laparoscopic vs open colectomy for sigmoid diverticulitis: a prospective comparative study in the elderly. Surg Endosc 14:1031–1033
Ueda Y, Shiraishi N, Kawasaki T, Akagi T, Ninomiya S, Shiroshita H, Etoh T, Inomata M (2020) Short- and long-term outcomes of laparoscopic surgery for colorectal cancer in the elderly aged over 80 years old versus non-elderly: a retrospective cohort study. BMC Geriatr 20:445
Vallribera Valls F, Landi F, Espín Basany E, Sánchez García JL, Jiménez Gómez LM, Martí Gallostra M, Salgado Cruz L, Armengol Carrasco M (2014) Laparoscopy-assisted versus open colectomy for treatment of colon cancer in the elderly: morbidity and mortality outcomes in 545 patients. Surg Endosc 28:3373–3378
van Harten MJ, Greenwood EB, Bedrikovetski S, Dudi-Venkata NN, Hunter RA, Kroon HM, Sammour T (2020) Minimally invasive surgery in elderly patients with rectal cancer: an analysis of the Bi-National Colorectal Cancer Audit (BCCA). Eur J Surg Oncol 46:1649–1655
Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C (2005) Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum 48:2070–2075
Wang YC, Yang HR, Chung PK, Jeng LB, Chen RJ (2006) Laparoscopic appendectomy in the elderly. Surg Endosc 20:887–889
Wang W, Shao M, Zhang R (2016) Long-term outcomes after laparoscopic versus open surgery for elderly patients with rectal cancer. Int J Clin Exp Med 9:18160–18167
Wei M, Zhang X, Ma P, He W, Bi L, Wang Z (2018) Outcomes of open, laparoscopic, and hand-assisted laparoscopic surgeries in elderly patients with right colon cancers: a case-control study. Medicine 97:e11907
White SI, Wright D, Taylor CJ (2012) A comparison of laparoscopic versus open rectal surgery in 114 consecutive octogenarians. Colorectal Dis 14:e395-399
Wu SC, Wang YC, Fu CY, Chen RJ, Huang HC, Huang JC, Lu CW, Hsieh CH, Lin CY (2011) Laparoscopic appendectomy provides better outcomes than open appendectomy in elderly patients. Am Surg 77:466–470
Wu TC, Lu Q, Huang ZY, Liang XH (2017) Efficacy of emergency laparoscopic appendectomy in treating complicated appendicitis for elderly patients. Saudi Med J 38:1108–1112
Yamamoto S, Hinoi T, Niitsu H, Okajima M, Ide Y, Murata K, Akamoto S, Kanazawa A, Nakanishi M, Naitoh T, Kanehira E, Shimamura T, Suzuka I, Fukunaga Y, Yamaguchi T, Watanabe M et al (2017) Influence of previous abdominal surgery on surgical outcomes between laparoscopic and open surgery in elderly patients with colorectal cancer: subanalysis of a large multicenter study in Japan. J Gastroenterol 52:695–704
Yap R, Oliva K, Wilkins S, McMurrick PJ (2016) Colorectal cancer surgery in the very elderly: nonagenarians. Dis Colon Rectum 59:501–507
Zeng WG, Zhou ZX, Hou HR, Liang JW, Zhou HT, Wang Z, Zhang XM, Hu JJ (2015) Outcome of laparoscopic versus open resection for rectal cancer in elderly patients. J Surg Res 193:613–618
Zhou S, Wang X, Zhao C, Liu Q, Zhou H, Zheng Z, Zhou Z, Wang X, Liang J (2019) Laparoscopic vs open colorectal cancer surgery in elderly patients: short- and long-term outcomes and predictors for overall and disease-free survival. BMC Surg 19:137
Abbassi-Ghadi N, Durakovic S, Piessen G, Gatenby P, Sultan J, Preston SR (2020) Laparoscopic versus open subtotal gastrectomy for adenocarcinoma of the stomach in a Western population: peri-operative and 5-year oncological outcomes. Surg Endosc 34:3818–3826
Chen WZ, Dong QT, Zhang FM, Cai HY, Yan JY, Zhuang CL, Yu Z, Chen XL (2021) Laparoscopic versus open resection for elderly patients with gastric cancer: a double-center study with propensity score matching method. Langenbecks Arch Surg 406:449–461
Costa G, Fransvea P, Podda M, Pisanu A, Carrano FM, Iossa A, Balducci G, Agresta F et al (2020) The use of emergency laparoscopy for acute abdomen in the elderly: the FRAILESEL Italian Multicenter Prospective Cohort Study. Updates Surg 72:513–525
Fransvea P, Costa G, Lepre L, Podda M, Giordano A, Bellanova G, Agresta F, Marini P, Sganga G et al (2020) laparoscopic repair of perforated peptic ulcer in the elderly: an interim analysis of the FRAILESEL Italian Multicenter Prospective Cohort Study. Surg Laparosc Endosc Percutan Tech 31:2–7
Inokuchi M, Tanioka T, Nakagawa M, Okuno K, Gokita K, Kojima K (2018) Laparoscopic distal gastrectomy is feasible in very elderly patients as compared with open distal gastrectomy. J Invest Surg 31:539–545
Kim SM, Youn HG, An JY, Choi YY, Noh SH, Oh SJ, Sohn TS, Kim S (2018) Comparison of open and laparoscopic gastrectomy in elderly patients. J Gastrointest Surg 22:785–791
Konishi H, Ichikawa D, Itoh H, Fukuda K, Kakihara N, Takemura M, Okugawa K, Uchiyama K, Nakata M, Nishi H, Kosuga T, Komatsu S, Okamoto K, Otsuji E (2017) Surgery for gastric cancer patients of age 85 and older: Multicenter survey. World J Gastroenterol 23:1215–1223
Li H, Han X, Su L, Zhu W, Xu W, Li K, Zhao Q, Yang H, Liu H (2014) Laparoscopic radical gastrectomy versus traditional open surgery in elderly patients with gastric cancer: benefits and complications. Mol Clin Oncol 2:530–534
Liu CA, Huang KH, Chen MH, Lo SS, Li AF, Wu CW, Shyr YM, Fang WL (2017) Comparison of the surgical outcomes of minimally invasive and open surgery for octogenarian and older compared to younger gastric cancer patients: a retrospective cohort study. BMC Surg 17:68
Lu J, Huang CM, Zheng CH, Li P, Xie JW, Wang JB, Lin JX, Chen QY, Cao LL, Lin M (2015) Short- and long-term outcomes after laparoscopic versus open total gastrectomy for elderly gastric cancer patients: a propensity score-matched analysis. J Gastrointest Surg 9:1949–1957
Mochiki E, Ohno T, Kamiyama Y, Aihara R, Nakabayashi T, Asao T, Kuwano H (2005) Laparoscopy-assisted gastrectomy for early gastric cancer in young and elderly patients. World J Surg 29:1585–1591
Molena D, Mungo B, Stem M, Feinberg RL, Lidor AO (2014) Outcomes of operations for benign foregut disease in elderly patients: a national surgical quality improvement program database analysis. Surgery 156:352–360
Pan Y, Chen K, Yu WH, Maher H, Wang SH, Zhao HF, Zheng XY (2018) Laparoscopic gastrectomy for elderly patients with gastric cancer: a systematic review with meta-analysis. Medicine 97:e0007
Qiu JF, Yang B, Fang L, Li YP, Shi YJ, Yu XC, Zhang MC (2014) Safety and efficacy of laparoscopy-assisted gastrectomy for advanced gastric cancer in the elderly. Int J Clin Exp Med 7:3562
Tsuchiya N, Kunisaki C, Makino H, Kimura J, Takagawa R, Sato S, Tanaka Y, Sato K, Miyamoto H, Kosaka T, Akiyama H, Endo I, Sakamaki K, Yamanaka T (2018) Feasibility of laparoscopy-assisted gastrectomy for gastric cancer in elderly patients: a case-control study. Surg Laparosc Endosc Percutan Tech 28:102–107
Ushimaru Y, Kurokawa Y, Takahashi T, Saito T, Yamashita K, Tanaka K, Makino T, Yamasaki M, Nakajima K, Mori M, Doki Y (2020) Is laparoscopic gastrectomy more advantageous for elderly patients than for young patients with resectable advanced gastric cancer? World J Surg 44:2332–2339
Wu D, Li Y, Yang Z, Feng X, Lv Z, Cai G (2016) Laparoscopic versus open gastrectomy for gastric carcinoma in elderly patients: a pair-matched study. Int J Clin Exp Med 9:3465–3472
Zheng L, Lu L, Jiang X, Jian W, Liu Z, Zhou D (2016) Laparoscopy-assisted versus open distal gastrectomy for gastric cancer in elderly patients: a retrospective comparative study. Surg Endosc 30:4069–4077
SAGES Guidelines Committee (2009) SAGES guideline for clinical application of laparoscopic bariatric surgery. Surg Obes Relat Dis 5:387–405
Amato B, Aprea G, De Rosa D, Milone M, di Domenico L, Amato M, Compagna R, Santoro M, Johnson LB, Sanguinetti A, Polistena A, Avenia N (2017) Laparoscopic hepatectomy for HCC in elderly patients: risks and feasibility. Aging Clin Exp Res 29:S179–S183
Aprea G, De Rosa D, Milone M, Rocca A, Bianco T, Massa G, Compagna R, Johnson LB, Sanguinetti A, Polistena A, Avenia N, Amato B (2017) Laparoscopic distal pancreatectomy in elderly patients: is it safe? Aging Clin Exp Res 29:S41–S45
Badawy A, Seo S, Toda R, Fuji H, Fukumitsu K, Ishii T, Taura K, Kaido T, Uemoto S (2019) A propensity score-based analysis of laparoscopic liver resection for liver malignancies in elderly patients. J Invest Surg 32:75–82
Cauchy F, Fuks D, Nomi T, Dokmak S, Scatton O, Schwarz L, Barbier L, Belghiti J, Soubrane O, Gayet B (2016) benefits of laparoscopy in elderly patients requiring major liver resection. J Am Coll Surg 222:174-184.e10
Chan AC, Poon RT, Cheung TT, Chok KS, Dai WC, Chan SC, Lo CM (2014) Laparoscopic versus open liver resection for elderly patients with malignant liver tumors: a single-center experience. J Gastroenterol Hepatol 29:1279–1283
Chapman BC, Gajdos C, Hosokawa P, Henderson W, Paniccia A, Overbey DM, Gleisner A, Schulick RD, McCarter MD, Edil BH (2018) Comparison of laparoscopic to open pancreaticoduodenectomy in elderly patients with pancreatic adenocarcinoma. Surg Endosc 32:2239–2248
Chau CH, Tang CN, Siu WT, Ha JP, Li MK (2002) Laparoscopic cholecystectomy versus open cholecystectomy in elderly patients with acute cholecystitis: retrospective study. Hong Kong Med J 8:394–399
Chen K, Pan Y, Mou YP, Yan JF, Zhang RC, Zhang MZ, Zhou JY, Wang XF, Maher H, Chen QL (2019) Surgical outcomes of laparoscopic distal pancreatectomy in elderly and octogenarian patients: a single-center, comparative study. Surg Endosc 33:2142–2151
Chen Y, Yu L, Quan C (2020) Laparoscopic versus open hepatectomy for elderly patients with hepatocellular carcinoma. J BUON 25:1404–1412
Delvecchio A, Conticchio M, Ratti F, Gelli M, Anelli FM, Laurent A, Vitali GC, Magistri P, Assirati G, Felli E, Wakabayashi T, Pessaux P, Piardi T, Di Benedetto F, de’Angelis N, Briceño-Delgado J, Adam R, Cherqui D, Aldrighetti L, Memeo R (2021) Laparoscopic major hepatectomy for hepatocellular carcinoma in elderly patients: a multicentric propensity score-based analysis. Surg Endosc 35:3642–3652
Dumronggittigule W, Han HS, Ahn S, Yoon YS, Cho JY, Choi Y (2020) laparoscopic versus open hepatectomy for hepatocellular carcinoma in elderly patients: a single-institutional propensity score matching comparison. Dig Surg 37:495–504
Fisichella PM, Di Stefano A, Di Carlo I, La Greca G, Russello D, Latteri F (2002) Efficacy and safety of elective laparoscopic cholecystectomy in elderly: a case- controlled comparison with the open approach. Ann Ital Chir 73:149–153
Goh BKP, Chua D, Syn N, Teo JY, Chan CY, Lee SY, Jeyaraj PR, Cheow PC, Chow PKH, Ooi LLPJ, Chung AYF (2018) Perioperative outcomes of laparoscopic minor hepatectomy for hepatocellular carcinoma in the elderly. World J Surg 42:4063–4069
Gurgenidze M, Kiladze M, Beriashvili Z (2013) Miniinvasive surgical management of cholelithiasis for elderly and senile patients: a retrospective study. Georgian Med News 6:7–13
Harada N, Maeda T, Yoshizumi T, Ikeda T, Kayashima H, Ikegami T, Harimoto N, Takaki S, Maehara Y (2016) Laparoscopic liver resection is a feasible treatment for patients with hepatocellular carcinoma and portal hypertension. Anticancer Res 36:3489–3497
Irojah B, Bell T, Grim R, Martin J, Ahuja V (2017) Are they too old for surgery? Safety of cholecystectomy in superelderly patients (≥ age 90). Perm J 21:16–013
Ke J, Liu Y, Liu F, Ji B (2020) Application of laparoscopic pancreatoduodenectomy in elderly patients. J Laparoendosc Adv Surg Tech A 30:797–802
Kim JM, Kim S, Rhu J, Choi GS, Kwon CHD, Joh JW (2020) Elderly hepatocellular carcinoma patients: open or laparoscopic approach? Cancers 12:2281
Le Roux F, Rebibo L, Cosse C, Chatelain D, Nguyen-Khac E, Badaoui R, Regimbeau JM (2018) Benefits of laparoscopic approach for resection of liver tumors in cirrhotic patients. J Laparoendosc Adv Surg Tech A 28:553–561
Leardi S, De Vita F, Pietroletti R, Simi M (2009) Cholecystectomy for gallbladder disease in elderly aged 80 years and over. Hepatogastroenterology 56:303–306
Liang Y, Zhao L, Jiang C, Hu P, Wang H, Cai Z, Wang W (2020) Laparoscopic pancreaticoduodenectomy in elderly patients. Surg Endosc 34(5):2028–2034
Lin YF, Tian YF, Uen YH (2017) Common bile duct exploration for elderly patients with choledocholithiasis: Is laparoscopic method better? Formosan J Surg 50:158–162
Martínez-Cecilia D, Cipriani F, Shelat V, Ratti F, Tranchart H, Barkhatov L, Tomassini F, Montalti R, Halls M, Troisi RI, Dagher I, Aldrighetti L, Edwin B, Abu Hilal M (2017) Laparoscopic versus open liver resection for colorectal metastases in elderly and octogenarian patients: a multicenter propensity score based analysis of short- and long-term outcomes. Ann Surg 265:1192–1200
Moyson J, Thill V, Simoens Ch, Smets D, Debergh N, Mendes da Costa P (2008) Laparoscopic cholecystectomy for acute cholecystitis in the elderly: a retrospective study of 100 patients. Hepatogastroenterology 55:1975–1980
Nomi T, Hirokawa F, Kaibori M, Ueno M, Tanaka S, Hokuto D, Noda T, Nakai T, Ikoma H, Iida H, Komeda K, Ishizaki M, Hayami S, Eguchi H, Matsumoto M, Morimura R, Maehira H, Sho M, Kubo S (2020) Laparoscopic versus open liver resection for hepatocellular carcinoma in elderly patients: a multi-centre propensity score-based analysis. Surg Endosc 34:658–666
Pessaux P, Regenet N, Tuech JJ, Rouge C, Bergamaschi R, Arnaud JP (2001) Laparoscopic versus open cholecystectomy: a prospective comparative study in the elderly with acute cholecystitis. Surg Laparosc Endosc Percutan Tech 11:252–255
Shin H, Song KB, Kim YI, Lee YJ, Hwang DW, Lee JH, Shin SH, Kwon J, Alshammary S, Park G, Park Y, Lee SJ, Kim SC (2019) Propensity score-matching analysis comparing laparoscopic and open pancreaticoduodenectomy in elderly patients. Sci Rep 9:12961
Souche R, Fuks D, Perinel J, Herrero A, Guillon F, Pirlet I, Perniceni T, Borie F, Cunha AS, Gayet B, Fabre JM (2018) Impact of laparoscopy in patients aged over 70 years requiring distal pancreatectomy: a French multicentric comparative study. Surg Endosc 32:3164–3173
Tanaka S, Takemura S, Shinkawa H, Nishioka T, Hamano G, Kinoshita M, Ito T, Kubo S (2015) Outcomes of pure laparoscopic versus open hepatic resection for hepatocellular carcinoma in cirrhotic patients: A case-control study with propensity score matching. Eur Surg Res 55:291–301
Tee MC, Chen L, Peightal D, Franko J, Kim PT, Brahmbhatt RD, Raman S, Scudamore CH, Chung SW, Segedi M (2020) Minimally invasive hepatectomy is associated with decreased morbidity and resource utilization in the elderly. Surg Endosc 34:5030–5040
Untereiner X, Cagniet A, Memeo R, Cherkaoui Z, Piardi T, Severac F, Mutter D, Kianmanesh R, Wakabayashi T, Sommacale D, Pessaux P (2019) Laparoscopic hepatectomy versus open hepatectomy for the management of hepatocellular carcinoma: a comparative study using a propensity score matching. World J Surg 43:615–625
Vanounou T, Steel JL, Nguyen KT, Tsung A, Marsh JW, Geller DA, Gamblin TC (2010) Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol 17:998–1009
Wang XT, Wang HG, Duan WD, Wu CY, Chen MY, Li H, Huang X, Zhang FB, Dong JH (2015) Pure laparoscopic versus open liver resection for primary liver carcinoma in elderly patients: a single-center, case-matched study. Medicine 94:e1854
Yin SM, Liu YW, Liu YY, Yong CC, Wang CC, Li WF, Yeh CH (2021) Short-term outcomes after minimally invasive versus open pancreaticoduodenectomy in elderly patients: a propensity score-matched analysis. BMC Surg 21:60
Zeng Y, Tian M (2016) Laparoscopic versus open hepatectomy for elderly patients with liver metastases from colorectal cancer. J BUON 21:1146–1152
Aly S, de Geus SWL, Carter CO, Hess DT, Tseng JF, Pernar LIM (2021) Laparoscopic versus open ventral hernia repair in the elderly: a propensity score-matched analysis. Hernia 25:673–677
Dallas KB, Froylich D, Choi JJ, Rosa JH, Lo C, Colon MJ, Telem DA, Divino CM (2013) Laparoscopic versus open inguinal hernia repair in octogenarians: a follow-up study. Geriatr Gerontol Int 13:329–333
Hernandez-Rosa J, Lo CC, Choi JJ, Colon MJ, Boudourakis L, Telem DA, Divino CM (2011) Laparoscopic versus open inguinal hernia repair in octogenarians. Hernia 15:655–658
Neupane R, Fayezizadeh M, Majumder A, Novitsky YW (2017) Is old age a contraindication to elective ventral hernia repair? Surg Endosc 31:4425–4430
Payiziwula J, Zhao PJ, Aierken A, Yao G, Apaer S, Li T, Tuxun T (2019) laparoscopy versus open incarcerated inguinal hernia repair in octogenarians: single-center experience with world review. Surg Laparosc Endosc Percutan Tech 29:138–140
Ostermann S, Morel P, Chalé JJ, Bucher P, Konrad B, Meier RPH, Ris F, Schiffer ERC (2019) Randomized controlled trial of enhanced recovery program dedicated to elderly patients after colorectal surgery. Dis Colon Rectum 62:1105–1116
Bu J, Li N, Huang X, He S, Wen J, Wu X (2015) Feasibility of fast-track surgery in elderly patients with gastric cancer. J Gastrointest Surg 19:1391–1398
Cao S, Zheng T, Wang H, Niu Z, Chen D, Zhang J, Lv L, Zhou Y (2021) Enhanced recovery after surgery in elderly gastric cancer patients undergoing laparoscopic total gastrectomy. J Surg Res 257:579–586
Jiang W, Mao Q, Xie Y, Ying H, Xu H, Ge H, Feng L, Liu H, Li J, Liang X (2020) Enhanced recovery after surgery (ERAS) program in elderly patients undergoing laparoscopic hepatectomy: a retrospective cohort study. Transl Cancer Res 9:4563–4572
Partelli S, Crippa S, Castagnani R, Ruffo G, Marmorale C, Franconi AM, De Angelis C, Falconi M (2016) Evaluation of an enhanced recovery protocol after pancreaticoduodenectomy in elderly patients. HPB 18:153–158
Acknowledgements
The authors acknowledge Ms. Therese Velthoven and Sunjay Kumar, MD, for their help organizing and supporting the participants and process of this work.
Funding
SAGES and EAES provided staff support and meeting space at their respective meetings for the conference preparation and planning. SAGES allocated funds for the methodologists, the librarian, and salary support for the fellow.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Al-Mansour—Medtronic honorarium; Abbvie honorarium; Intuitive surgery—educational payments; Gore general payments; Duval general payments. Leeds—Intuitive surgery—product development consultant. Deborah S Keller, Nathan Curtis, Holly Ann Burt, Carlo Alberto Ammirati, Amelia T Collings, Francisco Carrano, Stavros A. Antoniou, Nader Hanna, Laure-Meline Piotet, Sarah Hill, Anne CM Cuijpers, Patricia Tejedor, Marco Milone, Eleni Andriopoulou, Christos Kontovounisios, Ziad T Awad, Meghan Wandtke Barber, George Nassif, Malcolm A West, Aurora D Pryor, Franco Carli, Nicholas Demartines, Nicole D Bouvy, Roberto Passera, Alberto Arezzo, and Nader Francis have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplement 1 PICO Questions and Literature Search Strategies
Supplementary file1 (DOCX 122 KB)
Supplement 2 PRISMA Flow Diagrams
Supplementary file2 (DOCX 614 KB)
Supplement 3 Quality Assessment for KQ1-KQ16
Supplementary file3 (DOCX 21 KB)
Supplement 4 Evidence to Decision (EtD) tables for KQ17-KQ24
Supplementary file4 (DOCX 103 KB)
Supplement 5 Forest plots for KQ17-KQ24
Supplementary file5 (PDF 349 KB)
Supplement 6 Quality assessment for KQ17-KQ24
Supplementary file6 (DOCX 39 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Keller, D.S., Curtis, N., Burt, H.A. et al. EAES/SAGES evidence-based recommendations and expert consensus on optimization of perioperative care in older adults. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-10977-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-10977-7