Abstract
Introduction
Colorectal cancer is the second most common cause of death from neoplastic disease in men and third in women of all ages. Globally, life expectancy is increasing, and consequently, an increasing number of operations are being performed on more elderly patients with the trend set to continue.
Elderly patients are more likely to have cardiovascular and pulmonary comorbidities that are associated with increased peri-operative risk. They further tend to present with more locally advanced disease, more likely to obstruct or have disseminated disease.
The aim of this review was to investigate the feasibility of laparoscopic colorectal resection in very elderly patients, and whether there are benefits over open surgery for colorectal cancer.
Methods
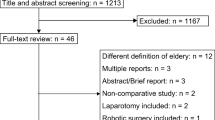
A systematic literature search was performed on Medline, Pubmed, Embase and Google Scholar. All comparative studies evaluating patients undergoing laparoscopic versus open surgery for colorectal cancer in the patients population over 85 were included.
The primary outcomes were 30-day mortality and 30-day overall morbidity. Secondary outcomes were operating time, time to oral diet, number of retrieved lymph nodes, blood loss and 5-year survival.
Results
The search provided 1507 citations. Sixty-nine articles were retrieved for full text analysis, and only six retrospective studies met the inclusion criteria. Overall mortality for elective laparoscopic resection was 2.92% and morbidity 23%. No single study showed a significant difference between laparoscopic and open surgery for morbidity or mortality, but pooled data analysis demonstrated reduced morbidity in the laparoscopic group (p = 0.032). Patients undergoing laparoscopic surgery are more likely to have a shorter hospital stay and a shorter time to oral diet.
Conclusion
Elective laparoscopic resection for colorectal cancer in the over 85 age group is feasible and safe and offers similar advantages over open surgery to those demonstrated in patients of younger ages.

Similar content being viewed by others
References
Malvezzi M, Arfe A, Bertuccio P et al (2011) European cancer mortality predictors for the year 2011. Ann Oncol 22:947–956
Rossi T, Malvezzi M, Bosetti C et al (2016) Cancer mortality in Europe, 1970–2009: an age, period and cohort anaysis. Eur J Cancer Prev. doi:10.1097/CEJ.0000000000000282
Yamauchi M, Lochhead P, Morikawa T et al (2012) Colorectal cancer: a tale of two sides or a continuum? Gut 61:794–797
Stepien S, Gluszek S, Koziel D et al (2014) The risk of surgical treatment in patients aged 85+, with special consideration of colorectal cancer. Pol Prezegl Chir 86(3):132–140
Merlin F, Prochilo T, Tondulli L et al (2008) Colorectal cancer treatment in elderly patients: an update on recent clinical studies. Clin Colorectal Cancer 7:357–363
Akiyoshi T, Kuroyanagi H, Oya M et al (2009) Short-term outcomes of laparoscopic rectal surgery for primary rectal cancer in elderly patients: is it safe and beneficial? J Gastrointest Surg 13:1614–1618
Amemiya T, Oda K, Ando M et al (2007) Activities of daily living and quality of life of elderly patients after elective surgery for gastric and colorectal cancer. Ann Surg 246:222–228
Ganai S, Lee KF, Merrill A et al (2007) Adverse outcomes of geriatric patients undergoing abdominal surgery who are at high risk for delirium. Arch Surg 142:1072–1078
Scott NA, Jeacock J, Kingston RD (1995) Risk factors in patients presenting as an emergency with colorectal cancer. Br J Surg 82:321–323
Turrentine FE, Wang H, Simpson V et al (2007) Surgical risk factors, morbidity and mortality in elderly patients. J Am Coll Surg 203:865–877
Jafari MD, Hafari F, Halabi WJ et al (2014) Colorectal cancer resections in the aging US population: a trend toward decreasing rates and improved outcomes. JAMA Surg 149:557–564
Longo WE, Virgo KS, Johnson FE et al (2000) Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum 43:4383–4391
Guillou PJ, Quirke P, Thorpe H et al (2005) Short term end points of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Neudecker J, Klein F, Bittner R et al (2009) Short-term outcomes from a prospective randomized trial comparing laparoscopic and open surgery for colorectal cancer. Br J Surg 96:1458–1467
Takahata O, Kunisawa T, Nagashima M et al (2007) Effect of age on pulmonary gas exchange during laparoscopy in the Trenedelenburg lithotomy position. Acta Anaesthesiol Scand 51:687–692
Van der Pas MH, Haglind E, Cuesta MA et al (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Moher D, Liberati A, Telzlaff J et al (2009) Preferred reporting items for systematic review and meta-analyses: the PRISMA statement. BMJ 339:b2535
Deeks JJ, Dinnes J, D’Amico R, International Stroke Trial Collaborative Group, European Carotid Surgery Trial Collaborative Group et al (2003) Evaluating non-randomised intervention studies. Health Technol Assess 7(27):iii-x):1–173
Tominaga T, Takeshita H, Arai J et al (2015) Short-term outcomes of laparoscopic surgery for colorectal cancer in oldest-old patients. Dig Surg 32:32–38
Mukai T, Akiyoshi T, Ueno M et al (2014) Outcomes of laparoscopic surgery for colorectal cancer in oldest-old patients. Surg Laparosc Endosc Percutan Tech 24:366–369
Vallribera Valls F, Landi F, Espin Basany E et al (2014) Laparoscopy-assisted versus open colectomy for treatment of colon cancer in the elderly: morbidity and mortality outcomes in 545 patients. Surg Endosc 28:3373–3378
Nakamura T, Sato T, Miura H et al (2014) Feasibility and outcomes of surgical therapy in very elderly patients with colorectal cancer. Surg Laparosc Endosc Percutan Tech 24:85–88
van Walraven C, Austin PC, Jennings A et al (2009) A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 47:626–633
Hernandas AK, Abdelrahman T, Flashman KG et al (2010) Laparoscopic colorectal surgery produces better outcomes for high risk cancer patients compared to open surgery. Ann Surg 252:84–89
Harari D, Hopper A, Dhesi J et al (2007) Proactive care of older people undergoing surgery (‘POPS’): designing, embedding, evaluating and funding a comprehensive geriatric assessment service for older elective surgical patients. Age Ageing 36(2):190–196
Marush F, Gastinger I, Schneider C et al (2001) Experience as a factor influencing the indications for laparoscopic colorectal surgery and the results. Surg Endosc 15:116–120
Giglio MC, Celentano V, Tarquini R et al (2015) Conversion during laparoscopic colorectal resections: a complication or a drawback? A systematic review and meta-analysis of short-term outcomes. Int J Color Dis 30(11):1445–1455
Tekkis PP, Senagore A, Delaney et al (2005) Evaluation for the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Mackenzie H, Miksovic D, Ni M et al (2013) Clinical and educational proficiency gain of supervised laparoscopic colorectal surgical trainees. Surg Endosc 27:2704–2711
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Devoto, L., Celentano, V., Cohen, R. et al. Colorectal cancer surgery in the very elderly patient: a systematic review of laparoscopic versus open colorectal resection. Int J Colorectal Dis 32, 1237–1242 (2017). https://doi.org/10.1007/s00384-017-2848-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2848-y