Abstract
Background
Artemether-lumefantrine (AL) and dihydroartemisinin-piperaquine (DP) are the currently recommended first- and second-line therapies for uncomplicated Plasmodium falciparum infections in Togo. This study assessed the efficacy of these combinations, the proportion of Day3-positive patients (D3 +), the proportion of molecular markers associated with P. falciparum resistance to anti-malarial drugs, and the variable performance of HRP2-based malaria rapid diagnostic tests (RDTs).
Methods
A single arm prospective study evaluating the efficacy of AL and DP was conducted at two sites (Kouvé and Anié) from September 2021 to January 2022. Eligible children were enrolled, randomly assigned to treatment at each site and followed up for 42 days after treatment initiation. The primary endpoint was polymerase chain reaction (PCR) adjusted adequate clinical and parasitological response (ACPR). At day 0, samples were analysed for mutations in the Pfkelch13, Pfcrt, Pfmdr-1, dhfr, dhps, and deletions in the hrp2/hrp3 genes.
Results
A total of 179 and 178 children were included in the AL and DP groups, respectively. After PCR correction, cure rates of patients treated with AL were 97.5% (91.4–99.7) at day 28 in Kouvé and 98.6% (92.4–100) in Anié, whereas 96.4% (CI 95%: 89.1–98.8) and 97.3% (CI 95%: 89.5–99.3) were observed at day 42 in Kouvé and Anié, respectively. The cure rates of patients treated with DP at day 42 were 98.9% (CI 95%: 92.1–99.8) in Kouvé and 100% in Anié. The proportion of patients with parasites on day 3 (D3 +) was 8.5% in AL and 2.6% in DP groups in Anié and 4.3% in AL and 2.1% DP groups in Kouvé. Of the 357 day 0 samples, 99.2% carried the Pfkelch13 wild-type allele. Two isolates carried nonsynonymous mutations not known to be associated with artemisinin partial resistance (ART-R) (A578S and A557S). Most samples carried the Pfcrt wild-type allele (97.2%). The most common Pfmdr-1 allele was the single mutant 184F (75.6%). Among dhfr/dhps mutations, the quintuple mutant haplotype N51I/C59R/S108N + 437G/540E, which is responsible for SP treatment failure in adults and children, was not detected. Single deletions in hrp2 and hrp3 genes were detected in 1/357 (0.3%) and 1/357 (0.3%), respectively. Dual hrp2/hrp3 deletions, which could affect the performances of HRP2-based RDTs, were not observed.
Conclusion
The results of this study confirm that the AL and DP treatments are highly effective. The absence of the validated Pfkelch13 mutants in the study areas suggests the absence of ART -R, although a significant proportion of D3 + cases were found. The absence of dhfr/dhps quintuple or sextuple mutants (quintuple + 581G) supports the continued use of SP for IPTp during pregnancy and in combination with amodiaquine for seasonal malaria chemoprevention.
Trial registration: ACTRN12623000344695.
Similar content being viewed by others
Background
Malaria, a preventable and treatable disease, is estimated to cause 247 million cases and 619,000 deaths in 2021 [1]. The African region of the World Health Organization (WHO) accounts for 94% of global cases and deaths, with the burden concentrated in children under five years of age. Prompt and effective treatment of uncomplicated Plasmodium falciparum infections is the cornerstone of malaria control and elimination. Currently, the WHO recommends six artemisinin-based combinations for the treatment of uncomplicated falciparum malaria [2]: artemether-lumefantrine (AL), artesunate-amodiaquine (ASAQ), dihydroartemisinin-piperaquine (DP), artesunate-mefloquine (ASMQ), artesunate-sulfadoxine/pyrimethamine (ASSP), and artesunate-pyronaridine (AP).
Plasmodium falciparum resistance to anti-malarial drugs remains a common threat to effective case management and undermines global efforts to control and eliminate the malaria burden. Artemisinin partial resistance (ART -R), first described in Southeast Asia in 2008 [3, 4], is defined as delayed clearance (persistent parasitaemia at day 3-D3 +—or parasite clearance half-life > 5 h) after administration of artemisinin-based combination therapy (ACT) or artesunate monotherapy [5]. In vitro, ART-R is manifested by increased survival of early ring stage parasites (0–3 h post-invasion) after exposure to 700 nM dihydroartemisinin for 6 h [6, 7]. The emergence and spread of ART-R parasites in Southeast Asia was later followed by high rates of DP and ASMQ treatment failure associated with piperaquine and mefloquine resistance [8]. Molecular studies have confirmed the presence of non-synonymous mutations in Pfkelch13 (PF3D7_1343700) as the primary determinant of ART-R [7, 9]. Currently, there are 13 validated (F446I, N458Y, M476I, Y493H, R539T, I543T, P553L, R561H, P574L, C580Y, C469Y, R622I, A675V) and nine candidate/associated (P441L, G449A, C469F, A481V, R515K, P527H, N537I/D, G538V, V568G) Pfkelch13 mutations [6].
In sub-Saharan Africa, where most of the malaria burden occurs, the recent emergence and spread of validated Pfkelch13 mutations in Rwanda (R561H), Uganda (A675V or C469Y), and the Horn of Africa (R622I) is of great concern [10,11,12,13,14]. This calls for frequent monitoring of the efficacy of first- and second-line ACT, including parasite clearance, and the prevalence of Pfkelch13 mutations, as recommended by the WHO [5]. Increased copy numbers in the plasmepsin II (pm2) and Plasmodium multi-drug resistance 1 (Pfmdr-1) genes have been associated with piperaquine [15] and mefloquine [16] resistance, respectively, resulting in decreased efficacy of DP [8, 17,18,19,20,21] and ASMQ [18, 22]. Although not yet validated [23], polymorphisms in the chloroquine resistance transporter (Pfcrt) and Pfmdr-1 have been implicated in resistance to piperaquine, mefloquine, lumefantrine, and amodiaquine [24, 25]. In sub-Saharan Africa, the WHO also recommends chemoprevention to protect pregnant women with intermittent preventive treatment (IPTp) with sulfadoxine/pyrimethamine (SP) [26] and children using seasonal malaria chemoprevention (SMC) with sulfadoxine/pyrimethamine-amodiaquine (SPAQ) [27]. Polymorphisms in several codons in the genes encoding dihydrofolate reductase (dhfr) and dihydropteroate synthase (dhps) of P. falciparum are associated with an increased risk of SP treatment failure [28]. A quintuple mutation (51I, 59R, and 108N in the dhfr genes and 437G + 540E in the dhps genes) is a predictor of SP treatment failure [29, 30]. A sextuple mutant (quintuple + A581G) defined as super-resistant is associated with reduced efficacy of IPT-SP in pregnant women [31, 32] and infants [33].
Malaria is a major health problem in Togo, and the entire population is at risk, with children under five years of age being the most affected. Malaria transmission is stable, but with seasonal peaks from June to October in the north and from April to July and then from August to October in the south [34]. The estimated number of malaria cases and deaths in 2021 were 2.1 million and 3,715, respectively [1]. Since 2004, the Togolese National Malaria Control Programme (NMCP) has recommended AL and ASAQ for the treatment of uncomplicated P. falciparum infection [35]. Following the recommendation of SPAQ for seasonal malaria chemoprevention (SMC) in 2016, ASAQ was replaced by DP as second-line therapy for the treatment of uncomplicated falciparum infection [36]. The NMCP monitored the therapeutic efficacy of AL and ASAQ until 2013 and showed high efficacy with PCR-corrected cure rates of 96% or more for AL and 94% or more for ASAQ [35, 37].
The objectives of the present study were to evaluate the proportion of patients testing positive at day 3 (D3 +) and to assess the efficacy of AL and DP for the treatment of children with uncomplicated P. falciparum malaria. In addition, mutations in Pfkelch13, Pfcrt, Pfmdr-1, dhfr, dhps associated with P. falciparum resistance to anti-malarial drugs and deletions in hrp2/hrp3 involved in variable performance of HRP2-based malaria rapid diagnostic tests (RDTs) were also investigated in isolates collected prior anti-malarial treatment.
Methods
Study design, population and areas
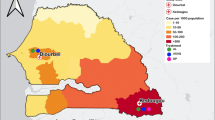
This single arm prospective study evaluated the efficacy of AL or DP for the treatment of uncomplicated P. falciparum malaria in children aged 6–59 months. Eligible children were randomly assigned (not blinded) to receive either the AL or the DP. The study was conducted at the “La Providence” hospital in Kouvé for the Yoto District and the district hospital in Anié. The Kouvé site, located in the Maritime region, is approximately 76 km from the capital city (Lomé), and the Anié site, located in the Plateaux region, is 188 km from Lomé (Fig. 1).
Recruitment
Patients attending the “La Providence hospital” in Kouvé and the Anié district hospital between 14 September 2021, and 29 January 2022, were screened for inclusion and exclusion criteria according to the WHO protocol [38]. After obtaining parental/guardian consent, children were enrolled if they were between 6 and 59 months of age, had an axillary temperature of ≥ 37.5 °C or a history of fever in the previous 24 h, had P. falciparum mono-infection with parasitaemia of at least 2,000 to 200,000 asexual parasites/µL based on microscopy, were able to take medicine orally, and agreed to be available for scheduled assessments during the study period. Children with severe falciparum malaria or danger signs according to the WHO definition [39], non-falciparum species or severe malnutrition, third-party administration of anti-malarial drugs, and non-malarial febrile illness were not enrolled, but received appropriate treatment according to national guidelines. Other exclusion criteria included body weight < 5 kg, haemoglobin level < 5 g/dl, regular medication interfering with anti-malarials pharmacokinetics, hypersensitivity to the test drugs, and treatment with AL or DP in the previous 48 h.
Treatment and follow-up assessment
Recruited children were treated with either the AL or DP using random allocation sheets designed for this purpose. AL (20 mg artemether + 120 mg lumefantrine) was administered twice daily for three days based on the recommended weight bands: 1 tablet for 5–14 kg, 2 tablets for 15–24 kg, and 3 tablets for 25–34 kg). DP with a target daily dose of 4 mg/kg dihydroartemisinin + 18 mg/kg piperaquine for three days was administered as follows: ½ tablet (20/160 mg) for 5–6 kg, 1 tablet (20/160 mg) for 7–12 kg, 1 tablet (40/320 mg) for 13–23 kg, and 2 tablets (40/320 mg) for 24–35 kg. The study drugs were provided by the WHO and stored in a cool place. AL and DP were manufactured by Cipla Pharmaceutical Company LTD (India) and Fosun Pharma (China), respectively.
All treatment doses were administered under the direct supervision of the study nurse and observed for 30 min after administration. Any patient who vomited during the observation period was re-treated with the same dose of the test drug and observed for an additional 30 min. Children who vomited a second time were excluded from the study and were referred or admitted to the hospital, where the nationally recommended injectable artesunate was administered according to the national treatment guidelines. The parent/guardian of each recruited child enrolled was asked not to give any other medication during the follow-up period and to bring the child back if the child’s condition worsened.
Enrolled children were followed up for 42 days after the start of the treatment. Clinical and parasitological responses were monitored at scheduled visits on days 1, 2, 3, 7,14, 21, 28, 35, and 42, and on unscheduled days if the child’s condition worsened or symptoms recurred during the unscheduled days. The time window allowed for weekly follow-up was one day. Adverse events and severe adverse events, defined according to the WHO protocol for monitoring the therapeutic efficacy of anti-malarials [38], were clinically monitored at each follow-up visit. Adverse events were managed according to local practice as dictated by the pharmacovigilance department and the NMCP.
Microscopy examination
Thick and thin blood smears were obtained from the fingerprick at day 0 and at follow-up visits. The blood slides were stained with Giemsa, and parasites were counted as the number of asexual parasites per 200 white blood cells (WBCs) or per 500 if the count was < 100 parasites/200 WBCs using the WHO method [38]. Each blood slide was examined independently by two qualified microscopists using Olympus CX23 microscope (Olympus Corporation, Tokyo, Japon), and the final parasitaemia was calculated by averaging the results of the two microscopists if they agreed (difference in parasite density < 50%). If the two counts differed by > 50% for parasite positivity, species, or density, the slides were re-examined by a third independent microscopist. For parasite species and positivity, two concordant results were considered the final result, whereas for parasite density, the average of the two closest estimates of parasitaemia was considered the final result. A blood slide was considered negative if no parasites were seen after counting 1000 WBCs. The presence of gametocytes at enrolment or follow-up was recorded. In addition, 100 fields of thick smears were examined on day 0 to exclude mixed infections. In cases of doubt, the thin film was examined for confirmation.
Parasite genotyping
Filter paper blood samples (prepared from 2 to 3 drops of blood applied to Whatman #3 filter paper) were collected from each patient on day 0 and on the day of parasite recurrence (from day 7 onwards) and stored in individual plastic bags with desiccant until analysis, protecting them safe from light, moisture, and extreme temperatures. Each dried blood spot (DBS) was cut and placed in an Eppendorf tube. The 96-well protocol developed by Zainabadi et al. [40] was used to extract parasite DNA.
The eluted DNA was then quantified using fluorometric quantification (Thermo Fisher's Qubit) to 20 ng/µL and stored at − 20 °C for later use. According to recent WHO recommendation [41], paired DNA from patients with recurrent parasites (day 0 and day of recurrence) was genotyped using nested polymerase chain reaction (PCR) targeting the highly polymorphic genes msp1 and msp2, and the microsatellite marker poly-α. All markers were systematically analysed. Capillary electrophoresis (Bioanalyzer, Agilent) was used to estimate fragment sizes, with cut-offs for PCR artifacts and stutter peaks set at 10% of the lower and upper control bands. The bins used to define a match were 10 bp for msp1/msp2, and 5 bp for poly-α. The genotyping data were compared with the previous genotyping approach for msp1, msp2, and glurp [42]. For glurp, the bin used to define a match was 20 bp. The WHO decision algorithm was used to calculate PCR-adjusted clinical efficacy rates. Recrudescence was defined as a genotype that had previously been detected in a blood sample taken prior to treatment (i.e., at least one allele was shared at all three loci on day 0 and the day of parasite recurrence). A new infection was defined as the absence of a shared allele at any of the three loci between day 0 and the day of parasite recurrence.
Markers of anti-malarial drug resistance
Day 0 DNA was examined for the presence of point mutations in the Pfkelch13 gene (codons 430-720) associated with ART-R [3], the Pfcrt gene (codons 72-76, 93, 145, 218, 343, 350, and 353), and Pfmdr-1 genes (codons 86, 184, 1034, 1042, and 1246) linked to 4-aminoquinolines and amino alcohol resistance [25] and the dhfr (codons 51, 59, 108, and 164) and dhps (codons 431, 436, 437, 540, 581, and 613) genes associated with pyrimethamine and sulfadoxine resistance [29]. Additionally, hrp2 and hrp3 gene deletions that may result in false-negative HRP2-based rapid diagnostic tests (RDTs) were examined [43].
As previously described [44], multiplex nested PCR assays with indexed primers with unique sample-specific tags (barcodes of individual 8-base indices) specific to the sample and adapter sequences (14 or 15 bases), which enabled the final PCR product to bind to the sequencing flow cell, were used to generated amplicons of targeted sequences were produced. To increase the sample volume and reduce the amount of sample for subsequent protocol steps, 4 µL of PCR reactions for each sample was pooled (96 samples). The amplicons were then purified for each pool using AMPure XP beads (Beckman Coulter), according to the manufacturer's instructions, to remove dNTPs, salts, primers, and primer dimers. The quality of the purified PCR products was assessed by analysing the eluates containing purified amplicons on a Bioanalyzer (Agilent). Fluorometric quantification (Qubit, Thermo Fisher) was used to determine the DNA concentration of the combined fragments. Prior to sequencing, the pooled libraries were denatured with 0.2 N NaOH, neutralized with 0.2 M Tris–HCL pH 7.5 before dilution with hybridisation buffer (HT1). Sequencing was performed using the MiSeq v2 reagent and the Illumina MiSeq Reagent kit v2 (300-cycles) according to the manufacturer’s instructions. Raw sequences were demultiplexed and quality reduced at a Phred score of 30. To avoid primer bias in the sequenced fragments, primer sequences were clipped from the 5′ end. Base calling was performed by comparing the reads to a custom database consisting of the 3D7 reference sequence. Bioinformatics analysis was carried out with the use of CLC Genomics Workbench 22 software (Qiagen). Laboratory reference parasite strains with known alleles for each gene (Dd2, 7G8, HB3, and a Cambodian strain 3601) were used as controls [13].
Haemoglobin blood concentration
Blood haemoglobin concentration was measured on day 0 (prior to treatment) and on days 7, 14, 21, 28, 35, and 42 using a HemoCue Hb 301 apparatus (HemoCue AB, Ängelholm, Sweden) to assess the recovery of hAemoglobin levels.
Classification of treatment outcome
Using WHO criteria [39], treatment outcomes were classified as an early treatment failure (ETF), late clinical failure (LCF), late parasitological failure (LPF) or adequate clinical and parasitological response (ACPR) before and after Polymerase Chain Reaction (PCR) correction. The primary endpoints were PCR-corrected per-protocol ACPR and Kaplan–Meier cure rates at day 28 and day 42 for AL and DP. The proportion of patients lost to follow-up and withdrawals was also calculated. Withdrawals included protocol violations, withdrawal of consent, failure to complete the study treatment (persistent vomiting, self- or third-party administration of anti-malarial drugs or antibiotics with anti-malarial activity, occurrence of concomitant disease during follow-up that would interfere with a clear classification of the treatment outcome, detection of mono-infection with another malaria species during follow-up, or misclassification of a patient due to a laboratory error (parasitaemia) leading to administration of rescue treatment).
Sample size
A treatment failure rate of 5% for both AL and DP was assumed. A minimum sample size of 73 patients per site per drug was estimated at 95% confidence level with 5% precision. With a 20% increase to account for loss to follow-up and withdrawals during the 28-day or 42-day follow-up period, 88 patients per site per drug were targeted.
Statistical analysis
Clinical and laboratory data for each patient were recorded on standard case record forms, double-entered independently, and analysed using a WHO Excel® database specifically designed for studies of anti-malarial drug efficacy (https://www.who.int/malaria/areas/drug_resistance/efficacy-monitoring-tools/en/).
Both per-protocol and Kaplan–Meier analyses were performed. For the per-protocol analysis, patients were excluded if they were lost to follow-up or withdrew during follow-up. In addition, patients with reinfection or indeterminate PCR results were excluded from the PCR-corrected per-protocol analysis. For the Kaplan–Meier analysis, patients who were lost to follow-up or withdrew during follow up were censored on the last day of follow-up, those with new infection were censored on the day of reinfection, and those with undetermined PCR were excluded. Baseline characteristics (age, sex, temperature, and parasitaemia) were compared between the two study sites according to the artemisinin-based combinations used for the treatment. Chi-square tests were used to compare categorical data. Differences in mean baseline age and parasite density were assessed using a two-sample Wilcoxon rank-sum (Mann–Whitney) test for non-normally distributed data. Gametocyte positivity rates at enrolment and follow-up were calculated. In addition, gametocyte clearance after treatment was assessed using Kaplan–Meier survival analysis. Confidence intervals were calculated for binomial proportions. Two-sided p-values of less than 0.05 were considered statistically significant.
Ethical considerations
The study protocol was approved by the Committee of Bioethics for Research in the Health of Togo. Parents or caregivers of the children were informed of the aims and procedures of the study and provided written informed consent. If a parent or caregiver was illiterate, they chose a witness to sign the consent form. All children enrolled in the study received free care throughout the follow-up period. All hospitalization costs were covered by the project. Travel expenses for scheduled and unscheduled visits were reimbursed and each child received treated mosquito bed nets. Community leaders in the areas surrounding the study sites were informed of the study objectives and procedures.
Results
Socio-demographic profile of the study children
Of the 741 children screened (343 in Anié and 398 in Kouvé) between September 2021 and January 2022, 165 (82 for AL and 83 for DP) in Anié and 192 (97 for AL and 95 for DP) in Kouvé were eligible and enrolled in the study (Table 1). The baseline characteristics of the different groups were comparable, except for parasitaemia. Patients in Kouvé had significantly higher parasitaemia compared to Anié for both AL and DP treatment groups (p < 0.0001 between AL groups; p < 0.0001 for AL vs. DP groups; and p < 0.0001 between the DP treated groups). Quality control of the blood slides by an experienced microscopist revealed that 20 children had parasitaemia above the upper limit of 200,000 asexual parasites/microlitre of blood on day 0 according to the protocol. Of these, three cases were in the DP group in Anié, 11 in the DP group in Kouvé, and 6 in the AL group in Kouvé. There was no significant difference between mean Hb levels on day 0 of children with parasitaemia ≥ 200,000 asexual parasites/microlitre and those above this threshold within each treatment group (p = 0.2 for Anié DP, p = 0.5 for Kouvé Al, and p = 0.7 for Kouvé DP).
Treatment outcome
Table 2 summarizes the unadjusted PCR outcomes at days 28 and 42 based on per-protocol and Kaplan–Meier analysis. At day 28, the per-protocol PCR-uncorrected cure rates for AL were 88.8% and 88.6% for Kouvé and Anié, respectively, and for DP were 98.9% and 97.4% for Kouvé and Anié, respectively. At day 42, the PCR-uncorrected cure rates for AL were 82.0% and 83.5% for Kouvé and Anié, respectively, while the cure rates for DP were 92.2%, and 94.7%, for Kouvé and Anié, respectively. Similar rates were observed in the Kaplan–Meier analysis (Table 2). Most recurrences were observed in the AL-treated group. In Kouvé, 10 patients (AL) and 1 patient (DP) experienced parasite recurrence on day 28. Similarly, in Anié, 9 patients (AL) and 2 patients (DP) had parasite recurrence on day 28. y day 42, the number of patients with parasite recurrence was 16 patients (AL) and 7 patients 4 patients (DP) had parasite recurrence in Anié.
Of the 40 recurrences detected at day 42, 6 were found to be recrudescent infections (true treatment failure), 5 gave non-conclusive genotyping results (3 in Kouvé and 2 in Anié of the AL-treated groups), and 29 were classified as new infections (based on the genotyping approach using nested polymerase chain reaction (PCR) targeting the highly polymorphic genes msp1 and msp2, and the microsatellite marker poly-α and the WHO/MMV match-counting algorithm (3/3), as recommended by the WHO) [42]. Details are shown in Additional file 1: Table S1.
On day 28, per-protocol PCR-corrected cure rates of 97.5% and 98.6% were observed for AL in Kouvé and Anié, respectively, while children treated with DP achieved a 100% cure rates in both sites (Table 3). At day 42, PCR-corrected AL cure rates of 96.1% and 97.1% were observed in Kouvé and Anié, respectively, and PCR-corrected DP cure rates of 98.8% and 100% were observed in Kouvé and Anié, respectively. Kaplan–Meier analysis showed almost similar cure rates (Table 3). Parasite persistence on day 3 (D3 +) in Anié were detected in 7/82 patients (8.5%, CI 95%: 3.5–16.8%) treated with AL and 2/76 patients (2.6%, CI 95%: 0.3–9.2%) treated with DP. The difference in proportions between AL and DP groups was not significant (p = 0.17, Fisher’s exact test). In Kouvé, 4/93 patients (4.3%, CI 95%: 1.2–10.6%) treated with AL and 2/94 patients (2.1%, CI 95%: 0.3–7.5%) treated with DP had parasites on day 3. Again, the difference in proportions was not significant (p = 0.44, Fisher’s exact test). Parasite densities found on day 3 were very low across all sites, ranging from 11 to 72 asexual parasites per microlitre. Out of the 20 cases with day 0 parasitaemia ≥ 200,000 asexual parasite/microlitre of blood, 19 were parasite free at day 3 and achieved ACPR. The remaining case was parasite positive on day 3 and had recrudescence at day 42.
Of the 357 children included in the cohorts, 35 (9.8%) reported mild adverse reactions on days 1 and 2: 16 with vomiting, 18 with weakness and 1 case with anorexia. Vomiting was more frequent in the DP group (6.2%, 11/179) than in the AL group (2.8%, 5/178), but the difference was not significant (p = 0.13, Fisher exact test).
Haemoglobin recovery
There was a significant progressive increase in mean haemoglobin levels during the follow-up visits except at day 7 for Kouvé where no significant increase or even a significant decrease was observed (Table 4). There was no significant difference between mean Hb levels of children with parasitaemia ≤ 200,000 and those above this threshold except for Kouvé DP group at day 14 (Hb day14 of 10.5 g/dl vs 9.3 g/dl, p = 0.01, respectively).
Molecular markers of anti-malarial drug resistance
All 357 day 0 samples were successfully analysed for mutations in the Pfkelch13, Pfcrt, Pfmdr-1, dhfr, and dhps genes. Details are shown in Table 5 and 6. Of these, 99.2% (354/357) carried the Pfkelch13 wild-type allele. Two isolates from Kouvé carried the A578S mutation, which is known not to confer resistance in vitro, and one isolate from Kouvé carried the A557S mutation, which is a non-validated Pfkelch13 mutation.
For Pfcrt, five mutations were identified, and five different alleles were detected, of which 97.2% were wild type. The most frequent other parasites were those carrying the 74I/75E/76 T/356 T allele (1.4%), followed by those carrying the 74I/75E/76 T allele (0.6%), the 356 T allele (0.6%), and the 72S/76 T allele (7G8 allele, 0.3%). It is noteworthy that a significant difference in proportion was observed between sites for the I356T mutation, which was only detected in Kouvé (3.6% in Kouvé vs. 0% in Anié, p = 0.01).
For Pfmdr-1, two mutations were found (N86Y and 184F) and three alleles were identified, including the 184F single mutant (75.6%), the wild-type allele (24.1%), and the 86Y/184F double mutants (0.3%). Similar proportions of mutations were found between the two sites.
Three mutations (N51I, C59R and S108N) and five different dhfr alleles were detected in the tested isolates. These included the triple 51I/59R/108N mutant allele (72.3%), the double 51I/59R mutant allele (22.4%), the double 59R/108N mutant allele (4.2%), the single 59R mutant allele (0.8%), and the wild-type allele (0.3%). Significant differences in proportions were observed for the S108N mutation (61.2% in Kouvé vs. 89.6% in Anié, p < 10–6) and for the distribution of the dhfr alleles between sites (p < 0.0001).
For dhps, 6 mutations (I431V, S436A, G437A, K540E, A581G and A613S) and 12 alleles were found. The most common allele was the wild-type allele (47.3%). The single 436A mutant allele was found in 32.8% of the isolates tested, followed by the double 436A/613S mutant allele (9.8%), the double 431 V/436A mutant allele (2.8%), and the double 436A/437A mutant allele (2.0%). The 540E and 581G mutations were observed in two and ten isolates, respectively. No significant difference in frequency was observed.
Combining the two dhfr/dhps loci without estimating the complexity of infection allowed the frequency of the dhfr/dhps haplotypes to be inferred. Twenty-five haplotypes were found. The most frequent dhfr/dhps haplotype was the triple 51I/59R/108N mutant (33.3%), followed by the quadruple 51I/59R/108N + 436A mutant (24.6%), the double 51I/59R mutant (10.6%), the triple 51I/59R + 436A mutant (7.3%), and the quintuple 51I/59R/108N + 436A/613S mutant (7.3%). The 59R/108N double mutant (2.5%) and the 51I/59R + 436A/613S quadruple mutant (2.2%) were found in proportions of < 10%. The 51I/59R/108N + 437A/540E quintuple mutant, which is associated with SP treatment failure in adults and children, was not detected.
hrp2/hrp3 genetic deletions
Genetic deletions in the hrp2 and hrp3 genes in the Togolese P. falciparum population were also sought, as there are two important factors responsible for the variable performance of malaria RDTs. For this analysis, 357 day 0 samples were tested. Only one isolate with hrp2 deletion and one with hrp3 deletion were found in Kouvé (0.3%) and Anié (0.3%), respectively. Dual hrp2/hrp3 deletions, which could potentially compromise the efficacy of HRP2-based RDTs, were not observed.
Discussion
This study shows that AL, the recommended first-line treatment in Togo, is achieving high cure rates (PCR-corrected cure rates of 97.8% in Kouvé and 98.7% in Anié on day 28 and 96.4% in Kouvé and 97.3% in Anié on day 42, respectively), eight years after the last clinical efficacy study, which was completed in 2013 [37]. The study also assessed, for the first time, the efficacy of DP, a second-line treatment introduced in 2016, and demonstrated high efficacy (PCR corrected cure rates of 100% in Kouvé and Anié on day 28 and 98.9% in Kouvé and 100% in Anié on day 42, respectively). These results are similar to those reported in neighboring countries such as Ghana [45] and Benin [46], but also as well as other West African countries [47,48,49,50,51,52,53,54], and Central and East African countries [55,56,57]. This contrasts with recent reports of the reduced PCR-corrected cure rates of AL (< 90%) found, in the absence of a Pfkelch13 validated variants, in Burkina Faso [58], Angola [59], and the Democratic Republic of Congo [60], suggesting lumefantrine resistance. In the Burkina Faso study, Rasmussen and Ringwald [61] noted some methodological deviations from the WHO standard procedure for assessing therapeutic efficacy on which the reported treatment outcome classifications are based. Similarly, studies in Angola and DRC used microsatellite-based PCR correction and Bayesian algorithm and not the WHO-recommended method for PCR correction [42]. The reported reduced efficacy of AL treatment is of great concern and calls for confirmatory studies in which lumefantrine blood levels are measured in addition to TES to ensure adequate blood levels of the drug [62]. In addition to parasite resistance, other factors affecting treatment outcomes, include suboptimal blood drug levels due to incorrect dosing, poor patient compliance, poor drug quality, and drug-drug interactions. Notable challenges include the difficulty of monitoring the second AL dose (evening) when patients are not hospitalized and the need for co-administration with fatty foods to improve lumefantrine absorption.
Currently, TES is the gold standard for monitoring anti-malarial drug efficacy and is the WHO standard on which the current treatment outcome grading and the 90% threshold for the treatment policy change are based [38]. TES is conducted in a controlled environment where drug administration is monitored, the results of microscopic examination of blood films are validated, and the origin and quality of drugs are verified. Therefore, adherence to the standard WHO-recommended protocol for monitoring the efficacy of first- and second-line treatments is critical to mitigate these patient-level cofactors of treatment response and to generate reliable data.
Molecular investigation of the Togolese isolates did not reveal any validated Pfkelch13 variant, suggesting a lack of artemisinin partial resistance. Only 2 isolates in Kouvé carried the A578S mutation, which is not known to confer resistance in vitro, and one isolate in Kouvé carried the A557S mutation, which is a non-validated Pfkelch13 mutation. Although the parasite densities found on day 3 were very low at all sites (ranging from 11 to 72 asexual parasites per microlitre), the parasite positivity rate at day 3 of up to 8.5% is of concern and require close monitoring as a positivity rate of more than 10% on day 3 after treatment initiation is a clinical surrogate marker for suspected artemisinin partial resistance [5]. This is particularly emphasized as recent reports of validated Pfkelch13 mutations with delayed parasite clearance after ACT treatment have been observed in Rwanda [10], and Uganda [11] and Eritrea [14] underlining the importance of continued monitoring of anti-malarial drug efficacy and resistance to artemisinins and partner drugs.
Analysis of the isolates to search for mutations in the Pfcrt gene showed that most of the parasites carried the Pfcrt wild-type allele (95.3% in Anié and 99.4% in Kouvé). The Pfcrt variant associated with resistance to chloroquine (CVIET) was detected in two isolates (one in Anié and one in Kouvé). This proportion is relatively low compared to other regions such as Democratic Republic of the Congo [63], Equatorial Guinea [64], and Liberia [54]. Notably, the 7G8 allele, which is predominant in South America, was detected in one isolate from Kouvé. For the Pfmdr-1 gene, the single 184F mutation, which has no clear impact on ACT drug efficacy, was highly prevalent in Togo (75.9%). This is usually reported in many African settings such as Ghana [65], Uganda [66], Madagascar [67], Tanzania [68], and Equatorial Guinea [69], Chad [44],
Molecular analysis looking for mutations in the dhfr gene revealed the virtual absence of the dhfr wild-type allele (0.3%, found in one isolate at Kouvé) contrasting with the near saturation of the N51I and the C59R mutations, with proportions estimated at 94.7% and 99.7%. However, the proportion of the S108N mutation was found at a lower frequency (76.5%) and varied significantly between sites (p < 10–6). For the dhps gene, the S436 mutation was dominant, reaching a mean of 50.1%. The other mutations were found in a proportion < 10%, except for the A613S mutation. Although, the complexity of infection was not estimated, the frequency of the dhfr/dhps haplotypes was inferred by combining the most predominant mutations found in the two dhfr/dhps loci. The most frequent dhfr/dhps haplotype was the 51I/59R/108N triple mutant (33.3%), followed by the 51I/59R/108N + 436A quadruple mutant (24.6%). Sulfadoxine/pyrimethamine is used for intermittent preventive treatment of malaria in pregnancy and in combination with amodiaquine in SMC to reduce the burden of malaria in the most vulnerable groups (pregnant women and children) in Togo, as recommended by the WHO [26, 27]. Mutations in the dhfr and dhps genes are markers of SP resistance, and quintuple dhfr/dhps mutations (N51I/C59R/S108N-A437G/K540E) have been associated with clinical treatment failure with SP [28, 29]. In addition, reduced efficacy of IPT-SP in infants and pregnant women has been observed in areas where parasites with the sextuple mutation (quintuple + 581G) are present [70, 71]. The absence of the quintuple mutation 51I/59R/108N + 437G/540E in the current study in Togo is encouraging and consistent with other West African countries where this mutation is absent or present at very low levels [54, 72,73,74,75,76,77,78], compared to the high frequency (> 70%) observed in East Africa [79,80,81,82,83]. Given the use of SP as part of chemoprevention strategies in Togo, the drug will continue to exert pressure on the parasites and therefore resistance markers of SP should be continuously monitored.
This study also provides, for the first time, an estimate of the proportion of hrp2, hrp3 and dual hrp2/3 gene deletions in Togo which could be used as baseline data for future surveys to determine the trend in the frequency of hrp2/3 gene deletions. Of the 357 isolates tested, only one isolate with an hrp2 deletion and one with an hrp3 deletion were found only in Kouvé. Dual hrp2/hrp3 deletions, which could compromise the efficacy of HRP2-based RDTs, were not observed [84, 85]. Similar to the proportions usually observed in African countries, this finding validates the continued used of HRP2-based RDTs in Togo.
Malaria is the leading cause of anemia in children under five living in areas of high transmission due to repeated malaria infections [86]. Nutritional deficiencies, helminth infections, and haemoglobinopathies also cause anemia in Africa [87, 88]. The results of the current study show a significant increase in Hb levels after treatment. In addition to prompt effective treatment to resolve the acute infections, prevention of repeated infections through chemoprevention and vector control measures (long-lasting insecticidal nets, insecticide residual spraying) is critical to control malaria-related anaemia [89].
Conclusion
The results of this study confirm that first-line (AL) and second line (DP) treatments are highly effective in treating uncomplicated falciparum infections, with a cure rate of over 96%. The absence of validated Pfkelch13 mutants in the study sites suggests the absence of ART-R. The absence of dhfr/dhps quintuple and quintuple + 581G sextuple mutations supports the continued use of SP for IPTp during pregnancy. However, routine monitoring of anti-malarial drug efficacy and resistance should continue in Togo to detect any changes in the susceptibility of the parasite populations.
Availability of data and materials
The dataset used in this study is available and can be shared upon reasonable request with NMCP through the corresponding author.
Abbreviations
- ACPR:
-
Adequate clinical and parasitological response
- ACTs:
-
Artemisinin-based combination therapies
- AL:
-
Artemether-lumefantrine
- SPAQ:
-
Sulfadoxine/pyrimethamine-amodiaquine
- ART-R:
-
Artemisinin resistance
- ASAQ:
-
Artesunate-amodiaquine
- ASMQ:
-
Artesunate-mefloquine
- ASPY:
-
Artesunate-pyronaridine
- ASSP:
-
Artesunate-sulfadoxine/pyrimethamine
- dhps :
-
dihydropteroate synthetase
- DP:
-
Dihydroartemisinin-piperaquine
- ETF:
-
Early treatment failure
- LCF:
-
Late clinical failure
- LPF:
-
Late parasitological failure
- msp1 :
-
Merozoite surface proteins 1
- msp2 :
-
Merozoite surface proteins 2
- glurp :
-
Glutamate rich-protein
- PCR:
-
Polymerase chain reaction
- dhfr :
-
Dihydrofolate reductase-thymidylate synthase
- Pfmdr-1:
-
Plasmodium falciparum multi drug resistance 1
- Pfkelch13:
-
Plasmodium falciparum kelch13
- SMC:
-
Seasonal malaria chemoprevention
- WHO:
-
World Health Organization
References
WHO. World Malaria Report 2022. Geneva: World Health Organization; 2022.
WHO. Guidelines for malaria. Geneva: World Health Organization; 2022.
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM. Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008;359:2619–20.
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, et al. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009;361:455–67.
WHO. Strategy to respond to antimalarial drug resistance in Africa. World Health Organization, 2022. https://www.who.int/publications/i/item/9789240060265 (Accessed on 15 Jan 2024).
Witkowski B, Amaratunga C, Khim N, Sreng S, Chim P, Kim S, et al. Novel phenotypic assays for the detection of artemisinin-resistant Plasmodium falciparum malaria in Cambodia: in-vitro and ex-vivo drug-response studies. Lancet Infect Dis. 2013;13:1043–9.
Ariey F, Witkowski B, Amaratunga C, Beghain J, Langlois AC, Khim N, et al. A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature. 2014;505:50–5.
van der Pluijm RW, Imwong M, Chau NH, Hoa NT, Thuy-Nhien NT, Thanh NV, et al. Determinants of dihydroartemisinin-piperaquine treatment failure in Plasmodium falciparum malaria in Cambodia, Thailand, and Vietnam: a prospective clinical, pharmacological, and genetic study. Lancet Infect Dis. 2019;19:952–61.
Straimer J, Gnädig NF, Witkowski B, Amaratunga C, Duru V, Ramadani AP, et al. Drug resistance. K13-propeller mutations confer artemisinin resistance in Plasmodium falciparum clinical isolates. Science. 2015;347:428–31.
Uwimana A, Umulisa N, Venkatesan M, Svigel SS, Zhou Z, Munyaneza T, et al. Association of Plasmodium falciparum kelch13 R561H genotypes with delayed parasite clearance in Rwanda: an open-label, single-arm, multicentre, therapeutic efficacy study. Lancet Infect Dis. 2021;21:1120–8.
Balikagala B, Fukuda N, Ikeda M, Katuro OT, Tachibana SI, Yamauchi M, et al. Evidence of artemisinin-resistant malaria in Africa. N Engl J Med. 2021;385:1163–71.
Fola AA, Feleke SM, Mohammed H, Brhane BG, Hennelly CM, Assefa A, et al. Plasmodium falciparum resistant to artemisinin and diagnostics have emerged in Ethiopia. Nat Microbiol. 2023;8:1911–9.
Mihreteab S, Platon L, Berhane A, Barbara H. Stokes BH, Warsame M, et al. Increasing prevalence of artemisinin-resistant HRP2-negative malaria in Eritrea. N Engl J Med. 2023;389:1191–202.
Adam M, Nahzat S, Kakar Q, Assada M, Witkowski B, Tag Eldin Elshafie A, et al. Antimalarial drug efficacy and resistance in malaria-endemic countries in HANMAT-PIAM_net countries of the Eastern Mediterranean Region 2016–2020: clinical and genetic studies. Trop Med Int Health. 2023;28:817–29.
Witkowski B, Duru V, Khim N, Ross LS, Saintpierre B, Beghain J, et al. A surrogate marker of piperaquine-resistant Plasmodium falciparum malaria: a phenotype-genotype association study. Lancet Infect Dis. 2017;17:174–83.
Price RN, Uhlemann AC, Brockman A, McGready R, Ashley E, Phaipun L, et al. Mefloquine resistance in Plasmodium falciparum and increased pfmdr1 gene copy number. Lancet. 2004;364:438–47.
Amato R, Lim P, Miotto O, Amaratunga C, Dek D, Pearson RD, et al. Genetic markers associated with dihydroartemisinin-piperaquine failure in Plasmodium falciparum malaria in Cambodia: a genotype-phenotype association study. Lancet Infect Dis. 2017;17:164–73.
Phyo AP, Ashley EA, Anderson TJC, Bozdech Z, Carrara VI, Sriprawat K, et al. Declining efficacy of artemisinin combination therapy against P. falciparum malaria on the Thai-Myanmar Border (2003–2013): the role of parasite genetic factors. Clin Infect Dis. 2016;63:
Amaratunga C, Lim P, Suon S, Sreng S, Mao S, Sopha C, et al. Dihydroartemisinin-piperaquine resistance in Plasmodium falciparum malaria in Cambodia: a multisite prospective cohort study. Lancet Infect Dis. 2016;16:357–65.
Thanh NV, Thuy-Nhien N, Tuyen NT, Tong NT, Nha-Ca NT, Dong LT, et al. Rapid decline in the susceptibility of Plasmodium falciparum to dihydroartemisinin-piperaquine in the south of Vietnam. Malar J. 2017;16:27.
Phuc BQ, Rasmussen C, Duong TT, Dong LT, Loi MA, Ménard D, et al. Treatment failure of dihydroartemisinin/piperaquine for Plasmodium falciparum malaria. Vietnam Emerg Infect Dis. 2017;23:715–7.
Carrara VI, Zwang J, Ashley EA, Price RN, Stepniewska K, Barends M, et al. Changes in the treatment responses to artesunate-mefloquine on the northwestern border of Thailand during 13 years of continuous deployment. PLoS ONE. 2009;4: e4551.
Rasmussen C, Alonso P, Ringwald P. Current and emerging strategies to combat antimalarial resistance. Expert Rev Anti Infect Ther. 2021;20:353–72.
Menard D, Dondorp A. Antimalarial drug resistance: a threat to malaria elimination. Cold Spring Harb Perspect Med. 2017;7: a025619.
Arya A, Kojom Foko LP, Chaudhry S, Sharma A, Singh V. Artemisinin-based combination therapy (ACT) and drug resistance molecular markers: A systematic review of clinical studies from two malaria endemic regions - India and sub-Saharan Africa. Int J Parasitol Drugs Drug Resist. 2021;15:43–56.
WHO. Policy brief for the implementation of intermittent preventive treatment of malaria in pregnancy using sulfadoxine-pyrimethamine (IPTp-SP). Geneva, World Health Organization, 2013. https://www.who.int/publications/i/item/WHO-HTM-GMP-2014.4 Accessed on 6 September 2023.
WHO. Policy recommendation: seasonal malaria chemoprevention (SMC) for Plasmodium falciparum malaria control in highly seasonal transmission areas of the Sahel sub-region in Africa. Geneva: World Health Organization; 2012. https://apps.who.int/iris/handle/10665/337978. Accessed on 6 September 2023.
Plowe CV. The evolution of drug-resistant malaria. Trans R Soc Trop Med Hyg. 2009;103(Suppl 1):S11–4.
Kublin JG, Dzinjalamala FK, Kamwendo DD, Malkin EM, Cortese JF, Martino LM, et al. Molecular markers for failure of sulfadoxinepyrimethamine and chlorproguanil-dapsone treatment of Plasmodium falciparum malaria. J Infect Dis. 2002;185:380–8.
Happi CT, Gbotosho GO, Folarin OA, Akinboye DO, Yusuf BO, Ebong OO, et al. Polymorphisms in Plasmodium falciparum Pfdhfr and Pfdhps genes and age related in vivo sulfadoxine-pyrimethamine resistance in malaria-infected patients from Nigeria. Acta Trop. 2005;95:183–93.
Harrington W, Mutabingwa T, Muehlenbachs A, Sorensen B, Bolla M, Fried M, et al. Competitive facilitation of drug-resistant Plasmodium falciparum malaria parasites in pregnant women who receive preventive treatment. Proc Natl Acad Sci USA. 2009;106:9027–32.
Chico RM, Cano J, Ariti C, Collier TJ, Chandramohan D, Roper C, et al. Influence of malaria transmission intensity and the 581G mutation on the efficacy of intermittent preventive treatment in pregnancy: systematic review and meta-analysis. Trop Med Int Health. 2015;20:1621–33.
Gosling RD, Gesase S, Mosha JF, Carneiro I, Hashim R, Lemnge M, et al. Protective efficacy and safety of three antimalarial regimens for intermittent preventive treatment for malaria in infants: a randomised, double- blind, placebo-controlled trial. Lancet. 2009;374:1521–32.
Ministère de la Santé, de l’Hygiène Publique et de l’Accès Universel aux Soins & Institut National de la Statistique et des Etudes Economiques et Démographiques. Enquête sur les indicateurs du paludisme au Togo (eipt) 2020. https://pnlptogo.org/page/enquete-sur-les-indicateurs-du-paludisme-au-togo-eipt-2020-38.
Dorkenoo MA, Barrette A, Agbo YM, Bogreau H, Kutoati S, Sodahlon YK, et al. Surveillance of the efficacy of artemether-lumefantrine and artesunate-amodiaquine for the treatment of uncomplicated Plasmodium falciparum among children under five in Togo, 2005–2009. Malar J. 2012;11:338.
Ministère de la santé et de la protection sociale du Togo, "Politique nationale de lutte contre le paludisme", aout 2016. https://pnlptogo.org/page/politique-nationale-de-lutte-contre-le-paludisme-40
Dorkenoo AM, Yehadji D, Agbo YM, Layibo Y, Agbeko F, Adjeloh P, et al. Therapeutic efficacy trial of artemisinin-based combination therapy for the treatment of uncomplicated malaria and investigation of mutations in k13 propeller domain in Togo, 2012–2013. Malar J. 2016;15:331.
WHO. Methods for Surveillance of Antimalarial Drug Efficacy. Geneva: World Health Organization; 2009. https://www.who.int/malaria/publications/atoz/9789241597531/en/
WHO. Severe Malaria. Trop Med Int Health. 2014;19 Suppl1:1–131.
Zainabadi K, Nyunt MM, Plowe CV. An improved nucleic acid extraction method from dried blood spots for amplification of Plasmodium falciparum kelch13 for detection of artemisinin resistance. Malar J. 2019;18:192.
WHO. Informal consultation on methodology to distinguish reinfection from recrudescence in high malaria transmission areas: report of a virtual meeting, 17–18 May 2021. Geneva: World Health Organization; 2021.
World Health Organization. Methods and techniques for clinical trials on antimalarial drug efficacy: genotyping to identify parasite populations: informal consultation organized by the Medicines for Malaria Venture and cosponsored by the World Health Organization, 29–31 May 2007, Amsterdam, The Netherlands. Geneva: World Health Organization; 2008. https://apps.who.int/iris/handle/10665/43824.
WHO. False-negative RDT results and implications of new reports of P. falciparum histidine-rich protein 2/3 gene deletions. Geneva: World Health Organization; 2017.
Issa MS, Warsame M, Mahamat MHT, Saleh IDM, Boulotigam K, Djimrassengar H, et al. Therapeutic efficacy of artesunate-amodiaquine and artemether-lumefantrine for the treatment of uncomplicated falciparum malaria in Chad: clinical and genetic surveillance. Malar J. 2023;22:240.
Abuaku B, Duah-Quashie NO, Quaye L, Matrevi SA, Quashie N, Gyasi A, et al. Therapeutic efficacy of artesunate-amodiaquine and artemether-lumefantrine combinations for uncomplicated malaria in 10 sentinel sites across Ghana: 2015–2017. Malar J. 2019;18:206.
Kpemasse A, Dagnon F, Saliou R, Yarou Maye AS, Affoukou CD, Zoulkaneri A, et al. Efficacy of artemether-lumefantrine for the treatment of Plasmodium falciparum malaria in Bohicon and Kandi, Republic of Benin, 2018–2019. Am J Trop Med Hyg. 2021;105:670–6.
Ebenebe JC, Ntadom G, Ambe J, Wammanda R, Jiya N, Finomo F, et al. Efficacy of Artemisinin-based combination treatments of uncomplicated falciparum malaria in under-five-year-old Nigerian children ten years following adoption as first-line antimalarials. Am J Trop Med Hyg. 2018;99:649–64.
Ibrahima I, Laminou IM, Adehossi E, Maman D, Boureima S, Harouna HK, et al. Étude de l’efficacité thérapeutique et de la tolérance de l’artéméther–luméfantrine et de l’artésunate–amodiaquine au Niger. Bull Soc Pathol Exot. 2020;113:17–23.
Smith SJ, Kamara ARY, Sahr F, Samai M, Swaray AS, Menard D, et al. Efficacy of artemisinin-based combination therapies and prevalence of molecular markers associated with artemisinin, piperaquine and sulfadoxine-pyrimethamine resistance in Sierra Leone. Acta Trop. 2018;185:363–70.
Konaté A, Barro-Kiki PCM, Angora KE, Bédia-Tanoh AV, Djohan V, Kassi KF, et al. Efficacy and tolerability of artesunate-amodiaquine versus artemether-lumefantrine in the treatment of uncomplicated Plasmodium falciparum malaria at two sentinel sites across Côte d’Ivoire. Ann Parasitol. 2018;64:49–57.
Beavogui AH, Camara A, Delamou A, Diallo MS, Doumbouya A, Kourouma K, et al. Efficacy and safety of artesunate-amodiaquine and artemether-lumefantrine and prevalence of molecular markers associated with resistance, Guinea: an open-label two-arm randomised controlled trial. Malar J. 2020;19:223.
Lingani M, Bonkian LN, Yerbanga I, Kazienga A, Valéa I, Sorgho H, et al. In vivo/ex vivo efficacy of artemether-lumefantrine and artesunate-amodiaquine as first-line treatment for uncomplicated falciparum malaria in children: an open label randomized controlled trial in Burkina Faso. Malar J. 2020;19:8.
Diallo MA, Yade MS, Ndiaye YD, Diallo I, Diongue K, Sy SA, et al. Efficacy and safety of artemisinin-based combination therapy and the implications of Pfkelch13 and Pfcoronin molecular markers in treatment failure in Senegal. Sci Rep. 2020;10:8907.
Koko VS, Warsame M, Vonhm B, Jeuronlon MK, Menard D, Ma L, et al. Artesunate-amodiaquine and artemether-lumefantrine for the treatment of uncomplicated falciparum malaria in Liberia: in vivo efficacy and frequency of molecular markers. Malar J. 2022;21:134.
Riloha Rivas M, Warsame M, Mbá Andeme R, Nsue Esidang S, Ncogo PR, Phiri WP, et al. Therapeutic efficacy of artesunate-amodiaquine and artemether-lumefantrine and polymorphism in Plasmodium falciparum kelch13-propeller gene in Equatorial Guinea. Malar J. 2021;20:275.
Niba PTN, Nji AM, Ali IM, Akam LF, Dongmo CH, Chedjou JPK, et al. Effectiveness and safety of artesunate-amodiaquine versus artemether-lumefantrine for home-based treatment of uncomplicated Plasmodium falciparum malaria among children 6–120 months in Yaoundé, Cameroon: a randomized trial. BMC Infect Dis. 2022;22:166.
Nambei WS, Biago U, Balizou O, Pounguinza S, Moyen M, Ndoua C, et al. Surveillance de l'efficacité d'artéméther-luméfantrine dans le traitement du paludisme simple à Plasmodium falciparum par étude des mutations des gènes kelch 13 à Bangui, République Centrafricaine. Med Trop Sante Int. 2021;1:mtsibulletin.n1.2021.82.
Gansané A, Moriarty LF, Ménard D, Yerbanga I, Ouedraogo E, Sondo P, et al. Anti-malarial efficacy and resistance monitoring of artemether-lumefantrine and dihydroartemisinin-piperaquine shows inadequate efficacy in children in Burkina Faso, 2017–2018. Malar J. 2021;20:48.
Dimbu PR, Horth R, Cândido ALM, Ferreira CM, Caquece F, Garcia LEA, et al. Continued low efficacy of artemether-lumefantrine in Angola in 2019. Antimicrob Agents Chemother. 2021;65:e01949-e2020.
Moriarty LF, Nkoli PM, Likwela JL, Mulopo PM, Sompwe EM, Rika JM, et al. Therapeutic efficacy of artemisinin-based combination therapies in Democratic Republic of the Congo and investigation of molecular markers of antimalarial resistance. Am J Trop Med Hyg. 2021;105:1067–75.
Rasmussen C, Ringwald P. Is there evidence of anti-malarial multidrug resistance in Burkina Faso? Malar J. 2021;20:320.
White NJ. Drug resistance in malaria. Br Med Bull. 1998;54:703–15.
Yobi DM, Kayiba NK, Mvumbi DM, Boreux R, Kabututu PZ, Akilimali PZ, et al. Biennial surveillance of Plasmodium falciparum anti-malarial drug resistance markers in Democratic Republic of Congo, 2017 and 2019. BMC Infect Dis. 2022;2:145.
Berzosa P, Molina de la Fuente I, Ta-Tang TH, González V, García L, Rodríguez-Galet A, et al. Temporal evolution of the resistance genotypes of Plasmodium falciparum in isolates from Equatorial Guinea during 20 years (1999 to 2019). Malar J. 2021;20:463.
Mensah BA, Aydemir O, Myers-Hansen JL, Opoku M, Hathaway NJ, Marsh PW, et al. Antimalarial drug resistance profiling of Plasmodium falciparum infections in Ghana using molecular inversion probes and next-generation sequencing. Antimicrob Agents Chemother. 2020;64:e01423-e1519.
Tumwebaze PK, Katairo T, Okitwi M, Byaruhanga O, Orena S, Asua V, et al. Drug susceptibility of Plasmodium falciparum in eastern Uganda: a longitudinal phenotypic and genotypic study. Lancet Microbe. 2021;2:e441–9.
Dentinger CM, Rakotomanga TA, Rakotondrandriana A, Rakotoarisoa A, Rason MA, Moriarty LF, et al. Efficacy of artesunate-amodiaquine and artemether-lumefantrine for uncomplicated Plasmodium falciparum malaria in Madagascar, 2018. Malar J. 2021;20:432.
Bwire GM, Ngasala B, Mikomangwa WP, Kilonzi M, Kamuhabwa AAR. Detection of mutations associated with artemisinin resistance at k13-propeller gene and a near complete return of chloroquine susceptible falciparum malaria in Southeast of Tanzania. Sci Rep. 2020;10:3500.
Liu Y, Liang X, Li J, Chen J, Huang H, Zheng Y, et al. Molecular surveillance of artemisinin-based combination therapies resistance in Plasmodium falciparum parasites from Bioko Island. Equatorial Guinea Microbiol Spectr. 2022;10: e0041322.
Braun V, Rempis E, Schnack A, Decker S, Rubaihayo J, Tumwesigye NM, et al. Lack of effect of intermittent preventive treatment for malaria in pregnancy and intense drug resistance in western Uganda. Malar J. 2015;14:372.
Gutman J, Kalilani L, Taylor S, Zhou Z, Wiegand RE, Thwai KL, et al. The A581G mutation in the gene encoding Plasmodium falciparum dihydropteroate synthetase reduces the effectiveness of sulfadoxine-pyrimethamine preventive therapy in Malawian pregnant women. J Infect Dis. 2015;211:1997–2005.
Souleymane IM, Toure OA, Mbanga D, Clément KH, Berenger AA, Baba C, et al. Prevalence of sulfadoxine–pyrimethamine resistance-associated mutations in Pfdhfr and Pfdhps gene of Plasmodium falciparum isolates collected in Pala west region of Chad. Afr J Parasitol Res. 2018;5:271–7.
Naidoo I, Roper C. Mapping “partially resistant”, “fully resistant”, and “super resistant” malaria. Trends Parasitol. 2013;29:505–15.
Dicko A, Sagara I, Djimdé AA, Touré SO, Traore M, Dama S, et al. Molecular markers of resistance to sulphadoxine-pyrimethamine one year after implementation of intermittent preventive treatment of malaria in infants in Mali. Malar J. 2010;9:9.
Afutu LL, Boampong JN, Quashie NB. High prevalence of molecular markers of Plasmodium falciparum resistance to sulphadoxine-pyrimethamine in parts of Ghana: a threat to IPTp-SP? J Trop Pediatr. 2021;67:fmaa120.
Das S, Kérah-Hinzoumbé C, Kebféné M, Srisutham S, Nagorngar TY, Saralamba N, et al. Molecular surveillance for operationally relevant genetic polymorphisms in Plasmodium falciparum in Southern Chad, 2016–2017. Malar J. 2022;21:83.
L’Episcopia M, Doderer-Lang C, Perrotti E, Priuli GB, Cavallari S, Guidetti C, et al. Polymorphism analysis of drug resistance markers in Plasmodium falciparum isolates from Benin. Acta Trop. 2023;245: 106975.
Tarama CW, Soré H, Siribié M, Débé S, Kinda R, Ganou A, et al. Plasmodium falciparum drug resistance-associated mutations in isolates fromDOIildren living in endemic areas of Burkina Faso. Malar J. 2023;22:213.
Tumwebaze P, Tukwasibwe S, Taylor A, Conrad M, Ruhamyankaka E, Asua V, et al. Changing antimalarial drug resistance patterns identified by surveillance at three sites in Uganda. J Infect Dis. 2017;215:631–5.
Asua V, Conrad MD, Aydemir O, Duvalsaint M, Legac J, Duarte E, et al. Changing prevalence of potential mediators of aminoquinoline, antifolate, and artemisinin resistance across Uganda. J Infect Dis. 2021;223:985–94.
Bwire GM, Mikomangwa WP, Kilonzi M. Occurrence of septuple and elevated Pfdhfr-Pfdhps quintuple mutations in a general population threatens the use of sulfadoxine-pyrimethamine for malaria prevention during pregnancy in eastern-coast of Tanzania. BMC Infect Dis. 2020;20:530.
Pacheco MA, Schneider KA, Cheng Q, Munde EO, Ndege C, Onyango C, et al. Changes in the frequencies of Plasmodium falciparum dhps and dhfr drug-resistant mutations in children from Western Kenya from 2005 to 2018: the rise of Pfdhps S436H. Malar J. 2020;19:378.
Gikunju SW, Agola EL, Ondondo RO, Kinyua J, Kimani F, LaBeaud AD, et al. Prevalence of pfdhfr and Pfdhps mutations in Plasmodium falciparum associated with drug resistance among pregnant women receiving IPTp-SP at Msambweni County Referral Hospital, Kwale County. Kenya Malar J. 2020;19:190.
Alemayehu GS, Blackburn K, Lopez K, Cambel Dieng C, Lo E, Janies D, Golassa L. Detection of high prevalence of Plasmodium falciparum histidine-rich protein 2/3 gene deletions in Assosa zone, Ethiopia: implication for malaria diagnosis. Malar J. 2021;20:109.
Golassa L, Messele A, Amambua-Ngwa A, Swedberg G. High prevalence and extended deletions in Plasmodium falciparum hrp2/3 genomic loci in Ethiopia. PLoS ONE. 2020;15: e0241807.
Menendez C, Fleming AF, Alonso PL. Malaria-related anaemia. Parasitol Today. 2000;16:469–76.
Stoltzfus RJ, Chwaya HM, Montresor A, Albonico M, Savioli L, Tielsch JM. Malaria, hookworms and recent fever are related to anemia and iron status indicators in 0- to 5-y old Zanzibari children and these relationships change with age. J Nutr. 2000;130:1724–33.
Nussenblatt V, Semba RD. Micronutrient malnutrition and the pathogenesis of malarial anemia. Acta Trop. 2002;82:321–37.
Björkman A. Malaria associated anaemia, drug resistance and antimalarial combination therapy. Int J Parasitol. 2002;32:1637–43.
Acknowledgements
The authors thank the parents or guardians of the children who participated in the study and the health workers at the study health facilities for their support in conducting the study. We also thank Dr. Pascal Ringwald for providing the technical guidance. The study was made possible by the Global Fund to Fight HIV/AIDS, TB, and Malaria (GFATM) for financial support at the country level, and the Bill and Melinda Gates Foundation for their financial support through the World Health Organization in Geneva. The authors would like to thank, the Ministry of Health (Togo), the University of Lomé (Togo), M. T. Tchadjobo (NMCP-Togo), Dr M. Davi (WHO- Togo) and staff members of the sentinel sites: Drs E. Folikoue and K Akpindi and their team (La Providence Hospital, Kouvé); Dr K Blu and his team (District hospital, Anié), Dr P. Assih (Health District of Yoto), Dr. A. Lambonkale (Maritime’s Health Region), and Dr. D. Nyametso (Plateaux’s Health Region).
Funding
This study was financed by the Global Fund to Fight HIV/AIDS, TB, and Malaria (GFATM) at the country level, and by the Bill and Melinda Gates Foundation support through the World Health Organization in Geneva. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The views expressed in this publication are those of the authors and not necessarily those of the funding organizations.
Author information
Authors and Affiliations
Contributions
AMD conceived the study design, revised the protocol, led training of local teams, and provided critical input to the manuscript. MW contributed to data analysis and led preparation of the manuscript with support from the other co-authors. EA prepared the protocol, guided data collection and data entry, and participated in parasite genotyping and drug resistance marker analysis. MH and KED supervised on-site clinical activities, managed clinical data quality control, and performed data cleaning. KY and ES supervised laboratory activities and blood slide quality control. MM tracked the pharmacovigilance aspects of the study. CDT participated in field laboratory activities and parasite genotyping analysis. TAO coordinated study implementation on the sites. CR provided technical input and validated the final version of the protocol. EC, LM and DM led the parasite genotyping and drug resistance marker analysis and DM contributed to the preparation of the manuscript. All authors read and approved the final version of the manuscript. Charlotte Rasmussen is an employee of the World Health Organization, and note that the views expressed in this publication do not necessarily represent the decisions, policy, or views of the World Health Organization.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the Ministry of Health, Public Hygiene, and Universal Health Coverage. Written informed consent was obtained from the adult patients, parents, or guardians of the children before enrollment in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Raw data of msp-1, msp-2, glurp and poly α polymorphisms (band size in bp) detected on day0 and day of recurrence (dayX) in isolates from recurrent infections, Togo, 2021-2022.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dorkenoo, A.M., Warsame, M., Ataba, E. et al. Efficacy of artemether-lumefantrine and dihydroartemisinin-piperaquine and prevalence of molecular markers of anti-malarial drug resistance in children in Togo in 2021. Malar J 23, 92 (2024). https://doi.org/10.1186/s12936-024-04922-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-024-04922-1