Abstract
Background
To evaluate the effects of acute hyperventilation on the central venous-to-arterial carbon dioxide tension difference (∆PCO2) in hemodynamically stable septic shock patients.
Methods
Eighteen mechanically ventilated septic shock patients were prospectively included in the study. We measured cardiac index (CI), ∆PCO2, oxygen consumption (VO2), central venous oxygen saturation (ScvO2), and blood gas parameters, before and 30 min after an increase in alveolar ventilation (increased respiratory rate by 10 breaths/min).
Results
Arterial pH increased significantly (from 7.35 ± 0.07 to 7.42 ± 0.09, p < 0.001) and arterial carbon dioxide tension decreased significantly (from 44.5 [41–48] to 34 [30–38] mmHg, p < 0.001) when respiratory rate was increased. A statistically significant increase in VO2 (from 93 [76–105] to 112 [95–134] mL/min/m2, p = 0.002) was observed in parallel with the increase in alveolar ventilation. While CI remained unchanged, acute hyperventilation led to a significant increase in ∆PCO2 (from 4.7 ± 1.0 to 7.0 ± 2.6 mmHg, p < 0.001) and a significant decrease in ScvO2 (from 73 ± 6 to 67 ± 8%, p < 0.001). A good correlation was found between changes in arterial pH and changes in VO2 (r = 0.67, p = 0.002). Interestingly, we found a strong association between the increase in VO2 and the increase in ∆PCO2 (r = 0.70, p = 0.001).
Conclusions
Acute hyperventilation provoked a significant increase in ∆PCO2, which was the result of a significant increase in VO2 induced by hyperventilation. The clinician should be aware of the effects of acute elevation of alveolar ventilation on ∆PCO2.
Similar content being viewed by others
Background
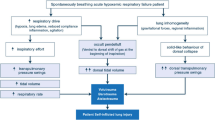
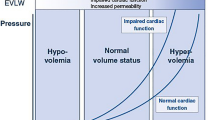
Awareness that tissue hypoperfusion is a key factor in the pathogenesis of the multiple organ failures has focused the attention on surrogate indicators of tissue perfusion in the critically ill patient [1, 2]. In this context, venous-to-arterial carbon dioxide tension difference (∆PCO2) has been proposed as a marker of tissue hypoperfusion in patients with septic shock [3–9]. In fact, the increase in ∆PCO2 that has been observed in low-flow states is mainly related to venous hypercapnia, rather than a decrease in arterial CO2 partial pressure (PaCO2), which can be explained by the tissue CO2 stagnation phenomenon. Indeed, due to the decrease in transit time, there is a higher than usual addition of CO2 per unit of blood passing the efferent microvessels, which leads to a rise in CO2 partial pressure in the venous blood (PvCO2) [10–12].
The reason for the preferred use of ∆PCO2 over PvCO2 as a marker of global tissue perfusion is that ∆PCO2 was found to be less influenced by changes in PaCO2 than PvCO2 [13–15]. However, acute changes in PaCO2 or arterial pH might have direct effects on microvascular tone and/or might induce variations in systemic oxygen consumption [15–18], and could then affect ∆PCO2. Recently, in healthy volunteers, acute hyperventilation was shown to be associated with an increase in the peripheral venous-to-arterial CO2 difference due to a reduction in peripheral blood flow induced by acute hypocapnia [19, 20]. Furthermore, Morel et al. [21] found, in a small study that included mechanically ventilated postoperative patients, that acute decreases in PaCO2 resulted in significant increases in ∆PCO2 without any change in cardiac output. Therefore, it is not clear so far what the impact of the rapid decrease in PaCO2 on ∆PCO2 is. This question is important because if PaCO2 or arterial pH fluctuations could influence ∆PCO2, this effect will have to be taken into account by the physician when interpreting ∆PCO2 at the bedside. The aim of this study was to investigate the impact of acute hyperventilation on ∆PCO2 in mechanically ventilated and hemodynamically stable septic shock patients.
Methods
This prospective and observational study was conducted in a single general adult intensive care unit (ICU). The study was approved by our local institutional ethics committee (Comité d’éthique du Centre Hospitalier du Dr. Shaffner de Lens, France). Informed consent was obtained from each subject’s next of kin.
Patients
The study included mechanically ventilated and hemodynamically stable septic shock patients. The diagnosis of septic shock was defined according to the criteria of the American College of Chest Physicians (ACCP)/Society of Critical Care Medicine (SCCM) Consensus Conference [22]. All patients had to be monitored by a transpulmonary thermodilution device (PiCCO, Pulsion Medical System, Munich, Germany) as part of routine management of septic shock in our ICU.
To avoid spontaneous breathing activity, patients remained sedated throughout the study via continuous infusions of propofol and remifentanil. Patients were ventilated in the control volume mode.
Exclusion criteria were pregnancy, age less than 18 years old, unstable hemodynamic condition (change in vasoactive drug dosage or fluid administration within 1 h preceding the protocol), high blood lactate levels (>2 mmol/L), and uncontrolled tachyarrhythmias (heart rate 140 beats/min).
Measurements
Demographic data, septic shock etiology, the Simplified Acute Physiology Score (SAPS) II, and the Sequential Organ Failure Assessment (SOFA) scores were obtained on the day of enrollment.
Cardiac index (CI) was obtained with the PiCCO monitor by triplicate central venous injections, in either the internal jugular or subclavian vein, of 20 mL of iced 0.9% saline solution and recorded as the average of the three measurements. In cases where the discrepancy in CI measurements was >10%, the measurement was repeated two more times (five times in total) with elimination of the highest and the lowest results.
Arterial and central venous blood gases analysis and arterial lactate levels were measured using the GEM Premier 4000 (Instrumentation Laboratory Co, Paris, France). To ensure accurate measurement, the blood gas analyzer was calibrated several times a day. Central venous blood was obtained from a central venous catheter with the tip confirmed to be in the superior vena cava at the entrance, or in the right atrium, by X-ray. ∆PCO2 was calculated as the difference between central venous carbon dioxide tension (PcvCO2) and arterial carbon dioxide tension (PaCO2). Arterial oxygen content was calculated as CaO2 (mL) = 1.34 × Hb (g/dL) × SaO2 + 0.003 × PaO2 (mmHg), where SaO2 is the oxygen saturation of arterial blood, Hb the hemoglobin concentration, and PaO2 the arterial oxygen tension. Central venous oxygen content was calculated as CcvO2 (mL) = 1.34 × Hb (g/dL) × ScvO2 + 0.003 × PcvO2 (mmHg), where PcvO2 is the central venous oxygen tension and ScvO2 the central venous oxygen saturation. DO2 was calculated by using the formula: DO2 (mL/min/m2) = CaO2 × CI × 10. VO2 was calculated using the following formula: VO2 (mL/m2) = CI × (CaO2 − CcvO2) × 10. Oxygen extraction was defined as: OE = VO2/DO2.
Heart rate (HR), mean arterial pressure (MAP), minute ventilation, respiratory rate, body temperature, and fractional inspired oxygen level were also recorded.
Study protocol
Patients were in steady state defined as less than 10% variation in HR, MAP, CI, and SaO2 over a 60-min period before baseline measurements were initiated. Each patient was quiet and well adapted to the respirator. Fluid, doses of the vasopressor, and sedation drugs were kept constant in the hour preceding the measurements and throughout the study period. Variations in body temperature must have been <±0.5 °C. Enteral and/or parenteral nutrition were continued and remained unchanged during the data collection period.
At baseline, a first set of measurements was performed, including hemodynamic and tissue oxygenation variables (HR, MAP, CI, VO2, ScvO2), arterial lactate level, ∆PCO2, respiratory rate, and minute ventilation. Alveolar ventilation was then increased by raising the respiratory rate by 10 breaths/min (hyperventilation period). The inspiratory time was decreased to avoid the generation of an intrinsic positive end-expiratory pressure (PEEP) and to keep the level of plateau pressure constant throughout the study period. Also, the external PEEP remained unchanged. After 30 min of stabilization, a second set of measurement was recorded, including the same hemodynamic, respiratory, and tissue oxygenation variables (Additional file 1).
Changes in variables induced by the increase in alveolar ventilation were expressed as relative changes: [(variable after − variable before)/variable before] × 100.
Statistical analysis
Data are presented as mean ± SD or as median (25–75%, interquartile range). Normality was evaluated using the Shapiro–Wilk test. Comparisons of variables between before versus after increase in alveolar ventilation were assessed using Student’s paired t test or Wilcoxon test, as appropriate. Linear correlations were tested using the Pearson or the Spearman test, as appropriate. The McNemar’s test was used to compare two paired proportions.
In a previous study [23], we found that the smallest detectable difference for ∆PCO2 was 2.0 mmHg. The smallest detectable difference is the minimum change (in absolute value) that needs to be measured by a laboratory analyzer in order to recognize a real change in measurement. Thus, for a power of 90% and α risk of 0.05, a sample size of 17 was required to detect a mean difference of 2.0 mmHg in ∆PCO2 with a standard deviation of 2.35 mmHg [23].
Statistical analysis was performed using STATA 14.0 (StataCorp LP, College Station, Texas, USA). p < 0.05 was considered statistically significant. All reported p values are 2-sided.
Results
Eighteen septic shock patients were prospectively included in this study. Basic characteristics of the cohort are presented in Table 1. The principal source of infection was pneumonia (61%) with ICU mortality rate of 39%. All patients were sedated, mechanically ventilated without spontaneous breathing, and hemodynamically stable at their inclusions. No changes in vasopressor therapy and sedation level occurred during the observation period.
Effect of acute hyperventilation on blood gases, metabolic, and hemodynamic variables
Acute hyperventilation induced a significant increase in arterial pH and a significant decrease in PaCO2 (Table 2). Changes in arterial pH and PaCO2 were paralleled by a statistically significant increase in VO2 (Table 2). Cardiac index, heart rate, and DO2 remained unaffected.
Acute hyperventilation led to a significant increase in ∆PCO2, which resulted in a significant decrease in the number of patients with normal ∆PCO2 value (∆PCO2 ≤ 6 mmHg) (Table 2). Furthermore, we observed a significant reduction in ScvO2 in parallel to the increase in alveolar ventilation. Interestingly, lactate levels significantly increased when minute ventilation was increased (Table 2). Abrupt elevation of alveolar ventilation was also associated with a significant increase in systemic vascular resistance index (Table 2).
Correlation analysis
We found a good correlation between the increase in arterial pH induced by hyperventilation and the increase in VO2 (r = 0.67, p = 0.002) (Fig. 1). Changes in PaCO2 and VO2 were also moderately correlated (r = −0.54, p = 0.02).
The increase in ∆PCO2 observed after the elevation of alveolar ventilation was strongly associated with the increase in VO2 (r = 0.70, p = 0.001) (Fig. 2a). Also, a strong relationship was found between the increase in VO2 induced by hyperventilation and the decrease in ScvO2 (r = −0.83, p < 0.001) (Fig. 2b).
We found that the increase in lactate levels after the acute increase in alveolar ventilation significantly correlated with the increase in VO2 (r = 0.54, p = 0.02).
Hyperventilation-induced increase in systemic vascular resistance index did not correlate with the change in ∆PCO2 (r = −0.20, p = 0.41), or the change in ScvO2 (r = −0.13, p = 0.62).
Discussion
The main findings of our study were as follows: (1) acute increase in alveolar ventilation resulted in a significant increase in ∆PCO2 accompanied with a significant decrease in ScvO2; (2) these changes were linked to a significant increase in oxygen consumption induced by acute hyperventilation.
Early identification and treatment of tissue hypoperfusion are critical factors in the management of septic shock patients. In this regard, ∆PCO2 has been considered as a marker that reflects the adequacy of tissue perfusion in septic shock states [3–9]. Increased ∆PCO2 is associated with venous hypercapnia, which is explained by the low-flow-induced CO2 stagnation phenomenon [11, 12]. Venous hypercapnia results from insufficient elimination of the CO2 produced by peripheral tissues, secondary to reductions in systemic and microcirculatory blood flow. However, under spontaneous breathing, hyperventilation may decrease PaCO2 and thus may preclude the CO2 stagnation-induced increase in PvCO2 [24]. Because alveolar hyperventilation would decrease both arterial and venous PCO2 without eliminating the increased venous-to-arterial PCO2 gap, it is recommended to assess ∆PCO2 rather than only monitor PvCO2 as a global marker of tissue perfusion [25].
However, a few studies have assessed the effects of acute hyperventilation on ∆PCO2 in critically ill patients [13, 14, 21]. We found that the acute increase in alveolar ventilation led to a significant increase in ∆PCO2 with an amplitude (2.2 mmHg) that was larger than its smallest detectable difference (2.0 mmHg) [23]. In addition, when the changes in ∆PCO2 are expressed as relative changes, acute hyperventilation induced a significant increase in ∆PCO2 with a magnitude (48.5%) that was also greater than its least significant change (32.4%) [23], which is the minimum change that needs to be measured by a laboratory analyzer in order to recognize a real change in measurement. In other words, the observed increase in ∆PCO2 can be considered as a true change and was not due to a random variation. Our findings are in agreement with the results of Morel et al. [21]. Indeed, these authors studied the effects of an acute decrease in PaCO2, obtained by increasing the respiratory rate, on ∆PCO2 in mechanically ventilated post-cardiac surgery patients. They found that acute hyperventilation provoked a significant increase in ∆PCO2 (from 4.2 ± 1.8 to 7.6 ± 1.7 mmHg), while the cardiac index was unaffected. In that study [21], ScvO2 also decreased in parallel with the increase in alveolar ventilation. Furthermore, in an animal study [16], the gradient between gastric mucosal PCO2 and PaCO2 (indicator of gut perfusion), obtained with gastric tonometry, increased significantly after hyperventilation. However, our results disagree with those of a previous study [13] that found no impact of hyperventilation on mixed venous-to-arterial PCO2 difference in mechanically ventilated patients. In that study, the increase in alveolar ventilation was obtained very progressively by increasing the tidal volume from 7 to 10 mL/kg over a period of 3 h, which might explain the absence of changes in mixed venous-to-arterial PCO2 difference. Also, the mean cardiac index at baseline was high (4.55 ± 0.90 mL/min/m2), which would have prevented any increase in mixed venous-to-arterial PCO2 difference by washing out any addition of CO2 from the peripheral circulation.
Several mechanisms can be suggested to explain the increase in ∆PCO2 observed in our study. A first potential explanation is that acute hyperventilation provoked the increase in systemic oxygen consumption and therefore CO2 production. Thus, for a given venous blood flow, the increase in tissue CO2 production should lessen the decrease in PcvCO2 (induced by hyperventilation) relatively to the decrease in PaCO2, leading to a rise in ∆PCO2. We believe that such a mechanism may have contributed to the increase in ∆PCO2 after acute hyperventilation in our study. Indeed, we observed a strong correlation between the increases in VO2 between before and after hyperventilation and the increases in ∆PCO2 (Fig. 2a). Also, the magnitude of the decrease in PcvCO2 after hyperventilation was significantly less than the decrease in PaCO2 (−16.5 ± 4.8 vs. −22.7 ± 5.5%, p < 0.001, respectively), explaining the observed increase in ∆PCO2. Similarly, the reduction in ScvO2 found after hyperventilation can be explained by the increase in VO2. It is unlikely that the increase in VO2 with hyperventilation was a result of an unstable state because of the lack of hemodynamic and temperature differences (Table 2), and the absence of changes in vasopressor and sedation drugs during the study period. We think that the observed increase in VO2 was induced by acute hyperventilation since we found a good association between changes in pH and changes in VO2 (Fig. 1). Acute respiratory alkalosis has been found, in some experiments in animals and humans, to increase VO2 and CO2 production independently of any significant hemodynamic changes [17, 18, 26, 27]. Indeed, hyperventilation alkalosis, in mechanically ventilated dogs, increased VO2 by 10–25% [17, 18]. In anesthetized paralyzed patients, contradictory findings were observed with some authors reporting a significant increase in whole-body VO2 [27], whereas others failed to demonstrate any significant variation [14]. Recently, Morel et al. [20], reported a twofold increase in VO2 in healthy volunteers with hypocapnic condition compared to hypercapnic condition for the same minute volume, suggesting a possible contribution of this mechanism to the observed increase in peripheral venous-to-arterial CO2 difference after induced acute respiratory alkalosis. The mechanism by which an acute respiratory alkalosis stimulates oxygen consumption is unclear and may involve many intracellular processes. A decrease in intracellular hydrogen ion concentration may stimulate the activity of phosphofructokinase, a key enzyme in the glycolytic cycle, which could result in increased intracellular adenosine triphosphate (ATP) hydrolysis and increased VO2 [28, 29]. Interestingly, we found a significant increase in lactate level induced by acute hyperventilation (Table 2). This finding could be an indirect marker supporting the activation of the phosphofructokinase enzyme and the increased rate of glycolysis in our study. Indeed, several studies reported increased lactate production with alkalosis [30, 31], reflecting increased glycolysis.
A second possibility is that acute hypocapnia resulted in systemic vasoconstriction, thus decreasing the elimination of the total CO2 produced by the peripheral tissues, and increasing the ∆PCO2. It has been shown that acute hypocapnia induces vasoconstrictive responses in various organs [14, 32, 33]. In healthy volunteers, Umeda et al. [19] observed that acute hyperventilation decreased both the minimal and mean flow velocity in the radial artery assessed by Doppler echography. The authors concluded that the decrease in mean blood flow, which was the result of increased vascular tone induced by hyperventilation, was responsible for the rise in peripheral venous-to-arterial CO2 difference that they observed after acute hyperventilation. Similarly, Morel et al. [20] found a significant drop in the skin microcirculatory blood flow of healthy volunteers, evaluated with in vivo reflectance confocal microscopy, secondary to acute hypocapnia. In our study, we observed a significant increase in systemic vascular resistance in parallel with the elevation of alveolar ventilation (Table 2). Nevertheless, changes in systemic vascular resistance were not significantly correlated with changes in ∆PCO2 nor with changes in ScvO2, which suggests, indirectly, a minimal participation of this mechanism to the increase in ∆PCO2. However, since we did not specifically evaluate the microcirculation we cannot eliminate or confirm the contribution of the vasoconstrictive mechanism to the observed increase in ∆PCO2 secondary to acute hyperventilation.
A third possibility of the increase in ∆PCO2 is that acute hyperventilation could induce variations in the PCO2/CO2 content relationship. This mechanism is, however, unlikely to have occurred in our patients. Indeed, the relationship between CO2 content and PCO2, which is curvilinear rather than linear, is influenced by many factors such as the degree of metabolic acidosis, the hematocrit, and the oxygen saturation (Haldane effect) [12, 34]. Our patients did not have metabolic acidosis, and acute hyperventilation did not change the base excess meaningfully (Table 2). Although venous oxygen saturation decreased significantly after acute hyperventilation, it is unlikely that this change could have affected the PCO2/CO2 content relationship, because first, it was not large; in this extent as stressed by Jakob et al. [35], changes in ∆PCO2 might not parallel changes in CO2 content differences under conditions of very low values of venous oxygen saturation (<30%), which was not the case in our patients. Second, if Haldane effect had affected the PCO2/CO2 content relationship, it would have resulted in a decrease in ∆PCO2, rather than an increase in ∆PCO2 [36].
Our results are of clinical importance. Indeed, changes in ventilator settings are regularly needed in mechanically ventilated patients. Since ∆PCO2 is now widely recognized as a valuable marker to evaluate tissue perfusion in septic shock, a clinician should be aware that acute changes in pH or PaCO2 induced by hyperventilation could impact ∆PCO2 independently of changes in tissue perfusion. These findings should not dismiss the clinical value of ∆PCO2 as a marker to detect tissue perfusion derangements. On the contrary, our results highlighted the usefulness of ∆PCO2, as an index of VCO2/cardiac output ratio, to detect the imbalance between the relative increase in VCO2 and the blood flow, whatever the mechanism of this imbalance is (increases in oxygen consumption [37, 38] or tissue hypoperfusion [9]).
We acknowledge some limitations to our study. First, the number of patients studied was small, but the study was sufficiently powered to detect a real change in ∆PCO2 induced by hyperventilation. Second, the study was performed in a sample of septic shock patients from a single center, potentially limiting the generalizability of the results. However, our results confirm those of a previous study performed in a different patient population (post-cardiovascular surgery patients) [21]. Third, VO2 was calculated from central venous oxygen saturation and not from mixed venous oxygen saturation or measured by indirect calorimetry, what might limit its accuracy. However, in our study, we were interested in investigating the changes in VO2 induced by acute hyperventilation rather than by its absolute value. Furthermore, it has recently been demonstrated that calculating the oxygen-derived variables from the central venous blood allowed the detection of global tissue hypoxia in critically ill patients [39, 40]. Finally, we did not evaluate the microcirculation, and thus, we were incapable of drawing any conclusions about the effects of acute hyperventilation on the local vascular tone and its relationship to ∆PCO2.
Conclusion
In stable septic shock patients, acute hyperventilation leads to a significant increase in ∆PCO2, which is associated with an increase in VO2, also induced by hyperventilation. Microcirculatory dysfunction is a key pathological mechanism involved in septic shock patients and could, also, be exacerbated by acute changes in alveolar ventilation. This finding should be taken into account when interpreting ∆PCO2 at the bedside. Further studies are needed to investigate the effects of acute hyperventilation on systemic oxygen consumption and local vascular tone.
Abbreviations
- CI:
-
cardiac index
- DO2 :
-
oxygen delivery
- VO2 :
-
oxygen consumption
- ScvO2 :
-
central venous oxygen saturation
- ∆PCO2 :
-
central venous-to-arterial carbon dioxide tension difference
- CaO2 :
-
oxygen content
- CcvO2 :
-
central venous oxygen content
- PaCO2 :
-
arterial carbon dioxide tension
- PcvCO2 :
-
central venous carbon dioxide tension
- SaO2 :
-
arterial oxygen saturation
- HR:
-
heart rate
- MAP:
-
mean arterial pressure
- Hb:
-
hemoglobin
- ICU:
-
intensive care unit
- PEEP:
-
end-expiratory pressure
- OE:
-
oxygen extraction
References
Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369:1726–34.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40:1795–815.
Bakker J, Vincent JL, Gris P, Leon M, Coffernils M, Kahn RJ. Veno-arterial carbon dioxide gradient in human septic shock. Chest. 1992;101:509–15.
Valleé F, Vallet B, Mathe O, Parraguette J, Mari A, Silva S, et al. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intensive Care Med. 2008;34:2218–25.
Mallat J, Pepy F, Lemyze M, Gasan G, Vangrunderbeeck N, Tronchon L, et al. Central venous-to-arterial carbon dioxide partial pressure difference in early resuscitation from septic shock: a prospective observational study. Eur J Anaesthesiol. 2014;31(7):371–80.
van Beest PA, Lont MC, Holman ND, Loef B, Kuiper MA, Boerma EC. Central venous–arterial PCO2 difference as a tool in resuscitation of septic patients. Intensive Care Med. 2013;39:1034–9.
Vallet B, Pinsky MR, Cecconi M. Resuscitation of patients with septic shock: please ‘‘mind the gap’’! Intensive Care Med. 2013;39:1653–5.
Ospina-Tascón GA, Bautista-Rincón DF, Umaña M, Tafur JD, Gutiérrez A, García AF, et al. Persistently high venous-to-arterial carbon dioxide differences during early resuscitation are associated with poor outcomes in septic shock. Crit Care. 2013;17:R294.
Ospina-Tascón GA, Umaña M, Bermúdez WF, Bautista-Rincón DF, Valencia JD, Madriñán HJ, et al. Can venous-to-arterial carbon dioxide differences reflect microcirculatory alterations in patients with septic shock? Intensive Care Med. 2016;42:211–21.
Vallet B, Teboul JL, Cain S, Curtis S. Venoarterial CO(2) difference during regional ischemic or hypoxic hypoxia. J Appl Physiol. 2000;89:1317–21.
Groeneveld AB. Interpreting the venous–arterial PCO2 difference. Crit Care Med. 1998;26:979–80.
Lamia B, Monnet X, Teboul JL. Meaning of arterio–venous PCO2 difference in circulatory shock. Minerva Anestesiol. 2006;72:597–604.
Bernardin G, Lucas P, Hyvernat H, Deloffre P, Mattéi M. Influence of alveolar ventilation changes on calculated gastric intramucosal pH and gastric-arterial PCO2 difference. Intensive Care Med. 1999;25:269–73.
Mas A, Saura P, Joseph D, Blanch L, Baigorri F, Artigas A, et al. Effect of acute moderate changes in PaCO2 on global hemodynamics and gastric perfusion. Crit Care Med. 2000;28:360–5.
Pernat A, Weil MH, Tang W, Yamaguchi H, Pernat AM, Sun S, et al. Effects of hyper- and hypoventilation on gastric and sublingual PCO2. J Appl Physiol. 1999;87:933–7.
Guzman JA, Kruse JA. Gut mucosal–arterial pCO2 gradient as an indicator of splanchnic perfusion during systemic hypo- and hypercapnia. Crit Care Med. 1999;27:2760–5.
Khambatta HJ, Sullivan SF. Effects of respiratory alkalosis on oxygen consumption and oxygenation. Anesthesiology. 1973;38:53–8.
Cain SM. Increased oxygen uptake with passive hyperventilation of dogs. J Appl Physiol. 1970;28:4–7.
Umeda A, Kawasaki K, Abe T, Watanabe M, Ishizaka A, Okada Y. Hyperventilation and finger exercise increase venous–arterial PCO2 and pH differences. Am J Emerg Med. 2008;26:975–80.
Morel J, Gergelé L, Dominé A, Molliex S, Perrot JL, Labeille B, et al. The venous–arterial difference in CO2 should be interpreted with caution in case of respiratory alkalosis in healthy volunteers. J Clin Monit Comput. 2016. doi:10.1007/s10877-016-9897-6.
Morel J, Gergele L, Verveche D, Costes F, Auboyer C, Molliex S. Do fluctuations of PaCO2 impact on the venous–arterial carbon dioxide gradient? Crit Care. 2011;15:456.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definition conference. Crit Care Med. 2003;31:1250–6.
Mallat J, Lazkani A, Lemyze M, Pepy F, Meddour M, Gasan G, et al. Repeatability of blood gas parameters, PCO2 gap, and PCO2 gap to arterial-to-venous oxygen content difference in critically ill adult patients. Medicine. 2015;943:e415.
Rackow EC, Astiz ME, Mecher CE, Weil MH. Increased venous–arterial carbon dioxide tension difference during severe sepsis in rats. Crit Care Med. 1994;22:121–5.
Benjamin E. Venous hypercarbia: a nonspecific marker of hypoperfusion. Crit Care Med. 1994;22:9–10.
Karetzky MS, Cain SM. Effect of carbon dioxide on oxygen uptake during hyperventilation in normal man. J Appl Physiol. 1970;28:8–12.
Slater RM, Symreng T, Ping ST, Starr J, Tatman D. The effect of respiratory alkalosis on oxygen consumption in anesthetized patients. J Clin Anesth. 1992;4:462–7.
Theye RA, Gronert GA, Heffron JJ. Oxygen uptake of canine whole body and hind limb with hypocapnic alkalosis. Anesthesiology. 1977;47:416–22.
Dobson GP, Yamamoto E, Hochachka PW. Phosphofructokinase control in muscle: nature and reversal of pH-dependent ATP inhibition. Am J Physiol. 1986;250:71–6.
Davies SF, Iber C, Keene SA, McArthur CD, Path MJ. Effect of respiratory alkalosis during exercise on blood lactate. J Appl Physiol. 1986;61:948–52.
Plum F, Posner JB. Blood and cerebrospinal fluid lactate during hyperventilation. Am J Physiol. 1967;212:864–70.
Richardson DW, Kontos HA, Raper AJ, et al. Systemic circulatory responses to hypocapnia in man. Am J Physiol. 1972;223:1308–12.
Winsö O, Biber B, Martner J. Effects of hyperventilation and hypoventilation on stress-induced intestinal vasoconstriction. Acta Anaesthesiol Scand. 1985;29:726–32.
Jakob SM, Groeneveld AB, Teboul JL. Venous–arterial CO2 to arterial–venous O2 difference ratio as a resuscitation target in shock states? Intensive Care Med. 2015;41:91–3.
Jakob SM, Kosonen P, Ruokonen E, Parviainen I, Takala J. Haldane effect-an alternative explanation for increasing gastric mucosal PCO2 gradients? Br J Anaesth. 1999;83:740–6.
Teboul JL, Scheeren T. Understanding the Haldane effect. Intensive Care Med. 2017;43:936–8.
Teboul JL, Mercat A, Lenique F, Berton C, Richard C. Value of the venous–arterial PCO2 gradient to reflect the oxygen supply to demand in humans: effects of dobutamine. Crit Care Med. 1998;26:1007–10.
Mallat J, Benzidi Y, Salleron J, Lemyze M, Gasan G, Vangrunderbeeck N, et al. Time course of central venous-to-arterial carbon dioxide tension difference in septic shock patients receiving incremental doses of dobutamine. Intensive Care Med. 2014;40:404–11.
Monnet X, Julien F, Ait-Hamou N, Lequoy M, Gosset C, Jozwiak M, et al. Lactate and venoarterial carbon dioxide difference/arterial–venous oxygen difference ratio, but not central venous oxygen saturation, predict increase in oxygen consumption in fluid responders. Crit Care Med. 2013;41:1412–20.
Mallat J, Lemyze M, Meddour M, Pepy F, Gasan G, et al. Ratios of central venous-to-arterial carbon dioxide content or tension to arteriovenous oxygen content are better markers of global anaerobic metabolism than lactate in septic shock patients. Ann Intensive Care. 2016;6:10.
Authors’ contributions
JM and UM contributed to study design. All authors contributed to data acquisition, analysis, and interpretation. JM designed and performed the statistical analysis. JM drafted the manuscript. All authors were involved in revising the draft. All authors read and approved the final manuscript.
Acknowledgements
The authors thank the nursing staff of the intensive care unit. Without their participations this work would not have been possible.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Consent for publication
A written informed consent was obtained from all the patients or their relatives.
Ethics approval and consent to participate
The study was approved by our local institutional ethics committee (Comité d’Ethique du Centre Hospitalier du Dr. Shaffner de Lens, France). Informed consent was obtained from each subject’s next of kin.
Author information
Authors and Affiliations
Corresponding author
Additional file
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mallat, J., Mohammad, U., Lemyze, M. et al. Acute hyperventilation increases the central venous-to-arterial PCO2 difference in stable septic shock patients. Ann. Intensive Care 7, 31 (2017). https://doi.org/10.1186/s13613-017-0258-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-017-0258-5