Abstract
Purpose
To assess the time course of the central venous–arterial carbon dioxide tension difference (∆PCO2)—as an index of the carbon dioxide production (VCO2)/cardiac index (CI) ratio—in stable septic shock patients receiving incremental doses of dobutamine.
Methods
Twenty-two hemodynamically stable septic shock patients with no signs of global tissue hypoxia, as testified by normal blood lactate levels, were prospectively included. A dobutamine infusion was administered at a dose of up to 15 μg/kg/min in increments of 5 μg/kg/min every 30 min. Complete hemodynamic and gas measurements were obtained at baseline, and at each dose of dobutamine.
Results
Dobutamine induced a significant dose-dependent increase of CI from 0 to 15 μg/kg/min (P < 0.001). Oxygen consumption (VO2) and VCO2 were progressively increased by dobutamine. These increases were more marked between 10 and 15 μg/kg/min (8.3 and 8.6 %, respectively) than between the lower doses. ∆PCO2 and oxygen extraction (EO2) significantly decreased between 0 (8.0 ± 2.0 mmHg and 43.8 ± 13.4 %, respectively) and 10 μg/kg/min of dobutamine (4.2 ± 1.6 mmHg and 28.9 ± 7.9 %, respectively), but remained unchanged from 10 to 15 μg/kg/min (5.4 ± 2.4 mmHg and 29.5 ± 8.2 %, respectively). The central venous oxygen saturation significantly (ScvO2) increased from 0 to 10 μg/kg/min and remained unchanged from 10 to 15 μg/kg/min. Time courses of ∆PCO2, ScvO2, and EO2 were linked therefore to the biphasic changes of VO2 and VCO2.
Conclusion
∆PCO2 is a good indicator of the change of VCO2 induced by dobutamine. Measurement of ∆PCO2, along with ScvO2 and EO2, may be presented as a useful tool to assess the adequacy of oxygen supply versus metabolic and oxygen demand.
Similar content being viewed by others
Introduction
Dobutamine is a synthetic catecholamine with strong inotropic effects on the myocardium owing to its predominately β1-adrenergic properties [1]. This drug is the first choice inotrope recommended by the Surviving Sepsis Campaign [2] for septic shock patients with low cardiac index (CI), or ongoing signs of tissue hypoperfusion in the presence of adequate fluid resuscitation. The aim of dobutamine administration in these patients is the restoration of an appropriate CI to provide adequate oxygen supply in an attempt to meet the elevated tissue oxygen requirements. However, dobutamine, in parallel to its effects on systemic hemodynamics, may increase oxygen consumption (VO2) and, therefore, tissue CO2 production (VCO2) through its direct cellular metabolic effects [3, 4]. According to the Fick equation applied to CO2, the determinants of the mixed venous-to-arterial CO2 difference (P[v–a]CO2) are tissue CO2 production and blood flow (cardiac output) [5, 6]. Previously, Teboul et al. [7] found that P[v–a]CO2 was helpful in assessing the adequacy of CI versus oxygen demand when incremental doses of dobutamine were infused into stable chronic heart failure (CHF) patients. Whether such phenomena can be observed in stable septic shock patients is presently not known. Interestingly, it has been demonstrated that P[v–a]CO2 can be substituted by the central venous-to-arterial carbon dioxide tension difference (∆PCO2) in critically ill patients [8, 9]. Therefore, the aim of our study was to assess the behavior of ∆PCO2—as an index of the VCO2/CI ratio—in hemodynamically stable septic shock patients, but with ongoing signs of tissue hypoperfusion, receiving incremental doses of dobutamine.
Materials and methods
This prospective and observational study was conducted in a single, mixed medical and surgical adult intensive care unit (ICU) with 15 beds. The study was approved by a local institutional ethics committee (comité d’éthique du centre hospitalier du Dr. Shaffner de Lens). Informed consent was obtained from the next of kin of each patient.
Patients
The study included 22 patients within 24 h of septic shock onset. The diagnosis of septic shock was defined according to the criteria of the American College of Chest Physicians (ACCP)/Society of Critical Care Medicine (SCCM) Consensus Conference [10]. As part of the routine management of septic shock in our ICU, all patients were already monitored by a transpulmonary thermodilution device (PiCCO, Pulsion Medical System, Munich, Germany) for CI measurement and were mechanically ventilated with a fractional inspired oxygen level (FiO2) no greater than 65 %, and a respiratory rate less than 35 breaths/min using an Engström Carestation ventilator (Engström, General Electrics, Madison, Michigan, USA). Sedation was provided with propofol and analgesia with remifentanil. Patients were included in the study if, as decided by the attending physician, dobutamine administration was needed to increase CI because of the persistence of signs of hypoperfusion (oliguria, mottled skin [11], central venous oxygen saturation (ScvO2) <70 % despite a hemoglobin >8 g/dl) despite achieving adequate intravascular volume and adequate mean arterial pressure (MAP) greater than 65 mmHg as recommended by the Surviving Sepsis Campaign [2]. Exclusion criteria were pregnancy, age less than 18 years old, unstable hemodynamic condition (change of vasoactive drug dosage or fluid administration within 1 h preceding the protocol), high blood lactate levels (>2 mmol/l), and uncontrolled tachyarrhythmias (heart rate >140 beats/min).
Measurements
Demographic data, septic shock etiology, the Acute Physiology and Chronic Health Evaluation (APACHE) II [12] and the Sequential Organ Failure Assessment (SOFA) scores [13] were obtained on the day of enrollment. CI was obtained with the PiCCO monitor by triplicate central venous injections of 20 ml of iced (<6 °C) 0.9 % saline solution and recorded as the average of the three measurements. In cases where the discrepancy in the CI measurements was greater than 10 %, the measurement was repeated two more times (five times in total) with elimination of the highest and lowest results. Blood gases analysis and lactate levels were measured using the GEM® Premier™ 3000 (Instrumentation Laboratory Co, Paris, France). ScvO2 was determined in a sample taken from the central venous catheter with the tip confirmed by X-ray to be in the superior vena cava near or at the right atrium. ∆PCO2 was calculated as the difference between central venous carbon dioxide tension and arterial carbon dioxide tension. Complete hemodynamic parameters were obtained (electronic supplementary material, ESM). Oxygen delivery (DO2) was calculated using the standard formula [14].
Transthoracic echocardiography was performed with a commercially available system. The left ventricular ejection fraction was calculated by the Simpson method [15].
Indirect calorimetry
Indirect calorimetry was obtained continuously using the new compact modular metabolic monitor E-COVX (GE Healthcare/Datex-Ohmeda, Helsinki, Finland). The characteristics of this monitor have previously been described in detail [16] (ESM).
The values of VO2 and VCO2 were recorded every 5 min to obtain a mean of six values collected (for each metabolic variable) over a 30-min period. Oxygen extraction ratio (EO2) was calculated as VO2/DO2.
Study protocol
Additional details on the study protocol are provided in ESM. Ventilation parameters, fluid, and doses of the vasopressor and sedation drugs were kept constant in the 60-min period preceding the measurements and throughout the study period. Hypovolemia was excluded by repeated volume challenges up to a point where CI did not increase further, or when the extravascular lung water indexed to predicted body weight reached 14 ml/kg [17]. After baseline measurements, an infusion of dobutamine was started at 5 μg/kg/min and increased by 5 μg/kg/min every 30 min up to 15 μg/kg/min. After each step, all measurements (hemodynamic, indirect calorimetry) were repeated, except for echocardiography, which was only performed at baseline. The study had to be stopped if adverse effects such as arterial hypotension (MAP <60 mmHg), tachycardia (heart rate >150 beats/min), acute atrial fibrillation, or changes in the ST segment of the electrocardiogram occurred.
Statistical analysis
Statistical analysis was performed by means of SAS software (SAS Institute Inc., Cary, NC 25513). The significance level was set at 0.05. Data are expressed as mean and standard deviation.
Comparisons of hemodynamic, blood gas, and metabolic parameters according to the incremental doses of dobutamine infusion were performed using a linear mixed model. This model is an extension of the classical ANOVA that allows the handling of both fixed effect (incremental doses of dobutamine infusion) and random effect (patient); thus, this model takes into account the correlation between the measures of one patient. The Bonferroni method was used to adjust for multiple comparisons.
The relationship between VO2 against DO2 was assessed with a linear mixed model with random coefficients. The dependent variable was VO2, the independent variable was DO2, and the subject effect was considered as a random effect. The correlation coefficient between VO2 and DO2 was computed by the method described by Roy [18] taking into account the repeated measures.
Results
Basic characteristics of the 22 patients are presented in Table 1. The left ventricular fraction collected in these patients (40 %) characterizes the global impairment of cardiac contractility. No changes in vasopressor therapy or ventilator settings occurred during the observation period. Dobutamine infusion was well tolerated in all patients. Its hemodynamic effects are listed in Table 2. Dobutamine induced a significant dose-dependent increase in CI, which was related to combined increases in heart rate and stroke volume index. Changes in CI were paralleled by a statistically significant increase in DO2 (Table 2). ScvO2 significantly increased in parallel with increasing doses of dobutamine from 0 to 10 μg/kg/min, and remained constant thereafter when dobutamine infusion rate was further increased to 15 μg/kg/min (Table 2).
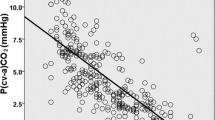
Dobutamine led to progressive increases in VO2 and VCO2 (Table 2). These increases were more pronounced when dobutamine was increased from 10 to 15 μg/kg/min (8.8 and 8.5 %, respectively) compared to the first two steps of dobutamine infusion (3.7 and 4 %, respectively between 0 and 5 μg/kg/min; 2.1 and 3 %, respectively between 5 and 10 μg/kg/min). The respiratory quotient remained unchanged (≈0.8) testifying to the accuracy of the indirect calorimetric measurements. The EO2 and ∆PCO2 significantly decreased from baseline to a dobutamine dose of 10 μg/kg/min, but stayed unchanged when dobutamine was increased from 10 to 15 μg/kg/min (Table 2). The time course of individual data and mean values of ∆PCO2 during dobutamine infusion is shown in Fig. 1a, b.
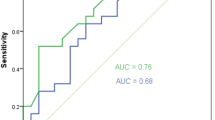
For each patient, regression lines of VO2 against DO2 were determined (mean r = 0.34) (Fig. 2a). The mean slope of the VO2/DO2 relationship was 6.4 ± 0.7 % (Fig. 2b).
Discussion
The main findings of our study were that (1) despite a dose-related increase in CI and DO2, dobutamine infusion up to 15 μg/kg/min did not result in a dose-dependent decrease in ∆PCO2, the central venous-to-arterial CO2 difference; (2) VO2 and VCO2 showed a statistically significant increase in parallel with the increased doses of dobutamine.
In patients with septic shock, global left ventricular hypokinesia, defined by left ventricular ejection fraction less than 45 %, has been observed in 60 % of cases during the first 3 days of hemodynamic support [19]. Dobutamine is recommended as the first-choice therapy to increase CI in the presence of signs of hypoperfusion after hypovolemia has been excluded, and adequate MAP has been achieved [2]. In our population, we observed a mean CI of 3 l/min/m2 along with an ScvO2 of only 59 % and a urinary output of 0.36 ml/kg/h before dobutamine was started. Furthermore, 41 % of patients had mottled skin (Table 1). These suggest the existence of tissue hypoperfusion associated with an inotropic defect as preload dependency was excluded by the absence of further increase of CI after repeated volume challenges. Additionally, the observed intrathoracic blood values index gave evidence against the presence of hypovolemia. Therefore, in our study, dobutamine was administered in order to increase CI in patients with established tissue hypoperfusion and cardiac dysfunction. This approach is completely different from the concept of supranormal oxygen delivery that refers to the use of dobutamine to drive up the oxygen delivery to achieve predefined supranormal hemodynamic end points for all patients at high risk of complications in an attempt to prevent organ failure and to improve outcome. Numerous controlled clinical trials of supranormal oxygen delivery involving patients with severe sepsis not only failed to demonstrate any benefit but also could be potentially harmful [20, 21].
Dobutamine may exert thermogenic effects and is able to increase both VO2 and VCO2. P[v–a]CO2 was shown to detect changes in oxygen demand accompanying dobutamine-induced changes in CI in stable CHF patients [7]. To the best of our knowledge there is no report on the behavior of ∆PCO2 in septic shock patients receiving incremental doses of dobutamine.
The increase in systemic blood flow can affect VCO2 production under situations of anaerobic metabolism activation. Indeed, under conditions of oxygen supply dependency, an increase in CI may concurrently lead to (1) an increase in aerobic VCO2 through the supply-dependent increase in VO2 and (2) a decrease of anaerobic VCO2 production [6, 7]. In this situation, the changes in CI may have no effect on the time course of ∆PCO2. Therefore, to better study the effects of dobutamine-induced increase in CI on ∆PCO2, we only included stable septic shock patients with no signs of anaerobic metabolism activation. Although the normal lactate levels after a resuscitation period up to 24 h might reflect an attenuated stress response and could not completely exclude the presence of anaerobic metabolism in our septic shock patients, the lack of previous oxygen debt was confirmed by the observation at the end of the study of a small positive slope (only 6.4 %) in the VO2–DO2 relationship during changes in DO2 testifying to an oxygen supply-independency state (Fig. 2a, b) [22–25]. Further evidence of the absence of anaerobic metabolism is that EO2 decreased and ScvO2 increased appropriately (instead of remaining constant) after increasing DO2 by dobutamine administration at between 0 and 10 μg/kg/min doses.
The change in ∆PCO2—as an index of VCO2/CI ratio—must be interpreted in line with changes in CI and VCO2. During the stepwise increase of dobutamine rate from 0 to 10 μg/kg/min, CI linearly increased resulting in a decrease of ∆PCO2, although VCO2 slightly increased. This is explained by the relatively much higher increase of CI compared to VCO2 (55 vs. 7.2 %, respectively) allowing removal of both stagnated and newly produced CO2 and resulting in a lower ∆PCO2. Our findings are, in part, in agreement with the results of Teboul et al. [7]. Indeed, these authors studied the effects of incremental doses of dobutamine on the time course of P[v–a]CO2 in ten stable CHF patients. They found that, from dobutamine doses of 0–10 μg/kg/min, P[v–a]CO2 decreased in parallel with a linear increase in CI. However, in that study VO2 and therefore VCO2 remained constant between these doses [7]. Differences between the two studies may stem from several factors. First, the studies involved dissimilar populations of patients. Second, in our study, VO2 and VCO2 were directly measured by indirect calorimetry, whereas VO2 was calculated from the reverse Fick equation in the study by Teboul et al. However, in accordance with our results, other studies [22, 24] reported a small increase in VO2 and VCO2 in patients with stable septic shock receiving incremental doses of dobutamine (from 0 to 10 μg/kg/min).
When dobutamine infusion rate was increased from 10 to 15 μg/kg/min, ∆PCO2 did not change significantly, whereas CI continued to increase. It is noteworthy that the relationship between CI and ∆PCO2 is curvilinear at constant VCO2 [6]. In this way, a change of CI will result in the smallest change of ∆PCO2 in the highest range of CI. However, in our study VCO2 was not constant but significantly increased when dobutamine was increased from 10 to 15 μg/kg/min. This increase of VCO2 was of the same magnitude as the increase of CI (8.3 vs. 7.5 %, respectively), which can mainly explain why ∆PCO2 remained unchanged or even slightly increased between 10 and 15 μg/kg/min of dobutamine. This hypothesis is further supported by the absence of significant changes in ScvO2 and EO2 observed at 15 μg/kg/min of dobutamine. Indeed, the increase of VO2 between 10 and 15 μg/kg/min of dobutamine counterbalances the increase of CI and explains the absence of any additional improvement in ScvO2 and EO2. Similar results were found in previous studies [7, 26].
Several mechanisms can be suggested to explain the increases of VO2 and VCO2 observed in our study. A first possibility is that, under anaerobic tissue metabolism conditions, VO2 becomes dependent on DO2, so that when DO2 is acutely increased, VO2 increases until the critical level of DO2 has been surpassed. This increase of VO2 is therefore due to the beneficial recovery of an oxygen debt situation. This mechanism is, however, unlikely to have occurred in our patients because of the normal blood lactate levels observed at baseline, the small slope in the VO2/DO2 relationship (Fig. 2b), and the increase of ScvO2, all of which rule out an oxygen supply dependency phenomenon. A second potential explanation is that the increase of VO2 and, therefore, VCO2 could be attributed to an increase of blood supply to organs such as the liver and the kidney whose needs are proportional to the blood flow. Indeed, increased blood flow to the kidneys is associated with an increase of renal metabolism [27]. We believe that such a mechanism may have contributed to the increase of VO2 between 0 and 10 μg/kg/min of dobutamine in our study. Indeed, we noted a substantial increase of DO2 (59 %) between 0 and 10 μg/kg/min of dobutamine whereas the increase of VO2 was only of 6 % suggesting that the increase in blood flow may largely explain the increase of VO2. A third possibility is that the increase of VO2 and VCO2 is due to an increase in cellular oxygen demand primarily under the influence of β-adrenergic stimulation by dobutamine. The thermogenic effects of catecholamines are well known [28]. Dobutamine, like other catecholamines, increases cellular metabolism in healthy volunteers even at low doses [3, 4]. However, the metabolic effects of dobutamine can differ between healthy subjects and critically ill patients who are under stress, probably because of some differences in basal catecholamine levels and a downregulation of β-adrenergic receptors in the latter group [29]. Interestingly, Uusaro et al. [30] demonstrated that the thermogenic effects of low doses of dobutamine were significantly reduced after a metabolic stress situation (that imitates the conditions of critically ill patients) has been induced in healthy subjects. Therefore, it is unlikely that the calorigenic effects of dobutamine might have played a considerable role in the increase of VO2 observed at low doses (<10 μg/kg/min) in our study. However, the thermogenic effects may be more pronounced at high doses of dobutamine in critically ill patients. In our study, VO2 increased markedly (8.6 %) between 10 and 15 μg/kg/min of dobutamine while DO2 increased by only 6 % (Table 2). Therefore, the proportionally higher increase of VO2 compared to DO2 associated with the absence of an oxygen supply dependency phenomenon suggests that the thermogenic effects of dobutamine were responsible for the increase of VO2 at the dose of 15 μg/kg/min. Our results are in agreement with the observations by Teboul et al. [7, 26] who reported calorigenic effects of dobutamine only at high doses (15 μg/kg/min) of the drug when infused in stable CHF patients.
Our results are of clinical importance. Since all patients in septic shock are usually equipped with central venous and arterial catheters, ∆PCO2 is easily obtained at the bedside. ∆PCO2 can assist the clinician in distinguishing between the hemodynamic and the metabolic effects of dobutamine. Indeed, dobutamine infusion at high doses may unfavorably alter the balance between tissue oxygen delivery and consumption through its thermogenic effects and thereby reduce tissue oxygenation. However, further clinical trials are required to assess the accuracy and utility of ∆PCO2 measurement in the choice of the dose of dobutamine to be administered to septic shock patients.
We acknowledge some limitations to our study. First, the number of patients studied was small. Second, the study was performed in a sample of septic shock patients from a single center with internal practices as reference. Third, our results do not pertain to septic shock patients with evidence of a supply dependency phenomenon.
Conclusion
Our study demonstrates that, in stable septic shock patients, dobutamine administration leads to an increase of DO2, which is associated with an increase of VO2 especially at high doses (calorigenic effects). ∆PCO2 appears to provide a good indication of the changes of VO2 induced by dobutamine. Monitoring ∆PCO2, along with ScvO2 and EO2, could be a useful tool to assess the adequacy of oxygen supply versus oxygen demand and, therefore, may help to guide therapy with dobutamine in stable septic shock patients.
Abbreviations
- ACCP:
-
American College of Chest Physicians
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- CI:
-
Cardiac index
- CHF:
-
Chronic heart failure
- DO2 :
-
Oxygen delivery
- EO2 :
-
Oxygen extraction
- FiO2 :
-
Fractional inspired oxygen level
- MAP:
-
Mean arterial pressure
- ∆PCO2 :
-
Central venous-to-arterial carbon dioxide tension difference
- P[v–a]CO2 :
-
Mixed venous-to-arterial carbon dioxide tension difference
- SCCM:
-
Society of Critical Care Medicine
- ScvO2 :
-
Central venous oxygen saturation
- SOFA:
-
Sequential Organ Failure Assessment
- VCO2 :
-
CO2 production
- VO2 :
-
Oxygen consumption
References
Ruffolo RR Jr (1987) The pharmacology of dobutamine. Am J Med Sci 294:244–248
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R (2013) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2012. Intensive Care Med 39:165–228
Bhatt SB, Hutchinson RC, Tomlinson B, Oh TE, Mak M (1992) Effect of dobutamine on oxygen supply and uptake in healthy volunteers. Br J Anaesth 69:298–303
Green CJ, Frazer RS, Underhill S, Maycock P, Fairhurst JA, Campbell IT (1992) Metabolic effects of dobutamine in normal man. Clin Sci 82:77–83
McHardy GJ (1967) The relationship between the differences in pressure and content of carbon dioxide in arterial and venous blood. Clin Sci 32:299–309
Dres M, Monnet X, Teboul JL (2012) Hemodynamic management of cardiovascular failure by using PCO(2) venous-arterial difference. J Clin Monit Comput 26:367–374
Teboul JL, Mercat A, Lenique F, Berton C, Richard C (1998) Value of the venous-arterial PCO2 gradient to reflect the oxygen supply to demand in humans: effects of dobutamine. Crit Care Med 26:1007–1010
Cuschieri J, Rivers EP, Donnino MW, Katilius M, Jacobsen G, Nguyen HB, Pamukov N, Horst HM (2005) Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med 31:818–822
van Beest PA, Lont MC, Holman ND, Loef B, Kuiper MA, Boerma EC (2013) Central venous-arterial PCO2 difference as a tool in resuscitation of septic patients. Intensive Care Med 39:1034–1039
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definition conference. Crit Care Med 31:1250–1256
Ait-Oufella H, Lemoinne S, Boelle PY, Galbois A, Baudel JL, Lemant J, Joffre J, Margetis D, Guidet B, Maury E, Offenstadt G (2011) Mottling score predicts survival in septic shock. Intensive Care Med 37:801–807
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG, On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710
Vincent JL, Van der Linden P, Domb M, Blecic S, Azimi G, Bernard A (1987) Dopamine compared with dobutamine in experimental septic shock: relevance to fluid administration. Anaesth Analg 66:565–571
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
McLellan S, Walsh T, Burdess A, Lee A (2002) Comparison between the Datex-Ohmeda M-COVX metabolic monitor and the Deltatrac II in mechanically ventilated patients. Intensive Care Med 28:870–876
Mallat J, Pepy F, Lemyze M, Barrailler S, Gasan G, Tronchon L, Thevenin D (2012) Extravascular lung water indexed or not to predicted body weight is a predictor of mortality in septic shock patients. J Crit Care 27:376–383
Roy A (2006) Estimating correlation coefficient between two variables with repeated observations using mixed effects model. Biom J 48:286–301
Vieillard-Baron A, Caille V, Charron C, Belliard G, Page B, Jardin F (2008) Actual incidence of global left ventricular hypokinesia in adult septic shock. Crit Care Med 36:1701–1706
Hayes MA, Timmins AC, Yau EH, Palazzo M, Hinds CJ, Watson D (1994) Elevation of systemic oxygen delivery in the treatment of critically ill patients. N Engl J Med 330:1717–1722
Gattinoni L, Brazzi L, Pelosi P, Latini R, Tognoni G, Pesenti A, Fumagalli R, SvO2 Collaborative Group (1995) A trial of goal-oriented hemodynamic therapy in critically ill patients. N Engl J Med 333:1025–1032
De Backer D, Moraine JJ, Berre J, Kahn RJ, Vincent JL (1994) Effects of dobutamine on oxygen consumption in septic patients. Direct versus indirect determinations. Am J Respir Crit Care Med 150:95–100
Vincent JL, Roman A, De Backer D, Kahn RJ (1990) Oxygen uptake/supply dependency. Effects of short-term dobutamine infusion. Am Rev Respir Dis 142:2–7
Schaffartzik W, Sanft C, Schaefer JH, Spies C (2000) Different dosages of dobutamine in septic shock patients: determining oxygen consumption with a metabolic monitor integrated in a ventilator. Intensive Care Med 26:1740–1746
De Backer D (2000) VO2/DO2 relationship: how to get rid of methodological pitfalls? Intensive Care Med 26:1719–1722
Teboul JL, Graini L, Boujdaria R, Berton C, Richard C (1993) Cardiac index versus oxygen-derived parameters for rational use of dobutamine in patients with congestive heart failure. Chest 103:81–85
Levy MN (1959) Influence of variations in blood flow and of dinitrophenol on renal oxygen consumption. Am J Physiol 196:937–942
Chioléro R, Flatt JP, Revelly JP, Jéquier E (1991) Effects of catecholamines on oxygen consumption and oxygen delivery in critically ill patients. Chest 100:1676–1684
Cohn JN, Levine TB, Olivari MT, Garberg V, Lura D, Francis GS, Simon AB, Rector T (1984) Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 311:819–823
Uusaro A, Hartikainen J, Parviainen M, Takala J (1995) Metabolic stress modifies the thermogenic effect of dobutamine in man. Crit Care Med 23:674–680
Acknowledgments
The authors are deeply indebted to the nursing staff of the intensive care unit for their help in this study.
Conflicts of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: Central venous-to-arterial carbon dioxide tension difference (∆PCO2) appears to provide a good indication of the changes in VO2 induced by dobutamine. Monitoring ∆PCO2 could be a useful tool to assess the adequacy of oxygen supply versus oxygen demand and, therefore, may help to guide therapy with dobutamine in stable septic shock patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mallat, J., Benzidi, Y., Salleron, J. et al. Time course of central venous-to-arterial carbon dioxide tension difference in septic shock patients receiving incremental doses of dobutamine. Intensive Care Med 40, 404–411 (2014). https://doi.org/10.1007/s00134-013-3170-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3170-y