Abstract
Purpose
To investigate the interchangeability of mixed and central venous-arterial carbon dioxide differences and the relation between the central difference (pCO2 gap) and cardiac index (CI). We also investigated the value of the pCO2 gap in outcome prediction.
Methods
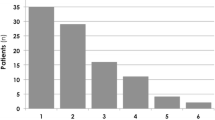
We performed a post hoc analysis of a well-defined population of 53 patients with severe sepsis or septic shock. Mixed and central venous pCO2 were determined earlier at a 6 h interval (T = 0 to T = 4) during the first 24 h after intensive care unit (ICU) admittance. The population was divided into two groups based on pCO2 gap (cut off value 0.8 kPa).
Results
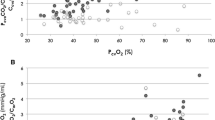
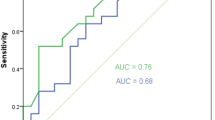
The mixed pCO2 difference underestimated the central pCO2 difference by a mean bias of 0.03± 0.32 kPa (95 % limits of agreement: −0.62–0.58 kPa). We observed a weak relation between pCO2 gap and CI. The in hospital mortality rate was 21 % (6/29) for the low gap group and 29 % (7/24) for the high gap group; the odds ratio was 1.6 (95 % CI 0.5–5.5), p = 0.53. At T = 4 the odds ratio was 5.3 (95 % CI 0.9–30.7); p = 0.08.
Conclusions
From a practical perspective, the clinical utility of central venous pCO2 values is of potential interest in determining the venous-arterial pCO2 difference. The likelihood of a bad outcome seems to be enhanced when a high pCO2 gap persists after 24 h of therapy.



Similar content being viewed by others
References
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall J, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM (2004) Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 32:858–873
Krafft P, Steltzer H, Hiesmayr M, Klimscha W, Hammerle AF (1993) Mixed venous oxygen saturation in critically ill septic shock patients. The role of defined events. Chest 103:900–906
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Tomlanovich M; for the Early Goal-Directed Therapy Collaborative Group (2001) Early Goal-Directed Therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
van Beest PA, Hofstra JJ, Schultz MJ, Boerma EC, Spronk PE, Kuiper MA (2008) The incidence of low venous oxygen saturation on admission in the ICU: a multicenter observational study in the Netherlands. Crit Care 12:R33
van Beest PA, van Ingen J, Boerma EC, Holman ND, Groen H, Koopmans M, Spronk PE, Kuiper MA (2010) No agreement of mixed venous and central venous saturation in sepsis, independent of sepsis origin. Crit Care 14:R219
Vallée F, Vallet B, Mathe O, Parraguette J, Mari A, Silva S, Samii K, Fourcade O, Genestal M (2008) Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intensive Care Med 34:2218–2225
Guyton AC, Hall JE (2000) Transport of oxygen and carbon dioxide in the blood and body fluids. In: Guyton AC (ed) Textbook of medical physiology, 10th edn. WB Saunders Co, Philidelphia, pp 463–472
Johnson BA, Weil MH (1991) Redefining ischemia due to circulatory failure as dual defects of oxygen deficits and of carbon dioxide excesses. Crit Care Med 19:1432–1438
Weil MH, Rackow EC, Trevino R, Grundler W, Falk JL, Griffel MI (1986) Difference in acid-based state between venous and arterial blood during cardiopulmonary resuscitation. N Engl J Med 315:153–156
Durkin R, Gergits MA, Reed JF, Fitzgibbons J (1993) The relationship between arteriovenous carbon dioxide gradient and cardiac index. J Crit Care 8:217–221
Cuschieri J, Rivers EP, Donnino MW, Katilius M, Jacobson G, Nguyen HB, Pamukov N, Horst HM (2005) Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med 31:818–822
Creteur J, De Backer D, Sakr Y, Koch M, Vincent JL (2006) Sublingual capnometry tracks microcirculatory changes in septic patients. Intensive Care Med 32:516–523
Fries M, Weil MH, Sun S, Huang L, Fang X, Cammarata G, Castillo C, Tang W (2006) Increases in tissue pCO2 during circulatory shock reflect selective decreases in capillary blood flow. Crit Care Med 34:446–452
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med 29:530–538
Chwala LS, Zia H, Guttierez G, Katz NM, Seneff MG, Shah M (2004) Lack of equivalence between central and mixed venous oxygen saturation. Chest 126:1891–1896
Gutierrez G, Comignanni P, Huespe L, Hurtado FJ, Dubin A, Jha V, Arzani Y, Lazzeri S, Sosa L, Riva J, Kohn W, Suarez D, Lacuesta G, Olmos D, Mizdraji C, Ojeda A (2008) Central venous to mixed venous blood oxygen and lactate gradients are associated with outcome in critically ill patients. Intensive Care Med 34:1662–1668
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Bland JM, Altman DG (2007) Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat 17:571–582
Lamia B, Monnet X, Teboul JL (2006) Meaning of arterio-venous pCO2 difference in circulatory shock. Minerva Anesthesiol 72:597–604
Mecher CE, Rackow EC, Astiz ME, Weil MH (1990) Venous hypercarbia associated with severe sepsis and systemic hypoperfusion. Crit Care Med 18:585–589
Bakker J, Vincent JL, Gris Ph, Leon M, Coffernils M, Kahn RJ (1992) Veno-arterial carbon dioxide gradient in human septic shock. Chest 101:509–515
Rackow EC, Astiz ME, Mecher CE, Weil MH (1994) Increased venous-arterial carbon dioxide tension difference during severe sepsis in rats. Crit Care Med 22:121–125
SvO2 collaborative group, Gattinoni L, Brazzi L, Pelosi P, Latini R MA, Tognoni G, Pesenti A, Fumagalli R (1995) A trial of goal-oriented hemodynamic therapy in critically ill patients. N Engl J Med 333:1025–1032
Hayes MA, Timmins AC, Yau E, Palazzo M, Hinds CJ, Watson D (1994) Elevation of systemic oxygen delivery in the treatment of critically ill patients. N Engl J Med 330:1717–1722
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Beest, P.A., Lont, M.C., Holman, N.D. et al. Central venous-arterial pCO2 difference as a tool in resuscitation of septic patients. Intensive Care Med 39, 1034–1039 (2013). https://doi.org/10.1007/s00134-013-2888-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2888-x