Abstract
Initiatives to eradicate malaria have a good impact on P. falciparum malaria worldwide. P. vivax, however, still presents significant difficulties. This is due to its unique biological traits, which, in comparison to P. falciparum, pose serious challenges for malaria elimination approaches. P. vivax's numerous distinctive characteristics and its ability to live for weeks to years in liver cells in its hypnozoite form, which may elude the human immune system and blood-stage therapy and offer protection during mosquito-free seasons. Many malaria patients are not fully treated because of contraindications to primaquine use in pregnant and nursing women and are still vulnerable to P. vivax relapses, although there are medications that could radical cure P. vivax. Additionally, due to CYP2D6's highly variable genetic polymorphism, the pharmacokinetics of primaquine may be impacted. Due to their inability to metabolize PQ, some CYP2D6 polymorphism alleles can cause patients to not respond to treatment. Tafenoquine offers a radical treatment in a single dose that overcomes the potentially serious problem of poor adherence to daily primaquine. Despite this benefit, hemolysis of the early erythrocytes continues in individuals with G6PD deficiency until all susceptible cells have been eliminated. Field techniques such as microscopy or rapid diagnostic tests (RDTs) miss the large number of submicroscopic and/or asymptomatic infections brought on by reticulocyte tropism and the low parasitemia levels that accompany it. Moreover, P. vivax gametocytes grow more quickly and are much more prevalent in the bloodstream. P. vivax populations also have a great deal of genetic variation throughout their genome, which ensures evolutionary fitness and boosts adaptation potential. Furthermore, P. vivax fully develops in the mosquito faster than P. falciparum. These characteristics contribute to parasite reservoirs in the human population and facilitate faster transmission. Overall, no genuine chance of eradication is predicted in the next few years unless new tools for lowering malaria transmission are developed (i.e., malaria elimination and eradication). The challenging characteristics of P. vivax that impede the elimination and eradication of malaria are thus discussed in this article.
Similar content being viewed by others
Introduction
The protozoan parasites of the genus Plasmodium are responsible for one of the deadliest and most common parasite infections: malaria [167]. Insects called vectors of infected female Anopheles mosquitoes carry the disease, which affects hundreds of millions of people worldwide [150]. Hundreds of millions of individuals worldwide are afflicted by the most lethal parasitic illness [177]. Malaria still affects approximately 50% of the global population [82]. In 2020, there were expected to be 241 million cases of malaria in 85 endemic countries, up from 227 million cases in 2019, according to data from the World Health Organization (WHO) (The World Malaria Report 2021), with 95% of cases coming from Africa [203].
The WHO has developed a new statistical technique that offers more accurate estimates of the causes of all diseases, including malaria, in young children. As opposed to earlier estimates of 4.8%, the updated technique found that 7.8% of childhood mortality was related to malaria. The updated methodology showed a consistent underestimate throughout the time series and a greater than previously recognized number of estimated deaths between 2000 and 2020 [131]. It is important to note that 96% of all malaria deaths worldwide are claimed to have occurred in Africa (with > 50% of deaths occurring in Nigeria, the Democratic Republic of the Congo, Uganda, Mozambique, and Angola) [34]. The continent of Africa is where most malaria infections and fatalities occur. In 2020, sub-Saharan Africa accounted for around 95% of all cases and 96% of all malaria deaths, with approximately 80% of these deaths reported in children under the age of 5 [144].
The most at-risk groups for malaria are children under five and expectant mothers. Malaria strikes these populations hardest [201]. According to the United Nations Children and Emergency Fund, a child under the age of five dies from malaria every two minutes [19]. In 2020, there were an estimated 11.6 million (34%) pregnancies exposed to malaria infection in the World Health Organization (WHO) African Region, which resulted in 900,000 low birth weight (LBW), 25,000 maternal deaths, and 100,000 neonatal deaths [110].
Approximately 102 million people in Latin America currently reside in locations where malaria transmission poses a concern, of whom at least 28 million do so in high-risk areas (where there are more than 10 cases per 1,000 population) [44]. In the past ten years, a lot of work has been done to eradicate malaria in the Americas. The WHO claimed that Paraguay, Argentina, and El Salvador were malaria-free in the years 2018–2021, which is noteworthy [169]. Despite this, malaria is still endemic in 17 nations and territories in the region [65]. P. vivax causes the majority of cases reported in Venezuela (76%), compared to P. falciparum (17.7%) and mixed P. vivax/P. falciparum infections (6%) and P. malariae (1%) [77]. Currently, the Amazon Basin, which encompasses nine South American nations, is the site of the great majority of malaria cases reported [187]. This is mostly linked to deforestation, ecological changes, and extensive human movement connected to a continuing process of land occupation [102].
Plasmodium infects a variety of animals, with at least five species posing a major health danger to humans [103]. The four limited or adapted species that have historically been identified as being the causes of human malaria are P. falciparum, P. ovale, P. malariae, and P. vivax [38]. The parasite P. knowlesi, which infects simian hosts, has been recognized as the fifth most significant Plasmodium in terms of human health [105]. There are other simian malaria parasites, P. cynomolgi and P. inui in Asia and P. brasilianum and P. simium in the Americas, that have also been shown to have the potential for zoonotic transmission to humans [33, 107].
The principal causes of malaria in humans are P. vivax and P. falciparum [103]. Although P. falciparum is the most frequent and widely spread malaria parasite, P. vivax is the most prevalent, most widely disseminated, and can also cause severe life-threatening sickness [125]. This parasitic infection remains the most challenging tropical disease to eradicate [165]. P. vivax malaria was once thought to be a benign infection but is now recognized as a significant global health threat due to its high morbidity and mortality rates [154]. The estimated yearly burden of P. vivax malaria (14.3 million [13.7 to 15.0 million]) is a significant order of magnitude lower than that of P. falciparum (193.5 million [142.0 to 254.7 million]) [27].
The Global Technical Strategy (GTS) for Malaria was established with the objective of fully eradicating malaria by 2030 [200]. The GTS aims to achieve global case incidence and fatality rates of at least 90% by 2030 and to totally eradicate malaria in at least 35 nations [151].
According to the 2016 World Malaria Report published by the World Health Organization (WHO), the incidence rate of malaria has fallen by 41% since 2000 [24]. Furthermore, there were no indigenous malaria cases in 23 countries for a total of three times between 2000 and 2020; 12 of these nations received the WHO certification for being malaria-free [203]. Despite these admirable accomplishments, many endemic countries still face enormous obstacles on the road to malaria eradication. The vast majority (85%) were in Africa, inflicting havoc primarily in Sub-Saharan Africa. P. vivax is progressively becoming the predominant source of malaria infection and disease in coendemic areas, although P. falciparum and P. vivax are the most common causes of human malaria.
Epidemiology of P. vivax
P. vivax, one of the five malaria parasites that may infect humans, has the widest geographic distribution [207]. Geographically, 48 percent of the world's population is at risk from P. vivax infection. Asia, South and Central America, Oceania, the Middle East, and some regions of Africa are all affected by it, which puts 2.85 billion people in danger each year [53]. P. vivax, found mostly in Asia and Latin America, is possibly the most prevalent malaria parasite globally and caused 4·5 million cases worldwide in 2020 [191]. Six nations accounted for more than 85% of all P. vivax cases worldwide: India, Afghanistan, Pakistan, Ethiopia, Papua New Guinea, and Indonesia [71]. P. vivax is assumed to be the cause of 8% of estimated malaria cases globally (approximately 50% when sub-Saharan Africa is omitted), with three countries (Ethiopia, India, and Pakistan) accounting for 80% of cases [166]. P. vivax, as opposed to P. falciparum, is the primary cause of malaria in the Americas [164]. Despite the fact that P. vivax is an uncommon species in Africa, where P. falciparum predominates, it is coendemic with P. falciparum in Ethiopia, where case incidence rates are roughly equal. P. vivax is responsible for approximately 40% of all malaria infections in Ethiopia, similar to other locations, according to several lines of evidence [16, 67].
Biology of P. vivax
In terms of biology, P. vivax and P. falciparum are highly distinct from one another [61]. This biological complexity helps it survive in situations that are not ideal for P. falciparum, allowing it to spread further [17]. This species appears to be more resistant to control efforts than P. falciparum, according to several control programs [88]. The therapies and monitoring methods designed for P. falciparum malaria may not be adequate or appropriate for P. vivax malaria [159]. Due to various unique aspects of P. vivax biology, eradication of malaria will eventually become a challenge [46].
P. vivax uses unique transmission strategies, such as (i) a dormant and relapsing stage in the liver (hypnozoites); (ii) reticulocyte tropism, the parasite strict reticulocyte preferences; (iii) gametocytes' rapid and consistent development; (iv) vivax malaria parasites are genetically highly variable; this genetic plasticity results in multiple clones of P. vivax infections, which may drive increases in parasite virulence, fitness, and survival, allowing it to respond to antimalarials differently than P. falciparum and other malaria parasites; (v) climatic conditions: the parasite's ability to replicate at lower temperatures than P. falciparum, allowing it to broaden its range far beyond the tropics; and (vi) drug resistance in the Malaria Parasite: CQ resistance appears to have spread globally [16, 16, 72, 96, 158].
In addition, many P. vivax vectors are early biters and outdoor feeders and exhibit outdoor-resting patterns [68]. These characteristics are supposed to make it easier to get through control measures such as insecticide-treated nets (ITNs) or indoor residual spray (IRS). As a result, P. vivax is less likely to be controlled by ITNs or IRS [104]. Because of this, P. vivax transmission would be more resilient to control measures over time than P. falciparum. Data from a scientific review by [115] overwhelmingly support this. Despite these findings, the WHO proposed a bold global goal of eliminating malaria in 35 countries by 2030 [200]. This goal is significantly hampered by the fact that this species has evolved. P. vivax must therefore have been recognized as a significant barrier to the control and eradication of malaria in coendemic areas. Table 1 summarizes the obstacles of eliminating vivax malaria as well as the implications.
Control challenges
Hypnozoite: the forgotten obstacle
Plasmodium parasites have a complicated life cycle [192]. Infected mosquito sporozoites move to the liver and begin the hepatic stage of the parasite life cycle by penetrating hepatocytes, where they multiply and develop into schizonts containing thousands of hepatic merozoites [167]. P. vivax, on the other hand, has unique biological properties, including an extra stage that greatly increases the epidemiological and clinical complexity of the disease compared to P. falciparum [5]. That is, not all sporozoites in the liver grow into schizonts right away; some evolve into small, nonreplicating, unnucleated latent forms in the liver stage, termed hypnozoites [32]. In a study that used a mouse model, [126] found that hypnozoites exist after the primary liver stage infection has occurred. They are significantly smaller and nonreplicating than replicating liver-stage schizonts [190]. Additionally, no diagnostic tools are available at this time that can identify this stage [78]. The parasite's hypnozoite form, which may evade the human immune system and blood-stage therapy and provide a safe haven during mosquito-free seasons, can remain inside liver cells for weeks to years [147, 195]. Due to its dormancy, the parasite may endure the winter when Anopheles mosquito transmission is not possible due to the environment [46]. Eventually, the hyponozoite reactivates and multiplies, producing a blood-stage relapse and subsequent parasite transmission unless drugs specifically targeting the infection are administered [81]. Each strain may have a different ratio of hypnozoites to sporozoites, and parasites with a larger proportion of hypnozoites may be more likely to relapse frequently [46]. Additionally, the latent hypnozoite may be lying in wait when forward transmission is questionable due to conditions that do not favor the mosquito. For instance, mosquito activity tends to be seasonal in temperate climates [148]. On the other hand, P. falciparum causes only one attack in less than two weeks following a single contagious bite [121]. Following the initial blood-stage infection, hypnozoites activate to produce subsequent relapsing infections, and it is believed that relapses account for 79–96% of all P. vivax infections [92]. According to data from the Thai-Myanmar border, 3 out of 4 patients relapsed after 1441 recurrent P. vivax infections in 1299 patients over the course of 1000 patient follow-up years [180]. According to other data from Southeast Asia and the South Pacific, hypnozoite-induced relapses account for the majority of the burden of acute P. vivax infection [140]. This undetectable hypnozoite reservoir represents one of the primary barriers to malaria control since it maintains active transmission of the disease and is resistant to the existing antimalarial medications used to clear exoerythrocytic stages [15]. Furthermore, no diagnostic tools are currently available that can diagnose this stage [78]. Thus, this trait promotes the spread of parasites throughout the year and increases the difficulty of controlling the parasite.
The frequency of relapses is mostly determined by numerous hypothesized variables, including the size of the sporozoite inoculum, the host's innate immunity, the primary therapeutic regimen, coinfections, fever, hemolysis, seasonality, mosquito bites, and epigenetic debates [190]. Tropical regions have a significant (> 80%) incidence of early relapse, with subsequent relapses occurring every 3–4 weeks [159]. Additionally, the latency duration may be influenced by the sporozoite inoculation load. Each strain may have a different ratio of hypnozoites to sporozoites, and parasites with a larger proportion of hypnozoites may be more likely to relapse frequently [46].
Furthermore, because hypnozoites serve as a reservoir for a variety of P. vivax strains, they will supply a large number of concurrently circulating parasite clones in the bloodstream, as well as effective genetic recombination between unrelated P. vivax parasites [198]. P. vivax-infected mosquitoes can produce numerous clinical attacks attributable to hypnozoites [11]. As a result, hypnozoites make malaria control more difficult by allowing P. vivax parasites to spread spatially and develop drug resistance. These characteristics make the distribution of vivax in a population less responsive to vector control techniques. As a result, P. vivax cannot be effectively controlled using falciparum malaria control strategies.
The primaquine issue and the puzzle of primaquine therapy
Primaquine in the real world
Primaquine (PQ), an 8-aminoquinoline, is one of the first synthetic antimalarial medicines and was discovered in 1946 [20]. Since 1952, PQ has been the sole FDA-approved treatment for the hypnozoite stage [176]. It works against P. falciparum mature gametocytes and the hepatic dormant stage, as well as the hypnozoites of two Plasmodium species (P. vivax and P. ovale) that can cause relapses [130]. According to a study by Cedillos RA. from El Salvador, 46–68% of individuals experienced repeated P. vivax episodes without receiving PQ treatment [170]. It is suspected to interfere with the parasite's oxygen consumption by creating oxygen free radicals yet disrupting the parasite's electron transport system, while the mechanism of action is unknown [35].
Despite the fact that PQ is the sole, unique, irreplaceable, and successful treatment for eradicating P. vivax hypnozoites, it is also accompanied by substantial risks and side effects [52]. Side effects such as gastrointestinal disturbances (nausea, dizziness, and vomiting), hypersensitivity reactions, and life-threatening severe hematological adverse effects, particularly in patients with inborn erythrocytic G6PDd (methemoglobinemia and hemolytic anemia), have limited the drug's utility [26, 31]. There are several PQ regimens in common use today. The currently WHO recommended treatment, people with P. vivax malaria should be treated with chloroquine for three days to kill the parasites that cause malaria symptoms in the blood, then 0.25 mg/kg of body weight (in a single daily dose) of PQ for 14 days to treat hypnozoite-derived relapses ('radical cure') of vivax malaria [118]. Based on a study conducted in Brazil by [50], the total dose given influences the radical curative efficacy so that compliance is essential for a radical treatment because effectiveness is correlated with the total PQ dose given. One of the clinical drawbacks of this treatment regimen is that it is more than four times longer than conventional schizontocidal regimens, which limits adherence to the lengthy regimen [118, 162]. Nonadherence to this PQ treatment varies from 2 to 40% [111]. Patients typically experience symptom improvement within a few days of beginning CQ, hence, they frequently do not adhere to the PQ treatment plan's 14-day duration [8]. Lack of an immediate advantage, a lack of knowledge of the long-term benefits for the individual and society, and the misconception that vivax malaria is a benign disease are other reasons that contribute to nonadherence [111].
On the other hand, for the radical cure of P. vivax, PQ 0.5 mg/day for 7 days is employed; this shorter, higher dose regimen is being used in several nations, such as Brazil [135]. The same total dose (0.5 mg/kg/day to 210 mg) administered over 7 days as opposed to 14 days may have little to no difference on P. vivax recurrences [127]. Several surveys showed that despite the short duration, less than 70% of people completed the short-course primaquine regimen. This may be because of its complicated treatment regimen, which still makes adherence difficult, and its occasional subpar effectiveness [136]. Even though research from South America suggests that a PQ dose of 0.5 mg/kg for 7 days is safe and well tolerated, overweight people have a greater rate of relapses caused by subtherapeutic PQ doses [118].
A significant portion of malaria patients are excluded from PQ use in pregnant and nursing mothers, leaving them partially cured and still susceptible to P. vivax relapses [45]. As a result, many women who breastfeed for an extended period of time are prohibited from receiving radical therapy. Contraindications to PQ usage in pregnant and breastfeeding mothers exclude a major number of malaria patients who are subsequently not fully cured and are nonetheless vulnerable to P. vivax relapses [73]. As a result, many women who continue to breastfeed for a long time are banned from obtaining radical treatment. Therefore, malaria relapses during pregnancy may result in congenital malaria, and radical treatment of P. vivax in this group is still challenging [46]. PQ resistance is sometimes confused with treatment failure, even though genuine resistance to PQ has not been demonstrated by independent sources (relapse incidence) [8]. In a recent study conducted in Ethiopia, individuals who had 14-day PQ had a 17% higher probability of developing P. vivax parasitaemia again [3]. The WHO goal of eliminating malaria by 2030 could therefore be jeopardized by the aforementioned variables if P. vivax transmission could be sustained.
To circumvent this roadblock, the possible inclusion of the hypnozoitocidal drug tafenoquine (TQ) (Krintafel) was approved by the Food and Drug Administration as a single-dose regimen to treat patients with confirmed P. vivax infection for radical cure [92]. Despite this benefit, hemolysis of the earlier erythrocytes continues in individuals with G6PD deficiency until all susceptible cells have been destroyed. This is because the drug's delayed clearance (terminal half-life of approximately 15 days) makes single-dose treatment possible [101]. This orally active, 8-aminoquinoline drug is eliminated much slower than PQ (14 to 28 days versus 4 to 6 h) [76]. Tafenoquine solves the potentially important problem of poor adherence to daily primaquine by providing a radical cure in a single dose [85]. In contrast, due to primaquine's quick elimination (4–9 h), stopping the drug can significantly reduce drug-induced hemolysis [176].
Hemolysis caused by PQ and TQ in G6PD deficiency
The most important danger of 8-aminoquinolines is dose-dependent hemolysis in people with G6PD deficiency [197]. G6PD is an enzyme that serves as a housekeeper in all cells and protects red blood cells from stress [186]. People who live in nations where malaria is endemic are more likely to have G6PDd. In fact, the frequency is significantly higher (8%) in countries with a high malaria infection rate [29]. G6PD deficiency can be frequent in these groups. Data showed that this X-linked abnormality is very common, affecting almost 400 million individuals worldwide [113].
In persons with G6PD deficiency, both drugs, PQ and TQ can hemolyze red blood cells, resulting in anemia [98]. PQ's hemolytic activity has long been thought to be caused by intraerythrocytic oxidative stress mediated by redox-active metabolites rather than the parent drug. Splenic macrophages are considered to recognize oxidatively damaged RBCs as the equivalent of senescent red cells, resulting in their removal from circulation [74]. On the other hand, TQ, as a single-dose medication, eliminates a significant drawback of the 7- or 14-day primaquine regimen: the possibility of poor adherence. However, this benefit comes with a significant risk of hemolytic toxicity with G6PD deficiency, too, because once tafenoquine is administered, it cannot be "stopped" if there is drug-induced hemolysis [111].
Both PQ and TQ use are made challenging by the lack of a quick G6PD test or the availability of a standard G6PD test. This problem could hinder efforts to eradicate malaria [60, 109]. Both PQ and TQ radical treatment have the potential to completely transform the management and eradication of vivax malaria, but to ensure its safe delivery, it will be required to create the requisite instruments for assessing G6PD status [55]. Testing for G6PD is currently offered in a variety of ways. Flow cytometry and spectrophotometry are the gold standard tests. Despite the fact that these tests measure enzyme activity, they are expensive and require an efficient lab infrastructure [109]. The most recent WHO treatment guidelines state that it is an excellent practice to use a patient's G6PD status to guide primaquine administration. Recently, more emphasis has been placed on safe primaquine medication, guided by testing for G6PD status before prescription. It is comforting to know that quick, point-of-care (PoC) G6PD test kits are available [99].
Genetic variation in CYP2D6 and PQ metabolism: PQ Pharmacogenomics
Numerous drugs are metabolized by an isoenzyme family called cytochrome P450 (CYP), which is mostly found in the endoplasmic reticulum of liver cells [84]. About 25% of all medications used in clinical practice are metabolized by the cytochrome P450 2D6 (CYP2D6) enzyme [119]. The drug-metabolizing enzyme Cytochrome P450 2D6 (CYP2D6) is produced by the CYP2D6 gene [152]. This human cytochrome P-450 isoenzyme 2D6 (CYP2D6) is essential for the conversion of primaquine to its active metabolites and for the hypnozoite killing procedure in hepatocytes [122]. CYP2D6 also contributes to the partial metabolization of TQ [124].
This gene is unique in that it exhibits a wide range of variants, ranging from complete inactivity (poor metabolizers) to manifold augmentation, which have a significant impact on the performance of the enzyme [194]. Among the variations in CYP2D6 (CNV), these are caused by single-nucleotide variants (SNVs), whole-gene deletions, small insertions and deletions, multiplications, tandem arrangements, and changes in gene copy number (CNV) [124, 179]. As a result, the CYP2D6 genetic polymorphism, which is very variable, may have an impact on the pharmacokinetics of primaquine [172]. False PQ tolerance assumptions in the parasite result from people with specific CYP2D6 polymorphism alleles being unable to metabolize PQ and possibly failing treatment [50]. It has been demonstrated in both animal models and people that primaquine's capacity to metabolize to its active metabolite is decreased by decreased CYP2D6 activity [156]. It influences plasma concentrations of PQ and its metabolites and is connected to PQ therapy failure in P. vivax malaria, as demonstrated in both animal models and humans As proven in both animal models and humans, it affects plasma concentrations of PQ and its metabolites and is linked to PQ treatment failure in P. vivax malaria [174].
Eradication attempts targeting PQ use could encounter significant difficulties due to the varied nature of CYP2D6 activity, as many groups worldwide, especially those in endemic locations, have a high prevalence of CYP2D6 impairments [171]. In Indonesia, directly monitored high-dose primaquine treatments resulted in 95% of therapeutic failures, according to research by [178] Therefore, it is crucial to establish methods to prevent relapse in individuals who are unable to undergo PQ treatment. In addition to safety issues, drug compliance, the ideal dose depending on bodyweight, and the follow-up duration need to be examined.
Plasmodium vivax tropism to reticulocytes and Duffy antigens
Bone marrow reticulocytes: the younger, the better?
RBC age appears to be a significant restriction for malaria parasites [42]. Reticulocytes are a diverse population of red blood cell precursors with ribonucleic acid residues that represent the final stage of erythropoiesis before full maturation into red blood cells (RBCs) [173]. Reduced expression of the transferrin receptor CD71 (TfR1 or CD71) indicates reticulocyte maturation [185]. P. vivax has a narrower cell tropism than previously assumed, infecting all reticulocytes but restricted preferences only to young reticulocytes with high transferrin receptor CD71 (TfR1 or CD71) [108]. This was well investigated by [120] from P. vivax isolated in Thailand. P. vivax preferentially invades very immature reticulocytes expressing high levels of the transferrin receptor CD71 on their surface. Immature CD71 + reticulocytes are most commonly found in the bone marrow, where they are created, reside, and are generally confined [184]. Due to the low proportion of reticulocytes (0.5–1%) among all cells in human blood, P. vivax parasitemia is maintained at low levels [80]. The high number of submicroscopic and/or asymptomatic infections caused by reticulocyte tropism and the low parasitemia levels that accompany reticulocyte tropism are undetected by field tests such as microscopy or fast diagnostic tests (RDTs) [10, 114]. These asymptomatic infections remain untreated and may contribute to transmission over several weeks or months [63].
This phenomenon raises the intriguing possibility that P. vivax biomass occurs in extravascular tissues of the marrow and spleen rather than in circulating blood [168]. Recent work has also demonstrated that a substantial proportion of the biomass of asexual P. vivax trophozoites and schizonts occurs in the extravascular spaces of marrow, spleen, and liver [11]. Consequently, parasite densities in the blood are often low and undetectable, creating significant challenges for the diagnosis and treatment of infected individuals. The dynamics of infection, parasite reservoirs, and putative parasite killing mechanisms are all impacted by P. vivax's tight affinity for young reticulocytes, making malaria elimination problematic.
Infection of Duffy-negative erythrocytes by P. vivax: a recent adaptation
P. vivax malaria was previously thought to be uncommon or nonexistent in African populations that did not express the Duffy blood group antigen. This remains an out-of-date viewpoint [83]. However, numerous instances of P. vivax infection in patients who tested negative for Duffy have recently been documented in a number of African nations, including Angola, Benin, Botswana, Cameroon, Ethiopia, Equatorial Guinea, Kenya, Madagascar, Mali, Mauritania, Senegal, Sudan, and Uganda [79]. Among Duffy-negative people in Africa, 24 (88.9%) experienced P. vivax infections, according to a meta-analysis by [204]. These results disprove the notion that P. vivax infection is completely prevented by erythrocytes lacking the Duffy antigen receptor for chemokines (DARC) [79]. This action raises important issues concerning how P. vivax enters the erythrocytes of Duffy-negative individuals. It has been hypothesized that copy number variation, which is either low expression of DARC in Duffy-negative individuals, binds easily to parasites that carry multiple copies of P. vivax Duffy binding protein (PvDBP), changes in PvDBP1 or duplication in the PvDBP gene created a new entryway and is responsible for the parasites' increased ability to spread [97, 155]. Due to this, it is challenging to control and eradicate P. vivax malaria, which highlights the concern that these 'new' P. vivax strains that infect Duffy-negative hosts could spread throughout much of Africa and have severe, significant effects on the general public health and economy.
In addition, a study from Ethiopia by [1] revealed that patients with P. vivax infection who had the Duffy-negative genotype displayed a consistently low asexual parasitaemia (median, 53 parasites/L). This low asexual parasitaemia in Duffy-negative patients may be an "undetected silent reservoir," which would undoubtedly make it more challenging to eradicate vivax malaria [21]. Additionally, this may make it more difficult to comprehend the epidemiology of vivax malaria in the area.
The tip of the iceberg: P. vivax submicroscopic
Considering that P. vivax invasion is entirely erythrocyte age specific, the rigorous requirement for young reticulocytes has implications for malaria diagnosis [95]. This is because P. vivax invades reticulocytes, which make up a minor portion of the circulating erythrocytes, and P. vivax infections are frequently misdiagnosed because parasitaemia is too low [75]. Duffy-binding protein (DBP) and host reticulocyte-binding protein (HRBP) appear to be required for erythrocyte invasion by the P. vivax merozoite (RBP) [86]. One of the P. vivax erythrocyte binding proteins (pvRBPs) and EBPs is thought to be important in reticulocyte recognition, particularly in young (CD71high) reticulocytes. DARC is not implicated, however, because reticulocytes and mature red cells (normocytes) both express identical amounts of DARC on their surfaces [40]. Because parasites also appear to "sequester" in the bone marrow [141], the number of P. vivax blood stages circulating in peripheral blood may not provide a realistic indication of the total parasite biomass retained by the host. One of the pvRBPs and EBPs is thought to be important in reticulocyte recognition, particularly in young (CD71high) reticulocytes [40]. These findings help to explain why P. vivax parasitemias are naturally and consistently lower than P. falciparum parasitemias [173]. For identical infection rates, the proportion of infections detected by microscopy appears to be similar for P. falciparum and P. vivax. However, because parasite prevalence rates for P. vivax in communities are often lower than those for P. falciparum, the proportion of missed infections may be larger overall for P. vivax than for P. falciparum [200].
P. vivax parasite counts at clinical presentation are typically 4 000 ± 3 000 parasites per liter of blood (p/L), which is three to four times lower than P. falciparum, and peak parasitemia seldom surpasses 100 000 p/L in P. vivax but is relatively common in P. falciparum. In low-prevalence locations, submicroscopic infections appear to be of greater relative relevance, posing an additional barrier to eradication attempts [54].
Furthermore, a positive parasitological test result from either microscopy or a rapid diagnostic test (RDT) is required before treatment can begin, according to WHO criteria for malaria diagnosis and treatment [157]. According to a review [90], 69.5 percent of all P. vivax blood-stage infections are submicroscopic, and asymptomatic P. vivax causes 89–100 percent of submicroscopic infections. Furthermore, according to a Brazilian cohort study [70], microscopy missed 4 percent of P. vivax infections discovered by polymerase chain reaction (PCR); 57 percent of them caused no clinical signs or symptoms indicative of malaria, and 33 percent were both subpatent and asymptomatic. As a result, some malaria patients do not receive prompt treatment, causing the disease to spread. Malaria diagnosis therfore requires sensitive and economical diagnostics for detecting low-load infections and infections in all population carriers who may or may not display clinical symptoms to accomplish elimination [134].
P. vivax cytoadhering: immune evasion occurrence
RBCs infected with P. falciparum have the capacity to cytoadhere to several host cell types, including endothelial cells and red blood cells that are not infected, and sequester in the microvasculature [175]. Due to its ability to stay in deep vascular beds and avoid being removed by the spleen, this occurrence is essential to the parasite's immune-evasion strategy [58, 106]. P. vivax's inability to cytoadhere has long been thought to exist. However, investigations have demonstrated that P. vivax-infected erythrocytes (Pv-iE) can cytoadhere to host cells in vitro [62].
Mature P. vivax-infected erythrocytes (Pv-IEs) have been demonstrated to cytoadhere to human lung endothelial cells, Saimiri brain endothelial cells, and cryosections of the placenta in earlier in vitro studies from Manaus (Brazil) [39]. The database for adhesion characteristics in P. vivax parasites is now expanding [188]. Carvalho and associates first showed that PvIRs can cling to human lung endothelial cells (HLECs), Saimiri brain endothelial cells (SBECs), placental cryosections, CSA, and the cell-surface receptor ICAM-1 in a study by [161] According to Brazilian research [123], rosetting was observed in 64% of the isolates, CSA adherence in 15%, ICAM1 adhesion in 12%, and placental cryosections in 9%. Additionally, the findings of a study by [206] show that P. vivax-infected red blood cells (PvIRBCs) rosette irreversibly with normocytes and are significantly stiffer than nonrosetting PvIRBCs. Further evidence reveals that P. vivax can, to some extent, exhibit pathogenic profiles comparable to P. falciparum given the presence of severe types of malaria in P. vivax infections, such as cerebral malaria and placental malaria, which were previously reported to be exclusively linked with P. falciparum [188].
Transmission and early development of sexual blood stages (gametocytes)
Gametocytes from P. falciparum and P. vivax have highly different biology [137]. These Plasmodium species have different maturation times for gametocytes [49]. Within a few days of the first appearance of the asexual stage, P. vivax gametocytes swiftly appeared in the bloodstream [100]. This differs significantly from P. falciparum, whose gametocytes mature one week later [23]. Because sequestration in tissues is not a key phase in P. vivax development, gametocytes mature significantly faster than P. falciparum gametocytes [100]. Evidence also suggests that P. vivax forms gametocytes at a rate that is higher (up to 20% every cycle) than that of P. falciparum [149]. Mature P. vivax gametocytes are found in the bloodstream far earlier and before the beginning of clinical illness, virtually certainly before patients seek treatment [142].
The relatively quick gametocyte development of P. vivax, which occurs concurrently with asexual parasite stages, as opposed to 10–12 days in P. falciparum, accounts for the early transmissibility [143]. This shorter embryonic cycle of P. vivax is thought to increase the likelihood of mosquito infections with various genotypes, resulting in more recombination among those genetically heterogeneous parasites [162]. This indicates that P. vivax will be more transmissible than P. falciparum because mosquito infections are more efficient [159]. The majority of gametocyte carriers were also asymptomatic, which suggests that silent infections may play a key role in the spread of malaria. This has been amply established in Thailand, where a significant percentage of P. vivax gametocytes are found in asymptomatic infections [138], indicating a potentially significant contribution to the transmission reservoir. As a result, the human parasite reservoir comprises asymptomatic P. vivax infections in people who do not seek medical help. This reveals that P. vivax gametocytes are a transmission control bottleneck [189]. When compared to P. falciparum, P. vivax transmission is more likely to be stable over time, undermining control efforts. As a result, the P. vivax malaria control strategies established for falciparum malaria will not be as effective [146].
Genetic diversity
Genetic diversity is one of the most important strategies by which the malaria parasite may maintain a long-term infection despite a continual immune response. P. vivax populations show higher genetic variation than P. falciparum populations across their genome [53]. Evolutionary fitness is provided by genetic diversity, which increases the possibility for adaptation to changing circumstances [128]. As a result, parasite populations with a wide genetic diversity are more likely to resist antimalarial host immunological responses [57]. Furthermore, the presence of distinct parasite forms in different geographic regions, as well as their diverse genotypes, presents challenges to the creation of a malaria vaccine [36, 207].
P. vivax has exhibited considerable genomic diversity in several population genetic studies based on microsatellite data and, more recently, whole genomes [18]. Furthermore, investigations have revealed that the genome of P. vivax parasites circulating in the same location is more diverse than that of P. falciparum parasites [53]. The parasite clones that coexist in natural infections are frequently genetically diverse. Reactivating genetically varied hypnozoites causes more frequent outcrossing during meiotic recombination and a quicker creation of new parasite strains, which increases the genetic complexity of blood-stage infections [64].
Antigenic variation, repeat-number variation in microsatellites, gene copy-number variation (CNV), and single-nucleotide polymorphisms (SNPs) have all been discovered in isolates from various geographic origins [48, 53]. Garzón-Ospina et al. [72] observed that such polymorphisms are often present in functionally irrelevant genes. This could open up new invasion paths that were previously unknown.
This high amount of antigenic polymorphism shows the presence of sophisticated mechanisms that have allowed this parasite species to escape and overcome host immune responses [193]. Because many critical immunological targets and vaccination candidates display significant polymorphism, high antigenic diversity poses a significant challenge when developing a vaccine [41]. That is perhaps why only limited candidate vaccines are believed to have entered Phase I clinical trials, compared to 23 P. falciparum vaccine candidates [13, 182]. According to another study by [116], sequence diversity was seen in gene families linked to immune evasion and erythrocyte invasion, suggesting that vaccines targeting polymorphic antigens may face an even greater challenge in eliciting an effective immune response than they do in P. falciparum, where strain-specific immunity has been shown to limit vaccine efficacy.
Furthermore, superinfection by genotypes that are unrelated can result in many parasite clones [208]. During their life cycles, these strains interact, and these interactions can result in intricate patterns of interspecies exchanges and intrahost competition [2]. Drug-resistant P. vivax strains are becoming more common, which could be linked to parasite genetic diversity [91]. According to [160], P. vivax is growing increasingly resistant to chloroquine, the first-line treatment, and is refractory to most types of antimalarial medicines. Furthermore, the reactivation of genetically varied P. vivax hypnozoites increases the genetic diversity of blood-stage infections by allowing for more frequent outcrossing during meiotic recombination and the formation of novel parasite strains [12].
Overall, genetic diversity assures evolutionary fitness, boosting the possibility of adapting to changing environmental conditions. Additionally, drug resistance is more likely to develop in parasite populations with a range of genetic make-ups [94]. In general, P. vivax's genetic diversity may help the parasite adapt to new challenges, such as improved treatments and control strategies.
Climate conditions: temperature
Climate factors, such as temperature, rainfall patterns, and humidity, have a significant impact on the life cycles and survival of parasites and vectors, which in turn greatly affects the susceptibility to transmission of diseases such as malaria [69]. The biology of parasites is heavily influenced by temperature [117]. The main reason why malaria is frequently referred to as a climate-dependent disease is that mosquito sporozoites require a specific range of temperatures to fully mature [196]. The amount of temperature variation that occurs throughout the day has an impact on site development [28]. An experimental report found that the P. falciparum sporogony in mosquito vectors is temperature-sensitive. When compared to P. falciparum, P. vivax has a lower minimum temperature at which sporogonic development takes place [27]. P. vivax, on the other hand, can tolerate a wider range of environmental temperatures than the more virulent P. falciparum (minimum: 16 °C vs. 21 °C for P. falciparum), which may help to explain why it is more distributed widely and exhibits very efficient transmission rates across a wider range of climates [38]. Unlike other human malaria species, P. vivax grows, although slowly, at lower temperatures to develop in the vector, between 16 and 18 °C, whereas P. falciparum can only grow at temperatures higher than 18 °C [129]. P. vivax sporogony in the vector is shorter (~ 10 days at 25 °C) than for P. falciparum (12 days) [153]. Due to its sporozoites' ability to mature at lower temperatures, P. vivax is temperature agnostic [158]. This form of development dramatically widens the parasite's worldwide range, allowing it to spread more widely across the globe and the parasite's ability to establish long-term transmission foci in temperate climates rather than only in tropical climates [200].
Furthermore, several major P. vivax vectors have specific characteristics, including early biting, outdoor feeding, and outdoor resting [25]. There are large rates of early and outdoor transmission of vivax malaria, according to data from various regions. According to data from western Eritrea, 36.4 percent of infective bites were acquired outside, while up to 49 percent of outdoor transmission in Uganda occurred before bedtime [59]. Thus, the two main vector control strategies, ITNs and IRS, are not necessarily as efficient against P. vivax as they are against P. falciparum in terms of reducing mosquito life duration by targeting indoor and nocturnal biting mosquitoes.
Implementing an environmental alteration known as "species sanitation" is one method for controlling vectors and eliminating P. vivax [15]. This method provides prevention without relying on the numerous issues and difficulties associated with diagnosis and treatment or the limitations of insecticidal methods.
Drug Resistance in the Malaria Parasite: A Threat to the Eradication of Malaria
It is very concerning that antimalarial drug resistance is steadily growing and spreading [30]. Additionally, it puts attempts to manage and eradicate malaria at risk [133]. P. vivax is currently known to be resistant to antimalarial drugs [87]. Additionally, pharmacological interactions that lead to cross-resistance between drugs with the same chemical family or similar modes of action can also be blamed for the worsening of antimalarial drug resistance [37]. There have been numerous reports of P. vivax resistance to chloroquine in endemic regions [43].
CQ resistance appears to have spread globally, based on the genetics of P. vivax [93] Numerous chloroquine and antifolate resistance-related mutations were discovered in P. vivax samples, including SNP and Pvcrt-o K10-insertion combinations that may indicate chloroquine-resistant P. vivax phenotypes, according to research from southern Thai provinces [139]. Additionally, due to the widespread incidence of P. vivax that is resistant to chloroquine, certain countries have been forced to transition from chloroquine to artemisinin-based combination therapy (ACTs), which has an effect on the use of primaquine as the only antirelapse drug [56, 66]. These include Papua New Guinea, the Solomon Islands, Sudan, Namibia, South Africa, and Vanuatu [22]. Because Plasmodium has developed drug resistance to the available antimalarial drugs, managing and eliminating malaria has thus become increasingly challenging. The evaluation of antimalarial efficacy offers a potential solution to this issue by lowering the chance of failure brought on by parasite resistance to certain therapies.
Despite the fact that primaquine resistance is sometimes mistaken for therapy failure or the inability to eradicate the P. vivax hypnozoite liver stage following the completion of the complete course of medication and the appropriate therapeutic dose [183], primaquine and chloroquine resistance in P. vivax has been well reported [16]. Primaquine treatment failure has been documented in several P. vivax strains, especially those from the Western Pacific, Southeast Asia, South America, and certain regions of Africa [199]. A case report from Ethiopia by [181] shows the failure of primaquine for the treatment of relapsed P. vivax malaria.
RTS, S/AS01 vaccine for falciparum but not for vivax malaria
There is currently no P. vivax vaccine that is widely available, and there will not be any very soon [51]. Children in sub-Saharan Africa and other areas with moderate to high P. falciparum malaria transmission are recommended to receive the malaria vaccine RTS,S/AS01 (RTS,S), which mimics protein-coated infectious sporozoites [205]. Other forms of malaria, such as P. vivax, are not protected against by vaccination. In contrast, the protective antibody responses against malaria sporozoites elicited by RTS,S rely on the neutralizing action of antibodies existing at the time of sporozoite infection [205].
The recommendation is based on the outcomes of a pilot program that has been running in Ghana, Kenya, and Malawi since 2019 and has reached more than 900,000 children [202]. The majority of children and adults will carry parasites that will infect mosquitoes, although because this vaccine does not confer extensive sterile immunity and RTS, S-induced immune responses do not interfere with the infectivity of gametocytes (the transmission stages of Plasmodium). As a result, transmission will not change, maintaining endemicity [205]. The suggested P. falciparum vaccine is ineffective against P. vivax and other types of malaria [14]. Adopting RTS,S would also provide indirect benefits, such as a decrease in malaria-related all-cause hospitalization, which would free up possibly limited health resource allocations for other people in need [47].
Alternative approaches to P. vivax elimination: Tafenoquine for radical cure and implementation of Rapid point-of-care diagnostics for G6PD
The malaria community as a whole recognizes that early diagnosis and treatment are essential to eliminating malaria. The US Food and Drug Administration (FDA, July 2018) and the Australian Therapeutic Goods Administration (TGA), two regulatory bodies, have officially approved the 8-aminoquinoline derivative tafenoquine (TQ) as a revolutionary treatment for P. vivax malaria [89]. As seen by more recent relative increases in the P. vivax/P. falciparum ratios in many coendemic countries, this method has been less successful in controlling P. vivax than P. falciparum. The main causes of this disparity are P. vivax's tendency for relapse and the lack of therapies that are both secure and efficient for the hypnozoite reservoirs. Two recent occurrences show that radical cure and, thus, hypnozoite eradication will be more commonly available. The first is TQ, an 8-aminoquinoline with a long half-life that has been licensed and is being implemented in endemic countries. TQ may provide an alternative to the current treatment options. The ideal alternative would have the following qualities: a shorter treatment period; greater efficacy in hypnozoite clearance; absence of PQ's important side effects, including hemolysis in those with G6PD deficiency; and absence of variance in the parasite's susceptibility (partially contributed by host genetic polymorphisms) [163]. The second also included the introduction of point of care. Rapid point-of-care diagnostics for G6PD are now available, which would make it possible to test for the disease in distant areas and avoid the need to transport patients to more advanced medical facilities for extreme measures.
Conclusions and future directions
Control measures such as mass drug administration, screening, vaccine development, vector control, and treatment campaigns could not affect P. vivax, unlike P. falciparum. In addition, due to the lack of an in vitro continuous culture that maintains the parasite erythrocytic cycle, P. vivax has received less study attention than P. falciparum, which has become a major hurdle. Overall, no genuine chance of eradication is predicted in the next few years unless new tools for lowering malaria transmission are developed (i.e., malaria elimination and eradication).
Therefore, what is next for malaria caused by P. vivax control and elimination? What will be the parasite's future defense strategies?
The study of Plasmodium parasites will benefit from systematic methodologies, which will lead to a major improvement in the fight against malaria. By utilizing further genome-wide sequencing tools, our understanding of Plasmodium biology is expanded, and new study routes are beginning to appear (such as "omics").
The "omics" field has the potential to clarify a number of biological problems. This field enables us to comprehend Plasmodium spp. biology, in particular the dynamics of RNA and protein expression and regulation throughout its complex, multistage life cycle, in host and vector interaction contexts and under varied environmental selective pressures. Comprehensive knowledge about cellular components and biomolecules, such as genes (genomics & epigenomics), RNA (transcriptomics), proteins (proteomics), and metabolites (metabolomics), will be provided by these "omics" methods to biological network dynamics [7].
-
(1)
Genomes & epigenomes:—A significant area of research in Plasmodium genome biology is the identification of genes evolving under selective forces favoring novel alleles or sustaining diversity within populations. Epigenomes to understand transcriptional regulation. Whole genome sequencing (WGS) enables a more thorough examination of an organism's genetic make-up and the discovery of protective antigens. The availability of primary Plasmodium genome sequences has also improved our knowledge of the host and parasite elements that contribute to infection and enabled the identification of potential treatment targets by combining them with animal models of infection to comprehend transcriptional control and use epigenomes.
-
(2)
Studies of P. vivax transcriptomes: transcriptomes to determine mRNA steady state may offer special insights into the biology of this parasite and its distinctions from P. falciparum. Furthermore, a study by Muller et al. [132] found that a number of transcripts implicated in the early infection of the vertebrate host are not immediately recognized as proteins and may be subject to translational repression.
-
(3)
Proteomes of parasite particles and parasite-secreted proteins in plasma, according to [7], create significant amounts of parasite proteins that can be utilized for diagnostic purposes. Proteomics may also examine proteomes and subproteomes simultaneously without needing any prior knowledge of the types of proteins. Large quantities of parasite proteins that can be exploited for diagnosis are produced by parasite particles and parasite-secreted proteins in plasma proteomics. Proteomics also offers a substantial advantage in the search for new target biomolecules since it can concurrently analyze proteomes and subproteomes without needing to know the type of proteins involved. There is also much potential in the study of protein expression, interactions, and alterations. Additionally, [4]’s research revealed 153 proteins from the P. vivax blood stages. A startling discovery was that more than 36% of the parasite proteome was made up of hypothetical proteins.
-
(4)
Using interactomes & Metabolomics’: to comprehend how protein‒protein interactions work, and with the development of metabolomics, it is now able to examine metabolites more easily and predict the chloroquine resistance of infected patients by finding altered pathways and significantly altered metabolites. These studies will offer a crucial direction for the eradication and extinction of malaria. Furthermore, molecular biology knowledge will support the development of rapid diagnostic tests (RDTs) for diagnosis, drug development, monitoring of drug resistance, and improved research into the manufacture of malaria vaccines.
In summary, it is quite likely that new methods for eliminating vivax malaria will be needed, necessitating the creation of high-value products, including vaccinations that prevent transmission, fresh drug combinations to treat chloroquine-resistant strains, and a secure, long-lasting 8-aminoquinoline.
Literature search strategy
This review article was created using published research on P. vivax malaria and malaria in general. Searches were conducted in online public databases such PubMed, Google Scholar, ScienceDirect, Web of Science, and other relevant journals that published reviews on P. vivax to locate published articles for the review. P. vivax-related malaria is researched and documented in these databases. The original research articles and review papers used in all of the studies included in the systematic review were published in English. The duplicate papers were not considered in the systematic review. EndNote version X8 was used to generate the arrangement.
Availability of data and materials
Not applicable for review work.
References
Abate A, Bouyssou I, Mabilotte S, Doderer-Lang C, Dembele L, Menard D, Golassa L. Vivax malaria in Duffy-negative patients shows invariably low asexual parasitaemia: implication towards malaria control in Ethiopia. Malar J. 2022;21:1–10.
Abkallo HM, Tangena J-A, Tang J, Kobayashi N, Inoue M, Zoungrana A, Colegrave N, Culleton R. Within-host competition does not select for virulence in malaria parasites; studies with Plasmodium yoelii. PLoS Pathog. 2015;11:e1004628.
Abreha T, Hwang J, Thriemer K, Tadesse Y, Girma S, Melaku Z, Assef A, Kassa M, Chatfield MD, Landman KZ. Comparison of artemether-lumefantrine and chloroquine with and without primaquine for the treatment of Plasmodium vivax infection in Ethiopia: a randomized controlled trial. PLoS Med. 2017;14:e1002299.
Acharya P, Pallavi R, Chandran S, Dandavate V, Sayeed SK, Rochani A, Acharya J, Middha S, Kochar S, Kochar D. Clinical proteomics of the neglected human malarial parasite Plasmodium vivax. PLoS One. 2011;6:e26623.
Adams JH, Mueller I. The biology of Plasmodium vivax. Cold Spring Harb Perspect Med. 2017;7(9):a025585.
Adapa SR, Taylor RA, Wang C, Thomson-Luque R, Johnson LR, Jiang RHY. Plasmodium vivax readiness to transmit: implication for malaria eradication. BMC Syst Biol. 2019;13:5.
Aggarwal S, Peng WK, Srivastava S. Multi-omics advancements towards Plasmodium vivax malaria diagnosis. Diagnostics (Basel). 2021;11(12):2222.
Ahmad SS, Rahi M, Sharma A. Relapses of Plasmodium vivax malaria threaten disease elimination: time to deploy tafenoquine in India? BMJ Glob Health. 2021;6:e004558.
Almeida AC, Kuehn A, Castro AJ, Vitor-Silva S, Figueiredo EF, Brasil LW, Brito MA, Sampaio VS, Bassat Q, Felger I. High proportions of asymptomatic and submicroscopic Plasmodium vivax infections in a peri-urban area of low transmission in the Brazilian Amazon. Parasit Vectors. 2018;11:1–13.
Almeida GG, Costa PAC, Araujo MdS, Gomes GR, Carvalho AF, Figueiredo MM, Pereira DB, Tada MS, Medeiros JF, Soares IdS. Asymptomatic Plasmodium vivax malaria in the Brazilian Amazon: Submicroscopic parasitemic blood infects Nyssorhynchus darlingi. PLoS Neglected Trop Dis. 2021;15:e0009077.
Angrisano F, Robinson LJ. Plasmodium vivax–How hidden reservoirs hinder global malaria elimination. Parasitol Int. 2022;87:102526.
Arévalo-Pinzón G, Bermúdez M, Hernández D, Curtidor H, Patarroyo MA. Plasmodium vivax ligand-receptor interaction: PvAMA-1 domain I contains the minimal regions for specific interaction with CD71+ reticulocytes. Sci Rep. 2017;7:1–13.
Arnott A, Mueller I, Ramsland PA, Siba PM, Reeder JC, Barry AE. Global population structure of the genes encoding the malaria vaccine candidate, Plasmodium vivax apical membrane antigen 1 (Pv AMA1). PLoS Negl Trop Dis. 2013;7:e2506.
Arora N, Anbalagan LC, Pannu AK. Towards eradication of malaria: is the WHO’s RTS, S/AS01 vaccination effective enough? Risk Manag Healthcare Policy. 2021;14:1033.
Asih PB, Syafruddin D, Baird JK. Challenges in the control and elimination of Plasmodium vivax malaria. In: Towards malaria elimination-A leap forward. IntechOpen; 2018.
Assemie A. Malaria prevalence and distribution of plasmodium species in Southern Region of Ethiopia. J Parasitol Res. 2022;2022:5665660.
Auburn S, Cheng Q, Marfurt J, Price RN. The changing epidemiology of Plasmodium vivax: insights from conventional and novel surveillance tools. PLoS Med. 2021;18:e1003560.
Auburn S, Getachew S, Pearson RD, Amato R, Miotto O, Trimarsanto H, Zhu SJ, Rumaseb A, Marfurt J, Noviyanti R, et al. Genomic analysis of Plasmodium vivax in Southern Ethiopia reveals selective pressures in multiple parasite mechanisms. J Infect Dis. 2019;220:1738–49.
Badmos AO, Alaran AJ, Adebisi YA, Bouaddi O, Onibon Z, Dada A, Lin X, Lucero-Prisno DE. What sub-Saharan African countries can learn from malaria elimination in China. Trop Med Health. 2021;49:86.
Baird JK. 8-Aminoquinoline therapy for latent malaria. Clin Microbiol Rev. 2019 Jul 31;32(4):e00011–19. https://doi.org/10.1128/CMR.00011-19. PMID: 31366609; PMCID: PMC6750137.
Baird, J.K. (2022). African Plasmodium vivax malaria improbably rare or benign. Trends in Parasitology.
Baird JK, Valecha N, Duparc S, White NJ, Price RN. Diagnosis and treatment of Plasmodium vivax malaria. Am J Trop Med Hyg. 2016;95:35–51.
Bantuchai S, Imad H, Nguitragool W. Plasmodium vivax gametocytes and transmission. Parasitol Int. 2022;87:102497.
Barber BE, Rajahram GS, Grigg MJ, William T, Anstey NM. World Malaria Report: time to acknowledge Plasmodium knowlesi malaria. Malar J. 2017;6:1–3.
Bassat Q, Velarde M, Mueller I, Lin J, Leslie T, Wongsrichanalai C, Baird JK. Key knowledge gaps for Plasmodium vivax control and elimination. Am J Trop Med Hyg. 2016;95:62.
Basso LG, Rodrigues RZ, Naal RM, Costa-Filho AJ. Effects of the antimalarial drug primaquine on the dynamic structure of lipid model membranes. Biochim Biophys Acta. 2011;1808:55–64.
Battle KE, Baird JK. The global burden of Plasmodium vivax malaria is obscure and insidious. PLoS Med. 2021;18:e1003799.
Blanford JI, Blanford S, Crane RG, Mann ME, Paaijmans KP, Schreiber KV, Thomas MB. Implications of temperature variation for malaria parasite development across Africa. Sci Rep. 2013;3:1–11.
Edith Christiane B, Sodiomon Bienvenu S. Inherited disorders of hemoglobin and Plasmodium falciparum malaria. In: Osaro E, Anjana M, editors. Human blood group systems and haemoglobinopathies. Rijeka: IntechOpen: 2020. p. Ch. 1.
Bourgard C, Albrecht L, Kayano A, Sunnerhagen P, Costa FTM. Plasmodium vivax biology: insights provided by genomics, transcriptomics and proteomics. Front Cell Infect Microbiol. 2018;8:34.
Braga CB, Martins AC, Cayotopa AD, Klein WW, Schlosser AR, da Silva AF, de Souza MN, Andrade BW, Filgueira-Júnior JA, Pinto Wde J, et al. Side effects of chloroquine and primaquine and symptom reduction in malaria endemic area (Mâncio Lima, Acre, Brazil). Interdiscip Perspect Infect Dis. 2015;2015:346853.
Briquet S, Marinach C, Silvie O, Vaquero C. Preparing for transmission: gene regulation in plasmodium sporozoites. Front Cell Infect Microbiol. 2020;10:618430.
Bykersma A. The new zoonotic malaria: Plasmodium cynomolgi. Trop Med Infect Dis. 2021;6:46.
Bylicka-Szczepanowska E, Korzeniewski K. Asymptomatic malaria infections in the time of COVID-19 Pandemic: experience from the Central African Republic. Int J Environ Res Public Health. 2022;19(6):3544.
Camarda G, Jirawatcharadech P, Priestley RS, Saif A, March S, Wong MH, Leung S, Miller AB, Baker DA, Alano P. Antimalarial activity of primaquine operates via a two-step biochemical relay. Nat Commun. 2019;10:1–9.
Camargo-Ayala PA, Garzón-Ospina D, Moreno-Pérez DA, Ricaurte-Contreras LA, Noya O, Patarroyo MA. On the evolution and function of Plasmodium vivax reticulocyte binding surface antigen (pvrbsa). Front Genet. 2018;9:372.
Capela R, Moreira R, Lopes F. An overview of drug resistance in protozoal diseases. Int J Mol Sci. 2019;20:5748.
Caputo A, Garavelli PL. Climate, environment and transmission of malaria. Infez Med. 2016;2:93–104.
Carvalho BO, Lopes SC, Nogueira PA, Orlandi PP, Bargieri DY, Blanco YC, Mamoni R, Leite JA, Rodrigues MM, Soares IS. On the cytoadhesion of Plasmodium vivax–infected erythrocytes. J Infect Dis. 2010;202:638–47.
Chan LJ, Dietrich MH, Nguitragool W, Tham WH. Plasmodium vivax Reticulocyte Binding Proteins for invasion into reticulocytes. Cell Microbiol. 2020;22:e13110.
Chu CS, White NJ. The prevention and treatment of Plasmodium vivax malaria. PLoS Med. 2021;18:e1003561.
Clark MA, Kanjee U, Rangel GW, Chery L, Mascarenhas A, Gomes E, Rathod PK, Brugnara C, Ferreira MU, Duraisingh MT. Plasmodium vivax infection compromises reticulocyte stability. Nat Commun. 2021;12:1629.
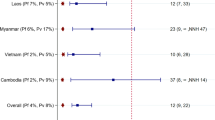
Commons RJ, Simpson JA, Thriemer K, Humphreys GS, Abreha T, Alemu SG, Añez A, Anstey NM, Awab GR, Baird JK. The effect of chloroquine dose and primaquine on Plasmodium vivax recurrence: a WorldWide Antimalarial Resistance Network systematic review and individual patient pooled meta-analysis. Lancet Infect Dis. 2018;18:1025–34.
Conn JE, Grillet, ME, Correa M, Sallum MAM. (2018). Malaria transmission in South America—present status and prospects for elimination. Towards malaria elimination—a leap forward London: InTech, 281–313.
Corder RM, de Lima AC, Khoury DS, Docken SS, Davenport MP, Ferreira MU. Quantifying and preventing Plasmodium vivax recurrences in primaquine-untreated pregnant women: an observational and modeling study in Brazil. PLoS Negl Trop Dis. 2020;14:e0008526.
Cui L, et al. Elimination of Plasmodium vivax malaria: problems and solutions. In: Rodriguez-Morales AJ, editor. Current topics and emerging issues in malaria elimination. London: IntechOpen; 2021. https://doi.org/10.5772/intechopen.96604.
D’Souza J, Nderitu D. Ethical considerations for introducing RTS, S/AS01 in countries with moderate to high Plasmodium falciparum malaria transmission. Lancet Glob Health. 2021;9:e1642–3.
Daniels RF, Rice BL, Daniels NM, Volkman SK, Hartl DL. The utility of genomic data for Plasmodium vivax population surveillance. Pathogens Global Health. 2015;109:153–61.
de Jong RM, Tebeje SK, Meerstein-Kessel L, Tadesse FG, Jore MM, Stone W, Bousema T. Immunity against sexual stage Plasmodium falciparum and Plasmodium vivax parasites. Immunol Rev. 2020;293:190–215.
de Pina-Costa A, Silvino ACR, Dos Santos EM, Pedro RS, Moreira J, Umana GL, da Silva ADT, da Rosa Santos OHL, de Deus Henriques KM, Daniel-Ribeiro CT. Increased primaquine total dose prevents Plasmodium vivax relapses in patients with impaired CYP2D6 activity: report of three cases. Malar J. 2021;20:1–6.
De SL, Ntumngia FB, Nicholas J, Adams JH. Progress towards the development of a Plasmodium vivax vaccine. Expert Rev Vaccines. 2021;20:97–112.
Devine A, Parmiter M, Chu CS, Bancone G, Nosten F, Price RN, Lubell Y, Yeung S. Using G6PD tests to enable the safe treatment of Plasmodium vivax infections with primaquine on the Thailand-Myanmar border: a cost-effectiveness analysis. PLoS Negl Trop Dis. 2017;11:e0005602.
Diez Benavente E, Ward Z, Chan W, Mohareb FR, Sutherland CJ, Roper C, Campino S, Clark TG. Genomic variation in Plasmodium vivax malaria reveals regions under selective pressure. PLoS One. 2017;12:e0177134.
Ding XC, Ade MP, Baird JK, Cheng Q, Cunningham J, Dhorda M, Drakeley C, Felger I, Gamboa D, Harbers M. Defining the next generation of Plasmodium vivax diagnostic tests for control and elimination: target product profiles. PLoS Negl Trop Dis. 2017;11:e0005516.
Domingo GJ, Satyagraha AW, Anvikar A, Baird K, Bancone G, Bansil P, Carter N, Cheng Q, Culpepper J, Eziefula C, et al. G6PD testing in support of treatment and elimination of malaria: recommendations for evaluation of G6PD tests. Malar J. 2013;12:391.
Douglas NM, Anstey NM, Angus BJ, Nosten F, Price RN. Artemisinin combination therapy for vivax malaria. Lancet Infect Dis. 2010;10:405–16.
Duah NO, Matrevi SA, Quashie NB, Abuaku B, Koram KA. Genetic diversity of Plasmodium falciparum isolates from uncomplicated malaria cases in Ghana over a decade. Parasit Vectors. 2016;9:416.
Duffy PE, Acharya P, Oleinikov AV. (2014). Journal: Encyclopedia of Malaria, 2014, 1–13. Journal: Encyclopedia of Malaria, 1–13.
Durnez L, Coosemans M. Residual transmission of malaria: an old issue for new approaches. In: Anopheles mosquitoes: new insights into malaria vectors/Manguin, Sylvie; 2013. p. 671–704.
Engel N, Ghergu C, Matin MA, Kibria MG, Thriemer K, Price RN, Ding XC, Howes RE, Ley B, Incardona S. Implementing radical cure diagnostics for malaria: user perspectives on G6PD testing in Bangladesh. Malar J. 2021;20:1–12.
Escalante AA, Cepeda AS, Pacheco MA. Why Plasmodium vivax and Plasmodium falciparum are so different? A tale of two clades and their species diversities. Malar J. 2022;21:1–19.
Fernandez-Becerra C, Bernabeu M, Castellanos A, Correa BR, Obadia T, Ramirez M, Rui E, Hentzschel F, López-Montañés M, Ayllon-Hermida A. Plasmodium vivax spleen-dependent genes encode antigens associated with cytoadhesion and clinical protection. Proc Natl Acad Sci. 2020;117:13056–65.
Ferreira MU, Corder RM, Johansen IC, Kattenberg JH, Moreno M, Rosas-Aguirre A, Ladeia-Andrade S, Conn JE, Llanos-Cuentas A, Gamboa D. Relative contribution of low-density and asymptomatic infections to Plasmodium vivax transmission in the Amazon: pooled analysis of individual participant data from population-based cross-sectional surveys. Lancet Regional Health-Americas. 2022;9:100169.
Ferreira MU, de Oliveira TC. Challenges for Plasmodium vivax malaria elimination in the genomics era. Pathogens Glob Health. 2015;109:89–90.
Ferreira MU, Gamboa D, Torres K, Rodriguez-Ferrucci H, Soto-Calle VE, Pardo K, Fontoura PS, Tomko SS, Gazzinelli RT, Conn JE. Evidence-based malaria control and elimination in the Amazon: input from the International Center of excellence in malaria research network in Peru and Brazil. Am J Trop Med Hyg. 2022;107:160–7.
Ferreira MU, Nobrega de Sousa T, Rangel GW, Johansen IC, Corder RM, Ladeia-Andrade S, Gil JP. Monitoring Plasmodium vivax resistance to antimalarials: Persisting challenges and future directions. Int J Parasitol Drugs Drug Resist. 2021;15:9–24.
File T, Dinka H, Golassa L. A retrospective analysis on the transmission of Plasmodium falciparum and Plasmodium vivax: the case of Adama City, East Shoa Zone, Oromia. Ethiopia Malaria Journal. 2019;18:193.
Finney M, McKenzie BA, Rabaovola B, Sutcliffe A, Dotson E, Zohdy S. Widespread zoophagy and detection of Plasmodium spp. in Anopheles mosquitoes in southeastern Madagascar. Malar J. 2021;20:1–12.
Fischer L, Gültekin N, Kaelin MB, Fehr J, Schlagenhauf P. Rising temperature and its impact on receptivity to malaria transmission in Europe: a systematic review. Travel Med Infect Dis. 2020;36:101815.
Fontoura PS, Finco BF, Lima NF, de Carvalho Jr JF, Vinetz JM, Castro MC, Ferreira MU. Reactive case detection for Plasmodium vivax malaria elimination in rural Amazonia. PLoS Negl Trop Dis. 2016;10:e0005221.
Gari T, Solomon T, Lindtjørn B. Older children are at increased risk of Plasmodium vivax in south-central Ethiopia: a cohort study. Malar J. 2021;20:251.
Garzón-Ospina D, Buitrago SP, Ramos AE, Patarroyo MA. Identifying potential Plasmodium vivax sporozoite stage vaccine candidates: an analysis of genetic diversity and natural selection. Front Genet. 2018;9:10.
Gilder ME, Hanpithakphong W, Hoglund RM, Tarning J, Win HH, Hilda N, Chu CS, Bancone G, Carrara VI, Singhasivanon P, et al. Primaquine pharmacokinetics in lactating women and breastfed infant exposures. Clin Infect Dis. 2018;67:1000–7.
Giovanella F, Ferreira GK, PRÁ SDD, Carvalho-Silva M, Gomes LM, Scaini G, Goncalves RC, Michels M, Galant LS, Longaretti LM. Effects of primaquine and chloroquine on oxidative stress parameters in rats. An Acad Bras Cienc. 2015;87:1487–96.
Golassa L, Amenga-Etego L, Lo E, Amambua-Ngwa A. The biology of unconventional invasion of Duffy-negative reticulocytes by Plasmodium vivax and its implication in malaria epidemiology and public health. Malar J. 2020;19:1–10.
Gopi G, Behera SM, Behera P. Tafenoquine: a breakthrough drug for radical cure and elimination of Malaria. Exploratory Res Hypothesis Med. 2019;4:29–34.
Grillet ME, Moreno JE, Hernández-Villena JV, Vincenti-González MF, Noya O, Tami A, Paniz-Mondolfi A, Llewellyn M, Lowe R, Escalante AA. Malaria in Southern Venezuela: the hottest hotspot in Latin America. PLoS Negl Trop Dis. 2021;15:e0008211.
Gualdrón-López M, Flannery EL, Kangwanrangsan N, Chuenchob V, Fernandez-Orth D, Segui-Barber J, Royo F, Falcón-Pérez JM, Fernandez-Becerra C, Lacerda MV. Characterization of Plasmodium vivax proteins in plasma-derived exosomes from malaria-infected liver-chimeric humanized mice. Front Microbiol. 2018;9:1271.
Gunalan K, Niangaly A, Thera MA, Doumbo OK, Miller LH. Plasmodium vivax infections of Duffy-negative erythrocytes: historically undetected or a recent adaptation? Trends Parasitol. 2018;34:420–9.
Gupta S, Singh S, Popovici J, Roesch C, Shakri AR, Guillotte-Blisnick M, Huon C, Menard D, Chitnis CE. Targeting a reticulocyte binding protein and Duffy binding protein to inhibit reticulocyte invasion by Plasmodium vivax. Sci Rep. 2018;8:10511.
Gural N, Mancio-Silva L, Miller AB, Galstian A, Butty VL, Levine SS, Patrapuvich R, Desai SP, Mikolajczak SA, Kappe SH. In vitro culture, drug sensitivity, and transcriptome of Plasmodium vivax hypnozoites. Cell Host Microbe. 2018;23(395–406):e394.
Haileselassie W, Parker DM, Taye B, David RE, Zemene E, Lee M-C, Zhong D, Zhou G, Alemu T, Tadele G. Burden of malaria, impact of interventions and climate variability in Western Ethiopia: an area with large irrigation based farming. BMC Public Health. 2022;22:1–11.
Haiyambo DH, Aleksenko L, Mumbengegwi D, Bock R, Uusiku P, Malleret B, Rénia L, Quaye IK. Children with Plasmodium vivax infection previously observed in Namibia, were Duffy negative and carried a c. 136G> A mutation. BMC Infect Dis. 2021;21:1–6.
Hammer H, Schmidt F, Marx-Stoelting P, Pötz O, Braeuning A. Cross-species analysis of hepatic cytochrome P450 and transport protein expression. Arch Toxicol. 2021;95:117–33.
Hanboonkunupakarn B, White NJ. Advances and roadblocks in the treatment of malaria. Br J Clin Pharmacol. 2022;88:374–82.
He W-Q, Karl S, White MT, Nguitragool W, Monteiro W, Kuehn A, Gruszczyk J, França CT, Sattabongkot J, Lacerda MV. Antibodies to Plasmodium vivax reticulocyte binding protein 2b are associated with protection against Plasmodium vivax malaria in populations living in low malaria transmission regions of Brazil and Thailand. PLoS Negl Trop Dis. 2019;13:e0007596.
Heidari A, Keshavarz H. The drug resistance of Plasmodium falciparum and Plasmodium vivax in Iran: a review article. Iran J Parasitol. 2021;16:173.
Hemingway J, Shretta R, Wells TN, Bell D, Djimdé AA, Achee N, Qi G. Tools and strategies for malaria control and elimination: what do we need to achieve a grand convergence in malaria? PLoS Biol. 2016;14:e1002380.
Hounkpatin AB, Kreidenweiss A, Held J. Clinical utility of tafenoquine in the prevention of relapse of Plasmodium vivax malaria: a review on the mode of action and emerging trial data. Infect Drug Resist. 2019;12:553–70.
Howes RE, Battle KE, Mendis KN, Smith DL, Cibulskis RE, Baird JK, Hay SI. Global Epidemiology of Plasmodium vivax. Am J Trop Med Hyg. 2016;95:15–34.
Huang F, Li S, Tian P, Pu LJS, Cui Y, Liu H, Yang L, Bi DY. Genetic polymorphisms in genes associated with drug resistance in Plasmodium vivax parasites from northeastern Myanmar. Malar J. 2022;21:66.
Huber JH, Koepfli C, España G, Nekkab N, White MT, Alex Perkins T. How radical is radical cure? Site-specific biases in clinical trials underestimate the effect of radical cure on Plasmodium vivax hypnozoites. Malar J. 2021;20:1–15.
Ippolito MM, Moser KA, Kabuya J-BB, Cunningham C, Juliano JJ. Antimalarial drug resistance and implications for the WHO global technical strategy. Curr Epidemiol Rep. 2021;8:46–62.
Jennison C, Arnott A, Tessier N, Tavul L, Koepfli C, Felger I, Siba PM, Reeder JC, Bahlo M, Mueller I. Plasmodium vivax populations are more genetically diverse and less structured than sympatric Plasmodium falciparum populations. PLoS Negl Trop Dis. 2015;9:e0003634.
Kanjee U, Rangel GW, Clark MA, Duraisingh MT. Molecular and cellular interactions defining the tropism of Plasmodium vivax for reticulocytes. Curr Opin Microbiol. 2018;46:109–15.
Kepple D, Ford A, Little E, Kolesar G, Abagero BR, Blackwell AN, De Silva Indrasekara S, Yewhalaw D, Lo E. From Genes to Biomarkers: Understanding the biology of malaria gametocytes and their detection. In: Çalışkan M, editor. Genetic polymorphisms - new insights [Internet]. London: IntechOpen; 2021 [cited 2022 Nov 30]. Available from: https://www.intechopen.com/chapters/78331. https://doi.org/10.5772/intechopen.99364.
Kepple D, Pestana K, Tomida J, Abebe A, Golassa L, Lo E. Alternative invasion mechanisms and host immune response to Plasmodium vivax malaria: trends and future directions. Microorganisms. 2021;9:15.
Khammanee T, Sawangjaroen N, Buncherd H, Tun AW, Thanapongpichat S. Prevalence of Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency among malaria patients in Southern Thailand: 8 years retrospective study. Korean J Parasitol. 2022;60:15.
Kitchakarn S, Lek D, Thol S, Hok C, Saejeng A, Huy R, Chinanonwait N, Thimasarn K, Wongsrichanalai C. Implementation of G6PD testing and primaquine for Plasmodium vivax radical cure: operational perspectives from Thailand and Cambodia. WHO South East Asia J Public Health. 2017;6:60–8.
Koepfli C, Nguitragool W, de Almeida ACG, Kuehn A, Waltmann A, Kattenberg E, Ome-Kaius M, Rarau P, Obadia T, Kazura J. Identification of the asymptomatic gametocyte reservoir under different transmission intensities. Plasmodium falciparum and Plasmodium vivaxoS Negl Trop Dis. 2021;15:e0009672.
Lacerda MVG, Llanos-Cuentas A, Krudsood S, Lon C, Saunders DL, Mohammed R, Yilma D, Batista Pereira D, Espino FEJ, Mia RZ, et al. Single-dose tafenoquine to prevent relapse of Plasmodium vivax Malaria. N Engl J Med. 2019;380:215–28.
Laporta GZ, Ilacqua RC, Bergo ES, Chaves LS, Rodovalho SR, Moresco GG, Figueira EA, Massad E, de Oliveira TM, Bickersmith SA. Malaria transmission in landscapes with varying deforestation levels and timelines in the Amazon: a longitudinal spatiotemporal study. Sci Rep. 2021;11:1–14.
Larson B. Origin of two most virulent agents of human malaria: Plasmodium falciparum and Plasmodium vivax. In: Fyson HK, editor. Malaria. Rijeka: IntechOpen; 2019. p. Ch. 1.
Lindblade KA, Steinhardt L, Samuels A, Kachur SP, Slutsker L. The silent threat: asymptomatic parasitemia and malaria transmission. Expert Rev Anti Infect Ther. 2013;11:623–39.
Lee W-C, Cheong FW, Amir A, Lai MY, Tan JH, Phang WK, Shahari S, Lau Y-L. Plasmodium knowlesi: the game changer for malaria eradication. Malar J. 2022;21:1–24.
Lee W-C, Russell B, Rénia L. Sticking for a cause: the falciparum malaria parasites cytoadherence paradigm. Front Immunol. 2019;10:1444.
Lempang MEP, Dewayanti FK, Syahrani L, Permana DH, Malaka R, Asih PBS, Syafruddin D. Primate malaria: an emerging challenge of zoonotic malaria in Indonesia. One Health (Amsterdam, Netherlands). 2022;14:100389.
Leong YW, Lee EQH, Rénia L, Malleret B. Rodent malaria erythrocyte preference assessment by an Ex Vivo Tropism Assay. Front Cell Infect Microbiol. 2021;11:680136.
Ley B, Thriemer K, Jaswal J, Poirot E, Alam MS, Phru CS, Khan WA, Dysoley L, Qi G, Kheong CC, et al. Barriers to routine G6PD testing prior to treatment with Primaquine. Malar J. 2017;16:329.
Lingani M, Zango SH, Valéa I, Sanou M, Ouoba S, Samadoulougou S, Robert A, Tinto H, Dramaix M, Donnen P. Prevalence and risk factors of malaria among first antenatal care attendees in rural Burkina Faso. Trop Med Health. 2022;50:1–8.
Llanos-Cuentas A, Manrrique P, Rosas-Aguirre A, Herrera S, Hsiang MS. Tafenoquine for the treatment of Plasmodium vivax malaria. Expert Opin Pharmacother. 2022;23:759–68.
Lo E, Russo G, Pestana K, Kepple D, Abagero BR, Dongho GBD, Gunalan K, Miller LH, Hamid MMA, Yewhalaw D. Contrasting epidemiology and genetic variation of Plasmodium vivax infecting Duffy-negative individuals across Africa. Int J Infect Dis. 2021;108:63–71.
Lo E, Zhong D, Raya B, Pestana K, Koepfli C, Lee M-C, Yewhalaw D, Yan G. Prevalence and distribution of G6PD deficiency: implication for the use of primaquine in malaria treatment in Ethiopia. Malar J. 2019;18:1–10.
Lo E, Zhou G, Oo W, Afrane Y, Githeko A, Yan G. Low parasitemia in submicroscopic infections significantly impacts malaria diagnostic sensitivity in the highlands of Western Kenya. PLoS One. 2015;10:e0121763.
Loeffel M, Ross A. The relative impact of interventions on sympatric Plasmodium vivax and Plasmodium falciparum malaria: A systematic review. PLoS Negl Trop Dis. 2022;16:e0010541.
Luo Z, Sullivan SA, Carlton JM. The biology of Plasmodium vivax explored through genomics. Ann N Y Acad Sci. 2015;1342:53–61.
Lyon B, Dinku T, Raman A, Thomson MC. Temperature suitability for malaria climbing the Ethiopian Highlands. Environ Res Lett. 2017;12:064015.
Mac Donald-Ottevanger MS, Adhin MR, Jitan JK, Bretas G, Vreden SG. Primaquine double dose for 7 days is inferior to single-dose treatment for 14 days in preventing Plasmodium vivax recurrent episodes in Suriname. Infect Drug Resist. 2018;11:3–8.
Magliocco G, Desmeules J, Matthey A, Quirós-Guerrero LM, Bararpour N, Joye T, Marcourt L, Queiroz EF, Wolfender JL, Gloor Y. Metabolomics reveals biomarkers in human urine and plasma to predict cytochrome P450 2D6 (CYP2D6) activity. Br J Pharmacol. 2021;178:4708–25.
Malleret B, Li A, Zhang R, Tan KS, Suwanarusk R, Claser C, Cho JS, Koh EGL, Chu CS, Pukrittayakamee S. Plasmodium vivax: restricted tropism and rapid remodeling of CD71-positive reticulocytes. Blood. 2015;125:1314–24.
Malvy D, Torrentino-Madamet M, l'Ollivier C, Receveur M-C, Jeddi F, Delhaes L, Piarroux R, Millet P, Pradines B. Plasmodium falciparum recrudescence two years after treatment of an uncomplicated infection without return to an area where malaria is endemic. Antimicrob Agents Chemother. 2018;62:e01892–01817.
Marcsisin SR, Reichard G, Pybus BS. Primaquine pharmacology in the context of CYP 2D6 pharmacogenomics: current state of the art. Pharmacol Ther. 2016;161:1–10.
Marín-Menéndez A, Bardají A, Martínez-Espinosa FE, Bôtto-Menezes C, Lacerda MV, Ortiz J, Cisteró P, Piqueras M, Felger I, Müeller I. Rosetting in Plasmodium vivax: a cytoadhesion phenotype associated with anaemia. PLoS Negl Trop Dis. 2013;7:e2155.
Mehlotra RK, Gaedigk A, Howes RE, Rakotomanga TA, Ratsimbasoa AC, Zimmerman PA. CYP2D6 genetic variation and its implication for vivax malaria treatment in Madagascar. Front Pharmacol. 2021;12:654054.
Menkin-Smith L, Winders WT. Plasmodium Vivax Malaria. [Updated 2022 Jul 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538333/.
Mikolajczak SA, Vaughan AM, Kangwanrangsan N, Roobsoong W, Fishbaugher M, Yimamnuaychok N, Rezakhani N, Lakshmanan V, Singh N, Kaushansky A. Plasmodium vivax liver stage development and hypnozoite persistence in human liver-chimeric mice. Cell Host Microbe. 2015;17:526–35.
Milligan R, Daher A, Graves PM. Primaquine at alternative dosing schedules for preventing relapse in people with Plasmodium vivax malaria. Cochrane Database Syst Rev. 2019;7:2656.
Minter M, Nielsen ES, Blyth C, Bertola LD, Kantar MB, Morales HE, Orland C, Segelbacher G, Leigh DM. What is genetic diversity and why does it matter? 2021.
Mironova V, Shartova N, Beljaev A, Varentsov M, Grishchenko M. Effects of climate change and heterogeneity of local climates on the development of malaria parasite (Plasmodium vivax) in Moscow megacity region. Int J Environ Res Public Health. 2019;16:694.
Mitali M, Vikash Kumar M, Varsha K, Sushil Kumar K. Molecular approaches for malaria therapy. In: Rajeev KT, editor. Plasmodium species and drug resistance. Rijeka: IntechOpen; 2021. p. Ch. 8.
Monroe A, Williams NA, Ogoma S, Karema C, Okumu F. Reflections on the 2021 World Malaria Report and the future of malaria control. Malar J. 2022;21:154.
Muller I, Jex AR, Kappe SH, Mikolajczak SA, Sattabongkot J, Patrapuvich R, Lindner S, Flannery EL, Koepfli C, Ansell B, Lerch A. Transcriptome and histone epigenome of Plasmodium vivax salivary-gland sporozoites point to tight regulatory control and mechanisms for liver-stage differentiation in relapsing malaria. Int J Parasitol. 2019;49(7):501–13.
Myers-Hansen JL, Abuaku B, Oyebola MK, Mensah BA, Ahorlu C, Wilson MD, Awandare G, Koram KA, Ngwa AA, Ghansah A. Assessment of antimalarial drug resistant markers in asymptomatic Plasmodium falciparum infections after 4 years of indoor residual spraying in Northern Ghana. PLoS One. 2020;15:e0233478.
Naing C, Htet NH, Aye SN, Aung HH, Tanner M, Whittaker MA. Detection of asymptomatic malaria in Asian countries: a meta-analysis of diagnostic accuracy. Malar J. 2022;21:50.
Nascimento JR, Brito-Sousa JD, Almeida ACG, Melo MM, Costa MRF, Barbosa LRA, Ramos RN, Silva-Neto AV, da Silva Balieiro PC, Figueiredo EFG. Prevalence of glucose 6-phosphate dehydrogenase deficiency in highly malaria-endemic municipalities in the Brazilian Amazon: A region-wide screening study. Lancet Regional Health-Americas. 2022;12:100273.
Nekkab N, Lana R, Lacerda M, Obadia T, Siqueira A, Monteiro W, Villela D, Mueller I, White M. Estimated impact of tafenoquine for Plasmodium vivax control and elimination in Brazil: A modelling study. PLoS Med. 2021;18:e1003535.
Ngotho P, Soares AB, Hentzschel F, Achcar F, Bertuccini L, Marti M. Revisiting gametocyte biology in malaria parasites. FEMS Microbiol Rev. 2019;43:401–14.
Nguitragool W, Mueller I, Kumpitak C, Saeseu T, Bantuchai S, Yorsaeng R, Yimsamran S, Maneeboonyang W, Sa-Angchai P, Chaimungkun W. Very high carriage of gametocytes in asymptomatic low-density Plasmodium falciparum and Plasmodium vivax infections in western Thailand. Parasit Vectors. 2017;10:1–9.
Noisang C, Prosser C, Meyer W, Chemoh W, Ellis J, Sawangjaroen N, Lee R. Molecular detection of drug resistant malaria in Southern Thailand. Malar J. 2019;18:275.
Noviyanti R, Carey-Ewend K, Trianty L, Parobek C, Puspitasari AM, Balasubramanian S, Park Z, Hathaway N, Utami RA, Soebianto S. Hypnozoite depletion in successive Plasmodium vivax relapses. PLoS Neglect Trop Dis. 2022;16:e0010648.
Obaldia N 3rd, Meibalan E, Sa JM, Ma S, Clark MA, Mejia P, Moraes Barros RR, Otero W, Ferreira MU, Mitchell JR, Milner DA, Huttenhower C, Wirth DF, Duraisingh MT, Wellems TE, Marti M. Bone marrow is a major parasite reservoir in Plasmodium vivax Infection. mBio. 2018;9(3):e00625–18. https://doi.org/10.1128/mBio.00625-18.
Obaldía N, Barahona I, Lasso J, Avila M, Quijada M, Nuñez M, Marti M. Comparison of PvLAP5 and Pvs25 qRT-PCR assays for the detection of Plasmodium vivax gametocytes in field samples preserved at ambient temperature from remote malaria endemic regions of Panama. PLoS Negl Trop Dis. 2022;16:e0010327.
Oduma CO, Koepfli C. Plasmodium falciparum and Plasmodium vivax Adjust investment in transmission in response to change in transmission intensity: a review of the current state of research. Front Cellular Infect Microbiol. 2021;11:1237.
Oladipo HJ, Tajudeen YA, Oladunjoye IO, Yusuff SI, Yusuf RO, Oluwaseyi EM, AbdulBasit MO, Adebisi YA, El-Sherbini MS. Increasing challenges of malaria control in sub-Saharan Africa: Priorities for public health research and policymakers. Ann Med Surg. 2022;81:104366.
Olliaro PL, Barnwell JW, Barry A, Mendis K, Mueller I, Reeder JC, Shanks GD, Snounou G, Wongsrichanalai C. Implications of Plasmodium vivax biology for control, elimination, and research. Am J Trop Med Hyg. 2016;95:4–14.
Ome-Kaius M, Kattenberg JH, Zaloumis S, Siba M, Kiniboro B, Jally S, Razook Z, Mantila D, Sui D, Ginny J. Differential impact of malaria control interventions on Plasmodium falciparum and Plasmodium vivax infections in young Papua New Guinean children. BMC Med. 2019;17:1–13.
Park JW. Changing Transmission Pattern of Plasmodium vivax malaria in the Republic of Korea: relationship with climate change. Environ Health Toxicol. 2011;26:e2011001. https://doi.org/10.5620/eht.2011.26.e2011001. Epub 2011 Mar 8.
Pasini EM, Kocken CH. Parasite-host interaction and pathophysiology studies of the human relapsing malarias Plasmodium vivax and Plasmodium ovale infections in non-human primates. Front Cell Infect Microbiol. 2021;10:614122.
Patankar S, Sharma S, Rathod PK, Duraisingh MT. Malaria in India: The need for new targets for diagnosis and detection of Plasmodium vivax. Proteomics Clin Appl. 2018;12:e1700024.
Paton DG, Childs LM, Itoe MA, Holmdahl IE, Buckee CO, Catteruccia F. Exposing Anopheles mosquitoes to antimalarials blocks Plasmodium parasite transmission. Nature. 2019;567:239–43.
Patouillard E, Griffin J, Bhatt S, Ghani A, Cibulskis R. Global investment targets for malaria control and elimination between 2016 and 2030. BMJ Glob Health. 2017;2:e000176.
Pett H, Bradley J, Okebe J, Dicko A, Tiono AB, Gonçalves BP, Stone W, Chen I, Lanke K, Neuvonen M. CYP2D6 polymorphisms and the safety and gametocytocidal activity of single-dose primaquine for Plasmodium falciparum. Antimicrob Agents Chemother. 2019;63:e00538-e519.
Pham Vinh T. Epidemiology of Plasmodium vivax malaria in Central Vietnam. UCL-Université Catholique de Louvain; 2018.
Phyo AP, Dahal P, Mayxay M, Ashley EA. Clinical impact of vivax malaria: a collection review. PLoS Med. 2022;19:e1003890.
Popovici J, Roesch C, Rougeron V. The enigmatic mechanisms by which Plasmodium vivax infects Duffy-negative individuals. PLoS Pathog. 2020;16:e1008258.
Potter BM, Xie LH, Vuong C, Zhang J, Zhang P, Duan D, Luong T-LT, Bandara Herath H, Dhammika Nanayakkara N, Tekwani BL. Differential CYP 2D6 metabolism alters primaquine pharmacokinetics. Antimicrob Agents Chemother. 2015;59:2380–7.
Prah JK, Amoah S, Yartey AN, Ampofo-Asiama A, Ameyaw EO. Assessment of malaria diagnostic methods and treatments at a Ghanaian health facility. Pan Afr Med J. 2021;39:251.
Price RN, Commons RJ, Battle KE, Thriemer K, Mendis K. Plasmodium vivax in the Era of the Shrinking Plasmodium falciparum Map. Trends Parasitol. 2020;36:560–70.
Price RN, Commons RJ, Battle KE, Thriemer K, Mendis K. Plasmodium vivax in the Era of the Shrinking Plasmodium falciparum Map. Trends Parasitol. 2020;36:560–70.
Price RN, von Seidlein L, Valecha N, Nosten F, Baird JK, White NJ. Global extent of chloroquine-resistant Plasmodium vivax: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14:982–91.
Rehn T, Lubiana P, Nguyen THT, Pansegrau E, Schmitt M, Roth LK, Brehmer J, Roeder T, Cadar D, Metwally NG. Ectopic expression of Plasmodium vivax vir Genes in Plasmodium falciparum affects cytoadhesion via increased expression of specific var genes. Microorganisms. 2022;10:1183.
Rishikesh K, Saravu K. Primaquine treatment and relapse in Plasmodium vivax malaria. Pathogens Global Health. 2016;110:1–8.
Rodrigo C, Rajapakse S, Fernando D. Tafenoquine for preventing relapse in people with Plasmodium vivax malaria. Cochrane Database Syst Rev. 2020;9:10458.
Rodríguez JAI, Rodríguez SNI, Olivera MJ. Plasmodium vivax malaria across South America: management guidelines and their quality assessment. Rev Soc Bras Med Trop. 2020;53:e20200179.
Rosenthal PJ. Malaria in 2022: Challenges and progress. Am J Trop Med Hyg. 2022;106:1565–7.
Russo G, Faggioni G, Paganotti GM, Djeunang Dongho GB, Pomponi A, De Santis R, Tebano G, Mbida M, Sanou Sobze M, Vullo V. Molecular evidence of Plasmodium vivax infection in Duffy negative symptomatic individuals from Dschang, West Cameroon. Malar J. 2017;16:1–9.
Sato S. Plasmodium—a brief introduction to the parasites causing human malaria and their basic biology. J Physiol Anthropol. 2021;40:1.
Shaikh MS, Ali B, Janjua M, Akbar A, Haider SA, Moiz B, Raheem A, Baird JK, Beg MA. Plasmodium in the bone marrow: case series from a hospital in Pakistan, 2007–2015. Malar J. 2021;20:1–6.
Sharma S, Verma R, Yadav B, Kumar A, Rahi M, Sharma A. What India can learn from globally successful malaria elimination programmes. BMJ Glob Health. 2022;7:e008431.
Soto AM, González-Cerón L, Santillán-Valenzuela F, Parrales ME, Montoya A. Recurrent Plasmodium vivax cases of both short and long latency increased with transmission intensity and were distributed year-round in the most affected municipalities of the RACCN, Nicaragua, 2013–2018. Int J Environ Res Public Health. 2022;19:6195.
Spring MD, Lon C, Sok S, Sea D, Wojnarski M, Chann S, Kuntawunginn W, Kheang Heng T, Nou S, Arsanok M, et al. Prevalence of CYP2D6 genotypes and predicted phenotypes in a cohort of Cambodians at high risk for infections with Plasmodium vivax. Am J Trop Med Hyg. 2020;103:756–9.
Spring MD, Sousa JC, Li Q, Darko CA, Morrison MN, Marcsisin SR, Mills KT, Potter BM, Paolino KM, Twomey PS, et al. Determination of cytochrome P450 isoenzyme 2D6 (CYP2D6) genotypes and pharmacogenomic impact on primaquine metabolism in an active-duty US military population. J Infect Dis. 2019;220:1761–70.
Stevens-Hernandez CJ, Flatt JF, Kupzig S, Bruce LJ. Reticulocyte maturation and variant red blood cells. Front Physiol. 2022;13:834463. https://doi.org/10.3389/fphys.2022.834463.
Stewart AGA, Zimmerman PA, McCarthy JS. Genetic Variation of G6PD and CYP2D6: Clinical Implications on the use of primaquine for elimination of Plasmodium vivax. Front Pharmacol. 2021;12:784909.
Storm J, Jespersen JS, Seydel KB, Szestak T, Mbewe M, Chisala NV, Phula P, Wang CW, Taylor TE, Moxon CA. Cerebral malaria is associated with differential cytoadherence to brain endothelial cells. EMBO Mol Med. 2019;11:e9164.
Styka AN, Savitz DA. 2020. Assessment of long-term health effects of antimalarial drugs when used for prophylaxis.
Su X-Z, Zhang C, Joy DA. Host-malaria parasite interactions and impacts on mutual evolution. Front Cell Infect Microbiol. 2020;10:587933.
Sutanto I, Tjahjono B, Basri H, Taylor WR, Putri FA, Meilia RA, Setiabudy R, Nurleila S, Ekawati LL, Elyazar I. Randomized, open-label trial of primaquine against vivax malaria relapse in Indonesia. Antimicrob Agents Chemother. 2013;57:1128–35.
Taylor C, Crosby I, Yip V, Maguire P, Pirmohamed M, Turner RM. A review of the important role of CYP2D6 in pharmacogenomics. Genes. 2020;11:1295.
Taylor AR, Watson JA, Chu CS, Puaprasert K, Duanguppama J, Day NPJ, Nosten F, Neafsey DE, Buckee CO, Imwong M, et al. Resolving the cause of recurrent Plasmodium vivax malaria probabilistically. Nat Commun. 2019;10:5595.
Teklehaimanot A, Teklehaimanot H, Girmay A, Woyessa A. Case report: primaquine failure for radical cure of Plasmodium vivax malaria in Gambella, Ethiopia. Am J Trop Med Hyg. 2020;103:415–20.
Tham W-H, Beeson JG, Rayner JC. Plasmodium vivax vaccine research–we’ve only just begun. Int J Parasitol. 2017;47:111–8.
Thomas D, Tazerouni H, Sundararaj KGS, Cooper JC. Therapeutic failure of primaquine and need for new medicines in radical cure of Plasmodium vivax. Acta Trop. 2016;160:35–8.
Thomson-Luque R, Bautista JM. Home Sweet Home: Plasmodium vivax-infected reticulocytes-the younger the better? Front Cell Infect Microbiol. 2021;11:675156.
Thomson-Luque R, Scopel KK. Immature reticulocytes as preferential host cells and the challenges for in vitro culture of Plasmodium vivax. Taylor & Francis; 2015.
Tiwari M. Glucose 6 phosphatase dehydrogenase (G6PD) and neurodegenerative disorders: mapping diagnostic and therapeutic opportunities. Genes Dis. 2017;4:196–203.
Torres K, Ferreira MU, Castro MC, Escalante AA, Conn JE, Villasis E, da Silva Araujo M, Almeida G, Rodrigues PT, Corder RM. Malaria resilience in South America: epidemiology, vector biology, and immunology insights from the Amazonian International Center of excellence in malaria research network in Peru and Brazil. Am J Trop Med Hyg. 2022;107:168–81.
Totino PR, Lopes SC. Insights into the cytoadherence phenomenon of Plasmodium vivax: the putative role of phosphatidylserine. Front Immunol. 2017;8:1148.
Vallejo AF, García J, Amado-Garavito AB, Arévalo-Herrera M, Herrera S. Plasmodium vivax gametocyte infectivity in sub-microscopic infections. Malar J. 2016;15:48.
Vantaux A, Péneau J, Cooper CA, Kyle DE, Witkowski B, Maher SP. Liver stage fate determination in Plasmodium vivax parasites: characterization of schizont growth and hypnozoite fating from patient isolates. bioRxiv. 2022.06.16.496373. https://doi.org/10.1101/2022.06.16.496373.
Venkatesan P. The future of malaria control in light of RTS. S The Lancet Microbe. 2022;3:e251.
Venugopal K, Hentzschel F, Valkiūnas G, Marti M. Plasmodium asexual growth and sexual development in the haematopoietic niche of the host. Nat Rev Microbiol. 2020;18:177–89.
Verma A, Joshi H, Singh V, Anvikar A, Valecha N. Plasmodium vivax msp-3α polymorphisms: analysis in the Indian subcontinent. Malar J. 2016;15:1–13.
Viviani R, Messina I, Bosch JE, Dommes L, Paul A, Schneider KL, Scholl C, Stingl JC. Effects of genetic variability of CYP2D6 on neural substrates of sustained attention during on-task activity. Transl Psychiatry. 2020;10:338.
Voorberg-van der Wel A, Kocken CHM, Zeeman AM. Modeling Relapsing Malaria: Emerging technologies to study parasite-host interactions in the liver. Front Cell Infect Microbiol. 2020;10:606033.
Waite JL, Suh E, Lynch PA, Thomas MB. Exploring the lower thermal limits for development of the human malaria parasite. Plasmodium falciparum Biol Lett. 2019;15:20190275.
Watson J, Taylor WRJ, Menard D, Kheng S, White NJ. Modelling primaquine-induced haemolysis in G6PD deficiency. eLife. 2017;6:e23061.
White NJ. Why do some primate malarias relapse? Trends Parasitol. 2016;32:918–20.
WHO. Control and elimination of Plasmodium vivax malaria: a technical brief. World Health Organization; 2015.
WHO. Global technical strategy for malaria 2016–2030 (WHO). 2015.
WHO. World Malaria Report 2019. Geneva: WHO; 2019. [Google Scholar].
WHO. WHO recommends groundbreaking malaria vaccine for children at risk. World Heal Organ 1. 2021. https://www.who.int/news/item/06-10-2021.
World Health Organization. World Malaria Report 2021: Reference Source. Geneva; World Health Organization; 2022.
Wilairatana P, Masangkay FR, Kotepui KU, De Jesus Milanez G, Kotepui M. Prevalence and risk of Plasmodium vivax infection among Duffy-negative individuals: a systematic review and meta-analysis. Sci Rep. 2022;12:1–13.
Zavala F. RTS,S: the first malaria vaccine. J Clin Invest. 2022;132(1):e156588. https://doi.org/10.1172/JCI156588.
Zhang R, Lee W-C, Lau Y-L, Albrecht L, Lopes SC, Costa FT, Suwanarusk R, Nosten F, Cooke BM, Rénia L. Rheopathologic consequence of Plasmodium vivax rosette formation. PLoS Negl Trop Dis. 2016;10:e0004912.
Zhang X, Wei H, Zhang Y, Zhao Y, Wang L, Hu Y, Nguitragool W, Sattabongkot J, Adams J, Cui L, et al. Genetic diversity of Plasmodium vivax reticulocyte binding protein 2b in global parasite populations. Parasit Vectors. 2022;15:205.
Zhong D, Koepfli C, Cui L, Yan G. Molecular approaches to determine the multiplicity of Plasmodium infections. Malar J. 2018;17:1–9.
Acknowledgements
Not applicable.
Funding
This work received no specific grant from any funding agency.
Author information
Authors and Affiliations
Contributions
KH. conceived of the presented idea and developed the draft, and KH, BP. GY contributed to the final manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Habtamu, K., Petros, B. & Yan, G. Plasmodium vivax: the potential obstacles it presents to malaria elimination and eradication. Trop Dis Travel Med Vaccines 8, 27 (2022). https://doi.org/10.1186/s40794-022-00185-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40794-022-00185-3