Abstract
Epidemiological studies support a general inverse association between the risk of cancer development and Parkinson’s disease (PD). In recent years however, increasing amount of eclectic evidence points to a positive association between PD and cancers through different temporal analyses and ethnic groups. This positive association has been supported by several common genetic mutations in SNCA, PARK2, PARK8, ATM, p53, PTEN, and MC1R resulting in cellular changes such as mitochondrial dysfunction, aberrant protein aggregation, and cell cycle dysregulation. Here, we review the epidemiological and biological advances of the past decade in the association between PD and cancers to offer insight on the recent and sometimes contradictory findings.
Similar content being viewed by others
Introduction
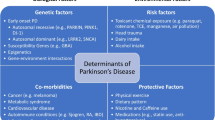
Parkinson’s disease (PD) is one of the most common and rigorously studied age-related neurodegenerative disorders, occurring in 0.3 % of the whole population and nearly 2 % in those over 65 years of age in industrialized countries [1]. Resting tremor, rigidity, hypokinesia, and postural instability are the four cardinal motor symptoms of PD resulting from the loss of dopaminergic neurons in the substantia nigra pars compacta. While the prevalence of this slowly debilitating disease is increasing, it remains incurable and irreversible due to its elusive mechanisms. Another chronic disease devastating human health and of substantial research focus is cancer. Many epidemiological studies have reported associations between PD and cancers, supporting a general inverse and more recently, positive association in certain cancers including skin, breast, and brain. This positive association is corroborated by advances in molecular genetics and cell biology revealing several genetic mutations that alter cell cycle control, protein turnover, and mitochondrial functions. This intriguing association between PD and cancers provides a new perspective to the well-known opposing cell fates of degeneration and death of post-mitotic neurons, and the uncontrolled division and enhanced resistance to death of cancer cells. The convergence of these processes provides new avenues to study both of the age-related conditions and address an urgent need for therapeutic options.
Epidemiological associations between PD and cancer
General trends between PD and common cancers
Many epidemiological studies have indicated an inverse association between the risk of developing cancers and PD. In a meta-analysis of 29 studies by Bajaj et al. that included 107598 PD patients, the diagnosis of PD was associated with an overall 27 % decreased risk of all cancers included in the studies, and 31 % decreased risk after exclusion of melanoma and other skin tumors [2]. Similarly, a recent 2014 meta-analysis by Catala-Lopez et al. found 17 % decreased risk of cancer in PD patients [3]. The most widely reported reduced risks in PD patients are cancers of the prostate, lung, bladder, stomach, colorectal, blood, and uterus (Table 1). While the lower risks of lung, bladder, and colorectal cancer, all smoking-related cancers, in PD patients are generally undisputed, stomach, leukemia, and uterine cancers fail to achieve significance in some studies for a clear inverse association.
Evidence also links PD to an increased prevalence of a few cancers (Table 1), in particular non-melanoma skin cancer. Associations of breast and brain cancers with PD are suspected but conflicting, as is the temporal association between cancers and PD occurrence. For instance, Olsen et al. found that individuals before PD diagnosis have significant risk of non-melanoma skin cancer [4], but is countered by a recent study by Wirdefeldt et al. showing increased risk of 40 % only after 1 year following PD diagnosis [5]. Likewise, other studies that investigate the risk of cancer before and after PD diagnosis reveal associations that differ in direction and statistical significance.
Trends differ across ethnicities and between Eastern and Western populations. In two Taiwanese and British cohort studies, brain, kidney, and uterine cancers were positively associated with PD after diagnosis, but stomach and lung cancer were negatively associated with PD in the British study [6], while they were positive in the Taiwanese study [7]. In fact, the authors of the Taiwanese study did not report negative risks for any cancer in PD patients. The validity of these differences, whether due to differential genetic, environmental factors, or technic variations, should be closely examined, as a previously published Taiwanese matched cohort study of the same database found that lung cancer had lower hazard ratio in PD versus non-PD patients [8], corroborating the negative association of studies in Danish [9, 10], American [11, 12], Swedish [5], and British [13] populations. Further investigations of cancer in Asian PD patients are warranted.
PD and melanoma
Melanoma has an established and consistently positive association with PD (Table 2). However, individual studies show relative risk with considerable variation from 0.5 to 20.9. Although the studies controlled for similar factors, including age, race, and sex, differences invariably arise from biases due to selection and inclusion criteria, diagnostic practices and confirmation of pathology, sample sizes, and unadjusted covariates. Smoking history and family history of melanoma or PD should be accounted for as confounders in the statistical models if possible. Smoking has long been associated with PD, and melanoma could introduce survival bias due to unrelated diseases and comorbidity. Similarly, there is an apparent genetic basis for the PD-melanoma association: individuals with first-degree family history of melanoma have 85 % higher relative risk of PD [14], and the association extends to third-degree relatives [11]. Melanoma is fairly uncommon amongst PD patients, as evidenced by 9 observed cases in a cohort of 806 PD patients of the PRECEPT study and 19 melanoma versus 1718 non-melanoma subjects of the NET-PD study, thereby allowing more room for variability in calculated risks and requiring greater statistical sensitivity in analyses. Furthermore, a temporal association seems to exist: melanoma risk increases closer to the index date of PD [4, 9, 15]. To consolidate some of these factors across studies, a meta-analysis of 12 studies report that the overall odds ratio for melanoma in people with PD versus no PD was 2.11 [16]. The authors also highlight that the odds ratio after PD diagnosis is 3.61 versus statistically insignificant 1.07 before PD diagnosis [16].
L-3,4-dihydroxyphenylalanine (L-DOPA), the main drug used to treat PD, was initially proposed to be responsible for the association with melanoma [17] although it has now been widely discredited [18, 19]. Several pigmentation interrelated proteins, including tyrosinase, tyrosine hydroxylase, melanin, and sphingolipids [20–22], and possible common risk factors including pesticide exposure [23] and lack of smoking, caffeine, and alcohol intake [24–29] have emerged to help explain the association. Tyrosine hydroxylase converts tyrosine to the dopamine precursor L-DOPA in both melanocytes and neurons while tyrosinase converts tyrosine to L-DOPA and dopaquinone, the precursor to pheomelanins and eumelanins [30]. Sorting of tyrosinase to melanosomes from the Golgi seems to require glycosphingolipids [31]. Dysregulation of glycosphingolipid metabolism, storage, and interaction with α-synuclein, as well as mutations of the phospholipase A2, group VI (PLA2G6) gene regulating synthesis of glycosphingolipids’ core component ceramide, are associated with both melanoma and PD [32–36]. Adding to the complexity, melanin, the end product of this pathway, could be a doubled-edged sword. Melanin serves to dissipate UV radiation and protect against DNA damage in skin cells, and neuromelanin binds to 1-methyl-4-phenylpyridinium ion (MPP+) and metal ions to reduce their toxicity [37]. Hence, a hypothesis put forward for the negative link between smoking and melanoma and PD is the stimulated production of melanin and neuromelanin by nicotine [38], although whether or not nicotine is truly beneficial is debatable as neuromelanin also activates microglia and stimulates their secretion of proinflammatory cytokines tumor-necrosis factor α, interleukin 6, and nitric oxide in a degenerate cycle [37].
Genetic determinants and associated cellular processes shared in PD and cancer
A growing body of evidence supports common genetic mechanisms in cancer and neurodegenerative diseases. Mutations in a variety of genes involved in the dysregulation of the cell cycle and protein turnover have been implicated in both PD and cancer.
SNCA
SNCA is perhaps the best known causal gene for PD, with several missense mutations (A53T, E46K, H50Q, G51D, A30T), gene duplications, or posttranslational modifications of α-synuclein that ultimately lead to its misfolding and aggregation of insoluble fibrils [39]. The function of α-synuclein has been postulated to facilitate the release of neurotransmitters at synapses, and recent evidence has shown support for this hypothesis. In mutated α-synuclein E57K mouse lines that accumulate oligomers, there were loss of synaptic terminals and dendrites and impairment of vesicle transport [40]. They exist in the unfolded monomeric form in the cytosol, but act as chaperones in the multimeric state when bound to plasma membrane or docked synaptic vesicles in the process of forming SNARE complexes, which are crucial for neurotransmitter release from the presynaptic membrane [41–43]. The soluble monomeric form, rather than the membrane bound α helical multimeric form, is the basis of aggregates and associated neurotoxicity [44]. The interaction with membranes is possibly stabilized through the positively charged N-terminus of α-synuclein binding to the negatively charged lipid membrane of vesicles through a lipid ordering effect [45, 46]. Interestingly, α-synuclein is now also implicated in reducing Aβ deposition and plaque formation in Alzheimer’s disease, although the interaction between α-synuclein and Aβ does not seem to attenuate, but rather exacerbate, synapse and dendritic loss [47].
α-synuclein is also linked to various cancers although the biological consequences are relatively unknown. Immunohistological studies revealed its expression in ependymoma, astrocytoma, breast and ovarian cancerous tissues, and these cancers co-occur with PD in epidemiological studies discussed previously [48, 49]. The methylated state of SNCA and the presence of α-synuclein in melanocytic lesions may be used as biomarkers for some lymphomas and melanoma [50, 51]. Although α-synuclein is a hallmark of PD, its propagation mechanism may help explain its appearance in cancers outside the brain and in human plasma and cerebrospinal fluid [52–54]. In melanoma, S129-phosphorylated form of α-synuclein, the pathological form in Lewy bodies of PD, but not the unphosphorylated form, is localized to the surface of melanoma cells and their released microvesicles’ membranes [55]. The exosomal secretion pathway, implicated in prion diseases, could also play a role. Neurons and astrocytes can secrete exosomes containing α-synuclein oligomers inside and on the surface of their membranes, conferring the oligomers greater chance of reuptake by another cell than when exosome-free [56, 57]. Strikingly, α-synuclein has recently been shown to cross the blood–brain barrier, which has increased permeability in PD, after intravenous injection in mice [58, 59]. Taken together, an emerging hypothesis for the aggregation and prion-like propagation of toxic α-synuclein present in PD and its co-appearance in brain and other cancers could be through its release and uptake via various mechanisms between neurons and cells outside of the central nervous system (CNS).
PARK2
PARK2 encodes parkin, which is a component of a multiprotein E3 ubiquitin ligase complex, a part of the ubiquitin-proteasome system (UPS) that mediates the targeting of proteins for degradation [60, 61]. Genetically, PARK2 is the most commonly mutated gene in autosomal recessive PD, accounting for nearly 50 % of cases [62, 63]. In one study of early onset PD, mutations were detected in 77 % of patients aged 20 or younger [64]. Heterozygous mutations of PARK2 in exon 7, the first RING finger (C253W, R256C, R275W, and D280N) act as susceptibility alleles for late onset PD [63, 65, 66]. In cancer, although the association between the exact alterations of PARK2 and cancer susceptibility is not well understood, the mutations, deletion, copy number alterations, promoter hypermethylation, and aberrant mRNA and protein expression of PARK2 have all been found to be prevalent across human malignancies, especially glioma, lung, breast, colon, and ovarian cancer [7, 67–70].
The precise mechanism by which mutations in PARK2 lead to PD and cancer remains unclear. However, accumulation of cyclin E, a substrate of PARK2, seems to be a central event [71]. Cyclin E is the primary cyclin that drives S-phase progression [72]. Loss of function of PARK2 mutations results in the deficiency of E3 ligase, leading to dysfunctional UPS, buildup of cyclin E and β-catenin, and upregulation of Wnt and EGFR-AKT pathways [60, 61, 73]. CDK2/cyclin E phosphorylates the tumor suppressor retinoblastoma, releasing the transcription factor E2F-1 from inhibition. In cycling cells, E2F-1 upregulates proteins facilitating progression through S phase, but in post-mitotic neurons, E2F-1 triggers apoptosis through p53 and Bax [74, 75]. Conversely, the overexpression of β-catenin, a protein overexpressed in many cancers, may partially explain why some cancers are inversely associated with PD, as signaling of Wnt/β-catenin promotes repairing mechanisms in dopaminergic neurons [76]. On the other hand, EGFR-AKT signaling is likely tissue specific and context dependent, as loss of PARK2 have been found to increase or decrease the activity of EGFR-AKT, and subsequently, promote or hinder neuronal survival, adding a complex layer to the conflicting association between PD and different cancers [73, 77].
PARK8
The PARK8 gene encodes the leucine-rich repeat kinase 2 (LRRK2) protein, with the G2019S, R1441G/C/H, Y1699C, G2385R, R1628P, I2020T mutations appears to increase the risk of PD [78–80]. LRRK2 has been reported to have complex and extensive roles related its well-known functions as a GTPase and kinase, including regulation of synaptogenesis, axon and dendritic growth, and synaptic vesicle release and interaction with tau, 14-3-3 proteins, and the presynaptic proteins syntaxin 1A, synapsin I, dynamin I, and VAMP2 [81–86]. One of the most notable causal autosomal dominant mutations for PD, G2019S, was first discovered in Ashkenazi Jewish and North African Arabian populations and since has been the focus of many genetic and translational studies in PD [87, 88]. Consequences of the G2019S mutation include gain-of-function increase in LRRK2 protein kinase activity and ubiquitination [89], increased glutamatergic synapse activity and synaptic vesicle release [90], decreased levels of neurotrophic protein progranulin in microglia and fibroblasts [91], a protein linked to neurite growth and neuronal survival [92], lysosomal aggregation [93], and inhibition of autophagic function in dopaminergic neurons [94, 95]. As a whole, G2019S related dysfunction affects synaptic transmission, autophagy, and neurite health in the pathological LRRK2-PD association.
The G2019S-cancer link is disputed by epidemiological studies [96–100] but is starting to be elucidated in the laboratory. In cultured neuroblastoma cells, the G2019S mutant protein initiated the formation of α-synuclein aggregates, propagation into neighboring cells, and subsequent cellular toxicity [101]. G2019S also activates the oncogenic MET/ERK pathway, which was demonstrated to increase basal autophagy and α-synuclein aggregation [102, 103]. These preliminary findings demonstrate potential in finding site-specific targets on LRRK2 as therapeutic options for PD and suspected positively associated cancers, such as breast and prostate.
Ataxia telangiectasia mutated (ATM) and p53
ATM provides another close genetic link between neurodegeneration and cancer through genome integrity maintenance and cell cycle control. Direct evidence is found in the rare genetic disease ataxia telangiectasia (AT) caused by mutations of ATM. AT is characterized by both severe cerebellar degeneration and predisposition for cancer and radiation sensitivity [104, 105]. The gene ATM encodes a serine/threonine protein kinase, a member of the phosphatidylinositol-3 kinase (PI3K) superfamily. ATM is recruited initially to the sites of DNA lesions, such as double strand breaks, and phosphorylates several key proteins such as checkpoint kinase CHK2, histone H2AX, the Rad50–Mre11–Nsb1 complex, tumor suppressors p53 and BRCA1, leading to the activation of DNA damage checkpoints, cell cycle arrest, DNA repair, or apoptosis [106–109]. Cells without any functional ATM protein are hypersensitive to radiation and do not respond normally to DNA damage; instead of activating DNA repair, the defective ATM protein allows mutations to accumulate in other genes. ATM-heterozygous germline mutations were shown to contribute to breast cancer, non-Hodgkin’s lymphomas and B-cell chronic lymphocytic leukemia, while ATM-homozygotes develop lymphoma and leukemia [110, 111]. Because ATM is an essential component of the DNA damage response and apoptosis, its normal expression is crucial for post-mitotic neurons. Camins et al. found that in cells treated with MPP+ as an experimental model of PD, cell viability was decreased through activation of ATM and possibly retinoblastoma protein, ultimately leading to initiation of apoptosis [112]. Inhibition of MPP+ induced ATM activation displayed neuroprotective effects and increased cell survival [112], although the finding is contradicted by another study showing reduced ATM activity causes neuronal death [113]
ATM can activate repair proteins in response to DNA double-strand breaks, but when the DNA repair machinery is overwhelmed, ATM can also activate p53 to induce cell-cycle arrest and apoptosis. p53 has been recently shown to be involved in aging and neurodegenerative disorders. In PD, p53 levels are increased, possibly through s-nitrosylation of parkin [114], where it mediates microglial activation and subsequent pro-inflammatory phenotypes, leading a p53-driven microglial-evoked neurotoxicity [115–119]. In addition, interaction of p53 with α-synuclein is purported to suppress Notch1 signaling, leading to retarded neurogenesis in mature neurons [120]. Inhibition of p53 prevents cell death [116, 118, 121, 122].
Phosphatase and tensin homolog (PTEN) and putative kinase 1 (PINK1)
PTEN was first identified as a tumor suppressor gene located on chromosome 10q23. PTEN removes the 3′phosphate from phosphatidylinositol 3,4,5-triphosphate (PIP3) and eventually shuts down PI3K-Akt-mTOR pathway leading to growth inhibition and apoptosis [123]. Frequent inactive mutations of PTEN were detected in a variety of human cancers including glioblastoma, advanced prostate, and endometrial cancers, and reduced expression is found in many other tumor types such as lung and breast cancer [124–129].
While its role as tumor suppressor is established unambiguously, emerging evidence shows that the biological function of PTEN extends to the CNS where it is widely expressed and localized to the cytoplasm and nucleus [130, 131]. Several studies indicate that PTEN is a crucial regulator of neuronal development, neuronal survival, axonal regeneration, and synaptic plasticity and has been linked to the pathogenesis of neurodegenerative disorders at the molecular level [132–137]. The main target of PTEN, mTOR, plays an essential role in maintaining the integrity of postmitotic neurons by regulating key cellular processes such as protein synthesis, autophagy, mitochondrial metabolism, and biogenesis [138]. The selective inhibitor of mTORC1, rapamycin was shown to be neuroprotective in experimental models of Alzheimer’s disease and PD [139, 140].
PTEN regulates the function of PTEN induced putative kinase 1 (PINK1), located on chromosome 1p36, a region frequently deleted in human cancers and mutated in familial forms of PD [141–143]. Similar to another common PD causal gene PARK2, PINK1 plays a key role in mitochondrial quality control by identifying damaged mitochondrial and targeting them for degradation, important functions dysregulated in neurodegeneration and cancer [144, 145]. PINK1 is linked with the AKT pathway through PTEN, which is the main driver for tumorigenesis and neuronal survival [145, 146]. Expression of PINK1 mRNA and protein ranges from high to low in different types of cancers, indicating the dual, context dependent pro and anti-tumorigenic role of PINK1 in cancer biology [147]. Flanagan et al. showed that PINK1 deletion reduced several cancer-related phenotypes like cell proliferation, colony formation and invasiveness through cell cycle control, demonstrating PINK1 as a potential oncogene [146].
Melanocortin 1 receptor (MC1R)
MC1R is the main pigmentation gene that encodes the MC1R protein. A cyclic AMP-stimulating G-protein-coupled receptor, MC1R contributes to regulation of skin physiology though the melanin synthetic pathway. MC1R is a genetic determinant of hair color and loss-of-function polymorphisms cause a shift of melanogenesis from the photoprotective, black-brown pigment eumelanin to red-yellow pheomelanin, resulting in a phenotypic spectrum of red hair color, pale skin, and freckles [148]. Epidemiological studies have shown loss-of-function MC1R variants are associated with higher risk of developing melanoma [148]. In the laboratory, disruption of MC1R increases oxidative damage and lowers the threshold for melanoma induction even in the absence of UV light [149].
In addition to skin melanocytes, MC1R is expressed in many other cell types including astrocytes [150], Schwann cells [151], and possibly certain neurons of the periaqueductal gray [152] in the brain, suggesting additional functions beyond skin. In two large prospectively followed cohorts, individuals with two copies of the MC1R gene loss-of-function variant R151C had a significant three-fold increased risk of developing PD [14]. Newly published findings in an independent cohort substantiate the MC1R-PD link via the R160W variant [153]. Another study did not replicate a significant MC1R-PD association; however, it also did not replicate the PD-melanoma association and was limited by technical/sequencing difficulty [154]. Together these epidemiological and biochemical findings indicate more general protective role of MC1R in both neurodegeneration and melanoma.
Other neurodegenerative diseases and cancers
Although the epidemiologic evidence of Alzheimer’s disease (AD)-cancer link is not as intensive as PD-cancer, an inverse association is indicated by several studies. In a prospective cohort study of individuals aged 65 and older, there was 69 % reduced risk of all cancers in AD patients [155]. Romero et al. reported cancer mortality hazard ratio of 0.5 in people with AD versus no dementia [156]. In specific cancers, there is significant 40 % decrease in risk of epithelial and lung cancers and 57 % decrease in risk of colorectal cancer in people with AD [157]. In a gender and age matched case control study, cancer had significant inverse association with AD only in women and endocrine-related tumors with odds ratios of 0.5 for both, although their study suggested overall inverse association with all types of cancers [158].
The association between AD and cancer is also bidirectional. Driver and et al. found a hazard ratio of 0.67 comparing 1278 study participants with and without cancer [159]. In population-based longitudinal study of aging including 1100 people aged 70 or older, non-melanoma skin cancer history is associated with about 79 % less AD risk [160]. Likewise, a study from the Alzheimer’s Disease Neuroimaging Initiative provides evidence that a history of non-melanoma skin cancer, but not breast or prostate cancer, has inverse association with AD diagnosis [161], contrary to the positive association observed in PD patients. Intriguingly, although cancer survivors have lower risk of AD, reduced cognitive function and cerebral gray matter density were also found in cancer patients pre and post-treatment, which complicates the apparent reverse link [161].
Although the biological evidence is scarce, the infamous PTEN gene and protein of PD has a role in AD progression. A significant loss and alteration of PTEN was found in AD neurons [162] and its downstream targets may explain its pathological significance. Glycogen synthase kinase regulates tau phosphorylation [163] while AKT mediates neuronal survival against β-amyloid neurotoxicity in experimental models of AD [164, 165].
We discussed the most researched biological mechanisms associated with PD genes, but they are not an exhaustive review. A brief summary of the genes in neurodegenerative diseases and some of their pathological effects are listed in Table 3. Table 4 lists genes in cancer that have been implicated PD.
Concluding remarks
Although overlap between PD and cancer is becoming evident, there are several concerns stemming from some of the contradictory results on both the epidemiological and laboratory fronts. One, there are undoubtedly differences in genetic mutations across ethnicities and races, as seen in the discrepancies in risk and prevalence of cancers between Eastern and Western populations, and genetic or pharmacological models with clinical applications should note the groups of most likely pertinence. Second, some studies have noted that cancers that were associated with PD approached significance depending on the range of time between the two diagnoses, which was not considered in the majority of studies, highlighting either complex temporal associations or ascertainment and survival bias that should be carefully considered. To eliminate spurious associations, stringent measures to ascertain the time of PD and cancer onset should be employed in study design and selection of available data. Third, more rigorous and cancer specific epidemiological studies are needed to support recent biological evidence linking PD and cancer, as many studies have included highly heterogeneous cancers on all-cancer risk in PD. For example, mutated PARK2 is expressed in glioblastoma, colon, and lung cancer, but the latter two cancers are associated with decreased risk of PD, contrary to increased risk in glioblastoma [3, 13, 69]. Whether or not the disparities arise from divergent pathways in different tissues is still relatively unknown, although pathological clues from neurodegenerative diseases applied to linked cancers have gained much interest due to strides in epidemiological research.
The associations between neurodegeneration and cancer presented here are likely a fraction of the plethora of shared mechanisms of these two distinct disorders. Further investigations of these links and shared genetic determinants implicated in these pathways may offer valuable perspectives and new therapeutic options for the two groups of traditionally disparate yet pathologically convergent diseases.
References
de Lau LML, Breteler MMB. Epidemiology of Parkinson's disease. The Lancet Neurology 5.6. 2006;525-535.
Bajaj A, Driver JA, Schernhammer ES. Parkinson’s disease and cancer risk: a systematic review and meta-analysis. Cancer Causes Control. 2010;21:697–707.
Catalá-López F, Suárez-Pinilla M, Suárez-Pinilla P, Valderas JM, Gómez-Beneyto M, Martinez S, et al. Inverse and direct cancer comorbidity in people with central nervous system disorders: a meta-analysis of cancer incidence in 577,013 participants of 50 observational studies. Psychother Psychosom. 2014;83:89–105.
Olsen JH, Friis S, Frederiksen K. Malignant melanoma and other types of cancer preceding Parkinson disease. Epidemiology. 2006;17:582–7.
Wirdefeldt K, Weibull CE, Chen H, Kamel F, Lundholm C, Fang F, et al. Parkinson’s disease and cancer: A register-based family study. Am J Epidemiol. 2014;179:85–94.
Ong ELH, Goldacre R, Goldacre M. Differential risks of cancer types in people with Parkinson’s disease: a national record-linkage study. Eur J Cancer. 2014;50:2456–62.
Lin P-Y, Chang S-N, Hsiao T-H, Huang B-T, Lin C-H, Yang P-C. Association Between Parkinson Disease and Risk of Cancer in Taiwan. JAMA Oncol. 2015;1(5):633–40.
Sun L-M, Liang J-A, Chang S-N, Sung F-C, Muo C-H, Kao C-H. Analysis of Parkinson’s disease and subsequent cancer risk in Taiwan: a nationwide population-based cohort study. Neuroepidemiology. 2011;37:114–9.
Olsen JH, Friis S, Frederiksen K, McLaughlin JK, Mellemkjaer L, Møller H. Atypical cancer pattern in patients with Parkinson’s disease. Br J Cancer. 2005;92:201–5.
Møller H, Mellemkjaer L, McLaughlin JK, Olsen JH. Occurrence of different cancers in patients with Parkinson’s disease. BMJ. 1995;310:1500–1.
Kareus SA, Figueroa KP, Cannon-Albright LA, Pulst SM. Shared predispositions of parkinsonism and cancer: a population-based pedigree-linked study. Arch Neurol. 2012;69:1572–7.
Driver JA, Logroscino G, Buring JE, Gaziano JM, Kurth T. A prospective cohort study of cancer incidence following the diagnosis of Parkinson’s disease. Cancer Epidemiol Biomarkers Prev. 2007;16:1260–5.
Fois AF, Wotton CJ, Yeates D, Turner MR, Goldacre MJ. Cancer in patients with motor neuron disease, multiple sclerosis and Parkinson’s disease: record linkage studies. J Neurol Neurosurg Psychiatry. 2010;81:215–21.
Gao X, Simon KC, Han J, Schwarzschild MA, Ascherio A. Family history of melanoma and Parkinson disease risk. Neurology. 2009;73:1286–91.
Rugbjerg K, Kathrine R, Søren F, Lassen CF, Beate R, Olsen JH. Malignant melanoma, breast cancer and other cancers in patients with Parkinson’s disease. Int J Cancer. 2012;131:1904–11.
Liu R, Gao X, Lu Y, Chen H. Meta-analysis of the relationship between Parkinson disease and melanoma. Neurology. 2011;76:2002–9.
Skibba JL, Pinckley J, Gilbert EF, Johnson RO. Multiple primary melanoma following administration of levodopa. Arch Pathol. 1972;93:556–61.
Vermeij J-D, Winogrodzka A, Trip J, Weber WEJ. Parkinson’s disease, levodopa-use and the risk of melanoma. Parkinsonism Relat Disord. 2009;15:551–3.
Zanetti R, Loria D, Rosso S. Melanoma, Parkinson’s disease and levodopa: causal or spurious link? A review of the literature. Melanoma Res. 2006;16:201–6.
Pan T, Li X, Jankovic J. The association between Parkinson’s disease and melanoma. Int J Cancer. 2011;128:2251–60.
Paisán-Ruiz C, Houlden H. Common pathogenic pathways in melanoma and Parkinson disease. Neurology. 2010;75:1653–5.
Platt FM. Sphingolipid lysosomal storage disorders. Nature. 2014;510:68–75.
Chorfa A, Bétemps D, Morignat E, Lazizzera C, Hogeveen K, Andrieu T, et al. Specific pesticide-dependent increases in α-synuclein levels in human neuroblastoma (SH-SY5Y) and melanoma (SK-MEL-2) cell lines. Toxicol Sci. 2013;133:289–97.
Noyce AJ, Bestwick JP, Silveira-Moriyama L, Hawkes CH, Giovannoni G, Lees AJ, et al. Meta-analysis of early nonmotor features and risk factors for Parkinson disease. Ann Neurol. 2012;72:893–901.
Freedman DM, Michal Freedman D, Alice S, Doody MM, Sowmya Rao R, Linet MS. Risk of melanoma in relation to smoking, alcohol intake, and other factors in a large occupational cohort. Cancer Causes Control. 2003;14:847–57.
DeLancey JO, Hannan LM, Gapstur SM, Thun MJ. Cigarette smoking and the risk of incident and fatal melanoma in a large prospective cohort study. Cancer Causes Control. 2011;22:937–42.
Song F, Qureshi AA, Gao X, Li T, Han J. Smoking and risk of skin cancer: a prospective analysis and a meta-analysis. Int J Epidemiol. 2012;41:1694–705.
Kenborg L, Lassen CF, Ritz B, Andersen KK, Christensen J, Schernhammer ES, et al. Lifestyle, family history, and risk of idiopathic Parkinson disease: a large Danish case–control study. Am J Epidemiol. 2015;181:808–16.
Van der Mark M, Nijssen PCG, Vlaanderen J, Huss A, Mulleners WM, Sas AMG, et al. A case–control study of the protective effect of alcohol, coffee, and cigarette consumption on Parkinson disease risk: time-since-cessation modifies the effect of tobacco smoking. PLoS One. 2014;9:e95297.
Fedorow H, Tribl F, Halliday G, Gerlach M, Riederer P, Double KL. Neuromelanin in human dopamine neurons: comparison with peripheral melanins and relevance to Parkinson’s disease. Prog Neurobiol. 2005;75:109–24.
Sprong H, Degroote S, Claessens T, van Drunen J, Oorschot V, Westerink BH, et al. Glycosphingolipids are required for sorting melanosomal proteins in the Golgi complex. J Cell Biol. 2001;155:369–80.
Paisán-Ruiz C, Li A, Schneider SA, Holton JL, Johnson R, Kidd D, et al. Widespread Lewy body and tau accumulation in childhood and adult onset dystonia-parkinsonism cases with PLA2G6 mutations. Neurobiol Aging. 2012;33:814–23.
Paisan-Ruiz C, Bhatia KP, Li A, Hernandez D, Davis M, Wood NW, et al. Characterization of PLA2G6 as a locus for dystonia-parkinsonism. Ann Neurol. 2009;65:19–23.
Falchi M, Bataille V, Hayward NK, Duffy DL, Bishop JAN, Pastinen T, et al. Genome-wide association study identifies variants at 9p21 and 22q13 associated with development of cutaneous nevi. Nat Genet. 2009;41:915–9.
Ichikawa S, Nakajo N, Sakiyama H, Hirabayashi Y. A mouse B16 melanoma mutant deficient in glycolipids. Proc Natl Acad Sci U S A. 1994;91:2703–7.
Piccinini M, Scandroglio F, Prioni S, Buccinnà B, Loberto N, Aureli M, et al. Deregulated sphingolipid metabolism and membrane organization in neurodegenerative disorders. Mol Neurobiol. 2010;41:314–40.
Zecca L, Luigi Z, Zucca FA, Henrik W, David S. Neuromelanin of the substantia nigra: a neuronal black hole with protective and toxic characteristics. Trends Neurosci. 2003;26:578–80.
Yerger VB, Malone RE. Melanin and nicotine: A review of the literature. Nicotine Tob Res. 2006;8:487–98.
Kim WS, Kågedal K, Halliday GM. Alpha-synuclein biology in Lewy body diseases. Alzheimers Res Ther. 2014;6:73.
Rockenstein E, Nuber S, Overk CR, Ubhi K, Mante M, Patrick C, et al. Accumulation of oligomer-prone α-synuclein exacerbates synaptic and neuronal degeneration in vivo. Brain. 2014;137(Pt 5):1496–513.
Chandra S, Sreeganga C, Gilbert G, Rafael F-C, Schlüter OM, Südhof TC. α-Synuclein Cooperates with CSPα in Preventing Neurodegeneration. Cell. 2005;123:383–96.
Burre J, Sharma M, Tsetsenis T, Buchman V, Etherton MR, Sudhof TC. Alpha-Synuclein Promotes SNARE-Complex Assembly in Vivo and in Vitro. Science. 2010;329:1663–7.
Burré J, Sharma M, Südhof TC. α-Synuclein assembles into higher-order multimers upon membrane binding to promote SNARE complex formation. Proc Natl Acad Sci U S A. 2014;111:E4274–83.
Burre J, Sharma M, Sudhof TC. Definition of a Molecular Pathway Mediating -Synuclein Neurotoxicity. J Neurosci. 2015;35:5221–32.
Pirc K, Ulrih NP. α-Synuclein interactions with phospholipid model membranes: Key roles for electrostatic interactions and lipid-bilayer structure. Biochim Biophys Acta. 2015;1848(10 Pt A):2002–12.
Bartels T, Tim B, Ahlstrom LS, Avigdor L, Frits K, Christian H, et al. The N-Terminus of the Intrinsically Disordered Protein α-Synuclein Triggers Membrane Binding and Helix Folding. Biophys J. 2010;99:2116–24.
Bachhuber T, Katzmarski N, McCarter JF, Loreth D, Tahirovic S, Kamp F, et al. Inhibition of amyloid-β plaque formation by α-synuclein. Nat Med. 2015;21:802–7.
Fung K-M, Rorke LB, Giasson B, Lee VM-Y, Trojanowski JQ. Expression of alpha-, beta-, and gamma-synuclein in glial tumors and medulloblastomas. Acta Neuropathol. 2003;106:167–75.
Bruening W, Giasson BI, Klein-Szanto AJ, Lee VM, Trojanowski JQ, Godwin AK. Synucleins are expressed in the majority of breast and ovarian carcinomas and in preneoplastic lesions of the ovary. Cancer. 2000;88:2154–63.
Welinder C, Jönsson GB, Ingvar C, Lundgren L, Baldetorp B, Olsson H, et al. Analysis of alpha-synuclein in malignant melanoma - development of a SRM quantification assay. PLoS One. 2014;9:e110804.
Bethge N, Lothe RA, Honne H, Andresen K, Trøen G, Eknæs M, et al. Colorectal cancer DNA methylation marker panel validated with high performance in Non-Hodgkin lymphoma. Epigenetics. 2014;9:428–36.
El-Agnaf O, Salem SA, Paleologou KE, Curran MD. Detection of oligomeric forms of α-synuclein protein in human plasma as a potential biomarker for Parkinson’s disease. FASEB J. 2006;20(3):419–25.
Gao L, Tang H, Nie K, Wang L, Zhao J, Gan R, et al. Cerebrospinal fluid alpha-synuclein as a biomarker for Parkinson’s disease diagnosis: a systematic review and meta-analysis. Int J Neurosci. 2014;125(9):645–54.
Hansson O, Hall S, Ohrfelt A, Zetterberg H. Levels of cerebrospinal fluid α-synuclein oligomers are increased in Parkinson’s disease with dementia and dementia with Lewy bodies compared to. Alzheimers Res Ther. 2014;6(3):25.
Lee BR, Matsuo Y, Cashikar AG, Kamitani T. Role of Ser129 phosphorylation of α-synuclein in melanoma cells. J Cell Sci. 2013;126(Pt 2):696–704.
Danzer KM, Kranich LR, Ruf WP, Cagsal-Getkin O, Winslow AR, Zhu L, et al. Exosomal cell-to-cell transmission of alpha synuclein oligomers. Mol Neurodegener. 2012;7:42.
Lachenal G, Pernet-Gallay K, Chivet M, Hemming FJ, Belly A, Bodon G, et al. Release of exosomes from differentiated neurons and its regulation by synaptic glutamatergic activity. Mol Cell Neurosci. 2011;46:409–18.
Gray MT, Woulfe JM. Striatal blood–brain barrier permeability in Parkinson’s disease. J Cereb Blood Flow Metab. 2015;35:747–50.
Peelaerts W, Bousset L, Van der Perren A, Moskalyuk A, Pulizzi R, Giugliano M, et al. α-Synuclein strains cause distinct synucleinopathies after local and systemic administration. Nature. 2015;522:340–4.
Shimura H, Schlossmacher MG, Hattori N, Frosch MP, Trockenbacher A, Schneider R, et al. Ubiquitination of a new form of alpha-synuclein by parkin from human brain: implications for Parkinson’s disease. Science. 2001;293:263–9.
Shimura H, Hattori N, Kubo SI, Mizuno Y, Asakawa S, Minoshima S, et al. Familial Parkinson disease gene product, parkin, is a ubiquitin-protein ligase. Nat Genet. 2000;25:302–5.
Hattori N, Kitada T, Matsumine H, Asakawa S, Yamamura Y, Yoshino H, et al. Molecular genetic analysis of a novel Parkin gene in Japanese families with autosomal recessive juvenile parkinsonism: evidence for variable homozygous deletions in the Parkin gene in affected individuals. Ann Neurol. 1998;44:935–41.
Singleton AB, Farrer MJ, Bonifati V. The genetics of Parkinson’s disease: progress and therapeutic implications. Mov Disord. 2013;28:14–23.
Lücking CB, Dürr A, Bonifati V, Vaughan J, De Michele G, Gasser T, et al. Association between Early-Onset Parkinson’s Disease and Mutations in the Parkin Gene. N Engl J Med. 2000;342:1560–7.
Oliveira SA, Scott WK, Martin ER, Nance MA, Watts RL, Hubble JP, et al. Parkin mutations and susceptibility alleles in late-onset Parkinson’s disease. Ann Neurol. 2003;53:624–9.
Foroud T, Uniacke SK, Liu L, Pankratz N, Rudolph A, Halter C, et al. Heterozygosity for a mutation in the parkin gene leads to later onset Parkinson disease. Neurology. 2003;60:796–801.
Alcalay RN, Clark LN, Marder KS, Bradley WEC. Lack of association between cancer history and PARKIN genotype: a family based study in PARKIN/Parkinson’s families. Genes Chromosomes Cancer. 2012;51:1109–13.
Xiong D, Wang Y, You M. PARK2 gene and familial lung cancer: what is the link? Future Oncol. 2015;11:1707–10.
Veeriah S, Taylor BS, Meng S, Fang F, Yilmaz E, Vivanco I, et al. Somatic mutations of the Parkinson’s disease-associated gene PARK2 in glioblastoma and other human malignancies. Nat Genet. 2010;42:77–82.
Xu L, Lin D-C, Yin D, Koeffler HP. An emerging role of PARK2 in cancer. J Mol Med. 2014;92:31–42.
Gong Y, Zack TI, Morris LGT, Lin K, Hukkelhoven E, Raheja R, et al. Pan-cancer genetic analysis identifies PARK2 as a master regulator of G1/S cyclins. Nat Genet. 2014;46:588–94.
Ohtsubo M, Theodoras AM, Schumacher J, Roberts JM, Pagano M. Human cyclin E, a nuclear protein essential for the G1-to-S phase transition. Mol Cell Biol. 1995;15:2612–24.
Lin D-C, Xu L, Chen Y, Yan H, Hazawa M, Doan N, et al. Genomic and Functional Analysis of the E3 Ligase PARK2 in Glioma. Cancer Res. 2015;75:1815–27.
Staropoli JF, Caroline M, Cécile M, Brenda S, Elena D, Asa A. Parkin Is a Component of an SCF-like Ubiquitin Ligase Complex and Protects Postmitotic Neurons from Kainate Excitotoxicity. Neuron. 2003;37:735–49.
Harbour JW, Luo RX, Dei Santi A, Postigo AA, Dean DC. Cdk phosphorylation triggers sequential intramolecular interactions that progressively block Rb functions as cells move through G1. Cell. 1999;98:859–69.
L’Episcopo F, Tirolo C, Caniglia S, Testa N, Morale MC, Serapide MF, et al. Targeting Wnt signaling at the neuroimmune interface for dopaminergic neuroprotection/repair in Parkinson’s disease. J Mol Cell Biol. 2014;6:13–26.
Fallon L, Bélanger CML, Corera AT, Kontogiannea M, Regan-Klapisz E, Moreau F, et al. A regulated interaction with the UIM protein Eps15 implicates parkin in EGF receptor trafficking and PI(3)K-Akt signalling. Nat Cell Biol. 2006;8:834–42.
Cookson MR. LRRK2 Pathways Leading to Neurodegeneration. Curr Neurol Neurosci Rep. 2015;15(7):42.
Inzelberg R, Hassin-Baer S, Jankovic J. Genetic movement disorders in patients of Jewish ancestry. JAMA Neurol. 2014;71:1567–72.
Di Fonzo A, Yah-Huei W-C, Chin-Song L, van Doeselaar M, Simons EJ, Rohé CF, et al. A common missense variant in the LRRK2 gene, Gly2385Arg, associated with Parkinson’s disease risk in Taiwan. Neurogenetics. 2006;7:133–8.
Cirnaru MD, Marte A, Belluzzi E, Russo I, Gabrielli M, Longo F, et al. LRRK2 kinase activity regulates synaptic vesicle trafficking and neurotransmitter release through modulation of LRRK2 macro-molecular complex. Front Mol Neurosci. 2014;7:49.
Piccoli G, Condliffe SB, Bauer M, Giesert F, Boldt K, De Astis S, et al. LRRK2 Controls Synaptic Vesicle Storage and Mobilization within the Recycling Pool. J Neurosci. 2011;31:2225–37.
Sepulveda B, Mesias R, Li X, Yue Z, Benson DL. Short- and long-term effects of LRRK2 on axon and dendrite growth. PLoS One. 2013;8:e61986.
Kawashima M, Masatou K, Suzuki SO, Katsumi D-U, Toru I. α-Synuclein is expressed in a variety of brain tumors showing neuronal differentiation. Acta Neuropathol 2000;99:154–160.
Nichols RJ, Dzamko N, Morrice NA, Campbell DG, Deak M, Ordureau A, et al. 14-3-3 binding to LRRK2 is disrupted by multiple Parkinson’s disease-associated mutations and regulates cytoplasmic localization. Biochem J. 2010;430:393–404.
Guerreiro PS, Ellen G, da Fonseca TL, Mathias B, Outeiro TF, Katrin E: LRRK2 Promotes Tau Accumulation, Aggregation and Release. Mol Neurobiol 2015. [Epub ahead of print]
Lesage S, Dürr A, Tazir M, Lohmann E, Leutenegger A-L, Janin S, et al. LRRK2 G2019S as a cause of Parkinson’s disease in North African Arabs. N Engl J Med. 2006;354:422–3.
Ozelius LJ, Senthil G, Saunders-Pullman R, Ohmann E, Deligtisch A, Tagliati M, et al. LRRK2 G2019S as a cause of Parkinson’s disease in Ashkenazi Jews. N Engl J Med. 2006;354:424–5.
Zhao J, Molitor TP, Langston JW, Nichols RJ. LRRK2 Dephosphorylation increases its ubiquitination. Biochem J. 2015;469(1):107–20.
Beccano-Kelly DA, Kuhlmann N, Tatarnikov I, Volta M, Munsie LN, Chou P, et al. Synaptic function is modulated by LRRK2 and glutamate release is increased in cortical neurons of G2019S LRRK2 knock-in mice. Front Cell Neurosci. 2014;8:301.
Caesar M, Felk S, Zach S, Brønstad G, Aasly JO, Gasser T, et al. Changes in matrix metalloprotease activity and progranulin levels may contribute to the pathophysiological function of mutant leucine-rich repeat kinase 2. Glia. 2014;62:1075–92.
Van Damme P, Van Hoecke A, Lambrechts D, Vanacker P, Bogaert E, van Swieten J, et al. Progranulin functions as a neurotrophic factor to regulate neurite outgrowth and enhance neuronal survival. J Cell Biol. 2008;181:37–41.
Hockey LN, Kilpatrick BS, Eden ER, Lin-Moshier Y, Brailoiu GC, Brailoiu E, et al. Dysregulation of lysosomal morphology by pathogenic LRRK2 is corrected by TPC2 inhibition. J Cell Sci. 2015;128:232–8.
Saha S, Shamol S, Ash PEA, Vivek G, Liqun L, Orian S, et al. Mutations in LRRK2 potentiate age-related impairment of autophagic flux. Mol Neurodegener. 2015;10:26.
Ramonet D, Daher JPL, Lin BM, Stafa K, Kim J, Banerjee R, et al. Dopaminergic neuronal loss, reduced neurite complexity and autophagic abnormalities in transgenic mice expressing G2019S mutant LRRK2. PLoS One. 2011;6:e18568.
Inzelberg R, Cohen OS, Aharon-Peretz J, Schlesinger I, Gershoni-Baruch R, Djaldetti R, et al. The LRRK2 G2019S mutation is associated with Parkinson disease and concomitant non-skin cancers. Neurology. 2012;78:781–6.
Agalliu I, San Luciano M, Mirelman A, Giladi N, Waro B, Aasly J, et al. Higher frequency of certain cancers in LRRK2 G2019S mutation carriers with Parkinson disease: a pooled analysis. JAMA Neurol. 2015;72:58–65.
Allegra R, Tunesi S, Cilia R, Pezzoli G, Goldwurm S. LRRK2-G2019S mutation is not associated with an increased cancer risk: A kin-cohort study. Mov Disord. 2014;29:1325–6.
Saunders-Pullman R, Barrett MJ, Stanley KM, Luciano MS, Shanker V, Severt L, et al. LRRK2 G2019S mutations are associated with an increased cancer risk in Parkinson disease. Mov Disord. 2010;25:2536–41.
Ruiz-Martínez J, de la Riva P, Rodríguez-Oroz MC, Mondragón Rezola E, Bergareche A, Gorostidi A, et al. Prevalence of cancer in Parkinson’s disease related to R1441G and G2019S mutations in LRRK2. Mov Disord. 2014;29:750–5.
Kondo K, Obitsu S, Teshima R. ALPHA.-Synuclein Aggregation and Transmission Are Enhanced by Leucine-Rich Repeat Kinase 2 in Human Neuroblastoma SH-SY5Y Cells. Biol Pharm Bull. 2011;34:1078–83.
Looyenga BD, Furge KA, Dykema KJ, Koeman J, Swiatek PJ, Giordano TJ, et al. Chromosomal amplification of leucine-rich repeat kinase-2 (LRRK2) is required for oncogenic MET signaling in papillary renal and thyroid carcinomas. Proc Natl Acad Sci U S A. 2011;108:1439–44.
Bravo-San Pedro JM, Niso-Santano M, Gómez-Sánchez R, Pizarro-Estrella E, Aiastui-Pujana A, Gorostidi A, et al. The LRRK2 G2019S mutant exacerbates basal autophagy through activation of the MEK/ERK pathway. Cell Mol Life Sci. 2013;70:121–36.
McKinnon PJ. Ataxia telangiectasia: new neurons and ATM. Trends Mol Med. 2001;7:233–4.
Lee Y, McKinnon PJ. Responding to DNA double strand breaks in the nervous system. Neuroscience. 2007;145:1365–74.
Kastan MB, Zhan Q, El-Deiry WS, Carrier F, Jacks T, Walsh WV, et al. A mammalian cell cycle checkpoint pathway utilizing p53 and GADD45 is defective in ataxia-telangiectasia. Cell. 1992;71:587–97.
Matsuoka S, Rotman G, Ogawa A, Shiloh Y, Tamai K, Elledge SJ. ATM phosphorylates Chk2 in vivo and in vitro. Proc Natl Acad Sci U S A. 2000;97:10389–94.
Shiloh Y. ATM and related protein kinases: safeguarding genome integrity. Nat Rev Cancer. 2003;3:155–68.
Friesner JD, Liu B, Culligan K, Britt AB. Ionizing Radiation–dependent γ-H2AX Focus Formation Requires Ataxia Telangiectasia Mutated and Ataxia Telangiectasia Mutated and Rad3-related. Mol Biol Cell. 2005;16:2566–76.
Renwick A, Thompson D, Seal S, Kelly P, Chagtai T, Ahmed M, et al. ATM mutations that cause ataxia-telangiectasia are breast cancer susceptibility alleles. Nat Genet. 2006;38:873–5.
Gumy-Pause F, Wacker P, Sappino A-P. ATM gene and lymphoid malignancies. Leukemia. 2004;18:238–42.
Camins A, Pizarro JG, Alvira D, Gutierrez-Cuesta J, de la Torre AV, Folch J, et al. Activation of ataxia telangiectasia muted under experimental models and human Parkinson’s disease. Cell Mol Life Sci. 2010;67:3865–82.
Petersen AJ, Rimkus SA, Wassarman DA. ATM kinase inhibition in glial cells activates the innate immune response and causes neurodegeneration in Drosophila. Proc Natl Acad Sci U S A. 2012;109:E656–64.
Sunico CR, Nakamura T, Rockenstein E, Mante M, Adame A, Chan SF, et al. S-Nitrosylation of parkin as a novel regulator of p53-mediated neuronal cell death in sporadic Parkinson’s disease. Mol Neurodegener. 2013;8:29.
Jayadev S, Nesser NK, Hopkins S, Myers SJ, Case A, Lee RJ, et al. Transcription factor p53 influences microglial activation phenotype. Glia. 2011;59:1402–13.
Davenport CM, Sevastou IG, Hooper C, Pocock JM. Inhibiting p53 pathways in microglia attenuates microglial-evoked neurotoxicity following exposure to Alzheimer peptides. J Neurochem. 2010;112:552–63.
Li J, Ghiani CA, Kim JY, Liu A, Sandoval J, DeVellis J, et al. Inhibition of p53 transcriptional activity: a potential target for future development of therapeutic strategies for primary demyelination. J Neurosci. 2008;28:6118–27.
Jebelli J, Hooper C, Pocock JM. Microglial p53 activation is detrimental to neuronal synapses during activation-induced inflammation: Implications for neurodegeneration. Neurosci Lett. 2014;583:92–7.
Jebelli JD, Hooper C, Garden GA, Pocock JM. Emerging roles of p53 in glial cell function in health and disease. Glia. 2012;60:515–25.
Desplats P, Spencer B, Crews L, Pathel P, Morvinski-Friedmann D, Kosberg K, et al. Synuclein Induces Alterations in Adult Neurogenesis in Parkinson Disease Models via p53-mediated Repression of Notch1. J Biol Chem. 2012;287:31691–702.
Jacobs WB, Kaplan DR, Miller FD. The p53 family in nervous system development and disease. J Neurochem. 2006;97:1571–84.
Lanni C, Racchi M, Memo M, Govoni S, Uberti D. p53 at the crossroads between cancer and neurodegeneration. Free Radic Biol Med. 2012;52:1727–33.
Maehama T, Dixon JE. The tumor suppressor, PTEN/MMAC1, dephosphorylates the lipid second messenger, phosphatidylinositol 3,4,5-trisphosphate. J Biol Chem. 1998;273:13375–8.
Li J, Yen C, Liaw D, Podsypanina K, Bose S, Wang SI, et al. PTEN, a putative protein tyrosine phosphatase gene mutated in human brain, breast, and prostate cancer. Science. 1997;275:1943–7.
Steck PA, Pershouse MA, Jasser SA, Yung WK, Lin H, Ligon AH, et al. Identification of a candidate tumour suppressor gene, MMAC1, at chromosome 10q23.3 that is mutated in multiple advanced cancers. Nat Genet. 1997;15:356–62.
Myers MP, Pass I, Batty IH, Van der Kaay J, Stolarov JP, Hemmings BA, et al. The lipid phosphatase activity of PTEN is critical for its tumor supressor function. Proc Natl Acad Sci U S A. 1998;95:13513–8.
Carver BS, Chapinski C, Wongvipat J, Hieronymus H, Chen Y, Chandarlapaty S, et al. Reciprocal feedback regulation of PI3K and androgen receptor signaling in PTEN-deficient prostate cancer. Cancer Cell. 2011;19:575–86.
Tan M-H, Mester JL, Ngeow J, Rybicki LA, Orloff MS, Eng C. Lifetime cancer risks in individuals with germline PTEN mutations. Clin Cancer Res. 2012;18:400–7.
Song MS, Salmena L, Pandolfi PP. The functions and regulation of the PTEN tumour suppressor. Nat Rev Mol Cell Biol. 2012;13:283–96.
Lachyankar MB, Sultana N, Schonhoff CM, Mitra P, Poluha W, Lambert S, et al. A role for nuclear PTEN in neuronal differentiation. J Neurosci. 2000;20:1404–13.
Sano T, Lin H, Chen X, Langford LA, Koul D, Bondy ML, et al. Differential expression of MMAC/PTEN in glioblastoma multiforme: relationship to localization and prognosis. Cancer Res. 1999;59:1820–4.
Di Cristofano A, Pesce B, Cordon-Cardo C, Pandolfi PP. Pten is essential for embryonic development and tumour suppression. Nat Genet. 1998;19:348–55.
Groszer M, Erickson R, Scripture-Adams DD, Lesche R, Trumpp A, Zack JA, et al. Negative regulation of neural stem/progenitor cell proliferation by the Pten tumor suppressor gene in vivo. Science. 2001;294:2186–9.
Backman SA, Stambolic V, Suzuki A, Haight J, Elia A, Pretorius J, et al. Deletion of Pten in mouse brain causes seizures, ataxia and defects in soma size resembling Lhermitte-Duclos disease. Nat Genet. 2001;29:396–403.
Kwon CH, Zhu X, Zhang J, Knoop LL, Tharp R, Smeyne RJ, et al. Pten regulates neuronal soma size: a mouse model of Lhermitte-Duclos disease. Nat Genet. 2001;29:404–11.
Park KK, Liu K, Hu Y, Smith PD, Wang C, Cai B, et al. Promoting axon regeneration in the adult CNS by modulation of the PTEN/mTOR pathway. Science. 2008;322:963–6.
Perandones C, Costanzo RV, Kowaljow V, Pivetta OH, Carminatti H, Radrizzani M. Correlation between synaptogenesis and the PTEN phosphatase expression in dendrites during postnatal brain development. Brain Res Mol Brain Res. 2004;128:8–19.
Huang J, Manning BD. A complex interplay between Akt, TSC2 and the two mTOR complexes. Biochem Soc Trans. 2009;37(Pt 1):217–22.
Malagelada C, Jin ZH, Jackson-Lewis V, Przedborski S, Greene LA. Rapamycin Protects against Neuron Death in In Vitro andIn Vivo Models of Parkinson’s Disease. J Neurosci. 2010;30:1166–75.
Bové J, Martínez-Vicente M, Vila M. Fighting neurodegeneration with rapamycin: mechanistic insights. Nat Rev Neurosci. 2011;12:437–52.
Valente EM, Abou-Sleiman PM, Caputo V, Muqit MMK, Harvey K, Gispert S, et al. Hereditary early-onset Parkinson’s disease caused by mutations in PINK1. Science. 2004;304:1158–60.
Rogaeva E, Johnson J, Lang AE, Gulick C, Gwinn-Hardy K, Kawarai T, et al. Analysis of the PINK1 gene in a large cohort of cases with Parkinson disease. Arch Neurol. 2004;61:1898–904.
Kaghad M, Bonnet H, Yang A, Creancier L, Biscan JC, Valent A, et al. Monoallelically expressed gene related to p53 at 1p36, a region frequently deleted in neuroblastoma and other human cancers. Cell. 1997;90:809–19.
Scarffe LA, Stevens DA, Dawson VL, Dawson TM. Parkin and PINK1: much more than mitophagy. Trends Neurosci. 2014;37:315–24.
Matsuda S, Nakanishi A, Minami A, Wada Y, Kitagishi Y. Functions and characteristics of PINK1 and Parkin in cancer. Front Biosci. 2015;20:491–501.
O’Flanagan CH, Morais VA, Wurst W, De Strooper B, O’Neill C. The Parkinson’s gene PINK1 regulates cell cycle progression and promotes cancer-associated phenotypes. Oncogene. 2015;34:1363–74.
O’Flanagan CH, O’Neill C. PINK1 signalling in cancer biology. Biochim Biophys Acta. 1846;2014:590–8.
Raimondi S, Sera F, Gandini S, Iodice S, Caini S, Maisonneuve P, et al. MC1R variants, melanoma and red hair color phenotype: a meta-analysis. Int J Cancer. 2008;122:2753–60.
D’Orazio JA, Nobuhisa T, Cui R, Arya M, Spry M, Wakamatsu K, et al. Topical drug rescue strategy and skin protection based on the role of Mc1r in UV-induced tanning. Nature. 2006;443:340–4.
Wong KY, Rajora N, Boccoli G, Catania A, Lipton JM. A potential mechanism of local anti-inflammatory action of alpha-melanocyte-stimulating hormone within the brain: modulation of tumor necrosis factor-alpha production by human astrocytic cells. Neuroimmunomodulation. 1997;4:37–41.
Teare KA, Pearson RG, Shakesheff KM, Haycock JW. Alpha-MSH inhibits inflammatory signalling in Schwann cells. Neuroreport. 2004;15:493–8.
Xia Y, Wikberg JE, Chhajlani V. Expression of melanocortin 1 receptor in periaqueductal gray matter. Neuroreport. 1995;6:2193–6.
Tell-Marti G, Puig-Butille JA, Potrony M, Badenas C, Mila M, Malvehy J, et al. The MC1R melanoma risk variant p. R160W is associated with Parkinson disease. Ann Neurol. 2015;77:889–94.
Dong J, Gao J, Nalls M, Gao X, Huang X, Han J, et al. Susceptibility loci for pigmentation and melanoma in relation to Parkinson’s disease. Neurobiol Aging. 2014;35:1512. e5–10.
Roe CM, Fitzpatrick AL, Xiong C, Sieh W, Kuller L, Miller JP, et al. Cancer linked to Alzheimer disease but not vascular dementia. Neurology. 2010;74:106–12.
Romero JP, Benito-León J, Louis ED, Bermejo-Pareja F. Alzheimer’s disease is associated with decreased risk of cancer-specific mortality: a prospective study (NEDICES). J Alzheimers Dis. 2014;40:465–73.
Musicco M, Adorni F, Di Santo S, Prinelli F, Pettenati C, Caltagirone C, et al. Inverse occurrence of cancer and Alzheimer disease: a population-based incidence study. Neurology. 2013;81:322–8.
Realmuto S, Cinturino A, Arnao V, Mazzola MA, Cupidi C, Aridon P, et al. Tumor diagnosis preceding Alzheimer’s disease onset: is there a link between cancer and Alzheimer's disease? J Alzheimers Dis. 2012;31:177–82.
Driver JA, Beiser A, Au R, Kreger BE, Splansky GL, Kurth T, et al. Inverse association between cancer and Alzheimer’s disease: results from the Framingham Heart Study. BMJ. 2012;344:e1442.
White RS, Lipton RB, Hall CB, Steinerman JR. Nonmelanoma skin cancer is associated with reduced Alzheimer disease risk. Neurology. 2013;80:1966–72.
Nudelman KNH, Risacher SL, West JD, McDonald BC, Gao S, Saykin AJ, et al. Association of cancer history with Alzheimer’s disease onset and structural brain changes. Front Physiol. 2014;5:423.
Griffin RJ, Moloney A, Kelliher M, Johnston JA, Ravid R, Dockery P, et al. Activation of Akt/PKB, increased phosphorylation of Akt substrates and loss and altered distribution of Akt and PTEN are features of Alzheimer’s disease pathology. J Neurochem. 2005;93:105–17.
Doble BW, Woodgett JR. GSK-3: tricks of the trade for a multi-tasking kinase. J Cell Sci. 2003;116(Pt 7):1175–86.
Stein TD, Johnson JA. Lack of neurodegeneration in transgenic mice overexpressing mutant amyloid precursor protein is associated with increased levels of transthyretin and the activation of cell survival pathways. J Neurosci. 2002;22:7380–8.
Wei W, Wang X, Kusiak JW. Signaling Events in Amyloid β-Peptide-induced Neuronal Death and Insulin-like Growth Factor I Protection. J Biol Chem. 2002;277:17649–56.
Lo RY, Tanner CM, Van Den Eeden SK, Albers KB, Leimpeter AD, Nelson LM. Comorbid cancer in Parkinson’s disease. Mov Disord. 2010;25:1809–17.
Becker C, Brobert GP, Johansson S, Jick SS, Meier CR. Cancer risk in association with Parkinson disease: a population-based study. Parkinsonism Relat Disord. 2010;16:186–90.
Elbaz A, Peterson BJ, Bower JH, Yang P, Maraganore DM, McDonnell SK, et al. Risk of cancer after the diagnosis of Parkinson’s disease: a historical cohort study. Mov Disord. 2005;20:719–25.
Minami Y, Yamamoto R, Nishikouri M, Fukao A, Hisamichi S. Mortality and cancer incidence in patients with Parkinson’s disease. J Neurol. 2000;247:429–34.
Constantinescu R, Elm J, Auinger P, Sharma S, Augustine EF, Khadim L, et al. Malignant melanoma in early-treated Parkinson’s disease: the NET-PD trial. Mov Disord. 2014;29:263–5.
Bertoni JM, Arlette JP, Fernandez HH, Fitzer-Attas C, Frei K, Hassan MN, et al. Increased melanoma risk in Parkinson disease: a prospective clinicopathological study. Arch Neurol. 2010;67:347–52.
Schwid SR, Janice B, David O, Lynn S, Caroline T, Misser F, et al. Cancer incidence in a trial of an antiapoptotic agent for Parkinson’s disease. Mov Disord. 2010;25:1801–8.
Baade PD, Fritschi L, Freedman DM. Mortality due to amyotrophic lateral sclerosis and Parkinson’s disease among melanoma patients. Neuroepidemiology. 2007;28:16–20.
Bellani S, Sousa VL, Ronzitti G, Valtorta F, Meldolesi J, Chieregatti E. The regulation of synaptic function by α-synuclein. Commun Integr Biol. 2010;3:106–9.
Janezic S, Threlfell S, Dodson PD, Dowie MJ, Taylor TN, Potgieter D, et al. Deficits in dopaminergic transmission precede neuron loss and dysfunction in a new Parkinson model. Proc Natl Acad Sci U S A. 2013;110:E4016–25.
Hüls S, Högen T, Vassallo N, Danzer KM, Hengerer B, Giese A, et al. AMPA-receptor-mediated excitatory synaptic transmission is enhanced by iron-induced α-synuclein oligomers. J Neurochem. 2011;117:868–78.
Cooper AA. Synuclein Blocks ER-Golgi Traffic and Rab1 Rescues Neuron Loss in Parkinson’s Models. Science. 2006;313:324–8.
Diógenes MJ, Dias RB, Rombo DM, Vicente Miranda H, Maiolino F, Guerreiro P, et al. Extracellular alpha-synuclein oligomers modulate synaptic transmission and impair LTP via NMDA-receptor activation. J Neurosci. 2012;32:11750–62.
Brück D, Wenning GK, Stefanova N, Fellner L: Glia and alpha-synuclein in neurodegeneration: A complex interaction. Neurobiol Dis 2015. [Epub ahead of print]
Sampaio-Marques B, Felgueiras C, Silva A, Rodrigues M, Tenreiro S, Franssens V, et al. SNCA (α-synuclein)-induced toxicity in yeast cells is dependent on sirtuin 2 (Sir2)-mediated mitophagy. Autophagy. 2012;8:1494–509.
Zhou C, Chen H, Han L, Wang A, Chen L-A. Identification of featured biomarkers in different types of lung cancer with DNA microarray. Mol Biol Rep. 2014;41:6357–63.
Li W-H, Zhang H, Guo Q, Wu X-D, Xu Z-S, Dang C-X, et al. Detection of SNCA and FBN1 methylation in the stool as a biomarker for colorectal cancer. Dis Markers. 2015;2015:657570.
Fung K-M, Kar-Ming F, Rorke LB, Benoit G, Lee VM-Y, Trojanowski JQ. Expression of alpha-, beta-, and gamma-synuclein in glial tumors and medulloblastomas. Acta Neuropathol. 2003;106:167–75.
Matsuo Y, Kamitani T. Parkinson’s Disease-Related Protein, alpha-Synuclein. Malignant Melanoma PLoS ONE. 2010;5:e10481.
Corcoran C, Rani S, O’Driscoll L. miR-34a is an intracellular and exosomal predictive biomarker for response to docetaxel with clinical relevance to prostate cancer progression. Prostate. 2014;74:1320–34.
Cirnaru MD, Marte A, Belluzzi E, Russo I, Gabrielli M, Longo F, et al. LRRK2 kinase activity regulates synaptic vesicle trafficking and neurotransmitter release through modulation of LRRK2 macro-molecular complex. Front Mol Neurosci. 2014;7:49.
Orenstein SJ, Kuo S-H, Tasset I, Arias E, Koga H, Fernandez-Carasa I, et al. Interplay of LRRK2 with chaperone-mediated autophagy. Nat Neurosci. 2013;16:394–406.
Bahnassawy L, Nicklas S, Palm T, Menzl I, Birzele F, Gillardon F, et al. The parkinson’s disease-associated LRRK2 mutation R1441G inhibits neuronal differentiation of neural stem cells. Stem Cells Dev. 2013;22:2487–96.
Ho CC-Y, Rideout HJ, Ribe E, Troy CM, Dauer WT. The Parkinson disease protein leucine-rich repeat kinase 2 transduces death signals via Fas-associated protein with death domain and caspase-8 in a cellular model of neurodegeneration. J Neurosci. 2009;29:1011–6.
Wang X, Yan MH, Fujioka H, Liu J, Wilson-Delfosse A, Chen SG, et al. LRRK2 regulates mitochondrial dynamics and function through direct interaction with DLP1. Hum Mol Genet. 2012;21:1931–44.
Li J-Q, Tan L, Yu J-T. The role of the LRRK2 gene in Parkinsonism. Mol Neurodegener. 2014;9:47.
Parisiadou L, Xie C, Cho HJ, Lin X, Gu X-L, Long C-X, et al. Phosphorylation of ezrin/radixin/moesin proteins by LRRK2 promotes the rearrangement of actin cytoskeleton in neuronal morphogenesis. J Neurosci. 2009;29:13971–80.
Kawakami F, Ichikawa T. The Role of α-Synuclein and LRRK2 in Tau Phosphorylation. Parkinsons Dis. 2015;2015:734746.
Tong Y, Yamaguchi H, Giaime E, Boyle S, Kopan R, Kelleher RJ, et al. Loss of leucine-rich repeat kinase 2 causes impairment of protein degradation pathways, accumulation of α-synuclein, and apoptotic cell death in aged mice. Proc Natl Acad Sci. 2010;107:9879–84.
Winner B, Melrose HL, Zhao C, Hinkle KM, Yue M, Kent C, et al. Adult neurogenesis and neurite outgrowth are impaired in LRRK2 G2019S mice. Neurobiol Dis. 2011;41:706–16.
Helton TD, Otsuka T, Lee M-C, Mu Y, Ehlers MD. Pruning and loss of excitatory synapses by the parkin ubiquitin ligase. Proc Natl Acad Sci U S A. 2008;105:19492–7.
Zhang Y, Gao J, Chung KK, Huang H, Dawson VL, Dawson TM. Parkin functions as an E2-dependent ubiquitin- protein ligase and promotes the degradation of the synaptic vesicle-associated protein, CDCrel-1. Proc Natl Acad Sci U S A. 2000;97:13354–9.
Pickrell AM, Youle RJ. The roles of PINK1, parkin, and mitochondrial fidelity in Parkinson’s disease. Neuron. 2015;85:257–73.
Cesari R, Martin ES, Calin GA, Pentimalli F, Bichi R, McAdams H, et al. Parkin, a gene implicated in autosomal recessive juvenile parkinsonism, is a candidate tumor suppressor gene on chromosome 6q25-q27. Proc Natl Acad Sci U S A. 2003;100:5956–61.
Devireddy S, Liu A, Lampe T, Hollenbeck PJ. The Organization of Mitochondrial Quality Control and Life Cycle in the Nervous System In Vivo in the Absence of PINK1. J Neurosci. 2015;35:9391–401.
Yang Y, Ouyang Y, Yang L, Beal MF, McQuibban A, Vogel H, et al. Pink1 regulates mitochondrial dynamics through interaction with the fission/fusion machinery. Proc Natl Acad Sci U S A. 2008;105:7070–5.
Kitada T, Pisani A, Porter DR, Yamaguchi H, Tscherter A, Martella G, et al. Impaired dopamine release and synaptic plasticity in the striatum of PINK1-deficient mice. Proc Natl Acad Sci U S A. 2007;104:11441–6.
Ye M, Zhou D, Zhou Y, Sun C. Parkinson’s disease-associated PINK1 G309D mutation increases abnormal phosphorylation of Tau. IUBMB Life. 2015;67:286–90.
Park J, Lee SB, Lee S, Kim Y, Song S, Kim S, et al. Mitochondrial dysfunction in Drosophila PINK1 mutants is complemented by parkin. Nature. 2006;441:1157–61.
Jin SM, Youle RJ. PINK1- and Parkin-mediated mitophagy at a glance. J Cell Sci. 2012;125(Pt 4):795–9.
Berthier A, Arnaud B, Samuel N, Judit J-S, Isabel R, Francisca R, et al. PINK1 displays tissue-specific subcellular location and regulates apoptosis and cell growth in breast cancer cells☆. Hum Pathol. 2011;42:75–87.
Devine MJ, Plun-Favreau H, Wood NW. Parkinson’s disease and cancer: two wars, one front. Nat Rev Cancer. 2011;11:812–23.
Kim RH, Smith PD, Aleyasin H, Hayley S, Mount MP, Pownall S, et al. Hypersensitivity of DJ-1-deficient mice to 1-methyl-4-phenyl-1,2,3,6-tetrahydropyrindine (MPTP) and oxidative stress. Proc Natl Acad Sci U S A. 2005;102:5215–20.
Shendelman S, Jonason A, Martinat C, Leete T, Abeliovich A. DJ-1 is a redox-dependent molecular chaperone that inhibits alpha-synuclein aggregate formation. PLoS Biol. 2004;2:e362.
Ariga H, Takahashi-Niki K, Kato I, Maita H, Niki T, Iguchi-Ariga SMM. Neuroprotective Function of DJ-1 in Parkinson’s Disease. Oxid Med Cell Longev. 2013;2013:683920.
Vasseur S, Afzal S, Tardivel-Lacombe J, Park DS, Iovanna JL, Mak TW. DJ-1/PARK7 is an important mediator of hypoxia-induced cellular responses. Proc Natl Acad Sci U S A. 2009;106:1111–6.
McCoy MK, Cookson MR. DJ-1 regulation of mitochondrial function and autophagy through oxidative stress. Autophagy. 2011;7:531–2.
Martinat C, Shendelman S, Jonason A, Leete T, Beal MF, Yang L, et al. Sensitivity to oxidative stress in DJ-1-deficient dopamine neurons: an ES- derived cell model of primary Parkinsonism. PLoS Biol. 2004;2, e327.
Hayashi T, Ishimori C, Takahashi-Niki K, Taira T, Kim Y-C, Maita H, et al. DJ-1 binds to mitochondrial complex I and maintains its activity. Biochem Biophys Res Commun. 2009;390:667–72.
Wang Y, Liu W, He X, Zhou F. Parkinson’s disease-associated DJ-1 mutations increase abnormal phosphorylation of tau protein through Akt/GSK-3β pathways. J Mol Neurosci. 2013;51:911–8.
Kawate T, Iwaya K, Kikuchi R, Kaise H, Oda M, Sato E, et al. DJ-1 protein expression as a predictor of pathological complete remission after neoadjuvant chemotherapy in breast cancer patients. Breast Cancer Res Treat. 2013;139:51–9.
Zeng H-Z, Qu Y-Q, Zhang W-J, Xiu B, Deng A-M, Liang A-B. Proteomic analysis identified DJ-1 as a cisplatin resistant marker in non-small cell lung cancer. Int J Mol Sci. 2011;12:3489–99.
He XY, Liu BY, Yao WY, Zhao XJ, Zheng Z, Li JF, et al. Serum DJ-1 as a diagnostic marker and prognostic factor for pancreatic cancer. J Dig Dis. 2011;12:131–7.
Li Y, Cui J, Zhang C-H, Yang D-J, Chen J-H, Zan W-H, et al. High-expression of DJ-1 and loss of PTEN associated with tumor metastasis and correlated with poor prognosis of gastric carcinoma. Int J Med Sci. 2013;10:1689–97.
Hod Y. Differential control of apoptosis by DJ-1 in prostate benign and cancer cells. J Cell Biochem. 2004;92:1221–33.
Drechsel DN, Hyman AA, Cobb MH, Kirschner MW. Modulation of the dynamic instability of tubulin assembly by the microtubule-associated protein tau. Mol Biol Cell. 1992;3:1141–54.
Mietelska-Porowska A, Wasik U, Goras M, Filipek A, Niewiadomska G. Tau protein modifications and interactions: their role in function and dysfunction. Int J Mol Sci. 2014;15:4671–713.
Pooler AM, Noble W, Hanger DP. A role for tau at the synapse in Alzheimer’s disease pathogenesis. Neuropharmacology. 2014;76:Pt A:1–8.
Souter S, Lee G. Tubulin-independent tau in Alzheimer’s disease and cancer: implications for disease pathogenesis and treatment. Curr Alzheimer Res. 2010;7:697–707.
Rouzier R, Rajan R, Wagner P, Hess KR, Gold DL, Stec J, et al. Microtubule-associated protein tau: a marker of paclitaxel sensitivity in breast cancer. Proc Natl Acad Sci U S A. 2005;102:8315–20.
Smoter M, Bodnar L, Grala B, Stec R, Zieniuk K, Kozlowski W, et al. Tau protein as a potential predictive marker in epithelial ovarian cancer patients treated with paclitaxel/platinum first-line chemotherapy. J Exp Clin Cancer Res. 2013;32:25.
Priller C, Bauer T, Mitteregger G, Krebs B, Kretzschmar HA, Herms J. Synapse formation and function is modulated by the amyloid precursor protein. J Neurosci. 2006;26:7212–21.
Thinakaran G, Koo EH. Amyloid Precursor Protein Trafficking, Processing, and Function. J Biol Chem. 2008;283:29615–9.
Müller UC, Zheng H. Physiological functions of APP family proteins. Cold Spring Harb Perspect Med. 2012;2:a006288.
Baldus CD, Liyanarachchi S, Mrózek K, Auer H, Tanner SM, Guimond M, et al. Acute myeloid leukemia with complex karyotypes and abnormal chromosome 21: Amplification discloses overexpression of APP, ETS2, and ERG genes. Proc Natl Acad Sci U S A. 2004;101:3915–20.
Yamada Y, Fujimura T, Takahashi S, Takayama K, Urano T, Murata T, et al. Clinical significance of amyloid precursor protein in patients with testicular germ cell tumor. Adv Urol. 2013;2013:348438.
Levine AJ, Jamil M, Finlay CA. The p53 tumour suppressor gene. Nature. 1991;351:453–6.
Lee J-H, Paull TT. ATM activation by DNA double-strand breaks through the Mre11-Rad50-Nbs1 complex. Science. 2005;308:551–4.
Thompson D, Duedal S, Kirner J, McGuffog L, Last J, Reiman A, et al. Cancer risks and mortality in heterozygous ATM mutation carriers. J Natl Cancer Inst. 2005;97:813–22.
Prokopcova J, Jana P, Zdenek K, Banwell CM, Petr P. The role of ATM in breast cancer development. Breast Cancer Res Treat. 2006;104:121–8.
Bishop DT, Demenais F, Iles MM, Harland M, Taylor JC, Corda E, et al. Genome-wide association study identifies three loci associated with melanoma risk. Nat Genet. 2009;41:920–5.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DF and WC wrote and XC revised the review. All authors read and approved the final manuscript.
Danielle D. Feng and Waijiao Cai contributed equally to this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Feng, D.D., Cai, W. & Chen, X. The associations between Parkinson’s disease and cancer: the plot thickens. Transl Neurodegener 4, 20 (2015). https://doi.org/10.1186/s40035-015-0043-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40035-015-0043-z