Abstract
α-Synuclein is an abundantly expressed neuronal protein that is at the center of focus in understanding a group of neurodegenerative disorders called α-synucleinopathies, which are characterized by the presence of aggregated α-synuclein intracellularly. Primary α-synucleinopathies include Parkinson's disease (PD), dementia with Lewy bodies and multiple system atrophy, with α-synuclein also found secondarily in a number of other diseases, including Alzheimer's disease. Understanding how α-synuclein aggregates form in these different disorders is important for the understanding of its pathogenesis in Lewy body diseases. PD is the most prevalent of the α-synucleinopathies and much of the initial research on α-synuclein Lewy body pathology was based on PD but is also relevant to Lewy bodies in other diseases (dementia with Lewy bodies and Alzheimer's disease). Polymorphism and mutation studies of SNCA, the gene that encodes α-synuclein, provide much evidence for a causal link between α-synuclein and PD. Among the primary α-synucleinopathies, multiple system atrophy is unique in that α-synuclein deposition occurs in oligodendrocytes rather than neurons. It is unclear whether α-synuclein originates from oligodendrocytes or whether it is transmitted somehow from neurons. α-Synuclein exists as a natively unfolded monomer in the cytosol, but in the presence of lipid membranes it is thought to undergo a conformational change to a folded α-helical secondary structure that is prone to forming dimers and oligomers. Posttranslational modification of α-synuclein, such as phosphorylation, ubiquitination and nitration, has been widely implicated in α-synuclein aggregation process and neurotoxicity. Recent studies using animal and cell models, as well as autopsy studies of patients with neuron transplants, provided compelling evidence for prion-like propagation of α-synuclein. This observation has implications for therapeutic strategies, and much recent effort is focused on developing antibodies that target extracellular α-synuclein.
Similar content being viewed by others
Introduction
α-synucleinis a 140 amino acid, natively unfolded protein predominantly localized in the presynaptic terminals of neurons. In the past two decades α-synucleinhas been the center of focus in understanding the etiology of a group of overlapping neurodegenerative disorders called α-synucleinopathies, which includes Parkinson's disease (PD), Parkinson's disease dementia (PDD), dementia with Lewy bodies (DLB), multiple system atrophy (MSA) and a number of less-well characterized neuroaxonal dystrophies. α-synucleinis encoded by the SNCA gene on 4q21, and was first identified as the nonamyloid component of β-amyloid plaques in the brain of patients with Alzheimer's disease (AD) [1]. Although AD is pathologically quite distinct from α-synucleinopathies, α-synucleinaggregates have been found in the majority of AD brains, mostly restricted to the amygdala [2],[3]. Despite much research into α-synucleinbiology, the exact function of α-synucleinis still elusive. α-synucleinis thought to play a role in maintaining a supply of synaptic vesicles in presynaptic terminals. The protein has also been suggested to be involved in regulating the release of the neurotransmitter dopamine in controlling voluntary and involuntary movements.
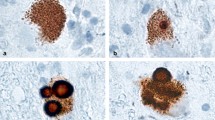
The universal feature of α-synucleinopathies is the presence of proteinaceous intracellular entities or bodies containing aggregates of α-synuclein. These bodies differ somewhat in appearance in different α-synucleinopathies, and are called Lewy bodies in PD and DLB [4], glial cytoplasmic inclusions in MSA [5] and axonal spheroids in neuroaxonal dystrophies [6]. Much evidence indicates that the mechanism underpinning α-synucleinopathies is the misfolding of α-synucleininto aggregates [4]. In vitro studies have shown that α-synucleinaggregates (that is, oligomers) cause a series of secondary processes leading to neuroinflammation, neurodegeneration and cell death [7]. Apart from the pathogenic dogma of neurotoxicity of aggregated α-synuclein, loss of α-synucleinmonomers (that is, loss of function) from their physiological location may also contribute to neurodegeneration [8]. A radical idea of prion-like propagation has been proposed for α-synucleintransmission between cells. New developments in α-synucleintransmission highlight the importance of extracellular α-synucleinin therapeutic strategies. In this review we will discuss α-synucleinbiology, α-synucleinopathies and recent developments in α-synucleindisease mechanisms and therapies.
α-synucleinbiology
α-synucleinis abundantly expressed in the human brain, making up as much as 1% of protein content in the cytosol. This protein is expressed throughout the brain, with high levels in the neocortex, hippocampus, substantia nigra, thalamus and cerebellum. It is predominantly expressed in neurons and to a lesser extent in glial cells. Apart from the predominant 140 amino acid protein, there are at least two other alternatively spliced variants of the protein; the 126 amino acid and 112 amino acid variants that lack exon 3 and exon 5, respectively [9]. The α-synucleinprotein has three distinct structural domains. The amphipathic N-terminal region (residues 1 to 60) contains 11 amino acid repeats including the consensus sequence KTKEGV, which is important in α-helix formation [10]. The central hydrophobic region (residues 61 to 95) contains the nonamyloid component region, which is important in protein aggregation [4]. Finally, the C-terminal region (residues 96 to 140) is highly acidic and proline rich.
α-synucleinis encoded by the SNCA gene. PD genome-wide association studies have shown that single nucleotide polymorphisms in SNCA are strongly associated with an increased risk for idiopathic PD [11]-[14]. The SNCA missense mutation Ala53Thr was the first causal mutation identified in dominantly inherited PD [15]. Several SNCA missense mutations (for example, Glu46Lys, His50Gln, Gly51Asp and Ala30Pro) have since been identified in dominantly inherited PD [16]-[19]. In 1998 Conway and colleagues demonstrated that SNCA missense mutations accelerated α-synucleinfibril formation in vitro, implicating α-synucleinmisfolding and aggregation in PD pathogenesis [20]. SNCA duplication and triplication have also been identified in PD subjects [21]-[25].
Although the exact function of α-synucleinis unknown, α-synucleinis thought to play a role in maintaining a supply of synaptic vesicles in mature presynaptic terminals, because its expression was detected only after synaptic development [26]. In vitro knockdown studies showed that α-synucleinregulates the quantity of different pools of synaptic vesicles in mature neurons [26], influencing synaptic activity as a molecular chaperone in the formation of SNARE complexes [27], a requirement for presynaptic nerve terminal release of neurotransmitters [28]. In this way, α-synucleinmay regulate the release of dopamine in controlling voluntary and involuntary movements, or might influence memory and cognitive function as shown in SNCA knockout mice [29]. This function of α-synucleinbecomes more important during increased synaptic activity and aging, and could be a contributory factor in neurodegeneration.
Posttranslational modification of α-synuclein
Posttranslational modification of α-synucleinis prevalent and altered α-synucleinproteins impact on a number of pathological processes, including α-synucleinaggregation, Lewy body formation and neurotoxicity. The most common posttranslational modification of α-synucleinis phosphorylation, which occurs predominantly at serine residues S129 and, to a lesser extent, S87 and at tyrosine residues Y125, Y133 and Y135 [30],[31]. In DLB brains, approximately 90% of insoluble α-synucleinis phosphorylated at S129 compared with only 4% in soluble cytosolic α-synuclein[32], implicating phosphorylated α-synucleinin the process of α-synucleinaggregation.
The second most common posttranslational modification of α-synuclein is ubiquitination - the attachment of ubiquitin to α-synuclein at lysine residues. Although α-synuclein contains 15 lysine residues, α-synuclein isolated from Lewy bodies shows that the protein is ubiquitinated mainly at K6, K10 and K12 residues. Ubiquitination of α-synuclein causes changes in α-synuclein function/activity, impacting on α-synuclein localization and α-synuclein degradation processes [33]-[35].
Another common posttranslational modification of α-synuclein is nitration - the attachment of a nitro molecule to α-synuclein at tyrosine residues (Y39, Y125, Y133 and Y136). High concentrations of nitrated α-synuclein are found in Lewy bodies [36]. Nitration of α-synuclein is enhanced under conditions of elevated oxidative stress, which is widely regarded as an important factor in Lewy body diseases. In vitro studies have shown that nitration of α-synuclein induced α-synuclein oligomer formation and mitochondrial impairment, leading to apoptosis via the integrin pathway [37]. In a PD cell model, nitration of α-synuclein (via increased nitric oxide production) caused increases in the level of neurotoxic α-synuclein species and cell death [38].
Prion-like propagation of α-synuclein
In 2008, two autopsy studies of patients with PD who survived more than 10 years after receiving successful transplants of embryonic dopamine neurons to treat their disease observed that the surviving transplanted neurons had α-synuclein accumulation in typical Lewy bodies [39],[40]. The only way these neurons could have such pathology was by a propagating mechanism, a concept of transmission more commonly associated with prion diseases [41]. It should be noted that Braak and colleagues had in 2003 proposed a transmissible mechanism for α-synuclein propagation based on observations that the disease seemed to start in the nose and/or gut and progress to invade the brain in a staged manner [42],[43]. A number of subsequent studies in animal and cell culture models have proven this concept of transmission of α-synuclein between neurons, showing that exogenous α-synucleininduces Lewy body pathology along neuroanatomical pathways in the brain (for example [44]-[48]). It should be noted that it is the conformation of the protein that is transmitted to endogenous protein residing within neurons, as in mouse models the aggregates from exogenous sources disappear in about a week with endogenous aggregates beginning around 3 months later [49]. This observation suggests that a particular strain of α-synuclein is transmitted between neurons.
Consistent with the concept of different prion strains [50], a number of studies have now identified and characterized different strains of α-synuclein. Strains made in vivo exhibit fundamentally different properties, including the packing of their building blocks and growth and amplification properties, as well as their tropism, cellular binding and penetration properties and toxicity [51],[52]. These differences can be exaggerated by modifying the solution concentration, molecular crowding, agitation, temperature, pH and ionic strength [53]. Exogenous factors that accelerate the in vitro aggregation of α-synuclein include agrochemicals, polycations, histones, metal ions, glycosaminoglycans, sodium dodecyl sulfate and organic solvents, while factors that inhibit α-synuclein aggregation include small chemical compounds, heat shock proteins, PAMAM dendrimers, α-synuclein and α-synuclein, catecholamines, phospholipids, rifampicin, trehalose and oxidative modifications [53]. The combination of different factors may impact on the strains of α-synuclein in different people and may explain some of the heterogeneity that is known both clinically and pathologically, and especially in the dynamics of the different types of Lewy body diseases [54]. Morphological and structural differences have been noted in patients with Lewy bodies consistent with the concept of different α-synuclein strains - Lewy bodies in the brainstem are morphologically different from those in the cortex [55], and conformationally different strains of α-synuclein have been identified from cortical tissue samples of patients with PD depending on the presence or absence of Alzheimer pathologies [52].
Binding and interaction of α-synucleinwith lipid membranes
Under normal conditions, α-synucleinexists as a randomly structured and natively unfolded protein and remains as a monomer within the cytoplasm. Under pathological conditions, however, α-synucleinundergoes structural/conformational changes causing the monomers to aggregate with each other and become insoluble. Much evidence suggests that changes to the α-synucleinstructure and properties are initiated when the protein binds and interacts with lipid surfaces, such as lipid droplets, phospholipid bilayers or lipid membranes. When α-synucleinmonomers, isolated from human neurons, were exposed to synthetic lipid membranes, they readily bound to the membrane surface and formed dimers and oligomers [56],[57]. Such an interaction is thought to induce a dramatic change in α-synucleinstructure from its unfolded form to a folded α-helical secondary structure [57]. The imperfect repeats of 11 amino acids present in α-synuclein, similar to the amphipathic α-helical motif common to apolipoproteins and other lipid-binding proteins, appear to play an important role in the lipid membrane binding process [58]. What is significant about such a change is that the α-helical form of α-synucleinis prone to forming different types of oligomers, the species that are thought to be toxic to cells. The lipid composition of membranes has been shown to affect the binding/interaction of α-synucleinto the membrane and subsequent oligomerization [56],[59]. α-synucleinis thought to preferentially bind to regions of membranes that are enriched in lipids [60]. These regions are called lipid rafts and are characterized by high concentrations of cholesterol and sphingolipids and altered surface charge that may favor α-synucleinbinding. The lipid rafts appear to serve as a platform that promotes α-synucleinbinding and oligomerization.
Contrary to overwhelming evidence that α-synuclein exists as an unfolded monomer in the cytosol, Bartels and colleagues reported that endogenous α-synuclein exists predominantly as a folded tetramer (~58 kDa) [61]. The explanation provided by the authors for this apparent difference is that most studies claiming the unfolded monomer hypothesis commonly use sample heating and denaturing gels to analyze α-synuclein, whereas the authors used nondenaturing conditions. They have also provided evidence by other means - that is, scanning transmission electron microscopy and cell cross-linking - to confirm the prevalence of α-synuclein tetramer in neurons and human brain tissues [61]. Bartels and colleagues proposed that since α-synuclein tetramers are less likely to form aggregates, the tetramers first undergo destabilization prior to forming aggregates. The authors suggested that stabilizing the physiological tetramers could reduce Contrary to overwhelming evidence that-synuclein pathogenicity in PD and other α-synucleinopathies.
Dementia with Lewy bodies
DLB was initially identified as a dementia syndrome with Lewy body pathology [62], which is now incorporated in the Diagnostic and Statistical Manual criteria as a clinical disease entity (neurocognitive disorder with Lewy bodies). Current objective data suggest that the sensitivity of accurate clinical diagnosis is very low, however, with most clinical cases identified actually having AD rather than DLB at autopsy [63]-[68], and therefore current diagnostic criteria for DLB exclude cases with coexisting AD pathology [62]. Although DLB remains easy to identify pathologically with different cellular pathologies differentiating it from other dementia syndromes, pathological identification using only Lewy body pathology has been shown to be inaccurate due to overlap with patients without dementia symptoms. Current neuropathological criteria state that neurocognitive syndromes with Lewy bodies are most likely when Lewy bodies are prevalent in at least limbic brain regions, but are also often found in association neocortices [69]. A number of studies have shown that a combination of cellular pathologies, which include α-synucleinand β-amyloid deposition as well as dopamine denervation, assist with differentiating this dementia syndrome from others [54]. Approximately 25% of DLB patients display significant parkinsonian symptoms at the onset of disease, consistent with an early dopamine denervation, whereas 25% of DLB patients never develop any parkinsonian symptoms and have less significant dopamine loss. DLB is best conceptualized as a dominant dementia syndrome with multiple pathologies that include Lewy bodies and more frequently has multiple pathologies compared with AD [70]. The diversity of clinical phenotypes associated with DLB is likely to reflect the timing and different combinations of these pathologies within different brain regions.
Because of the difficulty in obtaining clinically proven cases with pathological DLB, studies of the underlying molecular changes in the brain are rare. Interesting pathological differences have been noted - the longer the duration of parkinsonism prior to dementia onset, the less severe the cortical α-synuclein and α-amyloid deposition as well as the cortical cholinergic deficit [71]. DLB patients present significant cholinergic deficits [72]-[74] and a decrease in serum α-synuclein [75].
Parkinson's disease and Parkinson's disease dementia
In contrast to DLB, which is a dominant dementia syndrome, PD is a dominant movement disorder characterized by the presence of two of four cardinal signs (that is, bradykinesia, rigidity, resting tremor, gait instability) that are responsive to levodopa therapy [76]. Current neuropathological criteria require moderate to severe loss of pigmented dopamine neurons in the substantia nigra along with Lewy bodies at least in the brainstem [69]. PDD was defined in 2007 as a dementia syndrome in patients with an initial diagnosis of PD for more than 1 year [77] and, as stated above for DLB, the cognitive symptoms are thought to occur when Lewy bodies are prevalent in at least limbic brain regions, but often also in association neocortices [69]. A smaller proportion of people with PDD have multiple pathologies [78] as observed in most DLB cases (see above).
Changes in the phosphorylation and solubility of α-synuclein occur prior to Lewy body formation in PD and PDD [79]-[81]. In terms of solubility, the amount of soluble α-synuclein is not substantially increased and actually decreases slightly over the course of PD [79],[82]. The levels of phosphorylation of α-synuclein greatly increase prior to Lewy body formation [79]-[81] and the Lewy body formation correlates with an enhanced lipid association of α-synuclein [79]. In a longitudinal study of patients with PD it took an average 13 years for the propagation of Lewy body aggregates to reach limbic brain regions, and 18 years before aggregates occurred in association cortices in 50% of PD cases [83]. These studies show that the intracellular changes in α-synuclein take considerable time to propagate and that posttranslational modifications of α-synuclein are substantial prior to its irreversible fibrilization.
Multiple system atrophy
MSA is a rapidly progressive neurodegenerative disease characterized by the clinical triad of parkinsonism (similar to PD), cerebellar ataxia and autonomic failure. The distribution of pathology classically encompasses three functional systems in the central nervous system - the striatonigral system, the olivopontocerebellar system and the autonomic system - impacting on movement, muscle control, blood pressure, heart rate and bladder function [84],[85]. Like PD and DLB, the dominant histopathology of MSA is the presence of misfolded and fibrillar α-synuclein in the cytoplasm. However, unlike PD and DLB, the principal site for α-synuclein deposition is in the oligodendrocytes rather than neurons. Based on current information, the sequence of pathological events in MSA is now recognized as myelin dysregulation first, followed by demyelination and then neurodegeneration and loss of neurons [86]-[88]; neurodegeneration therefore appears to be a secondary effect in MSA.
No causal mutations or multiplications of the coding sequence of α-synuclein have been identified in MSA cases [89]-[91], although the search is not exhaustive because MSA is a rare disease. Earlier studies, based on small numbers of MSA cases, have reported that genetic variants of SNCA were associated with MSA [92]-[94]; however, a recent pioneering genome-wide association study of 918 MSA cases and 3,884 controls found no risk-conferring loci on the SNCA gene [95]. Posttranslational modification studies of α-synuclein in MSA have shown that phosphorylation and ubiquitination are implicated in the deposition of α-synuclein [96], although no definitively causative relationships have yet been established. Furthermore, the origin of α-synucleinin oligodendrocytes remains stubbornly enigmatic. Although the evidence of significant physiological expression of α-synucleinin mature oligodendrocytes is conflicting [97]-[99], it has been proposed that upregulation of the SNCA gene in these cells could be the cause of α-synucleinaggregation. Nevertheless, successful animal models of MSA, which recapitulate both neuropathological and clinical features, have been generated by overexpression of α-synucleinin the oligodendrocytes [96],[100],[101]. Alternatively, aberrant uptake of α-synucleinfrom the extracellular environment has also been proposed as a possible mechanism of α-synucleinaggregation in oligodendrocytes [97],[102],[103].
Lewy body pathology in Alzheimer's disease
Although Lewy bodies are the pathological hallmark of PD and DLB, recent studies suggest a considerable proportion of AD brains show α-synucleinpathology. In a recent study of 22 clinically diagnosed cases of AD, 10 were found to have α-synucleinimmunoreactive Lewy bodies by subsequent pathological examination [104]. Other studies showed that as many as one-half of patients with AD, including both sporadic and familial cases, have α-synucleinaggregates [2],[105]-[107]. In these studies, α-synucleinaggregates were mostly restricted to the amygdala, implying that the spread of α-synucleininclusions is different to that of PD. Lewy pathology in AD has also been reported to be formed mainly in the cell body of neurons, and not in the axonal terminals and dendrites as in PD [107],[108]. The Lewy pathology therefore possibly mirrors a nonspecific end stage of AD. However, genetic or lifestyle factors might prime neurons to accumulate α-synucleinaggregates in a subset of AD patients, and thus α-synucleinaggregates might reflect a causal pathogenic mechanism in AD.
Several studies show that high levels of AD pathology are often observed in patients with PD and DLB [78] and correlate with the decline in cognitive function more than the amount of α-synucleinaggregates [109]-[111]. Interestingly, PD/DLB cases with AD pathology have higher α-synucleinlevels in cortical and limbic areas than cases without AD pathology [112], which implies a possible interaction between α-synucleinand AD pathology in these disorders. How the pathologies of α-synuclein, β-amyloid and tau relate to each other in PD and AD is poorly understood. Recent work using a transgenic mouse model of DLB-AD provides some clues to the interaction between β-amyloid, tau and α-synuclein[113]. This mouse model was generated from a cross between 3 × Tg-AD mice and mice that express the A53T mutation in α-synuclein[114]. The DLB-AD mice exhibited accelerated cognitive decline, compared with 3 × Tg-AD mice alone, with more severe β-amyloid, tau and α-synucleinpathologies [113]. These data suggest that the three pathologies interact and somehow enhance each other, resulting in accelerated cognitive dysfunction.
Therapeutic strategies
Because of the marked cholinergic deficit associated with DLB (see above), cholinesterase inhibitors are routinely used for clinical improvement [115]. In PDD these agents have been shown to improve cognitive function, behavioral disturbances and activities of daily living [115]. Their effect in DLB is less clear [115], potentially because DLB is poorly diagnosed clinically and often has multiple underlying pathologies (see above). Interestingly, successful treatment with cholinesterase inhibitors was shown to decrease β-amyloid deposition in a small study of DLB patients [116], suggesting that these drugs have mechanistic as well as symptomatic effects. Considering the molecular events surrounding α-synucleindeposition, a number of strategies are being developed [117],[118]. These strategies include small anti-aggregating molecules and chaperones [119]-[123], but perhaps the most promising strategy is the development of antibody therapies for α-synuclein. These therapies target extracellular α-synucleinbinding the protein to reduce its self-aggregation and increase its clearance, with a number of antibodies already in production [124]-[127]. Another promising development is the use of the β-lactum antibiotic ceftriaxone as a therapeutic agent to block α-synucleinaggregation [128], although the macrocyclic antibiotic rifampicin has not been successful in MSA [129].
Conclusions
The assessment of different α-synucleinopathies focuses on a variety of mechanisms that affect the pathogenesis of Lewy body diseases. While all α-synucleinopathies are characterized by α-synuclein aggregates with similar posttranslational modifications and lipid associations, the cell type involved, their location and their association with other protein depositions vary substantially, and recent data suggest that perhaps the strain of α-synucleininvolved may also differ. An increase in α-synuclein is hypothesized to precipitate the protein's aggregation, and this is evident in some familial forms of PD, but the precipitating events for most of the α-synucleinopathies remain to be determined. It is clear for Lewy body disorders that the neuronal propagation can be slow or rapid, and is impacted on by AD pathology; however, Lewy bodies in AD are focused in the amygdala, suggesting that the initiating region of α-synuclein aggregation in the brain can be diverse. Importantly, the concept of propagation of α-synuclein pathology between neurons has resulted in the development of new therapies that target this mechanism with the potential to halt or slow this aspect of Lewy body diseases.
Abbreviations
- AD:
-
Alzheimer's disease
- DLB:
-
Dementia with Lewy bodies
- MSA:
-
Multiple system atrophy
- PD:
-
Parkinson's disease
- PDD:
-
Parkinson's disease dementia
References
Ueda K, Fukushima H, Masliah E, Xia Y, Iwai A, Yoshimoto M, Otero DA, Kondo J, Ihara Y, Saitoh T: Molecular cloning of cDNA encoding an unrecognized component of amyloid in Alzheimer disease. Proc Natl Acad Sci U S A. 1993, 90: 11282-11286.
Lippa CF, Fujiwara H, Mann DM, Giasson B, Baba M, Schmidt ML, Nee LE, O'Connell B, Pollen DA, St George-Hyslop P, Ghetti B, Nochlin D, Bird TD, Cairns NJ, Lee VM, Iwatsubo T, Trojanowski JQ: Lewy bodies contain altered alpha-synuclein in brains of many familial Alzheimer's disease patients with mutations in presenilin and amyloid precursor protein genes. Am J Pathol. 1998, 153: 1365-1370.
Arai Y, Yamazaki M, Mori O, Muramatsu H, Asano G, Katayama Y: Alpha-synuclein-positive structures in cases with sporadic Alzheimer's disease: morphology and its relationship to tau aggregation. Brain Res. 2001, 888: 287-296.
Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M: Alpha-synuclein in Lewy bodies. Nature. 1997, 388: 839-840.
Gai WP, Power JH, Blumbergs PC, Blessing WW: Multiple-system atrophy: a new alpha-synuclein disease?. Lancet. 1998, 352: 547-548.
Newell KL, Boyer P, Gomez-Tortosa E, Hobbs W, Hedley-Whyte ET, Vonsattel JP, Hyman BT: Alpha-synuclein immunoreactivity is present in axonal swellings in neuroaxonal dystrophy and acute traumatic brain injury. J Neuropathol Exp Neurol. 1999, 58: 1263-1268.
Wolozin B, Behl C: Mechanisms of neurodegenerative disorders: part 1: protein aggregates. Arch Neurol. 2000, 57: 793-796.
Lashuel HA, Overk CR, Oueslati A, Masliah E: The many faces of alpha-synuclein: from structure and toxicity to therapeutic target. Nat Rev Neurosci. 2013, 14: 38-48.
Beyer K: Alpha-synuclein structure, posttranslational modification and alternative splicing as aggregation enhancers. Acta Neuropathol. 2006, 112: 237-251.
Clayton DF, George JM: The synucleins: a family of proteins involved in synaptic function, plasticity, neurodegeneration and disease. Trends Neurosci. 1998, 21: 249-254.
Pals P, Lincoln S, Manning J, Heckman M, Skipper L, Hulihan M, Van den Broeck M, De Pooter T, Cras P, Crook J, Van Broeckhoven C, Farrer MJ: alpha-Synuclein promoter confers susceptibility to Parkinson's disease. Ann Neurol. 2004, 56: 591-595.
Rajput A, Vilarino-Guell C, Rajput ML, Ross OA, Soto-Ortolaza AI, Lincoln SJ, Cobb SA, Heckman MG, Farrer MJ: Alpha-synuclein polymorphisms are associated with Parkinson's disease in a Saskatchewan population. Mov Disord. 2009, 24: 2411-2414.
Pankratz N, Wilk JB, Latourelle JC, DeStefano AL, Halter C, Pugh EW, Doheny KF, Gusella JF, Nichols WC, Foroud T, Myers RH: Genome-wide association study for susceptibility genes contributing to familial Parkinson disease. Hum Genet. 2009, 124: 593-605.
Maraganore DM, de Andrade M, Elbaz A, Farrer MJ, Ioannidis JP, Kruger R, Rocca WA, Schneider NK, Lesnick TG, Lincoln SJ, Hulihan MM, Aasly JO, Ashizawa T, Chartier-Harlin MC, Checkoway H, Ferrarese C, Hadjigeorgiou G, Hattori N, Kawakami H, Lambert JC, Lynch T, Mellick GD, Papapetropoulos S, Parsian A, Quattrone A, Riess O, Tan EK, Van Broeckhoven C: Collaborative analysis of alpha-synuclein gene promoter variability and Parkinson disease. JAMA. 2006, 296: 661-670.
Polymeropoulos MH, Lavedan C, Leroy E, Ide SE, Dehejia A, Dutra A, Pike B, Root H, Rubenstein J, Boyer R, Stenroos ES, Chandrasekharappa S, Athanassiadou A, Papapetropoulos T, Johnson WG, Lazzarini AM, Duvoisin RC, Di Iorio G, Golbe LI, Nussbaum RL: Mutation in the alpha-synuclein gene identified in families with Parkinson's disease. Science. 1997, 276: 2045-2047.
Kruger R, Kuhn W, Muller T, Woitalla D, Graeber M, Kosel S, Przuntek H, Epplen JT, Schols L, Riess O: Ala30Pro mutation in the gene encoding alpha-synuclein in Parkinson's disease. Nat Genet. 1998, 18: 106-108.
Zarranz JJ, Alegre J, Gomez-Esteban JC, Lezcano E, Ros R, Ampuero I, Vidal L, Hoenicka J, Rodriguez O, Atares B, Llorens V, Gomez Tortosa E, del Ser T, Munoz DG, de Yebenes JG: The new mutation, E46K, of alpha-synuclein causes Parkinson and Lewy body dementia. Ann Neurol. 2004, 55: 164-173.
Proukakis C, Dudzik CG, Brier T, MacKay DS, Cooper JM, Millhauser GL, Houlden H, Schapira AH: A novel alpha-synuclein missense mutation in Parkinson disease. Neurology. 2013, 80: 1062-1064.
Lesage S, Anheim M, Letournel F, Bousset L, Honore A, Rozas N, Pieri L, Madiona K, Durr A, Melki R, Verny C, Brice A: G51D alpha-synuclein mutation causes a novel Parkinsonian-pyramidal syndrome. Ann Neurol. 2013, 73: 459-471.
Conway KA, Harper JD, Lansbury PT: Accelerated in vitro fibril formation by a mutant alpha-synuclein linked to early-onset Parkinson disease. Nat Med. 1998, 4: 1318-1320.
Singleton AB, Farrer M, Johnson J, Singleton A, Hague S, Kachergus J, Hulihan M, Peuralinna T, Dutra A, Nussbaum R, Lincoln S, Crawley A, Hanson M, Maraganore D, Adler C, Cookson MR, Muenter M, Baptista M, Miller D, Blancato J, Hardy J, Gwinn-Hardy K: alpha-Synuclein locus triplication causes Parkinson's disease. Science. 2003, 302: 841-
Chartier-Harlin MC, Kachergus J, Roumier C, Mouroux V, Douay X, Lincoln S, Levecque C, Larvor L, Andrieux J, Hulihan M, Waucquier N, Defebvre L, Amouyel P, Farrer M, Destee A: Alpha-synuclein locus duplication as a cause of familial Parkinson's disease. Lancet. 2004, 364: 1167-1169.
Ibanez P, Bonnet AM, Debarges B, Lohmann E, Tison F, Pollak P, Agid Y, Durr A, Brice A: Causal relation between alpha-synuclein gene duplication and familial Parkinson's disease. Lancet. 2004, 364: 1169-1171.
Fuchs J, Nilsson C, Kachergus J, Munz M, Larsson EM, Schule B, Langston JW, Middleton FA, Ross OA, Hulihan M, Gasser T, Farrer MJ: Phenotypic variation in a large Swedish pedigree due to SNCA duplication and triplication. Neurology. 2007, 68: 916-922.
Nishioka K, Ross OA, Ishii K, Kachergus JM, Ishiwata K, Kitagawa M, Kono S, Obi T, Mizoguchi K, Inoue Y, Imai H, Takanashi M, Mizuno Y, Farrer MJ, Hattori N: Expanding the clinical phenotype of SNCA duplication carriers. Mov Disord. 2009, 24: 1811-1819.
Murphy DD, Rueter SM, Trojanowski JQ, Lee VM: Synucleins are developmentally expressed, and alpha-synuclein regulates the size of the presynaptic vesicular pool in primary hippocampal neurons. J Neurosci. 2000, 20: 3214-3220.
Bonini NM, Giasson BI: Snaring the function of alpha-synuclein. Cell. 2005, 123: 359-361.
Burre J, Sharma M, Tsetsenis T, Buchman V, Etherton MR, Sudhof TC: Alpha-synuclein promotes SNARE-complex assembly in vivo and in vitro. Science. 2010, 329: 1663-1667.
Kokhan VS, Afanasyeva MA, Van'kin GI: alpha-Synuclein knockout mice have cognitive impairments. Behav Brain Res. 2012, 231: 226-230.
Okochi M, Walter J, Koyama A, Nakajo S, Baba M, Iwatsubo T, Meijer L, Kahle PJ, Haass C: Constitutive phosphorylation of the Parkinson's disease associated alpha-synuclein. J Biol Chem. 2000, 275: 390-397.
Nakamura T, Yamashita H, Takahashi T, Nakamura S: Activated Fyn phosphorylates alpha-synuclein at tyrosine residue 125. Biochem Biophys Res Commun. 2001, 280: 1085-1092.
Anderson JP, Walker DE, Goldstein JM, de Laat R, Banducci K, Caccavello RJ, Barbour R, Huang J, Kling K, Lee M, Diep L, Keim PS, Shen X, Chataway T, Schlossmacher MG, Seubert P, Schenk D, Sinha S, Gai WP, Chilcote TJ: Phosphorylation of Ser-129 is the dominant pathological modification of alpha-synuclein in familial and sporadic Lewy body disease. J Biol Chem. 2006, 281: 29739-29752.
Nonaka T, Iwatsubo T, Hasegawa M: Ubiquitination of alpha-synuclein. Biochemistry. 2005, 44: 361-368.
House CM, Hancock NC, Moller A, Cromer BA, Fedorov V, Bowtell DD, Parker MW, Polekhina G: Elucidation of the substrate binding site of Siah ubiquitin ligase. Structure. 2006, 14: 695-701.
Lee JT, Wheeler TC, Li L, Chin LS: Ubiquitination of alpha-synuclein by Siah-1 promotes alpha-synuclein aggregation and apoptotic cell death. Hum Mol Genet. 2008, 17: 906-917.
Giasson BI, Duda JE, Murray IV, Chen Q, Souza JM, Hurtig HI, Ischiropoulos H, Trojanowski JQ, Lee VM: Oxidative damage linked to neurodegeneration by selective alpha-synuclein nitration in synucleinopathy lesions. Science. 2000, 290: 985-989.
Liu Y, Qiang M, Wei Y, He R: A novel molecular mechanism for nitrated α-synuclein-induced cell death. J Mol Cell Biol. 2011, 3: 239-249.
Danielson SR, Held JM, Schilling B, Oo M, Gibson BW, Andersen JK: Preferentially increased nitration of alpha-synuclein at tyrosine-39 in a cellular oxidative model of Parkinson's disease. Anal Chem. 2009, 81: 7823-7828.
Kordower JH, Chu Y, Hauser RA, Freeman TB, Olanow CW: Lewy body-like pathology in long-term embryonic nigral transplants in Parkinson's disease. Nat Med. 2008, 14: 504-506.
Li JY, Englund E, Holton JL, Soulet D, Hagell P, Lees AJ, Lashley T, Quinn NP, Rehncrona S, Bjorklund A, Widner H, Revesz T, Lindvall O, Brundin P: Lewy bodies in grafted neurons in subjects with Parkinson's disease suggest host-to-graft disease propagation. Nat Med. 2008, 14: 501-503.
Brundin P, Melki R, Kopito R: Prion-like transmission of protein aggregates in neurodegenerative diseases. Nat Rev Mol Cell Biol. 2010, 11: 301-307.
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E: Staging of brain pathology related to sporadic Parkinson's disease. Neurobiol Aging. 2003, 24: 197-211.
Braak H, Rub U, Gai WP, Del Tredici K: Idiopathic Parkinson's disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J Neural Transm. 2003, 110: 517-536.
Hansen C, Angot E, Bergstrom AL, Steiner JA, Pieri L, Paul G, Outeiro TF, Melki R, Kallunki P, Fog K, Li JY, Brundin P: alpha-Synuclein propagates from mouse brain to grafted dopaminergic neurons and seeds aggregation in cultured human cells. J Clin Invest. 2011, 121: 715-725.
Ulusoy A, Rusconi R, Perez-Revuelta BI, Musgrove RE, Helwig M, Winzen-Reichert B, Di Monte DA: Caudo-rostral brain spreading of alpha-synuclein through vagal connections. EMBO Mol Med. 2013, 5: 1051-1059.
Rey NL, Petit GH, Bousset L, Melki R, Brundin P: Transfer of human alpha-synuclein from the olfactory bulb to interconnected brain regions in mice. Acta Neuropathol. 2013, 126: 555-573.
Luk KC, Lee VM: Modeling Lewy pathology propagation in Parkinson's disease. Parkinsonism Relat Disord. 2014, 20: S85-S87.
Recasens A, Dehay B, Bove J, Carballo-Carbajal I, Dovero S, Perez-Villalba A, Fernagut PO, Blesa J, Parent A, Perier C, Farinas I, Obeso JA, Bezard E, Vila M: Lewy body extracts from Parkinson disease brains trigger alpha-synuclein pathology and neurodegeneration in mice and monkeys. Ann Neurol. 2014, 75: 351-362.
Masuda-Suzukake M, Nonaka T, Hosokawa M, Oikawa T, Arai T, Akiyama H, Mann DM, Hasegawa M: Prion-like spreading of pathological alpha-synuclein in brain. Brain. 2013, 136: 1128-1138.
Kretzschmar H, Tatzelt J: Prion disease: a tale of folds and strains. Brain Pathol. 2013, 23: 321-332.
Bousset L, Pieri L, Ruiz-Arlandis G, Gath J, Jensen PH, Habenstein B, Madiona K, Olieric V, Bockmann A, Meier BH, Melki R: Structural and functional characterization of two alpha-synuclein strains. Nat Commun. 2013, 4: 2575-
Guo JL, Covell DJ, Daniels JP, Iba M, Stieber A, Zhang B, Riddle DM, Kwong LK, Xu Y, Trojanowski JQ, Lee VM: Distinct alpha-synuclein strains differentially promote tau inclusions in neurons. Cell. 2013, 154: 103-117.
Narkiewicz J, Giachin G, Legname G: In vitro aggregation assays for the characterization of alpha-synuclein prion-like properties. Prion. 2014, 8: 19-32.
Halliday GM, Holton JL, Revesz T, Dickson DW: Neuropathology underlying clinical variability in patients with synucleinopathies. Acta Neuropathol. 2011, 122: 187-204.
Spillantini MG, Crowther RA, Jakes R, Hasegawa M, Goedert M: alpha-Synuclein in filamentous inclusions of Lewy bodies from Parkinson's disease and dementia with lewy bodies. Proc Natl Acad Sci U S A. 1998, 95: 6469-6473.
Leng Y, Chase TN, Bennett MC: Muscarinic receptor stimulation induces translocation of an alpha-synuclein oligomer from plasma membrane to a light vesicle fraction in cytoplasm. J Biol Chem. 2001, 276: 28212-28218.
Davidson WS, Jonas A, Clayton DF, George JM: Stabilization of alpha-synuclein secondary structure upon binding to synthetic membranes. J Biol Chem. 1998, 273: 9443-9449.
Segrest JP, Jones MK, De Loof H, Brouillette CG, Venkatachalapathi YV, Anantharamaiah GM: The amphipathic helix in the exchangeable apolipoproteins: a review of secondary structure and function. J Lipid Res. 1992, 33: 141-166.
Cole NB, Murphy DD, Grider T, Rueter S, Brasaemle D, Nussbaum RL: Lipid droplet binding and oligomerization properties of the Parkinson's disease protein alpha-synuclein. J Biol Chem. 2002, 277: 6344-6352.
Fortin DL, Troyer MD, Nakamura K, Kubo S, Anthony MD, Edwards RH: Lipid rafts mediate the synaptic localization of alpha-synuclein. J Neurosci. 2004, 24: 6715-6723.
Bartels T, Choi JG, Selkoe DJ: alpha-Synuclein occurs physiologically as a helically folded tetramer that resists aggregation. Nature. 2011, 477: 107-110.
McKeith IG, Dickson DW, Lowe J, Emre M, O'Brien JT, Feldman H, Cummings J, Duda JE, Lippa C, Perry EK, Aarsland D, Arai H, Ballard CG, Boeve B, Burn DJ, Costa D, Del Ser T, Dubois B, Galasko D, Gauthier S, Goetz CG, Gomez-Tortosa E, Halliday G, Hansen LA, Hardy J, Iwatsubo T, Kalaria RN, Kaufer D, Kenny RA, Korczyn A: Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology. 2005, 65: 1863-1872.
Weisman D, Cho M, Taylor C, Adame A, Thal LJ, Hansen LA: In dementia with Lewy bodies, Braak stage determines phenotype, not Lewy body distribution. Neurology. 2007, 69: 356-359.
Fujishiro H, Ferman TJ, Boeve BF, Smith GE, Graff-Radford NR, Uitti RJ, Wszolek ZK, Knopman DS, Petersen RC, Parisi JE, Dickson DW: Validation of the neuropathologic criteria of the third consortium for dementia with Lewy bodies for prospectively diagnosed cases. J Neuropathol Exp Neurol. 2008, 67: 649-656.
Oinas M, Polvikoski T, Sulkava R, Myllykangas L, Juva K, Notkola IL, Rastas S, Niinisto L, Kalimo H, Paetau A: Neuropathologic findings of dementia with lewy bodies (DLB) in a population-based Vantaa 85+ study. J Alzheimers Dis. 2009, 18: 677-689.
Walker Z, Jaros E, Walker RW, Lee L, Costa DC, Livingston G, Ince PG, Perry R, McKeith I, Katona CL: Dementia with Lewy bodies: a comparison of clinical diagnosis, FP-CIT single photon emission computed tomography imaging and autopsy. J Neurol Neurosurg Psychiatry. 2007, 78: 1176-1181.
Nelson PT, Jicha GA, Kryscio RJ, Abner EL, Schmitt FA, Cooper G, Xu LO, Smith CD, Markesbery WR: Low sensitivity in clinical diagnoses of dementia with Lewy bodies. J Neurol. 2010, 257: 359-366.
Ferman TJ, Boeve BF, Smith GE, Lin SC, Silber MH, Pedraza O, Wszolek Z, Graff-Radford NR, Uitti R, Van Gerpen J, Pao W, Knopman D, Pankratz VS, Kantarci K, Boot B, Parisi JE, Dugger BN, Fujishiro H, Petersen RC, Dickson DW: Inclusion of RBD improves the diagnostic classification of dementia with Lewy bodies. Neurology. 2011, 77: 875-882.
Dickson DW, Braak H, Duda JE, Duyckaerts C, Gasser T, Halliday GM, Hardy J, Leverenz JB, Del Tredici K, Wszolek ZK, Litvan I: Neuropathological assessment of Parkinson's disease: refining the diagnostic criteria. Lancet Neurol. 2009, 8: 1150-1157.
Kovacs GG, Alafuzoff I, Al-Sarraj S, Arzberger T, Bogdanovic N, Capellari S, Ferrer I, Gelpi E, Kovari V, Kretzschmar H, Nagy Z, Parchi P, Seilhean D, Soininen H, Troakes C, Budka H: Mixed brain pathologies in dementia: the BrainNet Europe consortium experience. Dement Geriatr Cogn Disord. 2008, 26: 343-350.
Ballard C, Ziabreva I, Perry R, Larsen JP, O'Brien J, McKeith I, Perry E, Aarsland D: Differences in neuropathologic characteristics across the Lewy body dementia spectrum. Neurology. 2006, 67: 1931-1934.
Tiraboschi P, Hansen LA, Alford M, Sabbagh MN, Schoos B, Masliah E, Thal LJ, Corey-Bloom J: Cholinergic dysfunction in diseases with Lewy bodies. Neurology. 2000, 54: 407-411.
Shimada H, Hirano S, Shinotoh H, Aotsuka A, Sato K, Tanaka N, Ota T, Asahina M, Fukushi K, Kuwabara S, Hattori T, Suhara T, Irie T: Mapping of brain acetylcholinesterase alterations in Lewy body disease by PET. Neurology. 2009, 73: 273-278.
Marcone A, Garibotto V, Moresco RM, Florea I, Panzacchi A, Carpinelli A, Virta JR, Tettamanti M, Borroni B, Padovani A, Bertoldo A, Herholz K, Rinne JO, Cappa SF, Perani D: [11C]-MP4A PET cholinergic measurements in amnestic mild cognitive impairment, probable Alzheimer's disease, and dementia with Lewy bodies: a Bayesian method and voxel-based analysis. J Alzheimers Dis. 2012, 31: 387-399.
Laske C, Fallgatter AJ, Stransky E, Hagen K, Berg D, Maetzler W: Decreased alpha-synuclein serum levels in patients with Lewy body dementia compared to Alzheimer's disease patients and control subjects. Dement Geriatr Cogn Disord. 2011, 31: 413-416.
Gelb DJ, Oliver E, Gilman S: Diagnostic criteria for Parkinson disease. Arch Neurol. 1999, 56: 33-39.
Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, Broe GA, Cummings J, Dickson DW, Gauthier S, Goldman J, Goetz C, Korczyn A, Lees A, Levy R, Litvan I, McKeith I, Olanow W, Poewe W, Quinn N, Sampaio C, Tolosa E, Dubois B: Clinical diagnostic criteria for dementia associated with Parkinson's disease. Mov Disord. 2007, 22: 1689-1707.
Irwin DJ, Lee VM, Trojanowski JQ: Parkinson's disease dementia: convergence of alpha-synuclein, tau and amyloid-beta pathologies. Nat Rev Neurosci. 2013, 14: 626-636.
Zhou J, Broe M, Huang Y, Anderson JP, Gai WP, Milward EA, Porritt M, Howells D, Hughes AJ, Wang X, Halliday GM: Changes in the solubility and phosphorylation of alpha-synuclein over the course of Parkinson's disease. Acta Neuropathol. 2011, 121: 695-704.
Lue LF, Walker DG, Adler CH, Shill H, Tran H, Akiyama H, Sue LI, Caviness J, Sabbagh MN, Beach TG: Biochemical increase in phosphorylated alpha-synuclein precedes histopathology of Lewy-type synucleinopathies. Brain Pathol. 2012, 22: 745-756.
Walker DG, Lue LF, Adler CH, Shill HA, Caviness JN, Sabbagh MN, Akiyama H, Serrano GE, Sue LI, Beach TG: Changes in properties of serine 129 phosphorylated alpha-synuclein with progression of Lewy-type histopathology in human brains. Exp Neurol. 2013, 240: 190-204.
Tong J, Wong H, Guttman M, Ang LC, Forno LS, Shimadzu M, Rajput AH, Muenter MD, Kish SJ, Hornykiewicz O, Furukawa Y: Brain alpha-synuclein accumulation in multiple system atrophy, Parkinson's disease and progressive supranuclear palsy: a comparative investigation. Brain. 2010, 133: 172-188.
Halliday G, Hely M, Reid W, Morris J: The progression of pathology in longitudinally followed patients with Parkinson's disease. Acta Neuropathol. 2008, 115: 409-415.
Wenning G, Tison F, Ben Shlomo Y, Daniel S, Quinn N: Multiple system atrophy: a review of 203 pathologically proven cases. Mov Disord. 1997, 12: 133-147.
Ozawa T, Okuizumi K, Ikeuchi T, Wakabayashi K, Takahashi H, Tsuji S: Analysis of the expression level of alpha-synuclein mRNA using postmortem brain samples from pathologically confirmed cases of multiple system atrophy. Acta Neuropathol. 2001, 102: 188-190.
Baker KG, Huang Y, McCann H, Gai WP, Jensen PH, Halliday GM: P25alpha immunoreactive but alpha-synuclein immunonegative neuronal inclusions in multiple system atrophy. Acta Neuropathol. 2006, 111: 193-195.
Huang Y, Song YJ, Murphy K, Holton JL, Lashley T, Revesz T, Gai WP, Halliday GM: LRRK2 and parkin immunoreactivity in multiple system atrophy inclusions. Acta Neuropathol. 2008, 116: 639-646.
Song YJ, Lundvig DM, Huang Y, Gai WP, Blumbergs PC, Hojrup P, Otzen D, Halliday GM, Jensen PH: p25alpha relocalizes in oligodendroglia from myelin to cytoplasmic inclusions in multiple system atrophy. Am J Pathol. 2007, 171: 1291-1303.
Jin H, Ishikawa K, Tsunemi T, Ishiguro T, Amino T, Mizusawa H: Analyses of copy number and mRNA expression level of the alpha-synuclein gene in multiple system atrophy. J Med Dental Sci. 2008, 55: 145-153.
Morris HR, Vaughan JR, Datta SR, Bandopadhyay R, Rohan De Silva HA, Schrag A, Cairns NJ, Burn D, Nath U, Lantos PL, Daniel S, Lees AJ, Quinn NP, Wood NW: Multiple system atrophy/progressive supranuclear palsy: alpha-synuclein, synphilin, tau, and APOE. Neurology. 2000, 55: 1918-1920.
Ozawa T, Takano H, Onodera O, Kobayashi H, Ikeuchi T, Koide R, Okuizumi K, Shimohata T, Wakabayashi K, Takahashi H, Tsuji S: No mutation in the entire coding region of the alpha-synuclein gene in pathologically confirmed cases of multiple system atrophy. Neurosci Lett. 1999, 270: 110-112.
Al-Chalabi A, Durr A, Wood NW, Parkinson MH, Camuzat A, Hulot JS, Morrison KE, Renton A, Sussmuth SD, Landwehrmeyer BG, Ludolph A, Agid Y, Brice A, Leigh PN, Bensimon G: Genetic variants of the alpha-synuclein gene SNCA are associated with multiple system atrophy. PLoS One. 2009, 4: e7114-
Scholz SW, Houlden H, Schulte C, Sharma M, Li A, Berg D, Melchers A, Paudel R, Gibbs JR, Simon-Sanchez J, Paisan-Ruiz C, Bras J, Ding J, Chen H, Traynor BJ, Arepalli S, Zonozi RR, Revesz T, Holton J, Wood N, Lees A, Oertel W, Wullner U, Goldwurm S, Pellecchia MT, Illig T, Riess O, Fernandez HH, Rodriguez RL, Okun M: SNCA variants are associated with increased risk for multiple system atrophy. Ann Neurol. 2009, 65: 610-614.
Stemberger S, Scholz SW, Singleton AB, Wenning GK: Genetic players in multiple system atrophy: unfolding the nature of the beast. Neurobiol Aging. 1924, 2011: e5-e14.
Sailer A: First genome-wide association study in multiple system atrophy. Mov Disord. 2012, 27: 1425-
Stefanova N, Reindl M, Neumann M, Haass C, Poewe W, Kahle PJ, Wenning GK: Oxidative stress in transgenic mice with oligodendroglial alpha-synuclein overexpression replicates the characteristic neuropathology of multiple system atrophy. Am J Pathol. 2005, 166: 869-876.
Miller DW, Johnson JM, Solano SM, Hollingsworth ZR, Standaert DG, Young AB: Absence of alpha-synuclein mRNA expression in normal and multiple system atrophy oligodendroglia. J Neural Transm. 2005, 112: 1613-1624.
Mori F, Tanji K, Yoshimoto M, Takahashi H, Wakabayashi K: Demonstration of alpha-synuclein immunoreactivity in neuronal and glial cytoplasm in normal human brain tissue using proteinase K and formic acid pretreatment. Exp Neurol. 2002, 176: 98-104.
Richter-Landsberg C, Gorath M, Trojanowski JQ, Lee VM: alpha-synuclein is developmentally expressed in cultured rat brain oligodendrocytes. J Neurosci Res. 2000, 62: 9-14.
Kahle PJ, Neumann M, Ozmen L, Muller V, Jacobsen H, Spooren W, Fuss B, Mallon B, Macklin WB, Fujiwara H, Hasegawa M, Iwatsubo T, Kretzschmar HA, Haass C: Hyperphosphorylation and insolubility of alpha-synuclein in transgenic mouse oligodendrocytes. EMBO Rep. 2002, 3: 583-588.
Yazawa I, Giasson BI, Sasaki R, Zhang B, Joyce S, Uryu K, Trojanowski JQ, Lee VM: Mouse model of multiple system atrophy alpha-synuclein expression in oligodendrocytes causes glial and neuronal degeneration. Neuron. 2005, 45: 847-859.
Lee HJ, Suk JE, Bae EJ, Lee SJ: Clearance and deposition of extracellular alpha-synuclein aggregates in microglia. Biochem Biophys Res Commun. 2008, 372: 423-428.
Lee HJ, Suk JE, Patrick C, Bae EJ, Cho JH, Rho S, Hwang D, Masliah E, Lee SJ: Direct transfer of alpha-synuclein from neuron to astroglia causes inflammatory responses in synucleinopathies. J Biol Chem. 2010, 285: 9262-9272.
Toledo JB, Cairns NJ, Da X, Chen K, Carter D, Fleisher A, Householder E, Ayutyanont N, Roontiva A, Bauer RJ, Eisen P, Shaw LM, Davatzikos C, Weiner MW, Reiman EM, Morris JC, Trojanowski JQ: Clinical and multimodal biomarker correlates of ADNI neuropathological findings. Acta Neuropathol Commun. 2013, 1: 65-
Mikolaenko I, Pletnikova O, Kawas CH, O'Brien R, Resnick SM, Crain B, Troncoso JC: Alpha-synuclein lesions in normal aging, Parkinson disease, and Alzheimer disease: evidence from the Baltimore Longitudinal Study of Aging (BLSA). J Neuropathol Exp Neurol. 2005, 64: 156-162.
Hamilton RL: Lewy bodies in Alzheimer's disease: a neuropathological review of 145 cases using alpha-synuclein immunohistochemistry. Brain Pathol. 2000, 10: 378-384.
Iseki E: Dementia with Lewy bodies: reclassification of pathological subtypes and boundary with Parkinson's disease or Alzheimer's disease. Neuropathology. 2004, 24: 72-78.
Marui W, Iseki E, Ueda K, Kosaka K: Occurrence of human alpha-synuclein immunoreactive neurons with neurofibrillary tangle formation in the limbic areas of patients with Alzheimer's disease. J Neurol Sci. 2000, 174: 81-84.
Compta Y, Parkkinen L, O'Sullivan SS, Vandrovcova J, Holton JL, Collins C, Lashley T, Kallis C, Williams DR, de Silva R, Lees AJ, Revesz T: Lewy- and Alzheimer-type pathologies in Parkinson's disease dementia: which is more important?. Brain. 2011, 134: 1493-1505.
Kovari E, Gold G, Herrmann FR, Canuto A, Hof PR, Bouras C, Giannakopoulos P: Lewy body densities in the entorhinal and anterior cingulate cortex predict cognitive deficits in Parkinson's disease. Acta Neuropathol. 2003, 106: 83-88.
Jellinger KA, Seppi K, Wenning GK, Poewe W: Impact of coexistent Alzheimer pathology on the natural history of Parkinson's disease. J Neural Transm. 2002, 109: 329-339.
Irwin DJ, White MT, Toledo JB, Xie SX, Robinson JL, Van Deerlin V, Lee VM, Leverenz JB, Montine TJ, Duda JE, Hurtig HI, Trojanowski JQ: Neuropathologic substrates of Parkinson disease dementia. Ann Neurol. 2012, 72: 587-598.
Clinton LK, Blurton-Jones M, Myczek K, Trojanowski JQ, LaFerla FM: Synergistic interactions between Abeta, tau, and alpha-synuclein: acceleration of neuropathology and cognitive decline. J Neurosci. 2010, 30: 7281-7289.
Giasson BI, Duda JE, Quinn SM, Zhang B, Trojanowski JQ, Lee VM: Neuronal alpha-synucleinopathy with severe movement disorder in mice expressing A53T human alpha-synuclein. Neuron. 2002, 34: 521-533.
Rolinski M, Fox C, Maidment I, McShane R: Cholinesterase inhibitors for dementia with Lewy bodies. Parkinson's disease dementia and cognitive impairment in Parkinson's disease. Cochrane Database Syst Rev. 2012, 3: CD006504-
Ballard CG, Chalmers KA, Todd C, McKeith IG, O'Brien JT, Wilcock G, Love S, Perry EK: Cholinesterase inhibitors reduce cortical Abeta in dementia with Lewy bodies. Neurology. 2007, 68: 1726-1729.
Vekrellis K, Stefanis L: Targeting intracellular and extracellular alpha-synuclein as a therapeutic strategy in Parkinson's disease and other synucleinopathies. Expert Opin Ther Targets. 2012, 16: 421-432.
Lee HJ, Bae EJ, Lee SJ: Extracellular alpha-synuclein - a novel and crucial factor in Lewy body diseases. Nat Rev Neurol. 2014, 10: 92-98.
Marchiani A, Mammi S, Siligardi G, Hussain R, Tessari I, Bubacco L, Delogu G, Fabbri D, Dettori MA, Sanna D, Dedola S, Serra PA, Ruzza P: Small molecules interacting with alpha-synuclein: antiaggregating and cytoprotective properties. Amino Acids. 2013, 45: 327-338.
Moloney TC, Hyland R, O'Toole D, Paucard A, Kirik D, O'Doherty A, Gorman AM, Dowd E: Heat shock protein 70 reduces alpha-synuclein-induced predegenerative neuronal dystrophy in the alpha-synuclein viral gene transfer rat model of Parkinson's disease. CNS Neurosci Ther. 2014, 20: 50-58.
Putcha P, Danzer KM, Kranich LR, Scott A, Silinski M, Mabbett S, Hicks CD, Veal JM, Steed PM, Hyman BT, McLean PJ: Brain-permeable small-molecule inhibitors of Hsp90 prevent alpha-synuclein oligomer formation and rescue alpha-synuclein-induced toxicity. J Pharmacol Exp Ther. 2010, 332: 849-857.
Toth G, Gardai SJ, Zago W, Bertoncini CW, Cremades N, Roy SL, Tambe MA, Rochet JC, Galvagnion C, Skibinski G, Finkbeiner S, Bova M, Regnstrom K, Chiou SS, Johnston J, Callaway K, Anderson JP, Jobling MF, Buell AK, Yednock TA, Knowles TP, Vendruscolo M, Christodoulou J, Dobson CM, Schenk D, McConlogue L: Targeting the intrinsically disordered structural ensemble of alpha-synuclein by small molecules as a potential therapeutic strategy for Parkinson's disease. PLoS One. 2014, 9: e87133-
Jones DR, Moussaud S, McLean P: Targeting heat shock proteins to modulate alpha-synuclein toxicity. Ther Adv Neurol Disord. 2014, 7: 33-51.
Sinha G: Roche bets on alpha-synuclein for Parkinson's. Nat Biotechnol. 2014, 32: 212-
Valera E, Masliah E: Immunotherapy for neurodegenerative diseases: focus on alpha-synucleinopathies. Pharmacol Ther. 2013, 138: 311-322.
Mandler M, Valera E, Rockenstein E, Weninger H, Patrick C, Adame A, Santic R, Meindl S, Vigl B, Smrzka O, Schneeberger A, Mattner F, Masliah E: Next-generation active immunization approach for synucleinopathies: implications for Parkinson's disease clinical trials. Acta Neuropathol. 2014, 127: 861-879.
Lindstrom V, Ihse E, Fagerqvist T, Bergstrom J, Nordstrom E, Moller C, Lannfelt L, Ingelsson M: Immunotherapy targeting alpha-synuclein, with relevance for future treatment of Parkinson's disease and other Lewy body disorders. Immunotherapy. 2014, 6: 141-153.
Ruzza P, Siligardi G, Hussain R, Marchiani A, Islami M, Bubacco L, Delogu G, Fabbri D, Dettori MA, Sechi M, Pala N, Spissu Y, Migheli R, Serra PA, Sechi G: Ceftriaxone blocks the polymerization of alpha-synuclein and exerts neuroprotective effects in vitro. ACS Chem Neurosci. 2014, 5: 30-38.
Low PA, Robertson D, Gilman S, Kaufmann H, Singer W, Biaggioni I, Freeman R, Perlman S, Hauser RA, Cheshire W, Lessig S, Vernino S, Mandrekar J, Dupont WD, Chelimsky T, Galpern WR: Efficacy and safety of rifampicin for multiple system atrophy: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2014, 13: 268-275.
Acknowledgements
This work was supported by a National Health and Medical Research Council of Australia (NHMRC) project grant (#1022325). GMH is a NHMRC Senior Principal Research Fellow (#630434).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kim, W.S., Kågedal, K. & Halliday, G.M. Alpha-synuclein biology in Lewy body diseases. Alz Res Therapy 6, 73 (2014). https://doi.org/10.1186/s13195-014-0073-2
Published:
DOI: https://doi.org/10.1186/s13195-014-0073-2