Abstract
The development of innovative wound dressing materials is crucial for effective wound care. It’s an active area of research driven by a better understanding of chronic wound pathogenesis. Addressing wound care properly is a clinical challenge, but there is a growing demand for advancements in this field. The synergy of medicinal plants and nanotechnology offers a promising approach to expedite the healing process for both acute and chronic wounds by facilitating the appropriate progression through various healing phases. Metal nanoparticles play an increasingly pivotal role in promoting efficient wound healing and preventing secondary bacterial infections. Their small size and high surface area facilitate enhanced biological interaction and penetration at the wound site. Specifically designed for topical drug delivery, these nanoparticles enable the sustained release of therapeutic molecules, such as growth factors and antibiotics. This targeted approach ensures optimal cell-to-cell interactions, proliferation, and vascularization, fostering effective and controlled wound healing. Nanoscale scaffolds have significant attention due to their attractive properties, including delivery capacity, high porosity and high surface area. They mimic the Extracellular matrix (ECM) and hence biocompatible. In response to the alarming rise of antibiotic-resistant, biohybrid nanofibrous wound dressings are gradually replacing conventional antibiotic delivery systems. This emerging class of wound dressings comprises biopolymeric nanofibers with inherent antibacterial properties, nature-derived compounds, and biofunctional agents. Nanotechnology, diminutive nanomaterials, nanoscaffolds, nanofibers, and biomaterials are harnessed for targeted drug delivery aimed at wound healing. This review article discusses the effects of nanofibrous scaffolds loaded with nanoparticles on wound healing, including biological (in vivo and in vitro) and mechanical outcomes.
Graphical Abstract

Similar content being viewed by others
Introduction
The skin is the body’s largest organ and acts as a protective barrier against various types of damages. It has two layers: the epidermis and the dermis. The epidermis consists of sensory axons, immune cells, and keratinocytes. The dermis is made up of skin appendages, fibroblasts, and mast cells. The goal of tissue engineering is to create a scaffold with biocompatibility, controlled biodegradability, and the right mechanical properties to repair damaged skin [1, 2]. During injury, it impacts the surface of our skin and the tissue beneath, forming a wound. Healing is a natural process that involves intricate mechanisms to restore the skin's normal structure and functions [3,4,5]. The skin has a variety of functions and acts as a protective barrier, shielding our bodies from harmful external factors like bacteria, UV radiation, and chemicals. The skin also helps regulate body temperature by sweating and dilating or constricting blood vessels. It allows us to sense touch, pressure, heat, and cold through specialized nerve endings. The skin plays a role in immune defense by housing immune cells that can detect and fight off pathogens. It also helps in the synthesis of vitamin D when exposed to sunlight [6]. The skin has developed a set of mechanisms called the wound-healing response to heal breaches quickly and effectively in its barrier [7]. According to recent research, the global market for wound care will increase from 19.8 billion USD in 2021 to up to 27.8 billion USD in 2026 at a CAGR of 7.6% [8]. Since the skin is increasingly susceptible to burns and injuries from operations or traumas. Several things can trigger wounds, including external injuries, genetic conditions, minored abrasions, burns, and surgical procedures [9]. Impaired healing can impact the recovery of various types of wounds, including both acute wounds (surgical incisions or traumatic injuries) and chronic wounds (diabetic foot ulcers). Acute wounds are minor cuts that usually heal within a few days [10]. As cells migrate, inflammation occurs, nerves grow, and new blood vessels form. Major surgeries can take a while to heal and may leave noticeable scars. Chronic wounds, which are persistent barrier defects that haven't healed in 3 months, can be challenging to treat [11]. To effectively manage wounds in modern therapy, it is crucial to ensure thorough cleaning, removal of foreign objects, relieving pressure, using a suitable dressing, and administering antibiotics if required [12].
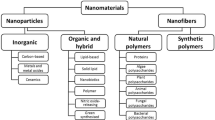
Traditional medicine has provided valuable insights into wound healing. Integrating nanotechnology into this field seems like a promising approach as shown in Fig.1. By incorporating bioactive compounds into nanomaterials, researchers can create innovative wound dressings and delivery systems that optimize tissue regeneration and minimize infection risks. The combination of ancient wisdom and modern science can lead to more effective and targeted interventions in wound healing. This interdisciplinary approach has the potential to greatly advance treatment outcomes. Since ancient times, the use of medicinal plant extracts has been a part of cultural heritage, especially in traditional medicine. These plant-based remedies, such as infusions, ointments, and compresses, have shown promising wound healing properties. This valuable knowledge has been passed down through generations and can be explored further in historical texts for pharmaceutical research [13]. Various therapies are used for wound management, surgical removal of necrotic tissue, and medication, but the results are still unsatisfactory. There is a need for new, affordable, and effective therapies in wound care. Researchers are now focusing on herbs used in folk medicines worldwide as potential therapeutic agents in wound healing [14]. Traditional medicine often touts the effectiveness of various medicinal plants for wound healing, but their scientific mechanisms and efficacy require further exploration. Wound healing is a well-coordinated process involving biochemical and cellular events, where damaged tissue attempts to repair itself. This intricate process involves the interaction of blood cells, mediators, and growth factors, ultimately regenerating healthy tissues and skin [15]. Plants contain phytochemicals that have antioxidant properties and can aid in wound healing. When reactive oxygen species (ROS) levels are high, they can hinder the wound-healing process by damaging cellular membranes. Additionally, excessive ROS can cause significant tissue injuries and potentially even lead to neoplastic transformation [16].
Nanotechnology revolves around nanoparticles, with a three-dimensional structure and a size ranging from 1 to 100 nm. Nanoparticles can be synthesized in various sizes and shapes including rod, spherical and crystal forms. There are different methods used to create nanoparticles. (i) Chemical methods can harm the environment and living organisms. Scientists are actively exploring and discovering highly efficient and cost-effective methods that are safe and eco-friendly for producing nanoparticles. (ii) The biological method is gaining popularity in nanoparticle production due to its minimal toxicity and environmental impact [17]. Water is used as a solvent to synthesize the nanoparticles from plant extracts. This method is safe and helps eliminate the potential risks. Water is a versatile and widely available solvent for many applications [18]. The green synthesis approach for nanoparticles is eco-friendly, cost-effective, and time-efficient. In addition, nanoparticles could be coated with bioorganic composites that make them proper for the biological environment. Using systemic antibiotics for wound therapy can lead to unwanted side effects and antimicrobial resistance. However, using topical antimicrobial agents allows the use of a higher concentration of medication directly in the affected area, reducing the negative effects of systemic drug administration and preventing the occurrence of antimicrobial resistance [19]. Therefore, wound dressing applications utilize many biopolymers and bioactive compounds obtained from natural resources [20] (Fig. 1).
Schematic representation [21]
Among the methods devised for the fabrication of nanofibers, electrospinning is one of the most popular techniques due to its cost-effectiveness and efficiency in producing ultrafine nanofibrous structures from diverse polymers. To increase the wound healing process, designing nanofibrous mat/wound dressing materials with antibiotic and antibacterial properties is essential [22]. Nanofibrous scaffolds have several advantages over conventional dressings (Fig. 2). They have a large surface area-to-volume ratio, tiny pore size, and high porosity. These properties allow for better exudate absorption improved wound permeation, and can help prevent further infection [23]. Electrospun nanofibers have the potential to revolutionize wound healing approaches. These nanofibers, made from both synthetic and natural polymers, can be incorporated with bioactive compounds to enhance wound healing outcomes. By exploring the synthesis techniques, material selection, and the synergistic effects of bioactive compounds, researchers can gain a comprehensive understanding of how to elevate wound healing.
Process of wound healing
There are four stages in the healing process: Hemostasis, inflammation, proliferation, and regeneration (Fig. 3) [24]. The process involves multiple growth factors, cytokines, and chemokines, forming a complex signalling mechanism. Cell proliferation plays a crucial role in tissue repair and regeneration during the healing process of wounds [25, 26].
Hemostasis phase
In the hemostasis phase after skin damage, collagen triggers intrinsic and external clotting cascades, stopping the initial bleeding. Thrombocythemia aggregates and causes vasoconstriction, leading to hypokalemia, increased glycolysis, and changes in pH to minimize the blood loss. A blood clot forms to fill the wound bed, which serves as a temporary wound matrix and provides a scaffold for the migration of various cell types (Fig. 3A). After 5 to 10 min of vasoconstriction, the blood vessels expand, and leukocytes and thrombocytes enter the posterior matrix [27, 28]. Additionally, several cytokines and growth factors are secreted within the wound during this stage to promote cell synergy and communication, allowing it to heal [29, 30].
Inflammatory phase
The inflammatory phase destroys bacteria that have entered the wound during injury and provides the immune system with a barrier against bacterial contamination. The inflammatory response is divided into two phases: (i) The first stage of this process begins when a hemostatic response occurs, and white blood cells are observed at the injury site after being stimulated by hemostatic substances. (ii) In the second stage, a group of immune cells work together to kill bacteria through processes like phagocytosis, the production of reactive oxygen species, and proteinases for the removal of dead tissue. Neutrophils are key players in tissue removal. They stimulate and gather cells involved in the process (Fig. 3B). In parallel, their actions make it harder for extraterrestrials to survive. Many neutrophils transmigrate through endothelial cells in the blood capillary walls, which are activated by pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-α), interferon-gamma (IFN-γ), and IL-1, just a few hours after the lesion forms (Fig. 4). Neutrophils are either phagocytosed by macrophages, going through apoptosis, or emerging from the injury surface. Several growth factors, including platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), fibroblast growth factor (FGF), and vascular endothelial growth factor (VEGF), reach their highest concentrations in the wound two to three days after injury in macrophages, which are large phagocytic cells (Fig. 5). These development factors are vital in controlling aggravation, animating angiogenesis, and arrangement of grind tissue [31].
Proliferative phase
During this phase, neovascularization, and re-epithelialization take place. That process may take a few weeks to complete. Angiogenesis, in which new blood vessels are made from existing arteries, and vasculogenesis, in which endothelial progenitor cells (EPCs) make new arteries, play a role in neovascularization. Neovascularization re-establishes the tissue's access to nutrients. The process of gradually reducing the size of a wound and removing keratinocytes from its periphery is known as epithelialization. Initially, a shallow, thin layer of epithelial cells forms. A layer of stronger and thicker cells will eventually cover the wound over time. Anti-inflammatory mediators that promote collagen deposition, fibroblast proliferation, and angiogenesis are secreted by macrophages when they acquire the M2 phenotype [32, 33].
The wound expands once the collagen fibers replace the temporary fibrin mixture. Revascularization of the wound proceeds in the same direction as fibroplasia. Angiogenesis is the result of proliferation and migration working together (Fig. 3C). Capillary buds emerge from nearby blood vessels and spread into the wound space, aiding in the healing process. The process of angiogenesis encourages endothelial cells to migrate from the side of vessels that are close to the wound. Endothelial cell growth and chemotaxis are mediated by cytokines produced by platelets, macrophages, and lymphocytes in the wound, low oxygen tension, lactic acid, and biogenic amines (Fig. 5) [34]. Two principle reasons animate the fresh blood vessel arrangement, one is the microenvironment, including low oxygen strain, low pH, and high lactate levels; Another is the FGF, TGF- β, and VEGF, which aid in the EC's integrin-mediated connection to the Extracellular matrix (ECM) and facilitate healing (Fig. 4) [35].
Remodelling phase
Redesigning is the last phase of twisted recuperating, during which the primary collagen organization of solid tissue is re-established. By synthesizing matrix metalloproteinases and new extracellular matrix, fibroblasts would control the decomposition of wound matrix, which promotes wound contraction, reduces epithelialization, and prevents scar formation (Fig. 4) [36]. In the healing process, the granulation tissue is gradually replaced by a more organized extracellular matrix, forming scar tissue with mechanical properties comparable to the tissue prior to the injury. Additionally, the blood vessel density in the granulation tissue returns to the level observed in healthy skin. Fibroblasts play a crucial role in the remodelling of collagen in the granulation tissue. They secrete matrix metalloproteinases that break down the collagen, allowing the formation of a more durable structure. The arrangement of the expressed collagens directly influences the process of wound healing (Fig. 3D). When wounds heal completely, the ratio of collagen type I to collagen type III increases, eventually matching that of normal skin. Over time, the collagen fibrils also increase in size, resembling a healthy dermis. Scar tissue, on the other hand, is predominantly composed of parallel bundles of collagen type I, which is weaker and less flexible compared to healthy skin tissue [37].
Medicinal plants
Plants are rich in compounds like triterpenes, flavonoids, and alkaloids that can enhance wound healing. They can help with coagulation, fibroplasia, inflammation, collagenation, wound contraction, and epithelialization [38]. Medicinal plants offer a significant alternative in therapeutics, especially while dealing with multidrug-resistant microbial pathogens. Their phytochemical components, including antioxidants like flavonoids, polyphenols, and vitamins, have remarkable medicinal and therapeutic properties (Table 1). These antioxidants help prevent oxidative stress caused by reactive oxygen species and free radicals [39]. The mucilaginous gel extracted from the plant leaves has been utilized for its wound-healing properties, including antibacterial effects, and promoting collagen synthesis. It works by blocking the production of reactive oxygen species, prostaglandins, and cytokines while stimulating the growth of fibroblasts and keratinocytes. Carbohydrates in the gel activate immune cells like macrophages, which play a role in inflammation by releasing inflammatory mediators and engulf foreign particles or damaged cells. Studies have shown that aloe vera formulations, such as creams, gels, and impregnated dressings, have improved wound healing in both acute and chronic wounds in animal models [40, 41].
Flavonoids are found in different parts of plants, like seeds, bark, roots, and buds. Plants belonging to the family Moraceae, Fabaceae, Guttiferae, Rutaceae, Euphorbiaceae, and Thymelaeaceae consist of flavonoids. The leaves, fruits, and vegetables of Artocarpus heterophyllus, Epimedium brevicornum, propolis, and Humulus lupulus are used as medicines. Prenylated flavonoids have diverse structures, including C-prenylated chalcones, flavanones, flavonols, and isoflavones, with side chains like farnesyl, geranyl, and 3,3-dimethylallyl, 1,1-dimethylallyl [74]. These structures undergo modifications such as oxidation, reduction, dehydration, and cyclization. Prenylated flavonoids offer several benefits compared to regular flavonoids. They have a stronger attraction to the cell membrane at the desired location and exhibit powerful inhibitory properties against P-glycoprotein. These properties contribute to their ability to promote health [75]. There are more than 8000 diverse polyphenols, which can be divided into non-flavonoids and flavonoids. These plant-derived polyphenolic compounds have strong antioxidant activity, combating free radicals by providing a hydrogen atom or an electron. They also possess antimicrobial properties against specific bacteria in infected wounds and act as anti-inflammatory agents, reducing the inflammatory mediators linked to chronic wounds [76]. Kigelia africana, a medicinal plant, has been found to have beneficial effects in alleviating fungal infestations, psoriatic arthritis, dermatitis, and even cancer. Compounds like kigelinone, vernolic acid, kigelin, iridoids, luteolin, and 6-hydroxyluteolin in different plant parts contribute to its healing properties. In a study conducted by the Agyare research team in 2013, the methanolic extract of Kigelia Africana from the leaves and roots showed a 100% healing rate compared to the control, which had a healing rate of 96.59% [77]. Dillenia indica fruit extracts containing betulinic acid were tested in a laboratory to assess their ability to protect against lipid peroxidation [78]. In an animal study using rats with psoriasis-like wounds, the extracts with a 50 mg/mL concentration in betulinic acid promoted faster wound healing, reduced immune cell infiltration and parakeratosis, and exhibited anti-inflammatory effects. Another research study investigated the anti-inflammatory effects of betulinic acid from Diospyros kaki in macrophages stimulated by lipopolysaccharide [79].
A significant amount of alkaloids in A. africana is believed to be a critical factor in its wound-healing properties. [80] Various alkaloids have been known for their effective wound-healing effects, as demonstrated in studies using alkaloid-enriched ointments on rats. Additionally, alkaloids have shown the ability to promote early stages of wound healing by stimulating fibroblast chemotaxis [81]. The wound-healing potential of A. africana is likely attributed to its abundant alkaloid content [82]. The study compared the effectiveness of Nigella sativa oil and Aloe vera gel in diabetic foot wound healing. Aloe treatment showed improved wound area resolution and re-epithelialization compared to the oil and control [83]. Another study assessed an aqueous aloe extract for skin wounds in mice, showing improvements in epithelization and some mutagenic and cytotoxic effects [84]. Additionally, a survey of a porous wound dressing with aloe extract found it promoted cell growth and attenuated scar-forming myofibroblast formation. However, a study on A. vera extract for open wounds in rats found no significant difference compared to the control group [85]. The research discovered that the leaf extract of Plumbago zeylanica L. exhibited the highest antimicrobial activity against Staphylococcus aureus, while the stem extract was more effective against Pseudomonas aeruginosa [86]. Another study investigated the antibacterial properties of ethanolic extract from the root bark of Plumbago zeylanica L. The findings showed that the antibacterial activity increased as the concentration of the extract increased. [87]. In a recent experiment, Plumbago zeylanica L. also had excellent inhibitory activity against Alternaria spp and relatively less activity against Sclerotium rolfsii [88].
Nanoparticle for a therapeutic drug
Nanomaterials are beneficial to speeding up the injury recuperating process because of their profitable proportion of surface region to volume and medication conveyance ability. Collagen deposition and skin tissue regeneration may be affected by this feature. Mainly, the size of the nanoparticles enables them to penetrate the wound, allowing contact with specific target molecules and the local release of bioactive agents or drugs that influence the healing rate. Drugs are protected from wound-bed proteases by being encapsulated in nanocarriers, allowing them to carry out their biological function [89]. Nanoparticle modes refer to different ways in which nanoparticles can be utilized or interact with their surroundings. These modes can include things like surface modification, functionalization, encapsulation, or aggregation (Fig. 6). It is widely recognized that providing therapeutic substances such as growth factors, antioxidants, antibiotics, and nucleic acids to affected tissue can significantly impact the healing of chronic wounds. These substances can stimulate cell growth, enhance cell movement, promote blood vessel formation, encourage collagen production, and combat microbial activity.
The nanoparticles and biomolecules can be added to hydrogels, leading to advanced topical drug delivery. This approach offers unique benefits like preventing sudden release, controlled sequential release, and improved targeting of specific tissues [90]. Over the past few decades, numerous nanomaterials with biological applications have received extensive research. Among these are Liposomes, dendrimers, quantum dots, fullerenes, carbon nanotubes, graphene, titanium oxide, iron, and gold nanoparticles. To encourage angiogenesis, NP-based delivery of ions like calcium and oxygen has been used [91]. NPs have become a crucial tool in various medical and pharmaceutical research areas. Their small size and customizable features make them highly effective for controlled and targeted drug release. In wound dressing development, NPs can be used as delivery vehicles or as bioactive components to enhance wound healing outcomes (Table 2). They are excellent carriers for transporting active compounds to improve wound healing [92].
Zinc nanoparticles
Zinc NPs are chemically stability, has antibacterial and anti-inflammatory properties, and release Zn2+ ions, which encourages keratinocyte migration during wound healing, ZnO NPs (Fig. 7a) used in wound dressings speed up the healing of acute and chronic wounds [117]. The carbohydrate-based polymer with ZnO NPs in chronic venous leg ulcers will enhance wound healing and anti-inflammatory effect [118]. When ZnO nanoparticles and cells come together, they form intercalated structures on the nanoparticle surface. These nanoparticles promote better cell adhesion and attachment, leading to high cell proliferation and growth. The extracellular matrix plays a role in cell attachment to the nanoparticles. Optimized ZnFe2O4 NPs show great potential in fighting drug-resistant bacteria and promoting wound healing. Nanoparticles are also being used in making bandages for burnt wounds. The potential of ZnS-NPs is demonstrated in both in vitro and in vivo studies as a possible therapy for skin regeneration. Before clinical application, further research is needed to validate these findings using advanced cell culture models and clinically relevant animal models. Overall, ZnS-NP shows promise in scarless wound repair [119]. Zinc ions released from ZnO have multiple beneficial effects on wound healing. They enhance keratinocyte migration toward the wound, promote healing, and exhibit antibacterial activity by interacting with bacterial cell membranes. Additionally, the topical application of ZnO-NPs stimulates angiogenesis re-epithelization and reduces inflammation and bacterial growth. These properties have been observed in equine wounds, leading to accelerated healing and clearance of visible signs of infection [120].
Silver nanoparticles
Silver nanoparticles (AgNPs) possess unique properties that enable them to disrupt the microbial membrane, infiltrate the microbe's body, and cause internal damage. Their small size and large surface area contribute to their effectiveness in combating microbes. When bacteria come in contact with silver nanoparticles (Fig. 7c), they tend to clump together near the bacterial membrane. Nanoparticles can lead to cell breakdown and lipopolysaccharide (LPS) removal through membrane protrusions that bind to the nanoparticles. The nanoparticles enter the cell through electrostatic attraction. Silver nanoparticles (Ag NPs) have antimicrobial properties due to their ability to induce oxidative stress, release metal ions, and employ other non-oxidative mechanisms [121]. Even after prolonged use, dressings containing Ag NP do not appear to inhibit the proliferation of fibroblasts and keratinocytes, restoring normal skin [122]. Late precise audits and meta-examinations report silver sulfadiazine to have more unfortunate recuperating results and little proof of viability in forestalling twisted contamination than substitute dressings. Components accepted to be answerable for these results are the prerequisite for customary injury dressing changes, unfortunate eschar infiltration, and cytotoxicity of silver to keratinocytes and fibroblasts, deferring wound recuperating [123, 124].
Gold nanoparticles
Gold nanoparticles (AuNPs) have shown (Fig. 7b) promising results in viability studies with immune system cells, as they were found to be non-toxic and even reduced harmful reactive oxygen species [125]. Citrate-capped gold nanospheres were also found to be non-toxic in skin cells. AuNPs can easily permeate the skin, making them potential carriers for transdermal drug delivery without any toxic effects. In studies on rabbits and guinea pigs, AuNPs thermos responsive gels did not cause skin irritation or sensitization, making them a smart option for topical antibacterial drug delivery in cases of skin inflammation and wound healing [126]. The combination of nanogold, hyaluronic acid, and an adipocyte-targeting peptide has shown great promise in promoting lipolysis and breaking down fats. Irradiating the targeted site with a near-infrared laser selectively induces lipolysis in white fat, reducing body weight in obese mice. Additionally, injecting nanogold-coated polyethylene glycol into adipose tissue can enhance the effects of liposuction. In recent years, nanogold has also played a crucial role in developing coronavirus vaccines and virus detection, highlighting its significance in biomedicine [127]. The wound-healing efficiency of Au NRs was remarkable, after 14 days of daily treatment, they demonstrated almost completely healed wounds due to their enhanced skin re-epithelization effect and collagen formation. They also impacted the gene expression of inflammatory and anti-inflammatory mediators. Additionally, the deposition of Au NRs into different organs after topical wound treatment was insignificant. Gold nanoparticles made Au NRs-loaded into poloxamer 407 hydrogel, a promising gold-based nano-platform for accelerating wound healing [128].
Copper nanoparticles
After a thorough toxicity evaluation, copper-based nanomaterials could be used to speed up wound healing (Fig. 7d). In rats, the growth of keratinocytes, blood vessel formation (angiogenesis), fibroblast activity, collagen production, and the process of skin cell regeneration were all boosted by copper nanoparticles and enhanced wound healing in diabetic mice by producing key signal proteins like TGF, MMP-2, and VEGF. Additionally, copper nanoparticle-based nanocomposites are important in guiding cytokines, cells, and growth factors that promote wound recovery. The wound healing in mice was sped up by copper nanocomposites made with chitosan. These nanocomposites increased the levels of interleukin-10 (IL-10), VEGF, and TGF-1, while reducing tumor necrosis factor (TNF) [129]. Copper has strong biocidal properties and is well-metabolized by the human body, unlike silver. It plays a crucial role in skin regeneration and angiogenesis, accelerating the healing process in animal models. Copper enhances the expression of HIF-1α, which induces VEGF and angiogenesis, promoting wound healing. HIF-1α also binds to essential regions in the promoter and enhancer of HIF-1-regulated genes, further aiding in wound healing induced by copper [130].
Titanium dioxide
TiO2 NPs have remarkable antibacterial efficacy against a wide range of pathogens (Fig. 7f). They can inhibit bacterial growth through various mechanisms, making them a promising antimicrobial agent for wound dressings and coatings. TiO2 NPs also possess angiogenic properties, promoting blood vessel formation and facilitating efficient wound healing [131]. They have antioxidant effects as well, helping to scavenge reactive oxygen species and reduce oxidative stress in the wound microenvironment. Recent clinical studies have shown promising outcomes, and researchers are exploring different formulations like gels, creams, and dressings [132].
Cerium oxide
CeO2 NPs have strong antibacterial efficacy and can inhibit bacterial growth and biofilm formation (Fig. 7e). This makes them a potential antimicrobial agent for wound dressings and coatings. It's fascinating that CeO2 NPs also have angiogenic properties, promoting neovascularization and improving blood flow and tissue regeneration in wounds [133]. They also exhibit antioxidant effects, helping to scavenge reactive oxygen species and reduce oxidative stress in the wound microenvironment. Tthe translational potential of CeO2 NPs in wound care, developing formulations like hydrogels or dressings [134, 135].
Bioactive glass nanoparticles
Bioactive glass nanoparticles (BG NPs) have shown that they have impressive antibacterial properties, inhibiting microbial growth and preventing biofilm formation. This makes them a promising solution for combating infections in wounds [136, 137]. BG NPs have angiogenic properties, stimulating the formation of new blood vessels and promoting efficient nutrient and oxygen delivery to the wound site. This contributes to accelerated tissue regeneration. Additionally, BG NPs have antioxidant effects, reducing oxidative stress in the wound microenvironment by scavenging reactive oxygen species [138, 139].
Carbon nanotubes
Carbon nanotube (CNTs) have antibacterial properties, keeping bacterial growth in check and preventing infections in wounds. CNTs also can stimulate the formation of new blood vessels, improving blood circulation and ensuring that nutrients reach the wound site for tissue regeneration. They have antioxidant properties, helping to reduce oxidative stress in the wound area and enhancing the wound healing process [140].
Graphene-based nanomaterials
Graphene nanoparticles have emerged as a revolutionary component in the realm of wound healing, showcasing distinctive antibacterial, angiogenic, and antioxidant properties. Recent studies highlight the remarkable antibacterial efficacy of graphene nanoparticles, illustrating their ability to inhibit microbial growth and thwart infection in wound sites [141]. The angiogenic potential of graphene nanoparticles reveal their capacity to stimulate the formation of new blood vessels, promoting efficient nutrient and oxygen delivery critical for accelerated tissue regeneration. The multifaceted nature of graphene nanoparticles positions them as a promising and versatile tool for enhancing wound healing outcomes, signaling a transformative avenue in the landscape of advanced wound care [142].
Electrospinning nanofiber technology
Electrospinning is a technique that involves applying an electrostatic force to a polymer solution or melted polymer, resulting in the production of ultra-thin fibers. A high-voltage electrical supply, a needle/spinneret, and a grounded conductive collector are the main components of electrospinning (Fig. 8). The syringe is filled with the polymer solution, and the surface-electrified polymer solution holds fluid droplets. When the electrostatic force is applied, it creates repulsion between the like charges in the solution, causing the droplet to elongate into a cone shape called the “Taylor cone”. This cone forms a fiber jet as the repulsive forces overcome the surface tension. The jet stretches as it moves towards the collector. Eventually, the solvent evaporates, creating a solid non-woven fiber matt on the collector [149]. Electrospinning is a straightforward and adaptable method for extracting nanofibers (NFs) from viscoelastic fluids using electrostatic repulsion between surface charges. Because of their controllable diameter, arrangement, porosity, and surface properties as well as their ability to simulate extracellular matrix, electrospun nanofibers have been extensively utilized in tissue engineering. Electrospinning nanofibers are an ideal scaffold for skin tissue engineering because of their numerous wound-healing properties, high porosity, good hydrophilicity, controllable biodegradation, and good biocompatibility (Table 3) [150]. Electrospinning has been widely used to create nanofibrous materials that can be used as wound dressings because it is a process that is simple to operate, a wide variety of material options are available, and is economical. By tailoring dressings' physical and chemical properties, we can create highly specific dressings for wound healing applications. This customization allows for more effective and targeted treatment; synthetic and natural polymers are typically processed in blended solutions or co-electro-spun from different solutions [151]. Nanofiber wound dressings can prevent microbial infections by promoting high-gas permeation, supporting dermal drug delivery, enhancing fluid absorption, and stimulating hemostasis of damaged tissues and cell respiration. Nanofibers have incredible properties like enhanced mechanical strength, high porosity, and the ability to deliver bioactive substances. Electrospinning is an outstanding and highly effective method for producing polymeric nanofibers [152].
Natural polymer
Natural polymers are often used in regenerative medicine for wound and burn dressings because they are biodegradable, biocompatible, and have a similar structure to the extracellular matrix. Prompting and animating the injury-mending process, regular polymers are engaged with the maintenance of harmed tissues and, subsequently, skin recovery. Radiation processing also produces novel biomaterials made from renewable, non-toxic, and biodegradable natural polymers (Fig. 9) [153]. Collagen and gelatin are commonly used in wound dressings and tissue engineering products because they have hemostatic properties, are biocompatible, have low cytotoxicity, and promote cellular attachment and growth [24]. It's incredible that there are over 3,000 different types of wound dressings available, catering to various aspects of wound care (Table 3).
Chitosan
The wound-healing properties of dressings made of chitosan that are used to repair wounds are quite intriguing. However, chitosan's low mechanical strength is the main constraint on its use in wound repair. It has been combined with various kinds of inorganic nanomaterials to create an efficient wound care solution to get around this limitation. It is used in a wide range of applications due to its ease of deformation into gel, nanocomposite, scaffolds, sponges, beads, powder, and film [154]. The exchange of gases between the wound and the environment plays a vital role in the healing process. Wound dressings need to allow the passage of water vapor to prevent the buildup of exudate. However, it's important to find a balance because high rates of water vapor transmission can lead to wound dehydration. Additionally, chitosan could bind to DNA, which in turn inhibits the synthesis of mRNA and interferes with the growth of microorganisms [155, 156]. Chitosan (CS) is derived from chitin and is the second most abundant polysaccharide. It has some great properties like antibacterial and hemostatic effects. The composites containing CS and cellulose were studied for their absorption of anticoagulated whole blood, antimicrobial activity, and anti-inflammatory effects. They also looked at the reduction of interleukin-6 (IL-6) and tumor necrosis factor-a (TNF-a), as well as the compatibility with human fibroblasts [157]. Chitosan has a positive charge because of its amino groups, which allows it to interact with negatively charged microbial cell membranes. This interaction disrupts the integrity of the membranes and increases permeability. As a result, the structural integrity of the microbial cells is compromised, leading to leakage of intracellular components and eventually cell death [158, 159]. Chitosan also can bind with various microorganisms like bacteria and fungi, preventing their adhesion and colonization on surfaces. It can even inhibit the activity of certain enzymes crucial for microbial survival, which adds to its antimicrobial effect. Additionally, chitosan can induce the production of reactive oxygen species within microbial cells, causing oxidative stress and further compromising their viability [160].
Cellulose
Cellulose, which is a biopolymer made from glucose, is widely used in various industries. While cellulose is found in both plants and bacteria, bacterial cellulose is preferred for industrial applications because of its high purity and lack of byproducts. In the context of wound healing, cellulose PCL nanofibers can be coated with chitosan and type I collagen to create chitosan collagen double layers. These layers provide support for normal fibroblast growth in human skin [161]. Cellulose derivatives have a unique chemical structure that improves their water solubility. Because of this, they can be used as a base for different formulations and have great gelation properties. These derivatives can absorb and retain exudates from the wound site, causing them to swell. As a result, the newly formulated wound dressings can effectively maintain moisture on the wound bed and allow gas exchange with the environment [162].
Alginate
Alginate, derived from brown marine algae, is an anionic polysaccharide that consists of β-D-mannuronic acid and β-L-guluronic acid. It forms a linear polysaccharide and is commonly used in wound treatments and dressings. Alginate dressings, particularly those with a high content of G blocks, are popular in biomedical applications because of their ease of use and low immunogenicity. These dressings work by exchanging ions like calcium and sodium, which help promote wound healing [163]. PVA/SA nanofibers containing calendula herbal extract have been used as antibacterial wound dressings in tissue engineering. Researchers have also loaded ciprofloxacin into PVA/SA nanofibers for controlled drug delivery. Growth factors including heparin-like growth factor and TGF-β1 have been loaded into PVA/alginate nanofibers to support tissue repair. Collagen-grafted PVA/SA nanofibrous has been successfully used as an artificial skin substitute. Recently, PVA/SA nanofibers blended with sodium alginate-g-N-isopropylacrylamide have shown promise as smart wound dressings for controlled delivery of diclofenac sodium, an anti-inflammatory drug [164].
Silk fibroin
Silk fibroin, which is produced by insects like silkworms, is a remarkable natural polymer with great potential for wound healing. It's highly biocompatible, has anti-inflammatory properties, and shows promising anti-scarring effects. Using electrospinning, silk fibroin can be transformed into nanofibers to create wound dressings with bioactive properties. These nanofibers have the potential to effectively treat burn wounds by providing a protective and healing environment. The study showed that silk fibroin was used to treat second-degree burn wounds in male Sprague–Dawley rats, resulting in significantly lower expression levels of the pro-inflammatory cytokine IL-1α compared to a gauze control treatment. This suggests that silk fibroin has anti-inflammatory properties that could contribute to promoting wound healing. The study you mentioned observed that in silk fibroin-treated wounds, the expression of TGF-β1 peaked at Day 21 post-wounding, while gauze-treated wounds peaked at Day 7. Additionally, the silk fibroin nanofibers promoted rapid collagen formation, resulting in wound healing that closely resembled normal skin rather than forming scar tissue. This suggests that silk fibroin can potentially enhance the skin's regenerative properties [165]. Natural polymers have excellent healing properties that speed up wound healing. Some biological polymers cannot be electrospuned independently because they require a lot of processing [166].
Collagen
Collagen, a naturally occurring protein, is renowned for its exceptional wound healing properties. As a crucial component of the extracellular matrix in tissues, collagen plays a vital role in providing structural support and facilitating cellular interactions during the wound healing process. Its inherent biocompatibility, bioresorbability, and ability to promote cell migration make collagen an ideal biomaterial for wound dressings and tissue engineering applications [167, 168]. Furthermore, collagen's unique ability to modulate various stages of wound healing, including inflammation, proliferation, and tissue remodeling, underscores its significance in promoting effective and efficient recovery of damaged tissues [24, 169].
Gelatin
Gelatin, derived from collagen through partial hydrolysis, possesses notable wound healing properties. This natural polymer is widely recognized for its biocompatibility, biodegradability, and versatility in various biomedical applications. Gelatin's ability to form stable gels, combined with its favorable interactions with cells and tissues, makes it an excellent candidate for wound dressings and tissue engineering scaffolds [170]. The presence of cell-binding motifs within gelatin promotes cellular adhesion and migration, contributing to tissue regeneration. Additionally, gelatin's hemostatic properties and modulation of inflammatory responses further enhance its efficacy in wound healing applications [171, 172].
Dextran
Dextran, a natural polymer, stands out for its notable wound healing and antimicrobial properties. Renowned for its biocompatibility and hydrophilic characteristics, dextran has garnered attention in the realm of wound care. Its ability to form films, hydrogels, or nanofibers enhances its utility in advanced wound dressings [173, 174]. Dextran's capacity to maintain moisture at the wound site creates an optimal environment for tissue repair, while its inherent antimicrobial properties contribute to preventing or managing infections. Furthermore, dextran's anti-inflammatory attributes and promotion of cell proliferation play pivotal roles in supporting the wound healing process. The multifaceted properties of dextran make it a valuable component in designing biomaterials that not only aid in the efficient recovery of damaged tissues but also provide antimicrobial benefits for enhanced wound care [175].
Gellan gum
Gellan gum, a natural polymer, possesses notable wound healing properties coupled with antimicrobial and anti-inflammatory attributes. Recognized for its biocompatibility and ability to form stable gels, gellan gum has emerged as a promising biomaterial in the field of wound care. Its gel-forming capabilities enable the creation of wound dressings with optimal moisture retention, promoting a conducive environment for tissue regeneration. Moreover, gellan gum exhibits inherent antimicrobial properties, contributing to infection prevention and control. The polymer's anti-inflammatory characteristics further enhance its therapeutic potential in wound healing applications by modulating the inflammatory response. Overall, gellan gum's multifaceted nature positions it as a valuable natural polymer for designing advanced wound care materials with combined wound healing, antimicrobial, and anti-inflammatory benefits [176].
Agarose
Agarose, a natural polymer, exhibits remarkable wound healing properties, complemented by antimicrobial and anti-inflammatory attributes, along with the capacity for nanofiber formation. Widely recognized for its biocompatibility and gel-forming abilities, agarose has found applications in advanced wound dressings and tissue engineering. Its ability to form nanofibers enhances its utility in creating biomaterials with structural similarities to the extracellular matrix, promoting cell adhesion and tissue regeneration. Additionally, agarose's inherent antimicrobial properties contribute to infection control, while its anti-inflammatory characteristics aid in modulating the immune response during the wound healing process [177, 178].
Synthetic polymer
Over the years, wound dressing has undergone significant advancements. Nowadays, synthetic polymer dressings play a major role in wound management (Fig. 10). These dressings can be either passive or interactive. Passive dressings, like tulle and gauze, are non-occlusive and are used to cover wounds while promoting healing underneath (Table 3). On the other hand, interactive dressings, which are occlusive or semi-occlusive, provide a protective barrier against bacteria [179].
Poly (lactic-co-glycolic acid)
Due to their distinct properties, CS and poly (lactic-co-glycolic acid) (PLGA) electrospinning presents additional difficulties. However, NFs were found to be produced by electrospinning an emulsion made by mixing CS and PVA into a PLGA solution. PVA was chosen as an emulsifier in this case and was later removed from the scaffolds. Electrospinning the remaining homogeneous emulsion, yields NFs. The mechanical test demonstrated the great mechanical strength of the framework for biomedical applications [180]. The CS/PLGA scaffold aided fibroblast attachment and proliferation, as were advantageous interactions between cells and the matrix. Consequently, CS/PLGA scaffolds produced by emulsion electrospinning are a promising candidate for wound healing [181]. One such nano-formulation is NPs, which have been extensively used in therapeutic settings. Curcumin-loaded poly (lactic-co-glycolic acid) (PLGA) NPs were prepared by emulsification solvent evaporation. The study you mentioned showed that the PLGA-curcumin nanoparticles had a slow and controlled release of curcumin over 8 days. When they were injected into the skin of mice with wounds, they found that these nanoparticles helped improve the healing of the wounds compared to using empty PLGA nanoparticles or just applying curcumin locally. Histological studies using hematoxylin–eosin and Masson's trichrome staining showed that the treatment increased collagen content, granulation tissue formation, and wound maturity. The PLGA-curcumin nanoparticles have the potential to promote tissue regeneration and improve wound healing outcomes [182]. Compared to other studies, the treatment with PLGA-curcumin nanoparticles showed a decrease in the mRNA expression of Q9GPx and NFkB. These nanoparticles have antioxidant and anti-inflammatory activity, which can benefit wound healing [183].
Poly (vinyl alcohol)
Poly (vinyl alcohol) (PVA) is a synthetic polymer that is not carcinogenic. It is produced by hydrolysis, alcoholysis, or aminolysis of vinyl acetate. It is utilized in various biomedical applications because of its biocompatibility, biodegradability, non-toxic, hydrophilicity, and low propensity for protein grip. It has been extensively used for drug delivery and tissue regeneration. It is a highly versatile material that can be easily shaped into different forms like fibers, particles, sponges, textiles, and films. It also has excellent hydrophilic properties and can effectively absorb fluids. Because of these characteristics, PVA, or polyvinyl alcohol, has indeed been extensively used in wound dressings for both acute and chronic wounds. It's been utilized in developing biopolymer-based dressings to improve their mechanical properties for wound healing and skin regeneration. PVA wound dressings could be particularly beneficial for treating diabetic wounds due to their strong binding affinity with glucose [184].
Poly caprolactone (PCL)
A biocompatible and biodegradable polymer is produced by ring-opening polymerising caprolactone called PCL. As a medication conveyance framework supported by the FDA for use in people, PCL is broadly utilized as a biomaterial for wound mending processes as it can animate collagen creation. In other aliphatic polyesters, PCL has high hydrophobicity and slowly breaks down in the body by hydrolyzing its ester linkages. PCL is used to plan mixes with normal polysaccharides such as chitosan, alginate, or gelatin to further develop hydrophilicity, mechanical opposition, and tissue fix process applications [185]. Although synthetic polymer nanofibers can carry out structural programming, they do not have the required biological functions (Fig. 11). Traditional collagen and gelatin wound dressings are often considered passive because they lack the inherent capacity to promote healing activety.
Characteristics of nanofiber scaffold
Electrospun scaffolds have shown great potential for tissue engineering. However, their applications are still limited due to pore size and interconnectivity. These factors affect how cells infiltrate and grow into the scaffold. Using nanofibers as wound dressings, smaller pore sizes may limit cell connection and expansion on the outer layer of the nanofibers in tissue engineering applications [204]. With the growing number of wound occurrences, wound management has become critical. It has gained significant attention and is a crucial aspect of healthcare. Dressings are effective in wound management because they protect the wound's surface from infection and speed up healing. Because they encourage the migration of cells on the site of the wound as well as protect it from damage, wound dressings are leading the market for wound care. The electrospinning method is indeed used to fabricate nanofibrous dressings, which have gained widespread use in wound management. The electrospinning method is commonly used to create nanofibers with varying shapes and orientations when constructing scaffolds. These nanofibers provide a versatile and interconnected structure that is beneficial for tissue engineering and wound healing applications. The resulting non-woven scaffolds have been utilized in regenerative tissue engineering and are useful for drug delivery and treating wounds [205]. PCL (polycaprolactone) has shown great potential in developing platforms for enhancing wound healing. Nanofibers help improve biocompatibility, antibacterial properties, and the overall promotion of wound healing. The epidermal growth factor (EGF) covalently immobilizes on PCL and collagen nanofibers, it enhances the absorbency and biodegradability of the PCL nanofibers but also significantly boosts the expression of loricrin gene [206]. The human fibroblast cells could proliferate, adhere to the membrane, and maintain viability. In a nutshell, the electrospun membrane scaffold's use of synthetic and natural polymers contributed to developing wound dressings with desirable properties. Future work in wound healing includes integrating development factors, nutrients, cytokines, and other biomolecules into the platform to enhance the healing process [207]. An ideal injury dressing ought to follow the referenced qualities: (1) Control of dampness around the injury, (2) Extraordinary transmission of gases, (3) Dispose of abundant exudates, (4) Safeguard the injury from contaminations and microorganisms, (5) Decline surface corruption of wound, (6) Have mechanical security, (7) Effortlessly different and eliminated, (8) Biocompatible, biodegradable, flexible, and nontoxic, (9) Remember the injury agony, and (10) Exorbitant adequate [208].
In-vitro studies
The antibacterial wound dressings stop the wound from getting infected. Bacteria and microorganisms can easily enter chronic wounds, causing inflammation and impeding the healing process for extended periods [209]. Cuts, surgeries, burns, and other wounds expose subcutaneous tissue, providing a moist, warm, and nutritious environment ideal for microorganism growth. Because they have the potential to increase trauma and put financial strain on patients, wound infections are a serious possibility. Metallic nanoparticles, like silver and gold, can interact with cellular components and generate reactive oxygen species (ROS) that can cause cellular damage. The mechanism is often associated with the toxicity observed in cancer cells, parasites, and other microorganisms. Due to their biological reactivity, silver and gold nanoparticles are known to be particularly toxic. It's crucial to prioritize the safety and compatibility of phylogenetic silver and gold nanoparticles before utilizing them in biomedical applications. In a recent study, researchers tested the toxicity of silver nanoparticles derived from Salacia chinensis on normal human fibroblast cells (L929) in vitro [210]. The results were promising, as the nanoparticles showed a non-toxic nature. The cell viability remained high, with over 95% viability at all the tested concentrations. The hemolysis induced was less than 3%, which falls within the biocompatible range [211]. Chitosan has strong antimicrobial properties against both Gram-positive and Gram-negative bacteria. The effectiveness of chitosan's antimicrobial properties can be influenced by factors such as the type of pathogen, the media's pH, the chitosan's structure, and its concentration. These factors play a role in determining how well chitosan can combat bacteria. The pH of the media is an essential component in the antimicrobial action of chitosan below pH 6.5, and chitosan has antimicrobial properties [212].
Recent studies have shown that a spray formulation made from the latex extract of Jatropha curcas has been found to possess wound-healing properties (Table 4) [213]. The formulation was observed to enhance the production of type I collagen in human fibroblasts. After just 24 h of treatment, it showed the ability to accelerate wound healing in human keratinocyte and fibroblast cells. The formulation's primary active component, curcacycline A, is a cyclic octapeptide. The formulation using Jatropha curcas extract exhibited antioxidant effects in the DPPH assay and displayed antibacterial properties (Fig. 12) against various bacteria typically linked to wound infections. This formulation holds tremendous promise for wound healing treatments [214]. Honey is a natural antibiotic that can effectively fight against bacterial biofilms and resistant microorganisms. Its high osmolality, acidity, and glucose oxidase content contribute to its strong antibacterial properties (Table 4). Biofilm refers to microorganism communities in wounds, which can hinder the healing process due to increased bacterial resistance. However, honey comes to the rescue by also being effective against biofilm bacteria [215]. When curcumin was released from electrospun nanofibers made of chitosan and polylactic acid, it showed no harmful effects on L-929 fibroblast cells and increased antioxidant activity in vitro. These nanofibers significantly reduced wound size in an extraction and cut rodent wound model. In the case of electrospinning curcumin-incorporated polycaprolactone/chitosan nanofibers, about 80% of the curcumin was released within the first hundred hours [216].
Bactericidal activity of (1) S. spinosa extract, (2) distilled water, and (3) biosynthesized Ag NPs from S. spinosa extract, against a E. coli, b B. subtilis and c B. vallismortis [124]
Lipoteichoic acid, found in Gram-positive bacteria's cell walls, can stimulate the immune system and play a vital role in bacterial growth and physiology. It acts as a pathogen-associated molecular motif, which leads to nitric oxide production and activates NF-kB. This, in turn, triggers the production of pro-inflammatory mediators and cytokines [232]. Lipoteichoic acid derived from beneficial probiotics has been shown to have some amazing effects. It promotes tolerance, prevents TNF-α sepsis by inhibiting pro-inflammatory cytokine production, and enhances resistance to microbial infection in dermal cells [233].
Moreover, when applied topically, lipoteichoic acid activates toll-like receptors and human β-defensin mechanisms, providing skin protection against microbial infections and exhibiting antimicrobial properties [234]. ROS, or reactive oxygen species, play a crucial role in cellular processes like communication, differentiation, immunity, and even fighting bacteria in wounds. However, exposure to ROS for too long can lead to oxidative stress, which is harmful to cells. This oxidative stress can hinder wound-healing by causing inflammation, lipid peroxidation, DNA degradation, and enzyme inactivity. Topical application of antioxidants can help heal wounds by neutralizing free radicals and promoting skin recovery. Clinical studies have indeed shown that curcumin has antioxidant properties. In vitro experiments with a collagen network treated with curcumin demonstrated its ability to scavenge peroxide radicals. Another study using an in vivo rat model found that applying curcumin significantly reduced H2O2-induced damage to fibroblasts and keratinocytes. The use of bioactive glass-loaded nanofibers in promoting wound closure is quite promising. In a study with SD rats, those treated with these nanofibers had the smallest skin wounds by day 14, indicating their potential for promoting re-epithelialization and wound healing. Additionally, collagen, gelatin, and PHB with ostholamide have shown impressive antibacterial activity against P. aeruginosa [192, 193]. In recent years, numerous hemostatic dressings based on chitosan have been developed. Due to their ability to form cationic clusters that can interact with anions on red blood cells, chitosan nanofibers have remarkable hemostatic properties, accelerating platelet aggregation and ultimately stopping blood loss. This mechanism is effective even in patients with coagulation disorders and does not depend on a patient's clotting mechanism [235].
In-vivo studies
The studies have established that rodents, especially mice, are the most commonly used animal models for wound care investigations. They have several advantages, such as their ability to reproduce quickly, allowing for multiple study generations. While higher animal models like rabbits and guinea pigs exist, porcine models, which have similar skin structure and biochemistry to humans, are less frequently employed due to cost, handling difficulties, and a lack of appropriate genetic tools [236]. Murine excisional wound models, using rats and mice, are the primary animal models used in wound healing research (Fig. 13). The anatomical, physiological, and genetic similarities between rodents and humans make them a preferred choice for various research areas. Using animal models with controlled experimental, environmental, and genetic variables allows for smaller sample sizes and more reliable results. These models will enable us to measure and monitor different stages of wound healing, especially the inflammatory and proliferative phases. Some studies tend to use male animals more frequently due to the impact of hormonal cycles in females and their heightened sensitivity to toxicity [237]. The in vivo evaluation of dual-growth factor-releasing meshes on rat skin wounds yielded promising results [238].
In-vivo healing effect a The photographs and wound size of full-thickness wound healing process after treating with control, 2D, 3D-TA1.0 at various day intervals [239]
Meshes can be easily attached to the wounds without the need for adhesives. The electrospun meshes kept the wounds hydrated and became invisible after a few hours. The meshes with growth factors showed significantly better wound closure rates compared to other samples at weeks 1 and 2. After 4 weeks, all wounds were closed, but the 2:1 CS/PEO-NPs mesh had the smallest scar formation and more hair coverage, indicating faster healing. The research investigated how effective Pκ-CaC 8:2 and Pκ-CaC 6:4 hydrogel wound dressings were on mice with full-thickness circular excision wounds [240]. The groups treated with hydrogel showed faster wound healing than the control group, with less noticeable scarring. It's amazing how composite hydrogel dressings, like Pκ-CaC 6:4, can speed up the closure of wounds. The study also emphasized the potential of natural polymers like chitosan in promoting wound healing [241]. The study investigated the wound healing effects of ENS Mh (manuka honey) 15%@PVP mats compared to a traditional wound dressing on mice with circular wounds on their dorsal back [242]. The advanced dressing with ENS Mh@PVP showed great results in wound healing. It helped with faster epithelialization, reduced wound size, and higher-quality healing with hair growth and minimal scarring. The immunomodulatory properties of ENS Mh played a role in accelerating the healing process and promoting collagen synthesis. Manuka honey dressings also effectively prevented scarring and reduced inflammation [243].
Perspective
Wound healing is a complex process, and traditional folk medicine has identified numerous plants with validated wound-healing properties. In vitro studies have used crude plant extracts or isolated secondary metabolites to explore their potential in wound healing further. These plants have medicinal properties for various conditions, including arthritis, snake bites, and skin diseases, and even have anticancer, anti-inflammatory, antifeedant, and muscle relaxant properties [244]. When tissue is damaged by physical, chemical, microbiological, or immunological agents, wound healing preserves the tissue's standard structure and function, ensuring its survival [245]. Electrospun nanofibers have numerous advantages for wound dressings, such as high air permeability, moisture absorption, and protection against external factors. When combined with herbal compounds, these nanofibers can further enhance their properties. It's great to see the integration of plant compounds into electrospinning techniques, as natural alternatives are in high demand due to concerns about antibiotic resistance and additives' side effects. Electro-spun fiber scaffolds will likely be multifunctional to aid in wound healing at multiple stages. Products should be designed to meet the specific needs and characteristics of different stages of wound healing. In particular, electro-spun fiber scaffolds can easily incorporate specialized stem cells, enabling a controlled and precise release of multiple drugs. This system can improve the anti-inflammatory and antibacterial activities of wounds, promote blood purification and blood separation in wounds, and ultimately promote wound healing by tailoring the amount and progress of drug release (simultaneous or continuous stepwise release) to the stage of wound healing [246]. Recent studies on electrospinning dressings in wound healing have shown great potential in enhancing the healing process. They have nanofibrous structures that mimic the extracellular matrix, controlled drug delivery systems, and even antimicrobial agents. Researchers are focusing on using biodegradable materials to make dressing removal easier, and they are also exploring ways to integrate cells within the electrospun scaffolds to promote tissue regeneration [247, 248].
Toll-like receptors (TlRs) recognize patterns in pathogens and trigger immune responses. They can detect components of protozoa, bacteria, and viruses, sending signals to the immune system. Interestingly, TlRs can also be activated by molecules released from damaged cells, known as damage-associated molecular patterns (DAMPs). These patterns are usually hidden but become recognizable during injury. TlRs and other receptors trigger inflammation when tissue damage occurs protecting tissue integrity and aiding in wound healing [249]. Gene expression regulation is a key factor in determining the quality of healing. There are significant changes in gene expression levels throughout the different stages of healing. Important genes involved in wound healing include VEGF, TGF-β, EGF, IL, and TNF-α. In the later stages of healing, EGF, TGF-β, and VEGF are upregulated, while TNF-α and IL are downregulated. In the future, we plan to study the molecular mechanisms of the healing process by quantitatively assessing the gene expression levels of these biomarkers using real-time PCR in rat skin at various stages of healing after treatment with our nanofiber [250]. While there is growing interest in using plant extracts and nanoparticles incorporated into nanofiber scaffolds for wound healing applications, there is a need for comprehensive research that assesses the effectiveness, safety, and long-term implications of such approaches in clinical settings. Many studies have shown promising results in laboratory settings, but translating these findings into safe and effective wound-healing therapies for human patients requires further investigation [251]. Research into personalized wound care takes into account an individual's genetics, microbiome, and specific wound characteristics. Optimized treatment plans based on patient-specific data to enhance the long-term healing process. Managing chronic wounds, like diabetic ulcers and pressure sores, can be quite challenging. Conventional treatments may not always be effective, leading to prolonged suffering for patients. It's crucial to explore and develop comprehensive strategies that prioritize prevention, early intervention, and long-term care for these types of wounds.
Summary
Due to their impressive biocompatibility and wet stability, cross-linked electrospun nanofibers have shown tremendous promise in wound healing. Researchers have been diving deep into different materials and bioactive agents to enhance the healing properties of electrospun wound dressings. One particularly exciting avenue of research is the use of natural products as antimicrobial and antioxidant additives in wound dressings. By harnessing the power of nature, scientists are exploring the potential of these natural compounds to accelerate the healing process. The idea of extracting bioactive substances from various sources is also captivating. However, it's crucial to conduct thorough clinical trials to ensure the safety and efficacy of these natural products. We must address toxicity and safety concerns when incorporating them into wound dressings. Trauma dressings face diverse challenges in the future, depending on the specific type of trauma. Infection control, rapid and effective hemostasis, personalization for different wound types, biocompatibility, moisture management, long-term stability, and ease of application are all important areas of concern. The continuous advancements in wound treatment techniques, such as integrating gene editing tools, material science engineering, and interdisciplinary approaches, offer immense potential to revolutionize wound care. These innovations can enhance skin regeneration and repair, ultimately leading to more effective and efficient wound-healing methods.
References
Mahmoudi N, Eslahi N, Mehdipour A, Mohammadi M, Akbari M, Samadikuchaksaraei A, et al. Temporary skin grafts based on hybrid graphene oxide-natural biopolymer nanofibers as effective wound healing substitutes: pre-clinical and pathological studies in animal models. J Mater Sci Mater Med. 2017. https://doi.org/10.1007/s10856-017-5874-y.
Tottoli EM, Dorati R, Genta I, Chiesa E, Pisani S, Conti B. Skin wound healing process and new emerging technologies for skin wound care and regeneration. Pharmaceutics. 2020. https://doi.org/10.3390/pharmaceutics12080735.
Muniandy K, Gothai S, Tan WS, Kumar SS, Esa NM, Chandramohan G, et al. In Vitro wound healing potential of stem extract of Alternanthera sessilis. Evid Based Complement Alternat Med. 2018;2018:1.
Ellis S, Lin EJ, Tartar D. Immunology of wound healing. Curr Dermatol Rep. 2018;7:350–8. https://doi.org/10.1007/s13671-018-0234-9.
Karppinen S-M, Heljasvaara R, Gullberg D, Tasanen K, Pihlajaniemi T. Toward understanding scarless skin wound healing and pathological scarring. Res. 2019;8:787.
Potekaev NN, Borzykh OB, Medvedev GV, Pushkin DV, Petrova MM, Petrov AV, et al. The role of extracellular matrix in skin wound healing. J Clin Med. 2021. https://doi.org/10.3390/jcm10245947.
Wilkinson HN, Hardman MJ. Wound healing: cellular mechanisms and pathological outcomes. Open Biol. 2020. https://doi.org/10.1098/rsob.200223.
Kaparekar PS, Anandasadagopan SK. The potential role of bioactive plant-based polyphenolic compounds and their delivery systems—as a promising opportunity for a new therapeutic solution for acute and chronic wound healing. Curr Pharmacol Rep. 2022;8:321–38.
Low JS, Mak KK, Zhang S, Pichika MR, Marappan P, Mohandas K, et al. In vitro methods used for discovering plant derived products as wound healing agents—an update on the cell types and rationale. Fitoterapia. 2021;154:1–8.
Cañedo-Dorantes L, Cañedo-Ayala M. Skin acute wound healing: a comprehensive review. Int J Inflam. 2019;2019:3706315. https://doi.org/10.1155/2019/3706315.
Martin P, Nunan R. Cellular and molecular mechanisms of repair in acute and chronic wound healing. Br J Dermatol. 2015;173:370–8.
Gebremeskel L, Bhoumik D, Sibhat GG, Tuem KB. In Vivo wound healing and anti-inflammatory activities of leaf latex of aloe megalacantha baker (Xanthorrhoeaceae). Evid Based Complement Alternat Med. 2018;2018:7.
Neto JA, Tarôco BR, Dos Santos HB, Thomé RG, Wolfram E, de Ribeiro ARI. Using the plants of Brazilian Cerrado for wound healing: from traditional use to scientific approach. J Ethnopharmacol. 2020;260:112547.
Diniz LRL, Calado LL, Duarte ABS, de Sousa DP. Centella asiatica and its metabolite asiatic acid: wound healing effects and therapeutic potential. Metabolites. 2023;13:13.
Saleem U, Khalid S, Zaib S, Anwar F, Ahmad B, Ullah I, et al. Phytochemical analysis and wound healing studies on ethnomedicinally important plant Malva neglecta Wallr. J Ethnopharmacol. 2020. https://doi.org/10.1016/j.jep.2019.112401.
Addis R, Cruciani S, Santaniello S, Bellu E, Sarais G, Ventura C, et al. Fibroblast proliferation and migration in wound healing by phytochemicals: evidence for a novel synergic outcome. Int J Med Sci. 2020;17:8.
Chinnasamy G, Chandrasekharan S, Koh TW. Synthesis, characterization, antibacterial and wound healing efficacy of silver nanoparticles from Azadirachta indica. Front Microbiol. 2021;12:1–14.
Zangeneh MM. Preparation, characterization, and evaluation of cytotoxicity, antioxidant, cutaneous wound healing, antibacterial, and antifungal effects of gold nanoparticles using the aqueous extract of Falcaria vulgaris leaves. Appl Organ Chem. 2019;33:1–17.
Kalalinia F, Taherzadeh Z, Foroghinia N, Beheshti M. Evaluation of wound healing effciency of vancomycin-loaded electrospun chitosan/poly ethylene oxide nano fibers in full thickness wound model of rat. Int J Biol Macromol. 2021;177:100–10.
Prasathkumar M, Sadhasivam S. Chitosan/Hyaluronic acid/Alginate and an assorted polymers loaded with honey, plant, and marine compounds for progressive wound healing—know-how. Int J Biol Macromol. 2021;186:656–85.
Pamu D, Tallapaneni V, Karri VVSR, Singh SK. Biomedical applications of electrospun nanofibers in the management of diabetic wounds. Drug Deliv Transl Res. 2022;12:158–66. https://doi.org/10.1007/s13346-021-00941-6.
Naeimi A, Payandeh M, Ghara AR, Ghadi FE. In vivo evaluation of the wound healing properties of bio-nano fiber chitosan/polyvinyl alcohol incorporating honey and Nepeta dschuparensis. Carbohydr Polym. 2020;240:116315.
Abou Zekry SS, Abdellatif A, Azzazy HME. Fabrication of pomegranate/honey nanofibers for use as antibacterial wound dressings. Wound Med. 2020. https://doi.org/10.1016/j.wndm.2020.100181.
Gaspar-Pintiliescu A, Stanciuc AM, Craciunescu O. Natural composite dressings based on collagen, gelatin and plant bioactive compounds for wound healing: a review. Int J Biol Macromol. 2019;138:854–65.
Vitor T, Lordani TV, de Lara CE, Ferreira FB, de Souza Terron MM, et al. Review article therapeutic effects of medicinal plants on cutaneous wound healing in humans : a systematic review. Mediat Inflamm. 2018. https://doi.org/10.1155/2018/7354250.
Piipponen M, Li D, Landén NX. The immune functions of keratinocytes in skin wound healing. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21228790.
Landén NX, Li D, Ståhle M. Transition from inflammation to proliferation: a critical step during wound healing. Cell Mol Life Sci. 2016;73:3861–85.
Shomita S, Mathew-Steiner, Roy S, Sen CK. Collagen in wound healing. Bioengineering. 2021;8:63.
Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16:585–601.
Wang Y, Luo M, Li T, Xie C, Li S, Lei B. Multi-layer-structured bioactive glass nanopowder for multistage-stimulated hemostasis and wound repair. Bioact Mater. 2023;25:319–32.
Okur ME, Karantas ID, Şenyiğit Z, Üstündağ Okur N, Siafaka PI. Recent trends on wound management: new therapeutic choices based on polymeric carriers. Asian J Pharm Sci. 2020;15:661–84.
Subramaniam T, Fauzi MB, Lokanathan Y, Law JX. The role of calcium in wound healing. Int J Mol Sci. 2021;22:6486.
Chen WYJ, Rogers AA, Lydon MJ. Characterization of biologic properties of wound fluid collected during early stages of wound healing. J Investig Dermatol. 1992;99:559–64.
Etxabide A, Kilmartin PA, Maté JI. Color stability and pH-indicator ability of curcumin, anthocyanin and betanin containing colorants under different storage conditions for intelligent packaging development. Food Control. 2020. https://doi.org/10.1016/j.foodcont.2020.107645.
Hou Y, Li J, Guan S, Witte F. The therapeutic potential of MSC-EVs as a bioactive material for wound healing. Eng Regen. 2021;2:182–94.
Huang C, Xu X, Fu J, Yu DG, Liu Y. Recent progress in electrospun polyacrylonitrile nanofiber-based wound dressing. Polymers. 2022;14:1–33.
Singer AJ. Healing mechanisms in cutaneous wounds: tipping the balance. Tissue Eng Part B Rev. 2021;28:1151–67. https://doi.org/10.1089/ten.teb.2021.0114.
Chingwaru AC, Bagar T, Maroyi A, Kapewangolo PT, Chingwaru W. Wound healing potential of selected Southern African medicinal plants: a review. J Herbal Med. 2019. https://doi.org/10.1016/j.hermed.2019.100263.
Steffy K, Shanthi G, Maroky AS, Selvakumar S. Potential bactericidal activity of S nux-vomica—ZnO nanocomposite against multidrug-resistant bacterial pathogens and wound-healing properties. J Trace Element Med Biol. 2018;50:229.
Shakib Z, Shahraki N, Razavi BM, Hosseinzadeh H. Aloe vera as an herbal medicine in the treatment of metabolic syndrome: a review. Phytother Res. 2019;33:2649–60.
Sharma A, Khanna S, Kaur G, Singh I. Medicinal plants and their components for wound healing applications. Futur J Pharm Sci. 2021;7:53. https://doi.org/10.1186/s43094-021-00202-w.
Fan S, Wykes MSD, Lin WE, Jones RL, Robins AG, Linden PF. A full-scale field study for evaluation of simple analytical models of cross ventilation and single-sided ventilation. Build Environ. 2020. https://doi.org/10.1016/j.buildenv.2020.107386.
Hou J, Gu Y, Zhao S, Huo M, Wang S, Zhang Y, et al. Anti-inflammatory effects of aurantio-obtusin from seed of Cassia obtusifolia L. through modulation of the NF-κB pathway. Molecules. 2018;23:3093.
Danna C, Bazzicalupo M, Ingegneri M, Smeriglio A, Trombetta D, Burlando B, et al. Anti-inflammatory and wound healing properties of leaf and rhizome extracts from the medicinal plant Peucedanum ostruthium (L.) W. D. J. Koch. Molecules. 2022;27:4271.
Nani M, Leone A, Bom VP, Buszinski AF, Oliveira de Souza R, Pinheiro VA, et al. Evaluation and comparison of wound healing properties of an ointment (AlpaWash) containing Brazilian micronized propolis and peucedanum ostruthium leaf extract in skin ulcer in rats. Int J Pharm Compd. 2018;22:154–63.
Ahmed HE, Iqbal Y, Aziz MH, Atif M, Batool Z, Hanif A, et al. Green synthesis of CeO2 nanoparticles from the abelmoschus esculentus extract: evaluation of antioxidant, anticancer, antibacterial, and wound-healing activities. Molecules. 2021;26:4659.
Korani S, Rashidi K, Hamelian M, Jalalvand AR, Tajehmiri A, Korani M, et al. Evaluation of antimicrobial and wound healing effects of gold nanoparticles containing Abelmoschus esculentus (L.) aqueous extract. Bioinorg Chem Appl. 2021;2021:1.
Mohanta YK, Biswas K, Jena SK, Hashem A, AbdAllah EF, Mohanta TK. Anti-biofilm and antibacterial activities of silver nanoparticles synthesized by the reducing activity of phytoconstituents present in the indian medicinal plants. Front Microbiol. 2020;11:1–15.
Sharma P, Dwivedee BP, Bisht D, Dash AK, Kumar D. The chemical constituents and diverse pharmacological importance of Tinospora cordifolia. Heliyon. 2019. https://doi.org/10.1016/j.heliyon.2019.e02437.
Modi B, Shah KK, Shrestha J, Shrestha P, Basnet A, Tiwari I, et al. Morphology, biological activity, chemical composition, and medicinal value of Tinospora cordifolia (willd) Miers. Adv J Chem-Sect B. 2021;3:36–53.
Liyanaarachchi GD, Samarasekera JKRR, Mahanama KRR, Hemalal KDP. Tyrosinase, elastase, hyaluronidase, inhibitory and antioxidant activity of Sri Lankan medicinal plants for novel cosmeceuticals. Ind Crops Prod. 2018;111:597–605.
Buzinaro MAP, Ferreira NS, Cunha F, Macêdo MA. Hopkinson effect, structural and magnetic properties of M-type Sm3+-doped SrFe12O19 nanoparticles produced by a proteic sol–gel process. Ceram Int. 2015. https://doi.org/10.1016/j.ceramint.2015.12.130.
Zofou D, Matumamboh EE, Shu G, Tsague Manfo FP, Teugwa Mofor C, Sofeu Feugaing DD, et al. In vivo assessment of antidiabetic activity and safety of polyherbal teas from selected Cameroonian medicinal plants: Persea americana, Ageratum conyzoides and Mangifera indica. Investig Med Chem Pharmacol. 2023;6:1–9.
Coelho EM, de Souza ME, Corrêa LC, Viana AC, de Azevêdo LC, dos Santos LM. Bioactive compounds and antioxidant activity of mango peel liqueurs (Mangifera indica L.) produced by different methods of maceration. Antioxidants. 2019. https://doi.org/10.3390/antiox8040102.
Moglad EH, Hamad AM, Fatima F, Devanathadesikan V. Biological sciences antimicrobial and wound healing activities of certain Sudanese medicinal plants. Saudi J Biol Sci. 2020;27:1766–72.
Boakye YD, Agyare C, Ayande GP, Titiloye N, Asiamah EA, Danquah KO. Assessment of wound-healing properties of medicinal plants : the case of Phyllanthus muellerianus. Front Pharmacol. 2018;9:1–12.
Addotey JN, Lengers I, Jose J, Hensel A. Hyal-1 inhibitors from the leaves of Phyllanthus muellerianus (Kuntze) excell. J Ethnopharmacol. 2019;236:326–35.
Alsarayreh AZ, Oran SA, Shakhanbeh JM, Khleifat KM, Al Qaisi YT, Alfarrayeh II, et al. Efficacy of methanolic extracts of some medicinal plants on wound healing in diabetic rats. Heliyon. 2022. https://doi.org/10.1016/j.heliyon.2022.e10071.
Paul ZA, Malla AT, Dar MA, Masoodi MH. Phytochemistry and pharmacological activity of Malva sylvestris L : a detailed insight. Comb Chem High Throughput Screen. 2023. https://doi.org/10.2174/0113862073269336231009110313.
Danna C, Bazzicalupo M, Ingegneri M, Smeriglio A, Trombetta D, Burlando B, et al. Anti-inflammatory and wound healing properties of leaf and rhizome extracts from the medicinal plant Peucedanum ostruthium (L.) W. D. J. Koch. Molecules. 2022;27:1–16.
Apiaceae LWDJK, Vitalini S, Palmioli A, Orlando F, Scarì G, Airoldi C, et al. Phytotoxicity, nematicidal activity and chemical constituents of Peucedanum ostruthium (L.) W. D. J. Koch (Apiaceae). Indus Crop Prod. 2021. https://doi.org/10.1016/j.indcrop.2021.113499.
Mirbehbahani FS, Hejazi F, Najmoddin N, Asefnejad A. Artemisia annua L. as a promising medicinal plant for powerful wound healing applications. Prog Biomater. 2020. https://doi.org/10.1007/s40204-020-00138-z.
Abate G, Zhang L, Pucci M, Morbini G, Mac Sweeney E, Maccarinelli G, et al. Phytochemical analysis and anti-inflammatory activity of different ethanolic phyto-extracts of Artemisia annua L. Biomolecules. 2021. https://doi.org/10.3390/biom11070975.
Kazemian H, Ghafourian S, Sadeghifard N, Houshmandfar R, Badakhsh B, Taji A, et al. In vivo antibacterial and wound healing activities of Roman Chamomile (Chamaemelum nobile). Infect Disord Drug Targets. 2018;18:41–5.
Liu X, Wang X, Chen Z, Ye J, Liao Y, Zhang W, et al. De novo assembly and comparative transcriptome analysis: novel insights into terpenoid biosynthesis in Chamaemelum nobile L. Plant Cell Rep. 2019;38:101–16. https://doi.org/10.1007/s00299-018-2352-z.
Lulseged K, Akele MZ, Abiye AA, Abebe B, Assefa HS. Wound healing and antioxidant properties of 80% methanol leaf extract of Verbascum sinaiticum (Scrophulariaceae): an Ethiopian medicinal plant. Evid-based Comp Alt Med. 2022. https://doi.org/10.1155/2022/9836773.
Asefa M, Teshome N, Degu A. Anti-Inflammatory and analgesic activity of methanolic root extract of Verbascum sinaiticum Benth. J Inflamm Res. 2022;15:6381–92.
Saqallah FG, Hamed WM, Talib WH. In vivo evaluation of Antirrhinum majus’ wound-healing activity. Sci Pharm. 2018;86:45.
Heffron LM, Korban SS. Elucidating the ethylene response and tolerance in non-mutagenized and mutagenized snapdragon (Antirrhinum majus L.) lines using 1-aminocyclopropane-1-carboxylic acid (ACC). Plant Growth Regul. 2023;100:133–45. https://doi.org/10.1007/s10725-022-00945-3.
Muniandy K, Gothai S, Tan WS, Kumar SS, Mohd Esa N, Chandramohan G, et al. In Vitro wound healing potential of stem extract of Alternanthera sessilis. Evidence-based Comp Alt Med. 2018;2018:13.
Qian L, Su W, Wang Y, Dang M, Zhang W, Wang C. Synthesis and characterization of gold nanoparticles from aqueous leaf extract of Alternanthera sessilis and its anticancer activity on cervical cancer cells (HeLa). Artif Cells Nanomed Biotechnol. 2019;47:1173–80. https://doi.org/10.1080/21691401.2018.1549064.
Soib HH, Ismail HF, Husin F, Bakar MHA, Yaakob H, Sarmidi MR. Bioassay-guided different extraction techniques of Carica papaya (Linn.) leaves on In Vitro wound-healing activities. Molecules. 2020;2020(25):1–13.
Khor B-K, Chear NJ, Azizi J, Khaw K-Y. Chemical composition, antioxidant and cytoprotective potentials of carica papaya leaf extracts: a comparison of supercritical fluid and conventional extraction methods. Molecules. 2021. https://doi.org/10.3390/molecules26051489.
Lordani TV, de Lara CE, Ferreira FB, de Souza Terron Monich M, Mesquita C, Felicetti Lordani CR, et al. Therapeutic effects of medicinal plants on cutaneous wound healing in humans: a systematic review. Mediators Inflamm. 2018; 2018: 7354250. https://doi.org/10.1155/2018/7354250
Sychrová A, Škovranová G, Čulenová M, Bittner FS. Prenylated flavonoids in topical infections and wound healing. Molecules. 2022;27:4491.
Kaparekar PS, Anandasadagopan SK. The potential role of bioactive plant-based polyphenolic compounds and their delivery systems—as a promising opportunity for a new therapeutic solution for acute and chronic wound healing. Curr Pharmacol Rep. 2022;8:321–38. https://doi.org/10.1007/s40495-022-00296-7.
Emmanuel S. Phytotherapeytic mechanism of medicinal plants with wound healing potential. 2021.
Ghiulai R, Roşca OJ, Antal DS, Mioc M, Mioc A, Racoviceanu R, et al. Tetracyclic and pentacyclic triterpenes with high therapeutic efficiency in wound healing approaches. Molecules. 2020;25:1–38.
Luo C, Huang C, Zhu L, Kong L, Yuan Z, Wen L, et al. Betulinic acid ameliorates the T-2 toxin-triggered intestinal impairment in mice by inhibiting inflammation and mucosal barrier dysfunction through the NF-κB signaling pathway. Toxins. 2020;12:794.
Komakech R, Matsabisa MG, Kang Y. The wound healing potential of Aspilia africana (Pers.) C. D. Adams (Asteraceae). Evid-based Comp Alt Med. 2019;2019:1.
Oguntibeju OO. Medicinal plants and their effects on diabetic wound healing. Vet World. 2019;12:653–63.
Sanik F, Rahman H, Rahman AO, Samudra AG, de Floris C, Muhaimin M. Incision wound healing test ethanolic extract gel from Ekor Naga (Rhaphidophora pinnata (L.f) Schott) leaves in white male rats. Pharmaciana. 2022;12:173.
Quave CL. Wound healing with botanicals : a review and future perspectives. Curr Dermatol Rep. 2018;7:287–95.
Aqsa T, Shafique MS, Qureshi U, Changeez M, Afzal S. Efficacy of Aloe Vera cream for healing diabetic foot ulcers. J Rawalpindi Med Coll. 2019;23:113–5.
Kędzierska M, Jamroży M, Kudłacik-Kramarczyk S, Drabczyk A, Bańkosz M, Potemski P, et al. Physicochemical evaluation of l-ascorbic acid and aloe vera-containing polymer materials designed as dressings for diabetic foot ulcers. Materials. 2022;15:1–19.
Aleem M. Anti-inflammatory and anti-microbial potential of Plumbago zeylanica L.: a review. J Drug Deliv and Ther. 2020;10:229–35.
Periasamy H, Iswarya S, Pavithra N, Senthilnathan S, Gnanamani A. In vitro antibacterial activity of plumbagin isolated from Plumbago zeylanica L. against methicillin-resistant Staphylococcus aureus. Lett Appl Microbiol. 2019;69:41–9.
Kakade PS, Zimare SB. Phytochemistry and pharmacological studies of plumbago indica L.: a medicinal plant review. Phytochem Pharmacol Med Plants. 2023;12:213–25.
De Luca I, Pedram P, Moeini A, Cerruti P, Peluso G, Di Salle A, et al. Nanotechnology development for formulating essential oils in wound dressing materials to promote the wound-healing process : a review. Appl Sci. 2021;11:1713.
Ezhilarasu H, Vishalli D, Dheen ST, Bay B-H, Srinivasan DK. Nanoparticle-based therapeutic approach for diabetic wound healing. Nanomaterials. 2020;10:1234.
Naderi N, Karponis D, Mosahebi A, Seifalian AM. Nanoparticles in wound healing ; from hope to promise , from promise to routine Division of Surgery and Interventional Science , University College London , London , UK , 2 Reconstructive Surgery and Regenerative Medicine Group , Institute of Life Science. 2018; 1038–59.
Loo HL, Goh BH, Lee LH, Chuah LH. Application of chitosan-based nanoparticles in skin wound healing. Asian J Pharm Sci. 2022;17:299–332.
Muhammad G, Hussain MA, Amin M, Hussain SZ, Hussain I, Abbas Bukhari SN, et al. Glucuronoxylan-mediated silver nanoparticles: Green synthesis, antimicrobial and wound healing applications. RSC Adv. 2017;7:42900–8.
Naraginti S, Kumari PL, Das RK, Sivakumar A, Patil SH, Andhalkar VV. Amelioration of excision wounds by topical application of green synthesized, formulated silver and gold nanoparticles in albino Wistar rats. Mater Sci Eng C. 2016;62:293–300.
Rafique M, Sadaf I, Rafique MS, Tahir MB. A review on green synthesis of silver nanoparticles and their applications. Artif Cells Nanomed Biotechnol. 2017;45:1272–91. https://doi.org/10.1080/21691401.2016.1241792.
Kaplan Ö, Gökşen Tosun N, Özgür A, Erden Tayhan S, Bilgin S, Türkekul İ, et al. Microwave-assisted green synthesis of silver nanoparticles using crude extracts of Boletus edulis and Coriolus versicolor: characterization, anticancer, antimicrobial and wound healing activities. J Drug Deliv Sci Technol. 2021;64:102641.
Veeraraghavan VP, Periadurai ND, Karunakaran T, Hussain S, Surapaneni KM, Jiao X. Green synthesis of silver nanoparticles from aqueous extract of Scutellaria barbata and coating on the cotton fabric for antimicrobial applications and wound healing activity in fibroblast cells (L929). Saudi J Biol Sci. 2021;28:3633–40.
Rather HA, Thakore R, Singh R, Jhala D, Singh S, Vasita R. Antioxidative study of cerium oxide nanoparticle functionalised PCL-Gelatin electrospun fibers for wound healing application. Bioact Mater. 2018;3:201–11.
Augustine R, Hasan A, Patan NK, Dalvi YB, Varghese R, Antony A, et al. Cerium oxide nanoparticle incorporated electrospun poly(3-hydroxybutyrate-co-3-hydroxyvalerate) membranes for diabetic wound healing applications. ACS Biomater Sci Eng. 2020;6:58–70. https://doi.org/10.1021/acsbiomaterials.8b01352.
Kalantari K, Mostafavi E, Saleh B, Soltantabar P, Webster TJ. Chitosan/PVA hydrogels incorporated with green synthesized cerium oxide nanoparticles for wound healing applications. Eur Polym J. 2020;134:109853.
Shanmugam DK, Madhavan Y, Manimaran A, Kaliaraj GS, Mohanraj KG, Kandhasamy N, et al. Efficacy of graphene-based nanocomposite gels as a promising wound healing biomaterial. Gels. 2023;9:22.
Shariati A, Hosseini SM, Chegini Z, Seifalian A, Arabestani MR. Graphene-based materials for inhibition of wound infection and accelerating wound healing. Biomed Pharmacother. 2023. https://doi.org/10.1016/j.biopha.2022.114184.
Waris A, Din M, Ali A, Ali M, Afridi S, Baset A, et al. A comprehensive review of green synthesis of copper oxide nanoparticles and their diverse biomedical applications. Inorg Chem Commun. 2021;123:108369.
Sukumar S, Rudrasenan A, Padmanabhan ND. Green-synthesized rice-shaped copper oxide nanoparticles using caesalpinia bonducella seed extract and their applications. ACS Omega. 2020;5:1040–51.
Awwad AMA. Green synthesis of zinc oxide nanoparticles (ZnO-NPs) using Ailanthus altissima fruit extracts and antibacterial activity. Chem Int. 2020;6:151–9.
Faisal S, Jan H, Shah SA, Shah S, Khan A, Akbar MT, et al. Green synthesis of zinc oxide (ZnO) nanoparticles using aqueous fruit extracts of myristica fragrans: their characterizations and biological and environmental applications. ACS Omega. 2021;6:9709–22. https://doi.org/10.1021/acsomega.1c00310.
Pillai AM, Sivasankarapillai VS, Rahdar A, Sadeghfar F, Rajesh K, Kyzas GZ, et al. Green synthesis and characterization of zinc oxide nanoparticles with antibacterial and antifungal activity. J Mol Struct. 2020;1211:128107.
Clarance P, Luvankar B, Sales J, Khusro A, Agastian P, Tack JC, et al. Green synthesis and characterization of gold nanoparticles using endophytic fungi Fusarium solani and its in-vitro anticancer and biomedical applications. Saudi J Biol Sci. 2020;27:706–12.
Biao L, Tan S, Meng Q, Gao J, Zhang X, Liu Z, et al. Green synthesis, characterization and application of proanthocyanidins-functionalized gold nanoparticles. Nanomaterials. 2018;8:53.
Sunderam V, Thiyagarajan D, Lawrence AV, Mohammed SSS, Selvaraj A. In-vitro antimicrobial and anticancer properties of green synthesized gold nanoparticles using Anacardium occidentale leaves extract. Saudi J Biol Sci. 2019;26:455–9.
Alagesan V, Venugopal S. Green synthesis of selenium nanoparticle using leaves extract of withania somnifera and its biological applications and photocatalytic activities. Bionanoscience. 2019;9:105–16.
Veisi H, Pirhayati M, Kakanejadifard A, Mohammadi P, Abdi MR, Gholami J, et al. In Situ green synthesis of pd nanoparticles on tannic acid-modified magnetite nanoparticles as a green reductant and stabilizer agent: its application as a recyclable nanocatalyst (Fe3O4@TA/Pd) for reduction of 4-nitrophenol and suzuki reactions. ChemistrySelect. 2018;3:1820–6.
Kora AJ, Rastogi L. Green synthesis of palladium nanoparticles using gum ghatti (Anogeissus latifolia) and its application as an antioxidant and catalyst. Arab J Chem. 2018;11:1097–106.
Sathishkumar G, Logeshwaran V, Sarathbabu S, Jha PK, Jeyaraj M, Rajkuberan C, et al. Green synthesis of magnetic Fe3O4 nanoparticles using Couroupita guianensis Aubl. fruit extract for their antibacterial and cytotoxicity activities. Artif Cells Nanomed Biotechnol. 2018;46:589–98.
Subhapriya S, Gomathipriya P. Green synthesis of titanium dioxide (TiO2) nanoparticles by Trigonella foenum-graecum extract and its antimicrobial properties. Microb Pathog. 2018;116:215–20.
Kombaiah K, Vijaya JJ, Kennedy LJ, Bououdina M, Ramalingam RJ, Al-Lohedan HA. Okra extract-assisted green synthesis of CoFe2O4 nanoparticles and their optical, magnetic, and antimicrobial properties. Mater Chem Phys. 2018;204:410–9.
Cleetus CM, Primo FA, Fregoso G, Raveendran NL, Noveron JC, Spencer CT, et al. Alginate hydrogels with embedded zno nanoparticles for wound healing therapy. Int J Nanomed. 2020;15:5097–111.
Bhattacharya D, Ghosh B, Mukhopadhyay M. Development of nanotechnology for advancement and application in wound healing: a review. IET Nanobiotechnol. 2019;13:778–85.
Han B, Fang WH, Zhao S, Yang Z, Hoang BX. Zinc sulfide nanoparticles improve skin regeneration. Nanomedicine. 2020;29:102263.
Metwally A, Abdel-Hady A-N, Ebnalwaled K, Morad S, Soliman A. Wound-healing activity of green and chemical zinc oxide nanoparticles (ZnO-NPs) gels in equine wounds: a clinical study. SVU-Int J Vet Sci. 2020;3:66–79.
Paladini F, Pollini M. Antimicrobial silver nanoparticles for wound healing application: progress and future trends. Materials. 2019;12:2540.
Rigo C, Ferroni L, Tocco I, Roman M, Munivrana I, Gardin C, et al. Active silver nanoparticles for wound healing. Int J Mol Sci. 2013;14:4817–40.
Wang Y, Beekman J, Hew J, Jackson S, Issler-Fisher AC, Parungao R, et al. Burn injury: challenges and advances in burn wound healing, infection, pain and scarring. Adv Drug Deliv Rev. 2018;123:3–17.
Pirtarighat S, Ghannadnia M, Baghshahi S. Green synthesis of silver nanoparticles using the plant extract of Salvia spinosa grown in vitro and their antibacterial activity assessment. J Nanostructure Chem. 2019;9:1–9. https://doi.org/10.1007/s40097-018-0291-4.
Surapaneni SK, Bashir S, Tikoo K. Gold nanoparticles-induced cytotoxicity in triple negative breast cancer involves different epigenetic alterations depending upon the surface charge. Sci Rep. 2018;8:1–12.
Arafa MG, El-Kased RF, Elmazar MM. Thermoresponsive gels containing gold nanoparticles as smart antibacterial and wound healing agents. Sci Rep. 2018;8:1–16. https://doi.org/10.1038/s41598-018-31895-4.
Ko WC, Wang SJ, Hsiao CY, Hung CT, Hsu YJ, Chang DC, et al. Pharmacological role of functionalized gold nanoparticles in disease applications. Molecules. 2022;27:1–12.
Mahmoud NN, Hikmat S, Abu Ghith D, Hajeer M, Hamadneh L, Qattan D, et al. Gold nanoparticles loaded into polymeric hydrogel for wound healing in rats: effect of nanoparticles’ shape and surface modification. Int J Pharm. 2019;565:174–86.
Shalaby MA, Anwar MM, Saeed H. Nanomaterials for application in wound healing: current state-of-the-art and future perspectives. J Polym Res. 2022. https://doi.org/10.1007/s10965-021-02870-x.
Salvo J, Sandoval C. Role of copper nanoparticles in wound healing for chronic wounds: literature review. Burns Trauma. 2022;10:047.
Ghosal K, Agatemor C, Špitálsky Z, Thomas S, Kny E. Electrospinning tissue engineering and wound dressing scaffolds from polymer-titanium dioxide nanocomposites. Chem Eng J. 2019;358:1262–78.
Zhang Y, Zhang C, Liu K, Zhu X, Liu F, Ge X. Biologically synthesized titanium oxide nanostructures combined with morphogenetic protein as wound healing agent in the femoral fracture after surgery. J Photochem Photobiol B. 2018;182:35–41.
Nosrati H, Heydari M, Khodaei M. Cerium oxide nanoparticles: synthesis methods and applications in wound healing. Mater Today Bio. 2023;23:100823.
Chigurupati S, Mughal MR, Okun E, Das S, Kumar A, McCaffery M, et al. Effects of cerium oxide nanoparticles on the growth of keratinocytes, fibroblasts and vascular endothelial cells in cutaneous wound healing. Biomaterials. 2013;34:2194–201.
Allu I, Kumar Sahi A, Kumari P, Sakhile K, Sionkowska A, Gundu S. A brief review on cerium oxide (CeO2NPs)-based scaffolds: recent advances in wound healing applications. Micromachines. 2023.
Chen Y-H, Rao Z-F, Liu Y-J, Liu X-S, Liu Y-F, Xu L-J, et al. Multifunctional injectable hydrogel loaded with cerium-containing bioactive glass nanoparticles for diabetic wound healing. Biomolecules. 2021.
Zhao Y, Jalili S. Dextran, as a biological macromolecule for the development of bioactive wound dressing materials: a review of recent progress and future perspectives. Int J Biol Macromol. 2022;207:666–82.
Sharaf SS, El-Shafei AM, Refaie R, Gibriel AA, Abdel-Sattar R. Antibacterial and wound healing properties of cellulose acetate electrospun nanofibers loaded with bioactive glass nanoparticles; in-vivo study. Cellulose. 2022;29:4565–77. https://doi.org/10.1007/s10570-022-04570-1.
Mehrabi T, Mesgar AS, Mohammadi Z. Bioactive glasses: a promising therapeutic ion release strategy for enhancing wound healing. ACS Biomater Sci Eng. 2020;6:5399–430. https://doi.org/10.1021/acsbiomaterials.0c00528.
Patil TV, Patel DK, Dutta SD, Ganguly K, Randhawa A, Lim K-T. Carbon nanotubes-based hydrogels for bacterial eradiation and wound-healing applications. Appl Sci. 2021;11:9550.
Shariati A, Hosseini SM, Chegini Z, Seifalian A, Arabestani MR. Graphene-based materials for inhibition of wound infection and accelerating wound healing. Biomed Pharmacother. 2023;158:114184.
Li J, Zeng H, Zeng Z, Zeng Y, Xie T. Promising graphene-based nanomaterials and their biomedical applications and potential risks: a comprehensive review. ACS Biomater Sci Eng. 2021;7:5363–96. https://doi.org/10.1021/acsbiomaterials.1c00875.
Yagi S, Nakanishi H, Matsubara E, Matsubara S, Ichitsubo T, Hosoya K, et al. Formation of Cu nanoparticles by electroless deposition using aqueous CuO suspension. J Electrochem Soc. 2008;155:D474. https://doi.org/10.1149/1.2904884.
Hu YC, Dai CL, Hsu CC. Titanium dioxide nanoparticle humidity microsensors integrated with circuitry on-a-chip. Sensors. 2014;14:4177–88.
Izu N, Matsubara I, Itoh T, Akamatsu T, Shin W. CO responses of sensors based on cerium oxide thick films prepared from clustered spherical nanoparticles. Sensors. 2013;13:3252–61.
Mahalakshmi S, Hema N, Vijaya PP. In Vitro biocompatibility and antimicrobial activities of zinc oxide nanoparticles (ZnO NPs) prepared by chemical and green synthetic route—a comparative study. Bionanoscience. 2020;10:112–21.
Rajasekar T, Karthika K, Muralitharan G, Maryshamya A, Sabarika S, Anbarasu S, et al. Green synthesis of gold nanoparticles using extracellular metabolites of fish gut microbes and their antimicrobial properties. Braz J Microbiol. 2020;51:957–67.
Goudarzi M, Mir N, Mousavi-Kamazani M, Bagheri S, Salavati-Niasari M. Biosynthesis and characterization of silver nanoparticles prepared from two novel natural precursors by facile thermal decomposition methods. Sci Rep. 2016;6:1–13. https://doi.org/10.1038/srep32539.
Jeckson TA, Neo YP, Sisinthy SP, Gorain B. Delivery of therapeutics from layer-by-layer electrospun nanofiber matrix for wound healing. 2020.
Liang J, Cui L, Li J, Guan S, Zhang K, Li J. Aloe vera: a medicinal plant used in skin wound healing. Tissue Eng Part B Rev. 2021;27:455–74.
Dong Y, Zheng Y, Zhang K, Yao Y, Wang L, Li X, et al. Electrospun nanofibrous materials for wound healing. Adv Fiber Mater. 2020;2:212–27.
Alven S, Nqoro X, Aderibigbe BA. Polymer-based materials loaded with curcumin for wound healing applications. Polymers. 2020;12:1–25.
Mogoşanu GD, Grumezescu AM. Natural and synthetic polymers for wounds and burns dressing. Int J Pharm. 2014;463:127–36.
Juncos Bombin AD, Dunne NJ, McCarthy HO. Electrospinning of natural polymers for the production of nanofibres for wound healing applications. Mater Sci Eng C. 2020;114:110994.
Pii C, Miguel P, Moreira F, Correia J. Chitosan based-asymmetric membranes for wound healing: a review Sónia. Int J Biol Macromol. 2019;127:160.
Simões D, Miguel SP, Ribeiro MP, Coutinho P, Mendonça AG, Correia IJ. Recent advances on antimicrobial wound dressing: a review. Eur J Pharm Biopharm. 2018;127:130–41.
Ali Khan Z, Jamil S, Akhtar A, Mustehsan Bashir M, Yar M. Chitosan based hybrid materials used for wound healing applications—a short review. Int J Polym Mater Polym Biomater. 2020;69:419–36.
Venkataprasanna KS, Prakash J, Mathapati SS, Bharath G, Banat F, Venkatasubbu GD. Development of chitosan/poly (vinyl alcohol)/graphene oxide loaded with vanadium doped titanium dioxide patch for visible light driven antibacterial activity and accelerated wound healing application. Int J Biol Macromol. 2021;193:1430–48.
Nosrati H, Heydari M, Tootiaei Z, Ganjbar S, Khodaei M. Delivery of antibacterial agents for wound healing applications using polysaccharide-based scaffolds. J Drug Deliv Sci Technol. 2023;84:104516.
Ali Khan Z, Jamil S, Akhtar A, Mustehsan Bashir M, Yar M. Chitosan based hybrid materials used for wound healing applications—a short review. Int J Polym Mater Polym Biomater. 2020;69:419–36. https://doi.org/10.1080/00914037.2019.1575828.
Alturki AM. Rationally design of electrospun polysaccharides polymeric nanofiber webs by various tools for biomedical applications. Int J Biol Macromol. 2018;184:648.
Tudoroiu EE, Dinu-Pîrvu CE, Kaya MGA, Popa L, Anuța V, Prisada RM, et al. An overview of cellulose derivatives-based dressings for wound-healing management. Pharmaceuticals. 2021;14:1215.
Gobi R, Ravichandiran P, Babu RS, Yoo DJ. Biopolymer and synthetic polymer-based nanocomposites in wound dressing applications: a review. Polymers. 2021;13:1962.
Kamoun EA, Lout SA, Hussein Y, Kenawy ES. Recent advances in PVA-polysaccharide based hydrogels and electrospun nanofibers in biomedical applications: a review. Int J Biol Macromol. 2021;187:755–68.
Mulholland EJ. Electrospun biomaterials in the treatment and prevention of scars in skin wound healing. Front Bioeng Biotechnol. 2020;8:1–15.
Yang Y, Du Y, Zhang J, Zhang H, Guo B. Structural and functional design of electrospun nanofibers for hemostasis and wound healing. Adv Fiber Mater. 2022. https://doi.org/10.1007/s42765-022-00178-z.
Vedhanayagam M, Nair BU, Sreeram KJ. Dimension effect: dendrimer functionalized carbon based nanomaterial mediated collagen scaffold for wound healing application. Materialia. 2019;7:100354.
Nosrati H, Khodaei M, Alizadeh Z, Banitalebi-Dehkordi M. Cationic, anionic and neutral polysaccharides for skin tissue engineering and wound healing applications. Int J Biol Macromol. 2021;192:298–322.
Yeung DA, Kelly NH. The role of collagen-based biomaterials in chronic wound healing and sports medicine applications. Bioengineering. 2021. https://doi.org/10.3390/bioengineering8010008.
Laffleur F, Strasdat B. Gelatin-based formulations for dermal application. Eur Polym J. 2019;118:542–50.
Sharma A, Mittal A, Puri V, Kumar P, Singh I. Curcumin-loaded, alginate–gelatin composite fibers for wound healing applications. Biotech. 2020;10:464. https://doi.org/10.1007/s13205-020-02453-5.
Salehi M, Niyakan M, Ehterami A, Haghi-Daredeh S, Nazarnezhad S, Abbaszadeh-Goudarzi G, et al. Porous electrospun poly(ε-caprolactone)/gelatin nanofibrous mat containing cinnamon for wound healing application: in vitro and in vivo study. Biomed Eng Lett. 2020;10:149–61. https://doi.org/10.1007/s13534-019-00138-4.
Zheng C, Liu C, Chen H, Wang N, Liu X, Sun G, et al. Effective wound dressing based on Poly (vinyl alcohol)/Dextran-aldehyde composite hydrogel. Int J Biol Macromol. 2019;132:1098–105.
Jin M, Shi J, Zhu W, Yao H, Wang DA. Polysaccharide-based biomaterials in tissue engineering: a review. Tissue Eng Part B Rev. 2021;27:604–26.
Andrabi SM, Majumder S, Gupta KC, Kumar A. Dextran based amphiphilic nano-hybrid hydrogel system incorporated with curcumin and cerium oxide nanoparticles for wound healing. Colloids Surf B Biointerfaces. 2020;195:111263.
Mahmood H, Khan IU, Asif M, Khan RU, Asghar S, Khalid I, et al. In vitro and in vivo evaluation of gellan gum hydrogel films: Assessing the co impact of therapeutic oils and ofloxacin on wound healing. Int J Biol Macromol. 2021;166:483–95.
Chen X, Li H, Qiao X, Jiang T, Fu X, He Y, et al. Agarose oligosaccharide- silver nanoparticle- antimicrobial peptide- composite for wound dressing. Carbohydr Polym. 2021;269:118258.
Zarrintaj P, Manouchehri S, Ahmadi Z, Saeb MR, Urbanska AM, Kaplan DL, et al. Agarose-based biomaterials for tissue engineering. Carbohydr Polym. 2018;187:66–84.
Mir M, Ali MN, Barakullah A, Gulzar A, Arshad M, Fatima S, et al. Synthetic polymeric biomaterials for wound healing: a review. Prog Biomater. 2018;7:1–21. https://doi.org/10.1007/s40204-018-0083-4.
Rafiuddin A, Cuauhtemoc J, Gaytan T, Mohnot R, Sisodia GS, Ahmed G. Growth evaluation of fintech connectedness with innovative thematic indices—an evidence through wavelet analysis. J Open Innov. 2023. https://doi.org/10.1016/j.joitmc.2023.100023.
Patel Z, Gharat S, Al-tabakha MM, Ashames A. Recent advancements in electrospun nano fibers for wound healing: polymers. Clin Regulatory Perspect. 2022;39:83–118.
Shahgordi S, Sankian M, Yazdani Y, Mashayekhi K, Hasan Ayati S, Sadeghi M, et al. Immune responses modulation by curcumin and allergen encapsulated into PLGA nanoparticles in mice model of rhinitis allergic through sublingual immunotherapy. Int Immunopharmacol. 2020;84:1–9.
Mohanty C, Sahoo SK. Curcumin and its topical formulations for wound healing applications. Drug Discov Today. 2017;22:1582–92.
Aderibigbe AB, Alven S. Fabrication of hybrid nanofibers from biopolymers and poly (vinyl alcohol)/poly (ε-caprolactone) for wound dressing applications. Polymers. 2021. https://doi.org/10.3390/polym13132104.
Bianchera A, Catanzano O, Boateng J, Elviri L. The place of biomaterials in wound healing. 2020.
Farzaei MH, Derayat P, Pourmanouchehri Z, Kahrarian M, Samimi Z, Hajialyani M, et al. Characterization and evaluation of antibacterial and wound healing activity of naringenin-loaded polyethylene glycol/polycaprolactone electrospun nanofibers. J Drug Deliv Sci Technol. 2023;81:104182.
Khoshnevisan K, Maleki H, Samadian H, Doostan M, Khorramizadeh MR. Antibacterial and antioxidant assessment of cellulose acetate/polycaprolactone nanofibrous mats impregnated with propolis. Int J Biol Macromol. 2019;140:1260–8.
Guidi AC, de Paula MN, Mosela M, Delanora LA, Soares GCA, de Morais GR, et al. Stem bark extract of Poincianella pluviosa incorporated in polymer film: evaluation of wound healing and anti-staphylococcal activities. Injury. 2020;51:840–9.
Zabidi NA, Nazri F, Syafinaz I, Amin M, Salahuddin M, Basri M, et al. Tannic acid-reinforced methacrylated chitosan/methacrylated silk fibroin hydrogels with multifunctionality for accelerating wound healing. Int J Biol Macromol. 2022;2:33–47. https://doi.org/10.1016/j.ijbiomac.2022.05.116.
Karaly AH, Sarhan WA, El-Sherbiny IM. Development of a silk fibroin-based multitask aerosolized nanopowder formula for efficient wound healing. Int J Biol Macromol. 2021;182:413–24.
Bialik-Wąs K, Pluta K, Malina D, Majka TM. Alginate/PVA-based hydrogel matrices with Echinacea purpurea extract as a new approach to dermal wound healing. Int J Polym Mater Polym Biomater. 2021;70:195–206.
Chanda A, Adhikari J, Ghosh A, Chowdhury SR, Thomas S, Datta P, et al. Electrospun chitosan/polycaprolactone-hyaluronic acid bilayered scaffold for potential wound healing applications. Int J Biol Macromol. 2018;116:774–85.
Razack SA, Lee Y, Shin H, Duraiarasan S, Chun B-S, Kang HW. Cellulose nanofibrils reinforced chitosan-gelatin based hydrogel loaded with nanoemulsion of oregano essential oil for diabetic wound healing assisted by low level laser therapy. Int J Biol Macromol. 2023;226:220–39.
Bektas N, Şenel B, Yenilmez E, Özatik O, Arslan R. Evaluation of wound healing effect of chitosan-based gel formulation containing vitexin. Saudi Pharm J. 2020;28:87–94.
Yuan N, Shao K, Huang S, Chen C. Chitosan, alginate, hyaluronic acid and other novel multifunctional hydrogel dressings for wound healing: a review. Int J Biol Macromol. 2023;240:124321.
Thomas N, Rusdin A, Tulsyahra M, Wathoni N, Kuswandi A. Accelerated wound healing ability of Jatropha sap by iota carrageenan-poly (vinyl alcohol) hydrogel film. J Adv Pharm Technol Res. 2020;11:226–32.
Safaee-Ardakani MR, Hatamian-Zarmi A, Sadat SM, Mokhtari-Hosseini ZB, Ebrahimi-Hosseinzadeh B, Rashidiani J, et al. Electrospun Schizophyllan/polyvinyl alcohol blend nanofibrous scaffold as potential wound healing. Int J Biol Macromol. 2019;127:27–38.
Zakerikhoob M, Abbasi S, Yousefi G, Mokhtari M, Noorbakhsh MS. Curcumin-incorporated crosslinked sodium alginate-g-poly (N-isopropyl acrylamide) thermo-responsive hydrogel as an in-situ forming injectable dressing for wound healing: In vitro characterization and in vivo evaluation. Carbohydr Polym. 2021;271:118434.
Naghshineh N, Tahvildari K, Nozari M. Preparation of chitosan, sodium alginate, gelatin and collagen biodegradable sponge composites and their application in wound healing and curcumin delivery. J Polym Environ. 2019;27:2819–30.
Rathinavel S, Sugumar M, Swaminathan E, Kubendren S, Samvasivan K, Sangeetha D. Development of electrospun Plectranthus amboinicus loaded PCL polymeric nanofibrous scaffold for skin wound healing application: in-vitro and in-silico analysis. J Polym Res. 2023. https://doi.org/10.1007/s10965-023-03474-3.
Kharat Z, Amiri Goushki M, Sarvian N, Asad S, Dehghan MM, Kabiri M. Chitosan/PEO nanofibers containing Calendula officinalis extract: preparation, characterization, in vitro and in vivo evaluation for wound healing applications. Int J Pharm. 2021;609:121132.
Kazemi MH, Sajadimajd S, Gorgin KZ. In vitro investigation of wound healing performance of PVA/chitosan/silk electrospun mat loaded with deferoxamine and ciprofloxacin. Int J Biol Macromol. 2023;253:126602.
Zahra D, Shokat Z, Ahmad A, Javaid A, Khurshid M, Ashfaq UA, et al. Exploring the recent developments of alginate silk fibroin material for hydrogel wound dressing: a review. Int J Biol Macromol. 2023;248:125989.
Yu R, Zhang H, Guo B. Conductive biomaterials as bioactive wound dressing for wound healing and skin tissue engineering. Nanomicro Lett. 2022. https://doi.org/10.1007/s40820-021-00751-y.
Raina N, Pahwa R, Khosla JK, Gupta PN, Gupta M. Polycaprolactone-based materials in wound healing applications. Polym Bull. 2022;79:7041–63. https://doi.org/10.1007/s00289-021-03865-w.
Xu R, Fang Y, Zhang Z, Cao Y, Yan Y, Gan L, et al. Recent advances in biodegradable and biocompatible synthetic polymers used in skin wound healing. Materials. 2023;16:1–21.
Stern D, Cui H. Crafting polymeric and peptidic hydrogels for improved wound healing. Adv Healthc Mater. 2019;8:1–17.
Rezvani Ghomi E, Khalili S, Nouri Khorasani S, Esmaeely Neisiany R, Ramakrishna S. Wound dressings: current advances and future directions. J Appl Polym Sci. 2019;136:1–12.
Homaeigohar S, Boccaccini AR. Antibacterial biohybrid nano fibers for wound dressings. Acta Biomater. 2021;107:25–49.
Jadhav K, Deore S, Dhamecha D, Hr R, Jagwani S, Jalalpure S, et al. Phytosynthesis of silver nanoparticles: characterization, biocompatibility studies, and anticancer activity. ACS Biomater Sci Eng. 2018;4:892–9.
Ovais M, Ahmad I, Khalil AT, Mukherjee S, Javed R, Ayaz M, et al. Wound healing applications of biogenic colloidal silver and gold nanoparticles: recent trends and future prospects. Appl Microbiol Biotechnol. 2018;102:4305–18.
Abd El-Hack ME, El-Saadony MT, Shafi ME, Zabermawi NM, Arif M, Batiha GE, et al. Antimicrobial and antioxidant properties of chitosan and its derivatives and their applications: a review. Int J Biol Macromol. 2020;164:2726–44.
Tinpun K, Nakpheng T, Padmavathi AR, Srichana T. In vitro studies of jatropha curcas l. Latex spray formulation for wound healing applications. Turk J Pharm Sci. 2020;17:271–9.
Criollo-Mendoza MS, Contreras-Angulo LA, Leyva-López N, Gutiérrez-Grijalva EP, Jiménez-Ortega LA, Heredia JB. Wound healing properties of natural products: mechanisms of action. Molecules. 2023;28:1–18.
Jaldin-Crespo L, Silva N, Martínez J. Nanomaterials based on honey and propolis for wound healing—a mini-review. Nanomaterials. 2022;12:1–23.
Ranjith R, Balraj S, Ganesh J, John Milton MC. Therapeutic agents loaded chitosan-based nanofibrous mats as potential wound dressings: a review. Mater Today Chem. 2019;12:386–95.
Kouhkan M, Ahangar P, Babaganjeh LA, Allahyari-Devin M. Biosynthesis of copper oxide nanoparticles using Lactobacillus casei Subsp. Casei and its anticancer and antibacterial activities. Curr Nanosci. 2019;16:101–11.
Haider MK, Ullah A, Sarwar MN, Saito Y, Sun L, Park S, et al. Lignin-mediated in-situ synthesis of CuO nanoparticles on cellulose nanofibers: a potential wound dressing material. Int J Biol Macromol. 2021;173:315–26.
Cai Y, Yang F, Wu L, Shu Y, Qu G, Fakhri A, et al. Hydrothermal-ultrasonic synthesis of CuO nanorods and CuWO4 nanoparticles for catalytic reduction, photocatalysis activity, and antibacterial properties. Mater Chem Phys. 2021;258:123919.
Gheidari D, Mehrdad M, Maleki S, Hosseini S. Synthesis and potent antimicrobial activity of CoFe2O4 nanoparticles under visible light. Heliyon. 2020. https://doi.org/10.1016/j.heliyon.2020.e05058.
Bhosale SV, Ekambe PS, Bhoraskar SV, Mathe VL. Effect of surface properties of NiFe 2 O 4 nanoparticles synthesized by dc thermal plasma route on antimicrobial activity. Appl Surf Sci. 2018;441:724–33.
Shubharani R, Mahesh M, Yogananda MV. Biosynthesis and characterization, antioxidant and antimicrobial activities of selenium nanoparticles from ethanol extract of bee propolis. J Nanomed Nanotechnol. 2019;10:1–7.
Ismail NA, Amin KAM, Majid FAA, Razali MH. Gellan gum incorporating titanium dioxide nanoparticles biofilm as wound dressing: physicochemical, mechanical, antibacterial properties and wound healing studies. Mater Sci Eng C. 2019;103:109770.
Razali MH, Ismail NA, Mat Amin KA. Titanium dioxide nanotubes incorporated gellan gum bio-nanocomposite film for wound healing: effect of TiO2 nanotubes concentration. Int J Biol Macromol. 2020;153:1117–35.
Roy A, Gauri SS, Bhattacharya M, Bhattacharya J. Antimicrobial activity of CaO nanoparticles. J Biomed Nanotechnol. 2013;9:1570–8.
Krishnamoorthy K, Manivannan G, Kim SJ, Jeyasubramanian K, Premanathan M. Antibacterial activity of MgO nanoparticles based on lipid peroxidation by oxygen vacancy. J Nanoparticle Res. 2012. https://doi.org/10.1007/s11051-012-1063-6.
Nguyen N-YT, Grelling N, Wetteland CL, Rosario R, Liu H. Antimicrobial activities and mechanisms of magnesium oxide nanoparticles (nMgO) against pathogenic bacteria, yeasts, and biofilms. Sci Rep. 2018;8:16260. https://doi.org/10.1038/s41598-018-34567-5.
Xinglong Yang, Junchuan Yang, Le Wang, Bei Ran, Yuexiao Jia, Lingmin Zhang, Guang Yang, Huawu Shao and XJ. Pharmaceutical Intermediate-Modified Gold Nanoparticles: Against Multidrug- Resistant Bacteria and Wound-Healing Application via Electrospun Scaffold. ACS Nano. 2017.
Hamelian M, Hemmati S, Varmira K, Veisi H. Green synthesis, antibacterial, antioxidant and cytotoxic effect of gold nanoparticles using Pistacia Atlantica extract. J Taiwan Inst Chem Eng. 2018;93:21–30.
Harandi FN, Khorasani AC, Shojaosadati SA, Hashemi-Najafabadi S. Surface modification of electrospun wound dressing material by Fe2O3 nanoparticles incorporating Lactobacillus strains for enhanced antimicrobial and antibiofilm activity. Surf Interfaces. 2022;28:101592.
Liu Z, Zhao X, Yu B, Zhao N, Zhang C, Xu F-J. Rough carbon-iron oxide nanohybrids for near-infrared-II light-responsive synergistic antibacterial therapy. ACS Nano. 2021;15:7482–90. https://doi.org/10.1021/acsnano.1c00894.
Rumora L, Hlapčić I, Hulina-Tomašković A, Somborac-Bačura A, Bosnar M, Rajković MG. Pathogen-associated molecular patterns and extracellular Hsp70 interplay in NLRP3 inflammasome activation in monocytic and bronchial epithelial cellular models of COPD exacerbations. APMIS. 2021;129:80–90.
Chiaki M, Tsukasa S, Tai-Ying C, Yukari N, Yasuki H, Shin-ichi Y, et al. Role of lipoteichoic acid from the genus apilactobacillus in inducing a strong IgA response. Appl Environ Microbiol. 2022;88:e00190-e222. https://doi.org/10.1128/aem.00190-22.
Hillman PF, Lee C, Nam SJ. Microbial natural products with wound-healing properties. Processes. 2023; 11.
Cui C, Sun S, Wu S, Chen S, Ma J, Zhou F. Electrospun chitosan nanofibers for wound healing application. Eng Regen. 2021;2:82–90.
Ali-Seyed M, Ayesha S. Calotropis—a multi-potential plant to humankind: special focus on its wound healing efficacy. Biocatal Agric Biotechnol. 2020;28:101725.
Mattosinhos PS, Sarandy MM, Novaes RD, Esposito D, Gonçalves RV. Anti-inflammatory, antioxidant, and skin regenerative potential of secondary metabolites from plants of the brassicaceae family: a systematic review of in vitro and in vivo preclinical evidence (biological activities brassicaceae skin diseases). Antioxidants. 2022;11:1–17.
Subbiah R, Cheng A, Ruehle MA, Hettiaratchi MH, Bertassoni LE, Guldberg RE. Effects of controlled dual growth factor delivery on bone regeneration following composite bone-muscle injury. Acta Biomater. 2020;114:63.
Huang Z, Wang D, Sønderskov SM, Xia D, Wu X, Liang C, et al. Tannic acid-functionalized 3D porous nanofiber sponge for antibiotic-free wound healing with enhanced hemostasis, antibacterial, and antioxidant properties. J Nanobiotechnology. 2023;21:1–15. https://doi.org/10.1186/s12951-023-01922-2.
Veld RC, Joosten L, Van Den Boomen OI, Boerman OC, Kouwer P, Middelkoop E, et al. Monitoring In-labelled polyisocyanopeptide (PIC) hydrogel wound dressings in full-thickness wounds. Biomater Sci. 2019;7:3041–50.
Chandika P, Kim M, Khan F, Kim Y, Heo S, Oh G, et al. Wound healing properties of triple cross-linked poly (vinyl alcohol)/ methacrylate kappa-carrageenan/chitooligosaccharide hydrogel. Carbohydr Polym. 2021;269:118272.
Doan VK, Tran CM, Ho TTP, Nguyen LKK, Nguyen YN, Tang NT, et al. Optimization of oligomer chitosan/polyvinylpyrrolidone coating for enhancing antibacterial, hemostatic effects and biocompatibility of nanofibrous wound dressing. Polymers. 2022;14:1–18.
Kassem LM, El-Deen AG, Zaki AH, El-Dek SI. Electrospun manuka honey@PVP nanofibers enclosing chitosan-titanate for highly effective wound healing. Cellulose. 2023;30:6487–505. https://doi.org/10.1007/s10570-023-05267-9.
Bolla SR, Mohammed Al-Subaie A, Yousuf Al-Jindan R, Papayya Balakrishna J, Kanchi Ravi P, Veeraraghavan VP, et al. In vitro wound healing potency of methanolic leaf extract of Aristolochia saccata is possibly mediated by its stimulatory effect on collagen-1 expression. Heliyon. 2019;5:1–7.
Mohammad Shafie N, Raja Shahriman Shah RNI, Krishnan P, Abdul Haleem N, Tan TYC. Scoping review: evaluation of Moringa oleifera (Lam.) for potential wound healing in In Vivo studies. Molecules. 2022; https://doi.org/10.3390/molecules27175541
Gao C, Zhang L, Wang J, Jin M, Tang Q, Chen Z, et al. Electrospun nanofibers promote wound healing: theories, techniques, and perspectives. J Mater Chem B. 2021;9:3106–30.
Akhmetova A, Heinz A. Electrospinning proteins for wound healing purposes: opportunities and challenges. Pharmaceutics. 2021;13:1–22.
Nosrati H, Aramideh Khouy R, Nosrati A, Khodaei M, Banitalebi-Dehkordi M, Ashrafi-Dehkordi K, et al. Nanocomposite scaffolds for accelerating chronic wound healing by enhancing angiogenesis. J Nanobiotechnology. 2021;19:1. https://doi.org/10.1186/s12951-020-00755-7.
Gwarzo ID, Mohd Bohari SP, Abdul Wahab R, Zia A. Recent advances and future prospects in topical creams from medicinal plants to expedite wound healing: a review. Biotechnol Biotechnol Equip. 2022;36:81–93. https://doi.org/10.1080/13102818.2022.2053340.
El-Aassar MR, Ibrahim OM, Fouda MMG, El-Beheri NG, Agwa MM. Wound healing of nanofiber comprising polygalacturonic/hyaluronic acid embedded silver nanoparticles: in-vitro and in-vivo studies. Carbohydr Polym. 2020;238:116175.
Veith AP, Henderson K, Spencer A, Sligar AD, Baker AB. Therapeutic strategies for enhancing angiogenesis in wound healing. Adv Drug Deliv Rev. 2019;146:97–125.
Funding
The authors do not have any funding sources for the preparation of the review article.
Author information
Authors and Affiliations
Contributions
Suriyaprakash Rajadesingu; Conceptualization, Supervision. Naveen Palani; Writing- Original draft preparation. Monisha P; Visualization, Investigation. Saravanakumar Ayyadurai; Validation. Pradeshwaran Vijayakumar; Reviewing, Editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
I hereby give my consent for the publication of the manuscript.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Palani, N., Vijayakumar, P., Monisha, P. et al. Electrospun nanofibers synthesized from polymers incorporated with bioactive compounds for wound healing. J Nanobiotechnol 22, 211 (2024). https://doi.org/10.1186/s12951-024-02491-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12951-024-02491-8