Abstract
Background
In patients with hormone receptor-positive breast cancer, differentiating between patients with a low and a high risk of recurrence is an ongoing challenge. In current practice, prognostic clinical parameters are used for risk prediction. DNA methylation markers have been proven to be of additional prognostic value in several cancer types. Numerous prognostic DNA methylation markers for breast cancer have been published in the literature. However, to date, none of these markers are used in clinical practice.
Methods
We conducted a systematic review of PubMed and EMBASE to assess the number and level of evidence of published DNA methylation markers for hormone receptor-positive breast cancer. To obtain an overview of the reporting quality of the included studies, all were scored according to the REMARK criteria that were established as reporting guidelines for prognostic biomarker studies.
Results
A total of 74 studies were identified reporting on 87 different DNA methylation markers. Assessment of the REMARK criteria showed variation in reporting quality of the studies. Eighteen single markers and one marker panel were studied in multiple independent populations. Hypermethylation of the markers RASSF1, BRCA, PITX2, CDH1, RARB, PCDH10 and PGR, and the marker panel GSTP1, RASSF1 and RARB showed a statistically significant correlation with poor disease outcome that was confirmed in at least one other, independent study.
Conclusion
This systematic review provides an overview on published prognostic DNA methylation markers for hormone receptor-positive breast cancer and identifies eight markers that have been independently validated. Analysis of the reporting quality of included studies suggests that future research on this topic would benefit from standardised reporting guidelines.
Similar content being viewed by others
Introduction
In women, breast cancer is the most frequently diagnosed cancer worldwide, with an incidence of 1.7 million cases each year [1]. Most cases, 75–80%, are hormone receptor positive, meaning that tumour cells express the oestrogen receptor (ER) and/or the progesterone receptor (PR). Curatively treated breast cancer patients are at risk of recurrence of disease. This occurs in approximately 10% of patients with hormone receptor-positive breast cancer within 5 years and continues to be a risk with an annual rate of 1.4–2.2% over more than 20 years [2, 3]. Adjuvant systemic treatment diminishes the risk of recurrence, but can have adverse effects that negatively impact quality of life [4].
The risk of recurrence in current clinical practice is estimated by considering classical prognostic factors, using nomograms such as the UK-based PREDICT tool or New Adjuvant Online [5,6,7]. Despite the success of these risk prediction models to identify patients at high risk of recurrence based on clinical characteristics, prediction is on a population level and as a result leads to over- and undertreatment at a patient level [8]. Prognostic biomarkers may improve the risk assessment, making it possible to better distinguish patients with a high risk of recurrence who may benefit from additional treatment, from patients with a low risk of recurrence for whom additional treatment may be omitted [9]. This principle was recently demonstrated for both the Mammaprint and Oncotype DX biomarker assays by the MINDACT and TAILOR trials [10, 11].
Biomarker research has increasingly incorporated epigenetic processes, particularly DNA methylation. DNA methylation is the addition of a methyl group to the carbon 5-position of cytosine within a cytosine guanine (CpG) dinucleotide. As methylation is a common and early event in cancer, and DNA methylation patterns differ between breast cancer molecular subtypes [12, 13], alterations in the methylome form a potential class of biomarkers for early detection, prognosis and prediction to therapy [14,15,16].
At the moment, DNA methylation markers are not yet being used in the clinical setting of breast cancer, despite the fact that many studies focused on the potential prognostic role of these markers and many DNA methylation markers have been suggested to have prognostic value [17, 18]. Currently, an overview of these studies describing potential prognostic markers is lacking. In this systematic review, we provide a comprehensive overview of potential prognostic DNA methylation biomarkers for hormone-sensitive breast cancer. In addition, we comment on various methodological aspects of these biomarker studies, aiming to provide guidelines for optimising research into this subject.
Methods
Review format
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [19]. No review protocol was previously published.
Eligibility criteria and study selection
Eligible articles were original research reports in the English language that had investigated hypo- or hypermethylated biomarkers in relation to patient survival or surrogate endpoints such as disease-free survival in breast cancer populations with oestrogen and/or progesterone receptor-positive breast cancer cases. We excluded in vitro studies, studies on non-human material, studies that focused on hereditary breast cancer cases, studies that focused on non-CpG DNA methylation and studies that had reported large amounts of data from biomarker arrays without further specification of the data to a single potential biomarker or biomarker panel.
Search strategy
PubMed and EMBASE were searched up to November 2018 for eligible studies using the following keywords and equivalents of these: ‘breast cancer’, ‘DNA based methylation biomarker’, ‘hormone receptor positive’ and ‘prognostic or predictive clinical outcome’ (see Additional file 1: Table S1 for a complete overview of the search terms).
Two reviewers (FH and TR) independently selected studies based on title, abstract and in selected cases full text. Disagreement was resolved by discussion between the reviewers until consensus was reached. References of selected studies were crosschecked for additional studies that were eligible for inclusion.
Data collection and extraction
The following data from all selected studies was collected independently by two reviewers (FH and TR): year of publication, study design, study population, length of follow-up, assay type and cut-off used, sequence of primer or probe, statistical methods used and reported association between marker and patient outcome were collected from all selected studies. When available, both univariate and multivariate outcome measures were collected. Study population information consisted of population size, country of patient selection, age, grade, hormone receptor status, HER2 status and stage according to the reported American Joint Committee on Cancer classification [20]. The level of evidence (LOE) was assessed for each publication according to criteria as defined by Hayes et al. [21] and the OCEBM Levels of Evidence Working Group [22].
For each publication, all study endpoints on outcome were collected and compared with ‘the proposed Standardized definitions for Efficacy EndPoints in adjuvant breast cancer trials’ (STEEP) [23]. Endpoints not defined in accordance to STEEP definitions were converted to STEEP-defined endpoints when sufficient information was provided. All defined biomarkers were checked for aliases in the NCBI Gene database and were reported by their current RefSeq gene names.
Analysis of reporting
All selected articles were scored according to the ‘REporting recommendations for tumour MARKer prognostic studies’ (REMARK) criteria [24, 25]. The REMARK checklist consists of 20 items containing one or multiple sub-items. A single item was scored with one point if all relevant sub-items were reported, half a point if only part of the information was reported or zero points if no information on this item was reported. The REMARK checklist is presented in Additional file 2: Table S2. Scoring was performed by two independent researchers (FH and TR). If the total score per article differed, the differences were discussed until agreement was achieved.
REMARK scores were used to assess the risk of potential selection, measurement and confounding bias. The risk for selection bias was assessed by REMARK item #2 (‘patient characteristics’) and #6 (‘sample selection and follow-up’). Studies obtaining < 1.5 points for these combined items were considered to have an increased risk. Measurement bias regarding the assay method was assessed using REMARK items #5 (‘assay method’) and #11 (‘handling of marker values’). REMARK item #7 (‘clinical endpoint definition’) was employed to assess the risk of measurement bias regarding outcome assessment; incomplete or lack of reporting of this item (score < 1) was considered at risk for measurement bias. Confounding bias was assessed using REMARK criterion #16 (‘multivariable analysis’), as in multivariate analysis (score = 1) potential confounding is taken into account. In order to investigate the effect of study design on marker significance, we compared REMARK scores between studies that found significant results and studies that did not find significant results using a Wilcoxon signed-rank test.
Forest plots
A forest plot was prepared for all methylation markers that were investigated in two or more study populations. When included studies reported results for more than one location per marker or reported results derived from more than one source of DNA, such as primary tumour tissue or blood serum, all reported results were represented in the forest plot. If available, multivariable hazard ratios (HRs), 95% confidence intervals (CI) and p values were used. When studies reported only p values without HRs, these were still included in the forest plot, in order to give a complete overview. The statistical programming language R (version 3.3.1) was used to perform all analyses and generate the figures.
Results
Search results
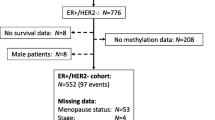
The search in the PubMed and EMBASE databases yielded a total of 788 potential publications. One hundred seventy-eight publications were removed as duplicates. After removal of 183 publications that either were not written in English or did not concern original research, 427 studies remained and were screened for eligibility based on title, abstract or full text. Three hundred seventy-two papers were excluded for not matching our inclusion and exclusion criteria. In addition to the remaining 55 papers, 17 papers were identified during reading and included in this review. This selection procedure resulted in 72 included papers [13, 20, 26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95]. A flowchart of this selection procedure is provided in Fig. 1.
Study characteristics
A summary of all studies, studied markers and study characteristics is provided in Additional file 3: Table S3. The number of included patients ranged between 34 and 1163, with a median study sample size of 119. Median or mean follow-up time per study ranged between 20 and 238 months. In 59 studies (82%), either fresh frozen or formalin-fixed paraffin-embedded primary tumour tissue from surgical resections was used for DNA extraction. Nine studies (13%) used plasma or serum derived from the blood and one study (1%) used serum derived from the bone marrow. Fine needle aspirates of the tumour were used in one study (1%). Two studies (3%) did not report the origin of the DNA samples. None of the studies reported selection of a specific tumour grade or stage. All but three papers studied hypermethylation as opposed to hypomethylation. Ten different techniques were applied to assess methylation status, of which methylation-specific PCR was used most frequently (n = 33, 46%) followed by quantitative methylation-specific PCR (n = 16, 22%).
We could categorise 55 papers as OCEBM level 4 and 19 studies OCEBM level 3. There were no level 1 or 2 studies.
Quality assessment
All included publications were scored for adherence to the REMARK criteria. Scores ranged from 4.5 to 19 out of the maximum 20 points; the median REMARK score was 12. Only four studies (6%) scored over 15 points.
Quality of reporting highly differed per REMARK item. Figure 2 depicts the number of papers that provided any information for each REMARK item and the number of papers that provided all information per item as required by the REMARK guidelines. For most items, information was provided by the authors, but often this information was incomplete. For example, all studies provided information on the study population, but in 72% of the papers, clear inclusion and exclusion criteria or key patient characteristics, needed to place study results into a clinical perspective, were lacking. The assay used to analyse DNA methylation was mentioned in all studies; however, only two studies (3%) provided all information required to reproduce the assay. Similarly, all studies provided information on statistical analysis, but information needed to reproduce the analyses such as handling of missing data and selection of variables was missing in over 95% of the included papers. Other items, such as patient treatment (65%), biological origin of samples (83%), handling of cut-off values (92%) and demographics of included patients (75%), were generally well reported. Correlations between markers and classical prognostic factors, as well as univariate outcome results were adequately provided by most authors. However, multivariable analyses adjusting for classical prognostic markers were performed in only 32% of included papers.
Comparison of REMARK scores between studies that produced significant results and studies that did not produce significant results showed that studies with low REMARK scores were less likely to report a statistically significant correlation between the investigated marker and disease outcome (p = 0.007). The risk of bias of each included study is summarised in Additional file 4: Table S4.
Prognostic marker findings
The 72 included studies reported on 87 different DNA methylation markers. Of these, 18 single markers were studied in more than one independent population. Forest plots summarising the results of these repeatedly studied markers are depicted in Fig. 3 and Additional file 5: Table S5. Hypermethylation of seven markers and one marker panel consisting of three markers was independently significantly associated with poor disease outcome [28, 32, 38,39,40,41, 48, 50, 52, 58, 61, 63, 66,67,68,69, 78, 79, 88, 92, 94]. Two markers were both significantly associated with poor and improved outcome in separate studies [54, 75, 78, 91]. Five markers showed a significant relation to poor outcome in one study, while other studies looking into the same marker found no correlation [44, 57, 58, 65, 83]. Finally, four markers showed no significant relation to disease outcome in any study [48, 63, 66, 68, 70, 88, 92, 95]. An overview of all markers studied in two or more independent populations is presented in Fig. 4. Of the 87 reported markers, 68 were only studied once in a single population. An overview of these markers is provided in Additional file 6: Figure S6 and Additional file 7: Table S7.
Forest plots of all methylation markers reported in two or more independent study populations. HRs with a statistically significant association are depicted with a solid line; HRs of reported markers with no significant association are depicted with a dotted line; univariate HRs (a) and confidence intervals (CI) are reported unless multivariate HRs (b) were available. Per marker, if results are derived from the same cohort, but with differing characteristics, such as differing DNA origin or location of methylation, this is represented by a coloured population bar. Per marker, if results originated from the same research group, this is indicated by an asterisk (*). Due to the vast number of individual results for these markers, for visualisation purposes, per marker, this figure shows one result per investigated population and tissue type. For a full representation of markers reported in two or more independent study populations, see Additional file 5: Table S5
Methylation markers studied in at least two independent populations, separated by relation to prognosis and achieved LOE. Underlined markers were analysed as hypomethylation markers. Italic markers do not correspond to Ref-Seq registered genes. Markers GSTP1 (*) and ESR (**) were both significantly correlated with good and poor prognosis in separate studies. The mentioned panel (***) is a multigene panel consisting of markers GSTP1, RASSF1 and RARB
Hypermethylation of the markers RASSF1, BRCA, PITX2, RARB, PGR, CDH1 and PCDH10, and the marker panel consisting of markers GSTP1, RASSF1 and RARB showed a statistically significant correlation with poor disease outcome. RASSF1 is the most extensively studied breast cancer methylation marker and was studied in 12 independent study populations [28, 32, 36, 40, 50, 52, 63, 68, 74, 79, 88, 92]. Eight studies found statistically significant results; all showed RASSF1 methylation to be associated with poor survival (HR ranging from 1.93 to 5.64). The remaining four studies found no statistically significant association. RASSF1 methylation was tested in DNA derived from primary surgical resections, blood serum, bone marrow-derived serum and in fine needle aspirates, and was capable of predicting outcome independently of DNA origin. Eleven independent studies investigated BRCA1 hypermethylation [20, 29, 42, 48, 55, 56, 76, 78, 79, 93, 94]. Statistically significant results, correlating hypermethylation of this gene with poor disease outcome, were found in four studies, both in DNA from surgical resections and in blood serum. PITX2 was studied in five independent studies, though it should be noted these studies were all performed by the same research group [40,41,42, 61, 69]. All but one study found a statistically significant association between PITX2 hypermethylation and poor outcome; this correlation seemed to be location specific and was found in primary surgical resections and blood serum but not in serum derived from the bone marrow [40]. Five studies reported on RARB hypermethylation in relation to breast cancer recurrence [50, 56, 67, 79, 88]. A statistically significant correlation was found in two studies and proved to be independent of studied tissue type. PGR was studied in five independent cohorts in four different studies [64, 66, 73, 79]. Two alternative promotor sites were analysed in these studies; for both alternative promotors, significant correlation to poor survival was found. Three studies reported on CDH1 methylation in relation to disease outcome [49, 50, 58]. Two studies identified a statistically significant correlation between CDH1 hypermethylation and poor disease outcome. PCDH10 was studied by two independent studies; both found PCDH10 hypermethylation significantly correlated with poor prognosis [32, 59]. A combined analysis of GSTP1, RASSF1 and RARB hypermethylation was the only gene panel analysed in two independent study populations [38, 39]. Fujita et al. studied this panel in blood serum derived from two independent study populations and found a strong correlation with poor overall survival in both cohorts.
For two methylation markers, significant correlations with both poor and improved disease outcome were reported. GSTP1 was analysed in four studies [27, 54, 78, 79]. Three studies found promoter methylation of this gene to be associated with poor survival in multivariable analysis. However, Klajic et al. found GSTP1 methylation to be strongly associated with better breast cancer-specific survival [54]. All four studies studied GSTP1 promoter methylation in primary tumour resections; Sharma et al. also investigated the relation between GSTP1 methylation detected in blood serum of breast cancer patients with the recurrence-free interval, but found no statistically significant correlation [78]. ESR1 was studied in eight independent cohorts; in six cohorts, no statistically significant correlation with disease outcome was found [56, 62, 66, 68, 75, 79, 91]. Widschwendter et al. analysed the impact of ESR1 in two patient cohorts in a univariate analysis, one consisting of patients treated with tamoxifen and one consisting of patients that had not received tamoxifen. In the non-treated cohort, no statistically significant correlation was found; however, in the tamoxifen-treated cohort, a borderline statistical significance with improved disease-free survival was shown (HR 0.7; 95% CI 0.5–1.0) [91]. Ramos et al. found a strong correlation of ESR1 hypermethylation and metastasis-free survival in a cohort of 67 patients; in this study, no details on treatment of the cohort were reported [75].
The markers CCND2, SFRP2, PTPRO, CDNK2A and LINE-1 showed all a correlation for methylation and patient outcome in one study, but these effects were not validated in other studies reporting on these markers [42, 44, 45, 48, 50, 54, 56, 57, 63, 65, 72, 79, 83, 87].
Hypermethylation of the markers SFN, APC, ID4 and CDH13 was analysed in two independent sub-populations, but did not show any statistically significant correlation with disease outcome [48, 63, 66, 68, 70, 88, 92, 95].
Discussion
In this systematic review, we provide an overview of prognostic DNA methylation markers for ER- and/or PR-positive breast cancer. We identified promoter hypermethylation of RASSF1, BRCA1, PITX2, CDH1, RARB, PCDH10 and PGR as well as the marker panel GSTP1, RASSF1 and RARB as possible markers of poor disease outcome. Four of these markers (RASSF1, PITX2, PCDH10 and the panel) were also shown to be of prognostic value independently of clinically relevant prognostic factors, suggesting that these markers may provide additional prognostic information. This may help to identify patients at increased risk of disease recurrence and to inform the choice of adjuvant therapy.
Although promising, current LOE for these markers is low, either level 3 or 4. Several explanations can be suggested for this low LOE. Most studies were performed retrospectively, which provides a lower LOE as compared to prospectively designed studies. To overcome this, biomarker research should preferably select patients from previously established prospective cohorts [96]. In addition, only 18 markers and one marker panel were tested in multiple patient populations, and studies that did investigate the same marker showed extensive heterogeneity in technical assays, study endpoints and patient selection. This heterogeneity impaired comparison between studies and the performance of meta-analyses, making it impossible to combine low LOE studies in order to reach a higher LOE.
Heterogeneity between individual studies was introduced by several factors. DNA methylation can be analysed using several different techniques. Studies included in this systematic review applied nine different assays for determining methylation status. Although it has been shown that varying techniques could lead to different results [97, 98], this is not always the case. In previous research, we have shown that the prognostic impact of a DNA methylation biomarker is not affected by the applied technique if the chosen technique is optimised correctly [99]. Optimisation depends on correctly chosen cut-off values, assay conditions, origin and quality of the used source DNA and the location in which methylation is analysed [99,100,101]. These factors all determine whether a sample is identified as methylated or unmethylated, directly influencing the sensitivity and specificity of the assay and should therefore be reported in great detail [24, 25]. In our review, almost none of the included studies sufficiently reported these factors, as is also illustrated by a median REMARK score of 12. Recent research has shown the 5-hydroxy-methylation is a separate entity in epigenetic DNA alterations; however, as most currently applied techniques are incapable of discerning DNA methylation from 5-hydroxy-methylation, we have considered this distinction outside the scope of this review.
Apart from the chosen assay characteristics, heterogeneity in study endpoints was seen for the included studies. Although 85% of all studies reported the used endpoint, these endpoints were frequently not clearly described. Due to the long median survival in early breast cancer patients, overall survival is generally not feasible as an endpoint. Therefore, surrogate endpoints relating to disease recurrence are often applied. Recurrence in breast cancer can have many forms, such as locoregional recurrence, distant recurrence or second primary disease. As different types of recurrence are related to different patient, tumour and treatment characteristics, a precise definition of surrogate endpoints is needed [23]. In addition, endpoint selection should be tailored to the envisioned purpose of the envisioned marker. For example, when a marker is studied with the goal of predicting the risk distant recurrence, distant recurrence-free survival or distant recurrence-free interval would include the most relevant events [23].
Differences in tumour and treatment characteristics between studies were an additional source of heterogeneity. The treatment patients received, the percentage of patients that had hormone receptor-positive breast cancer or amplification of the HER2 gene differed markedly. Moreover, these characteristics, though vital for interpretation of the results of the studies, were often reported incompletely. The treatment regimen was only specified in 65% of the included studies. When treatment was specified, it was often described as ‘according to local guidelines’, which can vary per region, but also per time period. In breast cancer, the status and prognostic effect of biomarkers may change due to a specific treatment and it should therefore be considered when interpreting study results [102]. The risk of breast cancer recurrence is directly correlated to the ER, PR and HER2 status [5,6,7]. A lack of a detailed description of the study population makes it difficult to perform a meta-analysis or to identify a clinical setting in which a marker may be of use [24, 25]. In addition, there was also a great variation in the covariates used in the multivariable analyses. In order to interpret the prognostic value of a marker, at least all currently used clinical prognostic factors, i.e. TNM classification, tumour grade, ER status, PR status and HER2 status, should be included [24, 25]. Many studies did not perform these analyses or omitted key covariates without explanation.
The studies summarised in this review show numerous promising DNA methylation biomarkers for hormone receptor-positive breast cancer. Unfortunately, a meta-analysis of these studies is not possible due to the differences between the included studies. Additional research is needed to establish the prognostic value of these markers in predicting distant recurrence when used in addition to existing tests. Future research should be designed to prevent selection and confounding bias and should report findings in adherence to the REMARK criteria. In addition, measurement bias should be prevented by the usage of internationally accepted endpoints reported in the STEEP guidelines for breast cancer endpoint reporting [23]. In order to get closer to clinical implementation, studies with a higher LOE are warranted. A feasible strategy may be to select patients from previously established prospective cohorts [96].
In this review, we have not addressed the rational mechanistic pathways linking the investigated markers to breast cancer recurrence, as in many of the included studies this aspect is not explored. Functional exploration of epigenetic markers can help in marker validation as it adds a hint towards causation, which often lacks in observational epigenetic research [18]. However, if a marker is thoroughly validated, it can be of clinical use without being mechanistically understood [18]. We acknowledge that the REMARK criteria were designed as reporting guidelines and not as a tool for quality assessment. As reporting quality and study quality are not synonymous, the REMARK score is not a quality indicator as such, although we did find a relation between the REMARK score and reporting of statistically significant results. The REMARK score should not be regarded as a rating, but as a tool used to identify weaknesses in research. Some included studies analysed methylation as a side objective, rather than a main study objective, resulting in less well-described methodology and thus poor REMARK performance. A low REMARK score should therefore not be mistaken for an indicator of a poor marker, but rather an indication this marker needs further investigation.
Conclusion
In this systematic review, we provided a comprehensive overview of the available literature on prognostic DNA methylation biomarkers in ER- and/or PR-positive breast cancer. We identified hypermethylation of RASSF1, BRCA1, PITX2, CDH1, RARB, PGR, PCDH10 and a panel of GSTP1, RASSF1 and RARB as potential markers of poor disease outcome. We also provided an analysis of study reporting, which indicates high heterogeneity in currently published literature on this subject. Future prognostic DNA methylation marker research would benefit from standardised DNA methylation assessment methods, thorough study reporting and the use of standardised endpoint definitions.
Availability of data and materials
Not applicable.
Abbreviations
- CI:
-
Confidence interval
- CpG:
-
Cytosine guanine dinucleotide
- ER:
-
Oestrogen receptor
- HR:
-
Hazard ratio
- LOE:
-
Level of evidence
- PR:
-
Progesterone receptor
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and meta-Analyses
- REMARK:
-
REporting recommendations for tumour MARKer prognostic studies
- STEEP:
-
The proposed Standardized definitions for Efficacy EndPoints in adjuvant breast cancer trials
References
American Cancer society. Global cancer facts & figures. 3rd ed. Atlanta: American Cancer Society; 2015.
Dowsett M, Forbes JF, Bradley R, Ingle J, Aihara T, Bliss J, et al. Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet. 2015;386(10001):1341–52.
Pan H, Gray R, Braybrooke J, Davies C, Taylor C, McGale P, et al. 20-year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N Engl J Med. 2017;377(19):1836–46.
Peto R, Davies C, Godwin J, Gray R, Pan HC, Clarke M, et al. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012;379(9814):432–44.
Wishart GC, Bajdik CD, Azzato EM, Dicks E, Greenberg DC, Rashbass J, et al. A population-based validation of the prognostic model PREDICT for early breast cancer. Eur J Surg Oncol. 2011;37(5):411–7.
Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart M, et al. Tailoring therapies-improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol. 2015;26(8):1533–46.
Olivotto IA, Bajdik CD, Ravdin PM, Speers CH, Coldman AJ, Norris BD, et al. Population-based validation of the prognostic model ADJUVANT! for early breast cancer. J Clin Oncol. 2005;23(12):2716–25.
Denduluri N, Somerfield MR, Eisen A, Holloway JN, Hurria A, King TA, et al. Selection of optimal adjuvant chemotherapy regimens for human epidermal growth factor receptor 2 (HER2)-negative and adjuvant targeted therapy for HER2-positive breast cancers: an American Society of Clinical Oncology Guideline Adaptation of the Cancer Care Ontario Clinical Practice Guideline. J Clin Oncol. 2016;34(20):2416–27.
Hudis CA. Biology before anatomy in early breast cancer--precisely the point. N Engl J Med. 2015;373(21):2079–80.
Cardoso F, van't Veer LJ, Bogaerts J, Slaets L, Viale G, Delaloge S, et al. 70-gene signature as an aid to treatment decisions in early-stage breast cancer. N Engl J Med. 2016;375(8):717–29.
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med. 2018;379(2):111–21.
Jeschke J, Collignon E, Fuks F. DNA methylome profiling beyond promoters - taking an epigenetic snapshot of the breast tumor microenvironment. FEBS J. 2015;282(9):1801–14.
Stefansson OA, Moran S, Gomez A, Sayols S, Arribas-Jorba C, Sandoval J, et al. A DNA methylation-based definition of biologically distinct breast cancer subtypes. Mol Oncol. 2015;9(3):555–68.
Baylin SB. DNA methylation and gene silencing in cancer. Nat Clin Pract Oncol. 2005;2(Suppl 1):S4–11.
Baylin SB, Herman JG. DNA hypermethylation in tumorigenesis: epigenetics joins genetics. Trends Genet. 2000;16(4):168–74.
Laird PW. The power and the promise of DNA methylation markers. Nat Rev Cancer. 2003;3(4):253–66.
Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2(8):e124.
Michels KB, Binder AM, Dedeurwaerder S, Epstein CB, Greally JM, Gut I, et al. Recommendations for the design and analysis of epigenome-wide association studies. Nat Methods. 2013;10(10):949–55.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Cerne JZ, Zong L, Jelinek J, Hilsenbeck SG, Wang T, Oesterreich S, et al. BRCA1 promoter methylation status does not predict response to tamoxifen in sporadic breast cancer patients. Breast Cancer Res Treat. 2012;135(1):135–43.
Hayes DF, Bast RC, Desch CE, Fritsche H Jr, Kemeny NE, Jessup JM, et al. Tumor marker utility grading system: a framework to evaluate clinical utility of tumor markers. J Natl Cancer Inst. 1996;88(20):1456–66.
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, et al. The Oxford 2011 levels of evidence. Oxford Centre for Evidence-Based Medicine. 2011. http://www.cebm.net/indexaspx?o=5653.
Hudis CA, Barlow WE, Costantino JP, Gray RJ, Pritchard KI, Chapman JA, et al. Proposal for standardized definitions for efficacy end points in adjuvant breast cancer trials: the STEEP system. J Clin Oncol. 2007;25(15):2127–32.
Altman DG, McShane LM, Sauerbrei W, Taube SE. Reporting recommendations for tumor marker prognostic studies (REMARK): explanation and elaboration. BMC Med. 2012;10:51.
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM. REporting recommendations for tumour MARKer prognostic studies (REMARK). Br J Cancer. 2005;93(4):387–91.
Angelova SG, Krasteva ME, Gospodinova ZI, Georgieva EI. CHEK2 gene alterations independently increase the risk of death from breast cancer in Bulgarian patients. Neoplasma. 2012;59(6):622–30.
Arai T, Miyoshi Y, Kim SJ, Taguchi T, Tamaki Y, Noguchi S. Association of GSTP1 CpG islands hypermethylation with poor prognosis in human breast cancers. Breast Cancer Res Treat. 2006;100(2):169–76.
Buhmeida A, Merdad A, Al-Maghrabi J, Al-Thobaiti F, Ata M, Bugis A, et al. RASSF1A methylation is predictive of poor prognosis in female breast cancer in a background of overall low methylation frequency. Anticancer Res. 2011;31(9):2975–81.
Chen Y, Zhou J, Xu Y, Li Z, Wen X, Yao L, et al. BRCA1 promoter methylation associated with poor survival in Chinese patients with sporadic breast cancer. Cancer Sci. 2009;100(9):1663–7.
Chimonidou M, Kallergi G, Georgoulias V, Welch DR, Lianidou ES. Breast cancer metastasis suppressor-1 promoter methylation in primary breast tumors and corresponding circulating tumor cells. Mol Cancer Res. 2013;11(10):1248–57.
Dietrich D, Krispin M, Dietrich J, Fassbender A, Lewin J, Harbeck N, et al. CDO1 promoter methylation is a biomarker for outcome prediction of anthracycline treated, estrogen receptor-positive, lymph node-positive breast cancer patients. BMC Cancer. 2010;10:247.
Ebeid SA, El Moneim NAA, Hewala TIM, Hemida MA, Shehata G, El-Taher N. Assessment of hypermethylation of RASSF1A and protocadherin-10 tumor suppressor genes in breast cancer females: a six-year disease-free survival case-control study. Middle East J Cancer. 2016;7(1):9–20.
Fang F, Turcan S, Rimner A, Kaufman A, Giri D, Morris LG, et al. Breast cancer methylomes establish an epigenomic foundation for metastasis. Sci Transl Med. 2011;3(75):75ra25.
Faryna M, Konermann C, Aulmann S, Bermejo JL, Brugger M, Diederichs S, et al. Genome-wide methylation screen in low-grade breast cancer identifies novel epigenetically altered genes as potential biomarkers for tumor diagnosis. FASEB J. 2012;26(12):4937–50.
Fiegl H, Jones A, Hauser-Kronberger C, Hutarew G, Reitsamer R, Jones RL, et al. Methylated NEUROD1 promoter is a marker for chemosensitivity in breast cancer. Clin Cancer Res. 2008;14(11):3494–502.
Fiegl H, Millinger S, Mueller-Holzner E, Marth C, Ensinger C, Berger A, et al. Circulating tumor-specific DNA: a marker for monitoring efficacy of adjuvant therapy in cancer patients. Cancer Res. 2005;65(4):1141–5.
Fu DY, Wang ZM, Wang BL, Chen L, Yang WT, Shen ZZ, et al. Frequent epigenetic inactivation of the receptor tyrosine kinase EphA5 by promoter methylation in human breast cancer. Hum Pathol. 2010;41(1):48–58.
Fujita N, Kagara N, Yamamoto N, Shimazu K, Shimomura A, Shimoda M, et al. Methylated DNA and high total DNA levels in the serum of patients with breast cancer following neoadjuvant chemotherapy are predictive of a poor prognosis. Oncol Lett. 2014;8(1):397–403.
Fujita N, Nakayama T, Yamamoto N, Kim SJ, Shimazu K, Shimomura A, et al. Methylated DNA and total DNA in serum detected by one-step methylation-specific PCR is predictive of poor prognosis for breast cancer patients. Oncology. 2012;83(5):273–82.
Gobel G, Auer D, Gaugg I, Schneitter A, Lesche R, Muller-Holzner E, et al. Prognostic significance of methylated RASSF1A and PITX2 genes in blood- and bone marrow plasma of breast cancer patients. Breast Cancer Res Treat. 2011;130(1):109–17.
Harbeck N, Nimmrich I, Hartmann A, Ross JS, Cufer T, Grutzmann R, et al. Multicenter study using paraffin-embedded tumor tissue testing PITX2 DNA methylation as a marker for outcome prediction in tamoxifen-treated, node-negative breast cancer patients. J Clin Oncol. 2008;26(31):5036–42.
Hartmann O, Spyratos F, Harbeck N, Dietrich D, Fassbender A, Schmitt M, et al. DNA methylation markers predict outcome in node-positive, estrogen receptor-positive breast cancer with adjuvant anthracycline-based chemotherapy. Clin Cancer Res. 2009;15(1):315–23.
Hill VK, Hesson LB, Dansranjavin T, Dallol A, Bieche I, Vacher S, et al. Identification of 5 novel genes methylated in breast and other epithelial cancers. Mol Cancer. 2010;9:51.
Hill VK, Ricketts C, Bieche I, Vacher S, Gentle D, Lewis C, et al. Genome-wide DNA methylation profiling of CpG islands in breast cancer identifies novel genes associated with tumorigenicity. Cancer Res. 2011;71(8):2988–99.
Huang YT, Li FF, Ke C, Li Z, Li ZT, Zou XF, et al. PTPRO promoter methylation is predictive of poorer outcome for HER2-positive breast cancer: indication for personalized therapy. J Transl Med. 2013;11:245.
Iorns E, Turner NC, Elliott R, Syed N, Garrone O, Gasco M, et al. Identification of CDK10 as an important determinant of resistance to endocrine therapy for breast cancer. Cancer Cell. 2008;13(2):91–104.
Jahangiri R, Mosaffa F, Emami Razavi A, Teimoori-Toolabi L, Jamialahmadi K. Altered DNA methyltransferases promoter methylation and mRNA expression are associated with tamoxifen response in breast tumors. J Cell Physiol. 2018;233(9):7305–19.
Jing F, Jun L, Yong Z, Wang Y, Fei X, Zhang J, et al. Multigene methylation in serum of sporadic Chinese female breast cancer patients as a prognostic biomarker. Oncology. 2008;75(1–2):60–6.
Jung SP, Kim S, Nam SJ, Kim I, Bae JW. The role of the CDH1 promoter hypermethylation in the axillary lymph node metastasis and prognosis. J Breast Cancer. 2013;16(1):16–22.
Karray-Chouayekh S, Trifa F, Khabir A, Boujelbane N, Sellami-Boudawara T, Daoud J, et al. Aberrant methylation of RASSF1A is associated with poor survival in Tunisian breast cancer patients. J Cancer Res Clin Oncol. 2010;136(2):203–10.
Kioulafa M, Balkouranidou I, Sotiropoulou G, Kaklamanis L, Mavroudis D, Georgoulias V, et al. Methylation of cystatin M promoter is associated with unfavorable prognosis in operable breast cancer. Int J Cancer. 2009;125(12):2887–92.
Kioulafa M, Kaklamanis L, Mavroudis D, Georgoulias V, Lianidou ES. Prognostic significance of RASSF1A promoter methylation in operable breast cancer. Clin Biochem. 2009;42(10–11):970–5.
Kioulafa M, Kaklamanis L, Stathopoulos E, Mavroudis D, Georgoulias V, Lianidou ES. Kallikrein 10 (KLK10) methylation as a novel prognostic biomarker in early breast cancer. Ann Oncol. 2009;20(6):1020–5.
Klajic J, Fleischer T, Dejeux E, Edvardsen H, Warnberg F, Bukholm I, et al. Quantitative DNA methylation analyses reveal stage dependent DNA methylation and association to clinico-pathological factors in breast tumors. BMC Cancer. 2013;13:456.
Krasteva ME, Bozhanov SS, Antov GG, Gospodinova ZI, Angelov SG. Breast cancer patients with hypermethylation in the promoter of BRCA1 gene exhibit favorable clinical status. Neoplasma. 2012;59(1):85–91.
Li S, Rong M, Iacopetta B. DNA hypermethylation in breast cancer and its association with clinicopathological features. Cancer Lett. 2006;237(2):272–80.
Li SY, Li R, Chen YL, Xiong LK, Wang HL, Rong L, et al. Aberrant PTPRO methylation in tumor tissues as a potential biomarker that predicts clinical outcomes in breast cancer patients. BMC Genet. 2014;15:67.
Liu J, Sun X, Qin S, Wang H, Du N, Li Y, et al. CDH1 promoter methylation correlates with decreased gene expression and poor prognosis in patients with breast cancer. Oncol Lett. 2016;11(4):2635–43.
Liu W, Wu J, Shi G, Yue X, Liu D, Zhang Q. Aberrant promoter methylation of PCDH10 as a potential diagnostic and prognostic biomarker for patients with breast cancer. Oncol Lett. 2018;16(4):4462–70.
Lu L, Katsaros D, Zhu Y, Hoffman A, Luca S, Marion CE, et al. Let-7a regulation of insulin-like growth factors in breast cancer. Breast Cancer Res Treat. 2011;126(3):687–94.
Maier S, Nimmrich I, Koenig T, Eppenberger-Castori S, Bohlmann I, Paradiso A, et al. DNA-methylation of the homeodomain transcription factor PITX2 reliably predicts risk of distant disease recurrence in tamoxifen-treated, node-negative breast cancer patients--technical and clinical validation in a multi-centre setting in collaboration with the European Organisation for Research and Treatment of Cancer (EORTC) PathoBiology group. Eur J Cancer (Oxford). 2007;43(11):1679–86.
Martinez-Galan J, Torres-Torres B, Nunez MI, Lopez-Penalver J, Del Moral R, Ruiz De Almodovar JM, et al. ESR1 gene promoter region methylation in free circulating DNA and its correlation with estrogen receptor protein expression in tumor tissue in breast cancer patients. BMC Cancer. 2014;14:59.
Martins AT, Monteiro P, Ramalho-Carvalho J, Costa VL, Dinis-Ribeiro M, Leal C, et al. High RASSF1A promoter methylation levels are predictive of poor prognosis in fine-needle aspirate washings of breast cancer lesions. Breast Cancer Res Treat. 2011;129(1):1–9.
Mc Cormack O, Chung WY, Fitzpatrick P, Cooke F, Flynn B, Harrison M, et al. Progesterone receptor B (PRB) promoter hypermethylation in sporadic breast cancer: progesterone receptor B hypermethylation in breast cancer. Breast Cancer Res Treat. 2008;111(1):45–53.
Mehrotra J, Ganpat MM, Kanaan Y, Fackler MJ, McVeigh M, Lahti-Domenici J, et al. Estrogen receptor/progesterone receptor-negative breast cancers of young African-American women have a higher frequency of methylation of multiple genes than those of Caucasian women. Clin Cancer Res. 2004;10(6):2052–7.
Mirza S, Sharma G, Parshad R, Srivastava A, Gupta SD, Ralhan R. Clinical significance of Stratifin, ERalpha and PR promoter methylation in tumor and serum DNA in Indian breast cancer patients. Clin Biochem. 2010;43(4–5):380–6.
Mirza S, Sharma G, Parshad R, Srivastava A, Gupta SD, Ralhan R. Clinical significance of promoter hypermethylation of ERbeta and RARbeta2 in tumor and serum DNA in Indian breast cancer patients. Ann Surg Oncol. 2012;19(9):3107–15.
Muller HM, Widschwendter A, Fiegl H, Ivarsson L, Goebel G, Perkmann E, et al. DNA methylation in serum of breast cancer patients: an independent prognostic marker. Cancer Res. 2003;63(22):7641–5.
Nimmrich I, Sieuwerts AM, Meijer-van Gelder ME, Schwope I, Bolt-de Vries J, Harbeck N, et al. DNA hypermethylation of PITX2 is a marker of poor prognosis in untreated lymph node-negative hormone receptor-positive breast cancer patients. Breast Cancer Res Treat. 2008;111(3):429–37.
Noetzel E, Veeck J, Niederacher D, Galm O, Horn F, Hartmann A, et al. Promoter methylation-associated loss of ID4 expression is a marker of tumour recurrence in human breast cancer. BMC Cancer. 2008;8:154.
Palmieri C, Rudraraju B, Monteverde M, Lattanzio L, Gojis O, Brizio R, et al. Methylation of the calcium channel regulatory subunit alpha2delta-3 (CACNA2D3) predicts site-specific relapse in oestrogen receptor-positive primary breast carcinomas. Br J Cancer. 2012;107(2):375–81.
Park SY, Seo AN, Jung HY, Gwak JM, Jung N, Cho NY, et al. Alu and LINE-1 hypomethylation is associated with HER2 enriched subtype of breast cancer. PLoS One. 2014;9(6):e100429.
Pathiraja TN, Shetty PB, Jelinek J, He R, Hartmaier R, Margossian AL, et al. Progesterone receptor isoform-specific promoter methylation: association of PRA promoter methylation with worse outcome in breast cancer patients. Clin Cancer Res. 2011;17(12):4177–86.
Perez-Janices N, Blanco-Luquin I, Torrea N, Liechtenstein T, Escors D, Cordoba A, et al. Differential involvement of RASSF2 hypermethylation in breast cancer subtypes and their prognosis. Oncotarget. 2015;6(27):23944–58.
Ramos EA, Camargo AA, Braun K, Slowik R, Cavalli IJ, Ribeiro EM, et al. Simultaneous CXCL12 and ESR1 CpG island hypermethylation correlates with poor prognosis in sporadic breast cancer. BMC Cancer. 2010;10:23.
Ren J, Jin F, Yu Z, Zhao L, Wang L, Bai X, et al. MYC overexpression and poor prognosis in sporadic breast cancer with BRCA1 deficiency. Tumour Biol. 2013;34(6):3945–58.
Rodriguez BA, Cheng AS, Yan PS, Potter D, Agosto-Perez FJ, Shapiro CL, et al. Epigenetic repression of the estrogen-regulated Homeobox B13 gene in breast cancer. Carcinogenesis. 2008;29(7):1459–65.
Sharma G, Mirza S, Parshad R, Srivastava A, Gupta SD, Pandya P, et al. Clinical significance of promoter hypermethylation of DNA repair genes in tumor and serum DNA in invasive ductal breast carcinoma patients. Life Sci. 2010;87(3–4):83–91.
Sharma G, Mirza S, Yang YH, Parshad R, Hazrah P, Datta Gupta S, et al. Prognostic relevance of promoter hypermethylation of multiple genes in breast cancer patients. Cell Oncol. 2009;31(6):487–500.
Shen Y, Wang Z, Loo LW, Ni Y, Jia W, Fei P, et al. LINC00472 expression is regulated by promoter methylation and associated with disease-free survival in patients with grade 2 breast cancer. Breast Cancer Res Treat. 2015;154(3):473–82.
Stephen HM, Khoury RJ, Majmudar PR, Blaylock T, Hawkins K, Salama MS, et al. Epigenetic suppression of neprilysin regulates breast cancer invasion. Oncogenesis. 2016;5:e207.
Ulirsch J, Fan C, Knafl G, Wu MJ, Coleman B, Perou CM, et al. Vimentin DNA methylation predicts survival in breast cancer. Breast Cancer Res Treat. 2013;137(2):383–96.
van Hoesel AQ, van de Velde CJ, Kuppen PJ, Liefers GJ, Putter H, Sato Y, et al. Hypomethylation of LINE-1 in primary tumor has poor prognosis in young breast cancer patients: a retrospective cohort study. Breast Cancer Res Treat. 2012;134(3):1103–14.
van Hoesel AQ, van de Velde CJ, Kuppen PJ, Putter H, de Kruijf EM, van Nes JG, et al. Primary tumor classification according to methylation pattern is prognostic in patients with early stage ER-negative breast cancer. Breast Cancer Res Treat. 2012;131(3):859–69.
Veeck J, Chorovicer M, Naami A, Breuer E, Zafrakas M, Bektas N, et al. The extracellular matrix protein ITIH5 is a novel prognostic marker in invasive node-negative breast cancer and its aberrant expression is caused by promoter hypermethylation. Oncogene. 2008;27(6):865–76.
Veeck J, Geisler C, Noetzel E, Alkaya S, Hartmann A, Knuchel R, et al. Epigenetic inactivation of the secreted frizzled-related protein-5 (SFRP5) gene in human breast cancer is associated with unfavorable prognosis. Carcinogenesis. 2008;29(5):991–8.
Veeck J, Noetzel E, Bektas N, Jost E, Hartmann A, Knuchel R, et al. Promoter hypermethylation of the SFRP2 gene is a high-frequent alteration and tumor-specific epigenetic marker in human breast cancer. Mol Cancer. 2008;7:83.
Wang S, Dorsey TH, Terunuma A, Kittles RA, Ambs S, Kwabi-Addo B. Relationship between tumor DNA methylation status and patient characteristics in African-American and European-American women with breast cancer. PLoS One. 2012;7(5):e37928.
Wee EJ, Peters K, Nair SS, Hulf T, Stein S, Wagner S, et al. Mapping the regulatory sequences controlling 93 breast cancer-associated miRNA genes leads to the identification of two functional promoters of the Hsa-mir-200b cluster, methylation of which is associated with metastasis or hormone receptor status in advanced breast cancer. Oncogene. 2012;31(38):4182–95.
Weissenborn C, Ignatov T, Nass N, Kalinski T, Dan Costa S, Zenclussen AC, et al. GPER promoter methylation controls GPER expression in breast cancer patients. Cancer Investig. 2017;35(2):100–7.
Widschwendter M, Siegmund KD, Muller HM, Fiegl H, Marth C, Muller-Holzner E, et al. Association of breast cancer DNA methylation profiles with hormone receptor status and response to tamoxifen. Cancer Res. 2004;64(11):3807–13.
Xu J, Shetty PB, Feng W, Chenault C, Bast RC Jr, Issa JP, et al. Methylation of HIN-1, RASSF1A, RIL and CDH13 in breast cancer is associated with clinical characteristics, but only RASSF1A methylation is associated with outcome. BMC Cancer. 2012;12:243.
Xu X, Gammon MD, Zhang Y, Bestor TH, Zeisel SH, Wetmur JG, et al. BRCA1 promoter methylation is associated with increased mortality among women with breast cancer. Breast Cancer Res Treat. 2009;115(2):397–404.
Xu Y, Diao L, Chen Y, Liu Y, Wang C, Ouyang T, et al. Promoter methylation of BRCA1 in triple-negative breast cancer predicts sensitivity to adjuvant chemotherapy. Ann Oncol. 2013;24(6):1498–505.
Zhang Y, Zhang B, Fang J, Cao X. Hypomethylation of DNA-binding inhibitor 4 serves as a potential biomarker in distinguishing acquired tamoxifen-refractory breast cancer. Int J Clin Exp Pathol. 2015;8(8):9500–5.
Simon RM, Paik S, Hayes DF. Use of archived specimens in evaluation of prognostic and predictive biomarkers. J Natl Cancer Inst. 2009;101(21):1446–52.
Claus R, Wilop S, Hielscher T, Sonnet M, Dahl E, Galm O, et al. A systematic comparison of quantitative high-resolution DNA methylation analysis and methylation-specific PCR. Epigenetics. 2012;7(7):772–80.
Quillien V, Lavenu A, Karayan-Tapon L, Carpentier C, Labussiere M, Lesimple T, et al. Comparative assessment of 5 methods (methylation-specific polymerase chain reaction, MethyLight, pyrosequencing, methylation-sensitive high-resolution melting, and immunohistochemistry) to analyze O6-methylguanine-DNA-methyltranferase in a series of 100 glioblastoma patients. Cancer. 2012;118(17):4201–11.
Draht MX, Smits KM, Jooste V, Tournier B, Vervoort M, Ramaekers C, et al. Analysis of RET promoter CpG island methylation using methylation-specific PCR (MSP), pyrosequencing, and methylation-sensitive high-resolution melting (MS-HRM): impact on stage II colon cancer patient outcome. Clin Epigenetics. 2016;8:44.
Koch A, Joosten SC, Feng Z, de Ruijter TC, Draht MX, Melotte V, et al. Analysis of DNA methylation in cancer: location revisited. Nat Rev Clin Oncol. 2018;15(7):459–66.
van Vlodrop IJ, Niessen HE, Derks S, Baldewijns MM, van Criekinge W, Herman JG, et al. Analysis of promoter CpG island hypermethylation in cancer: location, location, location! Clin Cancer Res. 2011;17(13):4225–31.
Stone A, Valdes-Mora F, Gee JM, Farrow L, McClelland RA, Fiegl H, et al. Tamoxifen-induced epigenetic silencing of oestrogen-regulated genes in anti-hormone resistant breast cancer. PLoS One. 2012;7(7):e40466.
Acknowledgements
The authors would like to thank Sophie Joosten and Muriel Draht for the constructive discussions on the design and contents of this systematic review.
Funding
This study was supported, in part, by a research grant from AstraZeneca (transDATA study; BOOG 2006-01, D5392-NL-003 – Sub study). AstraZeneca had no role in the design of this study, its execution, analyses, interpretation of the data or decision to submit results.
Author information
Authors and Affiliations
Contributions
TCDR contributed to the study design and data acquisition and drafted the manuscript. FH contributed to the data acquisition and co-drafted the manuscript. KMS contributed to the study design and co-drafted the manuscript. MJA contributed to the study design. MVE contributed to the conception of the study and study design and co-drafted the manuscript. VCGH contributed to the conception of the study and study design and co-drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Prof. dr. Tjan-Heijnen reports grants from AstraZeneca, during the conduct of the study; grants and non-financial support from Roche; grants and non-financial support from Pfizer; grants and non-financial support from Novartis; grants and non-financial support from E Lilly; and grants from Eisai, outside the submitted work. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Tables S1.
Complete search terms pubmed and embase. Complete overview of keywords and equivalents used for the literature search in pubmed and embase.
Additional file 2: Table S2.
REMARK checklist for scoring the reviewed studies as published by McShane et al. British journal of cancer. 2005;93 (4):387–91. REMARK checklist used for calculating the remark score for all included studies.
Additional file 3: Table S3.
studies, studied markers and outcomes. Review Data Table. Complete review data containing all included studies, markers and outcome values.
Additional file 4: Table S4.
Risk of potential bias and confounders of the included studies. Table indicating risks for potential bias for all included studies.
Additional file 5: Table S5.
Results table of multiple investigated markers. Table summarising all results from markers that were investigated in two or more independent study populations.
Additional file 6: FigureS6.
Correlation of single tested markers with prognosis. Overview of all markers tested in a single study population and reported correlation with prognosis. Italic markers do not correspond to Ref-Seq registered genes.
Additional file 7: Table S7.
Correlation of methylation marker panels with prognosis. Correlation of methylation marker panels with prognosis in early stage breast cancer. Overview of all marker panels tested in a single study population and reported correlation with prognosis.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
de Ruijter, T.C., van der Heide, F., Smits, K.M. et al. Prognostic DNA methylation markers for hormone receptor breast cancer: a systematic review. Breast Cancer Res 22, 13 (2020). https://doi.org/10.1186/s13058-020-1250-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-020-1250-9