Abstract
Background
The epidural stimulation test can help detect if a catheter is correctly positioned in the epidural space. Previous studies showed that a current of up to 16 mA was required to elicit a motor response, but few peripheral nerve stimulators can produce a current this high. Manipulating pulse width can produce a positive response at a lower current. To clarify the effects of pulse width on the epidural stimulation test, we performed a single-blinded study in a porcine model to estimate the equivalent current needed at varying pulse widths.
Methods
After obtaining local ethics approval, an 18G insulated Tuohy needle was advanced into the epidural space at the lower lumbar spinal level, and a 20G stimulating epidural catheter was advanced 30 cm cephalad. A gradually increasing electrical current was applied, and a motor response was elicited at pulse widths of 0.1, 0.2, 0.3, 0.5, and 1 msec. This was followed by a 1-2 cm catheter withdrawal, and the process was repeated for a total of 15 locations per pig.
Results
Recorded threshold currents ranged from 0.36-9.5 mA at a pulse width of 0.2 msec. Our results show a linear relationship between threshold current and pulse width.
Conclusions
In situations where different pulse widths are needed, the nomograms presented here may be useful to estimate the equivalent threshold current which is required to elicit a motor response according to previously published criteria for epidural stimulation tests.
Résumé
Contexte
Le test de stimulation péridurale permet de détecter le bon positionnement d’un cathéter dans l’espace péridural. Les études précédentes ont démontré que le courant nécessaire pour provoquer une réponse motrice allait jusqu’à 16 mA, mais il n’existe que peu de stimulateurs de nerfs périphériques qui puissent produire un courant aussi élevé. En jouant sur la durée de l’impulsion, on peut obtenir une réponse positive à un courant plus bas. Afin de clarifier les effets de la durée de l’impulsion sur le test de stimulation péridurale, nous avons réalisé une étude en simple aveugle sur un modèle porcin pour estimer le courant équivalent nécessaire à différentes durées d’impulsion.
Méthode
Après avoir obtenu le consentement du comité de déontologie local, une aiguille Tuohy 18G électriquement neutre a été insérée dans l’espace péridural à un niveau lombaire bas, et un cathéter péridural stimulant de 20G a été avancé de 30 cm en direction de la tête. Un courant électrique croissant a été appliqué, et une réponse motrice a été obtenue à des durées d’impulsion de 0,1, 0,2, 0,3, 0,5 et 1 msec. Cette réponse a été suivie par un retrait de 1-2 cm du cathéter, et le processus a été répété à 15 emplacements au total par animal.
Résultats
Les courants seuils enregistrés étaient situés entre 0,36-9,5 mA à une durée d’impulsion de 0,2 msec. Nos résultats démontrent une relation linéaire entre le courant seuil et la durée d’impulsion.
Conclusion
Dans les cas où des durées d’impulsion différentes sont nécessaires, les nomogrammes présentés ici pourraient être utiles pour évaluer le courant seuil équivalent nécessaire pour provoquer une réponse motrice selon les critères publiés précédemment pour les tests de stimulation péridurale.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nerve stimulation can help determine accurate catheter tip location.1,2 The original criteria for the epidural stimulation test (EST) state that the catheter is correctly positioned within the epidural space if an electrical current of 1-10 mA at a pulse width of 0.2 msec is applied through the epidural catheter and an appropriate motor response is elicited.3 A response elicited at < 1 mA may indicate catheter placement in the subarachnoid or subdural space or in proximity to a nerve root. Research subsequent to the original criteria for the EST has also found that, in some patients, a current of up to 16 mA is required to elicit a motor response.4-6 Nevertheless, many peripheral nerve stimulators are incapable of producing a current > 5 mA. Thus, pulse width is occasionally lengthened in an ad hoc fashion in an attempt to produce a positive response at a lower current.
Although a few studies have performed the EST using different pulse widths ranging from 0.3-1 msec (as opposed to 0.2 msec),7,8 there is a lack of studies assessing the significance and implications of using different pulse widths to interpret threshold currents for the EST. We hypothesized that an equivalent factor for each pulse width could be estimated based on simple linear regression. The objective of this study was to standardize the equivalent electrical current (mA) with respect to pulse width by applying simple linear regression in a porcine model. We also sought to determine the chronaxie value associated with this porcine model.
Methods
Procedure
After local ethics approval (Animal Care and Use Committee, University of Alberta), four Duroc pigs weighing approximately 30 kg were anesthetized with ketamine (5 mg·kg−1 iv). Anesthesia was maintained with isoflurane, and spontaneous breathing was continued. Neuromuscular blocking drugs were not used during this study. Four pigs were chosen for convenience and to keep the overall number of animals used to a minimum.
In each pig, an 18G insulated Tuohy needle (PAJUNK®, Dyna Medical Corp, London, ON, Canada) was advanced into the epidural space using the loss of resistance technique at the lower lumbar spinal level. Once in the epidural space, a 20G stimulating epidural catheter (PAJUNK, Geisingen, Germany) was inserted and advanced 30 cm cephalad. An electrical current was applied to the catheter using a peripheral nerve stimulator (MultiStim SENSOR, PAJUNK, Geisingen, Germany), and the current was gradually increased until a motor response was elicited at pulse widths of 0.1, 0.2, 0.3, 0.5, and 1 msec. A single independent observer, blinded to the current intensity and pulse width being administered, established a consistent minimum motor response (twitch) that would constitute the desired amplitude of reaction to stimulation. The observer then alerted the investigator operating the stimulator to record the current applied when the established motor response was observed. This test was repeated five times, once for each of the five pulse widths. Following the five tests, the catheter was withdrawn by 1-2 cm and the process was repeated for a total of 15 locations per pig, resulting in 75 data points for each pig. All catheters were checked carefully and aspirated for cerebrospinal fluid to ensure that the catheter had not entered the intrathecal space.
Following the experiment, the pigs were euthanized by increasing the isoflurane to 5% for ten minutes, followed by intracardial administration of a supersaturated potassium chloride solution as per institutional standard operating procedure.
Data analysis
A linear regression model was developed using Microsoft Excel (Microsoft, Redmond, WA, USA) to obtain the slope of the linear regression equation. The equivalent current value was converted to charge according to the following equation:9
where Q is the charge applied to the nerve (nanocoulombs; nC); I(t) is the current (mA) at the time (t); Ir is the rheobase (the minimum current intensity required to depolarize the nerve); t is the duration of the applied current (pulse width measured in msec); and C is the chronaxie (the minimum pulse width required to depolarize the nerve when the current intensity is twice the rheobase). The charge was then plotted against the pulse width as the charge duration curve defined by the following equation:
Linear regression analysis was used to determine the slope (a) and the y-intercept (b). From this, chronaxie values were determined according to the following formula:
Confidence intervals (95%) were calculated from linear regression using SPSS® version 20 (IBM Corp., Armonk, NY, USA).
Results
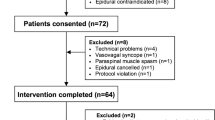
Sixty different locations (15 × 4 pigs) were used to record in the epidural space. Aspiration of cerebrospinal fluid was negative for all catheters. Threshold currents were recorded using five pulse widths (0.1, 0.2, 0.3, 0.5, and 1 msec) at each location in each pig. Equivalent threshold currents for each pulse width are presented in Fig. 1, and coefficients at a pulse width of 0.2 msec are shown in the Table. Nomograms for threshold currents of 1-10 mA with different pulse widths5 are presented in terms of current (mA) vs pulse width (Fig. 2). Chronaxie was calculated as 0.17 msec.
Discussion
This study shows that, in a porcine model, equivalent threshold currents for the EST using different pulse widths can be estimated using simple linear regression. With regard to the original criteria for the EST, namely, a motor response at a threshold current of 1-10 mA with a pulse width of 0.2 msec, the equivalent threshold current would decrease to a range of 0.63-6.3 mA if the pulse width were increased to 1.0 msec, as exemplified in Fig. 2.
Similar to peripheral nerve simulation, current intensity in epidural stimulation is expressed in mA, while the duration of the generated impulse is expressed in milliseconds. Although the product of these two values provides the total amount of electric power delivered to the area being stimulated,10 one common misconception is that the clinical effect would be the same when the same total number of charges (nC) are delivered, as reported in an article by Charghi et al.7 In their article, the significance of pulse width on nerve stimulation is critical but mostly ignored in these cases, since grouping all stimulation thresholds together and simply reporting the mean charge without distinguishing between pulse widths provides an inaccurate measure of the threshold current actually being delivered. This error serves to show why the mean charge described in their study (1.9 nC) was substantially higher than that in the original studies of the EST (3.78 mA/0.76 nC3 and 4.9 mA/0.98 nC5). The stimulation of motor fibres is more effective with delivery of less charge when approaching the fibres’ chronaxie (0.17 msec) and when comparing with the relatively long pulse width (1 msec). This corresponds with the fact that pulse widths of both 0.3 and 1.0 msec were used for their study, as stated by the authors.7 Thus, our study may partly explain the discrepancy in the observations made by Charghi et al. by providing a more detailed examination of the relationship between current (mA) and pulse width (msec) during epidural stimulation.
Electrical stimulation provides an objective method of confirming epidural catheter placement in real-time.3,11,12 Currents of 1-10 mA are generally used to elicit motor responses upon appropriate placement of the stimulating catheter tip in the epidural space proximal to the nerve roots. For practicality and ease of illustrating our purpose, we have represented and exemplified our results using a range of currents with 1 (lower limit) and 10 (upper limit) mA values highlighted (Fig. 2). Nevertheless, as suggested in the original article describing the EST,3 current settings are merely intended as guidelines and may require adjustment depending on the situation. Indeed, currents of well over 10 mA may be required for motor response,4,5 and motor responses elicited at ≤ 1 mA can serve as a warning to indicate possible placement of the catheter in the subarachnoid or subdural space or in proximity to the nerve root.13,14 In general, the distribution of an elicited motor response is more important than the current required to obtain it (provided it is above 1 mA); appropriate motor responses can confirm both the correct placement and the level of the catheter tip in the epidural space.13,15,16
Chronaxie values of mammalian peripheral nerves (in cats) are 0.05-0.17 msec for motor nerves and 0.4 msec for sensory nerves.17 In this study, the chronaxie value of 0.17 msec is in accordance with the results of the previous studies, despite the fact that these studies were performed in different species.18 Nevertheless, there may be differences in the pulse width-current relationship among species, and further studies are needed to establish whether the equivalent values for humans are similar to those obtained in the porcine model. Regardless, the results of this study support the notion that the underlying mechanism of epidural stimulation tests is primarily via peripheral nerve stimulation (i.e., the nerve root), as the electrophysiological behaviours in both species are similar.
Although the present study has yielded findings that have both theoretical and pedagogical merit, its design is not without flaws. The first limitation concerns the small sample size which was chosen to reduce the number of animals used. As mentioned above, the second limitation relates to the use of an animal model which, although unlikely, carries the risk that electrophysiology of nerve stimulation may be significantly different when tested in humans.
Nerve localization by stimulation has been described for nearly a century, but it is still regarded as part art and part science.19 As nerve stimulation equipment and techniques evolve, nerve localization becomes more science and less art; however, these improvements will not reach their full potential unless the basic electrical properties of nerves are fully understood, particularly for epidural stimulation. This study has taken a step towards understanding the relationship between threshold current (mA) and pulse width (msec). The experiments reported here show that the equivalent current with different pulse widths can be calculated and predicted. Such information should be of importance, not only in helping to interpret results with the nomograms but also in leading to a better understanding of the science of nerve stimulation. We hope that this work will generate further interest in the field of epidural stimulation.
References
McAuliffe NA, Pickworth S, Direnna T, Hong A. Electrophysiological stimulation (Tsui test) is feasible for epidural catheter positioning in adults with chronic back pain: a cohort study. Can J Anesth 2013; 60: 976-81.
Sutherland MA, Viscomi CM, Dominick TS, Anderson EL. Minimum current requirements for epidural stimulation test confirmation of epidural and intrathecal catheter placement. Reg Anesth Pain Med 2009; 34: 575-7.
Tsui BC, Gupta S, Finucane B. Confirmation of epidural catheter placement using nerve stimulation. Can J Anesth 1998; 45: 640-4.
Goobie SM, Montgomery CJ, Basu R, et al. Confirmation of direct epidural catheter placement using nerve stimulation in pediatric anesthesia. Anesth Analg 2003; 97: 984-8.
Tsui BC, Wagner A, Cave D, Seal R. Threshold current for an insulated epidural needle in pediatric patients. Anesth Analg 2004; 99: 694-6.
Tsui BC. Epidural stimulation test criteria. Anesth Analg 2006; 103: 775-6.
Charghi R, Chan SY, Kardash KJ, Finlayson RJ, Tran DQ. Electrical stimulation of the epidural space using a catheter with a removable stylet. Reg Anesth Pain Med 2007; 32: 152-6.
Jeong JS, Shim JC, Shim JH, Kim DW, Kang MS. Minimum current requirement for confirming the localization of an epiradicular catheter placement. Korean J Anesthesiol 2012; 63: 238-44.
Weiss G. Sur la possibilité de rendre comparables entre eux les appareils servant a l’excitation electrique. Arch Ital Biol 1901; 35: 413-46.
Bollini CA, Cacheiro F. Peripheral nerve stimulation. Tech Reg Anesth Pain Manag 2006; 10: 79-88.
Tsui BC, Gupta S, Finucane B. Determination of epidural catheter placement using nerve stimulation in obstetric patients. Reg Anesth Pain Med 1999; 24: 17-23.
Tsui BC, Wagner A, Cave D, Kearney R. Thoracic and lumbar epidural analgesia via the caudal approach using electrical stimulation guidance in pediatric patients: a review of 289 patients. Anesthesiology 2004; 100: 683-9.
Tsui BC, Gupta S, Finucane B. Detection of subarachnoid and intravascular epidural catheter placement. Can J Anesth 1999; 46: 675-8.
Tsui BC, Gupta S, Emery D, Finucane B. Detection of subdural placement of epidural catheter using nerve stimulation. Can J Anesth 2000; 47: 471-3.
Tsui BC, Wagner A, Finucane B. The threshold current in the intrathecal space to elicit motor response is lower and does not overlap that in the epidural space: a porcine model. Can J Anesth 2004; 51: 690-5.
Tsui BC, Wagner AM, Cunningham K, Perry S, Desai S, Seal R. Threshold current of an insulated needle in the intrathecal space in pediatric patients. Anesth Analg 2005; 100: 662-5.
Pither CE, Raj PP, Ford DJ. The use of peripheral nerve stimulators for regional anesthesia: a review of experimental characteristics, technique, and clinical applications. Reg Anesth Pain Med 1985; 10: 49-58.
Tsui BC. Atlas of Ultrasound and Nerve Stimulation-Guided Regional Anesthesia. New York, Springer; 2007: 9-18.
Hadzic A. Peripheral nerve stimulators: cracking the code-one at a time. Reg Anesth Pain Med 2004; 29: 185-8.
Financial support
This work was supported by a Clinical Scholar Award from the Alberta Heritage Foundation for Medical Research (AHFMR), a CAS/Abbott Laboratories Career Scientist Award from the Canadian Anesthesiologists’ Society, and a Canadian Institutes of Health Research (CIHR) Operating Grant to Ban Tsui.
Conflict of interest/other associations
Ban Tsui has a patent licensing agreement with PAJUNK® for the StimuLong SONO epidural kit.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Ban Tsui made substantial contributions to the conception and design of the study and the acquisition, analysis, and interpretation of data. Ban Tsui and Gareth Corry made substantial contributions to drafting the article and revising it critically for important intellectual content. Gareth Corry made contributions to the acquisition of data. Jeremy Tsui and Gareth Corry made contributions to the analysis and interpretation of data, and Jeremy Tsui contributed to the statistical analysis.
Rights and permissions
About this article
Cite this article
Tsui, B.C.H., Tsui, J.H. & Corry, G.N. Estimation of equivalent threshold currents using different pulse widths for the epidural stimulation test in a porcine model. Can J Anesth/J Can Anesth 61, 249–253 (2014). https://doi.org/10.1007/s12630-013-0096-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-013-0096-3