Abstract
Although over the last few decades, numerous attempts have been made to halt Alzheimer’s disease (AD) progression and mitigate its symptoms, only a few have been proven beneficial. Most medications available, still only cater to the symptoms of the disease rather than fixing the cause at the root level. A novel approach involving the use of miRNAs, which work on the principle of gene silencing, is being explored by scientists. Naturally present miRNAs in the biological system help to regulate various genes than may be implicated in AD-like BACE-1 and APP. One miRNA thus, holds the power to keep a check on several genes, conferring it the ability to be used as a multi-target therapeutic. With aging and the onset of diseased pathology, dysregulation of these miRNAs is observed. This flawed miRNA expression is responsible for the unusual buildup of amyloid proteins, fibrillation of tau proteins in the brain, neuronal death and other hallmarks leading to AD. The use of miRNA mimics and miRNA inhibitors provides an attractive perspective for fixing the upregulation and downregulation of miRNAs that led to abnormal cellular activities. Furthermore, the detection of miRNAs in the CSF and serum of diseased patients might be considered an earlier biomarker for the disease. While most of the therapies designed around AD have not succeeded completely, the targeting of dysregulated miRNAs in AD patients might give a new direction to scholars to develop an effective treatment for Alzheimer’s disease.
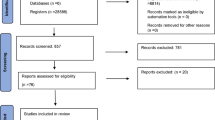
Graphical Abstract










Similar content being viewed by others
Data Availability
Not applicable.
References
Vacher MC, Durrant CS, Rose J, Hall AJ, Spires-Jones TL, Gunn-Moore F, Dagleish MP (2023) Alzheimer’s disease-like neuropathology in three species of oceanic dolphin. Eur J Neurosci 57:1161–1179. https://doi.org/10.1111/ejn.15900
Targa Dias Anastacio H, Matosin N, Ooi L (2022) Neuronal hyperexcitability in Alzheimer’s disease: what are the drivers behind this aberrant phenotype? Transl Psychiatry 12:1–14. https://doi.org/10.1038/s41398-022-02024-7
Risacher SL, Saykin AJ (2013) Neuroimaging and other biomarkers for Alzheimer’s disease: the changing landscape of early detection. Annu Rev Clin Psychol 9:621–648. https://doi.org/10.1146/annurev-clinpsy-050212-185535
Johnson KA, Fox NC, Sperling RA, Klunk WE (2012) Brain imaging in Alzheimer disease. Cold Spring Harb Perspect Med 2:a006213. https://doi.org/10.1101/cshperspect.a006213
Clément F, Belleville S (2009) Test–retest reliability of fMRI verbal episodic memory paradigms in healthy older adults and in persons with mild cognitive impairment. Hum Brain Mapp 30:4033–4047. https://doi.org/10.1002/hbm.20827
Putcha D, O’Keefe K, LaViolette P, O’Brien J, Greve D, Rentz DM, Locascio J, Atri A et al (2011) Reliability of functional magnetic resonance imaging associative encoding memory paradigms in non-demented elderly adults. Hum Brain Mapp 32:2027–2044. https://doi.org/10.1002/hbm.21166
Engler H, Forsberg A, Almkvist O, Blomquist G, Larsson E, Savitcheva I, Wall A, Ringheim A et al (2006) Two-year follow-up of amyloid deposition in patients with Alzheimer’s disease. Brain 129:2856–2866. https://doi.org/10.1093/brain/awl178
Cairns NJ, Ikonomovic MD, Benzinger T, Storandt M, Fagan AM, Shah AR, Reinwald LT, Carter D et al (2009) Absence of Pittsburgh compound B detection of cerebral amyloid β in a patient with clinical, cognitive, and cerebrospinal fluid markers of Alzheimer disease: a case report. Arch Neurol 66:1557–1562. https://doi.org/10.1001/archneurol.2009.279
Fabian MR, Sundermeier TR, Sonenberg N (2010) Understanding how miRNAs post-transcriptionally regulate gene expression. In: Rhoads RE (ed) miRNA Regulation of the Translational Machinery. Springer, Berlin, Heidelberg, pp 1–20
Bekris LM, Leverenz JB (2015) The biomarker and therapeutic potential of miRNA in Alzheimer’s disease. Neurodegener Dis Manag 5:61–74. https://doi.org/10.2217/nmt.14.52
Filipowicz W, Jaskiewicz L, Kolb FA, Pillai RS (2005) Post-transcriptional gene silencing by siRNAs and miRNAs. Curr Opin Struct Biol 15:331–341. https://doi.org/10.1016/j.sbi.2005.05.006
Moreno-Moya JM, Vilella F, Simón C (2014) MicroRNA: key gene expression regulators. Fertil Steril 101:1516–1523. https://doi.org/10.1016/j.fertnstert.2013.10.042
Putteeraj M, Fairuz YM, Teoh SL (2017) MicroRNA dysregulation in Alzheimer’s disease. CNS Neurol Disord - Drug Targets- CNS Neurol Disord 16:1000–1009. https://doi.org/10.2174/1871527316666170807142311
Schonrock N, Ke YD, Humphreys D, Staufenbiel M, Ittner LM, Preiss T, Götz J (2010) Neuronal MicroRNA deregulation in response to Alzheimer’s disease amyloid-β. PLOS ONE 5:e11070. https://doi.org/10.1371/journal.pone.0011070
Sun C, Liu J, Duan F, Cong L, Qi X (2021) The role of the microRNA regulatory network in Alzheimer’s disease: a bioinformatics analysis. Arch Med Sci 18:206–222. https://doi.org/10.5114/aoms/80619
Szweykowska-Kulińska Z, Jarmołowski A, Figlerowicz M (2003) RNA interference and its role in the regulation of eucaryotic gene expression. Acta Biochim Pol 50(217–229):035001217
Fire A, Xu S, Montgomery MK, Kostas SA, Driver SE, Mello CC (1998) Potent and specific genetic interference by double-stranded RNA in Caenorhabditis elegans. Nature 391:806–811. https://doi.org/10.1038/35888
Pushparaj PN, Aarthi JJ, Manikandan J, Kumar SD (2008) siRNA, miRNA, and shRNA: in vivo Applications. J Dent Res 87:992–1003. https://doi.org/10.1177/154405910808701109
Crick F (1970) Central dogma of molecular biology. Nature 227:561–563. https://doi.org/10.1038/227561a0
MacFarlane L-A, Murphy PR (2010) MicroRNA: biogenesis, function and role in cancer. Curr Genomics 11:537–561. https://doi.org/10.2174/138920210793175895
Li N, You X, Chen T, Mackowiak SD, Friedländer MR, Weigt M, Du H, Gogol-Döring A et al (2013) Global profiling of miRNAs and the hairpin precursors: insights into miRNA processing and novel miRNA discovery. Nucleic Acids Res 41:3619–3634. https://doi.org/10.1093/nar/gkt072
Han J, Lee Y, Yeom K-H, Kim Y-K, Jin H, Kim VN (2004) The drosha-DGCR8 complex in primary microRNA processing. Genes Dev 18:3016–3027. https://doi.org/10.1101/gad.1262504
Yi R, Qin Y, Macara IG, Cullen BR (2003) Exportin-5 mediates the nuclear export of pre-microRNAs and short hairpin RNAs. Genes Dev 17:3011–3016. https://doi.org/10.1101/gad.1158803
Arbuthnot P (2015) Chapter 2 - harnessing RNAi to silence viral gene expression. In: Arbuthnot P (ed) Gene Therapy for Viral Infections. Academic Press, Amsterdam, pp 29–61
Meng H, Wang Z, Wang Y, Zhu H, Huang B (2017) Dicer and Argonaute genes involved in RNA interference in the entomopathogenic fungus Metarhizium robertsii. Appl Environ Microbiol 83:e03230-e3316. https://doi.org/10.1128/AEM.03230-16
El-Sappah AH, Yan K, Huang Q, Islam MM, Li Q, Wang Y, Khan MS, Zhao X et al (2021) Comprehensive mechanism of gene silencing and its role in plant growth and development. Front Plant Sci 12. https://doi.org/10.3389/fpls.2021.705249
Choudhary S, Lee H-C, Maiti M, He Q, Cheng P, Liu Q, Liu Y (2007) A double-stranded-RNA response program important for RNA interference efficiency. Mol Cell Biol 27:3995–4005. https://doi.org/10.1128/MCB.00186-07
Savva YA, Rieder LE, Reenan RA (2012) The ADAR protein family. Genome Biol 13:252. https://doi.org/10.1186/gb-2012-13-12-252
Clark DP, Pazdernik NJ (2016) Chapter 5 - RNA-based technologies. In: Clark DP, Pazdernik NJ (eds) Biotechnology, 2nd edn. Academic Cell, Boston, pp 131–179
Sakurai K, Amarzguioui M, Kim D-H, Alluin J, Heale B, Song M, Gatignol A, Behlke MA et al (2011) A role for human dicer in pre-RISC loading of siRNAs. Nucleic Acids Res 39:1510–1525. https://doi.org/10.1093/nar/gkq846
Lam JKW, Chow MYT, Zhang Y, Leung SWS (2015) siRNA versus miRNA as therapeutics for gene silencing. Mol Ther - Nucleic Acids 4:e252. https://doi.org/10.1038/mtna.2015.23
Felekkis K, Touvana E, Stefanou C, Deltas C (2010) microRNAs: a newly described class of encoded molecules that play a role in health and disease. Hippokratia 14:236–240
Hamilton ML, Van Remmen H, Drake JA, Yang H, Guo ZM, Kewitt K, Walter CA, Richardson A (2001) Does oxidative damage to DNA increase with age? Proc Natl Acad Sci 98:10469–10474. https://doi.org/10.1073/pnas.171202698
Oliver CN, Ahn BW, Moerman EJ, Goldstein S, Stadtman ER (1987) Age-related changes in oxidized proteins. J Biol Chem 262:5488–5491. https://doi.org/10.1016/S0021-9258(18)45598-6
Kim GH, Kim JE, Rhie SJ, Yoon S (2015) The role of oxidative stress in neurodegenerative diseases. Exp Neurobiol 24:325–340. https://doi.org/10.5607/en.2015.24.4.325
Xu S, Zhang R, Niu J, Cui D, Xie B, Zhang B, Lu K, Yu W et al (2012) Oxidative stress mediated-alterations of the MicroRNA expression profile in mouse hippocampal neurons. Int J Mol Sci 13:16945–16960. https://doi.org/10.3390/ijms131216945
Dimmeler S, Nicotera P (2013) MicroRNAs in age-related diseases. EMBO Mol Med 5:180–190. https://doi.org/10.1002/emmm.201201986
de Lencastre A, Pincus Z, Zhou K, Kato M, Lee SS, Slack FJ (2010) MicroRNAs both promote and antagonize longevity in C. elegans. Curr Biol 20:2159–2168. https://doi.org/10.1016/j.cub.2010.11.015
Kato M, Chen X, Inukai S, Zhao H, Slack FJ (2011) Age-associated changes in expression of small, noncoding RNAs, including microRNAs, in C. elegans. RNA 17:1804–1820. https://doi.org/10.1261/rna.2714411
Williams J, Smith F, Kumar S, Vijayan M, Reddy PH (2017) Are microRNAs true sensors of ageing and cellular senescence? Ageing Res Rev 35:350–363. https://doi.org/10.1016/j.arr.2016.11.008
Tian M, Ding Y, Hou D, Deng Y, Li W, Feng X (2013) Real-time PCR for detecting differential expressions of microRNAs in the brain of a transgenic mouse model of Alzheimer’s disease. Nan Fang Yi Ke Da Xue Xue Bao 33:262–266
Hébert SS, Horré K, Nicolaï L, Papadopoulou AS, Mandemakers W, Silahtaroglu AN, Kauppinen S, Delacourte A et al (2008) Loss of microRNA cluster miR-29a/b-1 in sporadic Alzheimer’s disease correlates with increased BACE1/β-secretase expression. Proc Natl Acad Sci 105:6415–6420. https://doi.org/10.1073/pnas.0710263105
Stoicea N, Du A, Lakis DC, Tipton C, Arias-Morales CE, Bergese SD (2016) The MiRNA journey from theory to practice as a CNS biomarker. Front Genet 7:11. https://doi.org/10.3389/fgene.2016.00011
Cogswell JP, Ward J, Taylor IA, Waters M, Shi Y, Cannon B, Kelnar K, Kemppainen J et al (2008) Identification of miRNA changes in Alzheimer’s disease brain and CSF yields putative biomarkers and insights into disease pathways. J Alzheimer’s Dis 14:27–41. https://doi.org/10.3233/JAD-2008-14103
Hara N, Kikuchi M, Miyashita A, Hatsuta H, Saito Y, Kasuga K, Murayama S, Ikeuchi T et al (2017) Serum microRNA miR-501–3p as a potential biomarker related to the progression of Alzheimer’s disease. Acta Neuropathol Commun 5:10. https://doi.org/10.1186/s40478-017-0414-z
Gupta P, Bhattacharjee S, Sharma AR, Sharma G, Lee S-S, Chakraborty C (2017) miRNAs in Alzheimer disease – a therapeutic perspective. Curr Alzheimer Res 14:1198–1206. https://doi.org/10.2174/1567205014666170829101016
Catanesi M, d’Angelo M, Tupone MG, Benedetti E, Giordano A, Castelli V, Cimini A (2020) MicroRNAs dysregulation and mitochondrial dysfunction in neurodegenerative diseases. Int J Mol Sci 21:5986. https://doi.org/10.3390/ijms21175986
Bian S, Sun T (2011) Functions of noncoding RNAs in neural development and neurological diseases. Mol Neurobiol 44:359–373. https://doi.org/10.1007/s12035-011-8211-3
Reddy PH, Williams J, Smith F, Bhatti JS, Kumar S, Vijayan M, Kandimalla R, Kuruva CS et al (2017) Chapter Five - MicroRNAs, aging, cellular senescence, and Alzheimer’s disease. In: Reddy PH (ed) Progress in Molecular Biology and Translational Science. Academic Press, pp 127–171
Smith P, Al Hashimi A, Girard J, Delay C, Hébert SS (2011) In vivo regulation of amyloid precursor protein neuronal splicing by microRNAs. J Neurochem 116:240–247. https://doi.org/10.1111/j.1471-4159.2010.07097.x
Fang M, Wang J, Zhang X, Geng Y, Hu Z, Rudd JA, Ling S, Chen W et al (2012) The miR-124 regulates the expression of BACE1/β-secretase correlated with cell death in Alzheimer’s disease. Toxicol Lett 209:94–105. https://doi.org/10.1016/j.toxlet.2011.11.032
Geng L, Zhang T, Liu W, Chen Y (2018) KoreaMed synapse. Yonsei Med J 59:1096–1106. https://doi.org/10.3349/ymj.2018.59.9.1096
Ma X, Liu L, Meng J (2017) MicroRNA-125b promotes neurons cell apoptosis and Tau phosphorylation in Alzheimer’s disease. Neurosci Lett 661:57–62. https://doi.org/10.1016/j.neulet.2017.09.043
Wang G, Huang Y, Wang L-L, Zhang Y-F, Xu J, Zhou Y, Lourenco GF, Zhang B et al (2016) MicroRNA-146a suppresses ROCK1 allowing hyperphosphorylation of tau in Alzheimer’s disease. Sci Rep 6:26697. https://doi.org/10.1038/srep26697
Le D-H (2015) Network-based ranking methods for prediction of novel disease associated microRNAs. Comput Biol Chem 58:139–148. https://doi.org/10.1016/j.compbiolchem.2015.07.003
Abuelezz NZ, Nasr FE, AbdulKader MA, Bassiouny AR, Zaky A (2021) MicroRNAs as potential orchestrators of Alzheimer’s disease-related pathologies: insights on current status and future possibilities. Front Aging Neurosci 13:743573. https://doi.org/10.3389/fnagi.2021.743573
Cervellati C, Valacchi G, Zuliani G (2021) BACE1: from biomarker to Alzheimer’s disease therapeutical target. Aging (Albany NY) 13:12299–12300. https://doi.org/10.18632/aging.203064
Nygaard HB, van Dyck CH, Strittmatter SM (2014) Fyn kinase inhibition as a novel therapy for Alzheimer’s disease. Alz Res Ther 6:8. https://doi.org/10.1186/alzrt238
Harada H, Tamaoka A, Ishii K, Shoji S, Kametaka S, Kametani F, Saito Y, Murayama S (2006) Beta-site APP cleaving enzyme 1 (BACE1) is increased in remaining neurons in Alzheimer’s disease brains. Neurosci Res 54:24–29. https://doi.org/10.1016/j.neures.2005.10.001
De Pietri TD, Mihailovich M, Di Cesare A, Codazzi F, Grohovaz F, Zacchetti D (2004) Translational regulation of BACE-1 expression in neuronal and non-neuronal cells. Nucleic Acids Res 32:1808–1817. https://doi.org/10.1093/nar/gkh348
Strömberg K, Eketjäll S, Georgievska B, Tunblad K, Eliason K, Olsson F, Radesäter A-C, Klintenberg R et al (2015) Combining an amyloid-beta (Aβ) cleaving enzyme inhibitor with a γ-secretase modulator results in an additive reduction of Aβ production. FEBS J 282:65–73. https://doi.org/10.1111/febs.13103
Das B, Yan R (2017) Role of BACE1 in Alzheimer’s synaptic function. Transl Neurodegener 6:23. https://doi.org/10.1186/s40035-017-0093-5
Mosquera-Heredia MI, Morales LC, Vidal OM, Barceló E, Silvera-Redondo C, Vélez JI, Garavito-Galofre P (2021) Exosomes: potential disease biomarkers and new therapeutic targets. Biomedicines 9:1061. https://doi.org/10.3390/biomedicines9081061
Improta-Caria AC, Nonaka CKV, Cavalcante BRR, De Sousa RAL, Aras Júnior R, de F Souza BS (2020) Modulation of MicroRNAs as a potential molecular mechanism involved in the beneficial actions of physical exercise in Alzheimer disease. Int J Mol Sci 21:4977. https://doi.org/10.3390/ijms21144977
Amakiri N, Kubosumi A, Tran J, Reddy PH (2019) Amyloid beta and microRNAs in Alzheimer’s disease. Front Neurosci 13:430. https://doi.org/10.3389/fnins.2019.00430
Hébert SS, Horré K, Nicolaï L, Bergmans B, Papadopoulou AS, Delacourte A, De Strooper B (2009) MicroRNA regulation of Alzheimer’s amyloid precursor protein expression. Neurobiol Dis 33:422–428. https://doi.org/10.1016/j.nbd.2008.11.009
Miya Shaik M, Tamargo IA, Abubakar MB, Kamal MA, Greig NH, Gan SH (2018) The role of microRNAs in Alzheimer’s disease and their therapeutic potentials. Genes 9:174. https://doi.org/10.3390/genes9040174
Hampel H, Vassar R, De Strooper B, Hardy J, Willem M, Singh N, Zhou J, Yan R et al (2021) The β-secretase BACE1 in Alzheimer’s disease. Biol Psychiatry 89:745–756. https://doi.org/10.1016/j.biopsych.2020.02.001
Li Q, Li X, Wang L, Zhang Y, Chen L (2016) miR-98-5p acts as a target for Alzheimer’s disease by regulating Aβ production through modulating SNX6 expression. J Mol Neurosci 60:413–420. https://doi.org/10.1007/s12031-016-0815-7
Lei X, Lei L, Zhang Z, Zhang Z, Cheng Y (2015) Downregulated miR-29c correlates with increased BACE1 expression in sporadic Alzheimer’s disease. Int J Clin Exp Pathol 8:1565–1574
Faghihi MA, Zhang M, Huang J, Modarresi F, Van der Brug MP, Nalls MA, Cookson MR, St-Laurent G et al (2010) Evidence for natural antisense transcript-mediated inhibition of microRNA function. Genome Biol 11:R56. https://doi.org/10.1186/gb-2010-11-5-r56
Cole SL, Vassar R (2007) The Alzheimer’s disease β-secretase enzyme, BACE1. Mol Neurodegener 2:22. https://doi.org/10.1186/1750-1326-2-22
Wei Z, Zhou C, Liu M, Yao Y, Sun J, Xiao J, Ma W, Zhu H et al (2015) MicroRNA involvement in a metastatic non-functioning pituitary carcinoma. Pituitary 18:710–721. https://doi.org/10.1007/s11102-015-0648-3
Ardekani AM, Naeini MM (2010) The role of MicroRNAs in human diseases. Avicenna J Med Biotechnol 2:161–179
Parsi S, Smith PY, Goupil C, Dorval V, Hébert SS (2015) Preclinical evaluation of miR-15/107 family members as multifactorial drug targets for Alzheimer’s disease. Mol Ther - Nucleic Acids 4:e256. https://doi.org/10.1038/mtna.2015.33
Shu B, Zhang X, Du G, Fu Q, Huang L (2018) MicroRNA-107 prevents amyloid-β-induced neurotoxicity and memory impairment in mice. Int J Mol Med 41:1665–1672. https://doi.org/10.3892/ijmm.2017.3339
Junn E, Mouradian MM (2012) MicroRNAs in neurodegenerative diseases and their therapeutic potential. Pharmacol Ther 133:142–150. https://doi.org/10.1016/j.pharmthera.2011.10.002
Zhang M, Bian Z (2021) Alzheimer’s disease and microRNA-132: a widespread pathological factor and potential therapeutic target. Front Neurosci 15:687973. https://doi.org/10.3389/fnins.2021.687973
Wang M, Qin L, Tang B (2019) MicroRNAs in Alzheimer’s disease. Front Genet 10:153. https://doi.org/10.3389/fgene.2019.00153
Patel N, Hoang D, Miller N, Ansaloni S, Huang Q, Rogers JT, Lee JC, Saunders AJ (2008) MicroRNAs can regulate human APP levels. Mol Neurodegener 3:10. https://doi.org/10.1186/1750-1326-3-10
Long JM, Ray B, Lahiri DK (2012) MicroRNA-153 physiologically inhibits expression of amyloid-β precursor protein in cultured human fetal brain cells and is dysregulated in a subset of Alzheimer disease patients *. J Biol Chem 287:31298–31310. https://doi.org/10.1074/jbc.M112.366336
Boissonneault V, Plante I, Rivest S, Provost P (2009) MicroRNA-298 and microRNA-328 regulate expression of mouse β-amyloid precursor protein-converting enzyme 1 *. J Biol Chem 284:1971–1981. https://doi.org/10.1074/jbc.M807530200
Liang C, Zhu H, Xu Y, Huang L, Ma C, Deng W, Liu Y, Qin C (2012) MicroRNA-153 negatively regulates the expression of amyloid precursor protein and amyloid precursor-like protein 2. Brain Res 1455:103–113. https://doi.org/10.1016/j.brainres.2011.10.051
Kim J, Yoon H, Chung D, Brown JL, Belmonte KC, Kim J (2016) miR-186 is decreased in aged brain and suppresses BACE1 expression. J Neurochem 137:436–445. https://doi.org/10.1111/jnc.13507
Vilardo E, Barbato C, Ciotti M, Cogoni C, Ruberti F (2010) MicroRNA-101 regulates Amyloid precursor protein expression in hippocampal neurons *. J Biol Chem 285:18344–18351. https://doi.org/10.1074/jbc.M110.112664
Liu W, Liu C, Zhu J, Shu P, Yin B, Gong Y, Qiang B, Yuan J et al (2012) MicroRNA-16 targets amyloid precursor protein to potentially modulate Alzheimer’s-associated pathogenesis in SAMP8 mice. Neurobiol Aging 33:522–534. https://doi.org/10.1016/j.neurobiolaging.2010.04.034
Delay C, Mandemakers W, Hébert SS (2012) MicroRNAs in Alzheimer’s disease. Neurobiol Dis 46:285–290. https://doi.org/10.1016/j.nbd.2012.01.003
Fournier NM, Lee B, Banasr M, Elsayed M, Duman RS (2012) Vascular endothelial growth factor regulates adult hippocampal cell proliferation through MEK/ERK- and PI3K/Akt-dependent signaling. Neuropharmacology 63:642–652. https://doi.org/10.1016/j.neuropharm.2012.04.033
Albert-Gascó H, Ros-Bernal F, Castillo-Gómez E, Olucha-Bordonau FE (2020) MAP/ERK signaling in developing cognitive and emotional function and its effect on pathological and neurodegenerative processes. Int J Mol Sci 21:4471. https://doi.org/10.3390/ijms21124471
Hébert SS, Papadopoulou AS, Smith P, Galas M-C, Planel E, Silahtaroglu AN, Sergeant N, Buée L et al (2010) Genetic ablation of dicer in adult forebrain neurons results in abnormal tau hyperphosphorylation and neurodegeneration. Hum Mol Genet 19:3959–3969. https://doi.org/10.1093/hmg/ddq311
Lewohl JM, Nunez YO, Dodd PR, Tiwari GR, Harris RA, Mayfield RD (2011) Up-regulation of MicroRNAs in brain of human alcoholics. Alcohol: Clin Exp Res 35:1928–1937. https://doi.org/10.1111/j.1530-0277.2011.01544.x
Julien C, Tremblay C, Émond V, Lebbadi M, Salem N Jr, Bennett DA, Calon F (2009) Sirtuin 1 reduction parallels the accumulation of tau in Alzheimer disease. J Neuropathol Exp Neurol 68:48–58. https://doi.org/10.1097/NEN.0b013e3181922348
Yin X, Zhou Z, Qiu Y, Fan X, Zhao C, Bao J, Liu C, Liu F, Qian W (2021) SIRT1 regulates tau expression and tau synaptic pathology. J Alzheimer’s Dis 84:895–904. https://doi.org/10.3233/JAD-215118
Min S-W, Cho S-H, Zhou Y, Schroeder S, Haroutunian V, Seeley WW, Huang EJ, Shen Y et al (2010) Acetylation of tau inhibits its degradation and contributes to tauopathy. Neuron 67:953–966. https://doi.org/10.1016/j.neuron.2010.08.044
Burgos K, Malenica I, Metpally R, Courtright A, Rakela B, Beach T, Shill H, Adler C et al (2014) Profiles of extracellular miRNA in cerebrospinal fluid and serum from patients with Alzheimer’s and Parkinson’s diseases correlate with disease status and features of pathology. PLOS ONE 9:e94839. https://doi.org/10.1371/journal.pone.0094839
Li S, Yan Y, Jiao Y, Gao Z, Xia Y, Kong L, Yao Y, Tao Z et al (2016) Neuroprotective effect of osthole on neuron synapses in an Alzheimer’s disease cell model via upregulation of microRNA-9. J Mol Neurosci 60:71–81. https://doi.org/10.1007/s12031-016-0793-9
Smith PY, Hernandez-Rapp J, Jolivette F, Lecours C, Bisht K, Goupil C, Dorval V, Parsi S et al (2015) miR-132/212 deficiency impairs tau metabolism and promotes pathological aggregation in vivo. Hum Mol Genet 24:6721–6735. https://doi.org/10.1093/hmg/ddv377
Hadar A, Milanesi E, Walczak M, Puzianowska-Kuźnicka M, Kuźnicki J, Squassina A, Niola P, Chillotti C et al (2018) SIRT1, miR-132 and miR-212 link human longevity to Alzheimer’s Disease. Sci Rep 8:8465. https://doi.org/10.1038/s41598-018-26547-6
Sun Z-Z, Lv Z-Y, Tian W-J, Yang Y (2017) Retracted: microRNA-132 protects hippocampal neurons against oxygen-glucose deprivation–induced apoptosis. Int J Immunopathol Pharmacol 30:253–263. https://doi.org/10.1177/0394632017715837
Yao X, Xian X, Fang M, Fan S, Li W (2019) Loss of miR-369 promotes tau phosphorylation by targeting the fyn and serine/threonine-protein kinase 2 signaling pathways in Alzheimer’s disease mice. Front Aging Neurosci 11:365. https://doi.org/10.3389/fnagi.2019.00365
Liu W, Zhao J, Lu G (2016) miR-106b inhibits tau phosphorylation at Tyr18 by targeting Fyn in a model of Alzheimer’s disease. Biochem Biophys Res Commun 478:852–857. https://doi.org/10.1016/j.bbrc.2016.08.037
Wang H, Liu J, Zong Y, Xu Y, Deng W, Zhu H, Liu Y, Ma C et al (2010) miR-106b aberrantly expressed in a double transgenic mouse model for Alzheimer’s disease targets TGF-β type II receptor. Brain Res 1357:166–174. https://doi.org/10.1016/j.brainres.2010.08.023
Matrone C, Petrillo F, Nasso R, Ferretti G (2020) Fyn tyrosine kinase as harmonizing factor in neuronal functions and dysfunctions. Int J Mol Sci 21:4444. https://doi.org/10.3390/ijms21124444
Yan Y, Yan H, Teng Y, Wang Q, Yang P, Zhang L, Cheng H, Fu S (2020) Long non-coding RNA 00507/miRNA-181c-5p/TTBK1/MAPT axis regulates tau hyperphosphorylation in Alzheimer’s disease. J Gene Med 22:e3268. https://doi.org/10.1002/jgm.3268
Desikan RS, Schork AJ, Wang Y, Witoelar A, Sharma M, McEvoy LK, Holland D, Brewer JB et al (2015) Genetic overlap between Alzheimer’s disease and Parkinson’s disease at the MAPT locus. Mol Psychiatry 20:1588–1595. https://doi.org/10.1038/mp.2015.6
Salta E, De Strooper B (2017) Noncoding RNAs in neurodegeneration. Nat Rev Neurosci 18:627–640. https://doi.org/10.1038/nrn.2017.90
Tomasello L, Cluts L, Croce CM (2019) Experimental validation of microRNA targets: luciferase reporter assay. In: Laganà A (ed) MicroRNA Target Identification: Methods and Protocols. Springer, New York, NY, pp 315–330
Bartel DP, Chen C-Z (2004) Micromanagers of gene expression: the potentially widespread influence of metazoan microRNAs. Nat Rev Genet 5:396–400. https://doi.org/10.1038/nrg1328
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116:281–297. https://doi.org/10.1016/S0092-8674(04)00045-5
Michaels YS, Barnkob MB, Barbosa H, Baeumler TA, Thompson MK, Andre V, Colin-York H, Fritzsche M et al (2019) Precise tuning of gene expression levels in mammalian cells. Nat Commun 10:818. https://doi.org/10.1038/s41467-019-08777-y
Rybak-Wolf A, Plass M (2021) RNA dynamics in Alzheimer’s disease. Molecules 26:5113. https://doi.org/10.3390/molecules26175113
Skeparnias I, Zhang J (2021) Cooperativity and Interdependency between RNA Structure and RNA–RNA Interactions. Non-Coding RNA 7:81. https://doi.org/10.3390/ncrna7040081
Cech TR, Steitz JA (2014) The noncoding RNA revolution—trashing old rules to forge new ones. Cell 157:77–94. https://doi.org/10.1016/j.cell.2014.03.008
Yao RW, Wang Y, Chen LL (2019) Cellular functions of long noncoding RNAs. Nat Cell Biol 21(5):542–551. https://doi.org/10.1038/s41556-019-0311-8
Grosjean H, Westhof E (2016) An integrated, structure- and energy-based view of the genetic code. Nucleic Acids Res 44:8020–8040. https://doi.org/10.1093/nar/gkw608
Hum C, Loiselle J, Ahmed N, Shaw TA, Toudic C, Pezacki JP (2021) MicroRNA mimics or inhibitors as antiviral therapeutic approaches against COVID-19. Drugs 81(5):517–531. https://doi.org/10.1007/s40265-021-01474-5
Gallant-Behm CL, Piper J, Lynch JM, Seto AG, Hong SJ, Mustoe TA, Maari C, Pestano LA et al (2019) A microRNA-29 mimic (Remlarsen) represses extracellular matrix expression and fibroplasia in the skin. J Investig Dermatol 139:1073–1081. https://doi.org/10.1016/j.jid.2018.11.007
Seto AG, Beatty X, Lynch JM, Hermreck M, Tetzlaff M, Duvic M, Jackson AL (2018) Cobomarsen, an oligonucleotide inhibitor of miR-155, co-ordinately regulates multiple survival pathways to reduce cellular proliferation and survival in cutaneous T-cell lymphoma. Br J Haematol 183:428–444. https://doi.org/10.1111/bjh.15547
van Rooji E, Kauppinen S (2014) Development of microRNA therapeutics is coming of age. EMBO Mol Med 6:851–864. https://doi.org/10.15252/emmm.201100899
Ibáñez-Ventoso C, Yang M, Guo S, Robins H, Padgett RW, Driscoll M (2006) Modulated microRNA expression during adult lifespan in Caenorhabditis elegans. Aging Cell 5:235–246. https://doi.org/10.1111/j.1474-9726.2006.00210.x
Wang Z (2011) The guideline of the design and validation of miRNA mimics. In: Wu W (ed) MicroRNA and Cancer: Methods and Protocols. Humana Press, Totowa, NJ, pp 211–223
Zhang Q-S, Liu W, Lu G-X (2017) miR-200a-3p promotes β-Amyloid-induced neuronal apoptosis through down-regulation of SIRT1 in Alzheimer’s disease. J Biosci 42:397–404. https://doi.org/10.1007/s12038-017-9698-1
Lei Y, Jin X, Sun M, Ji Z (2021) miR-129-5p ameliorates ischemic brain injury by binding to SIAH1 and activating the mTOR signaling pathway. J Mol Neurosci 71:1761–1771. https://doi.org/10.1007/s12031-021-01872-0
Barros-Viegas AT, Carmona V, Ferreiro E, Guedes J, Cardoso AM, Cunha P, Pereira de Almeida L, Resende de Oliveira C et al (2020) miRNA-31 improves cognition and abolishes amyloid-β pathology by targeting APP and BACE1 in an animal model of Alzheimer’s disease. Mol Ther - Nucleic Acids 19:1219–1236. https://doi.org/10.1016/j.omtn.2020.01.010
Yue J (2011) miRNA and vascular cell movement. Adv Drug Deliv Rev 63:616–622. https://doi.org/10.1016/j.addr.2011.01.001
Wei W, Wang Z-Y, Ma L-N, Zhang T-T, Cao Y, Li H (2020) MicroRNAs in Alzheimer’s disease: function and potential applications as diagnostic biomarkers. Front Mol Neurosci 13:160. https://doi.org/10.3389/fnmol.2020.00160
O’Brien J, Hayder H, Zayed Y, Peng C (2018) Overview of microRNA biogenesis, mechanisms of actions, and circulation. Front Endocrinol (Lausanne) 9:402. https://doi.org/10.3389/fendo.2018.00402
Krek A, Grün D, Poy MN, Wolf R, Rosenberg L, Epstein EJ, MacMenamin P, da Piedade I et al (2005) Combinatorial microRNA target predictions. Nat Genet 37:495–500. https://doi.org/10.1038/ng1536
Wu S, Huang S, Ding J, Zhao Y, Liang L, Liu T, Zhan R, He X (2010) Multiple microRNAs modulate p21Cip1/Waf1 expression by directly targeting its 3′ untranslated region. Oncogene 29:2302–2308. https://doi.org/10.1038/onc.2010.34
Juźwik CA, S Drake S, Zhang Y, Paradis-Isler N, Sylvester A, Amar-Zifkin A, Douglas C, Morquette B et al (2019) microRNA dysregulation in neurodegenerative diseases: a systematic review. Prog Neurobiol 182:101664. https://doi.org/10.1016/j.pneurobio.2019.101664
Soreq H, Wolf Y (2011) NeurimmiRs: microRNAs in the neuroimmune interface. Trends Mol Med 17:548–555. https://doi.org/10.1016/j.molmed.2011.06.009
Peter ME (2010) Targeting of mRNAs by multiple miRNAs: the next step. Oncogene 29:2161–2164. https://doi.org/10.1038/onc.2010.59
Klein ME, Lioy DT, Ma L, Impey S, Mandel G, Goodman RH (2007) Homeostatic regulation of MeCP2 expression by a CREB-induced microRNA. Nat Neurosci 10:1513–1514. https://doi.org/10.1038/nn2010
Vo N, Klein ME, Varlamova O, Keller DM, Yamamoto T, Goodman RH, Impey S (2005) A cAMP-response element binding protein-induced microRNA regulates neuronal morphogenesis. Proc Natl Acad Sci 102:16426–16431. https://doi.org/10.1073/pnas.0508448102
Mellios N, Sugihara H, Castro J, Banerjee A, Le C, Kumar A, Crawford B, Strathmann J et al (2011) miR-132, an experience-dependent microRNA, is essential for visual cortex plasticity. Nat Neurosci 14:1240–1242. https://doi.org/10.1038/nn.2909
El Fatimy R, Li S, Chen Z, Mushannen T, Gongala S, Wei Z, Balu DT, Rabinovsky R et al (2018) MicroRNA-132 provides neuroprotection for tauopathies via multiple signaling pathways. Acta Neuropathol 136:537–555. https://doi.org/10.1007/s00401-018-1880-5
Salta E, De Strooper B (2017) microRNA-132: a key noncoding RNA operating in the cellular phase of Alzheimer’s disease. FASEB J 31:424–433. https://doi.org/10.1096/fj.201601308
Walgrave H, Balusu S, Snoeck S, Vanden Eynden E, Craessaerts K, Thrupp N, Wolfs L, Horré K et al (2021) Restoring miR-132 expression rescues adult hippocampal neurogenesis and memory deficits in Alzheimer’s disease. Cell Stem Cell 28:1805-1821.e8. https://doi.org/10.1016/j.stem.2021.05.001
Nahid MA, Yao B, Dominguez-Gutierrez PR, Kesavalu L, Satoh M, Chan EKL (2013) Regulation of TLR2-mediated tolerance and cross-tolerance through IRAK4 modulation by miR-132 and miR-212. J Immunol 190:1250–1263. https://doi.org/10.4049/jimmunol.1103060
Kong H, Yin F, He F, Omran A, Li L, Wu T, Wang Y, Peng J (2015) The effect of miR-132, miR-146a, and miR-155 on MRP8/TLR4-induced astrocyte-related inflammation. J Mol Neurosci 57:28–37. https://doi.org/10.1007/s12031-015-0574-x
Shaked I, Meerson A, Wolf Y, Avni R, Greenberg D, Gilboa-Geffen A, Soreq H (2009) MicroRNA-132 potentiates cholinergic anti-inflammatory signaling by targeting acetylcholinesterase. Immunity 31:965–973. https://doi.org/10.1016/j.immuni.2009.09.019
Deng Y, Zhang J, Sun X, Ma G, Luo G, Miao Z, Song L (2020) miR-132 improves the cognitive function of rats with Alzheimer’s disease by inhibiting the MAPK1 signal pathway. Exp Ther Med 20:1–1. https://doi.org/10.3892/etm.2020.9288
Wang Y, Veremeyko T, Wong AH-K, El Fatimy R, Wei Z, Cai W, Krichevsky AM (2017) Downregulation of miR-132/212 impairs S-nitrosylation balance and induces tau phosphorylation in Alzheimer’s disease. Neurobiol Aging 51:156–166. https://doi.org/10.1016/j.neurobiolaging.2016.12.015
Hernandez-Rapp J, Rainone S, Goupil C, Dorval V, Smith PY, Saint-Pierre M, Vallée M, Planel E et al (2016) microRNA-132/212 deficiency enhances Aβ production and senile plaque deposition in Alzheimer’s disease triple transgenic mice. Sci Rep 6:30953. https://doi.org/10.1038/srep30953
Salta E, Sierksma A, Vanden-Eynden E, De Strooper B (2016) miR-132 loss de-represses ITPKB and aggravates amyloid and TAU pathology in Alzheimer’s brain. EMBO Mol Med 8:1005–1018. https://doi.org/10.15252/emmm.201606520
Wong H-KA, Veremeyko T, Patel N, Lemere CA, Walsh DM, Esau C, Vanderburg C, Krichevsky AM (2013) De-repression of FOXO3a death axis by microRNA-132 and -212 causes neuronal apoptosis in Alzheimer’s disease. Hum Mol Genet 22:3077–3092. https://doi.org/10.1093/hmg/ddt164
Gromova M, Vaggelas A, Dallmann G, Seimetz D (2020) Biomarkers: opportunities and challenges for drug development in the current regulatory landscape. Biomark Insights 15:1177271920974652. https://doi.org/10.1177/1177271920974652
Pradeepkiran JA, Reddy PH (2021) Phosphorylated tau targeted small-molecule PROTACs for the treatment of Alzheimer’s disease and tauopathies. Biochim Biophys Acta (BBA) - Mol Basis Dis 1867:166162. https://doi.org/10.1016/j.bbadis.2021.166162
Nielsen MS, Simonsen AH, Siersma V, Hasselbalch SG, Høgh P (2016) Are CSF biomarkers useful as prognostic indicators in diagnostically unresolved cognitively impaired patients in a normal clinical setting. DEE 6:465–476. https://doi.org/10.1159/000449410
Blennow K, Dubois B, Fagan AM, Lewczuk P, de Leon MJ, Hampel H (2015) Clinical utility of cerebrospinal fluid biomarkers in the diagnosis of early Alzheimer’s disease. Alzheimer’s Dement 11:58–69. https://doi.org/10.1016/j.jalz.2014.02.004
Kiko T, Nakagawa K, Tsuduki T, Furukawa K, Arai H, Miyazawa T (2014) MicroRNAs in Plasma and Cerebrospinal Fluid as Potential Markers for Alzheimer’s Disease. J Alzheimer’s Dis 39:253–259. https://doi.org/10.3233/JAD-130932
Wu HZY, Ong KL, Seeher K, Armstrong NJ, Thalamuthu A, Brodaty H, Sachdev P, Mather K (2016) Circulating microRNAs as biomarkers of Alzheimer’s disease: a systematic review. J Alzheimer’s Dis 49:755–766. https://doi.org/10.3233/JAD-150619
Precazzini F, Detassis S, Imperatori AS, Denti MA, Campomenosi P (2021) Measurements methods for the development of microRNA-based tests for cancer diagnosis. Int J Mol Sci 22:1176. https://doi.org/10.3390/ijms22031176
Wiedrick JT, Phillips JI, Lusardi TA, McFarland TJ, Lind B, Sandau US, Harrington CA, Lapidus JA et al (2019) Validation of microRNA biomarkers for Alzheimer’s disease in human cerebrospinal fluid. J Alzheimer’s Dis 67:875–891. https://doi.org/10.3233/JAD-180539
Takousis P, Sadlon A, Schulz J, Wohlers I, Dobricic V, Middleton L, Lill CM, Perneczky R et al (2019) Differential expression of microRNAs in Alzheimer’s disease brain, blood, and cerebrospinal fluid. Alzheimer’s Dement 15:1468–1477. https://doi.org/10.1016/j.jalz.2019.06.4952
Shu J, Silva BVRE, Gao T, Xu Z, Cui J (2017) Dynamic and modularized microRNA regulation and its implication in human cancers. Sci Rep 7:13356. https://doi.org/10.1038/s41598-017-13470-5
He B, Zhao Z, Cai Q, Zhang Y, Zhang P, Shi S, Xie H, Peng X et al (2020) miRNA-based biomarkers, therapies, and resistance in Cancer. Int J Biol Sci 16:2628–2647. https://doi.org/10.7150/ijbs.47203
Sørensen SS, Nygaard A-B, Christensen T (2016) miRNA expression profiles in cerebrospinal fluid and blood of patients with Alzheimer’s disease and other types of dementia – an exploratory study. Transl Neurodegener 5:6. https://doi.org/10.1186/s40035-016-0053-5
Kaur P, Armugam A, Jeyaseelan K (2012) MicroRNAs in neurotoxicity. J Toxicol 2012:e870150. https://doi.org/10.1155/2012/870150
Ma Y-H, Deng W-J, Luo Z-Y, Jing J, Pan P-W, Yao Y-B, Fang Y-B, Teng J-F (2021) Inhibition of microRNA-29b suppresses oxidative stress and reduces apoptosis in ischemic stroke. Neural Regen Res 17:433–439. https://doi.org/10.4103/1673-5374.314319
Butterfield DA, Swomley AM, Sultana R (2013) Amyloid β-Peptide (1–42)-Induced oxidative stress in Alzheimer disease: importance in disease pathogenesis and progression. Antioxid Redox Signal 19:823–835. https://doi.org/10.1089/ars.2012.5027
Sano T, Reynolds JP, Jimenez-Mateos EM, Matsushima S, Taki W, Henshall DC (2012) MicroRNA-34a upregulation during seizure-induced neuronal death. Cell Death Dis 3:e287–e287. https://doi.org/10.1038/cddis.2012.23
Zhan-Qiang H, Hai-Hua Q, Chi Z, Miao W, Cui Z, Zi-Yin L, Jing H, Yi-Wei W (2021) miR-146a aggravates cognitive impairment and Alzheimer disease-like pathology by triggering oxidative stress through MAPK signaling. Neurologia (Engl Ed) S0213–4853(21):00022. https://doi.org/10.1016/j.nrl.2020.12.006
Nunomura A, Perry G (2020) RNA and oxidative stress in Alzheimer’s disease: focus on microRNAs. Oxidative Medicine and Cellular Longevity 2020:e2638130. https://doi.org/10.1155/2020/2638130
Liu C, Wang J, Li L, Xue L, Zhang Y, Wang P (2014) MicroRNA-135a and -200b, potential biomarkers for Alzheimer׳s disease, regulate β secretase and amyloid precursor protein. Brain Res 1583:55–64. https://doi.org/10.1016/j.brainres.2014.04.026
van Leuven F (2000) Single and multiple transgenic mice as models for Alzheimer’s disease. Prog Neurobiol 61:305–312. https://doi.org/10.1016/s0301-0082(99)00055-6
Herrera-Espejo S, Santos-Zorrozua B, Álvarez-González P, Lopez-Lopez E, Garcia-Orad Á (2019) A systematic review of microRNA expression as biomarker of late-onset Alzheimer’s Disease. Mol Neurobiol 56:8376–8391. https://doi.org/10.1007/s12035-019-01676-9
Swarbrick S, Wragg N, Ghosh S, Stolzing A (2019) Systematic review of mirna as biomarkers in Alzheimer’s disease. Mol Neurobiol 56:6156–6167. https://doi.org/10.1007/s12035-019-1500-y
Cha DJ, Mengel D, Mustapic M, Liu W, Selkoe DJ, Kapogiannis D, Galasko D, Rissman RA et al (2019) miR-212 and miR-132 are downregulated in neurally derived plasma exosomes of Alzheimer’s patients. Front Neurosci 13:1208. https://doi.org/10.3389/fnins.2019.01208
Denk J, Oberhauser F, Kornhuber J, Wiltfang J, Fassbender K, Schroeter ML, Volk AE, Diehl-Schmid J et al (2018) Specific serum and CSF microRNA profiles distinguish sporadic behavioural variant of frontotemporal dementia compared with Alzheimer patients and cognitively healthy controls. PLOS ONE 13:e0197329. https://doi.org/10.1371/journal.pone.0197329
Sheinerman KS, Tsivinsky VG, Abdullah L, Crawford F, Umansky SR (2013) Plasma microRNA biomarkers for detection of mild cognitive impairment: biomarker validation study. Aging 5:925–938. https://doi.org/10.18632/aging.100624
Cheng L, Doecke JD, Sharples RA, Villemagne VL, Fowler CJ, Rembach A, Martins RN, Rowe CC et al (2015) Prognostic serum miRNA biomarkers associated with Alzheimer’s disease shows concordance with neuropsychological and neuroimaging assessment. Mol Psychiatry 20:1188–1196. https://doi.org/10.1038/mp.2014.127
Kumar P, Dezso Z, MacKenzie C, Oestreicher J, Agoulnik S, Byrne M, Bernier F, Yanagimachi M et al (2013) Circulating miRNA biomarkers for Alzheimer’s disease. PLOS ONE 8:e69807. https://doi.org/10.1371/journal.pone.0069807
Lusardi TA, Phillips JI, Wiedrick JT, Harrington CA, Lind B, Lapidus JA, Quinn JF, Saugstad JA (2017) MicroRNAs in human cerebrospinal fluid as biomarkers for Alzheimer’s disease. J Alzheimer’s Dis 55:1223–1233. https://doi.org/10.3233/JAD-160835
Anoop A, Singh PK, Jacob RS, Maji SK (2010) CSF biomarkers for Alzheimer’s disease diagnosis. Int J Alzheimer’s Dis 2010:e606802. https://doi.org/10.4061/2010/606802
Serpente M, Fenoglio C, D’Anca M, Arcaro M, Sorrentino F, Visconte C, Arighi A, Fumagalli GG et al (2020) MiRNA profiling in plasma neural-derived small extracellular vesicles from patients with Alzheimer’s disease. Cells 9:1443. https://doi.org/10.3390/cells9061443
Gurunathan S, Kang M-H, Jeyaraj M, Qasim M, Kim J-H (2019) Review of the isolation, characterization, biological function, and multifarious therapeutic approaches of exosomes. Cells 8:307. https://doi.org/10.3390/cells8040307
Masyuk AI, Masyuk TV, LaRusso NF (2013) Exosomes in the pathogenesis, diagnostics and therapeutics of liver diseases. J Hepatol 59:621–625. https://doi.org/10.1016/j.jhep.2013.03.028
Hannafon BN, Ding W-Q (2013) Intercellular communication by exosome-derived micrornas in cancer. Int J Mol Sci 14:14240–14269. https://doi.org/10.3390/ijms140714240
Vella LJ, Sharples RA, Nisbet RM, Cappai R, Hill AF (2008) The role of exosomes in the processing of proteins associated with neurodegenerative diseases. Eur Biophys J 37:323–332. https://doi.org/10.1007/s00249-007-0246-z
Vella LJ, Hill AF, Cheng L (2016) Focus on extracellular vesicles: exosomes and their role in protein trafficking and biomarker potential in Alzheimer’s and Parkinson’s disease. Int J Mol Sci 17:173. https://doi.org/10.3390/ijms17020173
Kapogiannis D, Boxer A, Schwartz JB, Abner EL, Biragyn A, Masharani U, Frassetto L, Petersen RC et al (2015) Dysfunctionally phosphorylated type 1 insulin receptor substrate in neural-derived blood exosomes of preclinical Alzheimer’s disease. FASEB J 29:589–596. https://doi.org/10.1096/fj.14-262048
Goetzl EJ, Boxer A, Schwartz JB, Abner EL, Petersen RC, Miller BL, Kapogiannis D (2015) Altered lysosomal proteins in neural-derived plasma exosomes in preclinical Alzheimer disease. Neurology 85:40–47. https://doi.org/10.1212/WNL.0000000000001702
Goetzl EJ, Boxer A, Schwartz JB, Abner EL, Petersen RC, Miller BL, Carlson OD, Mustapic M et al (2015) Low neural exosomal levels of cellular survival factors in Alzheimer’s disease. Ann Clin Transl Neurol 2:769–773. https://doi.org/10.1002/acn3.211
Yin Q, Ji X, Lv R, Pei J-J, Du Y, Shen C, Hou X (2020) Targetting exosomes as a new biomarker and therapeutic approach for Alzheimer’s disease. Clin Interv Aging 15:195–205. https://doi.org/10.2147/CIA.S240400
Lee S, Mankhong S, Kang J-H (2019) Extracellular vesicle as a source of Alzheimer’s biomarkers: opportunities and challenges. Int J Mol Sci 20:1728. https://doi.org/10.3390/ijms20071728
Lugli G, Cohen AM, Bennett DA, Shah RC, Fields CJ, Hernandez AG, Smalheiser NR (2015) Plasma exosomal miRNAs in persons with and without Alzheimer disease: altered expression and prospects for biomarkers. PLOS ONE 10:e0139233. https://doi.org/10.1371/journal.pone.0139233
Schneider R, McKeever P, Kim T, Graff C, van Swieten JC, Karydas A, Boxer A, Rosen H et al (2018) Downregulation of exosomal miR-204-5p and miR-632 as a biomarker for FTD: a GENFI study. J Neurol Neurosurg Psychiatry 89:851–858. https://doi.org/10.1136/jnnp-2017-317492
Wei H, Xu Y, Xu W, Zhou Q, Chen Q, Yang M, Feng F, Liu Y et al (2018) Serum exosomal miR-223 serves as a potential diagnostic and prognostic biomarker for dementia. Neuroscience 379:167–176. https://doi.org/10.1016/j.neuroscience.2018.03.016
Goetzl EJ, Mustapic M, Kapogiannis D, Eitan E, Lobach IV, Goetzl L, Schwartz JB, Miller BL (2016) Cargo proteins of plasma astrocyte-derived exosomes in Alzheimer’s disease. FASEB J 30:3853–3859. https://doi.org/10.1096/fj.201600756R
Kapogiannis D, Mustapic M, Shardell MD, Berkowitz ST, Diehl TC, Spangler RD, Tran J, Lazaropoulos MP et al (2019) Association of extracellular vesicle biomarkers with Alzheimer disease in the baltimore longitudinal study of aging. JAMA Neurol 76:1340–1351. https://doi.org/10.1001/jamaneurol.2019.2462
Kim KM, Meng Q, Perez de Acha O, Mustapic M, Cheng A, Eren E, Kundu G, Piao Y et al (2020) Mitochondrial RNA in Alzheimer’s disease circulating extracellular vesicles. Front Cell Dev Biol 8:581882. https://doi.org/10.3389/fcell.2020.581882
Vidal L, Blagden S, Attard G, de Bono J (2005) Making sense of antisense. Eur J Cancer 41:2812–2818. https://doi.org/10.1016/j.ejca.2005.06.029
Jackson AL, Burchard J, Schelter J, Chau BN, Cleary M, Lim L, Linsley PS (2006) Widespread siRNA “off-target” transcript silencing mediated by seed region sequence complementarity. RNA 12:1179–1187. https://doi.org/10.1261/rna.25706
Birmingham A, Anderson EM, Reynolds A, Ilsley-Tyree D, Leake D, Fedorov Y, Baskerville S, Maksimova E et al (2006) 3’ UTR seed matches, but not overall identity, are associated with RNAi off-targets. Nat Methods 3:199–204. https://doi.org/10.1038/nmeth854
Fedorov Y, Anderson EM, Birmingham A, Reynolds A, Karpilow J, Robinson K, Leake D, Marshall WS et al (2006) Off-target effects by siRNA can induce toxic phenotype. RNA 12:1188–1196. https://doi.org/10.1261/rna.28106
Grimm D, Streetz KL, Jopling CL, Storm TA, Pandey K, Davis CR, Marion P, Salazar F et al (2006) Fatality in mice due to oversaturation of cellular microRNA/short hairpin RNA pathways. Nature 441:537–541. https://doi.org/10.1038/nature04791
Liu Z, Sall A, Yang D (2008) MicroRNA: an emerging therapeutic target and intervention tool. Int J Mol Sci 9:978–999. https://doi.org/10.3390/ijms9060978
McCall R, Miles M, Lascuna P, Burney B, Patel Z, Sidoran KJ, Sittaramane V, Kocerha J et al (2017) Dual targeting of the cancer antioxidant network with 1,4-naphthoquinone fused Gold( i ) N-heterocyclic carbene complexes. Chem Sci 8:5918–5929. https://doi.org/10.1039/C7SC02153D
Hopkins AL (2008) Network pharmacology: the next paradigm in drug discovery. Nat Chem Biol 4:682–690. https://doi.org/10.1038/nchembio.118
Kumar S, Vijayan M, Bhatti JS, Reddy PH (2017) Chapter three - microRNAs as peripheral biomarkers in aging and age-related diseases. In: Reddy PH (ed) Progress in Molecular Biology and Translational Science. Academic Press, pp 47–94
Condrat CE, Thompson DC, Barbu MG, Bugnar OL, Boboc A, Cretoiu D, Suciu N, Cretoiu SM et al (2020) miRNAs as biomarkers in disease: latest findings regarding their role in diagnosis and prognosis. Cells 9:276. https://doi.org/10.3390/cells9020276
McKeever PM, Schneider R, Taghdiri F, Weichert A, Multani N, Brown RA, Boxer AL, Karydas A et al (2018) MicroRNA expression levels are altered in the cerebrospinal fluid of patients with young-onset Alzheimer’s disease. Mol Neurobiol 55:8826–8841. https://doi.org/10.1007/s12035-018-1032-x
Bhatnagar S, Chertkow H, Schipper HM, Yuan Z, Shetty V, Jenkins S, Jones T, Wang E (2014) Increased microRNA-34c abundance in Alzheimer’s disease circulating blood plasma. Front Mol Neurosci 7:2. https://doi.org/10.3389/fnmol.2014.00002
Cosín-Tomás M, Antonell A, Lladó A, Alcolea D, Fortea J, Ezquerra M, Lleó A, Martí MJ et al (2017) Plasma miR-34a-5p and miR-545-3p as early biomarkers of Alzheimer’s disease: potential and limitations. Mol Neurobiol 54:5550–5562. https://doi.org/10.1007/s12035-016-0088-8
Wang T, Chen K, Li H, Dong S, Su N, Liu Y, Cheng Y, Dai J et al (2015) The feasibility of utilizing plasma <em>MiRNA107</em> and <em>BACE1</em> messenger RNA gene expression for clinical diagnosis of amnestic mild cognitive impairment. J Clin Psychiatry 76:7223. https://doi.org/10.4088/JCP.13m08812
Moncini S, Lunghi M, Valmadre A, Grasso M, Del Vescovo V, Riva P, Denti MA, Venturin M (2017) The miR-15/107 family of microRNA genes regulates CDK5R1/p35 with Implications for Alzheimer’s disease pathogenesis. Mol Neurobiol 54:4329–4342. https://doi.org/10.1007/s12035-016-0002-4
Müller M, Kuiperij HB, Versleijen AAM, Chiasserini D, Farotti L, Baschieri F, Parnetti L, Struyfs H et al (2016) Validation of microRNAs in cerebrospinal fluid as biomarkers for different forms of dementia in a multicenter study. J Alzheimer’s Dis 52:1321–1333. https://doi.org/10.3233/JAD-160038
Git A, Dvinge H, Salmon-Divon M, Osborne M, Kutter C, Hadfield J, Bertone P, Caldas C (2010) Systematic comparison of microarray profiling, real-time PCR, and next-generation sequencing technologies for measuring differential microRNA expression. RNA 16:991–1006. https://doi.org/10.1261/rna.1947110
Wang J, Chen J, Sen S (2016) MicroRNA as biomarkers and diagnostics. J Cell Physiol 231:25–30. https://doi.org/10.1002/jcp.25056
Bader AG, Brown D, Stoudemire J, Lammers P (2011) Developing therapeutic microRNAs for cancer. Gene Ther 18:1121–1126. https://doi.org/10.1038/gt.2011.79
Martinez B, Peplow PV (2019) MicroRNAs as diagnostic and therapeutic tools for Alzheimer’s disease: advances and limitations. Neural Regen Res 14:242–255. https://doi.org/10.4103/1673-5374.244784
Eikmans M, Rekers NV, Anholts JDH, Heidt S, Claas FHJ (2013) Blood cell mRNAs and microRNAs: optimized protocols for extraction and preservation. Blood 121:e81–e89. https://doi.org/10.1182/blood-2012-06-438887
Yoon H, Belmonte KC, Kasten T, Bateman R, Kim J (2017) Intra- and inter-individual variability of microRNA levels in human cerebrospinal fluid: critical implications for biomarker discovery. Sci Rep 7:12720. https://doi.org/10.1038/s41598-017-13031-w
Gustafson D, Tyryshkin K, Renwick N (2016) microRNA-guided diagnostics in clinical samples. Best Pract Res Clin Endocrinol Metab 30:563–575. https://doi.org/10.1016/j.beem.2016.07.002
Shi D, Han M, Liu W, Tao J, Chen L (2020) Circulating microRNAs as diagnostic biomarkers of clinical cognitive impairment: a meta-analysis. Am J Alzheimers Dis Other Demen 35:1533317520951686. https://doi.org/10.1177/1533317520951686
Rawlings-Goss R, Campbell M, Tishkoff S (2014) Global population-specific variation in miRNA associated with cancer risk and clinical biomarkers. BMC Med Genomics 7:53. https://doi.org/10.1186/1755-8794-7-53
Chiu Y-L, Rana TM (2003) siRNA function in RNAi: a chemical modification analysis. RNA 9:1034–1048. https://doi.org/10.1261/rna.5103703
Harborth J, Elbashir SM, Vandenburgh K, Manninga H, Scaringe SA, Weber K, Tuschl T (2003) Sequence, chemical, and structural variation of small interfering RNAs and short hairpin RNAs and the effect on mammalian gene silencing. Antisense Nucleic Acid Drug Dev 13:83–105. https://doi.org/10.1089/108729003321629638
Rupaimoole R, Han H-D, Lopez-Berestein G, Sood AK (2011) MicroRNA therapeutics: principles, expectations, and challenges. Chin J Cancer 30:368–370. https://doi.org/10.5732/cjc.011.10186
Brüggenwirth IMA, Martins PN (2020) RNA interference therapeutics in organ transplantation: the dawn of a new era. Am J Transplant 20:931–941. https://doi.org/10.1111/ajt.15689
Dalkara T, Alarcon-Martinez L (2015) Cerebral microvascular pericytes and neurogliovascular signaling in health and disease. Brain Res 1623:3–17. https://doi.org/10.1016/j.brainres.2015.03.047
Mathupala SP, Mittal S, Guthikonda M, Sloan AE (2007) MicroRNA and brain tumors: a cause and a cure? DNA Cell Biol 26:301–310. https://doi.org/10.1089/dna.2006.0560
Kumar S, Reddy PH (2016) Are circulating microRNAs peripheral biomarkers for Alzheimer’s disease? Biochim Biophys Acta (BBA) - Mol Basis Dis 1862:1617–1627. https://doi.org/10.1016/j.bbadis.2016.06.001
Li T, Zhu L, Zhu L, Wang P, Xu W, Huang J (2021) Recent developments in delivery of microRNAs utilizing nanosystems for metabolic syndrome therapy. Int J Mol Sci 22:7855. https://doi.org/10.3390/ijms22157855
Fu Y, Chen J, Huang Z (2019) Recent progress in microRNA-based delivery systems for the treatment of human disease. ExRNA 1:24. https://doi.org/10.1186/s41544-019-0024-y
Etheridge A, Lee I, Hood L, Galas D, Wang K (2011) Extracellular microRNA: a new source of biomarkers. Mutat Res/Fundam Mol Mech Mutagen 717:85–90. https://doi.org/10.1016/j.mrfmmm.2011.03.004
Sun Yat-sen U (2020) Protein and microRNA markers for early detection of Alzheimer’s disease. Available from: https://classic.clinicaltrials.gov/show/NCT03388242
Walgrave H, Zhou L, De Strooper B, Salta E (2021) The promise of microRNA-based therapies in Alzheimer’s disease: challenges and perspectives. Mol Neurodegener 16:76. https://doi.org/10.1186/s13024-021-00496-7
Beierlein JM, McNamee LM, Ledley FD (2017) As Technologies for Nucleotide Therapeutics Mature, Products Emerge. Mol Ther Nucleic Acids 9:379–386. https://doi.org/10.1016/j.omtn.2017.10.017
Bonneau E, Neveu B, Kostantin E, Tsongalis GJ, De Guire V (2019) How close are miRNAs from clinical practice? A perspective on the diagnostic and therapeutic market. EJIFCC 30:114–127
Acknowledgements
Authors acknowledge support from Poona College of Pharmacy, BVDU, Pune.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Informed Consent
Not applicable.
Consent to Participate
Yes.
Consent for Publication
Yes.
Conflict of Interest
The authors declare no competing interests.
Research Involving Human Participants and/or Animals
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhatnagar, D., Ladhe, S. & Kumar, D. Discerning the Prospects of miRNAs as a Multi-Target Therapeutic and Diagnostic for Alzheimer’s Disease. Mol Neurobiol 60, 5954–5974 (2023). https://doi.org/10.1007/s12035-023-03446-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-023-03446-0