Abstract
Background
Several bedside assessments are used to evaluate respiratory muscle function and to predict weaning from mechanical ventilation in patients on the intensive care unit. It remains unclear which assessments perform best in predicting weaning success. The primary aim of this systematic review and meta-analysis was to summarize and compare the accuracy of the following assessments to predict weaning success: maximal inspiratory (PImax) and expiratory pressures, diaphragm thickening fraction and excursion (DTF and DE), end-expiratory (Tdiee) and end-inspiratory (Tdiei) diaphragm thickness, airway occlusion pressure (P0.1), electrical activity of respiratory muscles, and volitional and non-volitional assessments of transdiaphragmatic and airway opening pressures.
Methods
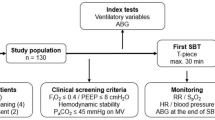
Medline (via Pubmed), EMBASE, Web of Science, Cochrane Library and CINAHL were comprehensively searched from inception to 04/05/2023. Studies including adult mechanically ventilated patients reporting data on predictive accuracy were included. Hierarchical summary receiver operating characteristic (HSROC) models were used to estimate the SROC curves of each assessment method. Meta-regression was used to compare SROC curves. Sensitivity analyses were conducted by excluding studies with high risk of bias, as assessed with QUADAS-2. Direct comparisons were performed using studies comparing each pair of assessments within the same sample of patients.
Results
Ninety-four studies were identified of which 88 studies (n = 6296) reporting on either PImax, DTF, DE, Tdiee, Tdiei and P0.1 were included in the meta-analyses. The sensitivity to predict weaning success was 63% (95% CI 47–77%) for PImax, 75% (95% CI 67–82%) for DE, 77% (95% CI 61–87%) for DTF, 74% (95% CI 40–93%) for P0.1, 69% (95% CI 13–97%) for Tdiei, 37% (95% CI 13–70%) for Tdiee, at fixed 80% specificity. Accuracy of DE and DTF to predict weaning success was significantly higher when compared to PImax (p = 0.04 and p < 0.01, respectively). Sensitivity and direct comparisons analyses showed that the accuracy of DTF to predict weaning success was significantly higher when compared to DE (p < 0.01).
Conclusions
DTF and DE are superior to PImax and DTF seems to have the highest accuracy among all included respiratory muscle assessments for predicting weaning success. Further studies aiming at identifying the optimal threshold of DTF to predict weaning success are warranted.
Trial registration: PROSPERO CRD42020209295, October 15, 2020.
Similar content being viewed by others
Introduction
Failure to wean from mechanical ventilation has a complex multifactorial pathophysiology which may involve impairments of pulmonary, brain, cardiac, endocrine and respiratory muscle function [1]. Most of these factors are routinely evaluated in mechanically ventilated patients. While respiratory muscle dysfunction is highly prevalent in these patients [2,3,4] and is strongly associated with failing a spontaneous breathing trial (SBT), weaning failure and mortality [3,4,5,6], its assessment is not yet routinely performed in most intensive care unit (ICU) settings. Early detection of respiratory muscle dysfunction may enable clinicians to identify patients at risk of weaning failure and poor prognosis who may benefit from treatment strategies to preserve or improve respiratory muscle function [7].
Several bedside tools for a comprehensive assessment of diaphragm and non-diaphragmatic respiratory muscle function are available [8]. These tools measure distinct aspects of respiratory muscle function and vary in ease of use. The gold standard to assess diaphragm contractility is a non-volitional assessment in which twitch transdiaphragmatic pressures or (artificial) airway opening pressures are recorded during phrenic nerve stimulation [8]. In cooperative patients, assessments of the maximal voluntary transdiaphragmatic pressure can be performed [8]. These assessments however require both sophisticated equipment and technical expertise and are therefore rarely performed in clinical settings [9]. Alternative, less invasive and more clinically accessible bedside respiratory muscle assessments are available. First, global respiratory muscle strength can be assessed by measuring the maximal inspiratory (PImax) and expiratory pressures [8]. PImax is often used in research and clinical context since reference values are available and the measurement is easy to perform [10]. Second, ultrasound imaging is increasingly used in research and in clinical settings as it is a non-invasive technique performed using devices that are readily available bedside in most intensive care units. It can evaluate multiple aspects of respiratory muscle function such as thickness, contractility, and excursion of the diaphragm [8, 11]. Third, the airway occlusion pressure during the first 100 ms of inspiratory effort (P0.1) reflects the neural respiratory drive and its transmission to respiratory muscles [8, 12, 13]. P0.1 is frequently used during SBTs since it is a rapid assessment that can be easily performed with a mechanical ventilator [14]. Fourth, electromyography of respiratory muscles assesses respiratory muscle activation [8, 9]. However, this assessment has been mostly used in research since reference values are lacking and technical expertise is necessary to perform the assessments and interpret the data.
Previous meta-analyses evaluating PImax, diaphragm ultrasound assessment or P0.1 described the associations between the respiratory muscle assessment and rates of mortality and/or weaning outcomes [15,16,17,18], but none compared their predictive accuracy. Comparing these assessments provide guidance to clinicians for making a well substantiated choice between available respiratory muscle assessment methods during the weaning process.
Since there is no general agreement on an assessment for predicting weaning outcomes, it is also difficult to determine what the minimal acceptable difference in accuracy between assessments should be. For the first time, this study provides data on comparative accuracy between respiratory muscle assessments.
The aim of this systematic review and meta-analysis was therefore to estimate and compare the accuracy of bedside respiratory muscle assessments to predict weaning outcomes, focusing on assessment methods evaluated in previous meta-analyses or recommended in a recent international statement to be used in the ICU setting [8].
Methods
Design and search strategy
This study protocol has been registered (PROSPERO, ID: CRD42020209295) and was conducted in accordance with the Cochrane handbook for systematic reviews of diagnostic test accuracy [19, 20] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses of Diagnostic Test Accuracy Studies (PRISMA-DTA) statement [21]. In collaboration with an expert on systematic reviews from the KU Leuven Biomedical library, a comprehensive search strategy was constructed including three concepts: intensive care unit, respiratory muscles, and the assessment methods of interest: maximal respiratory pressures, ultrasound, airway occlusion pressure, twitch airway opening pressure, electromyography, transdiaphragmatic pressure and twitch transdiaphragmatic pressure.
Studies published in English from database inception until 04/05/2023 in Medline (via Pubmed), EMBASE, Web of Science, Cochrane Library and CINAHL databases were searched for these concepts, synonyms, and MeSH terms in title and abstract (See Additional file 1: Table S1 for the search string). Reference lists of included studies and published systematic reviews were additionally searched.
Given the focus on respiratory muscle assessments, we did not consider indices aggregating results from multiple assessments of functions other than respiratory muscle function.
Study selection and data extraction
Deduplication, screening, and data extraction were performed with Covidence software (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia).
Title and abstract screening were performed by two independent reviewers for each study (YQC, TG, DRC, MRS, DP, MVH). MVH and DP resolved any conflicts. Remaining issues were resolved following discussion with senior researchers RG and DL. Peer-reviewed studies written in English were included when fulfilling all inclusion criteria: patients ≥ 18 years, accuracy to predict weaning outcomes reported and not fulfilled an exclusion criterion: animal studies, no full text available, non-peer reviewed, non-original research studies, case reports and interventional studies. The target condition was weaning success. We accepted all the various definitions of weaning from mechanical ventilation as employed in the included studies. Data extraction was performed by YQC, DP, DRC and MVH.
In case more than one threshold were evaluated for an assessment and that assessment was conducted while patients were supported with different mechanical ventilation settings, the threshold associated with mechanical ventilation settings closest to unsupported spontaneous breathing was retained.
If multiple studies reported on the same patients, multiple inclusions of the same patients were avoided by including the studies providing data on the largest sample. In case the confusion matrix (2 by 2 table) was not reported, it was computed from the provided values of sensitivity, specificity and the occurrence (prevalence) of patients presenting with and without the target condition. Studies for which the confusion matrix was reported are marked in the tables of characteristics.
Any missing data or information was requested from the corresponding authors by e-mail. If no response, two reminders were sent, or other authors of the team were contacted. In case raw data were obtained and no threshold was specified in the study, the median threshold of the other included studies reporting on the same assessment and target condition was used to compute the confusion matrix.
Methodological quality
The methodological quality of studies included in the meta-analysis was assessed with the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool [22] and evaluated by DP, DRC and MVH. A pilot was performed before assessing all studies in which reviewers developed and agreed on review-specific rating guidance (Additional file 1: Table S2). Each study was independently evaluated by two reviewers, and conflicts were resolved by the third. Remaining issues were resolved following discussion with senior researchers RG and DL.
Statistical analyses
Results of individual studies reporting on predictive accuracy were summarized for weaning success with forest plots of sensitivity and specificity. Therefore, when studies reported on weaning failure, the confusion matrix of test accuracy was reversed. Meta-analyses were performed if at least 4 studies evaluating the accuracy of the same assessment to predict weaning success could be included [19, 20]. Predictive accuracy for each assessment was summarized as sensitivity at fixed 80% specificity with corresponding 95% confidence intervals [20, 23].
The hierarchical summary receiver operating characteristic (HSROC) model was used to estimate the SROC curves of each assessment, while accounting for different thresholds used across studies [19, 20]. HSROC meta-regression models were used to compare SROC curves between assessments included in the meta-analysis. Three meta-regression models were fitted: Model 1: “Varied,” which included covariates to allow accuracy, threshold and shape to vary for each SROC curve under comparison; Model 2: “Fixed shape,” where the covariate term for shape was removed, to assume that the SROC curves under comparison have the same shapes; Model 3: “Fixed accuracy,” where the covariate term for accuracy was removed to assume that the SROC curves under comparison have the same accuracy [20].
Potential sources of heterogeneity were investigated with meta-regression analyses. These included the condition during which the assessment was performed [i.e., SBT or during mechanical ventilation] and the threshold. Thresholds were categorized depending on the median threshold of the included studies for the respective assessment, as low or high when lower or higher than the median threshold, respectively.
Sensitivity analyses were performed: (1) after excluding studies with potential high risk of bias or applicability concerns for at least one of the domains of the QUADAS-2 tool [22], and (2) after excluding studies that conducted assessments early after start of mechanical ventilation and not during the weaning process.
Direct comparisons between assessments were performed for studies which compared each pair of assessments within the same sample of patients.
Relative diagnostic odds ratio (RDOR) was computed for each comparison between assessments (SAS macro MetaDAS). RDOR is the ratio of diagnostic odds ratios (DORs) of the compared assessments, which are summary indicators of the accuracy of each assessment [20]. An RDOR greater than 1 indicates a better performance of the first assessment compared to the second one.
SAS OnDemand for Academics (SAS Institute Inc. 2021) was used to perform the meta-analyses (SAS macro MetaDAS, by fitting the HSROC model [23]) and HSROC meta-regression analyses (using Proc NLMIXED in SAS [23]) to compare summary curves. Forest and SROC plots were created with Review manager (Review Manager, RevMan, [Computer program] Version 5.4, Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2020).
Results
Study selection and characteristics.
The search identified 13 909 unique studies, retaining 1 830 studies for full text screening (Fig. 1). Ninety-four studies were included in the systematic review of which 88 studies reporting on accuracy of the assessments of interest to predict weaning outcomes were included in the meta-analyses (Fig. 1).
Studies included in the meta-analysis were published between 1987 and 2023. The studies were most frequently conducted in Asia (34%), followed by Europe (25%), Africa (22%), North America (12%), South America (7%) and Oceania (1%). In total, 6296 patients were included in the present meta-analyses.
Studies reporting on accuracy to predict weaning outcomes and included in the meta-analysis involved assessment of PImax (n = 18 studies) [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41], diaphragm ultrasound assessments with diaphragm excursion (DE, n = 53 studies) [6, 26, 30, 31, 35, 37, 39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85], diaphragm thickening fraction (DTF, n = 48 studies) [38, 40, 43,44,45,46,47,48,49,50,51,52,53,54,55,56, 62, 65,66,67, 69, 71,72,73, 75,76,77, 79, 81,82,83,84, 86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101] and end-expiratory (Tdiee, n = 11 studies) [45, 48, 53,54,55, 66, 73, 89, 90, 99, 100], end-inspiratory diaphragm thickness (Tdiei, n = 8 studies) [48, 53,54,55, 66, 73, 89, 100] and P0.1 (n = 15 studies) [25, 27, 29, 36, 73, 81, 102,103,104,105,106,107,108,109,110] (See Additional file 1: Table S3 for study characteristics). Different weaning outcome definitions were used across studies (Additional file 1: Table S3).
Less than 4 studies reported on accuracy to predict weaning outcomes for maximal expiratory pressure [28, 32], parasternal intercostal thickening fraction [101, 111], thickness of the abdominal muscles [47], electromyography of the diaphragm [112, 113], phrenic nerve stimulation [114, 115] and transdiaphragmatic pressure [116]. Therefore the data on these assessments were not considered in the meta-analysis in case the studies were already included in the meta-analysis for other assessments [28, 32, 47, 101]. Conversely, the studies exclusively focusing on these assessments were excluded from the meta-analysis [111,112,113,114,115,116].
The characteristics of these studies and their sensitivity and specificity are presented in Additional file 1: Table S4 and Fig. S1.
Methodological quality
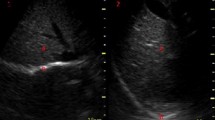
Overview of risk of bias and applicability concerns is provided in Fig. 2. Most frequent source of potential high risk of bias involved patient selection, due to non-consecutive patient recruitment. Methodological quality per study and assessment method are provided in Additional file 1: Figs. S2–S4.
Risk of bias and applicability concerns for weaning success per assessment method. Risk of bias analyses and applicability concerns have been performed with QUADAS 2 tool for predicting weaning success by assessing the maximal inspiratory pressure (panel A), airway occlusion pressure, P0.1 (panel B), diaphragm excursion (panel C), diaphragm thickening fraction (panel D), diaphragm end-expiratory thickness (panel E) or diaphragm end inspiratory thickness (panel F)
Accuracy of respiratory muscle assessments
Figures 3 and 4 provide the values of sensitivity and specificity of individual studies. At a fixed value of 80% for specificity to predict weaning failure, the estimated values of sensitivity were 63% (95% CI 47–77%) for PImax, 75% (95% CI 67–82%) for DE, 77% (95% CI 61–87%) for DTF, 74% (95% CI 40–93%) for P0.1, 69% (95% CI 13–97%) for Tdiei, 37% (95% CI 13–70%) for Tdiee. Comparison of these tests showed that the accuracy for predicting weaning success was statistically significantly higher for DE versus PImax (p = 0.04) and for DTF versus PImax (p < 0.01) (Table 1). The curves estimated with the HSROC model for each assessment method are provided in Additional file 1: Fig. S5. The results on one-to-one comparisons of SROC curves included in the meta-analyses, are presented in Table 1.
Accuracy of respiratory muscle assessment methods for predicting weaning success—part 1 of 2. Figure depicts the individual sensitivity and specificity of each study on the respiratory assessment method of interest for predicting weaning success. Condition: Indicates whether the assessment was performed while the patients was mechanically ventilated (MV) or during spontaneous breathing/spontaneous breathing trial (SBT). If no or insufficient data was provided on the condition it is marked as not reported (NR). Risk of bias: Studies that were identified as having a high risk of bias on one of the domains of the QUADAS 2 tool were indicated as high risk of bias (High). Studies which had no domain in which a potential high risk of bias was identified were indicated as low risk of bias (Low). Abbreviations: TP True positive, FP False positive, FN False negative, TN True negative, n Sample size of the study, SBT Spontaneous breathing trial, MV Mechanical ventilation, NR Not reported, CI Confidence interval
Accuracy of respiratory muscle assessment methods for predicting weaning success—part 2 of 2. Figure depicts the individual sensitivity and specificity of each study on the respiratory assessment method of interest for predicting weaning success. Condition: Indicates whether the assessment was performed while the patients was mechanically ventilated (MV) or during spontaneous breathing/spontaneous breathing trial (SBT). If no or insufficient data was provided on the condition it is marked as not reported (NR). Risk of bias: Studies that were identified as having a high risk of bias on one of the domains of the QUADAS 2 tool were indicated as high risk of bias (High). Studies which had no domain in which a potential high risk of bias was identified were indicated as low risk of bias (Low). Abbreviations: TP True positive, FP False positive, FN False negative, TN True negative, n Sample size of the study, SBT Spontaneous breathing trial, MV Mechanical ventilation, NR Not reported, CI Confidence interval
Heterogeneity analyses
The condition of the assessments (i.e., during mechanical ventilation or during an SBT) and the chosen threshold were t identified as a source of heterogeneity for PImax, DE, DTF, P0.1 (Additional file 1: Tables S5, S6).
Sensitivity analyses
Sensitivity analyses were performed based on a total of 44 studies after exclusion of studies with high potential risk of bias from the meta-analyses. The count included studies that reported results for multiple assessments only once. At a fixed value of 80% for specificity to predict weaning failure, the estimated values of sensitivity were 61% (95% CI 44–75%) for PImax, 78% (95% CI 63–88%) for DTF and 76% (95% CI 64–85%) for DE. SROC curves of PImax (n = 7 studies) [26, 27, 29, 30, 33, 36, 38], DTF (n = 23 studies) [38, 47,48,49,50,51,52, 62, 65, 67, 69, 71,72,73, 75, 88, 89, 93, 94, 96, 98, 101], DE(n = 23 studies) [6, 26, 30, 42, 47,48,49,50,51,52, 60, 62, 64, 65, 67,68,69,70,71,72,73,74,75] and P0.1 (n = 11 studies) [29, 36, 73, 102,103,104,105,106, 108,109,110], Tdiee (n = 4 studies) [48, 73, 89, 100] and Tdiei (n = 4 studies) [48, 73, 89, 100] were estimated (Additional file 1: Fig. S6 and Table S7). The one-to-one comparisons showed that accuracy for predicting weaning success was significantly higher for DTF versus DE (Additional file 1: Table S8).
Results of SROC comparisons after exclusion of studies that conducted assessments early after start of mechanical ventilation [53, 98] and not during the weaning process did not substantially differ from the results presented in Table 1 (Additional file 1: Table S9).
Direct comparisons
At least 4 direct comparative studies reporting on accuracy to predict weaning success were found for the following pairs of assessments: DE versus PImax (n = 8 studies) [30, 31, 35, 37, 39,40,41], DE versus DTF (n = 28 studies) [40, 43,44,45, 47,48,49,50,51,52, 54, 56, 62, 65,66,67, 69, 71,72,73, 75, 77, 79, 81,82,83,84, 117], DE versus Tdiee (n = 5 studies) [45, 48, 54, 66, 73], DE versus Tdiei (n = 4 studies) [48, 54, 66, 73], DTF versus Tdiee (n = 11 studies) [45, 48, 53,54,55, 66, 73, 89, 90, 99, 100], DTF versus Tdiei (n = 8 studies) [48, 54, 55, 66, 73, 89, 100] and P0.1 versus PImax (n = 4 studies) [25, 27, 29, 36]. The SROC curves estimated based on direct comparative studies are presented in Additional file 1: Fig. S7 (DE vs. DTF) and in Additional file 1: Fig. S8 (DE vs. PImax, DE vs. Tdiee, DE vs. Tdiei, Tdiee vs. DTF, Tdiei vs. DTF and P0.1 vs. PImax).
At a fixed value of 80% for specificity to predict weaning failure, the estimated values of sensitivity were 88% (95% CI 78–93%) for DTF and 79% (95% CI 68–87%) for DE. The results of the one-to-one comparisons of SROC curves of the identified paired of assessments showed that predictive accuracy was higher for DTF versus DE (p < 0.01, Table 2).
Discussion
Main findings
This systematic review and meta-analysis aimed to estimate and compare the accuracy of multiple bedside respiratory muscle assessments to predict weaning outcomes in critically ill patients. The estimated values of sensitivity were 63% for PImax, 75% for DE, 77% for DTF, 74% P0.1, 69% for Tdiei, and 37% for Tdiee at 80% specificity for predicting weaning success. DTF and DE performed significantly better than PImax, with DTF showing the highest accuracy in direct comparative studies. Our findings indicate that among the evaluated bedside respiratory muscle assessments, DTF is the most accurate tool to identify mechanically ventilated patients who may be successfully weaned.
Accuracy of respiratory muscle assessment methods to predict weaning outcomes
Our findings confirm the results of previous studies when considering all the studies included in our meta-analysis for DTF, DE and PImax to predict weaning outcomes [15, 16, 18, 118]. In fact, when visually inspecting the estimated SROC curves in previous meta-analyses [15, 16, 18], values of sensitivity to predict weaning success at a fixed value of 80% specificity were between 70 and 80% for DE and DTF and close to 60% for PImax.
Importantly, our study provides new valuable information on accuracy differences between respiratory muscle assessment methods to predict weaning success: 1) DTF and DE are more accurate than PImax; 2) DTF has higher accuracy than DE when excluding studies with potential high risk of bias or considering direct comparative studies.
DTF and DE showed higher accuracy to predict weaning success compared to PImax when considering all the studies in the meta-analysis. However, these differences were no longer statistically significant in sensitivity analyses despite the unchanged magnitude of difference in sensitivity at 80% specificity (sensitivity ranging from 75 to 78% for DTF and DE and from 61 to 63% for PImax). Additionally, no study directly compared DTF with PImax and the SROC curves estimated based on only eight direct comparative studies of DE versus PImax showed minimal sensitivity differences at 80% specificity. These findings are likely due to result variability and the limited number of studies reporting on PImax or directly comparing PImax with DTF and DE. The use of different assessment protocols, such as a 20–30 s occlusion method [119] or a single complete expiration followed by a forceful inspiration against a closed valve [120] likely contributed to the variability in predictive accuracy of PImax.
Hence, it remains plausible that DE and DTF would have shown a higher accuracy than PImax in sensitivity and direct comparison analyses if a larger number of studies similar to the number used in the overall meta-analysis had been available.
The superiority of DTF over DE may be explained by the influence of mechanical ventilation support, patient’s positioning, and variation in thoracic and abdominal pressures on the interpretation of DE [18, 121].
Although P0.1 is frequently used during SBTs due to its rapid assessment using a mechanical ventilator, published data on its predictive accuracy are few and widely variable. The variability of predictive accuracy of P0.1 may be due to variations in P0.1 formulas across mechanical ventilator brands [12, 14] or to the use of an external device for measurement.
The paucity of data also hindered the summarization and interpretation of predictive accuracy of Tdiei and Tdiee.
Strengths and weaknesses
To our knowledge, this is the largest systematic review and meta-analysis to summarize and the first to formally compare accuracy of several bedside respiratory muscle assessments to predict weaning success in critically ill patients using indirect and direct comparative studies and sensitivity analyses excluding studies with potentially high risk of bias. Through a comprehensive search string across diverse databases and the retrieval of missing data from authors, we obtained a maximum of published data.
Our study has limitations. Direct comparisons, which are considered as more reliable and less likely to be biased compared to indirect comparisons [20, 122], could not be performed for all the assessment methods of interest. Another limitation is that no estimation of predictive accuracy could be carried out for all the assessment methods of interest for our review due to limited available data. Moreover, deriving the confusion matrix of studies for which we received individual (raw) patient data by using the median threshold from other included studies reporting on the same assessment method could potentially introduce bias. However, we deemed this approach logical in the absence of a consensus on threshold values to predict weaning outcomes.
The use of different thresholds across the included studies introduces limitations to this work. Despite using the HSROC model as recommended by the Cochrane Handbook [19, 20], this approach did not allow for determining the most optimal threshold to predict weaning success for each assessment method.
Furthermore, most of the studies selected thresholds post-hoc relying on assessments at a single point in time and using the Youden index (i.e., sensitivity + specificity − 1), leading to potential overestimation of the sensitivity and specificity of the assessment method [123] and timing of testing may influence the capability of an assessment method to predict weaning outcomes.
Finally, patient heterogeneity may have also influenced the prediction characteristics of the assessment methods considered in this study.
Implications for clinical practice
A spontaneous breathing trial is a recommended for assessing whether a patient’s readiness for mechanical ventilator weaning [124]. Previous studies reported a 10 to 20% weaning failure rate among patients who passed the trial [125]. Respiratory muscle assessment methods are promising tools to further assist clinician at the bedside during the weaning process.
This meta-analysis supports the use of DE and DTF over PImax to predict weaning outcomes in mechanically ventilated patients. Further sensitivity analyses suggest that DTF may outperform DE.
PImax and P0.1 are accessible tools in the hands of clinicians, but the results of this meta-analysis and the greater variability in their sensitivity to predict weaning success compared to DTF and DE, are not currently supporting their use to predict weaning success.
In contrast to PImax and P0.1, the need for specific training to learn diaphragm ultrasonography has been recently highlighted [126]. Although DTF measurements may have a slower learning curve than DE [126], there is indication that clinicians previously lacking experience can produce accurate measurements when compared to measurements performed by experts and that a good intra-rater and inter-rater agreement among assessors can be achieved after a relatively brief training [96, 127]. Moreover, ICU allied healthcare professionals can also easily acquire the skills required for diaphragm ultrasonography assessment. Among them, respiratory physiotherapists are becoming very involved in the applications of thoracic ultrasound (including diaphragm) imaging in their clinical practice [128,129,130,131]. They can certainly support physicians during the weaning process by performing DE and DTF measurements, which can be rapidly performed even in uncooperative patients without causing discomfort or prolonging the weaning process. Additionally, DTF assessments have moderate reproducibility [132].
Subsequently, we encourage integrating DTF assessments during SBTs after specific training [126] and following the recently published recommendations on methodology for diaphragm ultrasonography [126]. However, despite the potential of DTF to guide the weaning process, to date only one single center study observed that incorporating DTF information in patients with a DTF > 30% significantly reduced the time to extubation [95]. Therefore more future prospective studies are needed to investigate its impact on clinical decision making and improvement of weaning outcomes.
Finally, most included studies used thresholds ranging from 25 to 33% for DTF (Fig. 4). We recommend using that range of thresholds for DTF in clinical practice to predict weaning outcomes.
Implications for research
Additional high-quality test accuracy studies comparing predefined thresholds and multiple respiratory muscle assessments within the same patient sample are needed to find optimal threshold values for predicting weaning outcomes, thus increasing their clinical usefulness and routine applicability. More homogeneity of weaning definitions can facilitate the interpretation and applicability of studies reporting on predictive accuracy of respiratory muscle assessment methods. A recent promising weaning definition is available and may be used to account for tracheostomized patients in future studies [133]. Notably, although P0.1 is a very fast and easy tool to use, data on its accuracy to predict weaning outcomes are lacking, warranting future research to further establish its accuracy and the optimal cut-off.
Methodology of ultrasound assessments varied in mode, probe type, probe and patient positioning and breathing condition. Clear reporting and uniformity in the methodology based on recent recommendations [126] will ensure reproducibility of predictive accuracy in research and clinical practice.
Exploring comparative accuracy of different combinations of multiple assessments of respiratory muscles would be important to determine the most accurate combination for predicting weaning outcomes. DE and DTF are promising assessments and accuracy may improve when their evaluation is combined which can be done efficiently using the same equipment.
Finally, successful weaning depends on various factors beyond respiratory muscle function, such as cardiac and respiratory failure, cognitive and endocrine dysfunction [1]. Machine learning, incorporating all these facets may be a powerful tool to predict weaning success [134] and diaphragm thickening fraction is a parameter that deserves inclusion in models for future evaluations [134].
Conclusions
Among several bedside respiratory muscle assessments, diaphragm thickening fraction and excursion have higher accuracy compared to maximal inspiratory pressure to predict weaning success. Predictive accuracy seems to be the highest when diaphragm thickening fraction is assessed. This assessment has a great potential to assist clinicians during weaning. It can be applied by clinicians lacking experience after specific training, even in non-cooperative patients, without causing discomfort.
Future research should validate the use of ultrasound assessments when incorporated in clinical decision-making around weaning and explore the accuracy of combining ultrasound with other respiratory muscle assessments. In addition, identifying the optimal threshold for diaphragm thickening fraction to predict weaning success would be of great clinical and research value. Lastly, it is worthy to investigate the potential of combining several bedside respiratory muscle assessments or of multifactorial models to predict weaning outcomes.
Availability of data and materials
The dataset used and/or analyzed for the current study is available from the corresponding author on reasonable request.
Abbreviations
- AECOPD:
-
Acute exacerbation chronic obstructive pulmonary disease
- ARF:
-
Acute respiratory failure
- ATS:
-
American Thoracic Society
- CCU:
-
Coronary care unit
- COPD:
-
Chronic obstructive pulmonary disease
- CPAP:
-
Continuous positive airway pressure
- DE:
-
Diaphragm excursion
- DTF:
-
Diaphragm thickening fraction
- DOR:
-
Diagnostic odds ratio
- EICU:
-
Emergency intensive care unit
- ERS:
-
European Respiratory Society
- FRC:
-
Functional residual capacity
- HSROC:
-
Hierarchical Summary Receiver Operating Characteristic
- ICU:
-
Intensive care unit
- MICU:
-
Medical intensive care unit
- MV:
-
Mechanically ventilated/mechanical ventilation
- NICU:
-
Neurointensive care unit
- NIV:
-
Non-invasive ventilation
- NIPPV:
-
Non-invasive positive pressure ventilation
- NR:
-
Not reported
- P0.1:
-
Airway occlusion pressure
- PEEP:
-
Positive end-expiratory pressure
- PImax:
-
Maximal inspiratory pressure
- PRISMA-DTA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses of Diagnostic Accuracy Studies
- PS:
-
Pressure support
- PSV:
-
Pressure support ventilation
- RDOR:
-
Relative diagnostic odds ratio
- QUADAS-2:
-
Quality Assessment of Diagnostic Accuracy Studies
- RICU:
-
Respiratory intensive care unit
- RV:
-
Residual volume
- SICU:
-
Surgical intensive care unit
- SB:
-
Spontaneous breathing
- SBT:
-
Spontaneous breathing trial
- Tdiee :
-
End-expiratory diaphragm thickness
- Tdiei :
-
End-inspiratory diaphragm thickness
- TLC:
-
Total lung capacity
References
Heunks LM, van der Hoeven JG. Clinical review: the ABC of weaning failure—a structured approach. Crit Care. 2010;14(6):245.
Demoule A, Jung B, Prodanovic H, Molinari N, Chanques G, Coirault C, et al. Diaphragm dysfunction on admission to the intensive care unit. Prevalence, risk factors, and prognostic impact-a prospective study. Am J Respir Crit Care Med. 2013;188(2):213–9.
Jung B, Moury PH, Mahul M, de Jong A, Galia F, Prades A, et al. Diaphragmatic dysfunction in patients with ICU-acquired weakness and its impact on extubation failure. Intensive Care Med. 2016;42(5):853–61.
Dres M, Dube BP, Mayaux J, Delemazure J, Reuter D, Brochard L, et al. Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am J Respir Crit Care Med. 2017;195(1):57–66.
Dres M, Goligher EC, Heunks LMA, Brochard LJ. Critical illness-associated diaphragm weakness. Intensive Care Med. 2017;43(10):1441–52.
Kim WY, Suh HJ, Hong SB, Koh Y, Lim CM. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med. 2011;39(12):2627–30.
Dres M, Demoule A. Diaphragm dysfunction during weaning from mechanical ventilation: an underestimated phenomenon with clinical implications. Crit Care. 2018;22(1):73.
Laveneziana P, Albuquerque A, Aliverti A, Babb T, Barreiro E, Dres M, et al. ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J. 2019;53(6).
Doorduin J, van Hees HW, van der Hoeven JG, Heunks LM. Monitoring of the respiratory muscles in the critically ill. Am J Respir Crit Care Med. 2013;187(1):20–7.
Neder JA, Andreoni S, Lerario MC, Nery LE. Reference values for lung function tests. II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Res. 1999;32(6):719–27.
Tuinman PR, Jonkman AH, Dres M, Shi ZH, Goligher C, Goffi A, et al. Respiratory muscle ultrasonography: methodology, basic and advanced principles and clinical applications in ICU and ED—a narrative review. Intensive Care Med. 2020;46(4):594–605.
Telias I, Damiani F, Brochard L. The airway occlusion pressure (P0.1) to monitor respiratory drive during mechanical ventilation: increasing awareness of a not-so-new problem. Intensive Care Med. 2018;44(9):1532–5.
Whitelaw WA, Derenne JP. Airway occlusion pressure. J Appl Physiol. 1993;74(4):1475–83.
Telias I, Junhasavasdikul D, Rittayamai N, Piquilloud L, Chen L, Ferguson ND, et al. Airway occlusion pressure as an estimate of respiratory drive and inspiratory effort during assisted ventilation. Am J Respir Crit Care Med. 2020;201(9):1086–98.
Le Neindre A, Philippart F, Luperto M, Wormser J, Morel-Sapene J, Aho SL, et al. Diagnostic accuracy of diaphragm ultrasound to predict weaning outcome: a systematic review and meta-analysis. Int J Nurs Stud. 2021;117:103890.
Medrinal C, Combret Y, Hilfiker R, Prieur G, Aroichane N, Gravier FE, et al. ICU outcomes can be predicted by noninvasive muscle evaluation: a meta-analysis. Eur Respir J. 2020;56(4).
Sato R, Hasegawa D, Hamahata NT, Narala S, Nishida K, Takahashi K, et al. The predictive value of airway occlusion pressure at 100 msec (P0.1) on successful weaning from mechanical ventilation: a systematic review and meta-analysis. J Crit Care. 2021;63:124–32.
Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J. Diaphragm and lung ultrasound to predict weaning outcome: systematic review and meta-analysis. Chest. 2017;152(6):1140–50.
Macaskill P TY, Deeks JJ, Gatsonis C. Chapter 9: understanding meta-analysis. Draft version (4 October 2022) for inclusion. In: Deeks JJ, Bossuyt PM, Leeflang MM, Takwoingi Y, editors. Cochrane handbook for systematic reviews of diagnostic test accuracy version 2. London: Cochrane. 2022.
Takwoingi Y DN, Schiller I, Rücker G, Jones HE, Partlett C, Macaskill P. Chapter 10: undertaking meta-analysis. Draft version (4 October 2022) for inclusion. In: Deeks JJ, Bossuyt PM, Leeflang MM, Takwoingi Y, editors. Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 2. London: Cochrane. 2022.
Salameh JP, Bossuyt PM, McGrath TA, Thombs BD, Hyde CJ, Macaskill P, et al. Preferred reporting items for systematic review and meta-analysis of diagnostic test accuracy studies (PRISMA-DTA): explanation, elaboration, and checklist. BMJ. 2020;370:m2632.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36.
Takwoingi Y DN, Schiller I, Rücker G, Jones HE, Partlett C, Macaskill P. Supplement 1 to chapter 10: code for undertaking meta-analysis. Draft version (4 October 2022) for inclusion. In: Deeks JJ, Bossuyt PM, Leeflang MM, Takwoingi Y, editors. Cochrane handbook for systematic reviews of diagnostic test accuracy version 2. London: Cochrane. Available from www.training.cochrane.org/handbook-diagnostic-test-accuracy. 2022.
Bruton A. A pilot study to investigate any relationship between sustained maximal inspiratory pressure and extubation outcome. Heart Lung. 2002;31(2):141–9.
Capdevila XJ, Perrigault PF, Perey PJ, Roustan JP, d’Athis F. Occlusion pressure and its ratio to maximum inspiratory pressure are useful predictors for successful extubation following T-piece weaning trial. Chest. 1995;108(2):482–9.
Carrie C, Gisbert-Mora C, Bonnardel E, Gauche B, Biais M, Vargas F, et al. Ultrasonographic diaphragmatic excursion is inaccurate and not better than the MRC score for predicting weaning-failure in mechanically ventilated patients. Anaesth Crit Care Pain Med. 2017;36(1):9–14.
Conti G, Montini L, Pennisi MA, Cavaliere F, Arcangeli A, Bocci MG, et al. A prospective, blinded evaluation of indexes proposed to predict weaning from mechanical ventilation. Intensive Care Med. 2004;30(5):830–6.
De Jonghe B, Bastuji-Garin S, Durand MC, Malissin I, Rodrigues P, Cerf C, et al. Respiratory weakness is associated with limb weakness and delayed weaning in critical illness. Crit Care Med. 2007;35(9):2007–15.
de Souza LC, da Silva Jr CT, Almeida JR, Lugon JR. Comparison of maximal inspiratory pressure, tracheal airway occlusion pressure, and its ratio in the prediction of weaning outcome: impact of the use of a digital vacuometer and the unidirectional valve. Respir Care. 2012;57(8):1285–90.
Flevari A, Lignos M, Konstantonis D, Armaganidis A. Diaphragmatic ultrasonography as an adjunct predictor tool of weaning success in patients with difficult and prolonged weaning. Minerva Anestesiol. 2016;82(11):1149–57.
Jiang JR, Tsai TH, Jerng JS, Yu CJ, Wu HD, Yang PC. Ultrasonographic evaluation of liver/spleen movements and extubation outcome. Chest. 2004;126(1):179–85.
Lim CK, Ruan SY, Lin FC, Wu CL, Chang HT, Jerng JS, et al. Effect of tracheostomy on weaning parameters in difficult-to-wean mechanically ventilated patients: a prospective observational study. PLoS ONE. 2015;10(9):e0138294.
Medrinal C, Prieur G, Frenoy É, Robledo Quesada A, Poncet A, Bonnevie T, et al. Respiratory weakness after mechanical ventilation is associated with one-year mortality—a prospective study. Crit Care. 2016;20(1):231.
O’Keefe GE, Hawkins K, Boynton J, Burns D. Indicators of fatigue and of prolonged weaning from mechanical ventilation in surgical patients. World J Surg. 2001;25(1):98–103.
Saeed AM, El Assal GI, Ali TM, Hendawy MM. Role of ultrasound in assessment of diaphragmatic function in chronic obstructive pulmonary disease patients during weaning from mechanical ventilation. Egypt J Bronchol. 2016;10(2):167–72.
Sassoon CS, Mahutte CK. Airway occlusion pressure and breathing pattern as predictors of weaning outcome. Am Rev Respir Dis. 1993;148(4 Pt 1):860–6.
Spadaro S, Grasso S, Mauri T, Dalla Corte F, Alvisi V, Ragazzi R, et al. Can diaphragmatic ultrasonography performed during the T-tube trial predict weaning failure? The role of diaphragmatic rapid shallow breathing index. Crit Care. 2016;20(1):305.
Tenza-Lozano E, Llamas-Alvarez A, Jaimez-Navarro E, Fernández-Sánchez J. Lung and diaphragm ultrasound as predictors of success in weaning from mechanical ventilation. Crit Ultrasound J. 2018;10(1):12.
Zaytoun TM, Elsayed HE, Elghazaly AM. The role of diaphragmatic rapid shallow breathing index and maximum inspiratory pressure in predicting outcome of weaning from mechanical ventilation. Egypt J Chest Dis Tu. 2021;70(4):526–33.
Shamil PK, Gupta NK, Ish P, Sen MK, Kumar R, Chakrabarti S, et al. Prediction of weaning outcome from mechanical ventilation using diaphragmatic rapid shallow breathing index. Indian J Crit Care Med. 2022;26(9):1000–5.
Vieira FN, Bertazzo RB, Nascimento GC, Anderle M, Coelho AC, Chaise FO, et al. Association between rectus femoris cross-sectional area and diaphragmatic excursion with weaning of tracheostomized patients in the intensive care unit. Rev Bras Ter Intensiva. 2022;34(4):452–60.
Abbas A, Embarak S, Walaa M, Lutfy SM. Role of diaphragmatic rapid shallow breathing index in predicting weaning outcome in patients with acute exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1655–61.
Abdelhafeez RM, Abumossalam AM, Arram EO, Elshafey MM, Abushehata ME. Diaphragm and weaning from mechanical ventilation: anticipation and outcome. Egypt J Bronchol. 2019;13(4):489–97.
Alam MJ, Roy S, Iktidar MA, Padma FK, Nipun KI, Chowdhury S, et al. Diaphragm ultrasound as a better predictor of successful extubation from mechanical ventilation than rapid shallow breathing index. Acute Crit Care. 2022;37(1):94–100.
Ali ER, Mohamad AM. Diaphragm ultrasound as a new functional and morphological index of outcome, prognosis and discontinuation from mechanical ventilation in critically ill patients and evaluating the possible protective indices against VIDD. Egypt J Chest Dis Tuberc. 2017;66(2):339–51.
Al Tayar AS, Abdelshafey EE. Diaphragm electromyography versus ultrasonography in the prediction of mechanical ventilation liberation outcome. Respir Care. 2022.
Amara V, Vishwas P, Maddani SS, Natarajan S, Chaudhuri S. Evaluation of abdominal expiratory muscle thickness pattern, diaphragmatic excursion, and lung ultrasound score in critically ill patients and their association with weaning patterns: a prospective observational study. Indian J Crit Care M. 2022;26(3):307–13.
Baess AI, Abdallah TH, Emara DM, Hassan M. Diaphragmatic ultrasound as a predictor of successful extubation from mechanical ventilation: Thickness, displacement, or both? Egypt J Bronchol. 2016;10(2):162–6.
Banerjee A, Mehrotra G. Comparison of lung ultrasound-based weaning indices with rapid shallow breathing index: Are they helpful? Indian J Crit Care Med. 2018;22(6):435–40.
ElGazzar A, Kamel KM, Mohammad OI, Abd EB. Diaphragmatic ultrasound as a predictor for successful weaning from mechanical ventilation. Egypt J Chest Dis Tuberc. 2019;68:585–9.
Elshazly MI, Kamel KM, Elkorashy RI, Ismail MS, Ismail JH, Assal HH. Role of bedside ultrasonography in assessment of diaphragm function as a predictor of success of weaning in mechanically ventilated patients. Tuberc Respir Dis (Seoul). 2020;83(4):295–302.
Eltrabili HH, Hasanin AM, Soliman MS, Lotfy AM, Hamimy WI, Mukhtar AM. Evaluation of diaphragmatic ultrasound indices as predictors of successful liberation from mechanical ventilation in subjects with abdominal sepsis. Respir Care. 2019;64(5):564–9.
Er B, Simsek M, Yildirim M, Halacli B, Ocal S, Ersoy EO, et al. Association of baseline diaphragm, rectus femoris and vastus intermedius muscle thickness with weaning from mechanical ventilation. Resp Med. 2021;185:106503.
Farghaly S, Hasan AA. Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients. Aust Crit Care. 2017;30(1):37–43.
Fossat G, Daillet B, Desmalles E, Boulain T. Does diaphragm ultrasound improve the rapid shallow breathing index accuracy for predicting the success of weaning from mechanical ventilation? Aust Crit Care. 2022;35(3):233–40.
Gok F, Mercan A, Kilicaslan A, Sarkilar G, Yosunkaya A. Diaphragm and lung ultrasonography during weaning from mechanical ventilation in critically ill patients. Cureus. 2021;13(5).
Haji K, Haji D, Canty DJ, Royse AG, Green C, Royse CF. The impact of heart, lung and diaphragmatic ultrasound on prediction of failed extubation from mechanical ventilation in critically ill patients: a prospective observational pilot study. Crit Ultrasound J. 2018;10(1):13.
Hayat A, Khan A, Khalil A, Asghar A. Diaphragmatic excursion: Does it predict successful weaning from mechanical ventilation? J Coll Physicians Surg Pak. 2017;27(12):743–6.
Helmy MA, Milad LM, Osman SH, Ali MA, Hasanin A. Diaphragmatic excursion: A possible key player for predicting successful weaning in patients with severe COVID-19. Anaesth Crit Care Pain Med. 2021;40(3).
Huang D, Ma H, Zhong W, Wang X, Wu Y, Qin T, et al. Using M-mode ultrasonography to assess diaphragm dysfunction and predict the success of mechanical ventilation weaning in elderly patients. J Thorac Dis. 2017;9(9):3177–86.
Khan MT, Munawar K, Hussain SW, Qadeer A, Saeed ML, Shad ZS, et al. Comparing ultrasound-based diaphragmatic excursion with rapid shallow breathing index as a weaning predictor. Cureus. 2018;10(12):e3710.
Li SG, Chen Z, Yan WF. Application of bedside ultrasound in predicting the outcome of weaning from mechanical ventilation in elderly patients. BMC Pulm Med. 2021;21(1).
Luo L, Li Y, Chen X, Sun B, Li W, Gu W, et al. Different effects of cardiac and diaphragm function assessed by ultrasound on extubation outcomes in difficult-to-wean patients: a cohort study. BMC Pulm Med. 2017;17(1):161.
Mariani LF, Bedel J, Gros A, Lerolle N, Milojevic K, Laurent V, et al. Ultrasonography for screening and follow-up of diaphragmatic dysfunction in the ICU: a pilot study. J Intensive Care Med. 2016;31(5):338–43.
Mawla TSA, Fattah SRA, Halim AMA, Elhefeny RA. Diaphragmatic function assessment using chest ultrasonography as a predictor for weaning from mechanical ventilation. Egypt J Crit Care Me. 2022;9(1):1–9.
Mohamed RSE, Mohamed ASE, Fathalah WF, Mohamed MF, Ahmed AA. The role of diaphragmatic ultrasound as a predictor of successful extubation from mechanical ventilation in respiratory intensive care unit. Egypt J Bronchol. 2021;15(1).
Osman A, Hashim R. Diaphragmatic and lung ultrasound application as new predictive indices for the weaning process in ICU patients. Egypt J Radiol Nucl Med. 2017;48.
Palkar A, Mayo P, Singh K, Koenig S, Narasimhan M, Singh A, et al. Serial diaphragm ultrasonography to predict successful discontinuation of mechanical ventilation. Lung. 2018;196(3):363–8.
Saad MA, Nashed SW, El-Shaer AN, Elagamy AE, El Derh MS. Ultrasound-assessed diaphragmatic dysfunction as a predictor of weaning outcome in mechanically ventilated patients with sepsis in intensive care unit. Ain Shams J Anesthes. 2022;14(1).
Saeed AM, El Maraghy AA, Raafat RH, Abd Elsamad AM. Assessment of diaphragmatic mobility by chest ultrasound in patients with chronic obstructive pulmonary disease on different modes of mechanical ventilation. Egypt J Bronchol. 2019;13(2):184–90.
Samanta S, Singh RK, Baronia AK, Poddar B, Azim A, Gurjar M. Diaphragm thickening fraction to predict weaning-a prospective exploratory study. J Intensive Care. 2017;5:62.
Spadaro S, Dalla Corte F, Scaramuzzo G, Grasso S, Cinnella G, Rosta V, et al. Circulating skeletal troponin during weaning from mechanical ventilation and their association to diaphragmatic function: a pilot study. Front Med-Lausanne. 2021;8.
Thabet D, Makhlouf HA, Hasan AA, Ghanem MA. Are diaphragmatic indices assessed by ultrasound good predictors of weaning outcome in mechanically ventilated respiratory patients? Egypt J Chest Dis Tuberc. 2020;69(4):681–7.
Theerawit P, Eksombatchai D, Sutherasan Y, Suwatanapongched T, Kiatboonsri C, Kiatboonsri S. Diaphragmatic parameters by ultrasonography for predicting weaning outcomes. BMC Pulm Med. 2018;18(1):175.
Varon-Vega F, Hernandez A, Lopez M, Caceres E, Giraldo-Cadavid LF, Uribe-Hernandez AM, et al. Usefulness of diaphragmatic ultrasound in predicting extubation success. Med Intensiva (Engl Ed). 2021;45(4):226–33.
Vivier E, Muller M, Putegnat JB, Steyer J, Barrau S, Boissier F, et al. Inability of diaphragm ultrasound to predict extubation failure: a multicenter study. Chest. 2019;155(6):1131–9.
Yoo JW, Lee SJ, Lee JD, Kim HC. Comparison of clinical utility between diaphragm excursion and thickening change using ultrasonography to predict extubation success. Korean J Intern Med. 2018;33(2):331–9.
Zhang X, Yuan J, Zhan Y, Wu J, Liu B, Zhang P, et al. Evaluation of diaphragm ultrasound in predicting extubation outcome in mechanically ventilated patients with COPD. Ir J Med Sci. 2020;189(2):661–8.
Eksombatchai D, Sukkratok C, Sutherasan Y, Junhasavasdikul D, Theerawit P. The ratio of respiratory rate to diaphragm thickening fraction for predicting extubation success. Bmc Pulm Med. 2023;23(1):109.
Huang D, Song F, Luo B, Wang S, Qin T, Lin Z, et al. Using automatic speckle tracking imaging to measure diaphragm excursion and predict the outcome of mechanical ventilation weaning. Crit Care. 2023;27(1):18.
Kaur A, Sharma S, Singh VP, Krishna MR, Gautam PL, Singh G. Sonographic assessment of diaphragmatic thickening and excursion as predictors of weaning success in the intensive care unit: a prospective observational study. Indian J Anaesth. 2022;66(11):776–82.
Saravanan R, Nivedita K, Karthik K, Venkatraman R. Role of diaphragm ultrasound in weaning mechanically ventilated patients: a prospective observational study. Indian J Anaesth. 2022;66(8):591–8.
Song J, Qian Z, Zhang H, Wang M, Yu Y, Ye C, et al. Diaphragmatic ultrasonography-based rapid shallow breathing index for predicting weaning outcome during a pressure support ventilation spontaneous breathing trial. BMC Pulm Med. 2022;22(1):337.
Xu Q, Yang X, Qian Y, Hu C, Lu W, Cai S, et al. Comparison of assessment of diaphragm function using speckle tracking between patients with successful and failed weaning: a multicentre, observational, pilot study. BMC Pulm Med. 2022;22(1):459.
Hirolli D, Srinivasaiah B, Muthuchellappan R, Chakrabarti D. Clinical scoring and ultrasound-based diaphragm assessment in predicting extubation failure in neurointensive care unit: a single-center observational study. Neurocrit Care. 2023.
Abdelwahed WM, Abd Elghafar MS, Amr YM, Alsherif SEI, Eltomey MA. Prospective study: diaphragmatic thickness as a predictor index for weaning from mechanical ventilation. J Crit Care. 2019;52:10–5.
Asmita AZ, Siddiqui AK, Mourya R, Singh GP, Abbas H. Comparison of ultrasound-based diaphragmatic thickness fraction (DTF) with rapid shallow breathing index and DTF alone for predicting successful weaning from mechanical ventilation: a randomised control trial. J Clin Diagn Res. 2020;16(6):67–71.
Blumhof S, Wheeler D, Thomas K, McCool FD, Mora J. Change in diaphragmatic thickness during the respiratory cycle predicts extubation success at various levels of pressure support ventilation. Lung. 2016;194(4):519–25.
Cavus MA, Bektas SG, Sipahioglu H, Zararsiz GE, Turan S. Power of diaphragm ultrasonography to predict weaning success. Cukurova Med J. 2022;47(2):747–55.
DiNino E, Gartman EJ, Sethi JM, McCool FD. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax. 2014;69(5):423–7.
Genty T, Laverdure F, Peyrouset O, Rezaiguia-Delclaux S, Thès J, Stéphan F. Extubation failure prediction by echography of the diaphragm after cardiothoracic surgery: the EXPEDIA study. Respir Care. 2022.
González-Aguirre JE, Rivera-Uribe CP, Rendón-Ramírez EJ, Cañamar-Lomas R, Serna-Rodríguez JA, Mercado-Longoría R. Pulmonary ultrasound and diaphragmatic shortening fraction combined analysis for extubation-failure-prediction in critical care patients. Arch Bronconeumol (Engl Ed). 2019;55(4):195–200.
Haaksma ME, Smit JM, Heldeweg M, Nooitgedacht JS, Atmowihardjo LN, Jonkman AH, et al. Holistic ultrasound to predict extubation failure in clinical practice. Respir Care. 2021;66(6):994–1003.
Kundu R, Baidya D, Anand R, Maitra S, Soni K, Subramanium R. Integrated ultrasound protocol in predicting weaning success and extubation failure: a prospective observational study. Anaesthesiol Intensive Ther. 2022;54(2):156–63.
McCool FD, Oyieng’o DO, Koo P. The utility of diaphragm ultrasound in reducing time to extubation. Lung. 2020;198(3):499–505.
Pirompanich P, Romsaiyut S. Use of diaphragm thickening fraction combined with rapid shallow breathing index for predicting success of weaning from mechanical ventilator in medical patients. J Intensive Care. 2018;6:6.
Soliman SB, Ragab F, Soliman RA, Gaber A, Kamal A. Chest ultrasound in predication of weaning failure. Open Access Maced J Med Sci. 2019;7(7):1143–7.
Trifi A, Abdellatif S, Ben Lamine F, Abdennebi C, Touil Y, Ben LS. Ultrasound assessment of the diaphragm during the first days of mechanical ventilation compared to spontaneous respiration: a comparative study. Tunis Med. 2021;99(11):1055–65.
Lalwani LK, Govindagoudar MB, Singh PK, Sharma M, Chaudhry D. The role of diaphragmatic thickness measurement in weaning prediction and its comparison with rapid shallow breathing index: a single-center experience. Acute Crit Care. 2022;37(3):347–54.
Vetrugno L, Orso D, Corradi F, Zani G, Spadaro S, Meroi F, et al. Diaphragm ultrasound evaluation during weaning from mechanical ventilation in COVID-19 patients: a pragmatic, cross-section, multicenter study. Respir Res. 2022;23(1):210.
Dres M, Similowski T, Goligher EC, Pham T, Sergenyuk L, Telias I, et al. Dyspnoea and respiratory muscle ultrasound to predict extubation failure. Eur Respir J. 2021;58(5).
Azeredo LM, Nemer SN, Barbas CS, Caldeira JB, Noé R, Guimarães BL, et al. The integrative weaning index in elderly ICU subjects. Respir Care. 2017;62(3):333–9.
Chittock DR, Uusaro A, Russell JA, Walley KR. Stress test and gastric-arterial PCO2 measurement improve prediction of successful extubation. Crit Care Med. 2000;28(7):2313–9.
Fernandez R, Raurich JM, Mut T, Blanco J, Santos A, Villagra A. Extubation failure: diagnostic value of occlusion pressure (P0.1) and P0.1-derived parameters. Intensive Care Med. 2004;30(2):234–40.
Hurtado FJ, Berón M, Olivera W, Garrido R, Silva J, Caragna E, et al. Gastric intramucosal pH and intraluminal PCO2 during weaning from mechanical ventilation. Crit Care Med. 2001;29(1):70–6.
Liu Y, Wei LQ, Li GQ, Lv FY, Wang H, Zhang YH, et al. A decision-tree model for predicting extubation outcome in elderly patients after a successful spontaneous breathing trial. Anesth Analg. 2010;111(5):1211–8.
Montgomery AB, Holle RH, Neagley SR, Pierson DJ, Schoene RB. Prediction of successful ventilator weaning using airway occlusion pressure and hypercapnic challenge. Chest. 1987;91(4):496–9.
Okamoto K, Sato T, Morioka T. Airway occlusion pressure (P0.1)—a useful predictor for the weaning outcome in patients with acute respiratory failure. J Anesth. 1990;4(2):95–101.
Rivera L, Weissman C. Dynamic ventilatory characteristics during weaning in postoperative critically ill patients. Anesth Analg. 1997;84(6):1250–5.
Vallverdú I, Calaf N, Subirana M, Net A, Benito S, Mancebo J. Clinical characteristics, respiratory functional parameters, and outcome of a two-hour T-piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med. 1998;158(6):1855–62.
Xu Q, Yang X, Qian Y, Hu C, Lu W, Cai S, et al. Speckle tracking quantification parasternal intercostal muscle longitudinal strain to predict weaning outcomes: a multicentric observational study. Shock. 2023;59(1):66–73.
Liu L, Liu H, Yang Y, Huang Y, Liu S, Beck J, et al. Neuroventilatory efficiency and extubation readiness in critically ill patients. Crit Care. 2012;16(4):R143.
Muttini S, Villani PG, Trimarco R, Bellani G, Grasselli G, Patroniti N. Relation between peak and integral of the diaphragm electromyographic activity at different levels of support during weaning from mechanical ventilation: a physiologic study. J Crit Care. 2015;30(1):7–12.
Dres M, Jung B, Molinari N, Manna F, Dubé BP, Chanques G, et al. Respective contribution of intensive care unit-acquired limb muscle and severe diaphragm weakness on weaning outcome and mortality: a post hoc analysis of two cohorts. Crit Care. 2019;23(1):370.
Qing Q, Liang M, Sun Q, Xie B, Yang C, Liang W, et al. Using twitch tracheal airway pressure, negative inhale forced pressure, and Medical Research Council score to guide weaning from mechanical ventilation. J Thorac Dis. 2018;10(7):4424–32.
Castro AA, Cortopassi F, Sabbag R, Torre-Bouscoulet L, Kümpel C, Ferreira PE. Respiratory muscle assessment in predicting extubation outcome in patients with stroke. Arch Bronconeumol. 2012;48(8):274–9.
Al Tayar AS, Abdelshafey EE. Diaphragm electromyography versus ultrasonography in the prediction of mechanical ventilation liberation outcome. Resp Care. 2022;67(11):1437–42.
Le Neindre A, Wormser J, Luperto M, Bruel C, Misset B, Bouhemad B, et al. Diaphragm function in patients with sepsis and septic shock: a longitudinal ultrasound study. Aust Crit Care. 2022.
Marini JJ, Smith T, Lamb V. Estimation of inspiratory muscle strength in mechanically ventilated patients: the measurement of maximal inspiratory pressure. J Crit Care. 1986;1(1):32–8.
American Thoracic Society. ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002;166(4):518–624.
Sabourin E, Carpentier C, Lai C, Monnet X, Pham T. “Under pressure”: Should we use diaphragm excursion to predict weaning success in patients receiving pressure support ventilation? Crit Care. 2023;27(1):238.
Takwoingi Y, Leeflang MM, Deeks JJ. Empirical evidence of the importance of comparative studies of diagnostic test accuracy. Ann Intern Med. 2013;158(7):544–54.
Leeflang MM, Moons KG, Reitsma JB, Zwinderman AH. Bias in sensitivity and specificity caused by data-driven selection of optimal cutoff values: mechanisms, magnitude, and solutions. Clin Chem. 2008;54(4):729–37.
Schmidt GA, Girard TD, Kress JP, Morris PE, Ouellette DR, Alhazzani W, et al. Official executive summary of an American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: liberation from mechanical ventilation in critically ill adults. Am J Respir Crit Care Med. 2017;195(1):115–9.
Thille AW, Richard JC, Brochard L. The decision to extubate in the intensive care unit. Am J Respir Crit Care Med. 2013;187(12):1294–302.
Haaksma ME, Smit JM, Boussuges A, Demoule A, Dres M, Ferrari G, et al. EXpert consensus On Diaphragm UltraSonography in the critically ill (EXODUS): a Delphi consensus statement on the measurement of diaphragm ultrasound-derived parameters in a critical care setting. Crit Care. 2022;26(1):99.
Garofalo E, Bruni A, Pelaia C, Landoni G, Zangrillo A, Antonelli M, et al. Comparisons of two diaphragm ultrasound-teaching programs: a multicenter randomized controlled educational study. Ultrasound J. 2019;11(1):21.
Le Neindre A, Hansell L, Wormser J, Gomes Lopes A, Diaz Lopez C, Romanet C, et al. Thoracic ultrasound influences physiotherapist’s clinical decision-making in respiratory management of critical care patients: a multicentre cohort study. Thorax. 2023;78(2):169–75.
Hayward SA, Janssen J. Use of thoracic ultrasound by physiotherapists: a scoping review of the literature. Physiotherapy. 2018;104(4):367–75.
Le Neindre A, Mongodi S, Philippart F, Bouhemad B. Thoracic ultrasound: potential new tool for physiotherapists in respiratory management. A narrative review. J Crit Care. 2016;31(1):101–9.
Lockstone J, Love A, Hung Lau Y, Hansell L, Ntoumenopoulos G. The use of diaphragm and lung ultrasound in acute respiratory physiotherapy practice and the impact on clinical decision-making: a systematic review and meta-analysis. Aust Crit Care. 2023.
Goligher EC, Laghi F, Detsky ME, Farias P, Murray A, Brace D, et al. Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensive Care Med. 2015;41(4):734.
Beduneau G, Pham T, Schortgen F, Piquilloud L, Zogheib E, Jonas M, et al. Epidemiology of weaning outcome according to a new definition. The WIND study. Am J Respir Crit Care Med. 2017;195(6):772–83.
Igarashi Y, Ogawa K, Nishimura K, Osawa S, Ohwada H, Yokobori S. Machine learning for predicting successful extubation in patients receiving mechanical ventilation. Front Med (Lausanne). 2022;9:961252.
Acknowledgements
We would like to thank Thomas Vandendriessche, expert on systematic reviews from the KU Leuven Biomedical library who helped us with the construction of the search string. The assistance of Tin Gojevic, Master student in Rehabilitation Sciences and Physiotherapy at KU Leuven, in title and abstract screening was much appreciated. We would also like to thank the authors who provided additional data and information when contacted: Guillaume Fossat, Mine Altınkaya Çavuş, Berrin Er, Clément Medrinal, Savino Spadaro, Eva Tenza-Lozano, Cédric Carrie, Martin Dres, Bharath Srinivasaiah, Nitesh Gupta, Luigi Vetrugno.
Funding
This study was funded by Research Foundation Flanders (FWO Project Grant G053721N). JYV was supported by the National Institute for Health and Care Research (NIHR) Community Healthcare MedTech and In Vitro Diagnostics Co-operative at Oxford Health NHS Foundation Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
DP, MVH, JYV, GH, RG, DL contributed to the conception and design of the study. DP, MVH, YQC, DRC, MRS, TG performed the title and abstract screening. DP, MVH, YQC, DRC performed the data extraction. YQC, DP, MVH and YQC organized the data and created the characteristic tables. DP, MVH and JYV performed the data analysis. DP and MVH wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Search string, characteristics tables of the studies, review-specific risk of bias rating guidance, supplementary figures and tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Poddighe, D., Van Hollebeke, M., Choudhary, Y.Q. et al. Accuracy of respiratory muscle assessments to predict weaning outcomes: a systematic review and comparative meta-analysis. Crit Care 28, 70 (2024). https://doi.org/10.1186/s13054-024-04823-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-024-04823-4