Abstract
Diaphragm weakness is highly prevalent in critically ill patients. It may exist prior to ICU admission and may precipitate the need for mechanical ventilation but it also frequently develops during the ICU stay. Several risk factors for diaphragm weakness have been identified; among them sepsis and mechanical ventilation play central roles. We employ the term critical illness-associated diaphragm weakness to refer to the collective effects of all mechanisms of diaphragm injury and weakness occurring in critically ill patients. Critical illness-associated diaphragm weakness is consistently associated with poor outcomes including increased ICU mortality, difficult weaning, and prolonged duration of mechanical ventilation. Bedside techniques for assessing the respiratory muscles promise to improve detection of diaphragm weakness and enable preventive or curative strategies. Inspiratory muscle training and pharmacological interventions may improve respiratory muscle function but data on clinical outcomes remain limited.
Similar content being viewed by others
Introduction
Skeletal muscle is a highly organized tissue, providing structural support, locomotion, breathing, shape, facial expression, and metabolic support to the body. The muscles of the respiratory system are precisely organized to facilitate inspiratory and expiratory air flow for respiration, airway clearance, and speech. The action of the diaphragm (the main inspiratory muscle) is usually quantified in terms of force generation (measured by inspiratory pressures) or shortening (measured by lung volume change or displacement of chest wall structures). Diaphragm weakness is defined as the inability of the diaphragm to generate normal levels of maximal force.
Accumulating evidence suggests that diaphragm weakness develops in a majority of critically ill patients exposed to mechanical ventilation [1,2,3,4,5]. The diaphragm is the main respiratory muscle and has a vital role in ventilation, but the prevalence and impact of diaphragm weakness have been often neglected with few recommendations for prevention and treatment. Different risk factors for critical illness-associated diaphragm weakness have been identified. Diaphragm weakness may pre-exist and precipitate respiratory failure. Acute diaphragm injury and weakness may also result from sepsis, trauma, systemic inflammation, or mechanical ventilation [6]. The wide range of potential injury mechanisms probably explains the high prevalence of diaphragm weakness observed in the ICU both in the early [2] and later stages of critical illness [3, 5]. We employ the term critical illness-associated diaphragm weakness to refer to the phenomenon of diaphragm weakness occurring in critically ill patients regardless of the cause and the timing. Herein we discuss the definition, prevalence, pathophysiology, and clinical consequences of critical illness-associated diaphragm weakness. We also discuss potential preventive and therapeutic strategies and highlight future avenues for research.
The normal diaphragm
The diaphragm is a thin, dome-shaped muscular structure separating the thoracic and abdominal cavities. Under normal conditions, the diaphragm acts much like a piston within a barrel, generating flow as its dome descends and displaces the abdominal contents beneath [7]. The pressure generated across the dome between the thoracic and abdominal cavities is called the transdiaphragmatic pressure (Pdi) and is proportional to the tension developed within the muscle fibers. The magnitude of the pressure swings on either side of the diaphragm depends on the volume change induced by diaphragmatic contraction and the elastance of the thorax and abdomen. For simplicity, the maximal Pdi is used as a global measure of diaphragm muscle force.
Techniques for monitoring diaphragm activity in critically ill patients
Diaphragm activity refers to the contractile forces generated by the muscle to maintain adequate ventilation under conditions of varying load. Strength refers to the maximal force-generating capacity of the muscle. These quantities can be assessed by the amount of pressure generated by diaphragm contraction. Hence, diaphragm force is evaluated on the basis of the pressure generated during maximal volitional inspiratory efforts (Pdi,max) or by non-volitional calibrated stimulation of the phrenic nerve (Table 1) [8].
The gold standard for assessing diaphragm force is measurement of Pdi generated by twitch magnetic stimulation of the phrenic nerves (Pdi,tw) [9]. The principal advantage of Pdi,tw is that it provides a standardized measure of pressure generation that is independent of the patient’s effort. This technique is performed by applying magnetic coils powered at their maximal output over the cervical portion of the phrenic nerves bilaterally (Fig. 1). Although not entirely identical to Pdi,tw, the twitch pressure generated at the outside tip of the endotracheal tube (Pet,tw) can be regarded as a surrogate of Pdi,tw that does not require esophageal and gastric balloons [9]. Pet,tw is now used widely in studies investigating diaphragm force [2,3,4,5].
Schematic representation of the phrenic nerve stimulation technique in patients ventilated with pressure support mode. Two magnetic coils are positioned at the initial portion of the phrenic nerves. Airway pressure is recorded at the tip of the endotracheal tube. First, the circuit is disconnected (white arrow) and twitches are generated by a magnetic stimulator (full black arrows). Diaphragm weakness is assessed by the amount of airway pressure generated during a magnetic twitch. Twitch A is followed by a reduced capacity to generate pressure (−8 cmH2O) [9], whereas twitch B is followed by normal drop of pressure (−30 cmH2O)
Diaphragm electromyography (EMG) can be used to assess diaphragm activity. The introduction of neurally adjusted ventilatory assist (NAVA), a ventilator mode that synchronizes ventilation to diaphragm electrical activity using a dedicated nasogastric tube with EMG electrodes, has greatly facilitated the bedside monitoring of crural diaphragm activity (EAdi). The ratio of actual EAdi to maximum EAdi (EAdi,max) can be used to estimate the patient’s effort to breathe [10]. For a given patient, EAdi is tightly correlated to the pressure generated by the diaphragm under various levels of ventilatory assistance [10]. EAdi is a promising tool to monitor diaphragm activity [11]; however, EAdi,max varies widely between subjects so that there is no clear reference range for EAdi.
Diaphragm ultrasound provides a direct visualization of the diaphragm. As the diaphragm contracts, it thickens, and the magnitude of the increase in thickness during inspiration can be expressed as a percentage increase in thickness (the thickening fraction of the diaphragm, TFdi) (Fig. 2). TFdi reflects the activity of the muscle during tidal breathing and provides an estimate of its strength during a maximal inspiratory effort (TFdi,max) [12]. There is a wide range of TFdi values: it is 0–5% in patients under neuromuscular blockade [13]; it ranges between 20% and 50% in spontaneously breathing patients after extubation [14]. TFdi is correlated with both the pressure–time product of the diaphragm and with EAdi [13, 14]. Some studies suggest that TFdi obtained during a maximal inspiratory effort [15] or quiet breathing in mechanically ventilated patients [16] can be employed to assess diaphragm force. Finally, ultrasound can also measure maximal diaphragm excursion, a marker that predicts extubation success and failure with reasonable sensitivity and specificity [17]. This latter index can only be interpreted during non-assisted breathing; otherwise the downward displacement of the diaphragm may reflect passive insufflation of the chest by the ventilator.
Diaphragm ultrasound using time-motion mode at three different conditions: quiet breathing, moderate inspiratory effort, and strong inspiratory effort. Note the increase in diaphragm end inspiratory thickness (Tei) at moderate and strong inspiratory effort. Tee end expiratory thickness, Tei end inspiratory thickness
Definition and prevalence of critical illness-associated diaphragm weakness
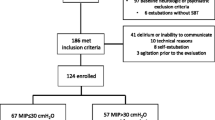
The pressure-based definition of diaphragm weakness using Pdi,tw is considered as the reference method but the Pet,tw method is easier to measure in the ICU [9]. Using the latter, one can define diaphragm weakness as a Pet,tw below 11 cmH2O [8, 18]. Several studies have characterized the prevalence of diaphragm weakness using this criterion (Table 2). With this definition, within 24 h after intubation, diaphragm weakness is present in up to 64% (54/85) of patients [2]. At the time of weaning, diaphragm weakness is present in between 63% [5] and 80% of patients [1, 3]. Approximately 80% of patients requiring prolonged mechanical ventilation exhibit diaphragm weakness [9, 19].
Ultrasound can also be used to define diaphragm weakness. Diaphragm excursion less than 1.1 cm during tidal breathing also defines diaphragm weakness [17]. Maximal TFdi below 20% is diagnostic of severe diaphragm weakness [15]. Studies employing the ultrasound-based definition of diaphragm weakness report that 29% of patients (24/82) have diaphragm weakness at the first spontaneous breathing trial [17] and 36% (20/55) at extubation [20].
Overlap with limb muscle acquired weakness
Critical illness polyneuropathy [21, 22] and myopathy are the major causes of limb weakness and wasting in the ICU. An extensive revision of the literature on ICU acquired weakness with indication on future research was recently published in this journal [23]. Mechanical ventilation may impose bed rest and may indirectly prolong immobility as a result of the use of sedatives or neuromuscular blocking agents which in turn may promote neuropathy, muscle wasting, and loss of muscle function [24]. Although it was initially thought to be rare, neuromuscular dysfunction is found in up to 25% of ICU patients requiring mechanical ventilation for more than 7 days [25]. While the diaphragm is characterized by a permanent cyclic activity, other striated muscles such as limb muscles are not constantly active. Furthermore, although both diaphragm and limb muscle are striated muscles, their fiber type composition differs [26]. Thus, the consequences of prolonged unloading of the diaphragm may be distinct from the consequences of unloading limb muscles, as demonstrated by experimental and clinical studies [27, 28]. At the time of weaning, diaphragm weakness is twice as frequent as limb muscle weakness [5] and patients with diaphragm weakness are no more or less likely to have limb muscle weakness [5]. While they share common features, diaphragm and limb muscle weakness likely represent two distinct entities with different pathophysiology.
Causes and mechanisms of critical illness-associated diaphragm weakness
Respiratory muscle weakness in critically ill patients may result from hyperinflation, neuropathies, myopathies, metabolic abnormalities, decreased oxygen delivery, and medications [29]. Myopathies are subdivided into several categories that include critical illness myopathy, sepsis-associated myopathy, ventilator-associated respiratory muscle injury, disuse atrophy, metabolic disturbances, and medications [29]. Another classification based on histology may be useful [21] but consideration of muscle unexcitability without muscle structural disarrangement is also possible [30]. In the sickest patients, it is likely that multiple factors take effect simultaneously. In addition, some factors (sepsis, injuriously high inspiratory efforts) present before admission in the ICU can contribute to diaphragm weakness and may in fact precipitate the need for mechanical ventilation. Certain patient factors may also prevent diaphragm weakness: one experimental model suggested a protective role for obesity [31]. We now summarize the complex interplay of contributors to diaphragm weakness before admission and during the ICU stay (Fig. 3).
Schematic illustration of mechanisms pathways involved in the occurrence of diaphragm weakness in critically ill patients. Note that the figure ignores cases of unexcitable muscle in which muscle injury may be reduced or nonexistent. Dashed lines represent uncertain causation and full black lines represent established causation
Mechanisms of diaphragm weakness at the time of ICU admission
Hypercapnic respiratory failure
Acute hypercapnia increases neural drive through chemoreflex activation; its effects on diaphragm contractility during spontaneous breathing are conflicting. In one study conducted in healthy subjects exposed to acute changes in CO2, diaphragm force was reduced [32]. Separately, hypercapnia did not intensify long-lasting fatigue but slightly reduced diaphragm contractility immediately after maximum voluntary ventilation [33]. However, no significant change in twitch pressure was reported while subjects breathed CO2 [34] or produced maximal contraction [33]. In vitro, respiratory acidosis induces diaphragm weakness in non-ventilated rats whereas metabolic acidosis has no effect [35]. In clinical practice, acute hypercapnia could contribute to clinical deterioration by favoring diaphragm weakness.
Cardiogenic shock
Cardiogenic shock is associated with both an increase in diaphragm work and a reduction in diaphragm oxygen delivery. The imbalance between oxygen supply and demand can ultimately result in diaphragm fatigue. This was demonstrated in dogs exposed to cardiogenic shock with tamponade, in which a marked reduction in Pdi was noted after 1 h despite an increase in central drive, ultimately causing death [36] (Fig. 4). Low cardiac output impairs respiratory muscle blood flow and the diaphragm may shift to anaerobic metabolism resulting in muscular lactate production [37]. Mechanical ventilation and muscle paralysis spare a large fraction of cardiac output used by the working respiratory muscles [38]. In one study highlighting the critical importance of respiratory muscle failure in shock states, spontaneously breathing dogs with cardiogenic shock were much more likely to die from ventilatory failure compared to mechanically ventilated dogs [37].

Adapted from Aubier et al. [36]
Schematic illustration of the effect of cardiogenic shock on transdiaphragmatic pressure (Pdi) and diaphragm electrical activity (Edi). While cardiogenic shock induced an important increase in Edi, late course is marked by a decrease in Pdi as a surrogate of diaphragm fatigue.
Sepsis
Both severe diaphragm weakness and increased susceptibility to injury and fatigue have been documented in animal models of sepsis [39,40,41]. Sepsis impairs diaphragm force apart from any effect on muscle mass or architecture [41], suggesting an important role for systemic inflammation. Sepsis acts at two levels [42]. First, disturbances in different steps of the chain of muscular energy supply including altered blood flow distribution (hypoxic ischemia) and use (cytopathic ischemia). Second, direct impairment of the contractile proteins resulting from the action of septic mediators such as cytokines can also result in dysfunction. Tumor necrosis factor alpha (TNF-α) has been shown to mediate the detrimental effects of endotoxin administration on the contractile function of the diaphragm [43].
Systemic inflammation also renders the diaphragm more sensitive to load-related injury, possibly by increasing sarcolemma membrane fragility [44]. In septic rats undergoing controlled mechanical ventilation, sepsis exacerbated diaphragm weakness resulting from controlled mechanical ventilation [45]. In the ICU, patients with sepsis are more likely to exhibit diaphragm atrophy [46]. Sepsis can be present early during the ICU stay as a primary reason for admission or later, complicating the course. Interestingly, experimental findings suggest that mechanical ventilation could alleviate the harmful effects of sepsis on diaphragm function [44]. Sepsis is associated with diaphragm weakness in more than half of mechanically ventilated patients [2, 19], and the potential interactions between sepsis and mechanical ventilation on diaphragm function require greater attention.
Surgery
Abdominal surgery, in particular of the upper abdomen, is associated with postoperative respiratory complications in which diaphragm dysfunction is frequently implicated [47, 48]. Although pain or general anesthesia may contribute to the phenomenon, pain relief does not ameliorate postoperative diaphragm force [49] and general anesthesia performed for lower abdominal surgery does not lead to diaphragm weakness. The attenuated phrenic nerve output following stimulation of visceral or somatic phrenic afferent pathways during surgery has been proposed as a possible alternate mechanism [29]. Diaphragm weakness has also been reported after coronary bypass surgery [48, 50]. In this case, the phrenic nerve can be directly injured (surgical manipulations, ischemia, cardioprotection) leading to left hemidiaphragm or bilateral weakness with important clinical consequences.
Risk factors for diaphragm weakness during ICU course
Sedatives, steroids, and neuromuscular blocking agents
Sedatives may have direct adverse effects on the diaphragm as well as promoting disuse. In patients undergoing anesthesia for elective surgery, propofol induces a decrease in the diaphragm’s capacity to generate pressure [51]. In ICU patients, the dose of propofol was correlated with the severity of diaphragm weakness [52]. Volatile anesthetics, some not in use anymore [53], have also been shown to cause diaphragm weakness [54].
Corticosteroids have been associated with the development of critical illness myopathy [25, 55]. Corticosteroids may affect contractile function of striated muscles by inhibition of protein synthesis and activation of protein degradation pathways. Nevertheless, the effects of corticosteroids on the diaphragm are not entirely predictable and may vary according to the regimen of administration, the specific corticosteroid, muscle fiber type, and possibly species. Importantly, corticosteroid doses administered in animal studies are often much higher than doses employed in clinical practice [56]. The effects of corticosteroids on diaphragm in ICU patients are therefore complex, but it is likely that diaphragm weakness is more severe with higher doses and a longer duration of exposure. Accordingly, administration of corticosteroids should be carefully guided by judicious evaluation of expected benefits and harm. While neuromuscular blockers are used to adapt patients to the ventilator, they render the diaphragm inactive and may contribute to diaphragm disuse and consequent atrophy. A particular concern exists when neuromuscular blockers are administrated in conjunction with glucocorticoids [55]. In animal models, rocuronium (aminosteroidal non-depolarizing neuromuscular blocker) exacerbates diaphragm weakness induced by controlled mechanical ventilation [57]. By contrast, cisatracurium (a non-steroidal benzyl isoquinoline non-depolarizing neuromuscular blocker) does not exacerbate the effects of ventilation on diaphragm force [58]. Importantly, when used for a short period (48 h) at the early phase of ARDS, cisatracurium did not induce ICU-acquired limb muscle weakness and increased ventilator-free days [59].
Mechanical ventilation
Mechanical ventilation has been clearly identified as a contributor to diaphragm weakness. It can be associated with adverse effects on respiratory muscles through two potentially competing mechanisms (Fig. 3): (1) disuse atrophy secondary to diaphragm inactivity from excessive ventilatory support, (2) load-induced injury due to insufficient ventilatory support and (3) hypercapnia under controlled mechanical ventilation.
Disuse atrophy
Just a few hours of fully controlled mechanical ventilation leads to rapid-onset atrophy and decreased contractile force both in vitro and in vivo [60–63]. Conversely, partially assisted mechanical ventilation mitigates atrophy and diaphragm weakness [61, 64]. Findings from animal models are difficult to replicate in critically ill patients who are frequently exposed to many risk factors for diaphragm injury. The first evidence in humans came from a study in 1988 by Knisely et al. who reported diaphragm atrophy in a postmortem series of neonates requiring long-term ventilation [65]. Twenty years later, Levine et al. found histological evidence of diaphragm atrophy among 14 adult brain-dead organ donors after meeting brain death criteria for 18–69 h [28]. Importantly, pectoralis muscle was unaffected in these patients over the same period of inactivity, suggesting that the rapid atrophy is specific to the diaphragm [28]. Diaphragm muscle fiber dysfunction is not only due to loss of muscle mass in these patients: the reduction in myofibrillar contractility also arises from deranged cross-bridge formation [66]. Diaphragm biopsies obtained from a heterogeneous group of ICU patients demonstrated the development of muscle fibers atrophy, activation of proteolysis, enhanced number of inflammatory cells in the muscle, and development of muscle fiber weakness [66]. Interestingly, force-generating capacity of the muscle fibers was reduced even after correction for loss of contractile protein, demonstrating the development of contractile protein dysfunction [66]. Although studies in animals and brain-dead patients suggested an important role for mitochondrial dysfunction and oxidative stress in the development of diaphragm dysfunction during mechanical ventilation [28, 67], mitochondrial morphology and function appeared normal in the diaphragm of ICU patients [68]. In addition, markers for oxidative stress and antioxidant enzymes in the diaphragm were not different between ICU and control patients [68].
Two studies reported a progressive decline of diaphragm force in vivo with increasing duration of mechanical ventilation [4, 52]. In a series of 76 patients, Dres et al. found that although the duration of mechanical ventilation from intubation to weaning was associated with the occurrence of diaphragm dysfunction, this effect did not persist in a multivariable analysis incorporating other risk factors [5]. More than mechanical ventilation itself, it is the unloading of the diaphragm under mechanical ventilation which is the critical contributor of diaphragm weakness. While the precise mechanism underlying disuse atrophy is debated [69], the deleterious effects of diaphragm unloading are strongly supported by experimental [60, 61] and clinical [70] data demonstrating that diaphragm atrophy and weakness can be attenuated by maintaining some level of respiratory muscle loading during ventilation.
Assuming that atrophy may be detected with ultrasound, Grosu et al. described a time-dependent decrease in diaphragm thickness in seven patients [71]. It was confirmed in larger cohorts [70, 72]. Goligher et al. reported a rapid decrease in diaphragm thickness in over 40% of mechanically ventilated patients [70]. Importantly, diaphragm atrophy occurred quickly and the largest magnitude in the change of diaphragm thickness was achieved by day 4. Moreover, the change in diaphragm thickness over time was related to the level of inspiratory effort [70]. Importantly, diaphragm thickness was relatively stable on days when diaphragm thickening fraction (a measure of inspiratory effort) was consistent with normal resting breathing [70].
Excessive loading
Excessive respiratory muscle loading can result in diaphragm injury, as demonstrated in both animal and human studies [73]. Tracheal banding (prolonged resistive loading) in hamsters resulted in ventilatory failure associated with diaphragm injury characterized by susceptibility of myofibrillar complexes to calpain-mediated degradation [74]. Diaphragm injury in this context is characterized by myofibrillar disarray and inflammatory infiltration [73]. Sepsis appears to sensitize the sarcolemma to stress-related injury (membrane hyperfragility) [44]. Load-induced diaphragm injury has also been demonstrated in humans, manifesting as a prolonged loss of force production after resistive loading [75] and sarcomere disruption on histology [76].
Eccentric contractions—where the muscle contracts as it is lengthened—may be particularly injurious [77]. Eccentric contractions may occur in the context of patient–ventilator dyssynchrony [77]. Contractile activity of the diaphragm during expiratory diaphragm lengthening was recently demonstrated in acute hypoxemic respiratory failure [78]. Whether eccentric contractions are sufficiently frequent and severe to cause diaphragm weakness in mechanically ventilated patients is unknown.
The concept of load-induced injury may explain recent findings showing increases in diaphragm thickness—possibly reflecting muscle inflammation and edema—in a subset of mechanically ventilated patients associated with high levels of inspiratory effort [70]. Insufficient or delayed unloading of the respiratory muscles in the context of acute respiratory failure may therefore contribute to diaphragm injury.
Hypercapnia under controlled ventilation
The effect of hypercapnia on diaphragm force under mechanical ventilation has been studied in experimental models. In ventilated and anesthetized piglets, acute and short exposure (6 h) to hypercapnia induces a marked reduction in diaphragm force as assessed by phrenic nerve stimulation [79]. However, when piglets are exposed to prolonged duration of mechanical ventilation (72 h), hypercapnia limited the occurrence of ventilator-induced diaphragm dysfunction (VIDD) [80], a finding that was confirmed in vitro [81]. Whether hypercapnia occurring in a patient failing a weaning test contributes to diaphragm weakness is unknown.
Clinical consequences of diaphragm weakness
Irrespective of whether it is present at admission [2] or at a later stage [3, 5, 19], diaphragm weakness is a marker of illness severity and of poor prognosis. Diaphragm weakness diagnosed at the time of ICU admission demonstrates that critical illness can impair diaphragm function even before the patient is admitted to the ICU. At the early stage of critical illness, diaphragm weakness is analogous to any other form of organ dysfunction and its presence is associated with higher mortality [2]. To what extent diaphragm weakness can contribute to a poor prognosis has not been elucidated. Importantly, diaphragm weakness can improve despite exposure to mechanical ventilation [82]. Similar to a reversible septic cardiomyopathy, sepsis-related diaphragm weakness observed upon admission may be readily reversible. Nevertheless, the time of course and the determinants of the recovery need to be clarified in further studies. The extent to which early diaphragm weakness [2] constitutes a risk factor for later critical illness-associated diaphragm weakness is unknown. Diaphragm weakness detected after several days of mechanical ventilation is strongly associated with weaning failure [3, 5, 17, 50]. Diaphragm weakness entails limited physiological reserve in the face of new pulmonary insults. In isolation, it is usually not sufficient to precipitate respiratory failure, but in the presence of high ventilatory demands or deteriorating respiratory mechanics it may rapidly result in weaning or extubation failure. Diaphragm weakness can indeed also be present in patients who are successfully liberated from ventilation [3, 5]. Some findings already suggest a high risk of hospital readmission in patients with chronic respiratory failure in case of respiratory muscle weakness 7 days after ICU discharge [83]. Another study reported increased mortality after 1 year [84]. Further research looking at the impact of diaphragm weakness on long-term survival, exercise tolerance, and quality of life is therefore warranted.
Prevention and treatment of diaphragm weakness
Prevention strategies
Table 3 summarizes a number of strategies aimed at preventing and treating diaphragm weakness in critically ill patients. Animal studies [64] and recent clinical investigations [70] suggest that maintaining spontaneous breathing under mechanical ventilation should minimize diaphragm atrophy. Muscle-protective ventilation strategies should therefore aim at titrating ventilation (and sedation) to maintain appropriate levels of inspiratory muscle effort and minimize patient–ventilator asynchrony [85].
In specific circumstances such as ARDS, some preliminary findings suggest that spontaneous breathing could be directly harmful to the lungs by generating or worsening lung injury [86], in particular in patients with high respiratory drive. Preliminary exploratory data suggest that in these patients control of the level of respiratory muscle activity and tidal volume with partial neuromuscular blockade could be feasible [87]. Monitoring diaphragm activity is possible at the bedside through NAVA catheter, esophageal catheter, or diaphragm ultrasound. Further studies are needed to determine the upper and lower boundaries of the amount of diaphragm activity preventing diaphragm atrophy and subsequent dysfunction and diaphragm injury. Monitoring P0.1 as an index of respiratory drive is also a potentially useful technique to guide the ventilator titration [88]. Proportional assist ventilation and NAVA are two modes during which the level of respiratory muscle activity can be monitored [10, 89]. Diaphragm pacing has been investigated in experimental [90] and human [91] studies suggesting that intermittent contractions of the diaphragm may prevent atrophy. This strategy has been applied through a transvenous phrenic nerve pacing system designed to be percutaneously placed in the left subclavian vein. Additionally, pharmacologic approaches aiming at targeting mitochondrial and cellular pathways of diaphragm dysfunction are currently being investigated [92].
Management strategies
Hypophosphatemia impairs the contractile properties of the diaphragm during acute respiratory failure [93]. In the case of weaning failure, the level of plasmatic phosphatemia may be therefore monitored and corrected if required [94]. There has been great interest in improving diaphragm inotropy, by using inhibition of phosphodiesterase (PDE)3 and PDE4 (theophylline, 1,3-dimethylxanthine) [95] or calcium sensitizer levosimendan [96]. Theophylline has been extensively studied but has a narrow non-toxic therapeutic range. A retrospective cohort analysis reported improvement in diaphragm movements in 21/40 patients with VIDD who received low-dose theophylline [97]. Levosimendan has been shown to reverse diaphragm contractility in healthy subjects exposed to loaded breathing [96]. A randomized clinical trial (NCT01721434) is currently investigating whether levosimendan could facilitate liberation from the ventilator. Inspiratory muscle training can be instituted to enhance muscle endurance or strength. It is a strategy that can be achieved with rehabilitation protocols that use progressive threshold loading [98]. Although an attractive approach, inspiratory muscle training has not been well tested and proven as an intervention enabling one to improve clinical outcomes significantly. As a treatment, diaphragm pacing may be interesting in difficult-to-wean patients as it is currently under investigation (NCT03096639).
Conclusion
There is an expanding body of evidence showing both that diaphragm force is influenced by many factors in the ICU and that diaphragm weakness is frequent. The right balance between lung protective mechanical ventilation strategy and maintaining diaphragm activity has to be better investigated and may be challenging for clinicians. Monitoring diaphragm activity may prove to be necessary. Diaphragm ultrasound is a promising tool for monitoring diaphragm activity but the optimal range of inspiratory effort warrants further investigation. In addition, the potential recovery of diaphragm weakness after extubation should be determined. It may provide guidance for future therapies.
References
Laghi F, Cattapan SE, Jubran A et al (2003) Is weaning failure caused by low-frequency fatigue of the diaphragm? Am J Respir Crit Care Med 167:120–127. doi:10.1164/rccm.200210-1246OC
Demoule A, Jung B, Prodanovic H et al (2013) Diaphragm dysfunction on admission to the intensive care unit. Prevalence, risk factors, and prognostic impact—a prospective study. Am J Respir Crit Care Med 188:213–219. doi:10.1164/rccm.201209-1668OC
Jung B, Moury PH, Mahul M et al (2016) Diaphragmatic dysfunction in patients with ICU-acquired weakness and its impact on extubation failure. Intensive Care Med 42:853–861. doi:10.1007/s00134-015-4125-2
Jaber S, Petrof BJ, Jung B et al (2011) Rapidly progressive diaphragmatic weakness and injury during mechanical ventilation in humans. Am J Respir Crit Care Med 183:364–371. doi:10.1164/rccm.201004-0670OC
Dres M, Dubé B-P, Mayaux J et al (2017) Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am J Respir Crit Care Med 195:57–66. doi:10.1164/rccm.201602-0367OC
Vassilakopoulos T, Petrof BJ (2004) Ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med 169:336–341. doi:10.1164/rccm.200304-489CP
Gauthier AP, Verbanck S, Estenne M et al (1994) Three-dimensional reconstruction of the in vivo human diaphragm shape at different lung volumes. J Appl Physiol (1985) 76:495–506
American Thoracic Society/European Respiratory Society (2002) ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med 166:518–624. doi:10.1164/rccm.166.4.518
Watson AC, Hughes PD, Louise Harris M et al (2001) Measurement of twitch transdiaphragmatic, esophageal, and endotracheal tube pressure with bilateral anterolateral magnetic phrenic nerve stimulation in patients in the intensive care unit. Crit Care Med 29:1325–1331
Bellani G, Mauri T, Coppadoro A et al (2013) Estimation of patient’s inspiratory effort from the electrical activity of the diaphragm. Crit Care Med. doi:10.1097/CCM.0b013e31827caba0
Dres M, Schmidt M, Ferre A et al (2012) Diaphragm electromyographic activity as a predictor of weaning failure. Intensive Care Med 38:2017–2025. doi:10.1007/s00134-012-2700-3
Ueki J, De Bruin PF, Pride NB (1995) In vivo assessment of diaphragm contraction by ultrasound in normal subjects. Thorax 50:1157–1161
Goligher EC, Laghi F, Detsky ME et al (2015) Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensive Care Med 41:642–649. doi:10.1007/s00134-015-3687-3
Vivier E, Mekontso Dessap A, Dimassi S et al (2012) Diaphragm ultrasonography to estimate the work of breathing during non-invasive ventilation. Intensive Care Med 38:796–803. doi:10.1007/s00134-012-2547-7
Gottesman E, McCool FD (1997) Ultrasound evaluation of the paralyzed diaphragm. Am J Respir Crit Care Med 155:1570–1574. doi:10.1164/ajrccm.155.5.9154859
Dubé B-P, Dres M, Mayaux J et al (2017) Ultrasound evaluation of diaphragm function in mechanically ventilated patients: comparison to phrenic stimulation and prognostic implications. Thorax. doi:10.1136/thoraxjnl-2016-209459
Kim WY, Suh HJ, Hong S-B et al (2011) Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med 39:2627–2630. doi:10.1097/CCM.0b013e3182266408
Hamnegåard CH, Wragg S, Kyroussis D et al (1995) Mouth pressure in response to magnetic stimulation of the phrenic nerves. Thorax 50:620–624
Supinski GS, Callahan LA (2013) Diaphragm weakness in mechanically ventilated critically ill patients. Crit Care 17:R120. doi:10.1186/cc12792
Jiang J-R, Tsai T-H, Jerng J-S et al (2004) Ultrasonographic evaluation of liver/spleen movements and extubation outcome. Chest 126:179–185. doi:10.1378/chest.126.1.179
Latronico N, Bolton CF (2011) Critical illness polyneuropathy and myopathy: a major cause of muscle weakness and paralysis. Lancet Neurol 10:931–941. doi:10.1016/S1474-4422(11)70178-8
Fan E, Cheek F, Chlan L et al (2014) An official American Thoracic Society clinical practice guideline: the diagnosis of intensive care unit-acquired weakness in adults. Am J Respir Crit Care Med 190:1437–1446. doi:10.1164/rccm.201411-2011ST
Latronico N, Herridge M, Hopkins RO et al (2017) The ICM research agenda on intensive care unit-acquired weakness. Intensive Care Med. doi:10.1007/s00134-017-4757-5
Puthucheary ZA, Rawal J, McPhail M et al (2013) Acute skeletal muscle wasting in critical illness. JAMA 310:1591–1600. doi:10.1001/jama.2013.278481
De Jonghe B, Sharshar T, Lefaucheur J-P et al (2002) Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA 288:2859–2867
Polla B, D’Antona G, Bottinelli R, Reggiani C (2004) Respiratory muscle fibres: specialisation and plasticity. Thorax 59:808–817. doi:10.1136/thx.2003.009894
Mrozek S, Jung B, Petrof BJ et al (2012) Rapid onset of specific diaphragm weakness in a healthy murine model of ventilator-induced diaphragmatic dysfunction. Anesthesiology 117:560–567. doi:10.1097/ALN.0b013e318261e7f8
Levine S, Nguyen T, Taylor N et al (2008) Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med 358:1327–1335. doi:10.1056/NEJMoa070447
Laghi F, Tobin MJ (2003) Disorders of the respiratory muscles. Am J Respir Crit Care Med 168:10–48. doi:10.1164/rccm.2206020
Friedrich O, Reid MB, Van den Berghe G et al (2015) The sick and the weak: neuropathies/myopathies in the critically ill. Physiol Rev 95:1025–1109. doi:10.1152/physrev.00028.2014
De Jong A, Carreira S, Na N et al (2017) Diaphragmatic function is enhanced in fatty and diabetic fatty rats. PLoS One 12:e0174043. doi:10.1371/journal.pone.0174043
Juan G, Calverley P, Talamo C et al (1984) Effect of carbon dioxide on diaphragmatic function in human beings. N Engl J Med 310:874–879. doi:10.1056/NEJM198404053101402
Rafferty GF, Lou Harris M, Polkey MI et al (1999) Effect of hypercapnia on maximal voluntary ventilation and diaphragm fatigue in normal humans. Am J Respir Crit Care Med 160:1567–1571. doi:10.1164/ajrccm.160.5.9801114
Mador MJ, Wendel T, Kufel TJ (1997) Effect of acute hypercapnia on diaphragmatic and limb muscle contractility. Am J Respir Crit Care Med 155:1590–1595. doi:10.1164/ajrccm.155.5.9154862
Michelet P, Carreira S, Demoule A et al (2015) Effects of acute respiratory and metabolic acidosis on diaphragm muscle obtained from rats. Anesthesiology 122:876–883. doi:10.1097/ALN.0000000000000574
Aubier M, Trippenbach T, Roussos C (1981) Respiratory muscle fatigue during cardiogenic shock. J Appl Physiol 51:499–508
Aubier M, Viires N, Syllie G et al (1982) Respiratory muscle contribution to lactic acidosis in low cardiac output. Am Rev Respir Dis 126:648–652. doi:10.1164/arrd.1982.126.4.648
Viires N, Sillye G, Aubier M et al (1983) Regional blood flow distribution in dog during induced hypotension and low cardiac output. Spontaneous breathing versus artificial ventilation. J Clin Invest 72:935–947. doi:10.1172/JCI111065
Hussain SN, Simkus G, Roussos C (1985) Respiratory muscle fatigue: a cause of ventilatory failure in septic shock. J Appl Physiol (1985) 58:2033–2040
Leon A, Boczkowski J, Dureuil B et al (1992) Effects of endotoxic shock on diaphragmatic function in mechanically ventilated rats. J Appl Physiol (1985) 72:1466–1472
Boczkowski J, Dureuil B, Branger C et al (1988) Effects of sepsis on diaphragmatic function in rats. Am Rev Respir Dis 138:260–265. doi:10.1164/ajrccm/138.2.260
Lanone S, Taillé C, Boczkowski J, Aubier M (2005) Diaphragmatic fatigue during sepsis and septic shock. Intensive Care Med 31:1611–1617. doi:10.1007/s00134-005-2748-4
Shindoh C, Hida W, Ohkawara Y et al (1995) TNF-alpha mRNA expression in diaphragm muscle after endotoxin administration. Am J Respir Crit Care Med 152:1690–1696. doi:10.1164/ajrccm.152.5.7582314
Ebihara S, Hussain SNA, Danialou G et al (2002) Mechanical ventilation protects against diaphragm injury in sepsis: interaction of oxidative and mechanical stresses. Am J Respir Crit Care Med 165:221–228. doi:10.1164/ajrccm.165.2.2108041
Maes K, Stamiris A, Thomas D et al (2014) Effects of controlled mechanical ventilation on sepsis-induced diaphragm dysfunction in rats. Crit Care Med 42:e772–e782. doi:10.1097/CCM.0000000000000685
Jung B, Nougaret S, Conseil M et al (2014) Sepsis is associated with a preferential diaphragmatic atrophy: a critically ill patient study using tridimensional computed tomography. Anesthesiology 120:1182–1191. doi:10.1097/ALN.0000000000000201
Dureuil B, Viirès N, Cantineau JP et al (1986) Diaphragmatic contractility after upper abdominal surgery. J Appl Physiol (1985) 61:1775–1780
Diehl JL, Lofaso F, Deleuze P et al (1994) Clinically relevant diaphragmatic dysfunction after cardiac operations. J Thorac Cardiovasc Surg 107:487–498
Simonneau G, Vivien A, Sartene R et al (1983) Diaphragm dysfunction induced by upper abdominal surgery. Role of postoperative pain. Am Rev Respir Dis 128:899–903
Lerolle N, Guérot E, Dimassi S et al (2009) Ultrasonographic diagnostic criterion for severe diaphragmatic dysfunction after cardiac surgery. Chest 135:401–407. doi:10.1378/chest.08-1531
Shaw IC, Mills GH, Turnbull D (2002) The effect of propofol on airway pressures generated by magnetic stimulation of the phrenic nerves. Intensive Care Med 28:891–897. doi:10.1007/s00134-002-1347-x
Hermans G, Agten A, Testelmans D et al (2010) Increased duration of mechanical ventilation is associated with decreased diaphragmatic force: a prospective observational study. Crit Care 14:R127. doi:10.1186/cc9094
Bouhemad B, Langeron O, Orliaguet G et al (2002) Effects of halothane and isoflurane on the contraction, relaxation and energetics of rat diaphragmatic muscle. Br J Anaesth 89:479–485
Veber B, Dureuil B, Viires N et al (1989) Effects of isoflurane on contractile properties of diaphragm. Anesthesiology 70:684–688
Kress JP, Hall JB (2014) ICU-acquired weakness and recovery from critical illness. N Engl J Med 371:287–288. doi:10.1056/NEJMc1406274
Sassoon CS, Caiozzo VJ (2009) Bench-to-bedside review: diaphragm muscle function in disuse and acute high-dose corticosteroid treatment. Crit Care 13:221. doi:10.1186/cc7971
Testelmans D, Maes K, Wouters P et al (2006) Rocuronium exacerbates mechanical ventilation-induced diaphragm dysfunction in rats. Crit Care Med 34:3018–3023. doi:10.1097/01.CCM.0000245783.28478.AD
Testelmans D, Maes K, Wouters P et al (2007) Infusions of rocuronium and cisatracurium exert different effects on rat diaphragm function. Intensive Care Med 33:872–879. doi:10.1007/s00134-007-0584-4
Papazian L, Forel J-M, Gacouin A et al (2010) Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 363:1107–1116. doi:10.1056/NEJMoa1005372
Le Bourdelles G, Viires N, Boczkowski J et al (1994) Effects of mechanical ventilation on diaphragmatic contractile properties in rats. Am J Respir Crit Care Med 149:1539–1544. doi:10.1164/ajrccm.149.6.8004310
Sassoon CS, Caiozzo VJ, Manka A, Sieck GC (2002) Altered diaphragm contractile properties with controlled mechanical ventilation. J Appl Physiol 92:2585–2595. doi:10.1152/japplphysiol.01213.2001
Powers SK, Shanely RA, Coombes JS et al (2002) Mechanical ventilation results in progressive contractile dysfunction in the diaphragm. J Appl Physiol 92:1851–1858. doi:10.1152/japplphysiol.00881.2001
Anzueto A, Peters JI, Tobin MJ et al (1997) Effects of prolonged controlled mechanical ventilation on diaphragmatic function in healthy adult baboons. Crit Care Med 25:1187–1190
Jung B, Constantin J-M, Rossel N et al (2010) Adaptive support ventilation prevents ventilator-induced diaphragmatic dysfunction in piglet: an in vivo and in vitro study. Anesthesiology 112:1435–1443. doi:10.1097/ALN.0b013e3181d7b036
Knisely AS, Leal SM, Singer DB (1988) Abnormalities of diaphragmatic muscle in neonates with ventilated lungs. J Pediatr 113:1074–1077
Hooijman PE, Beishuizen A, Witt CC et al (2015) Diaphragm muscle fiber weakness and ubiquitin–proteasome activation in critically ill patients. Am J Respir Crit Care Med 191:1126–1138. doi:10.1164/rccm.201412-2214OC
Picard M, Jung B, Liang F et al (2012) Mitochondrial dysfunction and lipid accumulation in the human diaphragm during mechanical ventilation. Am J Respir Crit Care Med 186:1140–1149. doi:10.1164/rccm.201206-0982OC
van den Berg M, Hooijman PE, Beishuizen A et al (2017) Diaphragm Atrophy and weakness in the absence of mitochondrial dysfunction in the critically ill. Am J Respir Crit Care Med. doi:10.1164/rccm.201703-0501OC
Sieck GC, Mantilla CB (2013) CrossTalk opposing view: the diaphragm muscle does not atrophy as a result of inactivity. J Physiol 591:5259–5262. doi:10.1113/jphysiol.2013.254698
Goligher EC, Fan E, Herridge MS et al (2015) Evolution of diaphragm thickness during mechanical ventilation: impact of inspiratory effort. Am J Respir Crit Care Med. doi:10.1164/rccm.201503-0620OC
Grosu HB, Lee YI, Lee J et al (2012) Diaphragm muscle thinning in patients who are mechanically ventilated. Chest 142:1455–1460. doi:10.1378/chest.11-1638
Schepens T, Verbrugghe W, Dams K et al (2015) The course of diaphragm atrophy in ventilated patients assessed with ultrasound: a longitudinal cohort study. Crit Care 19:422. doi:10.1186/s13054-015-1141-0
Jiang TX, Reid WD, Belcastro A, Road JD (1998) Load dependence of secondary diaphragm inflammation and injury after acute inspiratory loading. Am J Respir Crit Care Med 157:230–236. doi:10.1164/ajrccm.157.1.9702051
Reid WD, Huang J, Bryson S et al (1994) Diaphragm injury and myofibrillar structure induced by resistive loading. J Appl Physiol (1985) 76:176–184
Laghi F, D’Alfonso N, Tobin MJ (1995) Pattern of recovery from diaphragmatic fatigue over 24 hours. J Appl Physiol (1985) 79:539–546
Orozco-Levi M, Lloreta J, Minguella J et al (2001) Injury of the human diaphragm associated with exertion and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 164:1734–1739. doi:10.1164/ajrccm.164.9.2011150
Gea J, Zhu E, Gáldiz JB et al (2009) Functional consequences of eccentric contractions of the diaphragm. Arch Bronconeumol 45:68–74. doi:10.1016/j.arbres.2008.04.003
Pellegrini M, Hedenstierna G, Roneus A et al (2016) The diaphragm acts as a brake during expiration to prevent lung collapse. Am J Respir Crit Care Med. doi:10.1164/rccm.201605-0992OC
Jaber S, Jung B, Sebbane M et al (2008) Alteration of the piglet diaphragm contractility in vivo and its recovery after acute hypercapnia. Anesthesiology 108:651–658. doi:10.1097/ALN.0b013e31816725a6
Jung B, Sebbane M, Le Goff C et al (2013) Moderate and prolonged hypercapnic acidosis may protect against ventilator-induced diaphragmatic dysfunction in healthy piglet: an in vivo study. Crit Care 17:R15. doi:10.1186/cc12486
Schellekens W-JM, van Hees HWH, Kox M et al (2014) Hypercapnia attenuates ventilator-induced diaphragm atrophy and modulates dysfunction. Crit Care 18:R28. doi:10.1186/cc13719
Demoule A, Molinari N, Jung B et al (2016) Patterns of diaphragm function in critically ill patients receiving prolonged mechanical ventilation: a prospective longitudinal study. Ann Intensive Care 6:75. doi:10.1186/s13613-016-0179-8
Adler D, Dupuis-Lozeron E, Richard J-C et al (2014) Does inspiratory muscle dysfunction predict readmission after intensive care unit discharge? Am J Respir Crit Care Med 190:347–350. doi:10.1164/rccm.201404-0655LE
Medrinal C, Prieur G, Frenoy É et al (2016) Respiratory weakness after mechanical ventilation is associated with one-year mortality—a prospective study. Crit Care 20:231. doi:10.1186/s13054-016-1418-y
Thille AW, Cabello B, Galia F et al (2008) Reduction of patient-ventilator asynchrony by reducing tidal volume during pressure-support ventilation. Intensive Care Med 34:1477–1486. doi:10.1007/s00134-008-1121-9
Yoshida T, Torsani V, Gomes S et al (2013) Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med 188:1420–1427. doi:10.1164/rccm.201303-0539OC
Doorduin J, Nollet JL, Roesthuis LH et al (2016) Partial neuromuscular blockade during partial ventilatory support in sedated patients with high tidal volumes. Am J Respir Crit Care Med. doi:10.1164/rccm.201605-1016OC
Iotti GA, Braschi A (2001) Closed-loop support of ventilatory workload: the P0.1 controller. Respir Care Clin N Am 7:441–464, ix
Carteaux G, Mancebo J, Mercat A et al (2013) Bedside adjustment of proportional assist ventilation to target a predefined range of respiratory effort. Crit Care Med 41:2125–2132. doi:10.1097/CCM.0b013e31828a42e5
Reynolds SC, Meyyappan R, Thakkar V et al (2017) Mitigation of ventilator-induced diaphragm atrophy by transvenous phrenic nerve stimulation. Am J Respir Crit Care Med 195:339–348. doi:10.1164/rccm.201502-0363OC
Martin AD, Joseph A-M, Beaver TM et al (2014) Effect of intermittent phrenic nerve stimulation during cardiothoracic surgery on mitochondrial respiration in the human diaphragm. Crit Care Med 42:e152–e156. doi:10.1097/CCM.0b013e3182a63fdf
Schellekens W-JM, van Hees HWH, Doorduin J et al (2016) Strategies to optimize respiratory muscle function in ICU patients. Crit Care 20:103. doi:10.1186/s13054-016-1280-y
Aubier M, Murciano D, Lecocguic Y et al (1985) Effect of hypophosphatemia on diaphragmatic contractility in patients with acute respiratory failure. N Engl J Med 313:420–424. doi:10.1056/NEJM198508153130705
Alsumrain MH, Jawad SA, Imran NB et al (2010) Association of hypophosphatemia with failure-to-wean from mechanical ventilation. Ann Clin Lab Sci 40:144–148
Aubier M (1987) Effect of theophylline on diaphragmatic muscle function. Chest 92:27S–31S
Doorduin J, Sinderby CA, Beck J et al (2012) The calcium sensitizer levosimendan improves human diaphragm function. Am J Respir Crit Care Med 185:90–95. doi:10.1164/rccm.201107-1268OC
Kim W-Y, Park SH, Kim WY et al (2016) Effect of theophylline on ventilator-induced diaphragmatic dysfunction. J Crit Care 33:145–150. doi:10.1016/j.jcrc.2016.01.007
Martin AD, Smith BK, Davenport PD et al (2011) Inspiratory muscle strength training improves weaning outcome in failure to wean patients: a randomized trial. Crit Care 15:R84. doi:10.1186/cc10081
DiNino E, Gartman EJ, Sethi JM, McCool FD (2014) Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax 69(5):423–427
Acknowledgements
This work was supported by the Department of Critical Care Medicine, St. Michael’s Hospital, Toronto, Canada. LB holds the Keenan Chair in Acute Respiratory Failure and Critical Care Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
MD gave lectures for Pulsion Medical Systems. LB’s research laboratory received research grants and/or equipment from Covidien, General Electric, Fisher Paykel, Maquet (with St. Michael’s Hospital), and Philips. LH received speakers fee from Maquet Critical Care and Orion Pharma. His lab received research grants from Orion Pharma and Liberate Medical. EG declares no conflict of interest.
Funding
MD was supported by the French Intensive Care Society, the Short-Term Fellowship Program of the European Respiratory Society, the Bernhard Dräger Award for advanced treatment of ARF of the European Society of Intensive Care Medicine, the Assistance Publique—Hôpitaux de Paris, and the Fondation pour la Recherche Médicale (FDM 20150734498).
Rights and permissions
About this article
Cite this article
Dres, M., Goligher, E.C., Heunks, L.M.A. et al. Critical illness-associated diaphragm weakness. Intensive Care Med 43, 1441–1452 (2017). https://doi.org/10.1007/s00134-017-4928-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-017-4928-4