Abstract
Background
Diaphragm ultrasound (DUS) is a well-established point of care modality for assessment of dimensional and functional aspects of the diaphragm. Amongst various measures, diaphragmatic thickening fraction (DTf) is more comprehensive. However, there is still uncertainty about its capability to predict weaning from mechanical ventilation (MV). The present prospective observational exploratory study assessed the diaphragm at variable negative pressure triggers (NPTs) with US to predict weaning in ICU patients.
Methods
Adult ICU patients about to receive their first T-piece were included in the study. Linear and curvilinear US probes were used to measure right side diaphragm characteristics first at pressure support ventilation (PSV) of 8 cmH2O with positive end expiratory pressure (PEEP) of 5 cmH2O against NPTs of 2, 4, and 6 cmH2O and then later during their first T-piece. The measured variables were then categorized into simple weaning (SW) and complicated weaning (CW) groups and their outcomes analyzed.
Results
Sixty-four (M:F, 40:24) medical (55/64, 86%) patients were included in the study. Sepsis of lung origin (65.5%) was the dominant reason for MV. There were 33 and 31 patients in the SW and CW groups, respectively. DTf predicts SW with a cutoff ≥ 25.5, 26.5, 25.5, and 24.5 for 2, 4, and 6 NPTs and T-piece, respectively, with ≥ 0.90 ROC AUC. At NPT of 2, DTf had the highest sensitivity of 97% and specificity of 81% [ROC AUC (CI), 0.91 (0.84–0.99); p < 0.001].
Conclusions
DTf may successfully predict SW and also help identify patients ready to wean prior to a T-piece trial.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Weaning from mechanical ventilation (MV) is one of the major challenges faced by intensivists. Premature [1, 2] and delayed [3, 4] weaning are both detrimental in patients admitted in the intensive care unit (ICU). Weaning consumes approximately 40% time of ventilation [5]. While majority weaning is simple, difficult weaning is encountered in 20–25% of patients [6]. The diaphragm, the main inspiratory muscle, is affected by multiple factors in critical illness [7, 8], including disuse atrophy as a result of MV itself [9,10,11,12]. Diaphragm dysfunction also results in prolonged MV, weaning failure [13, 14], and increased mortality [15].
In 2007, the International Task Force of Respiratory and Critical Care Societies categorized weaning into simple, difficult, and prolonged [16]. Later in 2010, the incidence and outcomes of these new weaning categories were further studied [17]. In spite of subjective and objective extubation and weaning criteria, predicting a successful outcome is still difficult. Although several traditional tools to predict successful outcomes exist, their precision and accuracy are variable [18,19,20]. Diaphragm ultrasound (DUS) is a well-established point of care modality for assessment of dimensional and functional aspects of the diaphragm [14, 21]. Diaphragmatic thickening fraction (DTf (%)) reflects the magnitude of diaphragmatic effort and may predict successful weaning [22, 23].
We proposed to confirm the utility of DUS to assess muscle function in response to a maximal volitional inspiratory effort. In order to test the hypothesis that DUS-based measurements can successfully predict weaning, we conducted the present prospective exploratory study in adult critically ill ICU patients at variable negative pressure triggers (NPTs) both prior and during a T-piece trial. We in our present study also attempted to explore DUS-based parameters in the above-mentioned weaning categories.
Methods
Ethics and consent
After prior approval from the ethics committee (Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, UP, India) and obtaining patient’s written informed consent, we conducted the present prospective exploratory study. The study period was from January 2015 to June 2016. A 12-bed closed, medical, surgical, adult, and pediatric ICU of a tertiary care referral hospital and academic institute in north of India was used for this purpose. The clinical management of patients was at the discretion of the ICU treating team in accordance with the contemporary best ICU practices. No interventions or therapy was modified based on the study findings.
Inclusion criteria
Patients aged ≥ 18 years, admitted to ICU and receiving MV longer than 24 h and about to be subjected to their first T-piece after satisfying conventional criteria for ready to wean from ventilator, were enrolled in the study. DUS examinations were performed initially at pressure support ventilation (PSV) with variable NPTs, and then 6–12 h later during the first T-piece trial.
Exclusion criteria
Patients aged < 18 years, ventilated for less than 24 h, with preexisting diaphragm disease, increased intra-abdominal pressure, any breach in skin preventing DUS examinations in subcostal area, phrenic nerve palsy, and refusal of consent were excluded from study. Patients who deteriorated with application of PSV at NPTs or during the T-piece were also excluded.
Study protocol
Patients on MV received their first T-piece when they were afebrile, alert, cooperative, and hemodynamically stable without vasopressor support and PaO2/FiO2 ratio > 200 was achievable at FiO2 < 0.5 with positive end expiratory pressure (PEEP) ≤ 5 cmH2O and respiratory rate of < 30 breaths per minute. The patients who were considered ready to wean from MV as per the above indices were included in the assessment of increasing ventilatory burden by subjecting them to non-randomized NPTs of 2, 4, and 6 during PSV of 8 cmH2O with PEEP 5 cmH2O. A period of 30 min of PSV without NPT was mandated to prevent exhaustion from burden of the test. Patients who successfully tolerated the variable NPT trial subsequently received their first T-piece trial after 6–12 h to prevent influence of any burden of test on the outcome of T-piece. Both PSV at NPTs and the T-piece trials were performed in semi-recumbent position. Decisions about tolerability of NPTs, T-piece, extubation, repeat T-piece, and or tracheostomy were as per the clinical judgment of the physician in-charge of the patient and were not in any way based on DUS measurements.
Diaphragm ultrasound
DUS measurements were performed on the right subcostal side using both brightness (B) and motion (M) mode.
Ultrasound machine and probe
High-resolution linear and curvilinear US probes of 10 and 3.5–5 MHz (FUJIFILM SonoSite, Inc.) were used to measure the diaphragm thickness (DT) and diaphragmatic excursion [amplitude (AMP)] respectively using both B and M modes.
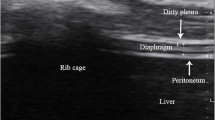
Probe placement
Both the amplitude and speed of contraction were assessed by placing the curvilinear probe on the right subcostal margin between the mid-clavicular and anterior axillary line allowing placement of the M mode line parallel to the excursion of the diaphragm. DT was measured in the zone of apposition of the diaphragm and rib cage in the mid-axillary line between the eighth and tenth intercostal space. The right-sided DUS measurements were used because of their reproducibility and feasibility in MV patients [21].
Measurements
DT [at end of inspiration (i) and expiration (e)], AMP [centimeters (cm)], and speed of contraction [SPcont (cm/s)] were measured. The DTf (%) was calculated as the difference between DTi and DTe divided by DTe × 100. These measurements were performed by a single intensivist experienced in performing DUS. In order to minimize intra-observer variability to less than 10% and establish reproducibility, an average of three readings measured in at least three sessions each lasting 10–15 min was ensured.
Inspiratory effort capacity
Within 6–12 h preceding the first T-piece, each patient was subjected to NPTs of 2, 4, and 6 cmH2O at PSV of 8 and 5 cmH2O PEEP for a minimum period of 20 min each to achieve a steady state. The measurements were recorded at the end of the 20th minute. Cooperative patient was instructed to perform breathing to total lung capacity (TLC) and then to exhale to residual volume (RV). DUS measurements at TLC and RV were then recorded. These points were considered as surrogates of end-inspiration and end-expiration respectively [22]. Several images of the diaphragm were captured and stored, including at least three at the point of maximum thickening at TLC and at least three at minimum thickening at RV. Diaphragm measurements were taken at PSV at three different NPTs and during the period of the first T-piece and at TLC and RV. Between each change over to a higher NPT, a rest period of 30 min on previous ventilatory support was mandatory to prevent exhaustion. The protocol was also interrupted for 30 min with increased pressure support after each trigger if signs of respiratory distress like respiratory rate > 35 breaths/min, SpO2 < 90%, heart rate > 140 beats/min, variation of > 30% from baseline, systolic blood pressure > 180 or < 90 mmHg, diaphoresis, or anxiety occurred. The time gap of 6–12 h between NPT trials and T-piece was incorporated to provide enough rest between the two procedures. SERVO-i-Maquet ventilator was used for mechanical ventilation of all patients included in the study.
Definitions
Patients were categorized based on the following weaning classification [16].
Simple weaning
Patients who proceeded from initiation of weaning to successful extubation on their first SBT without any difficulty were categorized as simple weaning (SW).
Difficult weaning
Patients who failed initial weaning and required up to three SBTs or as long as 7 days from the first SBT to achieve successful weaning were categorized as having difficult weaning.
Prolonged weaning
Patients who failed at least three weaning attempts or required 7 days of weaning after the first SBT were said to have prolonged weaning.
Weaning failure
It was defined as resumption of ventilatory support within 48 h of liberation from MV.
Complicated weaning
We grouped all patients with difficult, prolonged, and failed weaning together as complicated weaning (CW).
Data collection
Demographic (age, gender, category of patient, care received prior to present admission, source of admission, type of illness, coexisting illness, and source of sepsis), severity [Acute Physiologic and Chronic Health Evaluation (APACHE-II) and Sequential Organ Dysfunction Assessment (SOFA)] scores, organ failure at admission, indication for intubation, ventilation-related characteristics like tracheostomy, spontaneous breathing trials (SBTs), time before initiation of T-piece, length of MV, and ICU stay, along with DUS-based parameters of thickness, amplitude, thickening fraction, and outcomes relating to SW and CW and 28-day survival, were all recorded.
Sample size and statistical analysis
Sample size
Sample size was calculated assuming simple weaning proportion of 0.5 and 25% relative error of the proportion at two-sided 95% confidence interval (CI). Finally, a minimum sample size of 62 was calculated for the study. Sample size was calculated using software power analysis and sample size (PASS version 8).
Statistical analysis
Normality of continuous data was tested using Shapiro-Wilk test. Non-normal, continuous data was expressed as median (interquartile range), while categorical data was expressed as frequency and percentage. Mann-Whitney U test was used to compare the medians between SW and CW. Kruskal-Wallis test was used for comparison of continuous variables between more than two groups. Chi-square test was used to compare the proportions/test the association between groups. For repeated observations over variable NPTs, Friedman analysis of variance (ANOVA) was used to estimate the significance. If in Friedman ANOVA the p value was observed to be significant, then the difference in medians between individual groups was further assessed using the Wilcoxon signed rank test. A two-tailed p value of < 0.05 was considered statistically significant. IBM, SPSS version 23 (SPSS Inc., Chicago, IL, USA), was used for statistical analysis.
Results
Sixty-four patients, 40 (62.5%) males, were included in the study. Baseline characteristics of the studied population were as depicted in Table 1. Approximately, 86% of patients were with medical illness. Prior to present ICU admission, nearly 73 and 48% received ICU and MV support, respectively. Nearly 45% of the studied patients had been transferred from ICUs of other hospitals. Sepsis was the predominant (17/64, ~ 27%) reason for admission, with nearly 66% of respiratory origin. Nearly 58% of patients had no coexisting illness. There were 33 and 31 patients in SW and CW group, respectively. The groups were not significantly different, except for the type of illness (p, 0.01) (Table 1). Amongst the CW group, there were 16, 10, and 5 patients with difficult, prolonged, and failed weaning, respectively. Their baseline characteristics were also comparable with SW (Table not shown).
The attributes of severity, MV, and outcomes were as depicted in Table 2. APACHE-II and SOFA scores were comparable. Nearly 95% (61/64) of patients had two or more organ failures at admission, and they differed significantly between SW and CW (p, 0.04). Nearly 37% (24/64) required tracheostomy (SW, 1 vs. CW, 23; p < 0.001) during ICU stay. Significantly delayed [CW, 13 (8–22) day vs. 6 (4–8.5) day in SW; p < 0.001)] and failed first T-piece [CW, 20 (64.5%) vs. Nil in SW; p < 0.001] along with prolonged MV [CW, 22 (14–28) vs. 6 (5–9) in SW; p < 0.001] and ICU stay [CW, 28 (15–35) days vs. 8 (7–14.5) days in SW; p < 0.001] were observed in CW relative to SW (Table 2). Similar significance (p < 0.001) for these characteristics were also observed when comparing SW with difficult, prolonged, and failed weaning (Table not shown). Only one patient in the SW group got re-intubated and was later tracheostomized during the follow-up period of 28 days. All patients in CW group (n, 31) failed the first T-piece trial, and 23 (23/31, 74%) were tracheostomized. The remaining eight patients were extubated following more than one T-piece trial in the follow-up period. Post extubation non-invasive ventilation was used in eight patients in the CW group.
While 100% of patients in SW, difficult and prolonged weaning, survived 28 days, one of five (20%) in the failed weaning died within this period (p < 0.001) (Table not shown). The 28-day survival and final outcomes were comparable (Table 2). However, the four patients with CW who finally died were also the ones who had failed weaning and three of them died beyond 28 days of ICU stay.
The measurements of diaphragm (DTi, DTe, DTf, AMP, and SPcont) at NPTs of 2, 4, and 6 and during first T-piece for SW and CW were as depicted in Table 3. Also depicted in the same table were inter- and intra-differences between groups. DTi exceeded DTe at all NPTs. The intergroup variability between SW and CW was statistically significant for DTi, DTf, AMP, and SPcont, at variable NPTs and T-piece (for each, p < 0.001). Similar comparison of SW with difficult, prolonged, and failed weaning patients was also significant (p < 0.001) (Table not shown). The intra-group variability at different triggers and T-piece as assessed by Friedman ANOVA was statistically significant (p ≤ 0.001) for all the measured diaphragm parameters except in the CW for DTf (p, 0.34). Similar results of significance were also observed when SW was compared with difficult and prolonged weaning (p ≤ 0.001), except that patients with failed weaning had a somewhat lower significance (p < 0.05) (Table not shown). The ∆2–4, ∆4–6, and ∆2–6 variables for SW and CW were as depicted in Table 3. For most, the significance was ≤ 0.001, except for 2, 3, and 4 variables in ∆2–4, ∆4–6, and ∆2–6 respectively, wherein it was comparable. However, the ∆ variability (Table 3) increased when patients in SW were compared with difficult, prolonged, and failed weaning (Table not shown).
The sensitivity and specificity of various diaphragm measurements to predict SW was analyzed using the receiver operative characteristics (Table 4). With a cutoff at or above 25.5, 26.5, 25.5, and 24.5 for 2, 4, and 6 NPTs and T-piece, respectively, the DTf had a ROC AUC of ≥ 0.90. At NPT of 2, DTf had the highest sensitivity of 97%, albeit 81% specificity [ROC AUC, 0.91 (0.84–0.99); p < 0.001] compared to AMP and SPcont.
Discussion
DUS is an acknowledged investigative tool for assessment of diaphragm in critically ill patients. The present prospective study utilized DUS measurements at variable inspiratory efforts to predict successful weaning. The main findings of our study were as follows: (1) DTf predicts simple weaning; (2) DUS parameters at variable NPTs can identify patients ready to wean; and (3) DUS can help analyze patients with complicated weaning.
DTf predicts simple weaning
In recent years, several DUS-based measurements and some derived parameters have been validated for predicting weaning in critically ill patients [13, 14, 21,22,23]. Similar to majority of previous studies [21, 24, 25], we too assessed the more feasible and highly reproducible right hemi-diaphragm via DUS. DTi, DTf, AMP, and SPcont were all significantly higher in SW compared to CW (Table 3) or difficult, prolonged, and failed weaning (Table not shown), both at variable NPTs and during T-piece (p < 0.001). These parameters were also relatively better at different NPTs than during T-piece for predicting SW. The DTf cutoff ≥ 25.5% with AUC of 0.91 had sensitivity and specificity of 97 and 81% respectively at NPT of 2 for predicting SW. This sensitivity was higher than the AMP (cutoff ≥ 1.21 cm) and SPcont (cutoff ≥ 1.24 cm/s) at same NPT, desirable to predict SW. Variable DTf cutoffs have been used previously. DiNino et al., in 2014, studied DUS in 63 patients before extubation, during SBT or pressure support trial [23]. They suggested that a threshold DTf of greater or equal to 30%, with a positive predictive value (PPV) and negative predictive value (NPV) of 91 and 63%, respectively, for extubation success, performed similarly during SBT or pressure support ventilation. Similarly, Ferrari et al., in 46 patients of repeated weaning failure, suggested that a cutoff DTf greater or equal to 36%, during SBT in tracheostomized patients, was associated with a PPV and NPV of 92 and 75%, respectively, for successful or failed weaning at 48 h [22]. By comparison, rapid shallow breathing index (RSBI) < 105 had sensitivity, specificity, PPV, and NPV of 93, 88, 93, and 88%, respectively, for determining successful SBT. The plausible explanation of a lower DTf threshold in our study is due to differences in methodology, variable inspiratory efforts, patient population, and severity of illness at ICU admission, metabolic conditions, and duration of MV. Several studies report superiority of DTf over diaphragm excursions as a marker of diaphragm function [26, 27]. However, we studied predictability of weaning via DUS at variable inspiratory efforts and observed a higher sensitivity and comparable AUC for DTf to predict SW.
DUS parameters at variable NPTs can identify patients ready to wean
The ROC AUC, sensitivity, and specificity during T-piece for DTf, AMP, and SPcont were lower as compared to NPTs at comparable cutoffs (Table 4). DUS measurements at NPT of 2 were observed to be more favorable for predicting SW compared to T-piece. Both, DTf and AMP, showed higher or comparable sensitivity and specificity at NPT of 2 relative to NPT of 6. Hence, SW prediction can be performed prior to T-piece and at lower NPTs. No previous studies have reported this.
DUS can help analyze patients with complicated weaning
Diaphragm excursion [13], twitch tracheal pressure [15], and trans-diaphragmatic twitch pressure [26, 27] have all been used to quantify diaphragm dysfunction. These studies have reported increased mortality and morbidity associated with diaphragm dysfunction. However, we categorized our patients into SW and CW. All DUS parameters were significantly lower in the CW group, and these patients also had delayed and failed SBT and prolonged MV and length of ICU stay. Similar outcomes were observed in the difficult, prolonged, and failed weaning patients. These were similar to findings of earlier study [17]. Only patients with failed weaning died.
Limitations
Several limitations of our study were as follows: (1) single-center study with a small sample size; (2) DTf cutoff not validated; (3) illness- and severity-specific variability not ascertained due to a small sample size; (4) minimal differences between measurements altered the weaning categorization; (5) small number of patients in difficult, prolonged, and failed weaning may have overestimated the differences; (6) trigger sensitivity not randomized; (7) due to small sample size, independent trigger sensitivity for each patient group could not be individually tested; (8) workload increase contributed by the burden of test and its impact on T-piece outcome could not be clearly ascertained; ideally, these two observations should have been done separately to avoid influence; (9) rest period of 30 min between variable triggers may have been insufficient to relieve the fatigue imposed; (10) DUS-based measurements were not compared against traditional weaning indices; (11) trends of DUS measurements overtime in CW group may have better correlated with outcomes; (12) inter-observer variability not assessed; (13) due to non-availability of ventilator-coupled USG machine, only cooperative patients could be included in the study; (14) factors affecting the DTf, their impact on weaning, and how they could be modified to optimize weaning were not studied.
Despite the abovementioned shortcomings, our study is a humble exploratory attempt to use DUS measurements to identify patients with SW even before their first T-piece trial. DTf, AMP, and SPcont with cutoffs ≥ 25.5%, ≥ 1.2 cm, and ≥ 1.24 cm/s, respectively, at NPT of 2 may help to not only determine which patient will safely endure the T-piece but also predict a successful T-piece trial. These measures may also help to further analyze patients with CW. Furthermore, DTf values could also be of use to optimize CW patients for further extubation trials.
Conclusion
Ultrasound-based diaphragm measurements at variable inspiratory efforts can help identify patients safe and ready to wean even without enduring a T-piece. Amongst these parameters, DTf, apart from recognizing readiness to wean, can also predict simple weaning. However, a larger multicenter study is still required to validate the observed DTf cutoff in our study. Research on factors which affect the DTf and their modification to optimize weaning need to be further explored.
Abbreviations
- AMP:
-
Amplitude
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- CW:
-
Complicated weaning
- DT:
-
Diaphragm thickening
- DTe :
-
Diaphragm thickening during expiration
- DTf :
-
Diaphragm thickening fraction
- DTi :
-
Diaphragm thickening during inspiration
- DUS:
-
Diaphragm ultrasound
- ICU:
-
Intensive care unit
- MV:
-
Mechanical ventilation
- NPTs:
-
Negative pressure triggers
- PSV:
-
Pressure support ventilation
- RV:
-
Residual volume
- SOFA:
-
Sequential Organ Failure Assessment
- SPcont :
-
Speed of contraction
- SW:
-
Simple weaning
- TLC:
-
Total lung capacity
References
Epstein SK, Ciubotaru RL, Wong JB. Effect of failed extubation on the outcome of mechanical ventilation. Chest. 1997;112:186–92.
Seymour CW, Martinez A, Christie JD, Fuchs BD. The outcome of extubation failure in a community hospital intensive care unit: a cohort study. Crit Care. 2004;8:R322–7.
Coplin WM, Pierson DJ, Cooley KD, Newell DW, Rubenfeld GD. Implications of extubation delay in brain-injured patients meeting standard weaning criteria. Am J Respir Crit Care Med. 2000;161:1530–6.
Esteban A, Alía I, Tobin MJ, Gil A, Gordo F, Vallverdú I, Blanch L, Bonet A, Vázquez A, de Pablo R, Torres A, de La Cal MA, Macías S. Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Spanish Lung Failure Collaborative Group. Am J Respir Crit Care Med. 1999;159:512–8.
Esteban A, Alía I, Ibañez J, Benito S, Tobin MJ. Modes of mechanical ventilation and weaning. A national survey of Spanish hospitals. The Spanish Lung Failure Collaborative Group. Chest. 1994;106:1188–93.
Esteban A, Frutos F, Tobin MJ, Alía I, Solsona JF, Valverdú I, Fernández R, de la Cal MA, Benito S, TomásR, et al. A comparison of four methods of weaning patients from mechanical ventilation. Spanish Lung Failure Collaborative Group. N Engl J Med. 1995;332:345–50.
Tobin MJ, Laghi F, Jubran A. Narrative review: ventilator-induced respiratory muscle weakness. Ann Intern Med. 2010;153:240–5.
Laghi F, Tobin MJ. Disorders of the respiratory muscles. Am J Respir Crit Care Med. 2003;168:10–48.
Powers SK, Shanely RA, Coombes JS, Koesterer TJ, McKenzie M, Van Gammeren D, Cicale M, Dodd SL. Mechanical ventilation results in progressive contractile dysfunction in the diaphragm. J Appl Physiol. 2002;92:1851–8.
Sassoon CS, Caiozzo VJ, Manka A, Sieck GC. Altered diaphragm contractile properties with controlled mechanical ventilation. J Appl Physiol. 2002;92:2585–95.
Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, Zhu J, Sachdeva R, Sonnad S, Kaiser LR, Rubinstein NA, Powers SK, Shrager JB. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med. 2008;358:1327–35.
Jaber S, Petrof BJ, Jung B, Chanques G, Berthet JP, Rabuel C, Bouyabrine H, Courouble P, Koechlin-Ramonatxo C, Sebbane M, Similowski T, Scheuermann V, Mebazaa A, Capdevila X, Mornet D, Mercier J, Lacampagne A, Philips A, Matecki S. Rapidly progressive diaphragmatic weakness and injury during mechanical ventilation in humans. Am J Respir Crit Care Med. 2011;183:364–71.
Kim WY, Suh HJ, Hong SB, Koh Y, Lim CM. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med. 2011;39:2627–30.
Matamis D, Soilemezi E, Tsagourias M, Akoumianaki E, Dimassi S, Boroli F, Richard JC, Brochard L. Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications. Intensive Care Med. 2013;39:801–10.
Demoule A, Jung B, Prodanovic H, Molinari N, Chanques G, Coirault C, Matecki S, Duguet A, Similowski T, Jaber S. Diaphragm dysfunction on admission to the intensive care unit. Prevalence, risk factors, and prognostic impact—a prospective study. Am J Respir Crit Care Med. 2013;188:213–9.
Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, Pearl R, Silverman H, Stanchina M, Vieillard-Baron A, Welte T. Weaning from mechanical ventilation. EurRespir J. 2007;29:1033–56.
Funk GC, Anders S, Breyer MK, Burghuber OC, Edelmann G, Heindl W, Hinterholzer G, Kohansal R, Schuster R, Schwarzmaier-D’Assie A, Valentin A. Incidence and outcome of weaning from mechanical ventilation according to new categories. Eur Respir J. 2010;35:88–94.
Conti G, Montini L, Pennisi MA, Cavaliere F, Arcangeli A, Bocci MG, Proietti R, Antonelli M. A prospective, blinded evaluation of indexes proposed to predict weaning from mechanical ventilation. Intensive Care Med. 2004;30:830–6.
Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med. 1991;324:1445–50.
Lee KH, Hui KP, Chan TB, Tan WC, Lim TK. Rapid shallow breathing (frequency-tidal volume ratio) did not predict extubation outcome. Chest. 1994;105:540–3.
Goligher EC, Laghi F, Detsky ME, Farias P, Murray A, Brace D, Brochard LJ, Bolz SS, Rubenfeld GD, Kavanagh BP, Ferguson ND. Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensive Care Med. 2015;41:642–9.
Ferrari G, De Filippi G, Elia F, Panero F, Volpicelli G, Aprà F. Diaphragm ultrasound as a new index of discontinuation from mechanical ventilation. Crit Ultrasound J. 2014;6:8.
DiNino E, Gartman EJ, Sethi JM, McCool FD. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax. 2014;69:423–7.
Houston JG, Morris AD, Howie CA, Ried JLNM. Technical report: quantitative assessment of diaphragmatic movement—a reproducible method using ultrasound. Clin Radiol. 1992;46:405–7.
Gerscovich EO, Cronan M, McGahan JP, Jain K, Jones CD, McDonald C. Ultrasonographic evaluation of diaphragmatic motion. J Ultrasound Med. 2001;20:597–604.
Umbrello M, Formenti P, Longhi D, Galimberti A, Piva I, Pezzi A, Mistraletti G, Marini JJ, Iapichino G. Diaphragm ultrasound as indicator of respiratory effort in critically ill patients undergoing assisted mechanical ventilation: a pilot clinical study. Crit Care. 2015;19:161.
Vivier E, Mekontso Dessap A, Dimassi S, Vargas F, Lyazidi A, Thille AW, Brochard L. Diaphragm ultrasonography to estimate the work of breathing during non-invasive ventilation. Intensive Care Med. 2012;38:796–803.
Acknowledgements
The authors wish to thank the Department of Biostatistics and Health Informatics, Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGIMS), Lucknow, Uttar Pradesh, India, for the support provided in the statistical analysis of the results.
Funding
The author(s) received no financial support for this study.
Availability of data and materials
Please contact the author for data requests.
Author information
Authors and Affiliations
Contributions
RKS and SS contributed equally to the design, data acquisition, statistical calculations, and manuscript preparation. AKB, BP, AZ, and MG contributed equally to the manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Ethics Committee of Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India, approved the study. Written informed consent was obtained from all patients or their first of kin as appropriate, prior to inclusion in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Samanta, S., Singh, R.K., Baronia, A.K. et al. Diaphragm thickening fraction to predict weaning—a prospective exploratory study. j intensive care 5, 62 (2017). https://doi.org/10.1186/s40560-017-0258-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40560-017-0258-4