Abstract
Background
Pulse pressure variation (PPV) has been widely used in hemodynamic assessment. Nevertheless, PPV is limited in low tidal volume ventilation. We conducted this systematic review and meta-analysis to evaluate whether the tidal volume challenge (TVC) could improve the feasibility of PPV in patients ventilated at low tidal volumes.
Methods
PubMed, Embase and Cochrane Library inception to October 2022 were screened for diagnostic researches relevant to the predictability of PPV change after TVC in low tidal volume ventilatory patients. Summary receiving operating characteristic curve (SROC), pooled sensitivity and specificity were calculated. Subgroup analyses were conducted for possible influential factors of TVC.
Results
Ten studies with a total of 429 patients and 457 measurements were included for analysis. The predictive performance of PPV was significantly lower than PPV change after TVC in low tidal volume, with mean area under the receiving operating characteristic curve (AUROC) of 0.69 ± 0.13 versus 0.89 ± 0.10. The SROC of PPV change yielded an area under the curve of 0.96 (95% CI 0.94, 0.97), with overall pooled sensitivity and specificity of 0.92 (95% CI 0.83, 0.96) and 0.88 (95% CI 0.76, 0.94). Mean and median cutoff value of the absolute change of PPV (△PPV) were 2.4% and 2%, and that of the percentage change of PPV (△PPV%) were 25% and 22.5%. SROC of PPV change in ICU group, supine or semi-recumbent position group, lung compliance less than 30 cm H2O group, moderate positive end-expiratory pressure (PEEP) group and measurements devices without transpulmonary thermodilution group yielded 0.95 (95%0.93, 0.97), 0.95 (95% CI 0.92, 0.96), 0.96 (95% CI 0.94, 0.97), 0.95 (95% CI 0.93, 0.97) and 0.94 (95% CI 0.92, 0.96) separately. The lowest AUROCs of PPV change were 0.59 (95% CI 0.31, 0.88) in prone position and 0.73 (95% CI 0.60, 0.84) in patients with spontaneous breathing activity.
Conclusions
TVC is capable to help PPV overcome limitations in low tidal volume ventilation, wherever in ICU or surgery. The accuracy of TVC is not influenced by reduced lung compliance, moderate PEEP and measurement tools, but TVC should be cautious applied in prone position and patients with spontaneous breathing activity.
Trial registration PROSPERO (CRD42022368496). Registered on 30 October 2022.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Fluid administration remains the first-line therapy wherever in ICU or operation room (OR). Both fluid overload and insufficient could cause deleterious effects, such as pulmonary edema, tissue hypoperfusion [1, 2]. However, only half of the patients are fluid responsiveness in clinical work [3].
Dynamic indices derived from arterial wave change, based on heart–lung interaction during mechanical ventilation, such as pulse pressure variation (PPV) or stroke volume variation (SVV), are proven to be superior than static indices [4, 5]. Among these indices, PPV is more reliable, quickly accessible from bedside and more extensively studied, and has been widely used in critically ill patients [4, 6]. However, since mechanical ventilation can trigger cardiac preload change in periodicity, in the condition of no arrhythmias and closed thoracic cavity, low tidal volumes are insufficient to produce significant change in thoracic pressure, so is the preload. This would add false negative results in fluid responsive patients, making PPV and other dynamic hemodynamic indices inaccurate [7,8,9]. It has been reported that PPV is reliable when tidal volume at least 8 ml/kg predicted body weight (PBW) [7]. But nowadays, low tidal volume ventilatory strategy (usually 6 ml/kg), improving outcomes and reducing pulmonary complications, has been widely used in ICU or general anesthesia surgery patients [10,11,12], which further restricts the application of PPV.
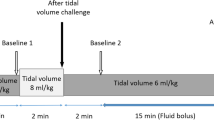
The concept of tidal volume challenge (TVC) was proposed to solve the dilemma for PPV in a concise manner [13]. The procedure of TVC is to adjust volume tidal from 6 (PBW) to 8 ml/kg (PBW) and obtains the increasing preload dependence of right ventricle and decreases the venous return, which cause patients more fluid responsive [13]. Many recent studies reported the change of PPV after TVC, including the absolute or percentage change of PPV (△PPV or △PPV%), in the assessment of fluid responsiveness in low tidal volume ventilation patients [14,15,16,17,18,19,20,21,22,23]. However, the results were conflicting and a recent meta-analysis of TVC only included 3 original studies in the early years [8]. Besides, except low tidal volume, some factors that would possibly influence intrathoracic pressure were existed in these study settings, such as position [24], lung compliance [25] or positive end-expiratory pressure (PEEP) [26].
We conducted this systematic review and meta-analysis to assess the ability of TVC to help PPV overcome the limitation in low tidal volume ventilation patients, and explore whether the factors influencing intra-thoracic pressure or other factors could possibly influence the accuracy of TVC.
Material and methods
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [27].
Registration and protocol
This meta-analysis was registered on PROSPERO (CRD42022368496).
Search strategy
Two authors independently searched relevant studies up to October 2022 in PubMed, Embase and Cochrane Library with the following terms and their combination: “tidal volume challenge” AND “pulse pressure variation” AND (“low tidal” OR” low tidal ventilation” OR “protective ventilation”) AND (“fluid responsiveness” OR “volume responsiveness”). All scanned abstracts, studies and citations were reviewed. If discrepancy existed, it was solved by the third arbitration. Moreover, references of the retrieved manuscripts were also manually cross-searched for further relevant publications.
Selection criteria
The inclusion criteria were as follows (according to PICO):
S (study design): diagnostic experiments of TVC in fluid responsive assessment in low tidal volume ventilation patients.
P (patients): adult patients under low tidal volume ventilation in ICU or OR.
I (interventions):change of PPV after TVC; TVC in the studies was defined as adjusting tidal volume from 6 to 8 ml/kg, and the measurements are performed one minute after TVC; △PPV defined as PPVvt8-PPVvt6 and △PPV% defined as (PPVvt8-PPVvt6)/ PPVvt6. The concepts of TVC and PPV change are presented in Fig. 1.
C (controls): fluid responsiveness assessment was performed with fluid challenge or response to PLR or its surrogates.
O (outcomes): the ability of TVC to improve the feasibility of PPV in low tidal volume ventilation.
(6) Others: studies published with full-text in any language; studies providing sufficient data for constructing 2-by-2 tables, including true positive (TP), false positive (FP), true negative (TN) and false negative (FN) [28].
We excluded those studies as follows: (1) studies with patients under normal or high tidal volume ventilation; (2) studies that used the same population or overlapping database; (3) studies without mechanically ventilation or spontaneously breathing patients; (4) animal studies; (5) studies on ventilated children.
Date extraction and quality assessment
Two authors independently browsed the research indicators of the included studies. Extracted data included three parts: (1) basic information about the research such as the number of patients, study year and places, study indicators, measurement tools and ventilation settings; (2) the statistical results, including sensitivity, specificity, AUROC of the change of PPV and cutoff value; (3) discrepancies among studies that could be the heterogeneity or potential factors that could influence the degree of preload change caused by TVC, such as patients, position, lung compliance, ventilator settings, measurement tools.
Two investigators independently assessed the included studies by Diagnostic Accuracy Studies-2 (QUADAS-2) recommended by the Cochrane Handbook [29]. The QUADAS-2 tool consists of four domains: patient selection, index test, reference standard and flow and timing. All domains were evaluated in terms of risk of bias and would be answered as “yes,” “no” and “unclear.” “Unclear” was defined if the original study failed to provide adequate information that the authors had difficulty to judge. The risk could be defined as low under the circumstance of a consistency of “yes.” Quality assessment was performed by RevMan software 5.3.
Statistical analysis
The bivariate mixed-effects regression model was performed in data synthesis to incorporate the negative correlation, which might arise between the sensitivity and specificity [30, 31]. We estimated overall pooling of sensitivity, specificity and diagnostic odds ratio (DOR) with 95% confidence interval (CI) using a bivariate random-effects model. Summary receiver operating characteristic curve (SROC) was potted and the area under the summary receiver operating characteristic curve (AUSROC) was calculated by Rutter and Gatsonis test [32]. Operative performance quality was graduated according to Fisher et al [33]. Diagnostic power was outstanding if the AUROC was more than 0.9 and was poor if the AUROC was less than 0.7 [34].The cutoff values of PPV change were performed in the scatter plot to observe the distribution, dispersion, central tendency and extremum.
Heterogeneity between studies was quantitatively assessed by the Chi-square test and Cochran’s Q test. P value for Q test < 0.1 or I2 > 50% was considered existing significant heterogeneity. Heterogeneity caused by the threshold effect in the diagnostic test was calculated in the Spearman correlation coefficient, which was estimated by the Moses–Shapiro–Littenberg [35]. If correlation coefficient was 1, which means the proportion of heterogeneity likely due to threshold effect was 100%, meta-regression was unnecessary [36]. Other methods, such as rule out one single study one by one to find heterogeneity sources, were also conducted.
Subgroup analysis was conducted according to factors which could possibly affecting intrathoracic pressure and the predictability of TVC. Since patients in ICU are more complicated, and the results of TVC in ICU were contradictory, we conducted ICU groups. We also conducted subgroup analysis including supine or semi-recumbent group, lung compliance < 30 cm H2O group, moderate PEEP group (5 cm H2O ≤ PEEP ≤ 15 cm H2O) and measurement tools without TPTD group. Spontaneous breathing subgroup was also observed. Since some studies included both △PPV and △PPV%, the primary and more accurate indicator was calculated when in analysis. Diagnostic accuracy parameters between groups were compared using the likelihood ratio Chi-square test if necessary.
Public bias was estimated by Deek’s funnel plot asymmetry test, with P < 0.1 indicating statistical significance [37].
The description of data was expressed as mean (95% CI) or as mean ± standard deviation. Meta-analysis was performed by Stata 15. 0 (StataCorp, College Station, TX) with the Midas module. A two-tailed P < 0.05 was considered statistically significant.
Results
Characteristics of included studies
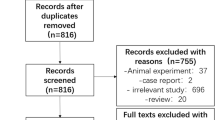
Our meta-analysis yielded 834 primary studies after initially screened; 735 studies were excluded because of obviously irrelevant and duplicates. In the remaining 99 studies, full-text manuscripts were screened and 88 full-text articles were excluded because of tidal volume more than 6 ml/kg or spontaneous breath, without the analysis of the variation in PPV after TVC, and review or not diagnostic research. Further screening the remaining 11 full articles, one was excluded because of ROC analysis missing. Finally, 10 studies with a total of 429 patients and 457 measurements were included in the meta-analysis, presented in Fig. 2. QUADAS-2 was presented in Fig. 3.
Characteristics of the included studied were summarized in Table 1. A total of 215 measurements (47.7%) were fluid responsive in the overall studies. 7 studies were conducted in ICU, while the left in OR. The position was varied, 6 studies were in supine or semi-recumbent position, while 3 studies were in prone position and 1 in Trendelenburg position. The mean lung compliance ranged from 16.8 to 83 ml/cm H2O. Except one study missing data, the mean PEEP ranged from 5 to 14 cm H2O. In the overall 10 studies, 5 studies acquired PPV with transpulmonary thermodilution (TPTD) and 5 studies with others.
Performance of TVC improve the accuracy of PPV in low tidal volume ventilation
The predictive performance of PPV was significantly lower than PPV change in low tidal volume, with mean AUROC of 0.69 ± 0.13 versus 0.89 ± 0.10, P < 0.01, presented in Table 2. SROC of the PPV change yielded an area under the curve of 0.96 (95% CI 0.94, 0.97) with overall I2 of 76% (95%47, 100), presented in Fig. 4 The pooled sensitivity and specificity of the change of PPV were 0.92 (95% CI 0.83, 0.96) and 0.88 (95% CI 0.76, 0.94) with I2 of 79% (95%67, 92) and 86% (95%78, 93) separately, presented in Fig. 5. DOR of the change of PPV was 81 (95% CI 23, 284) with I2 of 67% (95% CI 0, 86).
Summary receiver operating characteristic curve for the change of pulse pressure variation after tidal volume challenge predicting fluid responsiveness in low tidal volume ventilation. The diamond is the summary point representing the average sensitivity and specificity estimates. AUC area under the curve, SENS sensitivity, SPEC specificity, SROC summary receiver operating characteristics. The ellipses around this summary point are the 95% confidence region (dashed line) and the 95% prediction region (dotted line)
Heterogeneity investigation
Significant heterogeneity in the 10 studies was observed with an overall Q = 8.3, I2 = 76%, P < 0.01. The Spearman correlation coefficient was 0.09; however, significant heterogeneity was not found in the latter meta-regression analysis (presented in Additional file 1: Fig. S1). We attempted to remove the study of Yonis et al. [15] in the analysis. The overall heterogeneity was significant decreased to I2 = 42% and Q = 3.605, P = 0.09. Spearman correlation coefficient was 1, whereas the value of I2 and Q test changed insignificantly when we removed any other study in the analysis (presented in Additional file 2: Table S1 and Additional files 3, 4: Figs. S2, S3).
Subgroup analysis
In ICU groups, TVC has good predictability in ICU with SROC yielding 0.95 (95%0.93, 0.97), pooled sensitivity of 0.91 (95%0.77, 0.97) and pooled specificity of 0.88 (95%0.69, 0.96), presented in Additional file 5: Fig. S4. The change of PPV after TVC in supine or semi-recumbent group, lung compliance < 30 cm H2O group, moderate PEEP group and measurement tools without TPTD group all performed good prediction of fluid responsiveness with SROC yielded the area of 0.95 (95% CI 0.92, 0.96), 0.96 (95% CI 0.94, 0.97), 0.95 (95% CI 0.93, 0.97) and 0.94 (95% CI 0.92, 0.96) separately (presented in Additional file 6: Fig. S5 and Table 3). However, the lowest AUROC of PPV change was 0.59 (95% CI 0.31–0.88) in prone position and 0.73 (95% CI 0.60–0.84) in patients with spontaneous breathing activity.
The comparison of △PPV and △PPV%
In groups comparison, there is no difference in AUC > 0.9 rate, △PPV versus △PPV%, p = 0.31. But interestingly, in the same study, △PPV always perform slightly better than △PPV%(presented in Table 2). The SROC of △PPV and △PPV% yielded the area of 0.94 (95% CI 0.92, 0.96) and 0.96 (95% CI 0.94, 0.97), with I2 of 19% (95% CI 0, 100) and 78% (95% CI 52, 100), presented in Additional file 7: Fig. S6. The mean and median cutoff values of △PPV were 2.4% and 2%, ranged from 1 to 3.5%, and that of △PPV% were 25% and 22.5%, ranged from 12 to 48%, presented in Fig. 6.
Scatter plot of cutoff value of △PPV and △PPV% in included studies. The purple black dots represent absolute change of pulse pressure variation (△PPV). The black diamond squares represent percentage change of pulse pressure variation (△PPV%). The cutoff values of △PPV are as follows: (1) Myatra 2017 [14], 3.5%; (2) Jun 2019 [16], 1%; (3) Elsayed 2021 [19], 3.5%; (4) Taccheri 2021 [20], 1%; Hamzaoui2021 [21]; (5) Shi 2022 [22], 3.5%; (6) Xu 2022 [23], 2%. The cutoff values of △PPV% are as follows: (1) Myatra 2017 [14], 48%; (2)Yonis 2017 [15], 29%; (3) Jun 2019 [16], 25%; (4) Messina 2019 [17], 13.3%; (5) Messina 2020 [18], 12%; (6) Taccheri 2021 [20], 20%;
Public bias
The Deek’s funnel plot asymmetry test of the meta-analysis is shown in Fig. 7, and no significant public bias was found in our meta-analysis (P = 0.27).
Discussion
This systematic review and meta-analysis mainly revealed that: (1) The change of PPV that caused by TVC is a good fluid responsiveness predictor in low tidal volume ventilation; (2) TVC is reliable in both ICU and OR, and the accuracy would not be affected by low lung compliance, moderate PEEP and the measurement devices of PPV; (3) But, TVC should be cautious applied in prone position and patients with spontaneous breathing activity. The exact research string of the whole study is presented in Fig. 8.
A recent meta-analysis showed PPV performed moderately in tidal volume less than 8 ml/kg due to not enough preload change triggered by mechanical ventilation [38]. Previous research observed PPV obviously increased 4.8% meanly in patients even 5 min after adjusting tidal volume from 6 to 8 ml/kg [39]; this challenge could help augmenting preload change when evaluating fluid responsiveness; soon after that, TVC was proposed [13]. As expected, in our meta-analysis, PPV change after TVC performed significantly better than PPV in low tidal volume ventilation, with SROC more than 0.9.
In subgroup analysis, patients in ICU are more complicated with shock, organ failure or other critically ill state, and the results were contradictory. But in statistical analysis, TVC is still highly reliable in ICU patients, with similar SROC to the overall data. Theoretically, the reduced lung compliance could enhance the transmission of airway pressure to the pericardium and the vena cava, thus, weaken the effect of SV change caused by ventilation [40, 41]. PPV was reported low predictability in lung compliance less than 30 cm H2O [25]. Fortunately, we found PPV change after TVC was less affected by reduced lung compliance, this could be relevant to the preload change weakened by low lung compliance is limited, and that was supplemented by TVC. Moderate PEEP could supply pressure on the end expiratory, enlarge cyclic cardiac output change caused by ventilation [26] and thus strength the effect of TVC. As a result, we found TVC performed well in patients with moderate PEEP. Except from the widely used and standard method TPTD, pulse contour analysis technique or noninvasive monitor which also acquires PPV is more convenient and noninvasive but more susceptible of interferences [5]. However, we observed that TVC was not influenced by measurement tools.
We found TVC would limit in some circumstances. In a patient with spontaneous breathing activity, the TVC may fail because of asynchronism between the increased Vt and the breathing pattern of the patient. This may cause a contrast between the patient and ventilator, affecting the right ventricle afterload and, hence, the changes in right ventricle stroke volume. As expected, TVC performs obviously bad with AUROC of only 0.73 in patients with spontaneous breathing activity [21], which is much lower than that in totally mechanical ventilation studies. The results of TVC were also contradictory in prone position [15, 18, 22]. Physiologically, the venous return could be impeded when intra-abdominal pressure is more than right atrial pressure because the abdominal inferior vena cava collapses and a vascular waterfall develops at the level of the diaphragm [24]; this could cause TVC fail to decrease preload. Different clinical settings were also accountable, but we disagreed with Shi et al. [22] who accounted the contradictory results to lung compliance since we found TVC was unaffected by reduced lung compliance. Besides, recent meta-analysis of EEO, the similar theory of heart–lung interaction functional test to TVC, was also proved to be limited in prone position [42].
The cutoff values of PPV change were varied in our study. In fact, this is the common phenomenon caused by different preload state before TVC. The extreme cutoff value of △PPV% was 48% in Mytra’ study [14]; this could be related to the fact that the selected people were circulatory failure patients, who were sensitive to preload change. In the study of Jun [16], the included patients were normal hemodynamic state but with extremely reduced lung compliance of 16.8 cm H2O. However, low lung compliance induces insignificant preload change due to more obstruction stress from chess or pulmonary to cardiac or vena, and consequently, the final cutoff value of △PPV was only 1%. Besides, some ventilation settings that could increase cyclic changes of intrathoracic pressure, such as PEEP [26] and larger tidal volume [7], as a result, acquire larger cutoff value.
To a certain extent, △PPV% is a surrogate of △PPV and they possessed the same tendency of predictability, whereas we found △PPV% was less practical and reliable than △PPV, which was in the agreement with Myatra [14]. Initially, heterogeneity of △PPV% group was significant and larger than △PPV group. Secondly, the AUSROC of △PPV% performed a slighter lower than △PPV when in the same studies [14, 16, 20]. Moreover, the cutoff values of △PPV were more central between 1 and 3.5%, while that of △PPV% were more dispersed in the scatter plot, which could cause more threshold effect heterogeneity and difficult to assess fluid responsiveness accurately. Last but not the least, the calculation of △PPV% is more complicated and not suitable for beside or emergency.
Some limitations in our meta-analysis should be acknowledged. Firstly, ten number of diagnostic studies was included with significant heterogeneity in the overall analysis representing a limitation of this study. Although the study of Yonis et al. [15] could be the heterogeneity of this meta-analysis, other potential heterogeneity should be considered. Secondly, due to some included researches missing data of sensitivity and specificity of PPV, we failed to calculate the SROC of PPV in low tidal volume ventilation in comparison. Instead, we statistically compare the AUROCs of PPV and PPV change in low tidal volume ventilation patients with original data. Thirdly, we did not perform the comparison of the opposite subgroups, such as low versus high lung compliance and prone versus supine, because, on the one hand, our main intention is to observe whether TVC is still reliable in some circumstance, like low lung compliance, some position, moderate PEEP and irregular measurement tools, rather than comparing the differences between the opposite two groups. After all, these conditions exit commonly in patients need lung protective strategies and probably influence TVC. On the other hand, some opposite groups only contained 2 or 3, or even 1 study, and small number subgroup is less convincing for comparison and has larger risk of statistical error. Fourthly, some other valuable target subgroups that could influence TVC were failed to analyze because of current studies restriction. Higher level of PEEP results in greater cyclic changes in preload [26], making patients more fluid responsive [43], while PEEP of 15 to 20 cm H2O could decrease cardiac output [44]. However, we failed to analyze PEEP more than 15 cm H2O group because all included studies used moderate PEEP. Spontaneous breathing activity during mechanical ventilation is common in ICU and TVC could fail in this condition, but currently, only one study proved that, and we failed to make summary statistical analysis. Fifthly, not all included studies used fluid challenge as golden standard preload challenge; this could bring more interferences to assess TVC. Actually, the essence of fluid responsiveness assessment is detecting preload change, apart from classic fluid challenge; other surrogates or called functional tests, such as PLR, mini-fluid challenge, EEO or Trendelenburg, could also trigger the same effect, and some even perform advantages over classic method [45].Thus, these studies with surrogates of fluid challenge are also vital and valuable. Finally, the current studies in our meta-analysis all used standard TVC (6 to 8 ml/kg Vt, 1 min). As we all know, TVC is the supplement of preload change; hence, change size of Vt or performance time could influence the SV change caused by TVC. Similar study of fluid challenge reported 100 ml and 250 ml crystalloid had the same effect in preload [46], but that decreased when performed over 30 min [47]. Overall, more researches are warrant in the future about TVC.
Conclusion
TVC could improve the feasibility of PPV in patients mechanically ventilated at low tidal volumes by calculating PPV change after TVC. Both △PPV and △PPV % have good predictability, but △PPV is recommended first. TVC performs well wherever in ICU or OR and would not be influenced by low lung compliance, moderate PEEP and measurement devices. But TVC should be cautious applied in prone position and patients with spontaneous breathing activity.
Availability of data and materials
The datasets used and/or analyzed in the present study are available from the corresponding author on reasonable request.
Abbreviations
- PPV:
-
Pulse pressure variation
- △PPV:
-
Absolute change of pulse pressure variation
- △PPV%:
-
Percentage change of pulse pressure variation
- TVC:
-
Tidal volume challenge
- SROC:
-
Summary receiver operating characteristic curve
- AUSROC:
-
Area under the summary receiving operating characteristic curve
- AUROC:
-
Area under the receiving operating characteristic curve
- DOR:
-
Diagnostic odds ratio
- QUADAS-2:
-
Quality assessment of diagnostic accuracy studies-2
- TPTD:
-
Transpulmonary thermodilution
- PEEP:
-
Positive end-expiratory pressure
- CI:
-
Cardiac index
- SVI:
-
Stoke volume index
- SV:
-
Stroke volume
- ODM:
-
Esophageal Doppler monitor
References
Marik PE, Monnet X. Teboul JL Hemodynamic parameters to guide fluid therapy. Ann Intensive Care. 2011;1:1.
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring: Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40:1795–815.
Michard F. Teboul JL Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest. 2002;121:2000–8.
Hong JQ, He HF, Chen ZY, Du ZS, Liu WF, Weng PQ, et al. Comparison of stroke volume variation with pulse pressure variation as a diagnostic indicator of fluid responsiveness in mechanically ventilated critically ill patients. Saudi Med J. 2014;35:261–8.
Marik PE, Cavallazzi R, Vasu T. Hirani A Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009;37:2642–7.
Yang X, Du B. Does pulse pressure variation predict fluid responsiveness in critically ill patients? A systematic review and meta-analysis. Critical Care (London, England). 2014;18:650.
De Backer D, Heenen S, Piagnerelli M, Koch M. Vincent JL Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med. 2005;31:517–23.
Alvarado Sánchez JI, Caicedo Ruiz JD, Diaztagle Fernández JJ, Amaya Zuñiga WF, Ospina-Tascón GA. Cruz Martínez LE Predictors of fluid responsiveness in critically ill patients mechanically ventilated at low tidal volumes: systematic review and meta-analysis. Ann Intensive Care. 2021;11:28.
Lakhal K, Ehrmann S, Benzekri-Lefèvre D, Runge I, Legras A, Dequin PF, et al. Respiratory pulse pressure variation fails to predict fluid responsiveness in acute respiratory distress syndrome. Critical Care (London, England). 2011;15:R85.
Colquhoun DA, Leis AM, Shanks AM, Mathis MR, Naik BI, Durieux ME, et al. A lower tidal volume regimen during one-lung ventilation for lung resection surgery is not associated with reduced postoperative pulmonary complications. Anesthesiology. 2021;134:562–76.
Kozian A, Schilling T, Schütze H, Senturk M, Hachenberg T, Hedenstierna G. Ventilatory protective strategies during thoracic surgery: effects of alveolar recruitment maneuver and low-tidal volume ventilation on lung density distribution. Anesthesiology. 2011;114:1025–35.
Aoyama H, Uchida K, Aoyama K, Pechlivanoglou P, Englesakis M, Yamada Y, et al. Assessment of therapeutic interventions and lung protective ventilation in patients with moderate to severe acute respiratory distress syndrome: a systematic review and network meta-analysis. JAMA Netw Open. 2019;2: e198116.
Myatra SN, Monnet X. Teboul JL Use of “tidal volume challenge” to improve the reliability of pulse pressure variation. Crit Care (London, England). 2017;21:60.
Myatra SN, Prabu NR, Divatia JV, Monnet X, Kulkarni AP, Teboul JL. The changes in pulse pressure variation or stroke volume variation after a “tidal volume challenge” reliably predict fluid responsiveness during low tidal volume ventilation. Crit Care Med. 2017;45:415–21.
Yonis H, Bitker L, Aublanc M, Perinel Ragey S, Riad Z, Lissonde F, et al. Change in cardiac output during Trendelenburg maneuver is a reliable predictor of fluid responsiveness in patients with acute respiratory distress syndrome in the prone position under protective ventilation. Crit Care (London, England). 2017;21:295.
Jun JH, Chung RK, Baik HJ, Chung MH, Hyeon JS, Lee YG, et al. The tidal volume challenge improves the reliability of dynamic preload indices during robot-assisted laparoscopic surgery in the Trendelenburg position with lung-protective ventilation. BMC Anesthesiol. 2019;19:142.
Messina A, Montagnini C, Cammarota G, De Rosa S, Giuliani F, Muratore L, et al. Tidal volume challenge to predict fluid responsiveness in the operating room: an observational study. Eur J Anaesthesiol. 2019;36:583–91.
Messina A, Montagnini C, Cammarota G, Giuliani F, Muratore L, Baggiani M, et al. Assessment of fluid responsiveness in prone neurosurgical patients undergoing protective ventilation: role of dynamic indices, tidal volume challenge, and end-expiratory occlusion test. Anesth Analg. 2020;130:752–61.
Elsayed AI, Selim KA, Zaghla HE, Mowafy HE. Fakher MA comparison of changes in PPV using a tidal volume challenge with a passive leg raising test to predict fluid responsiveness in patients ventilated using low tidal volume. Indian J Crit Care Med Peer-Rev Off Publ Indian Soc Crit Care Med. 2021;25:685–90.
Taccheri T, Gavelli F, Teboul JL, Shi R. Monnet X Do changes in pulse pressure variation and inferior vena cava distensibility during passive leg raising and tidal volume challenge detect preload responsiveness in case of low tidal volume ventilation? Crit Care (London, England). 2021;25:110.
Hamzaoui O, Shi R, Carelli S, Sztrymf B, Prat D, Jacobs F, et al. Changes in pulse pressure variation to assess preload responsiveness in mechanically ventilated patients with spontaneous breathing activity: an observational study. Br J Anaesth. 2021;127:532–8.
Shi R, Ayed S, Moretto F, Azzolina D, De Vita N, Gavelli F, et al. Tidal volume challenge to predict preload responsiveness in patients with acute respiratory distress syndrome under prone position. Crit Care (London, England). 2022;26:219.
Xu Y, Guo J, Wu Q, Chen J. Efficacy of using tidal volume challenge to improve the reliability of pulse pressure variation reduced in low tidal volume ventilated critically ill patients with decreased respiratory system compliance. BMC Anesthesiol. 2022;22:137.
Takata M, Wise RA. Robotham JL Effects of abdominal pressure on venous return: abdominal vascular zone conditions. J Appl Physiol. 1990;69:1961–72.
Monnet X, Bleibtreu A, Ferré A, Dres M, Gharbi R, Richard C, et al. Passive leg-raising and end-expiratory occlusion tests perform better than pulse pressure variation in patients with low respiratory system compliance. Crit Care Med. 2012;40:152–7.
Kang WS, Kim SH, Kim SY, Oh CS, Lee SA. Kim JS The influence of positive end-expiratory pressure on stroke volume variation in patients undergoing cardiac surgery: an observational study. J Thorac Cardiovasc Surg. 2014;148:3139–45.
Moher D, Liberati A, Tetzlaff J. Altman DG Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(264–9): w64.
Alberg AJ, Park JW, Hager BW, Brock MV. Diener-West M The use of “overall accuracy” to evaluate the validity of screening or diagnostic tests. J Gen Intern Med. 2004;19:460–5.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–36.
Field AP. Meta-analysis of correlation coefficients: a Monte Carlo comparison of fixed- and random-effects methods. Psychol Methods. 2001;6:161–80.
Riley RD, Abrams KR, Sutton AJ, Lambert PC, Thompson JR. Bivariate random-effects meta-analysis and the estimation of between-study correlation. BMC Med Res Methodol. 2007;7:3.
Rutter CM, Gatsonis CA. A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med. 2001;20:2865–84.
Fischer JE, Bachmann LM, Jaeschke R. A readers’ guide to the interpretation of diagnostic test properties: clinical example of sepsis. Intensive Care Med. 2003;29:1043–51.
Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thora Oncol Off Publ Int Assoc Study Lung Cancer. 2010;5:1315–6.
Moses LE, Shapiro D, Littenberg B. Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic approaches and some additional considerations. Stat Med. 1993;12:1293–316.
de Winter JC, Gosling SD. Potter J Comparing the Pearson and Spearman correlation coefficients across distributions and sample sizes: a tutorial using simulations and empirical data. Psychol Methods. 2016;21:273–90.
Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58:882–93.
Alvarado Sánchez JI, Caicedo Ruiz JD, Diaztagle Fernández JJ, Ospina-Tascón GA. Use of pulse pressure variation as predictor of fluid responsiveness in patients ventilated with low tidal volume: a systematic review and meta-analysis. Clin Medi Insights Circ Resp Pulm Med. 2020;14:1179548420901518.
Freitas FG, Bafi AT, Nascente AP, Assunção M, Mazza B, Azevedo LC, et al. Predictive value of pulse pressure variation for fluid responsiveness in septic patients using lung-protective ventilation strategies. Br J Anaesth. 2013;110:402–8.
Gattinoni L, Chiumello D, Carlesso E, Valenza F. Bench-to-bedside review: chest wall elastance in acute lung injury/acute respiratory distress syndrome patients. Crit Care (London, England). 2004;8:350–5.
Lansdorp B, Hofhuizen C, van Lavieren M, van Swieten H, Lemson J, van Putten MJ, et al. Mechanical ventilation-induced intrathoracic pressure distribution and heart-lung interactions*. Crit Care Med. 2014;42:1983–90.
Si X, Song X, Lin Q, Nie Y, Zhang G, Xu H, et al. Does end-expiratory occlusion test predict fluid responsiveness in mechanically ventilated patients? A systematic review and meta-analysis. Shock (Augusta, Ga). 2020;54:751–60.
Jun IJ, Chung MH, Kim JE, Lee HS, Son JM, Choi EM. The influence of positive end-expiratory pressure (PEEP) in predicting fluid responsiveness in patients undergoing one-lung ventilation. Int J Med Sci. 2021;18:2589–98.
Luecke T, Pelosi P. Clinical review: positive end-expiratory pressure and cardiac output. Crit Care (London, England). 2005;9:607–21.
Monnet X, Shi R, Teboul JL. Prediction of fluid responsiveness: What’s new? Ann Intensive Care. 2022;12:46.
Biais M, de Courson H, Lanchon R, Pereira B, Bardonneau G, Griton M, et al. Mini-fluid challenge of 100 ml of crystalloid predicts fluid responsiveness in the operating room. Anesthesiology. 2017;127:450–6.
Toscani L, Aya HD, Antonakaki D, Bastoni D, Watson X, Arulkumaran N, et al. What is the impact of the fluid challenge technique on diagnosis of fluid responsiveness? A systematic review and meta-analysis. Crit Care (London, England). 2017;21:207.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
XW designed the study and modified the manuscript. LJ, YZ and JG participated in the design of the study. XW, LJ and TH performed the statistical analysis, and drafted the manuscript. Search strategy, study selection, data extraction and quality assessment were performed independently by XW and LJ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Fig. S1.
Graphs for meta-regression analysis. CI = confidence interval. Meta-regression was performed by position (supine or semi- recumbent vs. prone or Trendelenburg), PEEP ((5mH2O≤PEEP ≤15mH2O vs. others), Place (ICU vs. OR) and Device (TPTD vs. other measurement tools other than TPTD).
Additional file 2: Table S1.
The influence of each trail for the meta-analysis.
Additional file 3: Fig. S2.
Summary receiver operating characteristic curve for the change of pulse pressure variation after tidal volume challenge predicting fluid responsiveness in low tidal volume ventilation except Yonis 2017.
Additional file 4: Fig. S3.
Sensitivity and specificity of the change of pulse pressure variation after tidal volume challenge predicting fluid responsiveness in low tidal volume ventilation for all data except Yonis 2017.
Additional file 5: Fig. S4.
Summary receiver operating characteristic curve for the change of pulse pressure variation after tidal volume challenge predicting fluid responsiveness in ICU subgroup.
Additional file 6: Fig. S5.
Summary receiver operating characteristic curve for the change of pulse pressure variation after tidal: volume challenge predicting fluid responsiveness in subgroups. a Supine or semi-recumbent group. b Lung compliance <30mH2O group. c Moderate PEEP group (5≤PEEP ≤15cmH2O). d Measurement tools without TPTD group.
Additional file 7: Fig. S6.
Summary receiver operating characteristic curve for △PPV and △PPV% after tidal volume challenge predicting fluid responsiveness. A absolute change of pulse pressure variation (△PPV). B percentage change of pulse pressure variation (△PPV%).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, X., Liu, S., Gao, J. et al. Does tidal volume challenge improve the feasibility of pulse pressure variation in patients mechanically ventilated at low tidal volumes? A systematic review and meta-analysis. Crit Care 27, 45 (2023). https://doi.org/10.1186/s13054-023-04336-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04336-6