Abstract
This article is one of ten reviews selected from the Annual Update in Intensive Care and Emergency Medicine 2017. Other selected articles can be found online at http://ccforum.com/series/annualupdate2017. Further information about the Annual Update in Intensive Care and Emergency Medicine is available from http://www.springer.com/series/8901.
Similar content being viewed by others
Background
Fluid loading is usually the first step in the resuscitation of patients with acute circulatory failure. Fluid responsiveness is defined as the ability of the left ventricle to increase its stroke volume in response to fluid administration [1]. Fluids are administered with the aim of increasing cardiac output and oxygen delivery. Thus giving fluid is not beneficial if cardiac output does not increase. According to the Frank‐Starling principle, increasing preload increases the left ventricular (LV) stroke volume if the ventricle is functioning on the steep portion of the Frank‐Starling curve. Once the left ventricle is functioning on the flat portion of the curve, further fluid loading has little effect on the stroke volume. In a normal heart, both ventricles generally operate on the steep portion of the Frank‐Starling curve and the patient is fluid responsive, unless large fluid volumes have already been administered (Fig. 1). In this case, the ventricles may operate on the flat part of the curve (Fig. 1). A failing heart operates on the flat portion of the curve, except for very low preload values and thus the same increase in cardiac preload induced by volume expansion may result in a negligible increase in stroke volume (Fig. 1).
Studies have shown that only about 50% of unstable critically ill patients will actually respond positively to a fluid challenge [1]. Uncorrected hypovolemia may result in inappropriate administration of vasopressor infusions, which may in turn affect tissue oxygenation, leading to organ dysfunction and death [2, 3]. On the other hand, excessive fluid loading is associated with increased complications, mortality and duration of intensive care unit (ICU) stay [4, 5]. Thus, it is important to identify fluid responders to know who can benefit from fluid administration and to avoid fluid overload in those who are not fluid responsive. However, identifying which patients will respond to volume expansion presents a daily challenge in ICUs today.
Dynamic changes in arterial waveform‐derived variables during mechanical ventilation, such as systolic pressure variation (SPV), pulse pressure variation (PPV) and stroke volume variation (SVV), have proven to be superior to traditionally used static indices, such as central venous pressure (CVP) and pulmonary artery occlusion pressure (PAOP), to predict fluid responsiveness [1, 6,7,8]. Of these indices, PPV and SVV are commonly used in clinical practice, with PPV being more reliable and having a higher level of evidence [7, 9, 10].
Heart‐lung interactions during mechanical ventilation: physiological principles underlying PPV and SVV
The PPV is calculated as the difference between the maximal and the minimal pulse pressure value over one ventilator cycle divided by their average value [6]. It can be automatically calculated by newer hemodynamic monitors. The SVV is derived from the arterial pressure waveform analysis and is automatically calculated by calibrated and uncalibrated pulse contour analysis cardiac output monitors. The principle mechanisms underlying how these parameters work are based on heart‐lung interactions during mechanical ventilation [11].
Intermittent positive‐pressure ventilation produces cyclic changes in the loading conditions of both the ventricles. The intrathoracic and transpulmonary pressures increase during inspiration leading to variable changes in the loading conditions of both the ventricles. Increase in intrathoracic pressures during mechanical insufflation decreases venous return and in turn decreases the right ventricular (RV) preload, whereas an increase in transpulmonary pressure increases RV afterload resulting in decreased RV stroke volume, which will be at its lowest at the end of inspiration [11,12,13,14,15,16]. At the same time, an increase in the intrathoracic and transpulmonary pressures results in decreased LV afterload and a transient increase in LV preload due to squeezing out of alveolar blood, leading to increased LV stroke volume, which will be at its maximum at the end of inspiration [11]. The reduction in RV stroke volume during inspiration leads to decreased LV filling after a lag period of two to three heart beats due to the pulmonary transit time [17]. This leads to decreased LV stroke volume, which will be its lowest during expiration.
Thus, intermittent positive‐pressure ventilation produces cyclic changes in LV stroke volume, which is maximum during inspiration and lowest during expiration. The magnitude of change in LV stroke volume, or of its surrogates, such as pulse pressure, will be magnified when the patient is preload‐dependent. Therefore, a high PPV value should be associated with preload responsiveness and a low PPV value with preload unresponsiveness (Fig. 1). A threshold value greater than 12–13% has been reported to be highly predictive of volume responsiveness [7, 9, 10].
Comparison of dynamic changes of arterial waveform‐derived variables during mechanical ventilation (SPV, PPV and SVV)
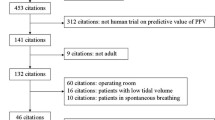
Since the earliest studies about PPV and SVV [6, 17], both indices have been consistently shown to be reliable predictors of fluid responsiveness. The first systematic review by Marik et al. [7] comparing PPV, SPV and SVV for prediction of fluid responsiveness in mechanically ventilated patients showed that the (AUROC) curves were 0.94, 0.84, and 0.86, respectively. The AUROC for PPV was significantly greater than that for either the SPV or the SVV (p < 0.001). Another meta‐analysis [9] comparing SVV and PPV as diagnostic indicators of fluid responsiveness in mechanically ventilated critically ill patients showed AUROC values of 0.84 for SVV and 0.88 for PPV. A recent meta‐analysis [10] that included only ICU patients ventilated with tidal volumes > 8 ml/kg, showed that PPV predicted fluid responsiveness accurately with an AUC of 0.94. A comparison of the predictive value of variables used to determine fluid responsiveness in these three systematic reviews [7, 9, 10] is given in Table 1. Among PPV, SVV and SPV, PPV has been most extensively studied and is more reliable.
Limitations with the use of PPV to predict fluid responsiveness
The PPV works on heart‐lung interactions and has several limitations for use in predicting fluid responsiveness, which are enumerated in Table 2. Recent studies [18,19,20] have questioned the applicability of PPV and SVV in the ICU. Tests like passive leg raising (PLR) [21,22,23] and end‐expiratory occlusion [24,25,26] can reliably predict fluid responsiveness and have been proposed as alternatives to be performed in these situations. PLR can help overcome most of the limitations of PPV. However, it requires continuous cardiac output monitoring and cannot be used in patients with neurotrauma or those requiring immobilization [27, 28]. The end‐expiratory occlusion test is not suitable for patients who are not intubated, whereas PLR can be reliably used in these patients. A mini‐fluid challenge [29] may also be used as an alternative to PPV, but requires a very precise technique for monitoring cardiac output. Using respiratory variations in the diameters of the superior [30] and inferior [31] vena cavae diameter obtained from transesophageal or transthoracic echocardiography to predict fluid responsiveness share the same limitations as PPV, except that they can be used in patients with cardiac arrhythmias. Although alternative tests have been proposed, few attempts have been made to improve the reliability of PPV itself in situations where it is currently not recommended for use [32].
Using a ‘tidal volume challenge’ to overcome the limitations associated with PPV during low tidal volume ventilation
Several studies have shown that PPV does not reliably predict fluid responsiveness during low tidal volume ventilation [25,34,35,36,, 33–37]. De Backer et al. [33] showed that PPV was a reliable predictor of fluid responsiveness, provided that the tidal volume was at least 8 ml/kg predicted body weight (PBW). During low tidal volume ventilation, PPV may indicate a non‐responsive status even in responders as the tidal volume might be insufficient to produce a significant change in the intrathoracic pressure [38, 39]. However, Freitas et al. [40] showed that PPV was a reliable marker of fluid responsiveness in septic patients with acute respiratory distress syndrome (ARDS) during low tidal volume ventilation using a lower cut‐off value of 6.5%.
Among the limitations with use of PPV during controlled mechanical ventilation in the ICU, the use of low tidal volume is the most common. Today the indications for use of low tidal volume in ICU are expanding [41, 42]. Two multicenter studies [18, 19] showed that the number of ICU patients in whom PPV was suitable for use was very low, with as many as 72–87% of the patients on controlled mechanical ventilation being unsuitable for use of this parameter, because of the use of low tidal volume ventilation. Two recent studies [43, 44] that used the ‘gray zone’ approach to investigate the clinical value of PPV, included several patients ventilated with low tidal volume. Biais et al. [44], in a subgroup analysis, showed that the gray zone was larger in patients ventilated with a low tidal volume than in patients with a tidal volume of at least 8 ml/kg PBW. These studies may mislead one to conclude that PPV has limited clinical value [32].
The ‘tidal volume challenge’ is a novel test proposed to improve the reliability of PPV during low tidal volume ventilation [45]. The test involves transiently increasing tidal volume from 6 ml/kg PBW to 8 ml/kg PBW for one minute and observing the change in PPV (∆PPV6–8) from baseline (PPV6) to that at 8 ml/kg PBW (PPV8). In a recent study testing the tidal volume challenge [45], 30 sets of measurements were recorded in 20 patients with acute circulatory failure receiving low tidal volume ventilation using volume assist‐control ventilation and without spontaneous breathing activity. Fluid responsiveness was defined as an increase in thermodilution cardiac output > 15% after giving a fluid bolus after reducing tidal volume back to 6 m/kg PBW. As expected, the PPV6 could not predict fluid responsiveness, with an AUROC of 0.69. Importantly, there was a significant increase in PPV (∆PPV6–8), following the tidal volume challenge only in fluid responders. The ∆PPV6–8 discriminated responders from non‐responders with an AUROC of 0.99 (sensitivity 94% and specificity 100%) with a cut off value of 3.5% [45]. The tidal volume challenge thus improved the reliability of PPV in predicting fluid responsiveness in patients receiving low tidal volume ventilation. Similar results were also seen using SVV (∆SVV6–8) obtained from a pulse contour analysis cardiac output device with an AUROC of 0.97 (sensitivity 88% and specificity 100%) with a cut off value of 2.5% [45]. The change in PPV after giving a fluid bolus (∆PPVfb) also accurately confirmed fluid responsiveness with an AUROC of 0.98 (sensitivity 94% and specificity 100%) with a cut off value of 1.5%.
How to perform and interpret the tidal volume challenge
This test is performed to assess fluid responsiveness in patents in shock, ventilated using low tidal volume without spontaneous breathing activity. The PPV is noted from the bedside monitor at baseline (tidal volume 6 ml/kg PBW). The tidal volume is then transiently increased from 6 ml/kg PBW to 8 ml/kg PBW for one minute. The PPV is recorded at 8 ml/kg PBW and the tidal volume is reduced back to 6 ml/kg PBW. The ∆PPV6–8 after performing the tidal volume challenge is recorded. A ∆PPV6–8 greater than 3.5% predicts fluid responsiveness with high accuracy.
PPV is unreliable in patients with low lung compliance, especially in patients with ARDS [38]. In these patients, airway pressure transmission is reduced, such that the cyclic changes in intrathoracic pressure may be attenuated even with marked changes in alveolar pressure [46]. Monnet et al. [25] showed that the predictive value of PPV was related to the compliance of the respiratory system and if the compliance was < 30 ml/cmH2O, PPV was less accurate in predicting fluid responsiveness. In our study, although the median compliance of the respiratory system was < 30 ml/cmH2O (25 [23,24,25,26,27,28,29,30,31,32,33]) during low tidal volume ventilation, it increased to > 30 ml/cmH2O (32 [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]) after the tidal volume challenge. Thus, the tidal volume challenge may help identify responders even when compliance of the respiratory system is low in patients receiving low tidal volume ventilation with recruitable lungs. This needs to be confirmed in an adequately powered study. Whether this approach will also work in patients who do not increase compliance of the respiratory system after giving a tidal volume challenge needs to be tested. Whether PPV will be reliable during spontaneous breathing attempts after giving a tidal volume challenge or in other situations where the use of PPV is limited also needs to be tested.
Advantages of using the tidal volume challenge
Use of a tidal volume challenge increases the reliability of PPV to predict fluid responsiveness during low tidal volume ventilation, which is now common practice in the ICU. It is a simple test that can be performed easily at the bedside. Importantly, observing the changes in PPV (obtained from a simple bedside hemodynamic monitor) during this test does not require a cardiac output monitor, making this test applicable even in resource‐limited settings. The ∆PPVfb accurately confirms fluid responsiveness. Thus, a combination of ∆PPV6–8 with ∆PPVfb can help predict and thereafter confirm fluid responsiveness when continuous cardiac output monitoring is unavailable.
Limitations of the tidal volume challenge
The tidal volume challenge may not be able to overcome the other limitations associated with the use of PPV, such as spontaneous breathing, cardiac arrhythmias, open chest, and raised intra-abdominal pressure and needs to be evaluated in these settings. Alternative techniques, such as PLR or end‐expiratory occlusion, when applicable, may be considered in these situations.
Conclusion
The PPV is a dynamic parameter that can be easily recorded from a bedside monitor and reliably predicts preload responsiveness. In addition, it does not require continuous cardiac output monitoring or any other tools or maneuvers to be performed. One of the major limitations with its use in patients receiving controlled mechanical ventilation is that it is unreliable during low tidal volume ventilation, which is now widely practiced in ICU patients. Discarding this useful parameter would, however, be like throwing the baby out with the bathwater. This major limitation can be easily overcome by using the ‘tidal volume challenge’ a simple bedside test, following which PPV can reliably predict fluid responsiveness. Whether this test may also have the potential to overcome other limitations associated with the use of PPV needs to be further studied. Alternative methods to assess preload responsiveness may be required to overcome the other limitations with the use of PPV.
References
Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest. 2002;121:2000–8.
Murakawa K, Kobayashi A. Effects of vasopressors on renal tissue gas tensions during hemorrhagic shock in dogs. Crit Care Med. 1998;16:789–92.
Pinsky MR, Brophy P, Padilla J, Paganini E, Pannu N. Fluid and volume monitoring. Int J Artif Organs. 2008;31:111–26.
Wiedemann HP, Wheeler AP, Bernard GR, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–75.
Acheampong A, Vincent JL. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care. 2015;19:251.
Michard F, Boussat S, Chemla D, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162:134–8.
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients. A systematic review of the literature. Crit Care Med. 2009;37:2642–7.
Perel A, Pizov R, Cotev S. Respiratory variations in the arterial pressure during mechanical ventilation reflect volume status and fluid responsiveness. Intensive Care Med. 2014;40:798–807.
Hong JQ, He HF, Chen ZY, et al. Comparison of stroke volume variation with pulse pressure variation as a diagnostic indicator of fluid responsiveness in mechanically ventilated critically ill patients. Saudi Med J. 2014;35:261–8.
Yang X, Du B. Does pulse pressure variation predicts fluid responsiveness in critically ill patients: a critical review and meta-analysis. Crit Care. 2014;18:650.
Michard F, Teboul JL. Using heart lung interactions to assess fluid responsiveness during mechanical ventilation. Crit Care. 2000;4:282–9.
Morgan BC, Martin WE, Hornbein TF, Crawford EW, Guntheroth WG. Hemodynamic effects of intermittent positive pressure ventilation. Anesthesiology. 1966;27:584–90.
Jardin F, Delorme G, Hardy A, Auvert B, Beauchet A, Bourdarias JP. Reevaluation of hemodynamic consequences of positive pressure ventilation: emphasis on cyclic right ventricular afterloading by mechanical lung inflation. Anesthesiology. 1990;72:966–70.
Permutt S, Wise RA, Brower RG. How changes in pleural and alveolar pressure cause changes in afterload and preload. In: Scharf SM, Cassidy SS, editors. Heart-Lung Interactions in Health and Disease. New York: Marcel Dekker; 1989. p. 243–50.
Jardin F, Farcot JC, Gueret P, Prost JF, Ozier Y, Bourdarias JP. Cyclic changes in arterial pulse during respiratory support. Circulation. 1983;68:266–74.
Scharf SM, Brown R, Saunders N, Green LH. Hemodynamic effects of positive-pressure inflation. J Appl Physiol. 1980;49:124–31.
Berkenstadt H, Margalit N, Hadani M, et al. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg. 2001;92:984–9.
Mahjoub Y, Lejeune V, Muller L, et al. Evaluation of pulse pressure variation validity criteria in critically ill patients: a prospective observational multicentre point prevalence study. Br J Anaesth. 2014;112:681–5.
Fischer MO, Mahjoub Y, Boisselier C, et al. Arterial pulse pressure variation suitability in critical care: A French national survey. Anaesth Crit Care Pain Med. 2015;34:23–8.
Benes J, Zatloukal J, Kletecka J, Simanova A, Haidingerova L, Pradl R. Respiratory induced dynamic variations of stroke volume and its surrogates as predictors of fluid responsiveness: applicability in the early stages of specific critical states. J Clin Monit Comput. 2013;28:225–31.
Monnet X, Marik P, Teboul JL. Passive leg raising for predicting fluid responsiveness: a systematic review and meta-analysis. Intensive Care Med. 2016;42:1935–47.
Monnet X, Teboul JL. Passive leg raising. Intensive Care Med. 2008;34:659–63.
Monnet X, Teboul JL. Passive leg raising: five rules, not a drop of fluid! Crit Care. 2015;19:18.
Monnet X, Osman D, Ridel C, Lamia B, Richard C, Teboul JL. Predicting volume responsiveness by using the end-expiratory occlusion in mechanically ventilated intensive care unit patients. Crit Care Med. 2009;37:951–6.
Monnet X, Bleibtreu A, Ferré A, et al. Passive leg-raising and end-expiratory occlusion tests perform better than pulse pressure variation in patients with low respiratory system compliance. Crit Care Med. 2012;40:152–7.
Silva S, Jozwiak M, Teboul JL, Persichini R, Richard C, Monnet X. End-expiratory occlusion test predicts preload responsiveness independently of positive end-expiratory pressure during acute respiratory distress syndrome. Crit Care Med. 2013;41:1692–701.
Guerin L, Monnet X, Teboul JL. Monitoring volume and fluid responsiveness: From static to dynamic indicators. Best Pract Res Clin Anaesthesiol. 2013;27:177–85.
De Backer D, Pinsky MR. Can one predict fluid responsiveness in spontaneously breathing patients? Intensive Care Med. 2007;33:1111–3.
Muller L, Toumi M, Bousquet PJ, et al. An increase in aortic blood flow after an infusion of 100 ml colloid over 1 minute can predict fluid responsiveness: the mini-fluid challenge study. Anesthesiology. 2011;115:541–7.
Vieillard-Baron A, Chergui K, Rabiller A, et al. Superior vena caval collapsibility as a gauge of volume status in ventilated septic patients. Intensive Care Med. 2004;30:1734–9.
Feissel M, Michard F, Faller JP, Teboul JL. The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med. 2004;30:1834–7.
Michard F, Chemla D, Teboul JL. Applicability of pulse pressure variation: how many shades of grey? Crit Care. 2015;19:144.
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent J. Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med. 2005;31:517–23.
Vallée F, Richard JC, Mari A, et al. Pulse pressure variations adjusted by alveolar driving pressure to assess fluid responsiveness. Intensive Care Med. 2009;35:1004–10.
Lakhal K, Ehrmann S, Benzekri-Lefèvre D, et al. Respiratory pulse pressure variation fails to predict fluid responsiveness in acute respiratory distress syndrome. Crit Care. 2011;15:R85.
Lansdorp B, Lemson J, vanPutten MJ, de Keijzer A, van der Hoeven JG, Pickkers P. Dynamic indices do not predict volume responsiveness in routine clinical practice. Br J Anaesth. 2012;108:395–401.
Reuter DA, Bayerlein J, Goepfert MS, et al. Influence of tidal volume on left ventricular stroke volume variation measured by pulse contour analysis in mechanically ventilated patients. Intensive Care Med. 2003;29:476–80.
Teboul JL, Monnet X. Pulse pressure variation and ARDS. Minerva Anestesiol. 2013;79:398–407.
Pinsky MR. Using ventilation-induced aortic pressure and flow variation to diagnose preload responsiveness. Intensive Care Med. 2004;30:1008–10.
Freitas FG, Bafi AT, Nascente AP, et al. Predictive value of pulse pressure variation for fluid responsiveness in septic patients using lung-protective ventilation strategies. Br J Anaesth. 2013;110:402–8.
Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA. 2012;308:1651–9.
Futier E, Pereira B, Jaber S. Intraoperative low-tidal-volume ventilation. N Engl J Med. 2013;369:1862–3.
Cannesson M, Le Manach Y, Hofer C, et al. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a “gray zone” approach. Anesthesiology. 2011;115:231–41.
Biais M, Ehrmann S, Mari A, et al. Clinical relevance of pulse pressure variations for predicting fluid responsiveness in mechanically ventilated intensive care unit patients: the grey zone approach. Crit Care. 2014;18:587.
Myatra SN, Prabu NR, Divatia JV, Monnet X, Kulkarni AP, Teboul JL. The changes in pulse pressure variation or stroke volume variation after a “tidal volume challenge” reliably predict fluid responsiveness during low tidal volume ventilation. Crit Care Med. 2017;45:415–21.
Teboul JL, Pinsky MR, Mercat A, et al. Estimating cardiac filling pressure in mechanically ventilated patients with hyperinflation. Crit Care Med. 2000;28:3631–6.
Acknowledgements
Not applicable.
Funding
The publication charges will be funded by the Division of Clinical Research of the Hôpitaux universitaires Paris-Sud (Assistance Publique-Hôpitaux de Paris).
Availability of data and materials
Not applicable.
Authors‘ contributions
SNM, XM and JLT contributed equally to the writing of this manuscript. All authors read and approved the final manuscript.
Competing interests
SNM has no competing interests. XM and JLT are members of the Medical Advisory Board of Pulsion Medical Systems.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Myatra, S., Monnet, X. & Teboul, JL. Use of ‘tidal volume challenge’ to improve the reliability of pulse pressure variation. Crit Care 21, 60 (2017). https://doi.org/10.1186/s13054-017-1637-x
Published:
DOI: https://doi.org/10.1186/s13054-017-1637-x