Abstract
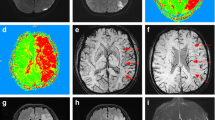
Intracerebral hemorrhage (ICH) is a common subtype of stroke and places a great burden on the family and society with a high mortality and disability rate and a poor prognosis. Many findings from imaging and pathologic studies have suggested that cerebral ischemic lesions visualized on diffusion-weighted imaging (DWI) in patients with ICH are not rare and are generally considered to be associated with poor outcome, increased risk of recurrent (ischemic and hemorrhagic) stroke, cognitive impairment, and death. In this review, we describe the changes in cerebral blood flow (CBF) and DWI lesions after ICH and discuss the risk factors and possible mechanisms related to the occurrence of DWI lesions, such as cerebral microangiopathy, cerebral atherosclerosis, aggressive early blood pressure lowering, hyperglycemia, and inflammatory response. We also point out that a better understanding of cerebral DWI lesions will be a key step toward potential therapeutic interventions to improve long-term recovery for patients with ICH.


Similar content being viewed by others
Data Availability
All data included in this article are available upon request by contact with the corresponding author.
References
de Oliveira Manoel, A.L., A. Goffi, F.G. Zampieri, D. Turkel-Parrella, A. Duggal, T.R. Marotta, R.L. Macdonald, and S. Abrahamson. The critical care management of spontaneous intracranial hemorrhage: a contemporary review. Crit Care. 2016; 20:272. https://doi.org/10.1186/s13054-016-1432-0.
Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. 2009;373(9675):1632–44. https://doi.org/10.1016/s0140-6736(09)60371-8.
Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001;344(19):1450–60. https://doi.org/10.1056/nejm200105103441907.
Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8(4):355–69. https://doi.org/10.1016/s1474-4422(09)70025-0.
Krishnamurthi RV, Feigin VL, Forouzanfar MH, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health. 2013;1(5):e259–81. https://doi.org/10.1016/s2214-109x(13)70089-5.
Krishnamurthi RV, Moran AE, Forouzanfar MH, Bennett DA, Mensah GA, Lawes CM, et al. The global burden of hemorrhagic stroke: a summary of findings from the GBD 2010 study. Glob Heart. 2014;9(1):101–6. https://doi.org/10.1016/j.gheart.2014.01.003.
Balami JS, Buchan AM. Complications of intracerebral haemorrhage. Lancet Neurol. 2012;11(1):101–18. https://doi.org/10.1016/s1474-4422(11)70264-2.
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9(2):167–76. https://doi.org/10.1016/s1474-4422(09)70340-0.
Sacco S, Marini C, Toni D, Olivieri L, Carolei A. Incidence and 10-year survival of intracerebral hemorrhage in a population-based registry. Stroke. 2009;40(2):394–9. https://doi.org/10.1161/strokeaha.108.523209.
Zia E, Engström G, Svensson PJ, Norrving B, Pessah-Rasmussen H. Three-year survival and stroke recurrence rates in patients with primary intracerebral hemorrhage. Stroke. 2009;40(11):3567–73. https://doi.org/10.1161/strokeaha.109.556324.
Gattellari M, Goumas C, Worthington J. Declining rates of fatal and nonfatal intracerebral hemorrhage: epidemiological trends in Australia. J Am Heart Assoc. 2014;3(6): e001161. https://doi.org/10.1161/jaha.114.001161.
Becker KJ, Baxter AB, Cohen WA, Bybee HM, Tirschwell DL, Newell DW, Winn HR, Longstreth WT Jr. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56(6):766–72. https://doi.org/10.1212/wnl.56.6.766.
Lei C, Wu B, Liu M, Tan G, Zeng Q. Pathogenesis and subtype of intracerebral hemorrhage (ICH) and ICH score determines prognosis. Curr Neurovasc Res. 2016;13(3):244–8. https://doi.org/10.2174/1567202613666160527141128.
Haque ME, Gabr RE, George SD, Zhao X, Boren SB, Zhang X, et al. Serial metabolic evaluation of perihematomal tissues in the intracerebral hemorrhage pig model. Front Neurosci. 2019;13:888. https://doi.org/10.3389/fnins.2019.00888.
Lim-Hing K, Rincon F. Secondary hematoma expansion and perihemorrhagic edema after intracerebral hemorrhage: from bench work to practical aspects. Front Neurol. 2017;8:74. https://doi.org/10.3389/fneur.2017.00074.
Selim M, Sheth KN. Perihematoma edema: a potential translational target in intracerebral hemorrhage? Transl Stroke Res. 2015;6(2):104–6. https://doi.org/10.1007/s12975-015-0389-7.
Fainardi E, Borrelli M, Saletti A, Schivalocchi R, Azzini C, Cavallo M, et al. CT perfusion mapping of hemodynamic disturbances associated to acute spontaneous intracerebral hemorrhage. Neuroradiology. 2008;50(8):729–40. https://doi.org/10.1007/s00234-008-0402-x.
Zhou J, Zhang H, Gao P, Lin Y, Li X. Assessment of perihematomal hypoperfusion injury in subacute and chronic intracerebral hemorrhage by CT perfusion imaging. Neurol Res. 2010;32(6):642–9. https://doi.org/10.1179/016164109x12445616596328.
Morotti A, Busto G, Bernardoni A, Leuci E, Casetta I, Fainardi E. Comparison of perihematomal perfusion in deep and lobar intracerebral hemorrhage. Neuroradiology. 2020;62(2):257–61. https://doi.org/10.1007/s00234-019-02331-9.
Morotti, A., G. Busto, G. Boulouis, E. Scola, A. Bernardoni, A. Fiorenza, et al. Delayed perihematomal hypoperfusion is associated with poor outcome in intracerebral haemorrhage. Eur J Clin Invest. 2021:e13696. https://doi.org/10.1111/eci.13696.
Rocha EA, Rocha F, Deliberalli I, de Andrade JBC, Ricarte IF, Singhal AB, Silva GS. Cerebral microembolism in intracerebral hemorrhage: a prospective case-control study. Neurocrit Care. 2020. https://doi.org/10.1007/s12028-020-01073-4.
Morotti A, Busto G, Bernardoni A, Marini S, Casetta I, Fainardi E. Association between perihematomal perfusion and intracerebral hemorrhage outcome. Neurocrit Care. 2020;33(2):525–32. https://doi.org/10.1007/s12028-020-00929-z.
Morotti A, Busto G, Scola E, Carlesi E, Di Pasquale F, Casetta I, Fainardi E. Association between perihematomal perfusion and intracerebral hemorrhage shape. Neuroradiology. 2021;63(9):1563–7. https://doi.org/10.1007/s00234-021-02709-8.
Boulanger, M., R. Schneckenburger, C. Join-Lambert, D.J. Werring, D. Wilson, J. Hodel, M. Zuber, and E. Touzé. Diffusion-weighted imaging hyperintensities in subtypes of acute intracerebral hemorrhage. Stroke. 2018:Strokeaha118021407. https://doi.org/10.1161/strokeaha.118.021407.
Smith EE, Schneider JA, Wardlaw JM, Greenberg SM. Cerebral microinfarcts: the invisible lesions. Lancet Neurol. 2012;11(3):272–82. https://doi.org/10.1016/s1474-4422(11)70307-6.
van Veluw SJ, Lauer A, Charidimou A, Bounemia N, Xiong L, Boulouis G, et al. Evolution of DWI lesions in cerebral amyloid angiopathy: evidence for ischemia. Neurology. 2017;89(21):2136–42. https://doi.org/10.1212/wnl.0000000000004668.
Auriel E, Edlow BL, Reijmer YD, Fotiadis P, Ramirez-Martinez S, Ni J, et al. Microinfarct disruption of white matter structure: a longitudinal diffusion tensor analysis. Neurology. 2014;83(2):182–8. https://doi.org/10.1212/wnl.0000000000000579.
Qureshi AI, Hanel RA, Kirmani JF, Yahia AM, Hopkins LN. Cerebral blood flow changes associated with intracerebral hemorrhage. Neurosurg Clin N Am. 2002;13(3):355–70. https://doi.org/10.1016/s1042-3680(02)00012-8.
Mayer SA, Lignelli A, Fink ME, Kessler DB, Thomas CE, Swarup R, Van Heertum RL. Perilesional blood flow and edema formation in acute intracerebral hemorrhage: a SPECT study. Stroke. 1998;29(9):1791–8. https://doi.org/10.1161/01.str.29.9.1791.
Pascual AM, López-Mut JV, Benlloch V, Chamarro R, Soler J, Láinez MJ. Perfusion-weighted magnetic resonance imaging in acute intracerebral hemorrhage at baseline and during the 1st and 2nd week: a longitudinal study. Cerebrovasc Dis. 2007;23(1):6–13. https://doi.org/10.1159/000095752.
Baron JC. Perfusion thresholds in human cerebral ischemia: historical perspective and therapeutic implications. Cerebrovasc Dis. 2001;11(Suppl 1):2–8. https://doi.org/10.1159/000049119.
Sinar EJ, Mendelow AD, Graham DI, Teasdale GM. Experimental intracerebral hemorrhage: effects of a temporary mass lesion. J Neurosurg. 1987;66(4):568–76. https://doi.org/10.3171/jns.1987.66.4.0568.
Wagner KR, Xi G, Hua Y, Kleinholz M, de Courten-Myers GM, Myers RE, Broderick JP, Brott TG. Lobar intracerebral hemorrhage model in pigs: rapid edema development in perihematomal white matter. Stroke. 1996;27(3):490–7. https://doi.org/10.1161/01.str.27.3.490.
Siddique MS, Fernandes HM, Wooldridge TD, Fenwick JD, Slomka P, Mendelow AD. Reversible ischemia around intracerebral hemorrhage: a single-photon emission computerized tomography study. J Neurosurg. 2002;96(4):736–41. https://doi.org/10.3171/jns.2002.96.4.0736.
Qureshi AI, Wilson DA, Hanley DF, Traystman RJ. No evidence for an ischemic penumbra in massive experimental intracerebral hemorrhage. Neurology. 1999;52(2):266–72. https://doi.org/10.1212/wnl.52.2.266.
Qureshi AI, Wilson DA, Hanley DF, Traystman RJ. Pharmacologic reduction of mean arterial pressure does not adversely affect regional cerebral blood flow and intracranial pressure in experimental intracerebral hemorrhage. Crit Care Med. 1999;27(5):965–71. https://doi.org/10.1097/00003246-199905000-00036.
Kuwata N, Kuroda K, Funayama M, Sato N, Kubo N, Ogawa A. Dysautoregulation in patients with hypertensive intracerebral hemorrhage. A SPECT study Neurosurg Rev. 1995;18(4):237–45. https://doi.org/10.1007/bf00383874.
Zazulia AR, Diringer MN, Videen TO, Adams RE, Yundt K, Aiyagari V, Grubb RL Jr, Powers WJ. Hypoperfusion without ischemia surrounding acute intracerebral hemorrhage. J Cereb Blood Flow Metab. 2001;21(7):804–10. https://doi.org/10.1097/00004647-200107000-00005.
Tayal AH, Gupta R, Yonas H, Jovin T, Uchino K, Hammer M, Wechsler L, Gebel JM. Quantitative perihematomal blood flow in spontaneous intracerebral hemorrhage predicts in-hospital functional outcome. Stroke. 2007;38(2):319–24. https://doi.org/10.1161/01.STR.0000254492.35504.db.
Warach S, Gaa J, Siewert B, Wielopolski P, Edelman RR. Acute human stroke studied by whole brain echo planar diffusion-weighted magnetic resonance imaging. Ann Neurol. 1995;37(2):231–41. https://doi.org/10.1002/ana.410370214.
Kim BJ, Kang HG, Kim HJ, Ahn SH, Kim NY, Warach S, Kang DW. Magnetic resonance imaging in acute ischemic stroke treatment. J Stroke. 2014;16(3):131–45. https://doi.org/10.5853/jos.2014.16.3.131.
Gioia LC, Kate M, Choi V, Sivakumar L, Jeerakathil T, Kosior J, Emery D, Butcher K. Ischemia in intracerebral hemorrhage is associated with leukoaraiosis and hematoma volume, not blood pressure reduction. Stroke. 2015;46(6):1541–7. https://doi.org/10.1161/strokeaha.114.008304.
Kidwell CS, Rosand J, Norato G, Dixon S, Worrall BB, James ML, et al. Ischemic lesions, blood pressure dysregulation, and poor outcomes in intracerebral hemorrhage. Neurology. 2017;88(8):782–8. https://doi.org/10.1212/wnl.0000000000003630.
Garg RK, Liebling SM, Maas MB, Nemeth AJ, Russell EJ, Naidech AM. Blood pressure reduction, decreased diffusion on MRI, and outcomes after intracerebral hemorrhage. Stroke. 2012;43(1):67–71. https://doi.org/10.1161/strokeaha.111.629493.
Xu XH, Gao T, Zhang WJ, Tong LS, Gao F. Remote diffusion-weighted imaging lesions in intracerebral hemorrhage: characteristics, mechanisms, outcomes, and therapeutic implications. Front Neurol. 2017;8:678. https://doi.org/10.3389/fneur.2017.00678.
Kang DW, Han MK, Kim HJ, Yun SC, Jeon SB, Bae HJ, Kwon SU, Kim JS. New ischemic lesions coexisting with acute intracerebral hemorrhage. Neurology. 2012;79(9):848–55. https://doi.org/10.1212/WNL.0b013e3182648a79.
Gregoire SM, Charidimou A, Gadapa N, Dolan E, Antoun N, Peeters A, et al. Acute ischaemic brain lesions in intracerebral haemorrhage: multicentre cross-sectional magnetic resonance imaging study. Brain. 2011;134(Pt 8):2376–86. https://doi.org/10.1093/brain/awr172.
Garg RK, Alberawi M, Ouyang B, John S, Silva ID, Shepherd S, et al. Timing of diffusion weighted imaging lesions in spontaneous intracerebral hemorrhage. J Neurol Sci. 2021;425: 117434. https://doi.org/10.1016/j.jns.2021.117434.
Gómez-Lado N, López-Arias E, Iglesias-Rey R, Díaz-Platas L, Medín-Aguerre S, Fernández-Ferreiro A, et al. [(18)F]-FMISO PET/MRI imaging shows ischemic tissue around hematoma in intracerebral hemorrhage. Mol Pharm. 2020;17(12):4667–75. https://doi.org/10.1021/acs.molpharmaceut.0c00932.
Hirano T, Read SJ, Abbott DF, Sachinidis JI, Tochon-Danguy HJ, Egan GF, et al. No evidence of hypoxic tissue on 18F-fluoromisonidazole PET after intracerebral hemorrhage. Neurology. 1999;53(9):2179–82. https://doi.org/10.1212/wnl.53.9.2179.
Nilsson, O.G., A. Polito, H. Säveland, U. Ungerstedt and C.H. Nordström. Are primary supratentorial intracerebral hemorrhages surrounded by a biochemical penumbra? A microdialysis study. Neurosurgery. 2006; 59(3):521–8; discussion 521–8. https://doi.org/10.1227/01.Neu.0000227521.58701.E5.
Tobieson L, Rossitti S, Zsigmond P, Hillman J, Marklund N. Persistent metabolic disturbance in the perihemorrhagic zone despite a normalized cerebral blood flow following surgery for intracerebral hemorrhage. Neurosurgery. 2019;84(6):1269–79. https://doi.org/10.1093/neuros/nyy179.
Murthy SB, Zhang C, Gupta A, Cho SM, Rivera-Lara L, Avadhani R, et al. Diffusion-weighted imaging lesions after intracerebral hemorrhage and risk of stroke: a MISTIE III and ATACH-2 analysis. Stroke. 2021;52(2):595–602. https://doi.org/10.1161/strokeaha.120.031628.
Murthy SB, Cho SM, Gupta A, Shoamanesh A, Navi BB, Avadhani R, et al. A pooled analysis of diffusion-weighted imaging lesions in patients with acute intracerebral hemorrhage. JAMA Neurol. 2020;77(11):1–9. https://doi.org/10.1001/jamaneurol.2020.2349.
Garg RK, Khan J, Dawe RJ, Conners J, John S, Prabhakaran S, et al. The influence of diffusion weighted imaging lesions on outcomes in patients with acute spontaneous intracerebral hemorrhage. Neurocrit Care. 2020;33(2):552–64. https://doi.org/10.1007/s12028-020-00933-3.
Ye XH, Cai XL, Nie DL, Chen YJ, Li JW, Xu XH, et al. Stress-induced hyperglycemia and remote diffusion-weighted imaging lesions in primary intracerebral hemorrhage. Neurocrit Care. 2020;32(2):427–36. https://doi.org/10.1007/s12028-019-00747-y.
Li JW, Xu YY, Chen YJ, Fan WW, Xu XH, Cai JS, Tong LS, Gao F. Early elevated neutrophil-to-lymphocyte ratio associated with remote diffusion-weighted imaging lesions in acute intracerebral hemorrhage. CNS Neurosci Ther. 2020;26(4):430–7. https://doi.org/10.1111/cns.13249.
Chen MY, Wang XC, Lou DN, Hu ZX, Zhou ML, Lu XD. Association between the hydrogenase level and the occurrence of remote diffusion-weighted imaging lesions after spontaneous intracerebral hemorrhage. J Clin Neurosci. 2020;77:49–54. https://doi.org/10.1016/j.jocn.2020.05.045.
Xu XH, Ye XH, Li JW, Cai JS, Gao T, Zhang WJ, et al. Association between remote diffusion-weighted imaging lesions and cerebral small vessel disease in primary intracerebral hemorrhage. Eur J Neurol. 2019;26(7):961–8. https://doi.org/10.1111/ene.13915.
Revel-Mouroz P, Viguier A, Cazzola V, Calviere L, Patsoura S, Rousseau V, et al. Acute ischaemic lesions are associated with cortical superficial siderosis in spontaneous intracerebral hemorrhage. Eur J Neurol. 2019;26(4):660–6. https://doi.org/10.1111/ene.13874.
Ye XH, Gao T, Xu XH, Cai JS, Li JW, Liu KM, et al. Factors associated with remote diffusion-weighted imaging lesions in spontaneous intracerebral hemorrhage. Front Neurol. 2018;9:209. https://doi.org/10.3389/fneur.2018.00209.
Xu XH, Ye XH, Cai JS, Gao T, Zhao GH, Zhang WJ, Tong LS, Gao F. Association of renal dysfunction with remote diffusion-weighted imaging lesions and total burden of cerebral small vessel disease in patients with primary intracerebral hemorrhage. Front Aging Neurosci. 2018;10:171. https://doi.org/10.3389/fnagi.2018.00171.
Wu B, Yao X, Lei C, Liu M, Selim MH. Enlarged perivascular spaces and small diffusion-weighted lesions in intracerebral hemorrhage. Neurology. 2015;85(23):2045–52. https://doi.org/10.1212/wnl.0000000000002169.
Menon RS, Burgess RE, Wing JJ, Gibbons MC, Shara NM, Fernandez S, et al. Predictors of highly prevalent brain ischemia in intracerebral hemorrhage. Ann Neurol. 2012;71(2):199–205. https://doi.org/10.1002/ana.22668.
Auriel E, Gurol ME, Ayres A, Dumas AP, Schwab KM, Vashkevich A, et al. Characteristic distributions of intracerebral hemorrhage-associated diffusion-weighted lesions. Neurology. 2012;79(24):2335–41. https://doi.org/10.1212/WNL.0b013e318278b66f.
Boulouis G, Charidimou A, Auriel E, Haley KE, van Etten ES, Fotiadis P, et al. Intracranial atherosclerosis and cerebral small vessel disease in intracerebral hemorrhage patients. J Neurol Sci. 2016;369:324–9. https://doi.org/10.1016/j.jns.2016.08.049.
Attems J, Jellinger K, Thal DR, Van Nostrand W. Review: sporadic cerebral amyloid angiopathy. Neuropathol Appl Neurobiol. 2011;37(1):75–93. https://doi.org/10.1111/j.1365-2990.2010.01137.x.
Charidimou A, Boulouis G, Haley K, Auriel E, van Etten ES, Fotiadis P, et al. White matter hyperintensity patterns in cerebral amyloid angiopathy and hypertensive arteriopathy. Neurology. 2016;86(6):505–11. https://doi.org/10.1212/wnl.0000000000002362.
Acampa, M., F. Guideri, I. Di Donato, R. Tassi, G. Marotta, G. Lo Giudice, P. D'Andrea, and G. Martini. Arterial stiffness in patients with deep and lobar intracerebral hemorrhage. J Stroke. 2014; 16(3):184–8. https://doi.org/10.5853/jos.2014.16.3.184.
Viswanathan A, Greenberg SM. Cerebral amyloid angiopathy in the elderly. Ann Neurol. 2011;70(6):871–80. https://doi.org/10.1002/ana.22516.
Smith EE, Greenberg SM. Beta-amyloid, blood vessels, and brain function. Stroke. 2009;40(7):2601–6. https://doi.org/10.1161/strokeaha.108.536839.
Tsai YH, Lee MH, Weng HH, Chang SW, Yang JT, Huang YC. Fate of diffusion restricted lesions in acute intracerebral hemorrhage. PLoS ONE. 2014;9(8): e105970. https://doi.org/10.1371/journal.pone.0105970.
Greenberg, S.M., M.W. Vernooij, C. Cordonnier, A. Viswanathan, R. Al-Shahi Salman, S. Warach, et al. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 2009; 8(2):165–74. https://doi.org/10.1016/s1474-4422(09)70013-4.
Lauer A, van Veluw SJ, William CM, Charidimou A, Roongpiboonsopit D, Vashkevich A, et al. Microbleeds on MRI are associated with microinfarcts on autopsy in cerebral amyloid angiopathy. Neurology. 2016;87(14):1488–92. https://doi.org/10.1212/wnl.0000000000003184.
Schmidt H, Zeginigg M, Wiltgen M, Freudenberger P, Petrovic K, Cavalieri M, et al. Genetic variants of the NOTCH3 gene in the elderly and magnetic resonance imaging correlates of age-related cerebral small vessel disease. Brain. 2011;134(Pt 11):3384–97. https://doi.org/10.1093/brain/awr252.
Meissner A. Hypertension and the brain: a risk factor for more than heart disease. Cerebrovasc Dis. 2016;42(3–4):255–62. https://doi.org/10.1159/000446082.
Smith CD, Johnson ES, Van Eldik LJ, Jicha GA, Schmitt FA, Nelson PT, et al. Peripheral (deep) but not periventricular MRI white matter hyperintensities are increased in clinical vascular dementia compared to Alzheimer’s disease. Brain Behav. 2016;6(3): e00438. https://doi.org/10.1002/brb3.438.
Fazekas F, Kleinert R, Offenbacher H, Schmidt R, Kleinert G, Payer F, Radner H, Lechner H. Pathologic correlates of incidental MRI white matter signal hyperintensities. Neurology. 1993;43(9):1683–9. https://doi.org/10.1212/wnl.43.9.1683.
Ogawa T, Okudera T, Fukasawa H, Hashimoto M, Inugami A, Fujita H, et al. Unusual widening of Virchow-Robin spaces: MR appearance. AJNR Am J Neuroradiol. 1995;16(6):1238–42.
Yin J, Lü TM, Qiu G, Huang RY, Fang M, Wang YY, Xiao D, Liu XJ. Intracerebral hematoma extends via perivascular spaces and perineurium. Tohoku J Exp Med. 2013;230(3):133–9. https://doi.org/10.1620/tjem.230.133.
Charidimou A, Meegahage R, Fox Z, Peeters A, Vandermeeren Y, Laloux P, et al. Enlarged perivascular spaces as a marker of underlying arteriopathy in intracerebral haemorrhage: a multicentre MRI cohort study. J Neurol Neurosurg Psychiatry. 2013;84(6):624–9. https://doi.org/10.1136/jnnp-2012-304434.
Charidimou A, Jaunmuktane Z, Baron JC, Burnell M, Varlet P, Peeters A, et al. White matter perivascular spaces: an MRI marker in pathology-proven cerebral amyloid angiopathy? Neurology. 2014;82(1):57–62. https://doi.org/10.1212/01.wnl.0000438225.02729.04.
Potter GM, Doubal FN, Jackson CA, Chappell FM, Sudlow CL, Dennis MS, Wardlaw JM. Enlarged perivascular spaces and cerebral small vessel disease. Int J Stroke. 2015;10(3):376–81. https://doi.org/10.1111/ijs.12054.
Arvanitakis Z, Capuano AW, Leurgans SE, Buchman AS, Bennett DA, Schneider JA. The relationship of cerebral vessel pathology to brain microinfarcts. Brain Pathol. 2017;27(1):77–85. https://doi.org/10.1111/bpa.12365.
Hilal S, Baaij LGA, de Groot M, Niessen WJ, Ikram MK, Ikram MA, Vernooij MW. Prevalence and clinical relevance of diffusion-weighted imaging lesions: the Rotterdam study. Neurology. 2019;93(11):e1058–67. https://doi.org/10.1212/wnl.0000000000008090.
Okamoto, Y., M. Ihara, H. Tomimoto, W. Taylor Kimberly and S.M. Greenberg. Silent ischemic infarcts are associated with hemorrhage burden in cerebral amyloid angiopathy. Neurology. 2010; 74(1):93; author reply 93. https://doi.org/10.1212/WNL.0b013e3181c77627.
Ter Telgte A, Scherlek AA, Reijmer YD, van der Kouwe AJ, van Harten T, Duering M, et al. Histopathology of diffusion-weighted imaging-positive lesions in cerebral amyloid angiopathy. Acta Neuropathol. 2020;139(5):799–812. https://doi.org/10.1007/s00401-020-02140-y.
Okamoto Y, Yamamoto T, Kalaria RN, Senzaki H, Maki T, Hase Y, et al. Cerebral hypoperfusion accelerates cerebral amyloid angiopathy and promotes cortical microinfarcts. Acta Neuropathol. 2012;123(3):381–94. https://doi.org/10.1007/s00401-011-0925-9.
Sato S, Uehara T, Hayakawa M, Nagatsuka K, Minematsu K, Toyoda K. Intra- and extracranial atherosclerotic disease in acute spontaneous intracerebral hemorrhage. J Neurol Sci. 2013;332(1–2):116–20. https://doi.org/10.1016/j.jns.2013.06.031.
Kalaria RN, Perry RH, O’Brien J, Jaros E. Atheromatous disease in small intracerebral vessels, microinfarcts and dementia. Neuropathol Appl Neurobiol. 2012;38(5):505–8. https://doi.org/10.1111/j.1365-2990.2012.01264.x.
Lammie GA. Hypertensive cerebral small vessel disease and stroke. Brain Pathol. 2002;12(3):358–70. https://doi.org/10.1111/j.1750-3639.2002.tb00450.x.
Zhang A, Ren M, Deng W, Xi M, Tian L, Han Z, et al. Ischemia in intracerebral hemorrhage: A comparative study of small-vessel and large-vessel diseases. Ann Clin Transl Neurol. 2022;9(1):79–90. https://doi.org/10.1002/acn3.51497.
Gao T, Yu W, Liu C. Mechanisms of ischemic stroke in patients with intracranial atherosclerosis: a high-resolution magnetic resonance imaging study. Exp Ther Med. 2014;7(5):1415–9. https://doi.org/10.3892/etm.2014.1600.
Bos D, Vernooij MW, Elias-Smale SE, Verhaaren BF, Vrooman HA, Hofman A, et al. Atherosclerotic calcification relates to cognitive function and to brain changes on magnetic resonance imaging. Alzheimers Dement. 2012;8(5 Suppl):S104–11. https://doi.org/10.1016/j.jalz.2012.01.008.
Wu XH, Chen XY, Wang LJ, Wong KS. Intracranial artery calcification and its clinical significance. J Clin Neurol. 2016;12(3):253–61. https://doi.org/10.3988/jcn.2016.12.3.253.
Hemphill, J.C., 3rd, S.M. Greenberg, C.S. Anderson, K. Becker, B.R. Bendok, M. Cushman, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46(7):2032–60. https://doi.org/10.1161/str.0000000000000069.
Rodriguez-Luna D, Piñeiro S, Rubiera M, Ribo M, Coscojuela P, Pagola J, et al. Impact of blood pressure changes and course on hematoma growth in acute intracerebral hemorrhage. Eur J Neurol. 2013;20(9):1277–83. https://doi.org/10.1111/ene.12180.
Sakamoto Y, Koga M, Yamagami H, Okuda S, Okada Y, Kimura K, et al. Systolic blood pressure after intravenous antihypertensive treatment and clinical outcomes in hyperacute intracerebral hemorrhage: the stroke acute management with urgent risk-factor assessment and improvement-intracerebral hemorrhage study. Stroke. 2013;44(7):1846–51. https://doi.org/10.1161/strokeaha.113.001212.
Butcher KS, Baird T, MacGregor L, Desmond P, Tress B, Davis S. Perihematomal edema in primary intracerebral hemorrhage is plasma derived. Stroke. 2004;35(8):1879–85. https://doi.org/10.1161/01.STR.0000131807.54742.1a.
Antihypertensive treatment of acute cerebral hemorrhage. Crit Care Med. 2010;38(2):637–48. https://doi.org/10.1097/CCM.0b013e3181b9e1a5.
Anderson CS, Huang Y, Wang JG, Arima H, Neal B, Peng B, et al. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): a randomised pilot trial. Lancet Neurol. 2008;7(5):391–9. https://doi.org/10.1016/s1474-4422(08)70069-3.
Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med. 2013;368(25):2355–65. https://doi.org/10.1056/NEJMoa1214609.
Butcher KS, Jeerakathil T, Hill M, Demchuk AM, Dowlatshahi D, Coutts SB, et al. The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial. Stroke. 2013;44(3):620–6. https://doi.org/10.1161/strokeaha.111.000188.
Buletko AB, Thacker T, Cho SM, Mathew J, Thompson NR, Organek N, Frontera JA, Uchino K. Cerebral ischemia and deterioration with lower blood pressure target in intracerebral hemorrhage. Neurology. 2018;91(11):e1058–66. https://doi.org/10.1212/wnl.0000000000006156.
Qureshi AI, Huang W, Lobanova I, Barsan WG, Hanley DF, Hsu CY, et al. Outcomes of intensive systolic blood pressure reduction in patients with intracerebral hemorrhage and excessively high initial systolic blood pressure: post hoc analysis of a randomized clinical trial. JAMA Neurol. 2020;77(11):1–11. https://doi.org/10.1001/jamaneurol.2020.3075.
Gioia L, Klahr A, Kate M, Buck B, Dowlatshahi D, Jeerakathil T, Emery D, Butcher K. The intracerebral hemorrhage acutely decreasing arterial pressure trial II (ICH ADAPT II) protocol. BMC Neurol. 2017;17(1):100. https://doi.org/10.1186/s12883-017-0884-4.
Aaslid R, Lindegaard KF, Sorteberg W, Nornes H. Cerebral autoregulation dynamics in humans. Stroke. 1989;20(1):45–52. https://doi.org/10.1161/01.str.20.1.45.
Castro P, Azevedo E, Sorond F. Cerebral Autoregulation in Stroke. Curr Atheroscler Rep. 2018;20(8):37. https://doi.org/10.1007/s11883-018-0739-5.
Xiao M, Li Q, Feng H, Zhang L, Chen Y. Neural vascular mechanism for the cerebral blood flow autoregulation after hemorrhagic stroke. Neural Plast. 2017;2017:5819514. https://doi.org/10.1155/2017/5819514.
Prabhakaran S, Naidech AM. Ischemic brain injury after intracerebral hemorrhage: a critical review. Stroke. 2012;43(8):2258–63. https://doi.org/10.1161/strokeaha.112.655910.
Carhuapoma JR, Ulatowski JA. Blood pressure control after intracerebral hemorrhage: have we reached the target? Crit Care Med. 2006;34(7):2023–4. https://doi.org/10.1097/01.Ccm.0000227117.08599.75.
Paulson OB, Waldemar G, Schmidt JF, Strandgaard S. Cerebral circulation under normal and pathologic conditions. Am J Cardiol. 1989;63(6):2c–5c. https://doi.org/10.1016/0002-9149(89)90396-2.
Yang J, Noyan-Ashraf MH, Meissner A, Voigtlaender-Bolz J, Kroetsch JT, Foltz W, et al. Proximal cerebral arteries develop myogenic responsiveness in heart failure via tumor necrosis factor-α-dependent activation of sphingosine-1-phosphate signaling. Circulation. 2012;126(2):196–206. https://doi.org/10.1161/circulationaha.111.039644.
Toth P, Tarantini S, Springo Z, Tucsek Z, Gautam T, Giles CB, et al. Aging exacerbates hypertension-induced cerebral microhemorrhages in mice: role of resveratrol treatment in vasoprotection. Aging Cell. 2015;14(3):400–8. https://doi.org/10.1111/acel.12315.
van Hooren KW, Spijkers LJ, van Breevoort D, Fernandez-Borja M, Bierings R, van Buul JD, et al. Sphingosine-1-phosphate receptor 3 mediates sphingosine-1-phosphate induced release of weibel-palade bodies from endothelial cells. PLoS ONE. 2014;9(3): e91346. https://doi.org/10.1371/journal.pone.0091346.
Garg RK, Ouyang B, Khan J, Panos N, Da Silva I, Hall D, et al. Association of longitudinal glycemia with diffusion weighted imaging lesions in spontaneous intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2021;30(3): 105554. https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105554.
Park HY, Kyeong H, Park DS, Lee HS, Chang H, Kim YS, Cho KH. Correlation between insulin resistance and intracranial atherosclerosis in patients with ischemic stroke without diabetes. J Stroke Cerebrovasc Dis. 2008;17(6):401–5. https://doi.org/10.1016/j.jstrokecerebrovasdis.2008.06.004.
Kernan WN, Inzucchi SE, Viscoli CM, Brass LM, Bravata DM, Horwitz RI. Insulin resistance and risk for stroke. Neurology. 2002;59(6):809–15. https://doi.org/10.1212/wnl.59.6.809.
Kaur R, Kaur M, Singh J. Endothelial dysfunction and platelet hyperactivity in type 2 diabetes mellitus: molecular insights and therapeutic strategies. Cardiovasc Diabetol. 2018;17(1):121. https://doi.org/10.1186/s12933-018-0763-3.
Saliba W, Barnett-Griness O, Gronich N, Molad J, Naftali J, Rennert G, Auriel E. Association of diabetes and glycated hemoglobin with the risk of intracerebral hemorrhage: a population-based cohort study. Diabetes Care. 2019;42(4):682–8. https://doi.org/10.2337/dc18-2472.
Del Bene A, Ciolli L, Borgheresi L, Poggesi A, Inzitari D, Pantoni L. Is type 2 diabetes related to leukoaraiosis? an updated review. Acta Neurol Scand. 2015;132(3):147–55. https://doi.org/10.1111/ane.12398.
Creager MA, Lüscher TF, Cosentino F, Beckman JA. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: Part I. Circulation. 2003;108(12):1527–32. https://doi.org/10.1161/01.Cir.0000091257.27563.32.
Carlotti, A.P., C. St George-Hyslop, A.M. Guerguerian, D. Bohn, K.S. Kamel, and M. Halperin. Occult risk factor for the development of cerebral edema in children with diabetic ketoacidosis: possible role for stomach emptying. Pediatr Diabetes. 2009; 10(8):522–33. https://doi.org/10.1111/j.1399-5448.2009.00529.x.
Justicia C, Salas-Perdomo A, Pérez-de-Puig I, Deddens LH, van Tilborg GAF, Castellví C, et al. Uric acid is protective after cerebral ischemia/reperfusion in hyperglycemic mice. Transl Stroke Res. 2017;8(3):294–305. https://doi.org/10.1007/s12975-016-0515-1.
Sehba FA, Mostafa G, Friedrich V Jr, Bederson JB. Acute microvascular platelet aggregation after subarachnoid hemorrhage. J Neurosurg. 2005;102(6):1094–100. https://doi.org/10.3171/jns.2005.102.6.1094.
Schwarzmaier SM, Kim SW, Trabold R, Plesnila N. Temporal profile of thrombogenesis in the cerebral microcirculation after traumatic brain injury in mice. J Neurotrauma. 2010;27(1):121–30. https://doi.org/10.1089/neu.2009.1114.
van Sloten TT, Sedaghat S, Carnethon MR, Launer LJ, Stehouwer CDA. Cerebral microvascular complications of type 2 diabetes: stroke, cognitive dysfunction, and depression. Lancet Diabetes Endocrinol. 2020;8(4):325–36. https://doi.org/10.1016/s2213-8587(19)30405-x.
Koga M, Yamagami H, Okuda S, Okada Y, Kimura K, Shiokawa Y, et al. Blood glucose levels during the initial 72 h and 3-month functional outcomes in acute intracerebral hemorrhage: the SAMURAI-ICH study. J Neurol Sci. 2015;350(1–2):75–8. https://doi.org/10.1016/j.jns.2015.02.018.
McCowen KC, Malhotra A, Bistrian BR. Stress-induced hyperglycemia. Crit Care Clin. 2001;17(1):107–24. https://doi.org/10.1016/s0749-0704(05)70154-8.
Feibel JH, Hardy PM, Campbell RG, Goldstein MN, Joynt RJ. Prognostic value of the stress response following stroke. JAMA. 1977;238(13):1374–6.
Huang YH, Chung CL, Tsai HP, Wu SC, Chang CZ, Chai CY, Lee TC, Kwan AL. Hyperglycemia aggravates cerebral vasospasm after subarachnoid hemorrhage in a rat model. Neurosurgery. 2017;80(5):809–15. https://doi.org/10.1093/neuros/nyx016.
Ago T, Matsuo R, Hata J, Wakisaka Y, Kuroda J, Kitazono T, Kamouchi M. Insulin resistance and clinical outcomes after acute ischemic stroke. Neurology. 2018;90(17):e1470–7. https://doi.org/10.1212/wnl.0000000000005358.
Chen ZQ, Yu H, Li HY, Shen HT, Li X, Zhang JY, et al. Negative regulation of glial Tim-3 inhibits the secretion of inflammatory factors and modulates microglia to antiinflammatory phenotype after experimental intracerebral hemorrhage in rats. CNS Neurosci Ther. 2019;25(6):674–84. https://doi.org/10.1111/cns.13100.
Gusdon AM, Gialdini G, Kone G, Baradaran H, Merkler AE, Mangat HS, et al. Neutrophil-lymphocyte ratio and perihematomal edema growth in intracerebral hemorrhage. Stroke. 2017;48(9):2589–92. https://doi.org/10.1161/strokeaha.117.018120.
Lattanzi S, Cagnetti C, Provinciali L, Silvestrini M. Neutrophil-to-lymphocyte ratio predicts the outcome of acute intracerebral hemorrhage. Stroke. 2016;47(6):1654–7. https://doi.org/10.1161/strokeaha.116.013627.
Wang F, Xu F, Quan Y, Wang L, Xia JJ, Jiang TT, et al. Early increase of neutrophil-to-lymphocyte ratio predicts 30-day mortality in patients with spontaneous intracerebral hemorrhage. CNS Neurosci Ther. 2019;25(1):30–5. https://doi.org/10.1111/cns.12977.
Al-Mufti F, Amuluru K, Damodara N, Dodson V, Roh D, Agarwal S, et al. Admission neutrophil-lymphocyte ratio predicts delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. J Neurointerv Surg. 2019;11(11):1135–40. https://doi.org/10.1136/neurintsurg-2019-014759.
De Meyer SF, Denorme F, Langhauser F, Geuss E, Fluri F, Kleinschnitz C. Thromboinflammation in stroke brain damage. Stroke. 2016;47(4):1165–72. https://doi.org/10.1161/strokeaha.115.011238.
Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol. 2011;11(8):519–31. https://doi.org/10.1038/nri3024.
Pfeiler S, Stark K, Massberg S, Engelmann B. Propagation of thrombosis by neutrophils and extracellular nucleosome networks. Haematologica. 2017;102(2):206–13. https://doi.org/10.3324/haematol.2016.142471.
Massberg S, Grahl L, von Bruehl ML, Manukyan D, Pfeiler S, Goosmann C, et al. Reciprocal coupling of coagulation and innate immunity via neutrophil serine proteases. Nat Med. 2010;16(8):887–96. https://doi.org/10.1038/nm.2184.
Miyoshi N, Tanigawa T, Nishioka S, Maruyama K, Eguchi E, Tanaka K, et al. Association of salivary lactate dehydrogenase level with systemic inflammation in a Japanese population. J Periodontal Res. 2018;53(4):487–94. https://doi.org/10.1111/jre.12537.
Liu Y, Yang S, Cai E, Lin L, Zeng P, Nie B, et al. Functions of lactate in the brain of rat with intracerebral hemorrhage evaluated with MRI/MRS and in vitro approaches. CNS Neurosci Ther. 2020;26(10):1031–44. https://doi.org/10.1111/cns.13399.
Hextrum S, Minhas JS, Liotta EM, Sorond FA, Naidech AM, Maas MB. Hypocapnia, ischemic lesions, and outcomes after intracerebral hemorrhage. J Neurol Sci. 2020;418: 117139. https://doi.org/10.1016/j.jns.2020.117139.
Williamson CA, Sheehan KM, Tipirneni R, Roark CD, Pandey AS, Thompson BG, Rajajee V. The association between spontaneous hyperventilation, delayed cerebral ischemia, and poor neurological outcome in patients with subarachnoid hemorrhage. Neurocrit Care. 2015;23(3):330–8. https://doi.org/10.1007/s12028-015-0138-5.
Kety SS, Schmidt CF. THE EFFECTS OF ACTIVE AND PASSIVE HYPERVENTILATION ON CEREBRAL BLOOD FLOW, CEREBRAL OXYGEN CONSUMPTION, CARDIAC OUTPUT, AND BLOOD PRESSURE OF NORMAL YOUNG MEN. J Clin Invest. 1946;25(1):107–19. https://doi.org/10.1172/jci101680.
Carrera E, Schmidt JM, Fernandez L, Kurtz P, Merkow M, Stuart M, et al. Spontaneous hyperventilation and brain tissue hypoxia in patients with severe brain injury. J Neurol Neurosurg Psychiatry. 2010;81(7):793–7. https://doi.org/10.1136/jnnp.2009.174425.
Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9(7):689–701. https://doi.org/10.1016/s1474-4422(10)70104-6.
Reijmer YD, van Veluw SJ, Greenberg SM. Ischemic brain injury in cerebral amyloid angiopathy. J Cereb Blood Flow Metab. 2016;36(1):40–54. https://doi.org/10.1038/jcbfm.2015.88.
Maas MB, Nemeth AJ, Rosenberg NF, Kosteva AR, Guth JC, Liotta EM, Prabhakaran S, Naidech AM. Subarachnoid extension of primary intracerebral hemorrhage is associated with poor outcomes. Stroke. 2013;44(3):653–7. https://doi.org/10.1161/strokeaha.112.674341.
Li X, Zhang B, Lou M. The relation between acute intracerebral hemorrhage and diffusion-weighted imaging lesions: a meta-analysis. J Thromb Thrombolysis. 2021. https://doi.org/10.1007/s11239-021-02430-6.
Morotti A, Busto G, Bernardoni A, Tamborino C, Fainardi E. Association between perihematomal cerebral blood volume and intracerebral hemorrhage expansion: a computed tomography perfusion study. Ann Neurol. 2019;85(6):943–7. https://doi.org/10.1002/ana.25466.
Dowlatshahi D, Demchuk AM, Flaherty ML, Ali M, Lyden PL, Smith EE. Defining hematoma expansion in intracerebral hemorrhage: relationship with patient outcomes. Neurology. 2011;76(14):1238–44. https://doi.org/10.1212/WNL.0b013e3182143317.
Schlunk F, Greenberg SM. The pathophysiology of intracerebral hemorrhage formation and expansion. Transl Stroke Res. 2015;6(4):257–63. https://doi.org/10.1007/s12975-015-0410-1.
Keep RF, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. 2012;11(8):720–31. https://doi.org/10.1016/s1474-4422(12)70104-7.
Murthy SB, Diaz I, Wu X, Merkler AE, Iadecola C, Safford MM, et al. Risk of arterial ischemic events after intracerebral hemorrhage. Stroke. 2020;51(1):137–42. https://doi.org/10.1161/strokeaha.119.026207.
Liotta EM, Singh M, Kosteva AR, Beaumont JL, Guth JC, Bauer RM, et al. Predictors of 30-day readmission after intracerebral hemorrhage: a single-center approach for identifying potentially modifiable associations with readmission. Crit Care Med. 2013;41(12):2762–9. https://doi.org/10.1097/CCM.0b013e318298a10f.
Wen T, Liu B, Wan X, Zhang X, Zhang J, Zhou X, Lau AYL, Zhang Y. Risk factors associated with 31-day unplanned readmission in 50,912 discharged patients after stroke in China. BMC Neurol. 2018;18(1):218. https://doi.org/10.1186/s12883-018-1209-y.
Auriel E, Westover MB, Bianchi MT, Reijmer Y, Martinez-Ramirez S, Ni J, et al. Estimating total cerebral microinfarct burden from diffusion-weighted imaging. Stroke. 2015;46(8):2129–35. https://doi.org/10.1161/strokeaha.115.009208.
Launer LJ, Hughes TM, White LR. Microinfarcts, brain atrophy, and cognitive function: the Honolulu Asia Aging Study Autopsy Study. Ann Neurol. 2011;70(5):774–80. https://doi.org/10.1002/ana.22520.
Raman MR, Preboske GM, Przybelski SA, Gunter JL, Senjem ML, Vemuri P, et al. Antemortem MRI findings associated with microinfarcts at autopsy. Neurology. 2014;82(22):1951–8. https://doi.org/10.1212/wnl.0000000000000471.
Blanco-Colio, L.M., J.L. Martín-Ventura, E. de Teresa, C. Farsang, A. Gaw, G. Gensini, et al. Elevated ICAM-1 and MCP-1 plasma levels in subjects at high cardiovascular risk are diminished by atorvastatin treatment. Atorvastatin on Inflammatory Markers study: a substudy of Achieve Cholesterol Targets Fast with Atorvastatin Stratified Titration. Am Heart J. 2007; 153(5):881–8. https://doi.org/10.1016/j.ahj.2007.02.029.
Biffi A, Devan WJ, Anderson CD, Ayres AM, Schwab K, Cortellini L, et al. Statin use and outcome after intracerebral hemorrhage: case-control study and meta-analysis. Neurology. 2011;76(18):1581–8. https://doi.org/10.1212/WNL.0b013e3182194be9.
Lei C, Chen T, Chen C, Ling Y. Pre-intracerebral hemorrhage and in-hospital statin use in intracerebral hemorrhage: a systematic review and meta-analysis. World Neurosurg. 2018;111:47–54. https://doi.org/10.1016/j.wneu.2017.12.020.
Lin, M.S., Y.S. Lin, S.T. Chang, P.C. Wang, V. Chien-Chia Wu, W.Y. Lin, and C.M. Chung. Effect of initiating statin therapy on long-term outcomes of patients with dyslipidemia after intracerebral hemorrhage. Atherosclerosis. 2019; 288:137–145. https://doi.org/10.1016/j.atherosclerosis.2019.07.009.
Noda H, Iso H, Irie F, Sairenchi T, Ohtaka E, Doi M, Izumi Y, Ohta H. Low-density lipoprotein cholesterol concentrations and death due to intraparenchymal hemorrhage: the Ibaraki Prefectural Health Study. Circulation. 2009;119(16):2136–45. https://doi.org/10.1161/circulationaha.108.795666.
Goldstein LB, Amarenco P, Szarek M, Callahan A 3rd, Hennerici M, Sillesen H, Zivin JA, Welch KM. Hemorrhagic stroke in the stroke prevention by aggressive reduction in cholesterol levels study. Neurology. 2008;70(24 Pt 2):2364–70. https://doi.org/10.1212/01.wnl.0000296277.63350.77.
Maestrini I, Altieri M, Di Clemente L, Vicenzini E, Pantano P, Raz E, et al. Longitudinal study on low-dose aspirin versus placebo administration in silent brain infarcts: the silence study. Stroke Res Treat. 2018;2018:7532403. https://doi.org/10.1155/2018/7532403.
Al-Shahi Salman, R., D.P. Minks, D. Mitra, M.A. Rodrigues, P. Bhatnagar, J.C. du Plessis, et al. Effects of antiplatelet therapy on stroke risk by brain imaging features of intracerebral haemorrhage and cerebral small vessel diseases: subgroup analyses of the RESTART randomised, open-label trial. Lancet Neurol. 2019; 18(7):643–652. https://doi.org/10.1016/s1474-4422(19)30184-x.
Biffi A, Halpin A, Towfighi A, Gilson A, Busl K, Rost N, et al. Aspirin and recurrent intracerebral hemorrhage in cerebral amyloid angiopathy. Neurology. 2010;75(8):693–8. https://doi.org/10.1212/WNL.0b013e3181eee40f.
Manerba M, Di Ianni L, Govoni M, Roberti M, Recanatini M, Di Stefano G. Lactate dehydrogenase inhibitors can reverse inflammation induced changes in colon cancer cells. Eur J Pharm Sci. 2017;96:37–44. https://doi.org/10.1016/j.ejps.2016.09.014.
Funding
This review was supported by grants from the National Natural Science Foundation of China (82071330, 81901219) and Hubei Provincial Department of Science & Technology (2021BCA109).
Author information
Authors and Affiliations
Contributions
JY, CP, and ZT conceived the review. JY performed the literature search and wrote the paper, and SC, XL, and JJ edited language. YT, CP, and ZT reviewed and edited the manuscript before submission. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical Approval
This article does not include any studies with human participants or animals performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, J., Jing, J., Chen, S. et al. Changes in Cerebral Blood Flow and Diffusion-Weighted Imaging Lesions After Intracerebral Hemorrhage. Transl. Stroke Res. 13, 686–706 (2022). https://doi.org/10.1007/s12975-022-00998-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-022-00998-6