Abstract
Background and Purpose
Stress-induced hyperglycemia (SIH) is the relative transient increase in glucose during a critical illness such as intracerebral hemorrhage (ICH) and is likely to play an important role in the pathogenesis of remote diffusion-weighted imaging (DWI) lesion (R-DWIL) in primary ICH. We sought to determine the association between SIH and the occurrence of R-DWILs.
Methods
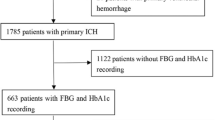
We prospectively enrolled primary ICH patients within 14 days after onset from November 2016 to May 2018. In these patients, cerebral magnetic resonance imaging was performed within 14 days after ICH onset. R-DWIL was defined as a hyperintensity signal in DWI with corresponding hypointensity in apparent diffusion coefficient, and at least 20 mm apart from the hematoma. SIH was measured by stress-induced hyperglycemia ratio (SHR). SHR was calculated by fasting blood glucose (FBG) divided by estimated average glucose derived from glycosylated hemoglobin. The included patients were dichotomized into two groups by the 50th percentile of SHR, and named as SHR (−P50) group and SHR (P50+) group, respectively. We evaluated the association between SHR and R-DWIL occurrence using multivariable logistic regression modeling adjusted for potential confounders.
Results
Among the 288 patients enrolled, forty-six (16.0%) of them had one or more R-DWILs. Compared with the patients in the lower 50% of SHR (SHR [−P50]), the odds ratio (OR) [95% confidence interval (CI)] for the higher 50% of SHR (SHR [P50+]) group for R-DWIL occurrence was 3.13 (1.39–7.07) in the total population and 6.33 (2.19–18.30) in population absent of background hyperglycemia after adjusting for potential covariates. Similar results were observed after further adjusted for FBG.
Conclusions
Our study demonstrated that SIH was associated with the occurrence of R-DWILs in patients with primary ICH within 14 days of symptom onset.



Similar content being viewed by others
References
Qureshi AI, Tuhrim S, Broderick JP, et al. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001;344(19):1450–60.
Hemphill JC, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32(4):891–7.
Menon RS, Burgess RE, Wing JJ, et al. Predictors of highly prevalent brain ischemia in intracerebral hemorrhage. Ann Neurol. 2012;71(2):199–205.
Prabhakaran S, Gupta R, Ouyang B, et al. Acute brain infarcts after spontaneous intracerebral hemorrhage: a diffusion-weighted imaging study. Stroke. 2010;41(1):89–94.
Tsai YH, Lee MH, Weng HH, et al. Fate of diffusion restricted lesions in acute intracerebral hemorrhage. PLoS ONE. 2014;9(8):e105970.
Gregoire SM, Charidimou A, Gadapa N, et al. Acute ischemic brain lesions in intracerebral haemorrhage: multicentre cross-sectional magnetic resonance imaging study. Brain. 2011;134(Pt 8):2376–86.
Kang DW, Han MK, Kim HJ, et al. New ischemic lesions coexisting with acute intracerebral hemorrhage. Neurology. 2012;79(9):848–55.
Kimberly WT, Gilson A, Rost NS, et al. Silent ischemic infarcts are associated with hemorrhage burden in cerebral amyloid angiopathy. Neurology. 2009;72(14):1230–5.
Gioia LC, Kate M, Choi V, et al. Ischemia in intracerebral hemorrhage is associated with leukoaraiosis and hematoma volume, not blood pressure reduction. Stroke. 2015;46(6):1541–7.
Wu B, Yao X, Lei C, Liu M, Selim MH. Enlarged perivascular spaces and small diffusion-weighted lesions in intracerebral hemorrhage. Neurology. 2015;85(23):2045–52.
Auriel E, Gurol ME, Ayres A, et al. Characteristic distributions of intracerebral hemorrhage-associated diffusion-weighted lesions. Neurology. 2012;79(24):2335–41.
Garg RK, Liebling SM, Maas MB, et al. Blood pressure reduction, decreased diffusion on MRI, and outcomes after intracerebral hemorrhage. Stroke. 2012;43(1):67–71.
Ye XH, Gao T, Xu XH, et al. Factors associated with remote diffusion-weighted imaging lesions in spontaneous intracerebral hemorrhage. Front Neurol. 2018;9:209.
Xu XH, Ye XH, Cai JS, et al. Association of renal dysfunction with remote diffusion-weighted imaging lesions and total burden of cerebral small vessel disease in patients with primary intracerebral hemorrhage. Front Aging Neurosci. 2018;10:171.
Xu XH, Ye XH, Li JW, et al. Association between remote diffusion-weighted imaging lesions and cerebral small vessel disease in primary intracerebral hemorrhage. Eur J Neurol. 2019;26(7):961–8.
Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein HC. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32(10):2426–32.
Yoon JA, Kim DY, Sohn MK, et al. Effect of stress hyperglycemia and intensive rehabilitation therapy in non-diabetic hemorrhagic stroke: Korean Stroke Cohort for Functioning and Rehabilitation. Eur J Neurol. 2016;23(11):1658–65.
Bejot Y, Aboa-Eboule C, Hervieu M, et al. The deleterious effect of admission hyperglycemia on survival and functional outcome in patients with intracerebral hemorrhage. Stroke. 2012;43(1):243–5.
Saxena A, Anderson CS, Wang X, et al. Prognostic significance of hyperglycemia in acute intracerebral hemorrhage: the INTERACT2 Study. Stroke. 2016;47(3):682–8.
Zheng J, Yu Z, Ma L, et al. Association between blood glucose and functional outcome in intracerebral hemorrhage: a systematic review and meta-analysis. World Neurosurg. 2018;114:S1878875018305552.
Guo X, Li H, Zhang Z, et al. Hyperglycemia and mortality risk in patients with primary intracerebral hemorrhage: a meta-analysis. Mol Neurobiol. 2016;53(4):2269–75.
Selvin E, Rawlings AM, Grams M, et al. Prognostic utility of fructosamine and glycated albumin for incident diabetes and microvascular complications. Lancet Diabetes Endocrinol. 2014;2(4):279.
Roberts GW, Quinn SJ, Valentine N, et al. Relative hyperglycemia, a marker of critical illness: introducing the stress hyperglycemia ratio. J Clin Endocrinol Metab. 2015;100(12):4490–7.
Yang Y, Kim TH, Yoon KH, et al. The stress hyperglycemia ratio, an index of relative hyperglycemia, as a predictor of clinical outcomes after percutaneous coronary intervention. Int J Cardiol. 2017;241:57–63.
Greenberg SM, Charidimou A. Diagnosis of cerebral amyloid angiopathy: evolution of the Boston criteria. Stroke. 2018;49(2):491–7.
Teo BW, Xu H, Wang D, et al. GFR estimating equations in a multiethnic Asian population. Am J Kidney Dis. 2011;58(1):56–63.
Coburn HJ, Carroll JJ. Improved manual and automated colorimetric determination of serum glucose, with use of hexokinase and glucose-6-phosphate dehydrogenase. Clin Chem. 1973;19(1):127–30.
Nathan DM, Kuenen J, Borg R, et al. Translating the A1C assay into estimated average glucose values. Diabetes Care. 2008;31(8):1473–8.
Greenberg SM, Vernooij MW, Cordonnier C, et al. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 2009;8(2):165–74.
Fazekas F, Barkhof F, Wahlund LO, et al. CT and MRI rating of white matter lesions. Cerebrovasc Dis. 2002;13(Suppl 2):31–6.
Maclullich AM, Wardlaw JM, Ferguson KJ, et al. Enlarged perivascular spaces are associated with cognitive function in healthy elderly men. J Neurol Neurosurg Psychiatry. 2004;75(11):1519–23.
Hansen TP, Cain J, Thomas O, Jackson A. Dilated perivascular spaces in the Basal Ganglia are a biomarker of small-vessel disease in a very elderly population with dementia. AJNR Am J Neuroradiol. 2015;36(5):893–8.
Lau KK, Li L, Schulz U, et al. Total small vessel disease score and risk of recurrent stroke: validation in 2 large cohorts. Neurology. 2017;88(24):2260–7.
Fan Z, Hao L, Juan Q, et al. Hyperglycemia is associated with island sign in patients with intracerebral hemorrhage. World Neurosurg. 2018;119:e703–9.
Zhang F, Li H, Qian J, et al. Hyperglycemia predicts blend sign in patients with intracerebral hemorrhage. Med Sci Monit. 2018;24:6237–44.
Wu TY, Putaala J, Sharma G, et al. Persistent hyperglycemia is associated with increased mortality after intracerebral hemorrhage. J Am Heart Assoc. 2017;6(8):e005760.
Wada S, Yoshimura S, Inoue M, et al. Outcome prediction in acute stroke patients by continuous glucose monitoring. J Am Heart Assoc. 2018;7(8):e008744.
Claude H, Greenberg SM, Anderson CS, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke J Cereb Circ. 2015;46(7):2032.
Prabhakaran S, Naidech AM. Ischemic brain injury after intracerebral hemorrhage: a critical review. Stroke. 2012;43(8):2258–63.
Bosarge PL, Kerby JD. Stress-induced hyperglycemia: is it harmful following trauma? Adv Surg. 2013;47:287–97.
McCowen KC, Malhotra A, Bistrian BR. Stress-induced hyperglycemia. Crit Care Clin. 2001;17(1):107–24.
Feibel JH, Hardy PM, Campbell RG, Goldstein MN, Joynt RJ. Prognostic value of the stress response following stroke. JAMA. 1977;238(13):1374–6.
Huang YH, Chung CL, Tsai HP, et al. Hyperglycemia aggravates cerebral vasospasm after subarachnoid hemorrhage in a rat model. Neurosurgery. 2017;80(5):809–15.
Ago T, Matsuo R, Hata J, et al. Insulin resistance and clinical outcomes after acute ischemic stroke. Neurology. 2018;90(17):e1470–7.
Dungan KM, Braithwaite SS, Preiser JC. Stress hyperglycaemia. Lancet. 2009;373(9677):1798–807.
Kosiborod M. Blood glucose and its prognostic implications in patients hospitalised with acute myocardial infarction. Diab Vasc Dis Res. 2008;5(4):269–75.
Wu TY, Putaala J, Sharma G, et al. Persistent hyperglycemia is associated with increased mortality after intracerebral hemorrhage. J Am Heart Assoc. 2017;6(8):e005760.
Acknowledgements
Dr. Ye, Dr. Cai, Dr. Nie, Dr. Chen, Dr. Li, Dr. Xu, Dr. Cai, Dr. Liu, Dr. Yin, Dr. Song, Dr. Tong and Dr. Gao report grants from National Natural Science Foundation of China, grants from Zhejiang Provincial Natural Science Foundation of China, grants from Zhejiang Provincial Science and Technology Project, during the conduct of the study.
Funding
This work was supported by grants from National Natural Science Foundation of China (NSFC) (81471168) to Feng Gao, National Natural Science Foundation of China (NSFC) (81500991) to Lu-sha Tong, Zhejiang Provincial Natural Science Foundation of China (LY17H090003) to Zhi-rong Liu, Zhejiang Provincial Natural Science Foundation of China (LY18H090003) to Xin-zhen Yin, and Zhejiang Provincial Science and Technology Project (2016C37128) to Xue-li Cai.
Author information
Authors and Affiliations
Contributions
X-hY brought up the main idea, developed the protocol, collected and analyzed data, and wrote the manuscript. X-lC developed the protocol, collected part of the data, searched for literatures, and offered some helpful suggestions. D-lN helped developing protocol, found some useful papers and provided helpful input on the theme. Y-jC collected part of the data and searched for useful papers. J-wL and X-hX helped to build the idea and collected part of the data. J-sC helped to read the images. Z-rL, X-zY, and S-jS offered available suggestions to write the manuscript. FG and L-sT supervised and offered guidance to all the authors, revised the manuscript, and polished the language.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The work was approved by the institutional Human Research Ethics Committee of the Second Affiliated Hospital of Zhejiang University.
Informed Consent
Informed consents were obtained from patients or their healthcare proxies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ye, Xh., Cai, Xl., Nie, Dl. et al. Stress-Induced Hyperglycemia and Remote Diffusion-Weighted Imaging Lesions in Primary Intracerebral Hemorrhage. Neurocrit Care 32, 427–436 (2020). https://doi.org/10.1007/s12028-019-00747-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00747-y