Abstract
This review will summarize artificial intelligence developments in acute ischemic stroke in recent years and forecasts for the future. Stroke is a major healthcare concern due to its effects on the patient’s quality of life and its dependence on the timing of the identification as well as the treatment. In recent years, attention increased on the use of artificial intelligence (AI) systems to help categorize, prognosis, and to channel these patients toward the right therapeutic procedure. Machine learning (ML) and in particular deep learning (DL) systems using convoluted neural networks (CNN) are becoming increasingly popular. Various studies over the years evaluated the use of these methods of analysis and prediction in the assessment of stroke patients, and at the same time, several applications and software have been developed to support the neuroradiologists and the stroke team to improve patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
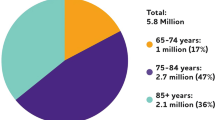
Stroke is a common cause of morbidity and mortality around the world. Between 1990 and 2019, the burden (measured in terms of the total number of cases) increased significantly (incident strokes increased by 70.0% and stroke deaths increased by 43.0%). One in four people over the age of 25 will experience a stroke in their lifetime, and there are over 12.2 million new cases of stroke each year worldwide. The most prevalent type of stroke, the ischemic subtype (AIS), accounts for more than 62% of all occurrences worldwide [1]. The first diagnostic test performed when a stroke is suspected is a CT scan without contrast medium (NCCT), which enables us to detect intracerebral hemorrhage (ICH) and assess parenchymal ischemia symptoms like decreased differentiation between white and gray matter [2]. Quantifying ischemic damage and determining whether a patient is a candidate for treatment are made possible by the Alberta stroke program early CT score (ASPECTS) [3]. The detection of a large vessel occlusion (LVO) and evaluation of collateral vessels are both possible with CT angiography (CTA). We can create time density curves for each voxel in perfusion CT by measuring the density change brought on by the arrival of contrast medium over time. From these curves, we can derive parameters like cerebral blood volume (CBV), cerebral blood flow (CBF), and time to peak (TTP). We can evaluate the mismatch between the penumbra and necrotic core using these parameters [2]. Diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) on MRI are the imaging modalities with the highest sensitivity for detecting cerebral ischemia, with 73–92% sensitivity in the first 3 h and 95–100% sensitivity in the first 6 h, respectively. In situations where the time of stroke onset is unknown, such as in wake-up strokes, FLAIR/T2 weighted imaging can also offer crucial information, such as the time of occlusion. Similar to CTA, MR angiography (MRA) can detect the presence of vessel occlusion; MRA has a sensitivity of 87% and a specificity of 98% compared to CTA’s maximum sensitivity and specificity of 98% [4].
Artificial intelligence (AI) describes the creation of computer systems that can carry out tasks that would typically require human intelligence. In machine learning (ML), a branch of artificial intelligence, computer systems get smarter over time. ML algorithms can be categorized into three groups: reinforcement learning, unsupervised learning, and both. A subtype of machine learning (ML) known as neural networks imitates neurons by having layers made up of nodes. The first layer in a neural network is the input layer, followed by a variable number of hidden layers and one output layer. An artificial neural network (ANN) uses a set of parameters called weights that represent the connections between the neurons to determine how strong the connections are [5]. Backpropagation, a technique used in training, involves adjusting the weights to reduce the discrepancy between the output and the predicted output [6]. The weights are calibrated to minimize the cost function during backpropagation, which compares the output with the “ground truth” in order to determine how far off the model is. In an ANN, which can be constructed as a CNN or a recurrent neural network pattern (RNN), DL is composed of numerous hidden layers. Because it is computationally expensive to have weights connecting every neuron, CNN applies a small “kernel” or “filter” of weights at each position in the image, sliding through the image to determine the value of the neuron of the next layer.
Different kernels can be used for each layer, resulting in multiple “channels” in each layer and assisting the model in detecting features like edges and textures in our datasets. Before the output layer, the CNN layers can be connected to “fully connected” neurons, and the various kernels and weights can be adjusted using backpropagation [7].
Over the years, maximum likelihood estimation and the Bayesian method have become popular statistical tools applied to machine learning for output validation. The asymptotic properties of both statistical methods are one of the main reasons that have increased their popularity in recent years. The difference between these two approaches is that the parameters for maximum likelihood estimation are fixed but unknown, while the parameters for the Bayesian method act as random variables with known priority distributions. Usually the Bayesian method performs better than maximum likelihood estimation in machine learning [8].
In comparison to visual inspection by human experts, these models may offer a number of advantages, including speed, large-scale deployment, objective and quantitative evaluation, and the ability to spot minute voxel-level patterns. Considerations like feature selection, classifier type, and DL are crucial when using these methods for imaging.
Stroke classification
A major concern is determining the subtype of stroke. Even though AIS is the most prevalent subtype, identifying intracranial hemorrhage (ICH) is crucial. Several studies emphasized the ICH identifications [9, 10] but we would like to bring the focus of this article to AIS. Distinguishing the subtype of AIS turns out to be particularly challenging, in contrast to hemorrhagic stroke. Garg et al. analyzed a group of cases and established stroke subtype categorization at admission using the Trial of Org 10,172 in acute stroke treatment (TOAST) classification system using electronic health records (EHRs) and ML algorithms for natural language processing. This classification separates ischemic stroke into five different subtypes: great artery atherosclerosis, cardio-embolic small vessel occlusion, other determined etiology stroke, and stroke with unknown etiology [11]. The concordance index kappa was the highest for the cardio-embolic subtype and lowest for the cryptogenic subtype [6, 12, 13].
Perinatal and pediatric stroke
Perinatal stroke comprises a specific group of cerebrovascular diseases that occur between 20 weeks of fetal life and 28 days postnatal life [14]. The estimated incidence is between 1:1600 and 1:3000 live births [15]. Stroke etiology is frequently poorly understood. By identifying specific prenatal stroke disease states, neuroimaging developments have aided clinical care and research growth. Neonatal periventricular venous infarction (PVI), neonatal arterial ischemia, neonatal cerebral sinus-venous thrombosis, neonatal hemorrhagic stroke, arterial presumed perinatal stroke, and presumed perinatal hemorrhagic stroke are the six distinct neonatal stroke disorders that can be distinguished based on clinical signs and neuroimaging. Hemiparetic cerebral palsy, also known as periventricular venous infarction, is primarily characterized by motor impairment. Large lesions, along with both motor and non-motor morbidities, are frequently brought on by arterial ischemic strokes in the near future [16]. About 90% of published cases are arterial ischemic variety [17]. Diffusion MRI is the gold standard for diagnosis [18]. The treatment is still debated and in most cases off-label. Anticoagulation is considered safe in pediatric patients [19], but studies focused on anticoagulation for neonatal arterial ischemic stroke are scarce. The use of steroids remains controversial but should be considered when there is evidence of arteriopathy. Acute therapy focuses on neuroprotection. Emergency recanalization strategies are precluded, because precise timing can never be known, the infarct is typically well established, and the affected artery is often open [20]. Supportive care is provided along with anti-seizure medication [21]. Stroke also affects infants (as previously described) and children. The incidence of childhood stroke has varied widely in the literature. The incidence of strokes in children ranges between 2.5 and 13:100,000 per year [22]. Stroke has a high rate of morbidity and mortality, even among children. Since it occurs at a young age and the duration of disability is longer, even lasting a lifetime. Additionally, there are significant diagnostic delays in children [23]. Pediatric strokes are linked to many diseases [24]. The most significant risk factors for stroke in children are coagulopathies, infections, vascular diseases, and cardiac causes. Head injury, autoimmune diseases, metabolic issues, child maltreatment, renal diseases, and hematological illnesses are additional risk factors [25]. Treatment for pediatric acute strokes is time-sensitive. Immediate mechanical thrombectomy or intravenous tissue plasminogen activator (tPA) therapy for children resulted in better functional and mortality outcomes. The earlier treatment begins, the greater the chance of maintaining the penumbra, restoring cerebral blood flow, and perhaps even curing the symptoms, which lessens disability. Early detection is essential for better patient care due to the narrow treatment window. It improves hospital care and lessens the chance of a stroke recurrence before recovery. Despite the lack of data and extensive randomized clinical trials, mechanical thrombectomy and intravenous tPA have both been used successfully in pediatrics [26,27,28].
To our knowledge, few authors have investigated the application of ML in the context of pediatric stroke; however, Carlson et al. [29]’s interesting work, which used an RF model to identify which factors might be more predictive of motor outcome in a group of 49 patients with a history of perinatal stroke (AIS and PVI), is worth mentioning. Their model included demographic information along with variables from neuroimaging using conventional MRI sequences and cutting-edge research like white matter tractography and functional MRI. A validated bimanual test known as the Assisting Hand Assessment (AHA) and a bimanual test known as the Box and Blocks Test (BBT), which was divided into two scores: one for the stroke-affected hand (BBTA) and one for the other side (BBTU), were used to assess the motor function. Twenty-seven volunteers who were roughly the same age as the comparison group made up the control group. The RRELIEFF algorithm was used to rank the features, and the RF model was then applied to model the regression for each motor outcome score.
Their research indicated that many features, including connectivity between bilateral primary motor, sensory, and supplementary areas, inter-hemispheric connectivity within the deep nuclei, and connectivity within the lesioned corticospinal tract, had lower functional and structural connectivity in children with a history of AIS. With differences in the lesioned CST and inter-hemispheric connection within the basal ganglia, it was discovered that children with a history of PVI were more similar to the control group. Enhancing our knowledge of neuroplasticity and brain remodeling after an event like a stroke may be fascinating in the future in order to create rehabilitation programs with even better results.
The use of AI software in pediatric stroke management would be desirable to optimize the management of perinatal and pediatric stroke. Even today, it seems off-label to use such software. In addition, given the pathologic variations, it would be preferable to support studies that advance knowledge of the appropriate diagnostic-therapeutic management of perinatal and pediatric stroke. To this end, it would be appropriate to start machine learning processes in order to get outcomes for adult stroke similar to those we describe below.
Early diagnose
ASPECTS, LVOs detection, segmentation of the necrotic core and the penumbra, and diagnosis timing all play significant roles in AIS. Numerous AI programs have been created to aid in diagnosis, and numerous studies have examined how they affect ASPECTS scoring. In the event of a middle cerebral artery (MCA) occlusion, ASPECTS is a quick method to evaluate the severity of the AIS. ASPECTS has high sensitivity and specificity for both functional outcome and intracerebral hemorrhage in thrombolytic therapy, deducting one point from a value of 10 for each MCA territory involved [3]. Correct scoring is crucial when determining thrombectomy eligibility. Using RAPID software, Maegerlein et al. assessed the agreement between the ASPECTS of two seasoned neuroradiologists. Consensus readings were determined using imaging data from the baseline and follow-up CT scans conducted after six weeks. The software analysis revealed optimal agreement (κ ≈ 0.9), whereas the neuroradiologists’ consensus agreement was only moderate (κ ≈ 0.56); the neuroradiologists’ consensus agreement became comparable to the software after the 4 h time period from onset [30].
Sundaram et al. conducted a comparative analysis of concurrent CBV ASPECTS based on CTP and evaluated ASPECTS by Brainomix against a neuroradiologist assessment. Automated scores were comparable to consensus readings and CTP-CBV ASPECTS when they were grouped by the time from symptom onset (> 6 or 6 h); automated scores agreed with consensus readings and CTP-CBV ASPECTS (κ ≈ 0.84) [31]. Albers et al. compared the ASPECTS and RAPID scores of four expert readers with diffusion-weighted imaging (DWI) results obtained following baseline CT; RAPID outperformed physicians in spotting early signs of cerebral ischemia identified by subsequent DWI [32].
Seker et al. investigated the consistency of the brainomix e-Aspects and the ASPECTS of two residents and two consultants. In contrast to the software, the residents displayed significant variation and lower internal concordance. However, the consultant and software scores were comparable [33].
In 214 patients undergoing EVT, Olive-Gadea et al. looked at the relationship between radiologist and e-ASPECTS scores and the infarct core CBV and infarct end-tidal volume as well as the long-term functional outcome. ASPECTS score was determined by a radiologist (Rx-ASPECTS) during acute stroke assessment and by Brainomix software (e-Aspects), while images were sent to RAPID software to quantify the ischemic core. The distribution of ASPECTS scores was similar according to their study. A mild and time-dependent correlation between ASPECTS and e-ASPECTS and CBV was found, with the best correlation occurring 180 min after the onset of symptoms. Only Rx-ASPECTS and e-ASPECTS were predictors of a good functional outcome, but CBV and e-ASPECTS predicted infarct volume after thrombectomy in a similar manner [34].
Chriashkova et al. looked at how well e-ASPECTS improved concordance with the ASPECTS reference standard and sped up the time it took to evaluate CT scans. Twenty-six clinicians with various levels of experience participated in the study. When using e-Aspects, the average time to score was reduced by 34%. All groups of clinicians who used e-ASPECTS assistance saw a twofold increase in their sensitivity to early ischemic changes, with the effects being more pronounced for less experienced clinicians [35]. The detection of LVOs has been the subject of other studies. In a cohort of 223 patients, Chung et al.’s CNN model for detecting the “hyperdense vessel sign” in the middle cerebral artery on NCCT, which is typically associated with an LVO, achieved 96% specificity [6, 36].
In a cohort of adult AIS patients with and without LVO, Barreira et al. compared the findings of a skilled neuroradiologist using CTA scans to those from Viz.ai software. The performance of Viz.ai for proximal intracranial LVOs was remarkably good [37]. For the purpose of detecting LVO in the acute setting, You et al. combined structured clinical data with unstructured CT imaging data; the evaluation system in their study contained three hierarchical models. Structured demographic and clinical data were used in the modeling’s first two levels, and a DL model’s additional CT imaging features were used in the third level. The third level of evaluation with the clinical and imaging features produced the best model performance on the test group; the accuracy, sensitivity, and area under the curve (AUC) were greater than 0.80 [38].
Tissue outcome
To decide which patients would benefit from thrombolysis or another attempt in the event of partial recanalization, it is essential to predict final infarct volumes. To predict final infarct volume directly from native CTP images and metadata like time parameters and treatment, Robben et al. used a deep neural network. They forecasted the hypothetical final infarct volume for each test subject in the scenarios of early complete recanalization (mTICI 3 at 60 min) and in the absence of recanalization. With a mean volume error of 2.8 ml and a mean absolute volume error of 36.7 ml, the results were satisfactory [39].
By using pseudo-continuous arterial spin labeling (pCASL), Wang et al. created and assessed a DL-based algorithm to help identify AIS patients who would benefit from endovascular therapy. The outcomes showed that the algorithm had a 92% accuracy rate and a 0.94 AUC [40].
To forecast the tissue result Nielsen et al. trained a deep CNN (CNNdeep) that outperformed competing approaches and was remarkably consistent with the final result as determined by T2-FLAIR measurements. They also developed CNNdeep,rtpa, which was used to assess patients who had received intravenous rtPA. The AUC for patients who had received intravenous rtPA evaluated with CNNdeep,rtPA was 0.85 ± 0.15 [41].
Without knowing the status of reperfusion, Yu et al. used a DL model trained with acute and follow-up image collection to predict the size and location of infarct lesions at 3–to 7 days after baseline. Three to seven days after the baseline, infarct lesions could be accurately predicted by their model. Comparable performance was shown by the model in patients with and without reperfusion [42].
Clinical outcome
Several studies looked into the use of AI to forecast stroke patients’ outcomes. Extreme gradient boosting and gradient boosting machine, which are decision tree-based algorithms, were used by Xie et al. to predict the 90 day modified Rankin scale (mRS) > 2 with AUCs greater than 0.745; performance improved when the National Institutes of health stroke scale (NIHSS) at 24 h and recanalization outcomes were taken into account [43, 44].
Bacchi et al. investigated the use of DL algorithms in predicting outcomes in patients who received r-TPA; a positive outcome was defined as the outcome of mRS 0–1 at 90 days (vs ≥ 2) (“mRS90”), or NIHSS improvement by ≥ 4 points at 24-h (NIHSS24). An AUC of 0.75 for the prediction of mRS90 and 0.70 for the prediction of NIHSS24 were obtained using CNN + ANN [45].
To identify patients who would benefit from thrombectomy and forecast both immediate and long-term clinical/functional outcomes, Tang et al. built ML logistic regression models. The mRS was used to evaluate clinical outcomes at 7 and 90 days, respectively. They combined early clinical data with the initial preprocedural diffusion and perfusion-weighted MRI datasets to create a combined model. This model was contrasted with two others that utilized clinical data alone and clinical data along with penumbra (mismatch) data. Their combined model was the most accurate at forecasting both short- and long-term clinical outcomes, with an AUC of 0.863 [6, 46].
In order to predict outcome measures (mRS ≤ 2 at 90 days) and good reperfusion (mTICI ≥ 2b), Hilbert et al. used DL techniques trained on CTA data. For this purpose, a number of artificial intelligence techniques were evaluated. The findings revealed that automated radiological image analysis using data-efficient DL methods outperformed the combination of multiple radiological image biomarkers for the prediction of a favorable stroke outcome. For functional outcome and reperfusion, DL models outperformed models using conventional radiological image biomarkers [47].
The accuracy of an algorithm based on functional imaging to predict deficits in various areas, including attention, visual memory, verbal memory, language, motor, and visual, was tested by Siegel et al. Lesion location performed better than functional connectivity in predicting verbal and visual memory deficits, while functional connectivity performed better than lesion location in predicting visual and motor deficits [48, 49].
A regression tree model was created by Alawieh et al. to predict mRS scores after 90 days in patients receiving ET. With a 0.952 AUC, the model successfully predicted the functional independence rates at 90 days with 89.36% sensitivity and 89.66% specificity. The outcomes far outperformed those of the NIHSS and the ASPECTS [50].
Hofmeister et al. demonstrated that a small subset of nine radiomic features was predictive of the success of first-attempt recanalization with thromboaspiration (AUC = 0.88); 4/9 radiomic features were positively associated with first-attempt recanalization after thromboaspiration (P < 0.05), including large area low gray level emphasis, gray level variance, large dependence emphasis, and short run emphasis; the other 5 were negatively associated (P < 0.05): entropy, maximum, run percentage, coarseness, and gray level nonuniformity normalized; additionally, it was demonstrated in their study that characteristics like higher HU values, texture randomness, coarseness, and clot heterogeneity were associated negatively with rapid recanalization [51]. The effectiveness of Diffusion Tensor Imaging (DTI) in predicting clinical outcomes has been examined in some studies. The functional outcome was evaluated at 3 months and was divided into two categories: good outcome (mRS ≤ 2) and poor outcome (mRS > 2). Moulton et al. retrospectively evaluated patients with AIS who received thrombolysis within 4.5 h of stroke onset and who underwent a DTI sequence at 24 h after stroke. The second and third branches of the superior longitudinal fasciculus (SLF), the corpus callosum, the corticospinal tract, the long, anterior, and posterior segments of the arcuate fasciculus (AF), and the frontal aslant tract were the regions that had the greatest influence on functional outcome [52, 53].
In other studies, the prognostic value of functional magnetic resonance imaging (fMRI) was examined to predict clinical outcomes in stroke patients at 4–6 months; 86% of patients had outcomes that their model correctly predicted [53, 54].
Stroke complications
The ability to predict complications can have a big clinical impact. To predict cerebral edema, changes in cerebrospinal fluid (CSF) dynamics were taken advantage of. 155 stroke patients’ CSF volumes, as determined by serial CT imaging, were examined using a random forest model. They proposed that variations in CSF volume over time might serve as a quantitative indicator of edema development. In addition, a correlation between infarct volume and the decrease in CSF volume between baseline and final CT was found (R = 0.715) [55].
Hemorrhagic transformation should also be taken into account or predicted as a complication. Yu et al. used a variety of DL and ML models, using follow-up gradient echo MRI performed at 24 h in comparison to diffusion- and perfusion-weighted MRI as the ground truth for the hemorrhage. The most accurate (84%) model was their kernel spectral regression model [56]. With the aid of a surface neural network, Wang et al. were able to predict intracranial hemorrhage (ICH) in AIS patients receiving thrombolysis with an AUC of 0.82. Age, sex, baseline NIHSS data, admission blood pressure and glucose, prior medical history, and smoking status were all taken into account; about 50% of patients were categorized as low-risk, and none of them experienced ICH in the prospective cohort [57, 58].
Main available software
In this Table 1, the main available software and their application were summarized.
Comparison between software
It is demonstrated that the performance of Brainomix’s e-ASPECTS is superior to or on par with that of humans (Fig. 1). Rapid similarly scores the ASPECTS, identifies LVOs, and assesses collaterals by examining the asymmetry of the contrasted vessels. e-CTA software provides a quick assessment of LVOs and performs a collaterals estimation. Additionally, RAPID automates the assessment of stroke patients’ suitability for thrombectomy (Fig. 2). Each program has the capacity to produce data, including CT and MR perfusion maps [59].
Hoelter et al. found high correlation between Brainomix and RAPID median ASPECTS: r = 0.835 (0.512, 0.923), P < 0.001. While there are some differences, such as automatic motion correction capabilities and the automatic activation of the stroke team, Viz.ai shares some characteristics with the software mentioned above (Fig. 3) [59, 60].
Potential and limits
AI has demonstrated a positive effect on stroke by making components like ASPECTS immediate and immune to inter-individual variation. An intriguing aspect of clinical practice is that helping neuroradiologists by performing a preliminary image analysis has the same overall impact as what the residents do for the signatory physician’s medical doctor—a reduction in the time between diagnosis and treatment. Limitations like false positives demonstrate the importance of the neuroradiologist’s assessment for accurate diagnosis. Other drawbacks might include the fact that the ML algorithm does not perform as well in patients with strokes who have abnormal brain features, as demonstrated by Gueberina et al. [61, 62].
The development of software that can automatically detect and/or segment the thrombus after it has been highlighted must take into account the possibility that in clinical practice the cohort of patients to whom this program would then be applied may present some discrepant characteristics with respect to the study group. For example, the developers must take into account the presence of calcifications, moveable thrombi, and other factors before considering using the programs in a commercial setting [63].
Ethical and legal issues
There are some medico-legal issues that cannot be disregarded when it comes to the use of AI in the medical and, in this case, radiological fields. There are numerous issues with deciding which AI algorithms or medical devices to approve for use in the U.S. and Europe, particularly for those that might not require human intervention. The majority of advancements in this area focus on developing tools that can support physicians rather than replace them [64]. Liability is still up for debate in the event that AI software causes a medical error. Currently, it is the physician’s responsibility to ensure that the algorithm’s output complies with diagnostic standards [53].
Economic impact
Due to the severe impairment it causes, stroke has a significant financial impact on the healthcare systems. Each minute of thrombectomy delay results in roughly a 4-day loss of disability-free life, according to the study Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials (HERMES) [65].
The average cost of thrombectomy delay is roughly $1059 per minute; if 10 min could be avoided on average in the USA, this would result in an annual savings of $249 million [66]. The great benefit of available software is that it ensures the least amount of time is spent on patient management. Hassan et al. compared transfer times before and after the implementation of the Viz.ai system for all LVO patients who were transferred from the spoke (PSC) to their hub center (HC). The median transfer times from the PSC to the HC were cut in half by 22.5 min, and from the CTA to the PSC to the puncture to the HC were cut in half by 89 min [67]. Reducing time from diagnosis to treatment has a profound effect on the amount of money saved each year.
Current state of AI software in AIS and future directions
As was already mentioned, current commercial software focuses on the detection of AIS and estimation of the key characteristics that are essential to understand during the emergency phase, such as collaterals, ASPECT, and perfusion parameters [30,31,32,33,34,35].
Future scientific research, however, is moving in a direction that includes the study of additional elements that could soon be used in clinical practice, such as, for example, the use of radiomics and advanced imaging parameters for the correlation with the patient’s long-term deficit; this scenario opens up new possibilities for the application of therapeutic pathways in the context of a personalized medicine [51].
Conclusion
As was already mentioned, current commercial software focuses on the detection of AIS and estimation of the key characteristics that are essential to understand during the emergency phase, such as collaterals, ASPECT, and perfusion parameters. Future scientific research, however, is moving in a direction that includes the study of additional elements that could soon be used in clinical practice, such as, for example, the use of radiomics and advanced imaging parameters for the correlation with the patient’s long-term deficit; this scenario opens up new possibilities for the application of therapeutic pathways in the context of a personalized medicine. AI will undoubtedly take up more and more space in both research and hospitals.
References
Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W et al (2022) World stroke organization (WSO): global stroke fact sheet 2022. Int J Stroke Off J Int Stroke Soc 17(1):18–29. https://doi.org/10.1177/17474930211065917
Wannamaker R, Buck B, Butcher K (2019) Multimodal CT in acute stroke. Curr Neurol Neurosci Rep 19:1–13
Barber PA, Demchuk AM, Zhang J, Buchan AM (2000) Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS study group. Alberta stroke programme early CT score. Lancet (London, England) 355(9216):1670–1674. https://doi.org/10.1016/s0140-6736(00)02237-6
Vilela P, Rowley HA (2017) Brain ischemia: CT and MRI techniques in acute ischemic stroke. Eur J Radiol 96:162–172
Lee EJ, Kim YH, Kim N, Kang DW (2017) Deep into the brain: artificial intelligence in stroke imaging. J Stroke 19(3):277–285. https://doi.org/10.5853/jos.2017.02054
Yedavalli VS, Tong E, Martin D, Yeom KW, Forkert ND (2021) Artificial intelligence in stroke imaging: current and future perspectives. Clin Imaging 69:246–254. https://doi.org/10.1016/j.clinimag.2020.09.005
Zaharchuk G, Gong E, Wintermark M, Rubin D, Langlotz CP (2018) Deep learning in neuroradiology. AJNR Am J Neuroradiol 39(10):1776–1784. https://doi.org/10.3174/ajnr.A5543
Kim C, Zhu V, Obeid J, Lenert L (2019) Natural language processing and machine learning algorithm to identify brain MRI reports with acute ischemic stroke. PLoS ONE 14(2):e0212778. https://doi.org/10.1371/journal.pone.0212778
Chilamkurthy S, Ghosh R, Tanamala S, Biviji M, Campeau NG, Venugopal VK et al (2018) Deep learning algorithms for detection of critical findings in head CT scans: a retrospective study. Lancet 392(10162):2388–2396
Arbabshirani MR, Fornwalt BK, Mongelluzzo GJ, Suever JD, Geise BD, Patel AA et al (2018) Advanced machine learning in action: identification of intracranial hemorrhage on computed tomography scans of the head with clinical workflow integration. NPJ Digit Med 1:9. https://doi.org/10.1038/s41746-017-0015-z
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke 24(1):35–41. https://doi.org/10.1161/01.str.24.1.35
Garg R, Oh E, Naidech A, Kording K, Prabhakaran S (2019) Automating ischemic stroke subtype classification using machine learning and natural language processing. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc 28(7):2045–2051. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.02.004
Shlobin NA, Baig AA, Waqas M, Patel TR, Dossani RH, Wilson M et al (2022) Artificial intelligence for large-vessel occlusion stroke: a systematic review. World Neurosurg 159:207-220.e1. https://doi.org/10.1016/j.wneu.2021.12.004
Raju TN, Nelson KB, Ferriero D, Lynch JK, NICHD-NINDS Perinatal Stroke Workshop Participants (2007) Ischemic perinatal stroke: summary of a workshop sponsored by the National Institute of child health and human development and the National Institute of neurological disorders and stroke. Pediatrics 120(3):609–616. https://doi.org/10.1542/peds.2007-0336
Laugesaar R, Kolk A, Tomberg T, Metsvaht T, Lintrop M, Varendi H et al (2007) Acutely and retrospectively diagnosed perinatal stroke: a population-based study. Stroke 38(8):2234–2240. https://doi.org/10.1161/STROKEAHA.107.483743
Dunbar M, Kirton A (2018) Perinatal stroke: mechanisms, management, and outcomes of early cerebrovascular brain injury. Lancet Child Adolesc Health 2(9):666–676
Benders MJ, Groenendaal F, Uiterwaal CS, de Vries LS (2008) Perinatal arterial stroke in the preterm infant. Semin Perinatol 32(5):344–349. https://doi.org/10.1053/j.semperi.2008.07.003
Siddiq I, Armstrong D, Surmava AM, Dlamini N, MacGregor D, Moharir M et al (2017) Utility of neurovascular imaging in acute neonatal arterial ischemic stroke. J Pediatr 188:110–114. https://doi.org/10.1016/j.jpeds.2017.05.046
Boelman C, Shroff M, Yau I, Bjornson B, Richrdson S, deVeber G et al (2014) Antithrombotic therapy for secondary stroke prevention in bacterial meningitis in children. J Pediatr 165(4):799–806. https://doi.org/10.1016/j.jpeds.2014.06.013
Monagle P, Chan AKC, Goldenberg NA, Ichord RN, Journeycake JM, Nowak-Göttl U, et al. (2012) Antithrombotic therapy in neonates and children: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of chest physicians evidence-based clinical practice guidelines. Chest, 141(2 Suppl), e737S–e801S. https://doi.org/10.1378/chest.11-2308
Shellhaas RA, Chang T, Wusthoff CJ, Soul JS, Massey SL, Chu CJ et al (2017) Treatment duration after acute symptomatic seizures in neonates: a multicenter cohort study. J Pediatr 181:298-301.e1. https://doi.org/10.1016/j.jpeds.2016.10.039
Kupferman JC, Zafeiriou DI, Lande MB, Kirkham FJ, Pavlakis SG (2017) Stroke and hypertension in children and adolescents. J Child Neurol 32(4):408–417. https://doi.org/10.1177/0883073816685240
Hollist M, Au K, Morgan L, Shetty PA, Rane R, Hollist A et al (2021) Pediatric stroke: overview and recent updates. Aging Dis 12(4):1043–1055. https://doi.org/10.14336/AD.2021.0219
Chiang KL, Cheng C-Y (2018) Epidemiology, risk factors and characteristics of pediatric stroke: a nationwide population-based study. QJM Int J Med 111(7):445–454
Riela AR, Steven Roach E (1993) Topical review article: etiology of stroke in children. J Child Neurol 8(3):201–220
Rivkin MJ, deVeber G, Ichord RN, Kirton A, Chan AK, Hovinga CA et al (2015) Thrombolysis in pediatric stroke study. Stroke 46(3):880–885. https://doi.org/10.1161/STROKEAHA.114.008210
Tabone L, Mediamolle N, Bellesme C, Lesage F, Grevent D, Ozanne A et al (2017) Regional pediatric acute stroke protocol: initial experience during 3 years and 13 recanalization treatments in children. Stroke 48(8):2278–2281. https://doi.org/10.1161/STROKEAHA.117.016591
Fragata I, Morais T, Silva R, Nunes AP, Loureiro P, Diogo Martins J et al (2021) Endovascular treatment of pediatric ischemic stroke: a single center experience and review of the literature. Interv Neuroradiol J Perither Neuroradiol Surg Proced Relat Neurosci 27(1):16–24. https://doi.org/10.1177/1591019920958827
Carlson HL, Craig BT, Hilderley AJ, Hodge J, Rajashekar D, Mouches P, Forkert ND, Kirton A (2020) Structural and functional connectivity of motor circuits after perinatal stroke: a machine learning study. NeuroImage Clinical 28:102508. https://doi.org/10.1016/j.nicl.2020.102508
Maegerlein C, Fischer J, Mönch S, Berndt M, Wunderlich S, Seifert CL et al (2019) Automated calculation of the Alberta stroke program early CT score: feasibility and reliability. Radiology 291(1):141–148. https://doi.org/10.1148/radiol.2019181228
Sundaram VK, Goldstein J, Wheelwright D, Aggarwal A, Pawha PS, Doshi A et al (2019) Automated ASPECTS in acute ischemic stroke: a comparative analysis with CT perfusion. AJNR Am J Neuroradiol 40(12):2033–2038. https://doi.org/10.3174/ajnr.A6303
Albers GW, Wald MJ, Mlynash M, Endres J, Bammer R, Straka M et al (2019) Automated calculation of Alberta stroke program early CT score: validation in patients with large hemispheric infarct. Stroke 50(11):3277–3279. https://doi.org/10.1161/STROKEAHA.119.026430
Seker F, Pfaff J, Nagel S, Vollherbst D, Gerry S, Möhlenbruch MA et al (2019) CT reconstruction levels affect automated and reader-based ASPECTS ratings in acute ischemic stroke. J Neuroimaging Off J Am Soc Neuroimaging 29(1):62–64. https://doi.org/10.1111/jon.12562
Olive-Gadea M, Martins N, Boned S, Carvajal J, Moreno MJ, Muchada M et al (2019) Baseline ASPECTS and e-ASPECTS correlation with infarct volume and functional outcome in patients undergoing mechanical thrombectomy. J Neuroimaging Off J Am Soc Neuroimaging 29(2):198–202. https://doi.org/10.1111/jon.12564
Chriashkova J, Menon N, Chakrabarti A, Guyler P, Kelavkar S, Kuhn A et al (2019) Abstract WMP14: e-ASPECTS improves sensitivity to early ischemic injury on acute computed tomography scans. Stroke 50(Suppl_1):AWMP14
Chung CY, Rodrigues GM, Haussen DC, Barreira CM, Grossberg J, Frankel MR et al (2019) Abstract WP76: automated detection of hyperdense MCA sign and automated notification of large vessel occlusion using artificial intelligence. Stroke 50(Suppl_1):AWP76
Barreira CM, Bouslama M, Haussen DC, Grossberg JA, Baxter B, Devlin T et al (2018) Abstract WP61: automated large artery occlusion detection IN stroke imaging-ALADIN study. Stroke 49(Suppl_1):AWP61
You J, Tsang AC, Yu PL, Tsui EL, Woo PP, Lui CS et al (2020) Automated hierarchy evaluation system of large vessel occlusion in acute ischemia stroke. Front Neuroinform 14:13
Robben D, Boers AM, Marquering HA, Langezaal LL, Roos YB, van Oostenbrugge RJ et al (2020) Prediction of final infarct volume from native CT perfusion and treatment parameters using deep learning. Med Image Anal 59:101589
Wang K, Shou Q, Ma SJ, Liebeskind D, Qiao XJ, Saver J et al (2020) Deep learning detection of penumbral tissue on arterial spin labeling in stroke. Stroke 51(2):489–497
Nielsen A, Hansen MB, Tietze A, Mouridsen K (2018) Prediction of tissue outcome and assessment of treatment effect in acute ischemic stroke using deep learning. Stroke 49(6):1394–1401
Yu Y, Xie Y, Thamm T, Gong E, Ouyang J, Huang C et al (2020) Use of deep learning to predict final ischemic stroke lesions from initial magnetic resonance imaging. JAMA Netw Open 3(3):e200772–e200772
Xie Y, Jiang B, Gong E, Li Y, Zhu G, Michel P et al (2019) Use of gradient boosting machine learning to predict patient outcome in acute ischemic stroke on the basis of imaging, demographic, and clinical information. Am J Roentgenol 212(1):44–51
Soun JE, Chow DS, Nagamine M, Takhtawala RS, Filippi CG, Yu W et al (2021) Artificial intelligence and acute stroke imaging. Am J Neuroradiol 42(1):2–11
Bacchi S, Zerner T, Oakden-Rayner L, Kleinig T, Patel S, Jannes J (2020) Deep learning in the prediction of ischaemic stroke thrombolysis functional outcomes: a pilot study. Acad Radiol 27(2):e19–e23
Tang TY, Jiao Y, Cui Y, Zeng CH, Zhao DL, Zhang Y et al (2018) Development and validation of a penumbra-based predictive model for thrombolysis outcome in acute ischemic stroke patients. EBioMedicine 35:251–259
Hilbert A, Ramos LA, van Os HJ, Olabarriaga SD, Tolhuisen ML, Wermer MJ et al (2019) Data-efficient deep learning of radiological image data for outcome prediction after endovascular treatment of patients with acute ischemic stroke. Comput Biol Med 115:103516
Siegel JS, Ramsey LE, Snyder AZ, Metcalf NV, Chacko RV, Weinberger K et al (2016) Disruptions of network connectivity predict impairment in multiple behavioral domains after stroke. Proc Natl Acad Sci 113(30):E4367–E4376
Shafaat O, Bernstock JD, Shafaat A, Yedavalli VS, Elsayed G, Gupta S (2022) Leveraging artificial intelligence in ischemic stroke imaging. J Neuroradiol 49(4):343–351
Alawieh A, Zaraket F, Alawieh MB, Chatterjee AR, Spiotta A (2019) Using machine learning to optimize selection of elderly patients for endovascular thrombectomy. J NeuroInterv Surg 11(8):847–851
Hofmeister J, Bernava G, Rosi A, Vargas MI, Carrera E, Montet X et al (2020) Clot-based radiomics predict a mechanical thrombectomy strategy for successful recanalization in acute ischemic stroke. Stroke 51(8):2488–2494
Moulton E, Valabregue R, Lehéricy S, Samson Y, Rosso C (2019) Multivariate prediction of functional outcome using lesion topography characterized by acute diffusion tensor imaging. NeuroImage Clin 23:101821
Bonkhoff AK, Grefkes C (2022) Precision medicine in stroke: towards personalized outcome predictions using artificial intelligence. Brain 145(2):457–475
Rehme AK, Volz LJ, Feis DL, Eickhoff SB, Fink GR, Grefkes C (2015) Individual prediction of chronic motor outcome in the acute post-stroke stage: behavioral parameters versus functional imaging. Hum Brain Mapp 36(11):4553–4565
Dhar R, Chen Y, An H, Lee JM (2018) Application of machine learning to automated analysis of cerebral edema in large cohorts of ischemic stroke patients. Front Neurol 9:687
Yu Y, Guo D, Lou M, Liebeskind D, Scalzo F (2017) Prediction of hemorrhagic transformation severity in acute stroke from source perfusion MRI. IEEE Trans Biomed Eng 65(9):2058–2065
Wang F, Huang Y, Xia Y, Zhang W, Fang K, Zhou X et al (2020) Personalized risk prediction of symptomatic intracerebral hemorrhage after stroke thrombolysis using a machine-learning model. Ther Adv Neurol Disord 13:1756286420902358
Yeo M, Kok HK, Kutaiba N, Maingard J, Thijs V, Tahayori B et al (2021) Artificial intelligence in clinical decision support and outcome prediction–applications in stroke. J Med Imaging Radiat Oncol 65(5):518–528
Murray NM, Unberath M, Hager GD, Hui FK (2020) Artificial intelligence to diagnose ischemic stroke and identify large vessel occlusions: a systematic review. J NeuroInterv Surg 12(2):156–164
Hoelter P, Muehlen I, Goelitz P, Beuscher V, Schwab S, Doerfler A (2020) Automated ASPECT scoring in acute ischemic stroke: comparison of three software tools. Neuroradiology 62:1231–1238
Guberina N, Dietrich U, Radbruch A, Goebel J, Deuschl C, Ringelstein A et al (2018) Detection of early infarction signs with machine learning-based diagnosis by means of the Alberta stroke program early CT score (ASPECTS) in the clinical routine. Neuroradiology 60:889–901
Mouridsen K, Thurner P, Zaharchuk G (2020) Artificial intelligence applications in stroke. Stroke 51(8):2573–2579
Tortora M, Pacchiano F (2023) Regarding “automated segmentation of intracranial thrombus on NCCT and CTA in patients with acute ischemic stroke using a coarse-to-fine deep learning model". AJNR Am J Neuroradiol. https://doi.org/10.3174/ajnr.A7972
Pesapane F, Volonté C, Codari M, Sardanelli F (2018) Artificial intelligence as a medical device in radiology: ethical and regulatory issues in Europe and the United States. Insights Imaging 9:745–753
Kunz WG, Hunink MG, Almekhlafi MA, Menon BK, Saver JL, Dippel DW et al (2020) Public health and cost consequences of time delays to thrombectomy for acute ischemic stroke. Neurology 95(18):e2465–e2475
Hassan AE (2021) New technology add-on payment (NTAP) for viz LVO: a win for stroke care. J Neurointerv Surg 13(5):406–408
Hassan AE, Ringheanu VM, Rabah RR, Preston L, Tekle WG, Qureshi AI (2020) Early experience utilizing artificial intelligence shows significant reduction in transfer times and length of stay in a hub and spoke model. Interv Neuroradiol 26(5):615–622
Funding
Open access funding provided by Università degli Studi di Napoli Federico II within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Ethical approval
Institutional Review Board approval was not required.
Informed consent
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pacchiano, F., Tortora, M., Criscuolo, S. et al. Artificial intelligence applied in acute ischemic stroke: from child to elderly. Radiol med 129, 83–92 (2024). https://doi.org/10.1007/s11547-023-01735-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-023-01735-1