Abstract
Background
Despite early and ongoing dietary management with a phe-restricted diet, suboptimal neuropsychological function has been observed in PKU. The restrictive nature of the PKU diet may expose patients to sub-optimal nutritional intake and deficiencies which may impact normal brain function. A systematic review of the published literature was carried out, where possible with meta-analysis, to compare the status of nutrients (Nutrients: DHA, EPA phospholipids, selenium, vitamins B6, B12, E, C, A, D, folic acid, choline, uridine, calcium, magnesium, zinc, iron, iodine and cholesterol) known to be important for brain development and functioning between individuals with PKU and healthy controls.
Results
Of 1534 publications identified, 65 studies met the entry criteria. Significantly lower levels of DHA, EPA and cholesterol were found for PKU patients compared to healthy controls. No significant differences in zinc, vitamins B12, E and D, calcium, iron and magnesium were found between PKU patients and controls. Because of considerable heterogeneity, the meta-analyses findings for folate and selenium were not reported. Due to an insufficient number of publications (< 4) no meta-analysis was undertaken for vitamins A, C and B6, choline, uridine, iodine and phospholipids.
Conclusions
The current data show that PKU patients have lower availability of DHA, EPA and cholesterol. Compliance with the phe-restricted diet including the micronutrient fortified protein substitute (PS) is essential to ensure adequate micronutrient status. Given the complexity of the diet, patients’ micronutrient and fatty acid status should be continuously monitored, with a particular focus on patients who are non-compliant or poorly compliant with their PS. Given their key role in brain function, assessment of the status of nutrients where limited data was found (e.g. choline, iodine) should be undertaken. Standardised reporting of studies in PKU would strengthen the output of meta-analysis and so better inform best practice for this rare condition.
Similar content being viewed by others
Background
Phenylketonuria (OMIM 261600) is a rare genetic disorder characterized by impaired conversion of phenylalanine (phe) to tyrosine (tyr) due to deficient activity of the hepatic enzyme L-phenylalanine-4- hydroxylase [1]. If untreated, the resulting high blood phe concentrations cross the blood brain barrier causing detrimental effects on brain development and function [2]. For the majority of patients with PKU, treatment is a phe-restricted diet that aims to prevent excessive accumulation of phe while also meeting requirements for growth and development [3]. Because of the severe restriction of many protein-containing foods, the diet requires supplementation with a phe-free protein substitute (PS) and a wide range of other nutrients including omega-3 fatty acids, vitamins, minerals and trace elements. However, nutrient intakes [4,5,6] and status [7,8,9] may be affected by factors such as poor dietary compliance, bioavailability of different nutrient sources, different management approaches in metabolic centres [2] and historical differences in the composition of the PS e.g. changes in selenium fortification practices [2, 4, 10,11,12]. Despite early and continuous low phe dietary management, PKU patients have been shown to have suboptimal neuropsychological function compared to healthy controls, in particular lower IQ, slower information processing [13, 14] and suboptimal executive functioning [15,16,17].
Tyr deficiency has been suggested as one reason for the decreased neuropsychological performance and cognitive dysfunction in PKU [18]. It has been suggested that tyr supplementation could have an important role in the treatment of PKU [19], however blood tyr concentrations do not correlate with cognitive outcomes in PKU, tyr supplementation alone does not prevent severe mental retardation [20] and 24 h tyr plasma levels show high variability. Reduced serotonin synthesis may be the result of reduced tryptophan (trp) brain concentrations caused by reduced blood-brain barrier transport of trp at elevated plasma phe concentrations [21, 22]. Different hypotheses focusing on the pathogenesis of PKU and disturbed amino acids transport from blood to brain on cerebral neurotransmitter and protein synthesis have been proposed, a detailed examination of this evidence is beyond the scope of this review.
Under normal physiological conditions, many other nutrients have an important role in brain development and function affecting multiple processes regulating neurotransmitter pathways, synaptic transmission, membrane fluidity and signal-transduction pathways [23]. Table 1 provides a summary of the key role of nutrients involved in brain development and functioning such as structural components of membranes, antioxidants, neurotransmitter precursors and co-factors [23,24,25,26,27,28,29]. For many of these nutrients, food sources are restricted in PKU diets (Table 1) and reduced levels of biomarkers for some of these nutrients have been observed in PKU [5, 30,31,32,33,34,35,36]. Poor status of some antioxidant nutrients have been associated with impaired cerebral function [30] and neuropsychological disturbances in PKU [37]. Improvements in markers of cognition (visual function and fine motor skills) have been found following supplementation with docosahexaenoic acid (DHA) in children with PKU [31, 38]. In addition to raised phe, sub-optimal levels of some of these nutrients could have an impact on cognition in PKU patients. Given this background, this is the first systematic review to investigate the status of multiple nutrients involved in brain function. Although the review will not investigate the functional outcomes of any altered levels of these nutrients found, there is a rationale that in PKU optimal levels of these nutrients, are key to achieve an optimal cognitive potential. Specifically, we have systematically reviewed, and performed meta-analysis where possible, the nutrient status of DHA, eicosapentanoic acid (EPA), phospholipids, selenium, vitamins B6, B12, E, C, A, D, folic acid, choline, uridine, calcium, magnesium, zinc, iron, iodine and cholesterol that are important for optimal brain function. This will indicate whether differences in nutrient status exist between individuals with PKU and healthy, non-PKU controls.
Methods
Search strategy and selection criteria
Literature published from 1990 to July 2016 was systematically searched in the Cochrane Central Register of Controlled Trials, Medline and Embase electronic databases in accordance with the PRISMA guidelines. The nutrients identified of interest were: DHA, EPA phospholipids, selenium, vitamins B6, B12, E, C, A, D folic acid, choline, uridine, calcium, magnesium, zinc, iron, iodine and cholesterol. To avoid the risk of bias, general search terms were chosen (such as nutrition and diet) to ensure that papers reporting nutrient levels as a secondary outcome would also be included. Further details of the search strategy are presented in the Additional file 1.
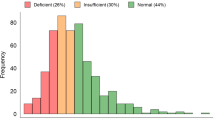
The search strategy identified 1534 publications (Fig. 1). Following the removal of conference reports, animal studies and obvious duplicates, the titles and abstracts of the remaining 741 were screened for relevance by a reviewer. Studies that may have contained results of biomarkers of a nutrient of interest, even if not explicitly mentioned in the title or abstract, were retained. One hundred and fifty-eight publications were identified as potentially relevant. Potentially eligible articles that were in a language other than English were translated. A 10% sample of the excluded articles was reviewed by a second reviewer to ensure none had been excluded that may have been relevant to the review.
The full-text publications considered possibly relevant were reviewed against the following inclusion criteria: contained a treated PKU population and healthy controls, observational or intervention study published in a peer-reviewed journal, included extractable data for biomarkers of the nutrients of interest, identified numbers of participants and their characteristics. The exclusion criteria were: untreated patients with PKU, studies in maternal PKU, in-vitro or animal studies and, if reported, studies in which the healthy control group took a vitamin and/or mineral supplement that contained any of the nutrients under review. All of the publications considered potentially relevant were reviewed by a second reviewer to determine if the same conclusion was reached about their suitability for inclusion or exclusion and any disagreements were resolved through discussion. Where the retrieved documents revealed duplication of the same patient population, the publication with the most complete set of data was included.
Data extraction
Data was extracted from the 65 publications that met the eligibility criteria (Fig. 1). Details of the participant characteristics, plasma phe control and nutrient supplementation, if provided, were extracted and relevant nutrient biomarkers of interest for PKU subjects and healthy controls were extracted from each study into a standard form by one of the reviewers and checked by a second reviewer. Biomarkers for the nutrients under review for all PKU subjects within a study were extracted, irrespective of phe control. Where the PKU population was sub-grouped (e.g. by phe control or baseline intervention group), the data were combined. The only subgroup excluded, where it was possible, was mild PKU (hyperphenylalaninaemia [HPA]), due to their less restrictive diet. Where more than one biomarker of interest for a nutrient was reported, a hierarchical approach was taken i.e. levels in plasma/serum were extracted over levels in erythrocytes, and levels in erythrocytes were extracted over other indicators of nutrient status. The most widely accepted indicator of status was extracted e.g. serum ferritin rather concentrations of iron in serum. For intervention studies, only the baseline data was utilised.
Statistical analysis
Reported comparisons of nutrient levels in PKU patients and controls were integrated and summarized into a final result per nutrient, using meta-analysis methods [39]. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for the reporting of systematic reviews and meta-analyses were followed in ensuring that an evidence-based minimum set of items were extracted [40]. For each nutrient, the information extracted from the articles included: levels expressed in mean and standard deviation of plasma/serum/other matrices in PKU patients and in controls, number of subjects and the average age per group. Where means and SDs were not reported, these values were estimated from other statistical measures. To allow comparison across studies, the standardized mean difference (SMD) was used to standardize the results of the studies to the same scale, which expresses the size of the effect in each study relative to the variability observed in that study.
These data were analysed using the random-effect meta-analysis model [39] fitted by restricted maximum likelihood estimation (REML) in SAS 9.4 (SAS Institute, Cary NC) using proc. mixed procedure. For this analysis, a minimum of four studies is generally recognized to be required [41, 42]. For parameters with a small number of studies where heterogeneity is not too high, fixed effect meta-analysis has been implemented using proc. mixed procedure in SAS 9.4 (SAS Institute, Cary NC). Due to small number of studies for some nutrients, it is preferred to calculate the 95% confidence intervals using a t-distribution (with a degrees of freedom = number of studies-1) instead of using a normal distribution. Estimate of the between-study variance in a random-effects meta-analysis is presented by Tau2 where p < 0.05 refers to a considerable amount of heterogeneity, and I2 statistic (introduced by Higgins and Thompson [43]) where and I2 > 95% indicates considerable amount of heterogeneity.
Results
Sixty-five publications were identified that provided outcomes for one or more of the nutrients reviewed, and the characteristics of these studies and the PKU populations included are summarized in Table 2.
Table 3 summarises the studies included in the systematic review and the differences in the outcomes in nutrient status markers between PKU patients and healthy controls in the individual studies. Where ≥4 studies were retrieved for a nutrient, meta-analyses of the data were performed and the overall effect estimate is presented (SMD with confidence intervals [CI]), illustrated in forest plots), although it should be noted that there was significant heterogeneity within the datasets for all nutrients. When the heterogeneity is high (I2 > 95%) and there is no statistically significant difference between the groups the overall conclusion is estimated and presented in the forest plots. Otherwise when heterogeneity is high for a given nutrient, the overall effect is not reported as it would not correctly represent the between group difference. Where < 4 studies were retrieved, the forest plots have been included to provide a graphical display of the data from individual studies which shows to which extent study results overlap without presenting the overall estimate.
Nutrients for which meta-analysis undertaken: DHA, EPA, cholesterol, zinc, vitamins B12, E and D, calcium, iron, magnesium, folate and selenium
Significantly lower levels of DHA (p = 0.0005; Fig. 2), EPA (p = 0.003; Fig. 3) and cholesterol (p < 0.0001; Fig. 4) were suggested in patients with PKU compared to healthy controls. Zinc levels tended to be lower in PKU patients compared to healthy controls, however this did not reach statistical significance but might be clinically relevant (p = 0.0534; Fig. 5).
DHA levels in PKU patients versus healthy controls. Results of meta-analyses for DHA levels in PKU patients versus healthy controls. Abbreviations: DHA, docosahexaenoic acid; LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
EPA levels in PKU patients versus healthy controls. Results of meta-analyses for EPA levels in PKU patients versus healthy controls. Abbreviations: EPA, eicosapentaenoic acid; LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
Cholesterol levels in PKU patients versus healthy controls. Results of meta-analyses for Cholesterol levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
Zinc levels in PKU patients versus healthy controls. Results of meta-analyses for Zinc levels in PKU patients versus healthy controls Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
No differences in status between PKU patients and healthy controls were apparent for vitamins B12 (p = 0.67; Fig. 6), E (p = 0.64; Fig. 7) and D (p = 0.67; Fig. 8), calcium (p = 0.32; Fig. 9), iron (p = 0.26; Fig. 10) and magnesium (p = 0.94; Fig. 11).
Vitamin B12 levels in PKU patients versus healthy controls. Results of meta-analyses for Vitamin B12 levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
Vitamin E levels in PKU patients versus healthy controls. Results of meta-analyses for Vitamin E levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
Vitamin D levels in PKU patients versus healthy controls. Results of meta-analyses for Vitamin D levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
Calcium levels in PKU patients versus healthy controls. Results of meta-analyses for Calcium levels in PKU patients versus healthy controls Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
Iron levels in PKU patients versus healthy controls. Results of meta-analyses for Iron levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
Magnesium levels in PKU patients versus healthy controls. Results of meta-analyses for Magnesium levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit
For folate (Fig. 12) and selenium (Fig. 13), the heterogeneity within the data was excessively high, so the overall conclusion of the meta-analysis was not reported. For selenium, whether the PS was supplemented or not varied for the seventeen studies identified. Therefore for studies (n = 5) where it was clearly stated in the publication that the PS was selenium-fortified [6, 30, 37, 44, 45], as there is less between-study variation, a further subgroup meta-analysis was undertaken for these five studies. This suggested that there was no difference in status between PKU patients taking a selenium-fortified PS compared to healthy controls (p = 0.0513; SMD: -0.61; 95% CI [− 1.23, 0.006]; 5 studies; 208 PKU patients; Tau2 = 0.193. It should be noted that four of the five studies in the subgroup analysis recruited subjects from the same European centre.
Nutrients for which systematic review only undertaken (no meta-analysis possible): Vitamins A, C and B6, PLs, choline, iodine and uridine (forest plots presented as additional files)
As summarized in Table 3, for vitamins A (3 studies; Additional file 2) C (3 studies; Additional file 3), B6 (2 studies; Additional file 4) and PLs (2 studies; Additional file 5), an insufficient number of publications were retrieved to perform meta-analyses. No studies reporting plasma concentrations of choline, iodine or uridine status (plasma uridine or uridine monophosphate) in PKU were retrieved. However, two studies reported brain choline concentrations, which correlate with plasma choline levels, were found in PKU patients using proton magnetic resonance spectroscopy (1H-MRS), [46, 47]) (Additional file 6).
Discussion
To the best of our knowledge, this is the first systematic review and meta-analysis of published studies investigating differences between PKU patients and healthy controls in the status of multiple nutrients involved in brain function. The nutrients investigated affect multiple structural and metabolic pathways within the brain and the potential implications of the altered nutrient status found or indeed the lack of data for some of these nutrients is discussed.
DHA, EPA, cholesterol, PL and choline are key structural components of neuronal membranes. Lower status of DHA, EPA and cholesterol levels are suggested by the meta-analyses for PKU patients compared to healthy controls. In healthy individuals, there is evidence of limited endogenous synthesis of DHA and EPA from the parent n-3 essential fatty acid, α linolenic acid [48,49,50] and in PKU patients the by-products of excessive phe may further inhibit synthesis of DHA [51]. Our findings of poorer DHA and EPA status concur with a previous meta-analysis carried out by Lohner et al. [36], who found suboptimal n-3 LC-PUFA status in PKU patients. As there have been many studies that have reported poor fatty acids status of PKU patients over the last 20 yrs, dietary advice has been modified and some PS have since been fortified with DHA, EPA and the parent essential fatty acids. Interestingly, some recent studies [52,53,54], where a few or all the patients were taking a fortified PS (essential or long chain n-3 fatty acids) or a modified fat diet, found no difference in DHA and EPA status in PKU patients compared to healthy controls.
Cholesterol is also a key component of neuronal membranes with 24S-hydroxycholesterol (24 s-OHC) [25] a specific metabolite of brain cholesterol metabolism measurable in blood. Decreased levels of plasma 24 s-OHC in PKU individuals have been reported which may indicate reduced cholesterol synthesis in the brain and/or disturbed conversion from cholesterol to 24S-OHC [55]. Some animal studies have reported that cholesterol synthesis maybe suppressed in PKU with reduced activity of two key cholesterol synthesis enzymes [55]. Furthermore, Colome et al., 2003 [44] reported a relationship between high plasma phenylalanine levels and an inhibition of cholesterogenesis, although the low fat and saturates intakes typical in PKU diets may also result in lower serum cholesterol levels. The finding of significantly lower total plasma cholesterol levels in PKU patients in this meta-analysis may suggest altered brain levels and given the importance of this nutrient for brain function, further studies directly measuring 24 s-OHC in patients with PKU should be considered.
A phe-dependent down regulation of the hydroxymethylglutaryl (HMG)-CoA reductase and the mevalonate-5-pyrophosphate decarboxylase activities, may potentially reduce the synthesis of both cholesterol and coenzyme Q10 (CoQ10) through their common mevalonate pathway [56,57,58]. CoQ10, a lipid component acting as an electron carrier in the mitochondrial respiratory chain, has been negatively correlated with phe levels in serum of PKU patients [59,60,61]. However, it is suggested that that HPA has less profound effect upon CoQ10 synthesis than cholesterol synthesis [57, 62] in PKU low plasma levels of CoQ10 may be caused by increased oxidative stress [45].
Only two studies reporting on PL status were identified; Galli et al. reported no significant difference in 15 children with PKU compared to controls and Pietz et al., using 31P-MR spectroscopy [34] reported significantly lower baseline brain membrane bound PL levels, but no differences in mobile PL or catabolic metabolites in 11 PKU patients.
Antioxidant nutrients such as zinc, selenium and vitamins A, C and E play a key role in detoxifying reactive intermediates in the brain. Where intakes of antioxidant nutrients are poor, such as in PKU, antioxidant defenses may be compromised, contributing to the highly oxidative environment observed in PKU. Increased markers of oxidative stress have been observed in PKU populations; for example, Colome et al. [44] found plasma lipid peroxidation to be increased in PKU and Artuch et al. [45] observed that ubiquinone-10 concentrations were significantly lower in PKU patients compared with healthy controls. High levels of circulating phe are known to exacerbate excessive production of reactive oxygen species [63]. It is suggested that systemic oxidative stress causes increased lipid peroxidation and altered plasmatic fatty acid profiles [64]. Also associated with a high number of double bonds, DHA/EPA are particularly susceptible to peroxidative breakdown, offering an additional explanation for the lower levels of these fatty acids as found in the current meta-analysis.
For the antioxidant nutrients, we found no apparent difference in status for vitamin E and zinc, too few studies identified to carry out meta-analyses for vitamins A and C, or the degree of heterogeneity was too high to draw a definitive conclusion for selenium. Selenium is a nutrient of particular concern in PKU given that dietary sources are very limited, and intakes are typically very poor when compliance with the PS prescription is inadequate. The selenium content of vegetation varies depending on the concentrations in soil, with Europe and China typically having lower concentrations than North America [65]. Selenium supplementation of PKU diets was introduced in the mid-1980s [6] when selenium essentiality became more widely accepted. Although there may be a suggestion from the limited cluster analysis in this review and evidence from intervention studies [66, 67] that selenium supplementation is effective in improving status, it is also observed that 14 of the 16 studies in this review had confidence intervals on the left side of the plot, suggesting lower levels in PKU patients compared to controls. Therefore, although improvement in selenium status is observed in clinical practice with supplementation, the findings from this meta-analysis are inconclusive because of the high heterogeneity within the data. This may be due to several factors including: variable selenium intakes depending on whether the PS was fortified/not over the timeframe of the literature review; variation in patient compliance with PS over a wide age range and bioavailability of different sources of selenium [68] and/or low concentrations of selenium in grains and vegetables (many studies identified were in European populations). Furthermore, both the PKU and the healthy control groups in the studies were found to have selenium status that was low or close to lower European population norms in some studies [44, 45, 67, 69,70,71,72,73,74] Therefore, at this time further research is warranted investigating selenium status in PKU and the effects of supplementation including measurement of plasma selenoprotein P (SEPP1) as a more informative marker of status.
Adherence to the phe-restricted diet is necessary to achieve plasma phe control including compliance with PS as the predominant source of many nutrients in the PKU diet, such as vitamin B12, calcium, vitamin D, zinc and iron and to ensure adequate micronutrient status. However, patients who are non- or poorly- compliant with their PS prescription are at greatest risk of suboptimal intakes of these nutrients. For example, there have been several case studies reporting poor vitamin B12 status in patients as a consequence of a relaxed PKU diet [7, 75] and low intakes of calcium have been reported in patients with PKU [76,77,78] particularly if compliance is poor in older children/adults. The meta-analysis found no difference in plasma calcium levels in PKUs compared to healthy controls; however, plasma calcium is not a suitable biomarker of status [79]. So no conclusion about the status of calcium related to brain function in PKU can be drawn from this finding. We did not find a between group difference in vitamin D status between PKUs and healthy controls, however, minimal cutaneous synthesis is now assumed and recommended dietary intakes for vitamin D have increased globally in recent years [80, 81]. There is also emerging knowledge of the role of vitamin D as a ‘neuro-steroid’ and regulator of brain serotonin synthesis [82, 83]. Given this increasing knowledge on vitamin D requirements, dietary intakes of vitamin D by those with PKU should be monitored to ensure recommended intakes are achieved.
Intakes of folic acid are much less likely to be compromised given that good food sources, such as fruit and vegetables, are allowed in controlled or unrestricted quantities in the diet and that PS are routinely supplemented. In the meta-analysis for folic acid the excessively high heterogeneity across the studies undermined its reliability to draw a conclusion on between group differences in status. Nonetheless 6 of the 7 studies [84,85,86,87,88,89] had confidence intervals on the right side of the plot (Fig. 6), suggesting positive differences between PKU patients and healthy controls. Intakes of folic acid by patients who are compliant with their PS prescription may be higher than desired when combined with intakes from normal foods that are also good sources of folic acid, and indeed high serum folate levels have been observed in PKU [90,91,92]. Vitamin B12 deficiency may be masked where circulating folate levels are high [93] and Walter et al. [9] reported that functional vitamin B12 deficiency can occur in the presence of normal B12 concentrations in PKU. Although we observed no apparent difference in vitamin B12 status in PKU patients compared to healthy controls suggesting that supplementation is effective in maintaining nutrient status comparable to controls, the physiological effect of potentially high folate intakes and levels needs consideration.
The systematic review found limited or no publications matching our entry criteria on nutritional status of some nutrients (vitamins A, C, B6, choline, uridine, iodine and PL). Although the status of some nutrients such as vitamin C is unlikely to be compromised in PKU, others such as choline and iodine warrant consideration. In healthy individuals, de-novo synthesis of choline is not sufficient to meet requirements and recommended or adequate intakes (AI) have been established [94, 95], however, sub-optimal intakes of choline are reported in the general population compared to the recommended AI [96, 97]. The main choline-rich food groups are restricted in PKU, and many PS are supplemented with choline. Dezortova et al. reported significantly lower brain choline concentrations (p < 0.05) in 15 adult PKU patients on a moderate/strict diet compared to controls [33]. Whereas, Sijens [98] reported no significant difference in brain choline levels between 10 adult PKU patients (including both compliant and non-compliant) and those of healthy controls. No detail on dietary intake of choline was provided in these studies. Because of the wide-ranging role of choline in brain function, if present, inadequate choline status in PKU may have an impact on neurological outcomes and so dietary intakes should be monitored and studies investigating choline status should be considered. This systematic review revealed no publications matching our inclusion criteria comparing iodine status of PKU patients with healthy controls. However, in PKU, an altered free thyroid hormone concentrations in PKU, in association with an impaired activity of thyroxine-5-deiodinase enzyme is described [35, 99],
Given that intakes of iodine from normal foods in PKU diets are likely to be very low and that iodine has an important role in thyroid function and brain development [100], the possibility of insufficiency among poorly compliant patients in particular should be considered.
Limitations and recommendations
The robustness of the conclusions drawn from any systematic review and meta-analysis is limited by the quality, quantity and content of the available data. In addition, the relationship between nutrient intakes and status is complex, and depends on many factors such as the bioavailability of nutrients, nutrient interactions and individual metabolism. Although these meta-analyses provide valuable insight into the status of nutrients, there was a high degree of within- and between- study heterogeneity. This may be due to a number of factors such as: variation in nutrient intake; historical differences in the fortification of PS; degree of dietary compliance; the wide age range of patients affecting compliance; broad phe tolerance determining natural food intakes and changes in management during the 25 years of literature included in this review. Also, there was a lack of information in several papers on dietary intake and compliance including nutrient fortification of the PS/not. Another limitation is that over the timeframe of the systematic review, improved markers of nutritional status have been identified for example, all of the studies reported plasma selenium concentrations as the status marker, whereas more recently plasma selenoprotein P (SEPP1) has been considered to be a more informative marker of status. Comparison with healthy controls assumes that their nutritional status is adequate however for some nutrients e.g. iron or vitamin D, status can be compromised in otherwise healthy populations [101].
As for all studies measuring nutritional status, it is important that the most relevant biomarkers are measured, and sampling procedures strictly followed. It is recommended that more details of patient characteristics (severity of PKU) and dietary information (details of protein tolerance, PS dosage, BH4 intake and adherence) is reported in studies. Given the small numbers of patients available for study in PKU and in the absence of multi-centre studies, systematically reviewing the literature and undertaking meta-analysis to inform and support best practice is a valuable tool. To allow extraction of data on key items from studies for future meta-analyses, we recommend that a standardised approach for the reporting of observational studies should be followed as this would allow more robust and definitive conclusions to be drawn from meta-analyses.
Concluding remarks
Whilst changes in fortification practices of PS and dietary advice more generally have led to improvements in status for some of the nutrients reviewed, to ensure optimal outcome in PKU, patients’ micronutrient and fatty acid status should continue to be monitored, with a particular focus on patients who are non-compliant or poorly compliant with their PS. We noted that for several of the nutrients we identified as being of interest in this review, only a few or no publications matching our inclusion criteria were found. We expect that for those nutrients for which patients depend almost exclusively on their PS, such as choline and iodine, nutrient insufficiency among poorly compliant PKU patients should be explored. As is standard practice, the importance of dietary compliance should continue to be emphasized to patients including adherence to the PS as an invaluable source of micronutrients. Dietary management is complex and changing with the advent of new pharmaceutical adjunctive therapies (e.g tetrahydrobiopterin and phenylalanine ammonium lysase) where a more liberal diet with more natural protein may be taken, for these patient groups it is important to ensure that there is an ongoing adequate intake of a range of micronutrients. Although the meta-analyses revealed differences between healthy controls and PKU patients in nutrient status for some of nutrients, we did not investigate whether poor status has a role in the pathophysiology of any of the neurological deficits observed in treated PKU patients. However, status of key nutrients known to have a role in cognitive development and functioning should be monitored.
Our recommendations for the biochemical monitoring for relevant nutrients for PKU brain function (using the European PKU guidelines [2] and the PKU Nutrition Management Guidelines of the Southeast Regional Newborn Screening Collaborative (SERC) and Genetic Metabolic Dietitians International (GMDI) [102] for direction) are given in Table 4.
Abbreviations
- BMD:
-
Bone mineral density
- CoQ10:
-
Coenzyme Q10
- DHA:
-
Docosahexaenoic acid
- EPA:
-
Eicosapentanoic acid
- HMG-CoA:
-
Hydroxymethylglutaryl coenzyme A
- HPA:
-
Hyperphenylalaninaemia
- LCPUFA:
-
Long chain polyunsaturated fatty acids
- phe:
-
Phenylalanine
- PKU:
-
Phenylketonuria
- PLs:
-
Phospholipids
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PS:
-
Protein substitute
- REML:
-
Restricted maximum likelihood estimation
- SEPP1:
-
Selenoprotein P
- SMD:
-
Standardized mean difference
- trp:
-
Tryptophan
- tyr:
-
Tyrosine
References
Scriver CR. In: Scriver CR BA, Sly WS, Valle D, Childs B, Kinzler KW, Vogelstein B, editors. Editor Hyperphenylalaninemia: phenylalanine hydroxylase deficiency, in The Metabolic and Molecular Bases of Inherited Disease. New York: Hill McGraw; 2001. p. 1667–724.
van Spronsen FJ, et al. Key European guidelines for the diagnosis and management of patients with phenylketonuria. Lancet Diabetes Endocrinol. 2017;5(9):743–56.
MacDonald A, et al. Nutrition in phenylketonuria. Mol Genet Metab. 2011;104(SUPPL):S10–8.
Evans S, et al. The micronutrient status of patients with phenylketonuria on dietary treatment: an ongoing challenge. Ann Nutr Metab. 2014;65(1):42–8.
Van Gool CJAW, Van Houwelingen AC, Hornstra G. The essential fatty acid status in phenylketonuria patients under treatment. J Nutr Biochem. 2000;11(11–12):543–7.
Smith AM, et al. Phenylketonuria affects the selenium status of children, adolescents, and young adults. J Trace Elem Exp Med. 1994;7(1):39–45.
Aung TT, et al. Vitamin B12 deficiency in an adult phenylketonuric patient. J Inherit Metab Dis. 1997;20(4):603–4.
Feillet F, Agostoni C. Nutritional issues in treating phenylketonuria. J Inherit Metab Dis. 2010;33(6):659–64.
Walter JH. Vitamin B12 deficiency and phenylketonuria. Mol Genet Metab. 2011;104(Suppl):S52–4.
Al Hafid N, Christodoulou J. Phenylketonuria: a review of current and future treatments. Transl Pediatr. 2015;4(4):304–17.
Belanger-Quintana A, et al. Up to date knowledge on different treatment strategies for phenylketonuria. Mol Genet Metab. 2011;104:S19–25.
Lammardo AM, et al. Main issues in micronutrient supplementation in phenylketonuria. Mol Genet Metab. 2013;110:S1–5.
Albrecht J, Garbade SF, Burgard P. Neuropsychological speed tests and blood phenylalanine levels in patients with phenylketonuria: a meta-analysis. Neurosci Biobehav Rev. 2009;33(3):414–21.
Anderson PJ, et al. Are neuropsychological impairments in children with early-treated phenylketonuria (PKU) related to white matter abnormalities or elevated phenylalanine levels? Dev Neuropsychol. 2007;32(2):645–68.
Brumm VL, Grant ML. The role of intelligence in phenylketonuria: a review of research and management. Mol Genet Metab. 2010;99(Suppl 1):S18–21.
Christ SE, et al. Executive function in early-treated phenylketonuria: profile and underlying mechanisms. Mol Genet Metab. 2010;99(Suppl 1):S22–32.
Leuzzi V, et al. Executive function impairment in early-treated PKU subjects with normal mental development. J Inherit Metab Dis. 2004;27(2):115–25.
Smith ML, et al. Randomised controlled trial of tyrosine supplementation on neuropsychological performance in phenylketonuria. Arch Dis Child. 1998;78(2):116–21.
Webster D, Wildgoose J. Tyrosine supplementation for phenylketonuria. Cochrane Database Syst Rev. 2010;4(8):Cd001507.
van Spronsen FJ, Smit PG, Koch R. Phenylketonuria: tyrosine beyond the phenylalanine-restricted diet. J Inherit Metab Dis. 2001;24(1):1–4.
van Spronsen FJ, Hoeksma M, Reijngoud DJ. Brain dysfunction in phenylketonuria: is phenylalanine toxicity the only possible cause? J Inherit Metab Dis. 2009;32(1):46–51.
de Groot MJ, et al. Pathogenesis of cognitive dysfunction in phenylketonuria: review of hypotheses. Mol Genet Metab. 2010;99(Suppl 1):S86–9.
Gomez-Pinilla F. Brain foods: the effects of nutrients on brain function. Nat Rev Neurosci. 2008;9(7):568–78.
Bourre JM. Effects of nutrients (in food) on the structure and function of the nervous system: update on dietary requirements for brain. Part 1: micronutrients. J Nutr Health Aging. 2006;10(5):377–85.
Martin MG, Pfrieger F, Dotti CG. Cholesterol in brain disease: sometimes determinant and frequently implicated. EMBO Rep. 2014;15(10):1036–52.
Zeisel SH. Nutritional genomics: defining the dietary requirement and effects of choline. J Nutr. 2011;141(3):531–4.
Zeisel SH, da Costa KA. Choline: an essential nutrient for public health. Nutr Rev. 2009;67(11):615–23.
Morris MC. Nutritional determinants of cognitive aging and dementia. Proc Nutr Soc. 2012;71(1):1–13.
Prado EL, Dewey KG. Nutrition and brain development in early life. Nutr Rev. 2014;72(4):267–84.
Gassió R, et al. Cognitive functions and the antioxidant system in phenylketonuric patients. Neuropsychology. 2008;22(4):426–31.
Agostoni C, et al. Effects of long-chain polyunsaturated fatty acid supplementation on fatty acid status and visual function in treated children with hyperphenylalaninemia. J Pediatr. 2000;137(4):504–9.
Moseley K, Koch R, Moser AB. Lipid status and long-chain polyunsaturated fatty acid concentrations in adults and adolescents with phenylketonuria on phenylalanine-restricted diet. J Inherit Metab Dis. 2002;25(1):56–64.
Dezortová M, et al. MR in phenylketonuria-related brain lesions. Acta radiologica (Stockholm, Sweden : 1987. 2001;42(5):459–66.
Pietz J, et al. Cerebral energy metabolism in phenylketonuria: findings by quantitative in vivo 31P MR spectroscopy. Pediatr Res. 2003;53(4):654–62.
van Bakel MM, et al. Antioxidant and thyroid hormone status in selenium-deficient phenylketonuric and hyperphenylalaninemic patients. Am J Clin Nutr. 2000;72(4):976–81.
Lohner S, Fekete K, Decsi T. Lower n-3 long-chain polyunsaturated fatty acid values in patients with phenylketonuria: a systematic review and meta-analysis. Nutr Res (New York, N.Y. 2013;33(7):513–20.
Sierra C, et al. Antioxidant status in hyperphenylalaninemia. Clin Chim Acta. 1998;276(1):1–9.
Koletzko B, et al. Does dietary DHA improve neural function in children? Observations in phenylketonuria. Prostaglandins Leukot Essent Fat Acids. 2009;81(2–3):159–64.
van Houwelingen HC, Arends LR, Stijnen T. Advanced methods in meta-analysis: multivariate approach and meta-regression. Stat Med. 2002;21(4):589–624.
Moher D, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Hoboken, NJ: Wiley; 2009.
Cochrane-Collaboration. T., Cochrane handbook for systematic reviews of interventions. Hoboken, NJ: Wiley-Blackwell; 2008.
Higgins JP, Thompson SG. Quantifying heterogenity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Colomé C, et al. Lipophilic antioxidants in patients with phenylketonuria. Am J Clin Nutr. 2003;77(1):185–8.
Artuch R, et al. A longitudinal study of antioxidant status in phenylketonuric patients. Clin Biochem. 2004;37(3):198–203.
Cohen BM, et al. Decreased brain choline uptake in older adults. An in vivo proton magnetic resonance spectroscopy study. JAMA. 1995;274(11):902–7.
Rijpma A, et al. Effects of Souvenaid on plasma micronutrient levels and fatty acid profiles in mild and mild-to-moderate Alzheimer's disease. Alzheimers Res Ther. 2015;7(1):51.
Calder PC. Mechanisms of action of (n-3) fatty acids. J Nutr. 2012;142(3):592S–9S.
Koletzko B, et al. Omega-3 LC-PUFA supply and neurological outcomes in children with phenylketonuria (PKU). J Pediatr Gastroenterol Nutr. 2009;48(Suppl 1):S2–7.
Plourde M, Cunnane SC. Extremely limited synthesis of long chain polyunsaturates in adults: implications for their dietary essentiality and use as supplements. Appl Physiol Nutr Metab. 2007;32(4):619–34.
Infante JP, Huszagh VA. Impaired arachidonic (20:4n-6) and docosahexaenoic (22:6n-3) acid synthesis by phenylalanine metabolites as etiological factors in the neuropathology of phenylketonuria. Mol Genet Metab. 2001;72(3):185–98.
Gramer G, et al. Long-chain polyunsaturated fatty acid status in children, adolescents and adults with phenylketonuria. Prostaglandins Leukot Essent Fat Acids. 2016;109:52–7.
Htun P, et al. Fish-free diet in patients with phenylketonuria is not associated with early atherosclerotic changes and enhanced platelet activation. PLoS One. 2015;10(8):e0135930.
LaVoie SM, Harding CO, Gillingham MB. Normal fatty acid concentrations in young children with phenylketonuria. Top Clin Nutr. 2009;24(4):333–40.
Nagasaka H, et al. Oxysterol changes along with cholesterol and vitamin D changes in adult phenylketonuric patients diagnosed by newborn mass-screening. Clinica chimica acta; international journal of clinical chemistry. 2013;416:54–9.
Shefer S, et al. Is there a relationship between 3-hydroxy-3-methylglutaryl coenzyme a reductase activity and forebrain pathology in the PKU mouse? J Neurosci Res. 2000;61(5):549–63.
Kyprianou N, et al. Assessment of mitochondrial respiratory chain function in hyperphenylalaninaemia. J Inherit Metab Dis. 2009;32(2):289–96.
Hargreaves IP. Coenzyme Q10 in phenylketonuria and mevalonic aciduria. Mitochondrion. 2007;7:S175–80.
Artuch R, et al. Plasma phenylalanine is associated with decreased serum ubiquinone-10 concentrations in phenylketonuria. J Inherit Metab Dis. 2001;24(3):359–66.
Artuch R, et al. Conzyme-Q10 concentration in human phenylketonuria (multiple letters). J Inherit Metab Dis. 2003;26(8):821–3.
Artuch R, et al. Decreased serum ubiquinone-10 concentrations in phenylketonuria. Am J Clin Nutr. 1999;70(5):892–5.
Castillo M, Zafra MF, Garcia-Peregrin E. Inhibition of brain and liver 3-hydroxy-3-methylglutaryl-CoA reductase and mevalonate-5-pyrophosphate decarboxylase in experimental hyperphenylalaninemia. Neurochem Res. 1988;13(6):551–5.
Rocha JC, Martins MJ. Oxidative stress in phenylketonuria: future directions. J Inherit Metab Dis. 2012;35(3):381–98.
Oborna I, et al. Increased lipid peroxidation and abnormal fatty acid profiles in seminal and blood plasma of normozoospermic males from infertile couples. Hum Reprod. 2010;25(2):308–16.
Fairweather-Tait SJ, Collings R, Hurst R. Selenium bioavailability: current knowledge and future research requirements. Am J Clin Nutr. 2010;91(5):1484S–91S.
Sitta A, et al. Beneficial effect of l-carnitine and selenium supplementation on oxidative stress in phenylketonuric patients. J Inherit Metab Dis. 2011;34:S103.
Wilke BC, et al. Selenium, glutathione peroxidase (GSH-Px) and lipid peroxidation products before and after selenium supplementation. Clin Chim Acta. 1992;207(1–2):137–42.
Nève J. Human selenium supplementation as assessed by changes in blood selenium concentration and glutathione peroxidase activity. J Trace Elem Med Biol. 1995;9(2):65–73.
Sitta A, et al. Evidence that L-carnitine and selenium supplementation reduces oxidative stress in phenylketonuric patients. Cell Mol Neurobiol. 2011;31(3):429–36.
Coskun T, et al. Serum selenium levels in phenylketonuric children on low phenylalanine diet. Doga - Turkish Journal of Medical Sciences. 1993;18(2):161–5.
Reilly C, et al. Trace element nutrition status and dietary intake of children with phenylketonuria. Am J Clin Nutr. 1990;52(1):159–65.
Rükgauer M, Klein J, Kruse-Jarres JD. Chromium, copper, manganese, selenium, and zinc in the serum of children with phenylketonuria. Aktuelle Ernährungsmedizin. 1998;23(1):23–7.
Terwolbeck, K., et al., Low selenium status, thyroid hormones, and other parameters in children with phenylketonuria (PKU), in Trace elements in man and animals - TEMA 8: Proceedings of the Eighth International Symposium on Trace Elements in Man and Animals. Dresden; 1993. p. 538. ISBN: 3894859997.
EFSA. Scientific Opinion on Dietary Reference Values for selenium. EFSA Panel on Nutrition, Dietetic products and allergies. EFSA J. 2014;12(10):67.
Hanley WB, et al. Vitamin B12 deficiency in adolescents and young adults with phenylketonuria. Eur J Pediatr. 1996;155(Suppl 1):S145–7.
Hillman L. Decreased bone mineralization in children with phenylketonuria under treatment. Eur J Pediatr, Supplement. 1996;155(1):S148–52.
McMurry MP, et al. Bone mineral status in children with phenylketonuria - relationship to nutritional intake and phenylalanine control. Am J Clin Nutr. 1992;55(5):997–1004.
Pérez-Dueñias B, et al. New approach to osteopenia in phenylketonuric patients. Acta Paediatr, International Journal of Paediatrics. 2002;91(8):899–904.
Efsa Panel on Dietetic Products, N. and Allergies. Scientific opinion on dietary reference values for calcium. EFSA J. 2015;13(5):4101.
EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies). Scientific opinion on dietary reference values for vitamin D. EFSA J. 2016;14(10):4547,145.
Medicine., I.o. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011.
Harms LR, et al. Vitamin D and the brain. Best Pract Res Clin Endocrinol Metab. 2011;25(4):657–69.
Patrick RP, et al. Vitamin D and the omega-3 fatty acids control serotonin synthesis and action, part 2: relevance for ADHD, bipolar disorder, schizophrenia, and impulsive behavior. FASEB J : official publication of the Federation of American Societies for Experimental Biology. 2015;29(6):2207–22.
Colomé C, et al. Plasma thiols and their determinants in phenylketonuria. Quimica Clinica. 2003;22(2):71–5.
Huemer M, et al. Total homocysteine, B-vitamins and genetic polymorphisms in patients with classical phenylketonuria. Mol Genet Metab. 2008;94(1):46–51.
Huemer M, et al. Free asymmetric dimethylarginine (ADMA) is low in children and adolescents with classical phenylketonuria (PKU). J Inherit Metab Dis. 2012;35(5):817–21.
Lucock M, et al. The impact of phenylketonuria on folate metabolism. Mol Genet Metab. 2002;76(4):305–12.
Robinson M, et al. Increased risk of vitamin B12 deficiency in patients with phenylketonuria on an unrestricted or relaxed diet. J Pediatr. 2000;136(4):545–7.
Gündüz M, et al. Comparison of atherogenic risk factors among poorly controlled and well-controlled adolescent phenylketonuria patients. Cardiol Young. 2016;26(5):901–8.
MacDonald A, et al. Long-term compliance with a novel vitamin and mineral supplement in older people with PKU. J Inherit Metab Dis. 2008;31(6):718–23.
Rohr FJ, Munier AW, Levy HL. Acceptability of a new modular protein substitute for the dietary treatment of phenylketonuria. J Inherit Metab Dis. 2001;24(6):623–30.
Stoelen LH, et al. High plasma folate levels in adults with PKU on protein substitute. J Inherit Metab Dis. 2010;33:S170.
Malouf M, Grimley EJ, Areosa SA. Folic acid with or without vitamin B12 for cognition and dementia. Cochrane Database Syst Rev. 2003;4:CD004514.
Institute of Medicine, F.a.N.B. Dietary Reference Intakes for Thiamine, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press; 1997.
EFSA NDA P. EFSA panel on dietetic products, N.A.a., Scientific opinion on Dietary Reference Values for choline. EFSA J. 2016;14(8):4484.
Vennemann FB, et al. Dietary intake and food sources of choline in European populations. Br J Nutr. 2015;114(12):2046–55.
Wallace TC, Fulgoni VL 3rd. Assessment of Total choline intakes in the United States. J Am Coll Nutr. 2016;35(2):108–12.
Sijens PE, et al. 1H MR chemical shift imaging detection of phenylalanine in patients suffering from phenylketonuria (PKU). Eur Radiol. 2004;14(10):1895–900.
Calomme MR, et al. Thyroid function parameters during a selenium repletion/depletion study in phenylketonuric subjects. Experientia. 1995;51(12):1208–15.
Redman K, et al. Iodine deficiency and the brain: effects and mechanisms. Crit Rev Food Sci Nutr. 2016;56(16):2695–713.
Beverley Bates, L.C., Sonja Nicholson Polly Page, Ann Prentice, Toni Steer and Gillian Swan (eds) National Diet and Nutrition Survey Results from Years 5 and 6 (combined) of the Rolling Programme (2012/2013–2013/2014). 2016: PHE publications gateway number: 2016248.
SERC&GMDI, PKU Nutrition Management Guidelines. 2016: https://southeastgenetics.org/ngp/guidelines.php/90/PKU%20Nutrition%20Guidelines/Version%201.12. Accessed 9 May 2018.
Dyall SC. Long-chain omega-3 fatty acids and the brain: a review of the independent and shared effects of EPA, DPA and DHA. Front Aging Neurosci. 2015;7:52.
van Wijk N, et al. Targeting synaptic dysfunction in Alzheimer's disease by administering a specific nutrient combination. J Alzheimers Dis. 2014;38(3):459–79.
Wurtman RJ. A nutrient combination that can affect synapse formation. Nutrients. 2014;6(4):1701–10.
Schreurs BG. The effects of cholesterol on learning and memory. Neurosci Biobehav Rev. 2010;34(8):1366–79.
Nagasaka H, et al. Changes of lipoproteins in phenylalanine hydroxylase-deficient children during the first year of life. Clin Chim Acta. 2014;433:1–4.
Frederickson CJ, et al. Importance of zinc in the central nervous system: the zinc-containing neuron. J Nutr. 2000;130(5S Suppl):1471S–83S.
Hidalgo C, Carrasco MA. Redox control of brain calcium in health and disease. Antioxid Redox Signal. 2011;14(7):1203–7.
de Baaij JH, Hoenderop JG, Bindels RJ. Magnesium in man: implications for health and disease. Physiol Rev. 2015;95(1):1–46.
Agostoni C, et al. Biochemical effects of supplemented long-chain polyunsaturated fatty acids in hyperphenylalaninemia. Prostaglandins Leukot Essent Fat Acids. 2001;64(2):111–5.
Galli C, et al. Reduced plasma C-20 and C-22 polyunsaturated fatty acids in children with phenylketonuria during dietary intervention. J Pediatr. 1991;119(4):562–7.
Giovannini M, et al. Long-chain polyunsaturated fatty acids profile in plasma phospholipids of hyperphenylalaninemic children on unrestricted diet. Prostaglandins Leukot Essent Fat Acids. 2011;84(1–2):39–42.
Lage S, et al. Fatty acid profile in patients with phenylketonuria and its relationship with bone mineral density. J Inherit Metab Dis. 2010;33(3):363–71.
Sanjurio P, et al. Polyunsaturated fatty acid status in patients with phenylketonuria. J Inherit Metab Dis. 1994;17(6):704–9.
Vilaseca MA, et al. Long-chain polyunsaturated fatty acid status in phenylketonuric patients treated with tetrahydrobiopterin. Clin Biochem. 2010;43(4–5):411–5.
Yi SHL, et al. A cross-sectional study of docosahexaenoic acid status and cognitive outcomes in females of reproductive age with phenylketonuria. J Inherit Metab Dis. 2011;34(2):455–63.
Acosta PB, et al. Intake and blood levels of fatty acids in treated patients with phenylketonuria. J Pediatr Gastroenterol Nutr. 2001;33(3):253–9.
Mütze U, et al. Metabolomics of dietary fatty acid restriction in patients with phenylketonuria. PLoS One. 2012;7(8):e43021.
Pöge AP, et al. Long-chain polyunsaturated fatty acids in plasma and erythrocyte membrane lipids of children with phenylketonuria after controlled linoleic acid intake. J Inherit Metab Dis. 1998;21(4):373–81.
Colomé C, et al. Is there a relationship between plasma phenylalanine and cholesterol in phenylketonuric patients under dietary treatment? Clin Biochem. 2001;34(5):373–6.
Mikołuć B, et al. Realization of nutrition recommendations and the serum lipid profile in children with PKU in Poland. Pediatr Pol. 2009;84(3):217–23.
Rocha JC, et al. Dietary treatment in phenylketonuria does not lead to increased risk of obesity or metabolic syndrome. Mol Genet Metab. 2012;107(4):659–63.
Schulpis KH. Haemostatic variables in phenylketonuric children under dietary treatment. J Inherit Metab Dis. 1996;19(5):603–9.
Schulpis KH, et al. The association of serum lipids, lipoproteins and apolipoproteins with selected trace elements and minerals in phenylketonuric patients on diet. Clin Nutr. 2004;23(3):401–7.
Schulpis KH, et al. Effect of diet on plasma total antioxidant status in phenylketonuric patients. Eur J Clin Nutr. 2003;57(2):383–7.
Schulpis KH, et al. The beneficial effect of adherence to the therapeutic diet on the main protein-energy wasting and several other biomarkers in children with phenylketonuria. Journal of Pediatric Biochemistry. 2013;3(2):99–106.
Schulpis KH, et al. The effect of diet on total antioxidant status, ceruloplasmin, transferrin and ferritin serum levels in phenylketonuric children. Acta Paediatr, International Journal of Paediatrics. 2010;99(10):1565–70.
Karam PE, et al. Cardiovascular disease biomarkers in patients with inborn errors of protein metabolism: a pilot study. J Hum Nutr Diet : the official journal of the British Dietetic Association. 2015;28(4):344–9.
Nagasaka H, et al. Cross-sectional study of bone metabolism with nutrition in adult classical phenylketonuric patients diagnosed by neonatal screening. J Bone Miner Metab. 2011;29(6):737–43.
Mikoluc B, et al. Impact of lipophilic antioxidants and level of antibodies against oxidized low-density lipoprotein in polish children with phenylketonuria. Antioxid Redox Signal. 2012;16(2):179–82.
Yang F, Yao H, Wang C. Effect of low phenylalanine diet on micro-nutrients and anti-oxidative capacity in patients with phenylketonuria. Maternal and Child Health Care of China. 2009;24(32):4539–41.
Gok F, Ekin S, Dogan M. Evaluation of trace element and mineral status and related to levels of amino acid in children with phenylketonuria. Environ Toxicol Pharmacol. 2016;45:302–8.
Jochum F, et al. Is there any health risk of low dietary selenium supply in PKU-children. Nutr Res. 1999;19(3):349–60.
Wilke BC, et al. Mineral balance in children treated for phenylketonuria. Consequences of selenium deficiency for lipid peroxidation. Arch Latinoam Nutr. 1993;43(2):119–22.
Schulpis KH, Karikas GA, Papakonstantinou E. Homocysteine and other vascular risk factors in patients with phenylketonuria on a diet. Acta Paediatr (Oslo, Norway : 1992. 2002;91(8):905–9.
Prince AP, Leklem JE. Vitamin B-6 status of alcohol-aged patients with phenylketonuria. Am J Clin Nutr. 1994;60(2):262–8.
Colomé C, et al. Plasma thiols and their determinants in phenylketonuria. Eur J Clin Nutr. 2003;57(8):964–8.
Al-Qadreh A, et al. Bone mineral status in children with phenylketonuria under treatment. Acta Paediatrica. International Journal of Paediatrics. 1998;87(11):1162–6.
Bushueva TV, et al. Calcium homeostasis and calcium-regulating hormones in young children with phenylketonuria. Voprosy Pitan. 1993;(3):16–21.
Arnold GL, et al. Iron and protein sufficiency and red cell indices in phenylketonuria. J Am Coll Nutr. 2001;20(1):65–70.
Miranda da Cruz BDO, Seidler H, Widhalm K. Iron status and iron supplementation in children with classical phenylketonuria. J Am Coll Nutr. 1993;12(5):531–6.
Beblo S, et al. Effect of fish oil supplementation on fatty acid status, coordination, and fine motor skills in children with phenylketonuria. J Pediatr. 2007;150(5):479–84.
Fisberg RM, et al. Plasma zinc, copper, and erythrocyte superoxide dismutase in children with phenylketonuria. Nutrition. 1999;15(6):449–52.
Bohles H, et al. Inadequate iron availability as a possible cause of low serum carnitine concentrations in patients with phenylketonuria. Eur J Pediatr. 1991;150(6):425–8.
Acknowledgements
The authors thank Dr. E. Cabral Monteiro for the support with the search strategy, A. Nabbe for the contribution to the statistical analysis, C. Dignum and H. Rose for professional writing services and second reviewers of data extracted, Dr. M van Rijn for her advice for data interpretation, Dr. M.C. de Wilde for his advice for the data analysis, extraction and management.
Funding
This review has been supported by Danone Nutricia Research.
Availability of data and materials
The datasets generated and/or analysed in this review are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
GAMP, MK, and AMD designed the study. GAMP extracted and analyzed the data with help of an external second reviewer, ACY performed the statistical analyses and together with GAMP produced the figures. GAMP prepared the first and revised drafts of this manuscript according to the suggestions from co-authors. RHS, AMD, ACY, GAMP and MK interpreted the data and revised the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
G.A.M.P, A.C.Y and M.K are Danone Nutricia Research employees.
A.M.D. has received research funding and honoraria from Nutricia, Vitaflo International and Merck Serono. She is a member of the European Nutrition Expert Panel (Biomarin), member of Sapropterin Advisory Board (Biomarin), member of the Advisory Board entitled ELEMENT (Danone-Nutricia), and member of an Advisory Board for Arla and Applied Pharma Research.
R.H.S. has served on the global medical advisory board for Nutricia and Biomarin, as well as the national medical advisory board for Horizon and SOBI.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Search Strategy (PDF 244 kb).
Additional file 2:
Vitamin A levels in PKU patients versus healthy controls. Vitamin A levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit (PDF 271 kb).
Additional file 3:
Vitamin C levels in PKU patients versus healthy controls. Vitamin C levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit (PDF 169 kb).
Additional file 4:
Vitamin B6 levels in PKU patients versus healthy controls. Vitamin B6 levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit (PDF 165 kb).
Additional file 5:
Phospholipid levels in PKU patients versus healthy controls. Phospholipid levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit (PDF 166 kb).
Additional file 6:
Choline levels in PKU patients versus healthy controls. Choline levels in PKU patients versus healthy controls. Abbreviations: LCL, lower confidence limit; REML, restricted maximum likelihood; SD, standard deviation; SMD, standardized mean difference; UCL, upper confidence limit (PDF 166 kb).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Montoya Parra, G.A., Singh, R.H., Cetinyurek-Yavuz, A. et al. Status of nutrients important in brain function in phenylketonuria: a systematic review and meta-analysis. Orphanet J Rare Dis 13, 101 (2018). https://doi.org/10.1186/s13023-018-0839-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-018-0839-x