Abstract
Background
This systematic review and network meta-analysis aimed to evaluate the three different administration routes of vitamin B12: oral, intramuscular (IM), and sublingual (SL) routes.
Methods
We searched four electronic databases (PubMed, Scopus, Web of Science, and Cochrane CENTRAL Register of Controlled Trials). We included only comparative studies. We performed a frequentist network meta-analysis to measure network estimates for the relative outcomes. Moreover, we conducted a pairwise meta-analysis using a random effect model to obtain direct estimates for outcomes. All outcomes were continuous, and the relative treatment effects were pooled as mean difference (MD) with 95% confidence intervals.
Results
Thirteen studies were included in the meta-analysis, with a total of 4275 patients. Regarding increasing vitamin B12 levels, the IM route ranked first, followed by the SL route (MD = 94.09 and 43.31 pg/mL, respectively) compared to the oral route. However, these differences did not reach statistical significance owing to the limited number of studies. Regarding the hemoglobin level, the pooled effect sizes showed no difference between all routes of administration that could reach statistical significance. However, the top two ranked administration routes were the oral route (78.3) and the IM route (49.6).
Conclusion
All IM, oral, and SL routes of administration of vitamin B12 can effectively increase the level of vitamin B12 without significant differences between them, as thought previously. However, the IM route was the top-ranked statistically but without clinical significance. We found no significant difference among studied administrated routes in all other CBC parameters and homocysteine levels.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin B12 is a water-soluble vitamin that may be derived from foods, including fish, meat, dairy products, and cereals that have been fortified. It can also be taken in supplement form. After being extracted by gastric acid, it travels to the terminal ileum, where it is co-absorbed along with the intrinsic factor, an enzyme from the stomach’s parietal cells (Fig. 1) [1, 2]. Vitamin B12 is essential for neurologic function, red blood cell creation, and DNA synthesis and is a coenzyme for three primary biochemical conversions: homocysteine to methionine, 5-methyltetrahydrofolate to tetrahydrofolate, and methylmalonic acid to succinyl coenzyme A [1, 2].
Reduced serum vitamin B12 levels (< 200 ng per mL [148 pmol per L]) are considered vitamin B12 deficiency [1, 2] and are associated with reduced hematopoietic and epithelial cell proliferation, elevated levels of methylmalonic acids, and propionic that impact the myelin sheaths of nerve fibers, and elevated serum homocysteine, a contributing factor for cardiovascular disorders [3]. Blood manifestations related to the deficiency in vitamin B12 are anemia (megaloblastic macrocytic), leukopenia, and thrombocytopenia; moreover, a paradoxical thrombocytosis may occur [4, 5]. In neuropsychiatry, it may cause areflexia, peripheral neuropathy, olfactory impairment, gait irregularities, proprioception, and vibratory sensation loss, cognitive problems (including dementia-like manifestations and psychosis), and irritability. In the gastrointestinal, it may cause glossitis [5,6,7,8]. So, the treatment of vitamin B12 deficiency is devastating.
There are different routes for the administration of any vitamin. Oral and intramuscular (IM) vitamin B12 are the most common routes for treating vitamin B12 deficiency, and several studies have evaluated their efficacy [9, 10]. However, in the case of vitamin B12 malabsorption, irrespective of the cause of malabsorption, the intramuscular route is preferred [11, 12]. According to the British Society for Hematology recommendations, for individuals with severe insufficiency and malabsorption syndromes, IM vitamin B12 delivery is preferable; however, oral replacement therapy may be recommended for patients with asymptomatic, moderate illness who have no concerns about absorption or compliance [13].
The sublingual (SL) route of vitamin B12 administration has been evaluated as an alternative route to oral and IM routes, especially in the case of vitamin B12 malabsorption [14,15,16], but there is no sufficient data to consider this route in the guidelines. This systematic review and network meta-analysis aimed to assess the efficacy of those three different routes of administration of vitamin B12.
Methods
For this research, we used the same format that the PRISMA statement recommends for systematic reviews and meta-analyses [17]. Every stage was carried out in a manner entirely consistent with the Cochrane Handbook of Systematic Reviews and Meta-analyses of Interventions [18].
Eligibility criteria
Studies were included in our review if they satisfied the following criteria:
-
Population: studies on patients with vitamin B12 deficiency
-
Intervention and comparator: studies where the experimental and control groups received vitamin B12 through any of these routes of administration: SL, IM, and oral
-
Outcome: studies reporting at least any of the following serum levels: vitamin B12, folate, hemoglobin, hematocrit, mean corpuscular volume, plasma homocysteine, urine methylmalonic acid, leukocyte, and platelets
-
Study design: comparative studies whose design was controlled trials with patients allocated to receive SL, IM, or oral vitamin B12 in a random or non-random allocation manner. We considered both blinded and open-label studies. We also included controlled prospective and retrospective observational studies with extreme caution; these studies were separated from randomized controlled trials in subgroups and were only considered in calculating the pooled effect size if their results were consistent with randomized controlled trials. In case of discrepancy between randomized controlled trials and observational studies, the results highlighted this, and the outcomes of randomized controlled trials were prioritized
Studies for which complete full texts were not accessible, studies not published in English, studies whose data were unsuitable for extraction and analysis, and studies that were described as abstracts only or thesis were all excluded.
Information sources and search strategy
We performed a comprehensive search of four electronic databases (PubMed, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials) from inception until May 7, 2022, using the following query: (B 12, Vitamin OR Vitamin B12 OR B12, Vitamin OR Cyanocobalamin OR Cobalamins OR Cobalamin OR Eritron OR Vitamin-B12 OR Hydroxocobalamin OR Deltavit B12) AND (Sublingual OR tongue OR Oral OR Intravenous OR IV OR Inhalation OR Buccal OR Cutaneous OR Mucosal OR Parenteral OR Subcutaneous OR SC OR Intramuscular OR IM OR Intranasal). The search was carried out by O.A.A.
Furthermore, the references of the included studies were manually searched for any potentially eligible studies. The detailed search strategy and results for each database are presented in Supplementary 1.
Selection process
Five authors (S.D., A.K., R.A.D., T.E., and T.F.) separately screened the titles and abstracts of all identified articles to determine their relevance to this meta-analysis. The second step involved screening the full-text articles of the included abstracts to determine the final eligibility for meta-analysis. Duplicates were excluded using Endnote (Clarivate Analytics, PA, USA). The discussion was used to settle any disagreements.
Data collection process and data items
Five reviewers (S.D., A.K., R.A.D., T.E., and T.F.) collected data onto a standardized data extraction sheet. Extracted information focused on four primary areas: (1) summary of the included studies (including study ID, title, study design, country, inclusion criteria, exclusion criteria, interventions, dose, sample size, treatment duration, and the main findings); (2) study population characteristics (including age, sex body mass index, serum level of vitamin B12, hematocrit, hemoglobin, and mean corpuscular volume (MCV) levels); (3) risk of bias domains according to the study design; and (4) outcome measures (the primary outcomes were the serum levels of vitamin B12 and hemoglobin and the secondary outcomes includes the levels of MCV, homocysteine, platelets count, and white blood cells count). The discussion was used to settle any disagreements.
Assessing the risk of bias in the individual studies
We independently evaluated the quality of each included study by two authors (S.D. and T.E.). The Cochrane assessment tool was used for randomized clinical trials (ROB2) [19]. Newcastle Ottawa scale (NOS) was used to assess the risk of bias for observational studies [20]. For non-randomized controlled trials, we used the Cochrane ROBINS-I tool [21]. A third author (O.A.A.) solved any disagreements.
Statistical analysis
We measured network estimates for the related outcomes using a frequentist network meta-analysis of aggregate data. The evident heterogeneity in the intervention comparison effects across studies was accommodated using the random effect model as a framework. Moreover, we conducted a pairwise meta-analysis using a random effect model to obtain direct estimates for outcomes. The transitivity assumption was examined to determine if patient and research characteristics were sufficiently comparable across comparisons. Additionally, using a loop-specific methodology, we assessed the consistency assumption locally in a closed loop [22]. The surface under the cumulative ranking (SUCRA) was used to rank the intervention’s hierarchy in the network model; then, we estimated the mean ranks [23]. A comparison-adjusted funnel plot was used to explore the potential publication bias [23].
We used a three-level hierarchical network meta-analysis to incorporate the exchangeability between different study designs to predict an effect estimate for each study design individually [24]. Thus, this model allows strength to be borrowed within the different classes of study designs, strengthening interference and potentially reducing the uncertainty around each study design and consequently increasing the ability to inform decision-making frameworks. All data of this approach were pooled as Cohen’s d with 95% confidence intervals.
All outcomes of interest were continuous, and the relative treatment effects were pooled as mean difference (MD) with 95% confidence intervals. All analyses were done in STATA version 17 using the network command.
Results
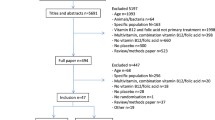
Literature search results
Our literature search process retrieved 22,262 records. Five thousand two hundred ten duplicates were removed using Endnote, and 17,052 were screened for title and abstract. One hundred forty-nine articles were qualified for full-text screening after being subjected to title and abstract screening. The meta-analysis comprised 13 of these investigations. No further papers were included after manually searching the references of the listed studies. Figure 2 illustrates the PRISMA flow diagram of the study recruitment process.
Characteristics of the included studies
Thirteen studies were included in the meta-analysis, with a total of 4275 patients. In all studies, patients were assigned to receive either oral, SL, or IM vitamin B12. A summary of the included studies and the characteristics of the population in each study are provided in Tables 1 and 2, respectively. According to the Cochrane ROB 2 tool, four studies had some concerns, two had high, and one had a low risk of bias. According to ROBINS-I checklists, one study had a high risk of bias, and one had a moderate risk of bias. Two studies had good quality, and one had fair quality, according to the NOS tool (Supplementary 2).
Primary outcomes
Vitamin B12
The network of treatment comparisons for vitamin B12 included three active individual nodes (Fig. S1; top panel). Each node represents a different administration route; the oral administration route was the most well-connected intervention with all other interventions directly linked to it; therefore, it has been used as the reference for comparison. Figure 3A shows network estimates of treatment effect on vitamin B12 levels for different route administrations compared with the oral route. Network meta-analysis showed that either the IM route (MD 94.09 pg/mL, 95% CI [− 93.36 to 281.54]) or the SL route (MD 43.31 pg/mL, 95% CI [− 228.92 to 315.54]) compared to the oral route did not reach a significant difference to increase vitamin B12 levels. According to SUCRA values, the top-ranked intervention for increasing levels of vitamin B12 was the IM route (74.2), followed by the SL route (48.4) (Table 3(A)).
We performed a three-level hierarchical model to investigate the pooled effect sizes according to the study design in which there was no significant difference between the IM and the oral routes compared to the SL route (P = 0.31, 0.16, respectively). There was a significant difference between the oral and the IM routes (Cohen’s d − 0.74, 95% CI [− 1.06 to − 0.43]; P < 0.001). The pooled effect sizes were not homogenous (I2 > 50%); Fig. S2.
Hb
Five studies comprising 3730 patients reported Hb. The network diagram included three individual nodes, (Fig. S1; bottom panel). Each node represents a different drug intervention, in which the oral route was the well-connected route of administration with all other routes directly linked to it.
Figure 3B shows network estimates of treatment effect on Hb levels for different administration routes compared to the oral route. Pooled effect sizes showed no difference between all routes of administration to increase Hb without substantial statistical evidence (Fig. 3B). According to SUCRA values, the top two ranked administration routes were the oral route (78.3) followed by the IM route (49.6) (Table 3(B)).
The three-level hierarchical model showed no significant difference among all comparisons of administration routes; Cohen’s d was 0.07 for IM vs SL routes, 0.06 for oral vs IM routes, and 0.22 for oral vs SL routes. The pooled effect size was homogenous (I2 = 0%) (Fig. S3).
Secondary outcomes
Five included studies comprising 3605 patients reported change in MCV, four studies comprising 140 patients reported change in homocysteine levels, four studies comprising 3588 patients reported change in platelets count, and only three studies with 3430 patients reported change in WBC count.
Figures S4 and S5 show networks of routes of administration for secondary outcomes. Figure 3C–F summarize the results for secondary outcomes. Network meta-analysis showed no evidence of differences among all possible comparisons for secondary outcomes (MCV, homocysteine levels, platelet counts, and WBC counts). Supplementary Table 5 presents SUCRA values. However, none of the three-level hierarchical models showed any significance among all possible comparisons of administration routes (Figs. S6-S9).
Discussion
Significance of the study
To our knowledge, this is the most comprehensive network meta-analysis comparing the efficacy of SL, IM, and oral routes of administration of vitamin B12 in patients with vitamin B12 deficiency. The significance of this paper is not only to compare the three routes of administration but also to evaluate them and determine which route is the best to administrate the drug. The study also opens the door for more future research about the administration routes of vitamin B12 and other vitamins.
Summary of the findings
The current article evaluated 13 studies, of which eight were randomized clinical trials comparing different administration routes of vitamin B12 in patients with vitamin B12 deficiency. A total of 4275 patients with vitamin B12 deficiency were included in the final analysis. We found that irrespective of the route of vitamin B12 administration, serum vitamin B12 levels were increased. When comparing the different routes, the top-ranked route for increasing levels of vitamin B12 was the IM route, followed by the SL route. However, this difference has no clinical significance.
Interestingly, we found no significant difference among studied administrated routes in all other CBC parameters such as Hb, MCV, platelets count, WBC count, and homocysteine level. Given the fact that vitamin B12 levels were increased insignificantly among all routes, the preference of the administrated route should be referenced to the advantages and disadvantages of each route as well as the patient situation, which will be decided according to the physician’s opinion.
We highlighted the summary of the advantages and disadvantages of each route in (Fig. 4) [37,38,39,40,41,42,43,44,45,46,47,48], as treatment decision depends on the patient’s condition and the physician’s opinion. The details about the advantages and disadvantages of each route are present in Supplementary 4.
Sublingual vs intramuscular and oral routes of administration
A previous systematic review by Cochrane compared the effectiveness of oral versus IM routes of vitamin B12 administration. It showed that both effectively improve serum vitamin B12 levels for people suffering from vitamin B12 deficiency. However, the dosage of oral vitamin B12 might be a clinical factor that affects this outcome [9]. This contributes to the absorption mechanism of oral vitamin B12, which does not depend only on intrinsic factors, but the absorption can be done through passive diffusion. Passive diffusion accounts for 1.2% of overall absorption, with little effect on bioavailability in patients with pernicious anemia or gastro-duodenal resection [49, 50].
As our results showed, there is no difference between them in terms of efficacy, but in terms of patients’ tolerance, advantages, and disadvantages of each route, the sublingual route is preferred over IM and oral routes. SL vitamin B12 is as adequate as IM and oral vitamin B12. However, the SL route of administration has more advantages and fewer disadvantages than IM and oral routes. So, we recommend using SL vitamin B12 rather than oral and IM, especially in patients who do not tolerate IM injection and patients who need prolonged vitamin B12 supplementation, such as patients with long-term metformin use and patients with pernicious anemia or with gastro-duodenal resection [51,52,53,54]. In terms of cost, the IM route is higher in cost than the SL and oral routes [2, 55].
We recommend future research directions to determine when to start with SL, IM, or oral vitamin B12 in different situations.
Implications in practice
As there is no apparent clinical significance, the treatment should depend on the patient’s condition. We advise physicians to examine every patient carefully to exclude every cause that may lead to malabsorption and then choose the most appropriate route. SL route could be used in patients with pernicious anemia or malabsorption causes. However, the oral route cannot be excluded as it did not depend on intrinsic factors only, as the simple diffusion (without the need for intrinsic factors) is now considered another mechanism for the absorption of vitamin B12 [49, 50].
Before this meta-analysis, the IM route was generally the preferred route, but our results showed that no route is usually preferred, and SL and oral routes should be considered comparable alternative routes.
Strength points and limitations
Based on our knowledge, this is the most updated meta-analysis on this topic, including all available evidence based on our inclusion criteria of including only controlled studies, either RCTs or controlled observational studies, to reach the highest accessible quality of evidence from the available evidence found in the literature. We are the first meta-analysis comparing the different administration routes of vitamin B12, and the first meta-analysis includes the SL route of administration in the analysis.
The limitations of this work are that we included RCTs, non-RCTs, and observational studies, which may lower the overall quality of evidence of the included studies. We cannot find the full text of one study which seems to be included. The head-by-head comparison between the three interventions was made only in one paper of the included studies. Additionally, there was variability between the included studies in the follow-up duration, which may cause heterogeneity in the results obtained.
Conclusion
All IM, oral, and SL routes of administration of vitamin B12 can effectively increase the level of vitamin B12 without significant differences between them, as thought previously. However, the IM route was the top-ranked statistically, followed by the SL and then the oral routes, but without clinical significance. We found no significant difference among studied administrated routes in all other CBC parameters such as Hb, MCV, platelets count, WBC count, and homocysteine level.
Availability of data and materials
The datasets used and/or analyzed during the current study are available as MS Excel files (.xlsx) and RevMan file (.rm5) from the corresponding author upon reasonable request.
References
Hunt A, Harrington D, Robinson S (2014) Vitamin B12 deficiency. BMJ (Online) 349. https://doi.org/10.1136/bmj.g5226
Stabler SP (2013) Clinical practice. Vitamin B12 deficiency. N Engl J Med 368. https://doi.org/10.1056/NEJMcp1113996
Carmel R (2000) Current concepts in cobalamin deficiency. Annu Rev Med 51. https://doi.org/10.1146/annurev.med.51.1.357
Green R, Allen LH, Bjørke-Monsen AL et al (2017) Vitamin B12 deficiency. Nat Rev Dis Primers 3. https://doi.org/10.1038/nrdp.2017.40
Langan RC, Zawistoski KJ (2011) Update on vitamin B12 deficiency. Am Fam Physician 83
Langan RC, Goodbred AJ (2017) Vitamin B12 deficiency: recognition and management. Am Fam Physician 96. https://doi.org/10.1097/00129300-200206000-00001
Parul Sahni (2021) The screening and treatment of vitamin B12 deficiency. Int Healthc Res J 5. https://doi.org/10.26440/ihrj/0504.07439
Bulut EA, Soysal P, Aydin AE et al (2017) Vitamin B12 deficiency might be related to sarcopenia in older adults. Exp Gerontol 95. https://doi.org/10.1016/j.exger.2017.05.017
Wang H, Li L, Qin LL et al (2018) Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency. Cochrane Database Syst Rev 2018. https://doi.org/10.1002/14651858.CD004655.pub3
Sanz-Cuesta T, Escortell-Mayor E, Cura-Gonzalez I et al (2020) Oral versus intramuscular administration of vitamin B12 for vitamin B12 deficiency in primary care: a pragmatic, randomized, non-inferiority clinical trial (OB12). BMJ Open 10. https://doi.org/10.1136/bmjopen-2019-033687
Gramer G, Hoffmann GF (2020) Vitamin B12 deficiency in newborns and their mothers—novel approaches to early detection, treatment and prevention of a global health issue. Curr Med Sci 40. https://doi.org/10.1007/s11596-020-2260-7
Carmel R (2008) How I treat cobalamin (vitamin B12) deficiency. Blood 112. https://doi.org/10.1182/blood-2008-03-040253
Devalia V, Hamilton MS, Molloy AM (2014) Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Br J Haematol 166. https://doi.org/10.1111/bjh.12959
Bensky MJ, Ayalon-Dangur I, Ayalon-Dangur R et al (2019) comparison of sublingual vs. intramuscular administration of vitamin B12 for the treatment of patients with vitamin B12 deficiency. Drug Deliv Transl Res 9. https://doi.org/10.1007/s13346-018-00613-y
Parry Strong A, Haeusler S, Weatherall M, Krebs J (2016) Sublingual vitamin B12 compared to intramuscular injection in patients with type 2 diabetes treated with metformin: a randomized trial. N Z Med J 129
Kotilea K, Quennery S, Decroës V, Hermans DA (2014) Successful sublingual cobalamin treatment in a child with short-bowel syndrome. J Pediatr Pharmacol Ther 19. https://doi.org/10.5863/1551-6776-19.1.60
Page MJ, McKenzie JE, Bossuyt PM et al (2020) statement: an updated guideline for reporting systematic reviews. BMJ 2021:372. https://doi.org/10.1136/bmj.n71
Higgins JPT, Thomas J, Chandler J et al (2021) Cochrane handbook for systematic reviews of interventions version 6.2
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomized trials. BMJ 366. https://doi.org/10.1136/bmj.l4898
Wells G, Shea B, O’Connell D et al (2004) The Newcastle–Ottawa Scale (NOQAS) for assessing the quality of non-randomized studies in meta-analysis. The Ottawa Hospital
Sterne JA, Hernán MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ (Online) 355. https://doi.org/10.1136/bmj.i4919
Higgins JPT, Jackson D, Barrett JK et al (2012) Consistency and inconsistency in network meta‐analysis: concepts and models for multi‐arm studies. Res Synth Methods 3. https://doi.org/10.1002/jrsm.1044
Chaimani A, Higgins JPT, Mavridis D et al (2013) Graphical tools for network meta-analysis in STATA. PLoS One 8. https://doi.org/10.1371/journal.pone.0076654
Soares MO, Dumville JC, Ades AE, Welton NJ (2014) Treatment comparisons for decision making: facing the problems of sparse and few data. J R Stat Soc Ser A Stat Soc 177. https://doi.org/10.1111/rssa.12010
Adachi S, Kawamoto T, Otsuka M et al (2000) Enteral vitamin B 12 supplements reverse postgastrectomy B 12 deficiency
Bensky MJ, Ayalon-Dangur I, Ayalon-Dangur R et al (2019) comparison of sublingual vs. intramuscular administration of vitamin B12 for the treatment of patients with vitamin B12 deficiency. Drug Deliv Transl Res 9:625–30. https://doi.org/10.1007/s13346-018-00613-y
Bolaman Z, Kadikoylu G, Yukselen V (2003) Oral versus intramuscular cobalamin treatment in megaloblastic anemia: a single-center, prospective, randomized, open-label study. 25
Castelli MC, Friedman K, Sherry J et al (2011) Comparing the efficacy and tolerability of a new daily oral vitamin B12 formulation and intermittent intramuscular vitamin B12 in normalizing low cobalamin levels: a randomized, open-label, parallel-group study. Clin Ther 33. https://doi.org/10.1016/j.clinthera.2011.03.003
Kuzminski AM, del Giacco EJ, Allen RH et al (1998) Effective treatment of cobalamin deficiency with oral cobalamin. Blood 92:1191–1198. https://doi.org/10.1182/blood.v92.4.1191.416k15_1191_1198
Metaxas C, Mathis D, Jeger C et al (2017) Early biomarker response and patient preferences to oral and intramuscular Vitamin B12 substitution in primary care: a randomized parallel-group trial. Swiss Med Wkly 147. https://doi.org/10.4414/smw.2017.14421
Orhan Kiliç B, Kiliç S, Şahin Eroğlu E et al (2021) Sublingual methylcobalamin treatment is as effective as intramuscular and peroral cyanocobalamin in children age 0–3 years. Hematology (United Kingdom) 26:1013–1017. https://doi.org/10.1080/16078454.2021.2010877
Schijns W, Homan J, van der Meer L et al (2018) efficacy of oral compared with intramuscular vitamin B-12 supplementation after Roux-en-Y gastric bypass: a randomized controlled trial. Am J Clin Nutr 108:6–12. https://doi.org/10.1093/ajcn/nqy072
Sezer RG, Akoğlu HA, Bozaykut A, Özdemir GN (2018) Comparison of the efficacy of parenteral and oral treatment for nutritional vitamin B12 deficiency in children. Hematology 23:653–657. https://doi.org/10.1080/10245332.2018.1456023
Sharabi A, Cohen E, Sulkes J, Garty M (2003) Replacement therapy for vitamin B12 deficiency: comparison between the sublingual and oral route. Br J Clin Pharmacol 56:635–638. https://doi.org/10.1046/j.1365-2125.2003.01907.x
Strong AP, Haeusler S, Weatherall M, Krebs J (2016) Sublingual vitamin B12 compared to intramuscular injection in patients with type 2 diabetes treated with metformin: a randomized trial. NZMJ 10:1436
Tuğba-Kartal A, Çağla-Mutlu Z (2020) Comparison of sublingual and intramuscular administration of vitamin B12 for the treatment of vitamin B12 deficiency in children. Rev Invest Clin 72:380–5. https://doi.org/10.24875/RIC.20000208
Patel P, Makwana S, Jobanputra U et al (2011) Sublingual route for the systemic delivery of ondansetron. Int J Drug Dev Res 3
Narang N, Sharma J (2011) Sublingual mucosa as a route for systemic drug delivery. Int J Pharm Pharm Sci 3
Singh M, Chitranshi N, Singh AP et al (2012) An overview on fast disintegrating sublingual tablets. Int J Drug Deliv 4
Pawar PP, Ghorpade HS, Kokane BA (2018) Sublingual route for systemic drug delivery. J Drug Deliv Ther 8. https://doi.org/10.22270/jddt.v8i6-s.2097
Raj GM, Raveendran R (2019) Introduction to basics of pharmacology and toxicology: volume 1: general and molecular pharmacology: Principles of drug action. https://doi.org/10.1007/978-981-32-9779-1
Kwatra S, Taneja G, Nasa N (2012) Alternative routes of drug administration- transdermal, pulmonary & parenteral. Indo Global J Pharm Sci 2
Saxen MA (2016) Pharmacologic management of patient behavior. McDonald and Avery’s Dentistry for the Child and Adolescent: Tenth Edition. https://doi.org/10.1016/B978-0-323-28745-6.00017-X
Polania Gutierrez JJ, Munakomi S (2022) Intramuscular injection. StatPearls, Treasure Island (FL): StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC
Sisson H (2015) Aspirating during the intramuscular injection procedure: a systematic literature review. J Clin Nurs 24. https://doi.org/10.1111/jocn.12824
Una Hopkins, RN, FNP-BC D et al (2013) Large-volume IM injections: a review of best practices. Oncol Nurse Advis IM
Talevi A, Quiroga PAM (2018) ADME Processes in Pharmaceutical Sciences (Dosage, Design, and Pharmacotherapy Success). Routes of Drug Administration Chapter 6
Giovannitti JA, Trapp LD (1991) Adult sedation: oral, rectal, IM, IV. Anesth Prog 38
Berlin R, Berlin H, Brante G, Pilbrant Å (1978) Vitamin B12 body stores during oral and parenteral treatment of pernicious anaemia. Acta Med Scand 204. https://doi.org/10.1111/j.0954-6820.1978.tb08402.x
Berlin H, Berlin R, Brante G (1968) Oral treatment of pernicious anemia with high doses of vitamin B12 without intrinsic factor. Acta Med Scand 184. https://doi.org/10.1111/j.0954-6820.1968.tb02452.x
Chapman LE, Darling AL, Brown JE (2016) Association between metformin and vitamin B12 deficiency in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Metab 42. https://doi.org/10.1016/j.diabet.2016.03.008
Chapman LE, Darling AL, Brown JE (2015) The association between the biguanide drug metformin and vitamin B 12 deficiency in diabetic patients: a systematic review. Proceedings of the Nutrition Society 74. https://doi.org/10.1017/s0029665115001433
Kornerup LS, Hvas CL, Abild CB (2019) Early changes in vitamin B12 uptake and biomarker status following Roux-en-Y gastric bypass and sleeve gastrectomy. Clin Nutr 38. https://doi.org/10.1016/j.clnu.2018.02.007
Lenti MV, Rugge M, Lahner E et al (2020) Autoimmune gastritis. Nat Rev Dis Primers 6. https://doi.org/10.1038/s41572-020-0187-8
Vidal-Alaball J, Butler CC, Potter CC (2006) Comparing costs of intramuscular and oral vitamin B12 administration in primary care: a cost-minimization analysis. Eur J Gen Pract 12. https://doi.org/10.1080/14017430601049449
Berlin R, Berlin H, Brante G, Pilbrant Å (1978) Vitamin B12 body stores during oral and parenteral treatment of pernicious anaemia. Acta Med Scand 204:81–84. https://doi.org/10.1111/J.0954-6820.1978.TB08402.X
Berlin H, Berlin R, Brante G (1968) ORAL Treatment of pernicious anemia with high doses of vitamin B12 without intrinsic factor. Acta Med Scand 184:247–258. https://doi.org/10.1111/J.0954-6820.1968.TB02452.X
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. SD, AK, TE, and TF did the screening, data extraction and quality assessment of the included studies. AA and RAD prepare the analysis plan, apply this plan, and write the results. OAA and AN wrote the whole manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Protocol registration
The protocol of this study was not registered.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelwahab, O.A., Abdelaziz, A., Diab, S. et al. Efficacy of different routes of vitamin B12 supplementation for the treatment of patients with vitamin B12 deficiency: A systematic review and network meta-analysis. Ir J Med Sci 193, 1621–1639 (2024). https://doi.org/10.1007/s11845-023-03602-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-023-03602-4