Abstract
Background
Plasmodium falciparum resistance to chloroquine (CQ) and sulfadoxine-pyrimethamine (SP) has historically posed a major threat to malaria control throughout the world. The country of Angola officially replaced CQ with artemisinin-based combination therapy (ACT) as a first-line treatment in 2006, but malaria cases and deaths have recently been rising. Many classic resistance mutations are relevant for the efficacy of currently available drugs, making it important to continue monitoring their frequency in Angola.
Methods
Plasmodium falciparum DNA was sampled from the blood of 50 hospital patients in Cabinda, Angola from October-December of 2018. Each infection was genotyped for 13 alleles in the genes crt, mdr1, dhps, dhfr, and kelch13, which are collectively involved in resistance to six common anti-malarials. To compare frequency patterns over time, P. falciparum genotype data were also collated from studies published from across Angola in the last two decades.
Results
The two most important alleles for CQ resistance, crt 76T and mdr1 86Y, were found at respective frequencies of 71.4% and 6.5%. Historical data suggest that mdr1 N86 has been steadily replacing 86Y throughout Angola in the last decade, while the frequency of crt 76T has been more variable across studies. Over a third of new samples from Cabinda were ‘quintuple mutants’ for SP resistance in dhfr/dhps, with a sixth mutation at dhps A581G present at 9.6% frequency. The markers dhfr 51I, dhfr 108N, and dhps 437G have been nearly fixed in Angola since the early 2000s, whereas dhfr 59R may have risen to high frequency more recently. Finally, no non-synonymous polymorphisms were detected in kelch13, which is involved in artemisinin resistance in Southeast Asia.
Conclusions
Genetic markers of P. falciparum resistance to CQ are likely declining in frequency in Angola, consistent with the official discontinuation of CQ in 2006. The high frequency of multiple genetic markers of SP resistance is consistent with the continued public and private use of SP. In the future, more complete haplotype data from mdr1, dhfr, and dhps will be critical for understanding the changing efficacy of multiple anti-malarial drugs. These data can be used to support effective drug policy decisions in Angola.
Similar content being viewed by others
Background
Anti-malarial drugs have long been important tools for malaria control [1]. However, their efficacy is constantly threatened by the evolution of drug resistance in Plasmodium falciparum [2]. Multiple P. falciparum genes are involved in drug resistance, and selection of them varies by allele, genetic background, and drug environment [3,4,5]. Therefore, frequent monitoring of resistance alleles is crucial to predicting the spread of drug resistance. This is especially true in the West African country of Angola, where malaria cases and deaths are on the rise [6].
The first anti-malarial drug to enjoy widespread use in Angola was chloroquine (CQ) in the 1950s [7]. CQ resistance was first confirmed in Angola in the 1980s, and by the early 2000s, CQ failure rates exceeded 80% [8, 9]. As a result, CQ was discontinued in Angola in favour of artemisinin-based combination therapy (ACT) starting in 2006 [6]. To discourage the evolution of artemisinin resistance, artemisinin is used in combination with the longer-acting partner drugs lumefantrine or amodiaquine, which is chemically related to CQ [10]. Artemisinin resistance has not yet appeared in Angola, although many partially resistant kelch13 mutations have emerged in Southeast Asia [5, 11]. Nonetheless, occasional ACT failures have been reported in Angola that could be due to partner drug resistance [6, 12].
Strong P. falciparum resistance to CQ and amodiaquine is caused by crt 76T, a lysine to threonine substitution at codon 76 of the chloroquine resistance transporter (Table 1). A meta-analysis found this allele to be 7.2-fold overrepresented in CQ treatment failures [13], reflecting its selection by CQ and amodiaquine in many clinical studies (Table 1). In Angola, 76T is typically found on the haplotype crt 72–76 CVIET, which is of Asian origin [14]. CQ resistance has also evolved independently through the haplotype crt 72–76 SVMNT in South America and Papua New Guinea [15].
The 86Y allele of mdr1, or multidrug resistance gene 1, also confers resistance to CQ and amodiaquine [13]. Although this specific polymorphism dominated early studies of mdr1 and CQ resistance, the evolution of mdr1 is complicated by linkage between position 86 and other functional polymorphisms [16]. Precise mdr1 haplotypes vary among P. falciparum populations and drug settings, but in Angola alone, at least six alleles at three mdr1 positions have been proposed to modulate resistance to CQ, amodiaquine, and lumefantrine (Table 1, Additional file 1: Table S1).
The drug sulfadoxine-pyrimethamine (SP) has also been in widespread use in many African countries since the 1960s [17]. Plasmodium falciparum quickly began evolving partial resistance to SP, mediated by numerous substitutions in dhps and dhfr [18]. The risk of SP treatment failure increases with the number of mutant alleles present, with “quintuple mutants” at codons 437/540 of dhps and codons 51/59/108 of dhfr of particular concern [19,20,21]. By the early 2000s, these alleles were common in Angola and 25–39% of P. falciparum infections failed to respond to SP treatment [9]. SP has since been discontinued as a first-line therapy in Angola, but it is still available at private pharmacies [22], where it comprised 10–40% of all anti-malarial sales in Huambo between 2009 and 2013 [23]. Intermittent, preventative SP is also recommended for pregnant women in Angola [24], although data from 2015 to 2016 indicate that only 30–40% of pregnant women actually received it during prenatal visits [25]. In other African countries, additional dhps mutations are emerging that appear to threaten the efficacy of SP treatment [26, 27]. It is, therefore, critical to continue monitoring genetic variation in dhfr and dhps.
In this work, 50 P. falciparum infections from Cabinda, Angola were genotyped for 13 markers of drug resistance in the genes crt, mdr1, dhps, dhfr, and kelch13. Similar data were also gathered from studies published on Angolan P. falciparum in the last two decades. For every gene but kelch13, the observed temporal patterns of allele frequency change are consistent with the current usage and availability of anti-malarial drugs. This work can inform future decisions on drug administration in Angola.
Methods
Sample collection and ethics statement
Patients reporting to the Hospital Regional de Cabinda between October and December 2018 with fever, chills, or other malaria symptoms were offered the option to be consented to this study. Sample collection followed protocols approved by Stanford University (IRB #39149) and the Medical Ethics Committee of the University 11th of November in Cabinda. In all, 8 children under 5 years, 14 children under 18 years, and 28 adults between 18 and 55 years were consented to participate. Participants’ blood was drawn from a vein and screened under a microscope for P. falciparum parasites. Parasitaemia was determined for adult participants and ranged from 1,787–35,424 (mean: 13,617) parasites/uL. All positive, whole blood samples were filtered through cellulose columns to remove leukocytes [28], and the filtered red blood cells were spotted on Whatman FTA cards (Sigma Aldrich), dried, and stored for at least 6 months.
DNA extraction and genotyping
To elute DNA, saturated circles were cut out of the Whatman FTA cards and incubated in 800 uL TE buffer (10 mM Tris–Cl, 1 mM EDTA, pH 8.0) with 20 uL Proteinase K (Invitrogen) for 2 h at 65 °C. DNA was extracted from the liquid supernatant using a phenol–chloroform protocol with phase-lock gel tubes [29].
PCR amplification of the P. falciparum genes crt, mdr1, dhfr, dphs, and kelch13 was performed with previously published primers [30,31,32]. Cycling protocols were based on manufacturer recommendations for OneTaq Hot Start 2X Master Mix (NEB) and/or Phusion High-Fidelity PCR Master Mix with HF Buffer (NEB) (Additional file 2: Table S2). Reactions were visualized in 1% agarose gels, and if successful, cleaned with ExoSAP-IT (ThermoFisher) and Sanger sequenced (Elim Bio). Sanger chromatogram data were compared to PlasmoDB reference P. falciparum sequences using Benchling. Analysis was focused on amino acid substitutions in the following positions: mdr1 N86Y, Y184F, and D1246Y; crt CMNVK 72–76 CVIET; dhfr C50G, N51I, C59R, and S108N; dhps S436A, A437G, K540E, and A581E. For kelch13, the entire amplified fragment spanning codons 389–649 was examined for polymorphisms.
Mixed infections and allele frequency calculations
For each sample, a mixed infection was inferred if the sequencing chromatogram showed equally sized, double peaks for any of the 13 analysed loci. The frequency of each allele was determined based on the total number of infections, with single infections contributing one genotype and mixed infections contributing two. These calculations are available in Additional file 5: Table S5. The 43 samples without missing data at dhfr or dhps were also assessed for the presence of seven SP-resistance alleles (dhfr-51I, dhfr-59R, dhfr-108N, dhps-436A, dhps-437G, dhps-540E, dhps-581G) [33, 34].
Collection of historical data
Publications reporting the prevalence of drug-resistance loci anywhere in Angola since 1995 were gathered from a recent review [7] and from the Worldwide Antimalarial Resistance Network (WWARN) Molecular Surveyor tool (http://www.wwarn.org/molecularsurveyor/). To avoid biases imposed by drug selection, studies were excluded if they selected samples for genotyping based on later treatment failure. In cases where details on mixed infections were provided, the original data were used to calculate allele frequencies as described above; other cases were treated as having 0 mixed infections. These calculations are available in Additional file 5: Table S5.
Results
Genotyping success and mixed infections
Each sample was successfully genotyped at an average of 12 out of 13 loci (Additional file 3: Table S3). The kelch13 locus had the highest success rate (100%), while crt had the lowest success rate (78%). The crt primers used here have performed well on other Angolan samples [30], but in this cohort, even the nested protocol amplified products of multiple sizes (Additional file 6: Fig. S1). Fifteen of 50 samples had sequence diversity (i.e., peaks of two bases) in at least one resistance marker site, indicating the presence of at least two genetically distinct strains.
Very little polymorphism in kelch13
Across the amplified kelch13 fragment, which spanned codons 389–649, only one synonymous polymorphism (R471R) was observed in one sample. No kelch13 polymorphisms were observed at any sequenced codons that have been linked to delayed parasite clearance in the presence of artemisinin by a recent meta-analysis by the Worldwide Antimalarial Resistance Network (WWARN) [35].
Markers of CQ resistance in crt and mdr1
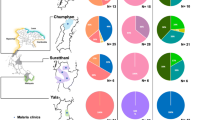
The crt 72–76 CVIET haplotype, which confers strong resistance to CQ, was detected in 73% of single isolates in this study (Table 2). Using a definition of allele frequency that incorporates mixed isolates (Methods; Additional file 5: Table S5), 76T was estimated to occur at 70.7% frequency in Cabinda in 2018 (Table 3). In contrast, earlier data from four other Angolan provinces collected between 2004 and 2011 indicated 76T at 89–97% frequency (Table 3). Later studies of Chinese migrant workers, sampled from unspecified locations within Angola in 2013 and 2014, estimated the frequency of 76T to be between 30 and 44%. Overall, despite appreciable variation across studies and sites, crt 76T appeared to be rarer in Angola in the 2010s than it was in the 2000s (Table 3).
The mdr1 allele 86Y, which also confers resistance to CQ, was detected in just 7.8% of single infections in Cabinda in 2018 (Table 2) and had an allele frequency of 6.5% when also considering mixed infections (Table 4). Accordingly, the alternate allele N86—which is associated with both CQ-sensitivity and artemether-lumefantrine (AL) treatment failure (Table 1)—had an allele frequency of 93.5% (Table 4). The linked polymorphism mdr1 184F was present at 44.0% frequency (Table 4). These estimates are substantially higher than those from all other studies conducted in Angola in the last 15 years (Table 4), which together suggest an increase of N86 and perhaps 184F across multiple sites over time. A single isolate from Cabinda in 2018 also contained the additional CQ-resistance allele mdr1 1246Y (Table 1), which occurred on an 86Y/Y184 background (Table 2).
Multiple markers of SP resistance are common in Angola
Over one third (37.5%) of P. falciparum isolates sampled here were “quintuple mutants” for five dhfr and dhps alleles that confer strong SP resistance (IRNSGEA, Table 2). For comparison, this haplotype was not observed among 66 samples collected in Uíge in 2004 [36], and was present in only 11.6% of samples from migrant workers collected between 2013–2016 [37]. A different set of five markers (IRNAGKA) was found in 15.6% of isolates in this study, while 43.7% contained four markers (IRNSGKA or ICNAGKA). No infection contained three or fewer markers (Table 2). One single infection contained six markers (IRNAGKG), as did two mixed infections (Additional file 3: Table S3); however, the 436A allele present on these haplotypes is considered less important for SP resistance than 540E [34], which was observed only in the canonical “quintuple” mutant (Table 2).
It was not straightforward to compare the prevalence of dhfr and dhps haplotypes across studies, due to inconsistencies in which amino acids were reported; how missing data were treated; and the relatively common practice of reporting dhfr and dhps haplotypes separately (Table 5; Additional file 4: Table S4). With these caveats, however, it was possible to examine the frequencies of individual amino acid variants in Angola over time (Table 5). Almost every study conducted between 2004 and 2018 found the mutant alleles dhfr 51I, dhfr 108N, and dhps 437G at high frequencies (85–99%, Table 5), consistent with constant selective pressure from continued use of SP. The mutant alleles dhfr 59R, dhps 581G, and especially dhps 540E were also detected at their highest frequencies within the most recent sample from Cabinda. However, only the data for dhfr 59R were consistent with the steady rise of the mutant allele over time in multiple parts of the country (Table 5).
Discussion
Discontinuation of CQ in several African countries including Malawi, the Gambia, Kenya, Ethiopia, Tanzania, and Grand Comore has led to major declines of crt 76T [38,39,40,41,42,43], the most important allele for CQ resistance in P. falciparum. Six studies conducted in Angola since 2010 similarly found reduced frequencies of crt 76T compared to the early 2000s (Table 3). However, precise frequency estimates have ranged widely among studies (30–89%, Table 3), perhaps because of local differences in anti-malarial use or parasite diversity. CQ is still available in some Angolan pharmacies, although it comprised fewer than 1% of sales in Huambo between 2009 and 2013 [23]. Another important source of selection could be the ACT partner drug amodiaquine (Table 1), which is found in one of two artemisinin-based combinations currently implemented in Angola. More information on anti-malarial drug usage across the country, as well as continued genetic monitoring of P. falciparum, will be useful for understanding the evolution of crt in Angola.
Discontinuation of CQ in Grand Comore and the Gambia also preceded the decline of mdr1 86Y [38, 40], the second most important allele for CQ resistance in P. falciparum. Several studies from across Angola are consistent with a steady decline of 86Y after 2007, with the exception of a 2011 household survey in Benguela (Table 4). One possible explanation for the faster loss of mdr1 86Y, as opposed to crt 76T, could be that mdr1 N86 or its linked alleles are involved in low-level lumefantrine resistance (Table 1; Table S1). Lumefantrine is a component of artemether-lumefantrine (AL), the most common ACT currently implemented in Angola [6, 44]. Since 2013, three large studies have reported that AL treatment efficacy in Zaire or Lunda Sul fell below the WHO standard of 90% [12, 45, 46]. These treatment failures have been interpreted as signs of decreased susceptibility to lumefantrine in the parasite population [12], although the genetic basis of lumefantrine resistance has yet to be conclusively demonstrated and could involve multiple loci. Further studies on the mechanisms of lumefantrine tolerance in P. falciparum will be key to enabling molecular monitoring in the future.
In contrast to markers of CQ resistance, markers of SP resistance have been on the rise in several African countries [40, 41, 47,48,49] where SP is used for malaria treatment and prevention. In Angola, the available data suggest a rapid increase in the prevalence of SP-resistant “quintuple mutants” in dhfr/dhps between 2004 (0%) [36], 2013–2016 (11.6%) [37], and 2018 (Table 2, 37.5%). This increase could be partially driven by the rise of one particular marker, dhfr 59R (Table 5), although dhfr/dhps genetic diversity may also vary among sites [50]. In Angola, it is likely that unregulated consumer use of SP [22, 23] and use of SP for intermittent preventive treatment in pregnancy [51] are sources of selection for SP resistance. This situation should continue to be monitored closely to avoid the eventual loss of important SP benefits during pregnancy [27, 52]. In the future, complete reporting of haplotype information for all combined dhfr/dhps alleles in each P. falciparum infection (e.g. Additional file 3: Table S3) will help accomplish this goal.
These interpretations of allele frequency change in Angola over time are subject to a number of limitations. First, the historical data were drawn from studies conducted in several geographical locations across Angola (Tables 3, 4, 5; Additional file 4: Table S4). Because provinces vary in patterns of malaria transmission [6] and anti-malarial availability [22, 23], selection on resistance alleles is not expected to be uniform across the entire country. Second, each study varied in its sampling and many also varied in their reporting of mixed infections (Tables 3, 4, 5; Additional file 4: Table S4), which has the potential to reduce or inflate estimates of mutant allele frequencies. Third, several studies (including this one) provide data for a relatively limited number of subjects, which may also lead to biases in allele frequency estimates. Despite these limitations, however, the apparent trends of drug resistance alleles over time (Tables 3, 4, 5) are consistent with the common usage of ACT and SP and discontinuation of CQ across Angola since the mid-2000s.
Finally, we detected no signs of alleles in kelch13 that confer partial resistance to artemisinin. This result is consistent with the lack of evidence in Africa for the spread of alleles that diminish ACT efficacy, although some countries have recently reported the presence of validated markers [53]. Continued monitoring of kelch13 in Africa is important, as artemisinin remains the cornerstone of anti-malarial drug policy in many countries.
Conclusions
Multiple drug resistance alleles in Angolan P. falciparum have experienced changes in frequency since CQ was officially discontinued in 2006. Markers of resistance to CQ appear to be declining, but markers of strong SP resistance and potential low-level lumefantrine resistance are rising. Continued monitoring and drug policy adjustments will be necessary in the future to regain control of P. falciparum malaria in Angola.
Availability of data and material
The new P. falciparum genotype data presented here may be found in Supplementary Table 3.
References
Butler A, Khan S, Ferguson E. A brief history of malaria chemotherapy. J R Coll Physicians Edinb. 2010;40:172–7.
Haldar K, Bhattacharjee S, Safeukui I. Drug resistance in Plasmodium. Nat Rev Microbiol. 2018;16:156–70.
Gabryszewski SJ, Modchang C, Musset L, Chookajorn T, Fidock DA. Combinatorial genetic modeling of pfcrt-mediated drug resistance evolution in Plasmodium falciparum. Mol Biol Evol. 2016;33:1554–70.
Veiga MI, Dhingra SK, Henrich PP, Straimer J, Gnädig N, Uhlemann AC, et al. Globally prevalent PfMDR1 mutations modulate Plasmodium falciparum susceptibility to artemisinin-based combination therapies. Nat Commun. 2016;7:1–12.
Woodrow CJ, White NJ. The clinical impact of artemisinin resistance in Southeast Asia and the potential for future spread. FEMS Microbiol Rev. 2017;41:34–48.
WHO. Angola African Region. In: World Malaria Report 2018. Geneva, World Health Organization. 2018. https://www.who.int/malaria/publications/country-profiles/profile_ago_en.pdf. Accessed 8 Aug 2020.
Fançony C, Brito M, Gil JP. Plasmodium falciparum drug resistance in Angola. Malar J. 2016;15:74.
Vestergaard Olsen V, Jensen T, Jorgensen M. Chloroquine-resistant Plasmodium falciparum malaria from Angola. Lancet. 1984;323:1462–3.
Guthmann JP, Ampuero J, Fortes F, van Overmeir C, Gaboulaud V, Tobback S, et al. Antimalarial efficacy of chloroquine, amodiaquine, sulfadoxine-pyrimethamine, and the combinations of amodiaquine + artesunate and sulfadoxine-pyrimethamine + artesunate in Huambo and Bié provinces, central Angola. Trans R Soc Trop Med Hyg. 2005;99:485–92.
Marquez VE, Cranston JW, Ruddon RW, Kier LB, Burckhalter JH. Mechanism of action of amodiaquine synthesis of its indoloquinoline analog. J Med Chem. 1972;15:36–9.
Fairhurst RM. Understanding artemisinin-resistant malaria: What a difference a year makes. Curr Opin Infect Dis. 2015;28:417–25.
Dimbu PR, Horth R, Cândido ALM, Ferreira CM, Caquece F, Garcia LEA, et al. Continued low efficacy of artemether-lumefantrine in Angola in 2019. Antimicrob Agents Chemother. 2021;65:e01949-e2020.
Picot S, Olliaro P, De Monbrison F, Bienvenu AL, Price RN, Ringwald P. A systematic review and meta-analysis of evidence for correlation between molecular markers of parasite resistance and treatment outcome in falciparum malaria. Malar J. 2009;8:89.
Ariey F, Fandeur T, Durand R, Randrianarivelojosia M, Jambou R, Legrand E, et al. Invasion of Africa by a single pfcrt allele of South East Asian type. Malar J. 2006;5:34.
Wootton JC, Feng X, Ferdig MT, Cooper RA, Mu J, Baruch DI, et al. Genetic diversity and chloroquine selective sweeps in Plasmodium falciparum. Nature. 2002;418:320–3.
Sanchez CP, Mayer S, Nurhasanah A, Stein WD, Lanzer M. Genetic linkage analyses redefine the roles of PfCRT and PfMDR1 in drug accumulation and susceptibility in Plasmodium falciparum. Mol Microbiol. 2011;82:865–78.
Flegg JA, Metcalf CJE, Gharbi M, Venkatesan M, Shewchuk T, Sibley CH, et al. Trends in antimalarial drug use in Africa. Am J Trop Med Hyg. 2013;89:857–65.
Sibley CH, Hyde JE, Sims PFG, Plowe CV, Kublin JG, Mberu EK, et al. Pyrimethamine-sulfadoxine resistance in Plasmodium falciparum: What next? Trends Parasitol. 2001;17:582–8.
Staedke SG, Sendagire H, Lamola S, Kamya MR, Dorsey G, Rosenthal PJ. Relationship between age, molecular markers, and response to sulphadoxine-pyrimethamine treatment in Kampala. Uganda Trop Med Int Health. 2004;9:624–9.
Zhao L, Pi L, Qin Y, Lu Y, Zeng W, Xiang Z, et al. Widespread resistance mutations to sulfadoxine-pyrimethamine in malaria parasites imported to China from Central and Western Africa. Int J Parasitol Drugs Drug Resist. 2020;12:1–6.
Nzila AM, Mberu EK, Sulo J, Dayo H, Winstanley PA, Sibley CH, et al. Towards an understanding of the mechanism of pyrimethamine-sulfadoxine resistance in Plasmodium falciparum: genotyping of dihydrofolate reductase and dihydropteroate synthase of Kenyan parasites. Antimicrob Agents Chemother. 2000;44:991–6.
Muila M, Gazin P. Les médicaments antipaludiques disponibles dans la ville de Cabinda (Angola) en 2016. Bull la Soc Pathol Exot. 2017;110:260–4.
Lussiana C, Floridia M, Martinho Do Rosário J, Fortes F, Allan R. Impact of introducing subsidized combination treatment with artemether-lumefantrine on sales of anti-malarial monotherapies: a survey of private sector pharmacies in Huambo, Angola. Trans R Soc Trop Med Hyg. 2016;110:588–96.
WHO. Policy brief for the implementation of intermittent preventive treatment of malaria in pregnancy using sulfadoxine-pyrimethamine (IPTp-SP). Geneva, World Health Organization. 2014. https://www.who.int/malaria/publications/atoz/iptp-sp-updated-policy-brief-24jan2014.pdf. Accessed 22 Mar 2021.
Andrada A, Herrera S, Yé Y. Are new national malaria strategic plans informed by the previous ones? A comprehensive assessment of sub-Saharan African countries from 2001 to present. Malar J. 2019;18:253.
Spalding MD, Eyase FL, Akala HM, Bedno SA, Prigge ST, Coldren RL, et al. Increased prevalence of the pfdhfr/phdhps quintuple mutant and rapid emergence of pfdhps resistance mutations at codons 581 and 613 in Kisumu. Kenya Malar J. 2010;9:338.
Gesase S, Gosling RD, Hashim R, Ord R, Naldoo I, Madebe R, et al. High resistance of Plasmodium falciparum to sulphadoxine/pyrimethamine in Northern Tanzania and the emergence of dhps resistance mutation at codon 581. PLoS ONE. 2009;4:e4569.
Venkatesan M, Amaratunga C, Campino S, Auburn S, Koch O, Lim P, et al. Using CF11 cellulose columns to inexpensively and effectively remove human DNA from Plasmodium falciparum-infected whole blood samples. Malar J. 2012;11:41.
Mukhopadhyay T, Roth JA. Silicone lubricant enhances recovery of nucleic acids after phenol-chloroform extraction. Nucleic Acids Res. 1993;21:781–2.
Gama BE, Pereira-Carvalho GAL, Lutucuta Kosi FJI, Almeida De Oliveira NK, Fortes F, Rosenthal PJ, et al. Plasmodium falciparum isolates from Angola show the StctVMNT haplotype in the pfcrt gene. Malar J. 2010;9:174.
Talundzic E, Chenet SM, Goldman IF, Patel DS, Nelson JA, Plucinski MM, et al. Genetic analysis and species specific amplification of the artemisinin resistance-associated kelch propeller domain in P. falciparum and P. vivax. PLoS One. 2015;10:e0136099.
Gama BE, Pereira-Carvalho GAL, Lutucuta Kosi FJI, Almeida De Oliveira NK, Fortes F, Rosenthal PJ, et al. Molecular markers of antifolate resistance in Plasmodium falciparum isolates from Luanda, Angola. Malar J. 2011;10:248.
Wernsdorfer WH, Noedl H. Molecular markers for drug resistance in malaria: use in treatment, diagnosis and epidemiology. Curr Opin Infect Dis. 2003;16:553–8.
Gregson A, Plowe CV. Mechanisms of resistance of malaria parasites to antifolates. Pharmacol Rev. 2005;57:117–45.
Group WKG-PS. Association of mutations in the Plasmodium falciparum Kelch13 gene (Pf3D7_1343700) with parasite clearance rates after artemisinin-based treatments-a WWARN individual patient data meta-analysis. BMC Med. 2019;17:1.
Menegon M, Pearce RJ, Inojosa WO, Pisani V, Abel PM, Matondo A, et al. Monitoring for multidrug-resistant Plasmodium falciparum isolates and analysis of pyrimethamine resistance evolution in Uige province. Angola Trop Med Int Health. 2009;14:1251–7.
Xu C, Sun H, Wei Q, Li J, Xiao T, Kong X, et al. Mutation Profile of pfdhfr and pfdhps in Plasmodium falciparum among returned Chinese migrant workers from Africa. Antimicrob Agents Chemother. 2019;63:e01927-e2018.
Huang B, Wang Q, Deng C, Wang J, Yang T, Huang S, et al. Prevalence of crt and mdr-1 mutations in Plasmodium falciparum isolates from Grande Comore island after withdrawal of chloroquine. Malar J. 2016;15:414.
Kublin JG, Cortese JF, Njunju EM, G. Mukadam RA, Wirima JJ, Kazembe PN, et al. Reemergence of chloroquine-sensitive Plasmodium falciparum malaria after cessation of chloroquine Use in Malawi. J Infect Dis. 2003;187:1870–5.
Nwakanma DC, Duffy CW, Amambua-Ngwa A, Oriero EC, Bojang KA, Pinder M, et al. Changes in malaria parasite drug resistance in an endemic population over a 25-year period with resulting genomic evidence of selection. J Infect Dis. 2014;209:1126–35.
Mwai L, Ochong E, Abdirahman A, Kiara SM, Ward S, Kokwaro G, et al. Chloroquine resistance before and after its withdrawal in Kenya. Malar J. 2009;8:106.
Mekonnen SK, Aseffa A, Berhe N, Teklehaymanot T, Clouse RM, Gebru T, et al. Return of chloroquine-sensitive Plasmodium falciparum parasites and emergence of chloroquine-resistant Plasmodium vivax in Ethiopia. Malar J. 2014;13:244.
Mohammed A, Ndaro A, Kalinga A, Manjurano A, Mosha JF, Mosha DF, et al. Trends in chloroquine resistance marker, Pfcrt-K76T mutation ten years after chloroquine withdrawal in Tanzania. Malar J. 2013;12:415.
Manguin S, Foumane V, Besnard P, Fortes F, Carnevale P. Malaria overdiagnosis and subsequent overconsumption of antimalarial drugs in Angola: consequences and effects on human health. Acta Trop. 2017;171:58–63.
Plucinski MM, Dimbu PR, Macaia AP, Ferreira CM, Samutondo C, Quivinja J, et al. Efficacy of artemether–lumefantrine, artesunate–amodiaquine, and dihydroartemisinin–piperaquine for treatment of uncomplicated Plasmodium falciparum malaria in Angola. Malar J. 2017;16:62.
Plucinski MM, Talundzic E, Morton L, Dimbu PR, Macaia AP, Fortes F, et al. Efficacy of artemether-lumefantrine and dihydroartemisinin-piperaquine for treatment of uncomplicated malaria in children in Zaire and Uíge provinces. Angola Antimicrob Agents Chemother. 2015;59:437–43.
Hemming-Schroeder E, Umukoro E, Lo E, Fung B, Tomás-Domingo P, Zhou G, et al. Impacts of antimalarial drugs on Plasmodium falciparum drug resistance markers, Western Kenya, 2003–2015. Am J Trop Med Hyg. 2018;98:692–9.
Deutsch-Feldman M, Aydemir O, Carrel M, Brazeau NF, Bhatt S, Bailey JA, et al. The changing landscape of Plasmodium falciparum drug resistance in the Democratic Republic of Congo. BMC Infect Dis. 2019;19:872.
Mandoko PN, Rouvier F, Kakina LM, Mbongi DM, Latour C, Likwela JL, et al. Prevalence of Plasmodium falciparum parasites resistant to sulfadoxine/pyrimethamine in the Democratic Republic of the Congo: emergence of highly resistant pfdhfr/pfdhps alleles. J Antimicrob Chemother. 2018;73:2704–15.
Fortes F, Dimbu R, Figueiredo P, Neto Z, Do Rosário VE, Lopes D. Evaluation of prevalence’s of pfdhfr and pfdhps mutations in Angola. Malar J. 2011;10:22.
Aziken ME, Akubuo KK, Gharoro EP. Efficacy of intermittent preventive treatment with sulfadoxine-pyrimethamine on placental parasitemia in pregnant women in midwestern Nigeria. Int J Gynecol Obstet. 2011;112:30–3.
Harrington WE, Morrison R, Fried M, Duffy PE. Intermittent preventive treatment in pregnant women is associated with increased risk of severe malaria in their offspring. PLoS ONE. 2013;8:e56183.
WHO. World malaria report 2020: 20 years of global progress and challenges. Geneva, World Health Organization. https://apps.who.int/iris/rest/bitstreams/1321872/retrieve. Accessed 26 Mar 2021.
Figueiredo P, Benchimol C, Lopes D, Bernardino L, Do Rosário VE, Varandas L, et al. Prevalence of pfmdr1, pfcrt, pfdhfr and pfdhps mutations associated with drug resistance, in Luanda. Angola Malar J. 2008;7:236.
Fançony C, Gamboa D, Sebastião Y, Hallett R, Sutherland C, Sousa-Figueiredo JC, et al. Various pfcrt and pfmdr1 genotypes of Plasmodium falciparum cocirculate with P. malariae, P. ovale spp., and P. vivax in Northern Angola. Antimicrob Agents Chemother. 2012;56:5271–7.
Foumane Ngane V, Allico Djaman J, Culeux C, Piette N, Carnevale P, Besnard P, et al. Molecular epidemiology of drug-resistant Plasmodium falciparum in Benguela province, Angola. Malar J. 2015;14.
Lu F, Zhang M, Culleton RL, Xu S, Tang J, Zhou H, et al. Return of chloroquine sensitivity to Africa? Surveillance of African Plasmodium falciparum chloroquine resistance through malaria imported to China. Parasit Vectors. 2017;10:355.
Zhou RM, Zhang HW, Yang CY, Liu Y, Zhao YL, Li SH, et al. Molecular mutation profile of pfcrt in Plasmodium falciparum isolates imported from Africa in Henan province. Malar J. 2016;15:265.
Zhang T, Xu X, Jiang J, Yu C, Tian C, Li W. Surveillance of antimalarial resistance molecular markers in imported Plasmodium falciparum malaria cases in Anhui, China, 2012–2016. Am J Trop Med Hyg. 2018;98:1132–6.
Pinheiro L, Franco S, Adagu IS, Rosa R, Rosário VE, Warhurst DC. Presence of the double pfmdr1 mutation 86Tyr and 1246 Tyr in clones of a chloroquine-resistant west African isolate of Plasmodium falciparum. Acta Med Port. 2003;16:229–33.
Kiaco K, Teixeira J, Machado M, do Rosário V, Lopes D. Evaluation of artemether-lumefantrine efficacy in the treatment of uncomplicated malaria and its association with pfmdr1, pfatpase6 and K13-propeller polymorphisms in Luanda, Angola. Malar J. 2015;14:504.
Ljolje D, Dimbu PR, Kelley J, Goldman I, Nace D, Macaia A, et al. Prevalence of molecular markers of artemisinin and lumefantrine resistance among patients with uncomplicated Plasmodium falciparum malaria in three provinces in Angola, 2015. Malar J. 2018;17:84.
Pearce RJ, Pota H, Evehe M-SB, Bâ E-H, Mombo-Ngoma G, Malisa AL, et al. Multiple origins and regional dispersal of resistant dhps in African Plasmodium falciparum malaria. PLoS Med. 2009;6:e1000055.
Kaingona-Daniel EPS, Gomes LR, Gama BE, Almeida-De-Oliveira NK, Fortes F, Ménard D, et al. Low-grade sulfadoxine-pyrimethamine resistance in Plasmodium falciparum parasites from Lubango. Angola Malar J. 2016;15:309.
Acknowledgements
We are immensely grateful to the study participants and staff of the Hospital Regional de Cabinda. Logistic support in sample collection was provided by Dr. Maria das Dores Sungo and Dr. Francisco Casimiro Lubalo, Rector and Vice-Rector of the Faculty of Medicine, University 11th of November, Cabinda. Rachael Madison, Bàrbara Baro Sastre, Elizabeth Egan, and Bernard Kim provided assistance in preparing and testing sampling materials. We also thank two anonymous reviewers whose comments helped improve the manuscript.
Funding
This study was supported with grants from the Stanford Center for Computational, Evolutionary, and Human Genomics to S.B. and E.R.E.; an MRC award (MR/M01987X/1) to S.B.; and an NIH award (5R35GM118165-05) to D.A.P.
Author information
Authors and Affiliations
Contributions
ERE, DAP, and SB designed the study. FR and SB supervised the study. ERE collected data, analysed data, and wrote the manuscript. All authors have approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval for this study was obtained from Stanford University IRB (#39149) and the Medical Ethics Committee of the University 11th of November in Cabinda.
Consent for publication
Prior to participation, all study subjects and/or their parents consented in writing to the publication of study results in the scientific literature.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Evidence and references supporting summary in Table 1 (XLSX 11 KB)
Additional file 2
: Table S2. PCR primers and cycling conditions (XLSX 14 KB)
Additional file 3
: Table S3. Full genotype results from Cabinda for the 13 loci (XLSX 13 KB)
Additional file 4
: Table S4. Summary of 17 studies of P. falciparum drug resistance markers in Angola (XLSX 13 KB)
Additional file 5
: Table S5. Calculations of allele frequencies from published count data. Mixed infections, if reported, were considered to contribute two genotypes. If not reported, or insufficiently reported, zero mixed infections were assumed. The year indicates date of sampling (XLSX 19 KB)
Additional file 6
: Figure S1. PCR with published crt primers amplified multiple bands. The expected product was <100 bp. In some but not all cases, it was still possible to determine the sequence for amino acids 72-76 using these reactions (DOCX 439 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ebel, E.R., Reis, F., Petrov, D.A. et al. Historical trends and new surveillance of Plasmodium falciparum drug resistance markers in Angola. Malar J 20, 175 (2021). https://doi.org/10.1186/s12936-021-03713-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-021-03713-2