Abstract
Purpose of Review
The purpose of this review is to provide an up-to-date understanding regarding the literature on sarcopenia and inflammation as prognostic factors in the context of renal cell carcinoma (RCC).
Recent Findings
Sarcopenia is increasingly recognized as a prognostic factor in RCC. Emerging literature suggests monitoring quantity of muscle on successive imaging and examining muscle density may be additionally informative. Inflammation has prognostic ability in RCC and is also considered a key contributor to development and progression of both RCC and sarcopenia. Recent studies suggest these two prognostic factors together may provide additional prognostic ability when used in combination. Ongoing developments include quality control regarding sarcopenia research and imaging, improving understanding of muscle loss mechanisms, and enhancing clinical incorporation of sarcopenia via improving imaging analysis practicality (i.e., artificial intelligence) and feasible biomarkers.
Summary
Sarcopenia and systemic inflammation are complementary prognostic factors for adverse outcomes in patients with RCC. Further study on high-quality sarcopenia assessment standardization and expedited sarcopenia assessment is desired for eventual routine clinical incorporation of these prognostic factors.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet [Internet]. 2019;393:2636–46. https://doi.org/10.1016/S0140-6736(19)31138-9.
Law ML. Cancer cachexia: Pathophysiology and association with cancer-related pain. Front Pain Res (Lausanne) [Internet]. 2022;3:971295. https://doi.org/10.3389/fpain.2022.971295.
Williams GR, Chen Y, Kenzik KM, McDonald A, Shachar SS, Klepin HD, et al. Assessment of sarcopenia measures, survival, and disability in older adults before and after diagnosis with cancer. JAMA Netw Open [Internet]. 2020;3:e204783. https://doi.org/10.1001/jamanetworkopen.2020.4783.
Shachar SS, Williams GR, Muss HB, Nishijima TF. Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer [Internet]. 2016;57:58–67. https://doi.org/10.1016/j.ejca.2015.12.030.
Best TD, Roeland EJ, Horick NK, Van Seventer EE, El-Jawahri A, Troschel AS, et al. Muscle loss is associated with overall survival in patients with metastatic colorectal cancer independent of tumor mutational status and weight loss. Oncologist [Internet]. 2021;26:e963-70. https://doi.org/10.1002/onco.13774.
Nipp RD, Fuchs G, El-Jawahri A, Mario J, Troschel FM, Greer JA, et al. Sarcopenia is associated with quality of life and depression in patients with advanced cancer. Oncologist [Internet]. 2018;23:97–104. https://doi.org/10.1634/theoncologist.2017-0255.
Padala SA, Barsouk A, Thandra KC, Saginala K, Mohammed A, Vakiti A, et al. Epidemiology of renal cell carcinoma. World J Oncol [Internet]. 2020;11:79–87. https://doi.org/10.14740/wjon1279.
Seer. Cancer Stat facts: kidney and renal pelvis cancer. 2022.
Anjanappa M, Corden M, Green A, Roberts D, Hoskin P, McWilliam A, et al. Sarcopenia in cancer: risking more than muscle loss. Tech Innov Patient Support Radiat Oncol [Internet]. 2020;16:50–7. https://doi.org/10.1016/j.tipsro.2020.10.001.
Shi J, Wang K, Xiong Z, Yuan C, Wang C, Cao Q, et al. Impact of inflammation and immunotherapy in renal cell carcinoma. Oncol Lett Internet]. 2020;20:272. https://doi.org/10.3892/ol.2020.12135.
•• Higgins MI, Martini DJ, Patil DH, Nabavizadeh R, Steele S, Williams M, et al. Sarcopenia and modified Glasgow prognostic score predict postsurgical outcomes in localized renal cell carcinoma. Cancer [Internet]. 2021;127:1974–83. https://doi.org/10.1002/cncr.33462. Important paper highlights complex relationships between sarcopenia, malignancy, inflammation, and malnutrition. Critical findings for renal cell carcinoma showing improved prognostic ability when features are combined rather than examined in isolation.
Cawthon PM, Visser M, Arai H, Ávila-Funes JA, Barazzoni R, Bhasin S, et al. Defining terms commonly used in sarcopenia research: a glossary proposed by the global leadership in sarcopenia (GLIS) steering committee. Eur Geriatr Med [Internet]. 2022;13:1239–44. https://doi.org/10.1007/s41999-022-00706-5.
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing [Internet]. 2019;48:16–31. https://doi.org/10.1093/ageing/afy169.
Dodds RM, Roberts HC, Cooper C, Sayer AA. The epidemiology of sarcopenia. J Clin Densitom [Internet]. 2015;18:461–6. https://doi.org/10.1016/j.jocd.2015.04.012.
Surov A, Wienke A. Prevalence of sarcopenia in patients with solid tumors: a meta-analysis based on 81,814 patients. JPEN J Parenter Enteral Nutr [Internet]. 2022. https://doi.org/10.1002/jpen.2415.
Burg ML, Clifford TG, Bazargani ST, Lin-Brande M, Miranda G, Cai J, et al. Frailty as a predictor of complications after radical cystectomy: a prospective study of various preoperative assessments. Urol Oncol [Internet]. 2019;37:40–7. https://doi.org/10.1016/j.urolonc.2018.10.002.
Psutka SP, Carrasco A, Schmit GD, Moynagh MR. Sarcopenia in patients with bladder cancer undergoing radical cystectomy: impact on cancer‐specific and all‐cause mortality. Cancer [Internet]. Wiley Online Library; 2014; Available from: https://acsjournals.onlinelibrary.wiley.com/doi/abs/10.1002/cncr.28798.
Psutka SP, Boorjian SA, Moynagh MR, Schmit GD, Frank I, Carrasco A, et al. Mortality after radical cystectomy: impact of obesity versus adiposity after adjusting for skeletal muscle wasting. J Urol [Internet]. 2015;193:1507–13. https://doi.org/10.1016/j.juro.2014.11.088.
Psutka SP, Boorjian SA, Moynagh MR, Schmit GD, Costello BA, Thompson RH, et al. Decreased skeletal muscle mass is associated with an increased risk of mortality after radical nephrectomy for localized renal cell cancer. J Urol [Internet]. 2016;195:270–6. https://doi.org/10.1016/j.juro.2015.08.072.
Ibilibor C, Psutka SP, Herrera J, Rivero JR, Wang H, Farrell AM, et al. The association between sarcopenia and bladder cancer-specific mortality and all-cause mortality after radical cystectomy: a systematic review and meta-analysis. Arab J Urol [Internet]. Informa UK Limited. 2021;19:98–103. Available from. https://www.tandfonline.com/doi/abs/10.1080/2090598X.2021.1876289.
Walston JD. Sarcopenia in older adults. Curr Opin Rheumatol [Internet]. 2012;24:623–7. https://doi.org/10.1097/BOR.0b013e328358d59b.
Kim JW, Kim R, Choi H, Lee S-J, Bae G-U. Understanding of sarcopenia: from definition to therapeutic strategies. Arch Pharm Res [Internet]. 2021;44:876–89. https://doi.org/10.1007/s12272-021-01349-z.
Priego T, Martín AI, González-Hedström D, Granado M, López-Calderón A. Role of hormones in sarcopenia. Vitam Horm [Internet]. 2021;115:535–70. https://doi.org/10.1016/bs.vh.2020.12.021.
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol [Internet]. 2011;12:489–95. https://doi.org/10.1016/S1470-2045(10)70218-7.
Ni J, Zhang L. Cancer cachexia: definition, staging, and emerging treatments. Cancer Manag Res [Internet]. 2020;12:5597–605.
Li C-W, Yu K, Shyh-Chang N, Jiang Z, Liu T, Ma S, et al. Pathogenesis of sarcopenia and the relationship with fat mass: descriptive review. J Cachexia Sarcopenia Muscle [Internet]. 2022;13:781–94. https://doi.org/10.1002/jcsm.12901.
Steffl M, Bohannon RW, Sontakova L, Tufano JJ, Shiells K, Holmerova I. Relationship between sarcopenia and physical activity in older people: a systematic review and meta-analysis. Clin Interv Aging [Internet]. 2017;12:835–45. https://doi.org/10.2147/CIA.S132940.
Sieber CC. Malnutrition and sarcopenia. Aging Clin Exp Res [Internet]. 2019;31:793–8. https://doi.org/10.1007/s40520-019-01170-1.
• Williams GR, Dunne RF, Giri S, Shachar SS, Caan BJ. Sarcopenia in the older adult with cancer. J Clin Oncol [Internet]. 2021;39:2068–78. https://doi.org/10.1200/JCO.21.00102. Informative overview of sarcopenia in malignancy, how it is assessed, and what it means.
Williams GR, Rier HN, McDonald A, Shachar SS. Sarcopenia & aging in cancer. J Geriatr Oncol [Internet]. 2019;10:374–7. https://doi.org/10.1016/j.jgo.2018.10.009.
Kwon YN, Yoon SS. Sarcopenia: neurological point of view. J Bone Metab [Internet]. 2017;24:83–9. https://doi.org/10.11005/jbm.2017.24.2.83.
Vella C, Kravitz L. Sarcopenia: the mystery of muscle loss. IDEA Pers Trainer [Internet]. unm.edu; 2002;13:30–5. Available from. https://www.unm.edu/~lkravitz/Article%20folder/sarcopenia.html.
Dalle S, Rossmeislova L, Koppo K. The role of inflammation in age-related sarcopenia. Front Physiol [Internet]. 2017;8:1045. https://doi.org/10.3389/fphys.2017.01045.
Pan L, Xie W, Fu X, Lu W, Jin H, Lai J, et al. Inflammation and sarcopenia: a focus on circulating inflammatory cytokines. Exp Gerontol [Internet]. 2021;154:111544. https://doi.org/10.1016/j.exger.2021.111544.
Franceschi C, Bonafè M, Valensin S, Olivieri F, De Luca M, Ottaviani E, et al. Inflamm-aging. An evolutionary perspective on immunosenescence. Ann N Y Acad Sci Internet. 2000;908:244–54. https://doi.org/10.1111/j.1749-6632.2000.tb06651.x.
Liang Z, Zhang T, Liu H, Li Z, Peng L, Wang C, et al. Inflammaging: the ground for sarcopenia? Exp Gerontol [Internet]. Elsevier; 2022;168:111931. https://doi.org/10.1016/j.exger.2022.111931.
Beyer I, Mets T, Bautmans I. Chronic low-grade inflammation and age-related sarcopenia. Curr Opin Clin Nutr Metab Care [Internet]. 2012;15:12–22. https://doi.org/10.1097/MCO.0b013e32834dd297.
Li C-W, Yu K, Shyh-Chang N, Li G-X, Jiang L-J, Yu S-L, et al. Circulating factors associated with sarcopenia during ageing and after intensive lifestyle intervention. J Cachexia Sarcopenia Muscle [Internet]. Wiley Online Library; 2019;10:586–600. https://doi.org/10.1002/jcsm.12417.
Bano G, Trevisan C, Carraro S, Solmi M, Luchini C, Stubbs B, et al. Inflammation and sarcopenia: a systematic review and meta-analysis. Maturitas [Internet]. Elsevier; 2017;96:10–5. https://doi.org/10.1016/j.maturitas.2016.11.006.
Visser M, Pahor M, Taaffe DR, Goodpaster BH, Simonsick EM, Newman AB, et al. Relationship of interleukin-6 and tumor necrosis factor-alpha with muscle mass and muscle strength in elderly men and women: the Health ABC Study. J Gerontol A Biol Sci Med Sci [Internet]. 2002;57:M326-32. https://doi.org/10.1093/gerona/57.5.m326.
Peixoto da Silva S, Santos JMO, Costa E Silva MP, Gil da Costa RM RM, Medeiros R. Cancer cachexia and its pathophysiology: links with sarcopenia, anorexia and asthenia. J Cachexia Sarcopenia Muscle Internet. 2020;11:619–35.
Baracos VE, Martin L, Korc M, Guttridge DC, Fearon KCH. Cancer-associated cachexia. Nat Rev Dis Primers [Internet]. 2018;4:17105. https://doi.org/10.1038/nrdp.2017.105.
McGovern J, Dolan RD, Skipworth RJ, Laird BJ, McMillan DC. Cancer cachexia: a nutritional or a systemic inflammatory syndrome? Br J Cancer [Internet]. 2022;127:379–82. https://doi.org/10.1038/s41416-022-01826-2.
• Feliciano EMC, Kroenke CH, Meyerhardt JA, Prado CM, Bradshaw PT, Kwan ML, et al. Association of systemic inflammation and sarcopenia with survival in nonmetastatic colorectal cancer: results from the C SCANS study. JAMA Oncol [Internet]. 2017;3:e172319. https://doi.org/10.1001/jamaoncol.2017.2319. Large study demonstrating relationship between sarcopenia and inflammation and their prognostic ability when combined.
Mountzias A, Hultdin J, Hlodan J, Kröger Dahlin B-I, Johansson M, Ljungberg B. Inflammatory response markers and survival prediction in patients with renal cell carcinoma. Scand J Urol [Internet]. 2022;56:47–52. https://doi.org/10.1080/21681805.2021.1983016.
Komai Y, Saito K, Sakai K, Morimoto S. Increased preoperative serum C-reactive protein level predicts a poor prognosis in patients with localized renal cell carcinoma. BJU Int [Internet]. 2007;99:77–80. https://doi.org/10.1111/j.1464-410X.2006.06497.x.
Patil D, Le T-L, Bens KB, Alemozaffar M, Lay A, Pattaras J, et al. Dynamic evaluation of the modified glasgow prognostic scale in patients with resected, localized clear cell renal cell carcinoma. Urology [Internet]. 2020;141:101–7. https://doi.org/10.1016/j.urology.2020.03.024.
Hu X, Wang Y, Yang W-X, Dou W-C, Shao Y-X, Li X. Modified Glasgow prognostic score as a prognostic factor for renal cell carcinomas: a systematic review and meta-analysis. Cancer Manag Res [Internet]. 2019;11:6163–73. https://doi.org/10.2147/CMAR.S208839.
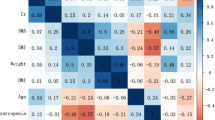
Hu Q, Mao W, Wu T, Xu Z, Yu J, Wang C, et al. High neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio are associated with sarcopenia risk in hospitalized renal cell carcinoma patients. Front Oncol [Internet]. ncbi.nlm.nih.gov; 2021;11:736640. https://doi.org/10.3389/fonc.2021.736640.
•• Midenberg E, Higgins MI, Schmeusser BN, Patil DH, Zaldumbide J, Martini DJ, et al. Prognostic value of sarcopenia and albumin in the surgical management of localized renal cell carcinoma. Urologic Oncology: Seminars and Original Investigations [Internet]. Elsevier; 2022; Available from: https://www.sciencedirect.com/science/article/pii/S1078143922003507. Important paper exhibiting relationship between sarcopenia with malnutrition in renal cell carcinoma. Critical findings for renal cell carcinoma showing improved prognostic ability when features of malnutrition and sarcopenia are combined rather than examined in isolation.
• Khan AI, Psutka SP, Patil DH, Hong G, Williams MA, Bilen MA, et al. Sarcopenia and systemic inflammation are associated with decreased survival after cytoreductive nephrectomy for metastatic renal cell carcinoma. Cancer [Internet]. 2022;128:2073–84. https://doi.org/10.1002/cncr.34174. Informative details regarding complex interplay between inflammation and sarcopenia in metastatic renal cell carcinoma.
Prado CMM, Heymsfield SB. Lean tissue imaging: a new era for nutritional assessment and intervention. JPEN J Parenter Enteral Nutr [Internet]. 2014;38:940–53. https://doi.org/10.1177/0148607114550189.
Higgins MI, Marquardt JP, Master VA, Fintelmann FJ, Psutka SP. Machine learning in body composition analysis. Eur Urol Focus [Internet]. 2021;7:713–6. https://doi.org/10.1016/j.euf.2021.03.013.
Troschel AS, Troschel FM, Best TD, Gaissert HA, Torriani M, Muniappan A, et al. Computed tomography-based body composition analysis and its role in lung cancer care. J Thorac Imaging [Internet]. 2020;35:91–100. https://doi.org/10.1097/RTI.0000000000000428.
Koo BK. Assessment of muscle quantity, quality and function. J Obes Metab Syndr [Internet]. 2022;31:9–16. https://doi.org/10.7570/jomes22025.
Boutin RD, Yao L, Canter RJ, Lenchik L. Sarcopenia: current concepts and imaging implications. AJR Am J Roentgenol [Internet]. 2015;205:W255-66. https://doi.org/10.2214/AJR.15.14635.
Bredella MA, Ghomi RH, Thomas BJ, Torriani M, Brick DJ, Gerweck AV, et al. Comparison of DXA and CT in the assessment of body composition in premenopausal women with obesity and anorexia nervosa. Obesity [Internet]. 2010;18:2227–33. https://doi.org/10.1038/oby.2010.5.
Sergi G, Trevisan C, Veronese N, Lucato P, Manzato E. Imaging of sarcopenia. Eur J Radiol [Internet]. 2016;85:1519–24. Available from: https://www.sciencedirect.com/science/article/pii/S0720048X16301206.
Albano D, Messina C, Vitale J, Sconfienza LM. Imaging of sarcopenia: old evidence and new insights. Eur Radiol [Internet]. 2020;30:2199–208. https://doi.org/10.1007/s00330-019-06573-2.
Blake GM, Naeem M, Boutros M. Comparison of effective dose to children and adults from dual X-ray absorptiometry examinations. Bone [Internet]. 2006;38:935–42. https://doi.org/10.1016/j.bone.2005.11.007.
Steward MJ, Taylor SA, Halligan S. Abdominal computed tomography, colonography and radiation exposure: what the surgeon needs to know. Colorectal Dis [Internet]. 2014;16:347–52. https://doi.org/10.1111/codi.12451.
Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge M-P, Albu J, et al. Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol [Internet]. journals.physiology.org; 2004;97:2333–8. https://doi.org/10.1152/japplphysiol.00744.2004.
Mourtzakis M, Prado CMM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab [Internet]. 2008;33:997–1006. https://doi.org/10.1139/H08-075.
• Steele S, Lin F, Le T-L, Medline A, Higgins M, Sandberg A, et al. Segmentation and linear measurement for body composition analysis using Slice-O-Matic and Horos. J Vis Exp [Internet]. 2021. https://doi.org/10.3791/61674. Fantastic resource for learning how to conduct body composition analysis on CT/MRI.
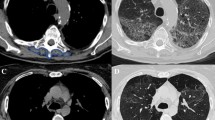
Abou Elkassem AM, Lo SS, Gunn AJ, Shuch BM, Dewitt-Foy ME, Abouassaly R, et al. Role of imaging in renal cell carcinoma: a multidisciplinary perspective. Radiographics [Internet]. Radiological Society of North America; 2021;41:1387–407. https://doi.org/10.1148/rg.2021200202.
Bates DDB, Pickhardt PJ. CT-derived body composition assessment as a prognostic tool in oncologic patients: from opportunistic research to artificial intelligence-based clinical implementation. AJR Am J Roentgenol [Internet]. 2022;219:671–80. https://doi.org/10.2214/AJR.22.27749.
Aleixo GFP, Shachar SS, Nyrop KA, Muss HB, Malpica L, Williams GR. Myosteatosis and prognosis in cancer: systematic review and meta-analysis. Crit Rev Oncol Hematol [Internet]. 2020;145:102839. https://doi.org/10.1016/j.critrevonc.2019.102839.
Lee K, Shin Y, Huh J, Sung YS, Lee IS, Yoon KH, et al. Recent issues on body composition imaging for sarcopenia evaluation. Korean J Radiol [Internet]. 2019;20:205–17. https://doi.org/10.3348/kjr.2018.0479.
Khan AI, Reiter DA, Sekhar A, Sharma P, Safdar NM, Patil DH, et al. MRI quantitation of abdominal skeletal muscle correlates with CT-based analysis: implications for sarcopenia measurement. Appl Physiol Nutr Metab [Internet]. Canadian Science Publishing; 2019;44:814–9. Available from: https://cdnsciencepub.com/doi/abs/10.1139/apnm-2018-0473.
• Higgins MI, Martini DJ, Patil DH, Steele S, Evans S, Petrinec BP, et al. Quantification of body composition in renal cell carcinoma patients: comparing computed tomography and magnetic resonance imaging measurements. Eur J Radiol [Internet]. 2020;132:109307. https://doi.org/10.1016/j.ejrad.2020.109307. Helpful manuscript validating expansion of body composition analysis to MRI.
Chianca V, Albano D, Messina C, Gitto S, Ruffo G, Guarino S, et al. Sarcopenia: imaging assessment and clinical application. Abdom Radiol (NY) [Internet]. 2022;47:3205–16. https://doi.org/10.1007/s00261-021-03294-3.
Guerri S, Mercatelli D, Aparisi Gómez MP, Napoli A, Battista G, Guglielmi G, et al. Quantitative imaging techniques for the assessment of osteoporosis and sarcopenia. Quant Imaging Med Surg [Internet]. 2018;8:60–85. https://doi.org/10.21037/qims.2018.01.05.
Stringer HJ, Wilson D. The role of ultrasound as a diagnostic tool for sarcopenia. J Frailty Aging [Internet]. 2018;7:258–61. https://doi.org/10.14283/jfa.2018.24.
Pinto-Ramos J, Costa-Santos C, Costa F, Tavares H, Cabral J, Moreira T, et al. Reliability of point-of-care ultrasound for measuring quadriceps femoris muscle thickness. Eur J Phys Rehabil Med [Internet]. 2022;58:767–73. https://doi.org/10.23736/S1973-9087.22.07432-9.
Tillquist M, Kutsogiannis DJ, Wischmeyer PE, Kummerlen C, Leung R, Stollery D, et al. Bedside ultrasound is a practical and reliable measurement tool for assessing quadriceps muscle layer thickness. JPEN J Parenter Enteral Nutr [Internet]. 2014;38:886–90. https://doi.org/10.1177/0148607113501327.
Watanabe Y, Yamada Y, Fukumoto Y, Ishihara T, Yokoyama K, Yoshida T, et al. Echo intensity obtained from ultrasonography images reflecting muscle strength in elderly men. Clin Interv Aging [Internet]. 2013;8:993–8. https://doi.org/10.2147/CIA.S47263.
Perkisas S, Bastijns S, Baudry S, Bauer J, Beaudart C, Beckwée D, et al. Application of ultrasound for muscle assessment in sarcopenia: 2020 SARCUS update. Eur Geriatr Med [Internet]. 2021;12:45–59. https://doi.org/10.1007/s41999-020-00433-9.
Peng PD, van Vledder MG, Tsai S, de Jong MC, Makary M, Ng J, et al. Sarcopenia negatively impacts short-term outcomes in patients undergoing hepatic resection for colorectal liver metastasis. HPB [Internet]. 2011;13:439–46. https://doi.org/10.1111/j.1477-2574.2011.00301.x.
Peyton CC, Heavner MG, Rague JT, Krane LS, Hemal AK. Does sarcopenia impact complications and overall survival in patients undergoing radical nephrectomy for stage III and IV kidney cancer? J Endourol [Internet]. 2016;30:229–36. https://doi.org/10.1089/end.2015.0492.
Smith AB, Deal AM, Yu H, Boyd B, Matthews J, Wallen EM, et al. Sarcopenia as a predictor of complications and survival following radical cystectomy. J Urol [Internet]. 2014;191:1714–20. https://doi.org/10.1016/j.juro.2013.12.047.
Valero V 3rd, Amini N, Spolverato G, Weiss MJ, Hirose K, Dagher NN, et al. Sarcopenia adversely impacts postoperative complications following resection or transplantation in patients with primary liver tumors. J Gastrointest Surg [Internet]. 2015;19:272–81. https://doi.org/10.1007/s11605-014-2680-4.
Taguchi S, Akamatsu N, Nakagawa T, Gonoi W, Kanatani A, Miyazaki H, et al. Sarcopenia evaluated using the skeletal muscle index is a significant prognostic factor for metastatic urothelial carcinoma. Clin Genitourin Cancer [Internet]. 2016;14:237–43. https://doi.org/10.1016/j.clgc.2015.07.015.
Eo W, Kwon J, An S, Lee S, Kim S, Nam D, et al. Clinical significance of paraspinal muscle parameters as a prognostic factor for survival in gastric cancer patients who underwent curative surgical resection. J Cancer [Internet]. 2020;11:5792–801. https://doi.org/10.7150/jca.46637.
Mao W, Wang K, Zhang H, Lu H, Sun S, Tian C, et al. Sarcopenia as a poor prognostic indicator for renal cell carcinoma patients undergoing nephrectomy in China: a multicenter study. Clin Transl Med [Internet]. ncbi.nlm.nih.gov; 2021;11:e270. https://doi.org/10.1002/ctm2.270.
Avrutin E, Moisey LL, Zhang R, Khattab J, Todd E, Premji T, et al. Clinically practical approach for screening of low muscularity using electronic linear measures on computed tomography images in critically Ill patients. JPEN J Parenter Enteral Nutr [Internet]. 2018;42:885–91. https://doi.org/10.1002/jpen.1019.
Cespedes Feliciano EM, Avrutin E, Caan BJ, Boroian A, Mourtzakis M. Screening for low muscularity in colorectal cancer patients: a valid, clinic-friendly approach that predicts mortality. J Cachexia Sarcopenia Muscle [Internet]. 2018;9:898–908. https://doi.org/10.1002/jcsm.12317.
• Schmeusser BN, Midenberg E, Palacios AR, Vettikattu N, Patil DH, Medline A, et al. Clinic friendly estimation of muscle composition: preoperative linear segmentation shows overall survival correlated with muscle mass in patients with nonmetastatic renal cell carcinoma. Front Oncol [Internet]. 2022;12:1068357. https://doi.org/10.3389/fonc.2022.1068357. Large study demonstrating association of sarcopenia with worse survival in renal cell carcinoma when utilizing a clinically practical muscle assessment method.
Gould H, Brennan SL, Kotowicz MA, Nicholson GC, Pasco JA. Total and appendicular lean mass reference ranges for Australian men and women: the Geelong osteoporosis study. Calcif Tissue Int [Internet]. 2014;94:363–72. https://doi.org/10.1007/s00223-013-9830-7.
Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol [Internet]. 2013;31:1539–47. https://doi.org/10.1200/JCO.2012.45.2722.
Zhang T, Ding C, Xie T, Yang J, Dai X, Lv T, et al. Skeletal muscle depletion correlates with disease activity in ulcerative colitis and is reversed after colectomy. Clin Nutr [Internet]. 2017;36:1586–92. https://doi.org/10.1016/j.clnu.2016.10.004.
Noguchi G, Kawahara T, Kobayashi K, Tsutsumi S, Ohtake S, Osaka K, et al. A lower psoas muscle volume was associated with a higher rate of recurrence in male clear cell renal cell carcinoma. PLoS One [Internet]. journals.plos.org; 2020;15:e0226581. https://doi.org/10.1371/journal.pone.0226581.
Higgins M, Manalo T, Patil DH, Nabavizadeh R, Martini D, Bilen MA, et al. Sarcopenia and modified Glasgow prognostic score predict outcomes following surgical resection of renal cell carcinoma with inferior vena cava thrombus. J Am Coll Surg [Internet]. Elsevier BV; 2021;233:e232. Available from. https://linkinghub.elsevier.com/retrieve/pii/S1072751521018767.
Xia L, Zhao R, Wan Q, Wu Y, Zhou Y, Wang Y, et al. Sarcopenia and adverse health-related outcomes: an umbrella review of meta-analyses of observational studies. Cancer Med [Internet]. 2020;9:7964–78. https://doi.org/10.1002/cam4.3428.
Beaudart C, Zaaria M, Pasleau F, Reginster J-Y, Bruyère O. Health outcomes of sarcopenia: a systematic review and meta-analysis. PLoS One [Internet]. journals.plos.org; 2017;12:e0169548. https://doi.org/10.1371/journal.pone.0169548.
Lee J, Suh J, Song C, You D, Jeong IG, Hong B, et al. Association between sarcopenia and survival of patients with organ-confined renal cell carcinoma after radical nephrectomy. Ann Surg Oncol [Internet]. 2022;29:2473–9. https://doi.org/10.1245/s10434-021-10881-7.
Watanabe S, Ishihara H, Takagi T, Kondo T, Ishiyama R, Fukuda H, et al. Impact of sarcopenia on post-operative outcomes following nephrectomy and tumor thrombectomy for renal cell carcinoma with inferior vena cava thrombus. Jpn J Clin Oncol [Internet]. 2021;51:819–25. https://doi.org/10.1093/jjco/hyaa275.
Midenberg E, Patil DH, Medline A, Higgins M, Williams M, Nazha B, et al. The prognostic role of sarcopenia and albumin in locally advanced renal cell carcinoma with IVC tumor thrombus. J Clin Oncol [Internet]. American Society of Clinical Oncology (ASCO); 2022;40:387–387. Available from: https://ascopubs.org/doi/10.1200/JCO.2022.40.6_suppl.387.
Darbas T, Forestier G, Leobon S, Pestre J, Jesus P, Lachatre D, et al. Impact of body composition in overweight and obese patients with localised renal cell carcinoma. In Vivo [Internet]. iv.iiarjournals.org; 2020;34:2873–81. https://doi.org/10.21873/invivo.12115.
Fukushima H, Nakanishi Y, Kataoka M, Tobisu K-I, Koga F. Prognostic significance of sarcopenia in patients with metastatic renal cell carcinoma. J Urol [Internet]. auajournals.org; 2016;195:26–32. https://doi.org/10.1016/j.juro.2015.08.071.
Sharma P, Zargar-Shoshtari K, Caracciolo JT, Fishman M, Poch MA, Pow-Sang J, et al. Sarcopenia as a predictor of overall survival after cytoreductive nephrectomy for metastatic renal cell carcinoma. Urol Oncol [Internet]. Elsevier; 2015;33:339.e17–23. https://doi.org/10.1016/j.urolonc.2015.01.011.
Antoun S, Baracos VE, Birdsell L, Escudier B, Sawyer MB. Low body mass index and sarcopenia associated with dose-limiting toxicity of sorafenib in patients with renal cell carcinoma. Ann Oncol [Internet]. Elsevier; 2010;21:1594–8. https://doi.org/10.1093/annonc/mdp605.
Cushen SJ, Power DG, Teo MY, MacEneaney P, Maher MM, McDermott R, et al. Body composition by computed tomography as a predictor of toxicity in patients with renal cell carcinoma treated with sunitinib. Am J Clin Oncol [Internet]. ingentaconnect.com; 2017;40:47–52. https://doi.org/10.1097/COC.0000000000000061.
Lee CH, Ku JY, Seo WI, Park YJ, Chung JI, Kim W, et al. Prognostic significance of sarcopenia and decreased relative dose intensity during the initial two cycles of first-line sunitinib for metastatic renal cell carcinoma. J Chemother [Internet]. 2021;33:245–55. https://doi.org/10.1080/1120009X.2020.1866825.
Huillard O, Mir O, Peyromaure M, Tlemsani C, Giroux J, Boudou-Rouquette P, et al. Sarcopenia and body mass index predict sunitinib-induced early dose-limiting toxicities in renal cancer patients. Br J Cancer [Internet]. nature.com; 2013;108:1034–41. https://doi.org/10.1038/bjc.2013.58.
Chen S, He T, Sun S, Wu J, Xu B, Mao W, et al. Prognostic significance of pre- to postoperative dynamics of sarcopenia for patients with renal cell carcinoma undergoing laparoscopic nephrectomy. Front Surg [Internet]. 2022;9:871731. https://doi.org/10.3389/fsurg.2022.871731.
Medline A, Midenberg E, Patil D, Evans S, Vettikattu N, Kamal F, et al. Muscle mass change using linear measurement analysis after nephrectomy for pT3 and pT4 renal cell carcinoma is associated with mortality. JCSM Rapid Communications [Internet]. Wiley; 2022;5:205–11. Available from: https://onlinelibrary.wiley.com/doi/10.1002/rco2.66.
Gu W, Wu J, Liu X, Zhang H, Shi G, Zhu Y, et al. Early skeletal muscle loss during target therapy is a prognostic biomarker in metastatic renal cell carcinoma patients. Sci Rep [Internet]. 2017;7:7587. https://doi.org/10.1038/s41598-017-07955-6.
Ishihara H, Takagi T, Kondo T, Fukuda H, Yoshida K, Iizuka J, et al. Effect of changes in skeletal muscle mass on oncological outcomes during first-line sunitinib therapy for metastatic renal cell carcinoma. Target Oncol [Internet]. 2018;13:745–55. https://doi.org/10.1007/s11523-018-0600-3.
Orcutt D, Wrobel MM, Mrah S, Marquardt JP, Fintelmann F, Hussey D, et al. Mp14–13 evaluating baseline and change in body composition in patients with metastatic renal cell carcinoma with front-line systemic therapy: implications for adverse events and overall survival. J Urol [Internet]. Ovid Technologies (Wolters Kluwer Health); 2021;206. Available from: https://www.auajournals.org/doi/abs/10.1097/JU.0000000000001995.13.
Schmeusser BN, Patil DH, Midenberg E, Higgins MI, Zaldumbide J, Martini DJ, et al. Data regarding covariates significantly associated with sarcopenia and varying albumin statuses in patients with renal cell carcinoma. Data Brief [Internet]. Elsevier BV; 2022;45:108724. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2352340922009283.
Ishihara H, Kondo T, Omae K, Takagi T, Iizuka J, Kobayashi H, et al. Sarcopenia and the modified glasgow prognostic score are significant predictors of survival among patients with metastatic renal cell carcinoma who are receiving first-line sunitinib treatment. Target Oncol [Internet]. Springer; 2016;11:605–17. https://doi.org/10.1007/s11523-016-0430-0.
Kays JK, Koniaris LG, Cooper CA, Pili R, Jiang G, Liu Y, et al. The combination of low skeletal muscle mass and high tumor interleukin-6 associates with decreased survival in clear cell renal cell carcinoma. Cancers [Internet]. mdpi.com; 2020;12. https://doi.org/10.3390/cancers12061605.
Aslan V, Kılıç ACK, Sütcüoğlu O, Eraslan E, Bayrak A, Öksüzoğlu B, et al. Cachexia index in predicting outcomes among patients receiving immune checkpoint inhibitor treatment for metastatic renal cell carcinoma. Urol Oncol [Internet]. 2022;40:494.e1-494.e10. https://doi.org/10.1016/j.urolonc.2022.07.018.
Psutka SP. Muscle mass matters in patients with renal cell carcinoma, but that is only the beginning… [Internet]. Ann Surg Oncol. Springer; 2022. p. 2152–4. https://doi.org/10.1245/s10434-021-11091-x.
Magudia K, Bridge CP, Bay CP, Babic A, Fintelmann FJ, Troschel FM, et al. Population-scale ct-based body composition analysis of a large outpatient population using deep learning to derive age-, sex-, and race-specific reference curves. Radiology [Internet]. Radiological Society of North America; 2021;298:319–29. https://doi.org/10.1148/radiol.2020201640.
Jensen B, Moritoyo T, Kaufer-Horwitz M, Peine S, Norman K, Maisch MJ, et al. Ethnic differences in fat and muscle mass and their implication for interpretation of bioelectrical impedance vector analysis. Appl Physiol Nutr Metab [Internet]. 2019;44:619–26. https://doi.org/10.1139/apnm-2018-0276.
Blue MNM, Hirsch KR, Brewer GJ, Cabre HE, Gould LM, Tinsley GM, et al. The validation of contemporary body composition methods in various races and ethnicities. Br J Nutr [Internet]. 2022;1–11. https://doi.org/10.1017/S0007114522000368.
Baracos VE. Psoas as a sentinel muscle for sarcopenia: a flawed premise [Internet]. J. Cachexia Sarcopenia Muscle. 2017;527–8. https://doi.org/10.1002/jcsm.12221.
Marquardt JP, Roeland EJ, Van Seventer EE, Best TD, Horick NK, Nipp RD, et al. Percentile-based averaging and skeletal muscle gauge improve body composition analysis: validation at multiple vertebral levels. J Cachexia Sarcopenia Muscle [Internet]. 2022;13:190–202. https://doi.org/10.1002/jcsm.12848.
Rutten IJG, Ubachs J, Kruitwagen RFPM, Beets-Tan RGH, Olde Damink SWM, Van Gorp T. Psoas muscle area is not representative of total skeletal muscle area in the assessment of sarcopenia in ovarian cancer. J Cachexia Sarcopenia Muscle [Internet]. 2017;8:630–8. https://doi.org/10.1002/jcsm.12180.
Bridge CP, Best TD, Wrobel MM, Marquardt JP, Magudia K, Javidan C, et al. A fully automated deep learning pipeline for multi-vertebral level quantification and characterization of muscle and adipose tissue on chest CT scans. Radiol Artif Intell [Internet]. 2022;4:e210080. https://doi.org/10.1148/ryai.210080.
Kim SI, Chung JY, Paik H, Seol A, Yoon SH, Kim TM, et al. Prognostic role of computed tomography-based, artificial intelligence-driven waist skeletal muscle volume in uterine endometrial carcinoma. Insights Imaging [Internet]. 2021;12:192. https://doi.org/10.1186/s13244-021-01134-y.
Yoo HJ, Kim YJ, Hong H, Hong SH, Chae HD, Choi J-Y. Deep learning-based fully automated body composition analysis of thigh CT: comparison with DXA measurement. Eur Radiol [Internet]. 2022;32:7601–11. https://doi.org/10.1007/s00330-022-08770-y.
Ying T, Borrelli P, Edenbrandt L, Enqvist O, Kaboteh R, Trägårdh E, et al. Automated artificial intelligence-based analysis of skeletal muscle volume predicts overall survival after cystectomy for urinary bladder cancer. Eur Radiol Exp [Internet]. 2021;5:50. https://doi.org/10.1186/s41747-021-00248-8.
Fuchs G, Chretien YR, Mario J, Do S, Eikermann M, Liu B, et al. Quantifying the effect of slice thickness, intravenous contrast and tube current on muscle segmentation: implications for body composition analysis. Eur Radiol [Internet]. 2018;28:2455–63. https://doi.org/10.1007/s00330-017-5191-3.
Antoun S, Lanoy E, Iacovelli R, Albiges-Sauvin L, Loriot Y, Merad-Taoufik M, et al. Skeletal muscle density predicts prognosis in patients with metastatic renal cell carcinoma treated with targeted therapies. Cancer [Internet]. Wiley Online Library; 2013;119:3377–84. https://doi.org/10.1002/cncr.28218.
Maurits JSF, Sedelaar JPM, Mulders PFA, Aben KKH, Kiemeney LALM, Vrieling A. Skeletal muscle radiodensity and visceral adipose tissue index are associated with survival in renal cell cancer - a multicenter population-based cohort study. Clin Nutr [Internet]. 2022;41:131–43. https://doi.org/10.1016/j.clnu.2021.11.012.
Weinberg MS, Shachar SS, Muss HB, Deal AM, Popuri K, Yu H, et al. Beyond sarcopenia: characterization and integration of skeletal muscle quantity and radiodensity in a curable breast cancer population. Breast J [Internet]. 2018;24:278–84. https://doi.org/10.1111/tbj.12952.
Park IK, Yang SS, Chung E, Cho E-S, Lee HS, Shin S-J, et al. Skeletal muscle gauge as a prognostic factor in patients with colorectal cancer. Cancer Med [Internet]. 2021;10:8451–61. Available from: https://doi.org/10.1002/cam4.4354.
Ganju RG, Morse R, Tennapel MJ, Hoover A, Kakarala K, Shnayder L, et al. Skeletal muscle gauge measured at the C3 vertebral body predicts for outcomes in men with P16-positive oropharynx cancer. Int J Radiat Oncol Biol Phys [Internet]. Elsevier; 2019;105:E420. https://doi.org/10.1016/j.ijrobp.2019.06.1528.
Temel JS, Abernethy AP, Currow DC, Friend J, Duus EM, Yan Y, et al. Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials. Lancet Oncol [Internet]. 2016;17:519–31. https://doi.org/10.1016/S1470-2045(15)00558-6.
Crawford J, Johnston MA, Taylor RP, Dalton JT, Steiner MS. Enobosarm and lean body mass in patients with non-small cell lung cancer. J Clin Orthod [Internet]. Wolters Kluwer; 2014;32:9618–9618. https://doi.org/10.1200/jco.2014.32.15_suppl.9618.
Ramage MI, Skipworth RJE. The relationship between muscle mass and function in cancer cachexia: smoke and mirrors? Curr Opin Support Palliat Care [Internet]. 2018;12:439–44. https://doi.org/10.1097/SPC.0000000000000381.
Hung C-J, Kang B-H, Chang K-M, Kang Y-Y, Yin C-H, Lee C-C. Chemotherapy dose per kilogram lean body mass increased dose-limiting toxicity event in male head and neck cancer with taxane and platinum-based induction therapy. BMC Cancer [Internet]. 2022;22:1084. https://doi.org/10.1186/s12885-022-10152-y.
de Jong C, Chargi N, Herder GJM, van Haarlem SWA, van der Meer F, van Lindert ASR, et al. The association between skeletal muscle measures and chemotherapy-induced toxicity in non-small cell lung cancer patients. J Cachexia Sarcopenia Muscle [Internet]. 2022;13:1554–64. https://doi.org/10.1002/jcsm.12967.
Paris MT. Body composition analysis of computed tomography scans in clinical populations: the role of deep learning. Lifestyle Genom [Internet]. 2020;13:28–31. https://doi.org/10.1159/000503996.
Hemke R, Buckless CG, Tsao A, Wang B, Torriani M. Deep learning for automated segmentation of pelvic muscles, fat, and bone from CT studies for body composition assessment. Skeletal Radiol [Internet]. 2020;49:387–95. https://doi.org/10.1007/s00256-019-03289-8.
• Cespedes Feliciano EM, Popuri K, Cobzas D, Baracos VE, Beg MF, Khan AD, et al. Evaluation of automated computed tomography segmentation to assess body composition and mortality associations in cancer patients. J Cachexia Sarcopenia Muscle [Internet]. Springer Nature; 2020;11:1258–69. Available from: https://doi.org/10.1002/jcsm.12573. A well conducted study examining artificial intelligence for muscle analysis in malignancy.
Naser MA, Wahid KA, Grossberg AJ, Olson B, Jain R, El-Habashy D, et al. Deep learning auto-segmentation of cervical skeletal muscle for sarcopenia analysis in patients with head and neck cancer. Front Oncol [Internet]. 2022;12:930432. Available from: https://doi.org/10.3389/fonc.2022.930432.
Dabiri S, Popuri K, Ma C, Chow V, Feliciano EMC, Caan BJ, et al. Deep learning method for localization and segmentation of abdominal CT. Comput Med Imaging Graph [Internet]. 2020;85:101776. Available from: https://doi.org/10.1016/j.compmedimag.2020.101776.
L’hôte C, Cordier B, Labasse A, Boileau C, Costes B, Henrotin Y. Identification of new biomarkers for sarcopenia and characterization of cathepsin D biomarker. JCSM Rapid Communications [Internet]. Wiley; 2021;4:122–32. Available from: https://onlinelibrary.wiley.com/doi/10.1002/rco2.26.
Qaisar R, Karim A, Muhammad T, Shah I, Khan J. Prediction of sarcopenia using a battery of circulating biomarkers. Sci Rep [Internet]. 2021;11:8632. https://doi.org/10.1038/s41598-021-87974-6.
Kwak JY, Hwang H, Kim S-K, Choi JY, Lee S-M, Bang H, et al. Prediction of sarcopenia using a combination of multiple serum biomarkers. Sci Rep [Internet]. Nature Publishing Group; 2018 [cited 2022 Nov 20];8:1–7. Available from: https://www.nature.com/articles/s41598-018-26617-9.
Lien Y-HH. Looking for sarcopenia biomarkers [Internet]. Am J Med 2017; 502–3. https://doi.org/10.1016/j.amjmed.2017.01.018.
Costanzo MR, Barasch J. Creatinine and cystatin C. Circulation [Internet]. American Heart Association; 2018;137:2029–31. https://doi.org/10.1161/CIRCULATIONAHA.118.033343.
Salazar JH. Overview of urea and creatinine. Lab Med [Internet]. Oxford Academic; 2014 [cited 2022 Oct 19];45:e19–20. https://academic.oup.com/labmed/article/45/1/e19/2657879.
Tlemsani C, Durand J-P, Raynard B, Revel M-P, Deluche E, Di Palma M, et al. Relationship between the creatinine/cystatin C ratio and muscle mass measured by CT-scan in cancer patients. Clin Nutr ESPEN [Internet]. 2022;51:412–8. https://doi.org/10.1016/j.clnesp.2022.07.010.
Tang T, Xie L, Hu S, Tan L, Lei X, Luo X, et al. Serum creatinine and cystatin C-based diagnostic indices for sarcopenia in advanced non-small cell lung cancer. J Cachexia Sarcopenia Muscle [Internet]. Wiley; 2022;13:1800–10. Available from: https://onlinelibrary.wiley.com/doi/10.1002/jcsm.12977.
Zheng C, Wang E, Li J-S, Xie K, Luo C, Ge Q-Y, et al. Serum creatinine/cystatin C ratio as a screening tool for sarcopenia and prognostic indicator for patients with esophageal cancer. BMC Geriatr [Internet]. 2022;22:207. https://doi.org/10.1186/s12877-022-02925-8.
Jung C-Y, Kim HW, Han SH, Yoo T-H, Kang S-W, Park JT. Creatinine-cystatin C ratio and mortality in cancer patients: a retrospective cohort study. J Cachexia Sarcopenia Muscle [Internet]. 2022. https://doi.org/10.1002/jcsm.13006.
Evans WJ, Hellerstein M, Orwoll E, Cummings S, Cawthon PM. D3 -Creatine dilution and the importance of accuracy in the assessment of skeletal muscle mass. J Cachexia Sarcopenia Muscle [Internet]. 2019;10:14–21. https://doi.org/10.1002/jcsm.12390.
Prado CM, von Haehling S. D3 -Creatine dilution for body composition assessment: a direct take on the matter [Internet]. J. Cachexia Sarcopenia Muscle. 2022. p. 2593–4. Available from: https://doi.org/10.1002/jcsm.13088.
Prado CMM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol [Internet]. 2008;9:629–35. https://doi.org/10.1016/S1470-2045(08)70153-0.
Auclin E, Bourillon C, De Maio E, By MA, Seddik S, Fournier L, et al. Prediction of everolimus toxicity and prognostic value of skeletal muscle index in patients with metastatic renal cell carcinoma. Clin Genitourin Cancer [Internet]. 2017;15:350–5. https://doi.org/10.1016/j.clgc.2017.01.022.
Buchler T, Kopecka M, Zemankova A, Wiesnerová M, Streckova E, Rozsypalova A, et al. Sarcopenia in metastatic renal cell carcinoma patients treated with cabozantinib. Target Oncol [Internet]. 2020;15:673–9. https://doi.org/10.1007/s11523-020-00744-8.
Funding
Dr. Psutka is funded by the National Institute on Aging, GEMSSTAR AWARD (RO3), Award ID#1R03AG073990-01A1.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
F.J.F. reports related patent and consulting fees from Pfizer.
Human and Animal Studies and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Viraj A. Master and Sarah P. Psutka are co-senior authors on this manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schmeusser, B.N., Ali, A.A., Fintelmann, F.J. et al. Imaging Techniques to Determine Degree of Sarcopenia and Systemic Inflammation in Advanced Renal Cell Carcinoma. Curr Urol Rep 24, 317–334 (2023). https://doi.org/10.1007/s11934-023-01157-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-023-01157-6