Abstract
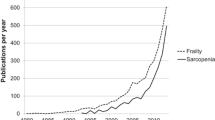
Risk for or established malnutrition is frequent in older adults, accompanied by functional limitations, increased morbidity and mortality. Protein-energy malnutrition is often observed and leads besides other predisposing factors to sarcopenia, the increased loss of muscle mass with aging. Sarcopenia is an integral correlate of the physical component of the frailty syndrome. Even though sarcopenia often reaches levels where mobility, balance and functionality on overall are hampered, its diagnosis has not become part of the standard diagnostic and therapeutic repertoire of geriatric medicine. This will hopefully change with a recently published revised international definition of sarcopenia, as well an own ICD-number. From a pathophysiological point of view, both malnutrition and sarcopenia share many components, a low-inflammatory state (inflamm-aging) being an important one. Nutritional interventions with and without parallel physical activity programs can prevent and often also reverse sarcopenia. It is hoped that upcoming even more potent nutritional treatment options—including for sarcopenic obesity—will lower the burden of malnutrition and sarcopenia for many older adults.
Similar content being viewed by others
References
Russell CA, Elia M (2012) Nutrition screening survey in the UK and Republic of Ireland in 2001. A report by the Malnutrition Advisory Group of the British Association for Parenteral and enteral Nutrition (BAPEN). http://www.bapen.org.uk/pdfs/nsw-2011-report.pdf. Accessed 2012
Morley JE (2001) Decreased food intake with aging. J Gerontol A Biol Sci Med Sci 56(Suppl. 2):81–88
Kaiser M, Bauer JM, Ramsch C et al (2009) MNA-International Group. J Nutr Health Aging 13:782–788
Frontera WR, Hughes VA, Fielding R et al (2000) Aging of skeletal muscle: a 12-yr longitudinal study. J Appl Physiol 88:1321–1326
Baumgartner RN, Waters LW (2006) Sarcopenia and sarcopenic-obesity. In: Pathy MS, Sinclair AJ, Morley JE (eds) Principles and practice of geriatric medicine. Wiley, Chichester, pp 909–933
Goodpaster B, Won Park S, Harris TB et al (2006) THe loss of skeletal muscle strength, mass, and quality in older adults: The Health, Aging and Body Composition Study. J Gerontol Biol Sci Med Sci 61A:1059–1064
Ferrucci L, Guralnik JM, Buchner D et al (2007) Departures of linearity tin the relationship between measures of muscular strength and physical performance of the lower extremities.: the Women’s Health and Aging Study. J Gerontol A Biol Sci Med Sci 52:M275–M285
Volkert D, Beck AM, Cederholm T et al (2018) ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr. https://doi.org/10.1016/j.clnu.2018.05.024
Morley JE (2010) Anorexia, weight loss, and frailty. J Am Med Dir Assoc 11:225–228
Fried L, Tangen CM, Walston J et al (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–M156
Deutz NE, Bauer JM, Barazzoni R et al (2014) Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr 33:929–936
Bauer JM, Biolo G, Cederholm T et al (2013) Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc 14:542–559
Goisser S, Kemmler W, Porzel S et al (2015) Sarcopenic obesity and complex interventions with nutrition and exercise in community-dwelling older persons—a narrative review. Clin Interv Aging 10:1267–1682
Barazzoni R, Bischoff SC, Boirie Y et al (2018) Sarcopenic obesity: time to meet the challenge. Clin Nutr 37:1787–1793
Cederholm T, Hellström K (1995) Reversibility of protein-energy malnutrition in a group of chronically ill elderly out-patients. Clin Nutr 14:81–87
Gingrich A, Rennekamp R, Brandl B et al (2018) Do aspects of protein intake vary across the week in healthy community-dwelling older adults? An enable Study. Nutrients. https://doi.org/10.3390/nu10091217
Cederholm T, Jensen GL, Correia MITD et al (2018) GLIM criteria for the diagnosis of malnutrition—a consensus report from the global clinical nutrition community. Clin Nutr. https://doi.org/10.1016/j.clnu.2018.08.002
Jensen GL, Cederholm T, Correia MITD et al (2019) GLIM criteria for the diagnosis of malnutrition—a consensus report from the global clinical nutrition community. JPEN 43:32–40
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127(5 Suppl):990S–991S
Mijnarends DM, Luiking YC, Halfens RJG et al (2018) Muscle health and costs: a glance at their relationship. J Nutr Health Aging 22:766–773
Malmstrom TK, Miller DK, Simonsick EM et al (2016) SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle 7:28–36
Antunes AC, Araujo DA, Verissimo MT et al (2017) Sarcopenia and hospitalisation costs in older adults: a cross-sectional study. Nutr Diet 74:46–50
Steffl M, Sima J, Shiells K et al (2017) The increase in health care costs associated with muscle weakness in older people without long-term illness in the Czech Republic: results from the Survey of Health, Ageing and Retirement in Europe (SHARE). Clin Interv Aging 12:2003–2007
De Buyser SI, Petrovic M, Taes YE et al (2016) Validation of the FNIH sarcopenia criteria and SOF frailty index as predictors of long-term mortality in ambulatory older men. Age Ageing 45:602–608
Janssen I, Heymsfield SB, Robert R (2002) Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc 50:889–896
Cruz-Jentoft AJ, Bayeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis. Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39:412–423
Muscaritoli M, Anker SD, Argiles J et al (2010) Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr 29:154–159
ICD-10 MC Diagnosis Code (2018) ICD-10 CMDiagnosis Code M62.84. Cited 12 Mar 2018. http://www.icd10data.com/ICD10CM/Codex/M00-M99/M60-M63/M62-/M62.84. Accessed 2012
Vellas B, Fielding RA, Bens C et al (2018) Implications of ICD-10 for sarcopenia clinical practice and clinical trials: report by the International Conference on Frailty and Sarcopenia Research Task Force. J Frailty Aging 7:2–9
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age and Ageing 48:16–31
Studenski S, Perera S, Patel K et al (2011) Gait speed and survival in older adults. JAMA 305:50–58
Zamboni M, Mazzali G, Fantin F et al (2008) Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis 18:388–395
Kemmler W, Teschler M, Weissenfels A et al (2017) Prevalence of sarcopenia and sarcopenic obesity in older German neb using recognized definitions: high accordance but low overlap! Osteoporosis Int 28:1881–1891
Evans WJ, Morley JE, Argiles J et al (2008) Cachexia: a new definition. Clin Nutr 27:793–799
Fearon K, Strasser F, Anker SD et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12:489–495
Salvioli S, Capri M, Valensin S et al (2006) Inflamm-aging, cytokines and aging: state of the art, new hypotheses on the role of mitochondria and new perspectives from systemic biology. Curr Pharm Des 12:3161–3171
Walston J, McBurnie MA, Newman A et al (2002) Frailty and activation of the inflammation and coagulation systems with and without clinical comorbidities: results from the Cardiovascular Health Study. Arch Intern Med 162:2333–2341
Leng SX, Tian X, Matteini A, Li H et al (2011) IL6-independent association of elevated serum neopterin levels with prevalent frailty in community-dwelling older adults. Age Ageing 40:475–481
Landi F, Cesari M, Calvani R et al (2017) The “Sarcopenia and Physical fRailty IN older people: multicomponent Treatment strategies” (SPRINTT) randomized controlled trial: design and methods. Aging Clin Exp Res 28:89–100
Landi F, Sieber C, Fielding RA et al (2018) Nutritional Intervention in Sarcopenia: report from the International Conference on Frailty and Sarcopenia Research Task Force. J Frailty Aging 7:247–252
Vasquez-Morales A, Wanden-Berghe C, Sanz-Valero J (2012) Exercise and nutritional supplements: effects of combined use in people over 65 years: a systematic review. Nutr Hosp 28:1077–1084
Wright J, Baldwin C (2018) Oral nutritional support with or without exercise in the management of malnutrition in nutritionally vulnerable older people: a systematic review and meta-analysis. Clin Nutr 37:1879–1891
Dent E, Morley JE, Cruz-Jentoft AJ et al (2018) International Clinical Practice Guidelines for Sarcopenia (ICFSR): screening, diagnosis and management. J Nutr Health Aging 22:1148–1161
Fiatarone MA, O’Neill EF, Ryan ND et al (1994) Exercise training and nutritional supplementation for physical frailty in very elderly people. N Engl J Med 330:1769–1775
Milne AC, Potter J, Vivanti A et al (2009) Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev 15:CD003288
Wilkinson DJ, Hossain T, Hill DS et al (2013) Effects of leucine and its metabolite beta-hydroxy-beta-methybutyrate on human skeletal muscle protein metabolism. J Physiol 591:2911–2923
Katsanos CS, Aarsland A, Cree MG et al (2009) Muscle protein synthesis and balance responsiveness to essential amino acids ingestion in the presence of elevated plasma free fatty acid concentrations. J Clin Endocrinol Metab 94:2984–2990
Komar B, Schwingshackl L, Hoffmann G (2015) Effects of leucine-rich protein supplements on anthropometric parameter and muscle strength in the elderly: a systematic review and meta-analysis. J Nutr Health Aging 19:437–446
Bauer JM, Verlaan S, Bautmans I et al (2015) Effects of a vitamin D and leucine-enriched whey protein nutritional supplement on measures of sarcopenia in older adults, the provide study: a randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc 16:740–747
Bo Y, Liu C, Ji Z et al (2018) A high whey protein, vitamin D and E supplement preserves muscle mass, strength, and quality of life in sarcopenic older adults: a double-blind randomized controlled trial. Clin Nutr. https://doi.org/10.1016/j.clnu.2017.12.020
Liberman K, Njemini R, Luiking Y et al (2019) 13 weeks of supplementation of vitamin D and leucine-enriched whey protein nutritional supplement attenuates chronic low grade inflammation in sarcopenic frail older adults: the PROVIDE study. Aging Clin Exp Res (in press)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The corresponding author states that there is no conflict of interest.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sieber, C.C. Malnutrition and sarcopenia. Aging Clin Exp Res 31, 793–798 (2019). https://doi.org/10.1007/s40520-019-01170-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01170-1