Abstract
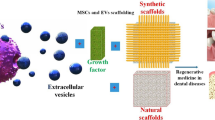
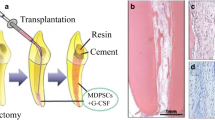
Tissue engineering as an important field in regenerative medicine is a promising therapeutic approach to replace or regenerate injured tissues. It consists of three vital steps including the selection of suitable cells, formation of 3d scaffolds, and adding growth factors. Mesenchymal stem cells (MSCs) and embryonic stem cells (ESCs) are mentioned as two main sources for this approach that have been used for the treatment of various types of disorders. However, the main focus of literature in the field of dental tissue engineering is on utilizing MSCs. On the other hand, biocompatible scaffolds play a notable role in this regenerative process which is mentioned to be harmless with acceptable osteoinductivity. Their ability in inhibiting inflammatory responses also makes them powerful tools. Indeed, stem cell functions should be supported by biomaterials acting as scaffolds incorporated with biological signals. Naturally derived polymeric scaffolds and synthetically engineered polymeric/ceramic scaffolds are two main types of scaffolds regarding their materials that are defined further in this review. Various strategies of tissue bioengineering can affect the regeneration of dentin-pulp complex, periodontium regeneration, and whole teeth bioengineering. In this regard, in vivo/ex vivo experimental models have been developed recently in order to perform preclinical studies of dental tissue engineering which make it more transferable to be used for clinic uses. This review summarizes dental tissue engineering through its different components. Also, strategies of tissue bioengineering and experimental models are introduced in order to provide a perspective of the potential roles of dental tissue engineering to be used for clinical aims.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
Abbreviations
- 3D:
-
Three dimensional
- ASF-CM:
-
Ameloblast serum-free conditioned medium
- a-TDM:
-
Autoclaved treated dentin matrix
- BMPs:
-
Bone Morphogenetic Proteins
- BMSCs:
-
Bone marrow stromal cells
- Ca/P:
-
Calcium phosphates
- CAD:
-
Computer-aided design
- c-Myc:
-
Myelocytomatosis oncogene
- CT:
-
Computerized tomography
- DFSCs:
-
Dental follicle stem cells
- DP-MSCs:
-
Dental pulp mesenchymal stem cells
- DPSCs:
-
Dental pulp stem cells
- ECM:
-
Extracellular matrix
- ESCs:
-
Embryonic stem cells
- FGF:
-
Fibroblast growth factor
- G-CSF:
-
Granulocyte colony-stimulating factor
- GTR:
-
Guided tissue regeneration
- HA:
-
Hydroxyapatite
- HDPC:
-
Human dental pulp cell
- IFN-γ:
-
Interferon-gamma
- IGF:
-
Insulin-like growth factor
- iPSCs:
-
Induced pluripotent stem cells
- Klf4:
-
Kruppel-like factor 4
- MAPK:
-
Mitogen-activated protein kinase
- mESCs:
-
Murine embryonic stem cells
- MRI:
-
Magnetic resonance imaging
- MSCs:
-
Mesenchymal stem cells
- NF-κB:
-
Nuclear factor kappa B
- NGF:
-
Nerve growth factor
- Oct4:
-
Octamer-binding transcription factor 4
- PDGF:
-
Platelet-derived growth factor
- PDL:
-
Periodontal ligament
- PDLSCs:
-
Periodontal ligament stem cells
- PEG:
-
Polyethylene glycol
- PGA:
-
Polyglycolic acid
- PLA:
-
Polylactic acid
- PLGA:
-
Poly(lactic-co-glycolic acid)
- PLLA:
-
Poly-L-lactic acid
- PRHds:
-
Platelet-rich hemoderivatives
- RP:
-
Rapid prototyping
- SCAP:
-
Stem cells from apical papilla
- SHED:
-
Stem cells from human exfoliated deciduous teeth
- Sox2:
-
Sex-determining region Y-Box 2
- ß –TCP:
-
ß-tricalcium phosphate
- TGF-ß:
-
Transforming growth factor-beta
- TLR4:
-
Toll-like receptor-4
- VEGF:
-
Vascular epithelial growth factor
References
Abdal-Wahab M, Abdel Ghaffar KA, Ezzatt OM, Hassan AAA, El Ansary MMS, Gamal AY (2020) Regenerative potential of cultured gingival fibroblasts in treatment of periodontal intrabony defects (randomized clinical and biochemical trial). J Periodontal Res 55(3):441–452
Abou Neel EA, Chrzanowski W, Salih VM, Kim H-W, Knowles JC (2014) Tissue engineering in dentistry. J Dent 42(8):915–928
Acri TM, Shin K, Seol D, Laird NZ, Song I, Geary SM et al (2019) Tissue engineering for the temporomandibular joint. Adv Healthc Mater 8(2):e1801236
Aghayan HR, Hosseini MS, Gholami M, Mohamadi-Jahani F, Tayanloo-Beik A, Alavi-Moghadam S et al (2021) Mesenchymal stem cells’ seeded amniotic membrane as a tissue-engineered dressing for wound healing. Drug Deliv Transl Res 12(3):538–549
Ahmad P, Della Bella E, Stoddart MJ (2020) Applications of bone morphogenetic proteins in dentistry: a bibliometric analysis. Biomed Res Int 2020:5971268
Ahmed GM, Abouauf EA, AbuBakr N, Dörfer CE, El-Sayed KF (2020) Tissue engineering approaches for enamel, dentin, and pulp regeneration: an update. Stem Cells Int 2020:5734539
Aimetti M, Ferrarotti F, Gamba MN, Giraudi M, Romano F (2018) Regenerative treatment of periodontal intrabony defects using autologous dental pulp stem cells: a 1-year follow-up case series. Int J Periodontics Restorative Dent 38(1):51–58
Alessandrini M, Preynat-Seauve O, De Bruin K, Pepper MS (2019) Stem cell therapy for neurological disorders. S Afr Med J 109(8b):70–77
AlKudmani H, Al Jasser R, Andreana S (2017) Is bone graft or guided bone regeneration needed when placing immediate dental implants? A systematic review. Implant Dent 26(6):936–944
Alraies A, Waddington RJ, Sloan AJ, Moseley R (2020) Evaluation of dental pulp stem cell heterogeneity and behaviour in 3D type I collagen gels. Biomed Res Int 2020:3034727
Amghar-Maach S, Gay-Escoda C, Sánchez-Garcés M (2019) Regeneration of periodontal bone defects with dental pulp stem cells grafting: systematic review. J Clin Exp Dent 11(4):e373–ee81
Anitua E, Troya M, Zalduendo M (2018) Progress in the use of dental pulp stem cells in regenerative medicine. Cytotherapy 20(4):479–498
Arjmand B, Goodarzi P, Mohamadi-Jahani F, Falahzadeh K, Larijani B (2017) Personalized regenerative medicine. Acta Med Iran 55:144–149
Arjmand B, Sarvari M, Alavi-Moghadam S, Payab M, Goodarzi P, Gilany K et al (2020) Prospect of stem cell therapy and regenerative medicine in osteoporosis. Front Endocrinol 11:430
Arthur A, Gronthos S (2020) Clinical application of bone marrow mesenchymal stem/stromal cells to repair skeletal tissue. Int J Mol Sci 21(24):9759
Ashraf R, Sofi HS, Beigh MA, Majeed S, Arjamand S, Sheikh FA (2018) Prospects of natural polymeric scaffolds in peripheral nerve tissue-regeneration. Adv Exp Med Biol 1077:501–525
Baba S, Yamada Y, Komuro A, Yotsui Y, Umeda M, Shimuzutani K et al (2016) Phase I/II trial of autologous bone marrow stem cell transplantation with a three-dimensional woven-fabric scaffold for periodontitis. Stem Cells Int 2016:6205910
Babo PS, Reis RL, Gomes ME (2017) Periodontal tissue engineering: current strategies and the role of platelet rich hemoderivatives. J Mater Chem B 5(20):3617–3628
Baier RV, Contreras Raggio JI, Giovanetti CM, Palza H, Burda I, Terrasi G et al (2021) Shape fidelity, mechanical and biological performance of 3D printed polycaprolactone-bioactive glass composite scaffolds. Mater Sci Eng C Mater Biol Appl 112540
Bakhtiar H, Mazidi SA, Mohammadi Asl S, Ellini MR, Moshiri A, Nekoofar MH et al (2018) The role of stem cell therapy in regeneration of dentine-pulp complex: a systematic review. Prog Biomater 7(4):249–268
Bar JK, Lis-Nawara A, Grelewski PG (2021) Dental pulp stem cell-derived secretome and its regenerative potential. Int J Mol Sci 22(21):12018
Baradaran-Rafii A, Sarvari M, Alavi-Moghadam S, Payab M, Goodarzi P, Aghayan HR et al (2020) Cell-based approaches towards treating age-related macular degeneration. Cell Tissue Bank:1–9
Baylan N, Bhat S, Ditto M, Lawrence JG, Lecka-Czernik B, Yildirim-Ayan E (2013) Polycaprolactone nanofiber interspersed collagen type-I scaffold for bone regeneration: a unique injectable osteogenic scaffold. Biomed Mater 8(4):045011
Benatti BB, Silvério KG, Casati MZ, Sallum EA, Nociti FH Jr (2007) Physiological features of periodontal regeneration and approaches for periodontal tissue engineering utilizing periodontal ligament cells. J Biosci Bioeng 103(1):1–6
Bhuptani RS, Patravale VB (2016) Porous microscaffolds for 3D culture of dental pulp mesenchymal stem cells. Int J Pharm 515(1–2):555–564
Bianco P, Riminucci M, Gronthos S, Robey PG (2001) Bone marrow stromal stem cells: nature, biology, and potential applications. Stem Cells 19(3):180–192
Boda SK, Almoshari Y, Wang H, Wang X, Reinhardt RA, Duan B et al (2019) Mineralized nanofiber segments coupled with calcium-binding BMP-2 peptides for alveolar bone regeneration. Acta Biomater 85:282–293
Boda SK, Wang H, John JV, Reinhardt RA, Xie J (2020) Dual delivery of alendronate and E7-BMP-2 peptide via calcium chelation to mineralized nanofiber fragments for alveolar bone regeneration. ACS Biomater Sci Eng 6(4):2368–2375
Bottino MC, Kamocki K, Yassen GH, Platt JA, Vail MM, Ehrlich Y et al (2013) Bioactive nanofibrous scaffolds for regenerative endodontics. J Dent Res 92(11):963–969
Boudriot U, Dersch R, Greiner A, Wendorff JH (2006) Electrospinning approaches toward scaffold engineering–a brief overview. Artif Organs 30(10):785–792
Bousnaki M, Bakopoulou A, Pich A, Papachristou E, Kritis A, Koidis P (2021) Mapping the secretome of dental pulp stem cells under variable microenvironmental conditions. Stem Cell Rev Rep 18:1372–1407
Brizuela C, Meza G, Urrejola D, Quezada MA, Concha G, Ramírez V et al (2020) Cell-based regenerative endodontics for treatment of periapical lesions: a randomized, controlled phase I/II clinical trial. J Dent Res 99(5):523–529
Carreira AC, Alves GG, Zambuzzi WF, Sogayar MC, Granjeiro JM (2014) Bone morphogenetic proteins: structure, biological function and therapeutic applications. Arch Biochem Biophys 561:64–73
Chai Y, Slavkin HC (2003) Prospects for tooth regeneration in the 21st century: a perspective. Microsc Res Tech 60(5):469–479
Chandrahasa S, Murray PE, Namerow KN (2011) Proliferation of mature ex vivo human dental pulp using tissue engineering scaffolds. J Endod 37(9):1236–1239
Chang H-I, Wang Y (2011) Cell responses to surface and architecture of tissue engineering scaffolds. IntechOpen, London
Chang CC, Lin TA, Wu SY, Lin CP, Chang HH (2020) Regeneration of tooth with allogenous, autoclaved treated dentin matrix with dental pulpal stem cells: an in vivo study. J Endod 46(9):1256–1264
Chen F, Shi S (2014) Principles of tissue engineering. Elsevier, New York
Chen FM, Gao LN, Tian BM, Zhang XY, Zhang YJ, Dong GY et al (2018) Correction to: treatment of periodontal intrabony defects using autologous periodontal ligament stem cells: a randomized clinical trial. Stem Cell Res Ther 9(1):260
Chen X, Chen Y, Hou Y, Song P, Zhou M, Nie M et al (2019) Modulation of proliferation and differentiation of gingiva-derived mesenchymal stem cells by concentrated growth factors: potential implications in tissue engineering for dental regeneration and repair. Int J Mol Med 44(1):37–46
Chen M, Chen J, Huang W, Li C, Luo H, Xue Z et al (2022) Exosomes from human induced pluripotent stem cells derived mesenchymal stem cells improved myocardial injury caused by severe acute pancreatitis through activating Akt/Nrf2/HO-1 axis. Cell Cycle:1–12
Chisini LA, Conde MCM, Grazioli G, Martin ASS, Carvalho RV, Sartori LRM et al (2019) Bone, periodontal and dental pulp regeneration in dentistry: a systematic scoping review. Braz Dent J 30(2):77–95
Chiu YC, Larson JC, Isom A Jr, Brey EM (2010) Generation of porous poly(ethylene glycol) hydrogels by salt leaching. Tissue Eng Part C Methods 16(5):905–912
Choi SH, Kim CK, Cho KS, Huh JS, Sorensen RG, Wozney JM et al (2002) Effect of recombinant human bone morphogenetic protein-2/absorbable collagen sponge (rhBMP-2/ACS) on healing in 3-wall intrabony defects in dogs. J Periodontol 73(1):63–72
Cristaldi M, Mauceri R, Tomasello L, Pizzo G, Pizzolanti G, Giordano C et al (2018) Dental pulp stem cells for bone tissue engineering: a review of the current literature and a look to the future. Regen Med 13(2):207–218
Demarco FF, Casagrande L, Zhang Z, Dong Z, Tarquinio SB, Zeitlin BD et al (2010) Effects of morphogen and scaffold porogen on the differentiation of dental pulp stem cells. J Endod 36(11):1805–1811
Dhandayuthapani B, Yoshida Y, Maekawa T, Kumar DS (2011) Polymeric scaffolds in tissue engineering application: a review. Int J Polym Sci 2011:290602
Dhote R, Charde P, Bhongade M, Rao J (2015) Stem cells cultured on beta tricalcium phosphate (β-TCP) in combination with recombinant human platelet-derived growth factor – BB (rh-PDGF-BB) for the treatment of human infrabony defects. J Stem Cells 10(4):243–254
Ding DC, Shyu WC, Lin SZ (2011) Mesenchymal stem cells. Cell Transplant 20(1):5–14
Dobie K, Smith G, Sloan AJ, Smith AJ (2002) Effects of alginate hydrogels and TGF-beta 1 on human dental pulp repair in vitro. Connect Tissue Res 43(2–3):387–390
Dorri M, Martinez-Zapata MJ, Walsh T, Marinho VC, Sheiham Deceased A, Zaror C (2017) Atraumatic restorative treatment versus conventional restorative treatment for managing dental caries. Cochrane Database Syst Rev 12(12):Cd008072
Douthwaite H, Arteagabeitia AB, Mukhopadhyay S (2022) Differentiation of human induced pluripotent stem cell into macrophages. Bio Protoc 12(6):e4361
Egusa H, Okita K, Kayashima H, Yu G, Fukuyasu S, Saeki M et al (2010) Gingival fibroblasts as a promising source of induced pluripotent stem cells. PLoS One 5(9):e12743
Eltom A, Zhong G, Muhammad A (2019) Scaffold techniques and designs in tissue engineering functions and purposes: a review. Adv Mater Sci Eng 2019:3429527
Eramo S, Natali A, Pinna R, Milia E (2018) Dental pulp regeneration via cell homing. Int Endod J 51(4):405–419
Fawzy El-Sayed KM, Doerfer CE (2017) Animal models for periodontal tissue engineering: a knowledge-generating process. Tissue Eng Part C Methods 23(12):900–925
Feng F, Akiyama K, Liu Y, Yamaza T, Wang TM, Chen JH et al (2010) Utility of PDL progenitors for in vivo tissue regeneration: a report of 3 cases. Oral Dis 16(1):20–28
Ferrarotti F, Romano F, Gamba MN, Quirico A, Giraudi M, Audagna M et al (2018) Human intrabony defect regeneration with micrografts containing dental pulp stem cells: a randomized controlled clinical trial. J Clin Periodontol 45(7):841–850
Galler KM, D’Souza RN (2011) Tissue engineering approaches for regenerative dentistry. Regen Med 6(1):111–124
Galler KM, Hartgerink JD, Cavender AC, Schmalz G, D’Souza RN (2012) A customized self-assembling peptide hydrogel for dental pulp tissue engineering. Tissue Eng Part A 18(1–2):176–184
Gaur S, Agnihotri R (2021) Application of adipose tissue stem cells in regenerative dentistry: a systematic review. J Int Soc Prev Community Dent 11(3):266–271
Genc B, Bozan HR, Genc S, Genc K (2019) Stem cell therapy for multiple sclerosis. Adv Exp Med Biol 1084:145–174
Gentile P, Chiono V, Carmagnola I, Hatton PV (2014) An overview of poly(lactic-co-glycolic) acid (PLGA)-based biomaterials for bone tissue engineering. Int J Mol Sci 15(3):3640–3659
Giannobile WV (1996) Periodontal tissue engineering by growth factors. Bone 19(1 Suppl):23s–37s
Giannobile WV, Lee CS, Tomala MP, Tejeda KM, Zhu Z (2001) Platelet-derived growth factor (PDGF) gene delivery for application in periodontal tissue engineering. J Periodontol 72(6):815–823
Goiato MC, Santos MR, Pesqueira AA, Moreno A, dos Santos DM, Haddad MF (2011) Prototyping for surgical and prosthetic treatment. J Craniofac Surg 22(3):914–917
Gong T, Heng BC, Lo ECM, Zhang C (2016) Current advance and future prospects of tissue engineering approach to dentin/pulp regenerative therapy. Stem Cells Int 2016:9204574
Gonzalez-Fernandez P, Rodríguez-Nogales C, Jordan O, Allémann E (2022) Combination of mesenchymal stem cells and bioactive molecules in hydrogels for osteoarthritis treatment. Eur J Pharm Biopharm 172:41–52
Goodarzi P, Aghayan HR, Soleimani M, Norouzi-Javidan A, Mohamadi-Jahani F, Jahangiri S et al (2014) Stem cell therapy for treatment of epilepsy. Acta Med Iran 52:651–655
Goodarzi P, Aghayan HR, Larijani B, Soleimani M, Dehpour A-R, Sahebjam M et al (2015) Stem cell-based approach for the treatment of Parkinson’s disease. Med J Islam Repub Iran 29:168
Goodarzi P, Falahzadeh K, Nematizadeh M, Farazandeh P, Payab M, Larijani B et al (2018a) Tissue engineered skin substitutes. Cell Biol Transl Med 3:143–188
Goodarzi P, Larijani B, Alavi-Moghadam S, Tayanloo-Beik A, Mohamadi-Jahani F, Ranjbaran N et al (2018b) Mesenchymal stem cells-derived exosomes for wound regeneration. Cell Biol Transl Med 4:119–131
Goodarzi P, Alavi-Moghadam S, Sarvari M, Beik AT, Falahzadeh K, Aghayan H et al (2018c) Adipose tissue-derived stromal cells for wound healing. In: Cell biology and translational medicine, vol 4. Springer, Cham, pp 133–149
Goodarzi P, Payab M, Alavi-Moghadam S, Larijani B, Rahim F, Bana N et al (2019) Development and validation of Alzheimer’s disease animal model for the purpose of regenerative medicine. Cell Tissue Bank 20(2):141–151
Granz CL, Gorji A (2020) Dental stem cells: the role of biomaterials and scaffolds in developing novel therapeutic strategies. World J Stem Cells 12(9):897–921
Gu Y, Sun Y, Shujaat S, Braem A, Politis C, Jacobs R (2022) 3D-printed porous Ti6Al4V scaffolds for long bone repair in animal models: a systematic review. J Orthop Surg Res 17(1):68
Hadjichristou C, Koidis P, Bakopoulou A (2021) Advanced in vitro experimental models for tissue engineering-based reconstruction of a 3D dentin/pulp complex: a literature review. Stem Cell Rev Rep 17(3):785–802
Han J, Menicanin D, Gronthos S, Bartold PM (2014) Stem cells, tissue engineering and periodontal regeneration. Aust Dent J 59(Suppl 1):117–130
Hashemi-Beni B, Khoroushi M, Foroughi MR, Karbasi S, Khademi AA (2017) Tissue engineering: dentin – pulp complex regeneration approaches (a review). Tissue Cell 49(5):552–564
He W, Wang Z, Luo Z, Yu Q, Jiang Y, Zhang Y et al (2015) LPS promote the odontoblastic differentiation of human dental pulp stem cells via MAPK signaling pathway. J Cell Physiol 230(3):554–561
He X, Jiang W, Luo Z, Qu T, Wang Z, Liu N et al (2017) IFN-γ regulates human dental pulp stem cells behavior via NF-κB and MAPK signaling. Sci Rep 7(1):40681
Hernández-Monjaraz B, Santiago-Osorio E, Monroy-García A, Ledesma-Martínez E, Mendoza-Núñez VM (2018) Mesenchymal stem cells of dental origin for inducing tissue regeneration in periodontitis: a mini-review. Int J Mol Sci 19(4):944
Hilkens P, Bronckaers A, Ratajczak J, Gervois P, Wolfs E, Lambrichts I (2017) The angiogenic potential of DPSCs and SCAPs in an in vivo model of dental pulp regeneration. Stem Cells Int 2017:2582080
Horst OV, Chavez MG, Jheon AH, Desai T, Klein OD (2012) Stem cell and biomaterials research in dental tissue engineering and regeneration. Dent Clin 56(3):495–520
Hu C, Zhao L, Zhang L, Bao Q, Li L (2020) Mesenchymal stem cell-based cell-free strategies: safe and effective treatments for liver injury. Stem Cell Res Ther 11(1):377
Huang GT-J, Yamaza T, Shea LD, Djouad F, Kuhn NZ, Tuan RS et al (2010) Stem/progenitor cell–mediated de novo regeneration of dental pulp with newly deposited continuous layer of dentin in an in vivo model. Tissue Eng Part A 16(2):605–615
Huang GTJ, Al-Habib M, Gauthier P (2013) Challenges of stem cell-based pulp and dentin regeneration: a clinical perspective. Endod Top 28(1):51–60
Hynes K, Menichanin D, Bright R, Ivanovski S, Hutmacher DW, Gronthos S et al (2015) Induced pluripotent stem cells: a new frontier for stem cells in dentistry. J Dent Res 94(11):1508–1515
Ikeda E, Morita R, Nakao K, Ishida K, Nakamura T, Takano-Yamamoto T et al (2009) Fully functional bioengineered tooth replacement as an organ replacement therapy. Proc Natl Acad Sci 106(32):13475–13480
Inanç B, Elçin AE, Elçin YM (2009) In vitro differentiation and attachment of human embryonic stem cells on periodontal tooth root surfaces. Tissue Eng Part A 15(11):3427–3435
Ishimatsu H, Kitamura C, Morotomi T, Tabata Y, Nishihara T, Chen KK et al (2009) Formation of dentinal bridge on surface of regenerated dental pulp in dentin defects by controlled release of fibroblast growth factor-2 from gelatin hydrogels. J Endod 35(6):858–865
Iwata T, Yamato M, Washio K, Yoshida T, Tsumanuma Y, Yamada A et al (2018) Periodontal regeneration with autologous periodontal ligament-derived cell sheets – a safety and efficacy study in ten patients. Regen Ther 9:38–44
Jain KK (2002) Ethical and regulatory aspects of embryonic stem cell research. Expert Opin Biol Ther 2(8):819–826
Jazayeri HE, Lee SM, Kuhn L, Fahimipour F, Tahriri M, Tayebi L (2020) Polymeric scaffolds for dental pulp tissue engineering: a review. Dent Mater 36(2):e47–e58
Jiang W, Ni L, Sloan A, Song B (2015) Tissue engineering and regenerative medicine, from and beyond the dentistry. Dentistry 5(6):1
Kaigler D, Cirelli JA, Giannobile WV (2006) Growth factor delivery for oral and periodontal tissue engineering. Expert Opin Drug Deliv 3(5):647–662
Kaneko T, Gu B, Sone PP, Zaw SYM, Murano H, Zaw ZCT et al (2018) Dental pulp tissue engineering using mesenchymal stem cells: a review with a protocol. Stem Cell Rev Rep 14(5):668–676
Kanimozhi K, Basha SK, Kumari VS, Kaviyarasu K (2018) Development of biomimetic hybrid porous scaffold of chitosan/polyvinyl alcohol/carboxymethyl cellulose by freeze-dried and salt leached technique. J Nanosci Nanotechnol 18(7):4916–4922
Karakaya I, Ulusoy N (2018) Basics of dentin-pulp tissue engineering. AIMS Bioeng 5(3):162–178
Kawai M, Kataoka Y, Sonobe J, Yamamoto H, Maruyama H, Yamamoto T et al (2018) Analysis of mineral apposition rates during alveolar bone regeneration over three weeks following transfer of BMP-2/7 gene via in vivo electroporation. Eur J Histochem 62(3):2947
Khademhosseini A, Langer R, Borenstein J, Vacanti JP (2006) Microscale technologies for tissue engineering and biology. Proc Natl Acad Sci USA 103(8):2480–2487
Khodakaram-Tafti A, Mehrabani D, Shaterzadeh-Yazdi H, Zamiri B, Omidi M (2018) Tissue engineering in maxillary bone defects. World J Plast Surg 7(1):3–11
Kim JY, Xin X, Moioli EK, Chung J, Lee CH, Chen M et al (2010) Regeneration of dental-pulp-like tissue by chemotaxis-induced cell homing. Tissue Eng Part A 16(10):3023–3031
Kim S, Shin SJ, Song Y, Kim E (2015) In vivo experiments with dental pulp stem cells for pulp-dentin complex regeneration. Mediat Inflamm 2015:409347
Kim SK, Cho TH, Han JJ, Kim IS, Park Y, Hwang SJ (2016) Comparative study of BMP-2 alone and combined with VEGF carried by hydrogel for maxillary alveolar bone regeneration. Tissue Eng Regen Med 13(2):171–181
King WJ, Krebsbach PH (2012) Growth factor delivery: how surface interactions modulate release in vitro and in vivo. Adv Drug Deliv Rev 64(12):1239–1256
Kitamura C, Nishihara T, Terashita M, Tabata Y, Jimi E, Washio A et al (2011) Regeneration approaches for dental pulp and periapical tissues with growth factors, biomaterials, and laser irradiation. Polymers 3(4):1776–1793
Koosha F, Alimohammadi N, Rafeian-Kopaei M (2021) The exosomes: staring biomarkers and novel therapeutic strategies. Curr Pharm Des 27(35):3714–3721
Kuboki Y, Jin Q, Takita H (2001) Geometry of carriers controlling phenotypic expression in BMP-induced osteogenesis and chondrogenesis. J Bone Joint Surg Am 83-A Suppl 1(Pt 2):S105–S115
Langer R, Vacanti JP (1993) Tissue engineering. Science 260(5110):920–926
Larijani B, Ghahari A, Warnock GL, Aghayan HR, Goodarzi P, Falahzadeh K et al (2015a) Human fetal skin fibroblasts: extremely potent and allogenic candidates for treatment of diabetic wounds. Med Hypotheses 84(6):577–579
Larijani B, Aghayan H, Goodarzi P, Mohamadi-Jahani F, Norouzi-Javidan A, Dehpour AR et al (2015b) Clinical grade human adipose tissue-derived mesenchymal stem cell banking. Acta Med Iran 53(9):540–546
Larijani B, Foroughi Heravani N, Alavi-Moghadam S, Goodarzi P, Rezaei-Tavirani M, Payab M et al (2020) Cell therapy targets for autism spectrum disorders: hopes, challenges and future directions. In: Cell biology and translational medicine, vol 13. Springer, Cham, pp 107–124
Leyendecker Junior A, Gomes Pinheiro CC, Lazzaretti Fernandes T, Franco Bueno D (2018) The use of human dental pulp stem cells for in vivo bone tissue engineering: a systematic review. J Tissue Eng 9:2041731417752766
Li X (2017) Tissue repair: reinforced scaffolds. Springer, Singapore, pp 1–304
Li Y, Fan P, Ding XM, Tian XH, Feng XS, Yan H et al (2017a) Polyglycolic acid fibrous scaffold improving endothelial cell coating and vascularization of islet. Chin Med J 130(7):832–839
Li Y, He L, Pan S, Zhang L, Zhang W, Yi H et al (2017b) Three-dimensional simulated microgravity culture improves the proliferation and odontogenic differentiation of dental pulp stem cell in PLGA scaffolds implanted in mice. Mol Med Rep 15(2):873–878
Liu H, Cao T (2010) Dental application potential of mesenchymal stromal cells and embryonic stem cells. Chin J Dent Res 13(2):95–103
Liu J, Jin T, Chang S, Ritchie HH, Smith AJ, Clarkson BH (2007) Matrix and TGF-beta-related gene expression during human dental pulp stem cell (DPSC) mineralization. In Vitro Cell Dev Biol Anim 43(3–4):120–128
Liu HC, Ling-Ling E, Wang DS, Su F, Wu X, Shi ZP et al (2011) Reconstruction of alveolar bone defects using bone morphogenetic protein 2 mediated rabbit dental pulp stem cells seeded on nano-hydroxyapatite/collagen/poly(L-lactide). Tissue Eng Part A 17(19–20):2417–2433
Liu XY, Yang LP, Zhao L (2020a) Stem cell therapy for Alzheimer’s disease. World J Stem Cells 12(8):787–802
Liu X, Wu H, Lu F, Li Q, Xu Z (2020b) Fabrication of porous bovine pericardium scaffolds incorporated with bFGF for tissue engineering applications. Xenotransplantation 27(1):e12568
Loh QL, Choong C (2013) Three-dimensional scaffolds for tissue engineering applications: role of porosity and pore size. Tissue Eng Part B Rev 19(6):485–502
Lu X, Chen X, Xing J, Lian M, Huang D, Lu Y et al (2019) miR-140-5p regulates the odontoblastic differentiation of dental pulp stem cells via the Wnt1/β-catenin signaling pathway. Stem Cell Res Ther 10(1):226
Lundquist P (2002) Odontoblast phosphate and calcium transport in dentinogenesis. Swed Dent J Suppl 154:1–52
Lymperi S, Ligoudistianou C, Taraslia V, Kontakiotis E, Anastasiadou E (2013) Dental stem cells and their applications in dental tissue engineering. Open Dent J 7:76–81
Maeda H, Tomokiyo A, Fujii S, Wada N, Akamine A (2011) Promise of periodontal ligament stem cells in regeneration of periodontium. Stem Cell Res Ther 2(4):33
Man RC, Sulaiman N, Idrus RBH, Ariffin SHZ, Wahab RMA, Yazid MD (2019) Insights into the effects of the dental stem cell secretome on nerve regeneration: towards cell-free treatment. Stem Cells Int 2019:4596150
Maroulakos M, Kamperos G, Tayebi L, Halazonetis D, Ren Y (2019) Applications of 3D printing on craniofacial bone repair: a systematic review. J Dent 80:1–14
Matai I, Kaur G, Seyedsalehi A, McClinton A, Laurencin CT (2020) Progress in 3D bioprinting technology for tissue/organ regenerative engineering. Biomaterials 226:119536
Miyaji H, Sugaya T, Ibe K, Ishizuka R, Tokunaga K, Kawanami M (2010) Root surface conditioning with bone morphogenetic protein-2 facilitates cementum-like tissue deposition in beagle dogs. J Periodontal Res 45(5):658–663
Monteiro N, Yelick PC (2017) Advances and perspectives in tooth tissue engineering. J Tissue Eng Regen Med 11(9):2443–2461
Morsczeck C, Götz W, Schierholz J, Zeilhofer F, Kühn U, Möhl C et al (2005) Isolation of precursor cells (PCs) from human dental follicle of wisdom teeth. Matrix Biol 24(2):155–165
Moussa DG, Aparicio C (2019) Present and future of tissue engineering scaffolds for dentin-pulp complex regeneration. J Tissue Eng Regen Med 13(1):58–75
Müller P, Lemcke H, David R (2018) Stem cell therapy in heart diseases – cell types, mechanisms and improvement strategies. Cell Physiol Biochem 48(6):2607–2655
Murphy CM, O’Brien FJ, Little DG, Schindeler A (2013) Cell-scaffold interactions in the bone tissue engineering triad. Eur Cell Mater 26:120–132
Murray PE (2012) Constructs and scaffolds employed to regenerate dental tissue. Dent Clin 56(3):577–588
Nada OA, El Backly RM (2018) Stem cells from the apical papilla (SCAP) as a tool for endogenous tissue regeneration. Front Bioeng Biotechnol 6:103
Nakashima M (2005) Bone morphogenetic proteins in dentin regeneration for potential use in endodontic therapy. Cytokine Growth Factor Rev 16(3):369–376
Nakashima M, Akamine A (2005) The application of tissue engineering to regeneration of pulp and dentin in endodontics. J Endod 31(10):711–718
Nam Y, Yoon J, Park T (2000) A novel fabrication method for macroporous scaffolds using gas foaming salt as Porogen additive. J Biomed Mater Res 53:1–7
Needleman I, Worthington HV, Giedrys-Leeper E, Tucker R (2019) Withdrawn: guided tissue regeneration for periodontal infra-bony defects. Cochrane Database Syst Rev 5(5):Cd001724
Nevins ML, Reynolds MA (2011) Tissue engineering with recombinant human platelet-derived growth factor BB for implant site development. Compend Contin Educ Dent 32(2):18, 20–27. quiz 8, 40
Ning F, Guo Y, Tang J, Zhou J, Zhang H, Lu W et al (2010) Differentiation of mouse embryonic stem cells into dental epithelial-like cells induced by ameloblasts serum-free conditioned medium. Biochem Biophys Res Commun 394(2):342–347
Okano H, Morimoto S (2022) iPSC-based disease modeling and drug discovery in cardinal neurodegenerative disorders. Cell Stem Cell 29(2):189–208
Oliveira SM, Santo VE, Gomes ME, Reis RL, Mano JF (2015) Layer-by-layer assembled cell instructive nanocoatings containing platelet lysate. Biomaterials 48:56–65
Ono M, Oshima M, Ogawa M, Sonoyama W, Hara ES, Oida Y et al (2017) Practical whole-tooth restoration utilizing autologous bioengineered tooth germ transplantation in a postnatal canine model. Sci Rep 7(1):44522
Ornitz DM, Itoh N (2015) The fibroblast growth factor signaling pathway. Wiley Interdiscip Rev Dev Biol 4(3):215–266
Orsini G, Ruggeri A, Mazzoni A, Nato F, Manzoli L, Putignano A et al (2009) A review of the nature, role, and function of dentin non-collagenous proteins. Part 1: proteoglycans and glycoproteins. Endod Top 21:1–18
Orti V, Collart-Dutilleul PY, Piglionico S, Pall O, Cuisinier F, Panayotov I (2018) Pulp regeneration concepts for nonvital teeth: from tissue engineering to clinical approaches. Tissue Eng Part B Rev 24(6):419–442
Oshima M, Tsuji T (2015) Whole tooth regeneration as a future dental treatment. In: Engineering mineralized and load bearing tissues. Springer, Cham, pp 255–269
Ozeki N, Hase N, Higuchi N, Hiyama T, Yamaguchi H, Kawai R et al (2017) Gelatin scaffold combined with bone morphogenetic protein-4 induces odontoblast-like cell differentiation involving integrin profile changes, autophagy-related gene 10, and Wnt5 sequentially in human induced pluripotent stem cells. Differentiation 93:1–14
Park JY, Park CH, Yi T, Kim SN, Iwata T, Yun JH (2020) rhBMP-2 pre-treated human periodontal ligament stem cell sheets regenerate a mineralized layer mimicking dental cementum. Int J Mol Sci 21(11):3767
Payab M, Goodarzi P, Heravani NF, Hadavandkhani M, Zarei Z, Falahzadeh K et al (2018) Stem cell and obesity: current state and future perspective. In: Cell biology and translational medicine, vol 2. Springer, Cham, pp 1–22
Peters OA, Paranjpe A, Gaudin A (2021) Dentine–pulp complex regeneration. In: Regenerative approaches in dentistry. Springer, Cham, pp 35–62
Piva E, Tarlé SA, Nör JE, Zou D, Hatfield E, Guinn T et al (2017) Dental pulp tissue regeneration using dental pulp stem cells isolated and expanded in human serum. J Endod 43(4):568–574
Qiu J, Wang X, Zhou H, Zhang C, Wang Y, Huang J et al (2020) Enhancement of periodontal tissue regeneration by conditioned media from gingiva-derived or periodontal ligament-derived mesenchymal stem cells: a comparative study in rats. Stem Cell Res Ther 11(1):1–15
Radwan IA, Rady D, Abbass MMS, El Moshy S, AbuBakr N, Dörfer CE et al (2020) Induced pluripotent stem cells in dental and nondental tissue regeneration: a review of an unexploited potential. Stem Cells Int 2020:1941629
Rahim F, Arjmand B, Shirbandi K, Payab M, Larijani B (2018) Stem cell therapy for patients with diabetes: a systematic review and meta-analysis of metabolomics-based risks and benefits. Stem Cell Investig 5:40
Rajan A, Eubanks E, Edwards S, Aronovich S, Travan S, Rudek I et al (2014) Optimized cell survival and seeding efficiency for craniofacial tissue engineering using clinical stem cell therapy. Stem Cells Transl Med 3(12):1495–1503
Rangasami VK, Nawale G, Asawa K, Kadekar S, Samanta S, Nilsson B et al (2021) Pluronic micelle-mediated tissue factor silencing enhances hemocompatibility, stemness, differentiation potential, and paracrine signaling of mesenchymal stem cells. Biomacromolecules 22(5):1980–1989
Ravindran S, George A (2015) Biomimetic extracellular matrix mediated somatic stem cell differentiation: applications in dental pulp tissue regeneration. Front Physiol 6:118
Rizk A, Rabie AB (2013) Human dental pulp stem cells expressing transforming growth factor β3 transgene for cartilage-like tissue engineering. Cytotherapy 15(6):712–725
Rolph DN, Deb M, Kanji S, Greene CJ, Das M, Joseph M et al (2020) Ferutinin directs dental pulp-derived stem cells towards the osteogenic lineage by epigenetically regulating canonical Wnt signaling. Biochim Biophys Acta (BBA) Mol Basis Dis 1866(4):165314
Rosa AR, Steffens D, Santi B, Quintiliano K, Steffen N, Pilger DA et al (2017) Development of VEGF-loaded PLGA matrices in association with mesenchymal stem cells for tissue engineering. Braz J Med Biol Res 50(9):e5648
Roseti L, Parisi V, Petretta M, Cavallo C, Desando G, Bartolotti I et al (2017) Scaffolds for bone tissue engineering: state of the art and new perspectives. Mater Sci Eng C Mater Biol Appl 78:1246–1262
Sachdeva S, Saluja H, Mani A, Phadnaik MB, Palekar U (2021) Tissue engineering in periodontics- a demystifying review. J Cell Biotechnol 7:19–23
Sakai VT, Cordeiro MM, Dong Z, Zhang Z, Zeitlin BD, Nör JE (2011) Tooth slice/scaffold model of dental pulp tissue engineering. Adv Dent Res 23(3):325–332
Sánchez N, Fierravanti L, Núñez J, Vignoletti F, González-Zamora M, Santamaría S et al (2020) Periodontal regeneration using a xenogeneic bone substitute seeded with autologous periodontal ligament-derived mesenchymal stem cells: a 12-month quasi-randomized controlled pilot clinical trial. J Clin Periodontol 47(11):1391–1402
Sengupta D, Heilshorn SC (2010) Protein-engineered biomaterials: highly tunable tissue engineering scaffolds. Tissue Eng Part B Rev 16(3):285–293
Shimabukuro Y, Ueda M, Ozasa M, Anzai J, Takedachi M, Yanagita M et al (2009) Fibroblast growth factor-2 regulates the cell function of human dental pulp cells. J Endod 35(11):1529–1535
Shinmura Y, Tsuchiya S, Hata K, Honda MJ (2008) Quiescent epithelial cell rests of Malassez can differentiate into ameloblast-like cells. J Cell Physiol 217(3):728–738
Sismanoglu S, Ercal P (2020) Dentin-pulp tissue regeneration approaches in dentistry: an overview and current trends. In: Cell biology and translational medicine, Volume 10: stem cells in tissue regeneration. Springer, Cham, pp 79–103
Smith EE, Yelick PC (2016) Progress in bioengineered whole tooth research: from bench to dental patient chair. Curr Oral Health Rep 3(4):302–308
Song J, Chen Z, Murillo LL, Tang D, Meng C, Zhong X et al (2021) Hierarchical porous silk fibroin/poly(L-lactic acid) fibrous membranes towards vascular scaffolds. Int J Biol Macromol 166:1111–1120
Stevens LR, Gilmore KJ, Wallace GG, In Het Panhuis M (2016) Tissue engineering with gellan gum. Biomater Sci 4(9):1276–1290
Su J, Hua S, Chen A, Chen P, Yang L, Yuan X et al (2021) Three-dimensional printing of gyroid-structured composite bioceramic scaffolds with tuneable degradability. Mater Sci Eng C Mater Biol Appl 133:112595
Subramanian A, Krishnan UM, Sethuraman S (2011) 14 – skin tissue regeneration. In: Bosworth LA, Downes S (eds) Electrospinning for tissue regeneration. Woodhead Publishing, Oxford, pp 298–316
Sultan N, Amin LE, Zaher AR, Scheven BA, Grawish ME (2019) Dental pulp stem cells: novel cell-based and cell-free therapy for peripheral nerve repair. World J Stomatol 7(1):1–19
Sunil PM (2016) Induced pluripotent stem cells in dentistry. J Pharm Bioallied Sci 8(Suppl 1):S23–Ss7
Tanikawa DYS, Pinheiro CCG, Almeida MCA, Oliveira C, Coudry RA, Rocha DL et al (2020) Deciduous dental pulp stem cells for maxillary alveolar reconstruction in cleft lip and palate patients. Stem Cells Int 2020:6234167
Tatullo M, Spagnuolo G, Codispoti B, Zamparini F, Zhang A, Esposti MD et al (2019) PLA-based mineral-doped scaffolds seeded with human periapical cyst-derived MSCs: a promising tool for regenerative healing in dentistry. Materials (Basel) 12(4):597
Thesleff I, Mikkola M (2002) The role of growth factors in tooth development. Int Rev Cytol 217:93–135
Tobita M, Uysal AC, Ogawa R, Hyakusoku H, Mizuno H (2008) Periodontal tissue regeneration with adipose-derived stem cells. Tissue Eng Part A 14(6):945–953
Tomokiyo A, Wada N, Maeda H (2019) Periodontal ligament stem cells: regenerative potency in periodontium. Stem Cells Dev 28(15):974–985
Vagropoulou G, Trentsiou M, Georgopoulou A, Papachristou E, Prymak O, Kritis A et al (2021) Hybrid chitosan/gelatin/nanohydroxyapatite scaffolds promote odontogenic differentiation of dental pulp stem cells and in vitro biomineralization. Dent Mater 37(1):e23–e36
Vainio S, Karavanova I, Jowett A, Thesleff I (1993) Identification of BMP-4 as a signal mediating secondary induction between epithelial and mesenchymal tissues during early tooth development. Cell 75(1):45–58
Vaseenon S, Chattipakorn N, Chattipakorn SC (2020) The possible role of basic fibroblast growth factor in dental pulp. Arch Oral Biol 109:104574
Wan PX, Wang BW, Wang ZC (2015) Importance of the stem cell microenvironment for ophthalmological cell-based therapy. World J Stem Cells 7(2):448–460
Wang J, Liu X, Jin X, Ma H, Hu J, Ni L et al (2010) The odontogenic differentiation of human dental pulp stem cells on nanofibrous poly(L-lactic acid) scaffolds in vitro and in vivo. Acta Biomater 6(10):3856–3863
Wang T, Tang W, Zeng Q, Miao S, Pi C, Li Y et al (2022a) Generation of induced pluripotent stem cell line (FMCPGHi001-a) from a 25-year-old Chinese Han healthy male donor. Stem Cell Res 60:102735
Wang J, Zhang D, Zhu Y, Mo X, McHugh PC, Tong Q (2022b) Astragalus and human mesenchymal stem cells promote wound healing by mediating immunomodulatory effects through paracrine signaling. Regen Med 17(4):219–232
Woo KM, Chen VJ, Jung HM, Kim TI, Shin HI, Baek JH et al (2009) Comparative evaluation of nanofibrous scaffolding for bone regeneration in critical-size calvarial defects. Tissue Eng Part A 15(8):2155–2162
Wu X, Qin K, Wang D, Xiang K, Peng J, Guo J et al (2022) Ultrasound-guided induced pluripotent stem cell-derived cardiomyocyte implantation in myocardial infarcted mice. J Vis Exp 181
Yamada Y, Ueda M, Hibi H, Baba S (2006) A novel approach to periodontal tissue regeneration with mesenchymal stem cells and platelet-rich plasma using tissue engineering technology: a clinical case report. Int J Periodontics Restorative Dent 26(4):363–369
Yamamiya K, Okuda K, Kawase T, Hata K, Wolff LF, Yoshie H (2008) Tissue-engineered cultured periosteum used with platelet-rich plasma and hydroxyapatite in treating human osseous defects. J Periodontol 79(5):811–818
Yao L, Flynn N (2018) Dental pulp stem cell-derived chondrogenic cells demonstrate differential cell motility in type I and type II collagen hydrogels. Spine J 18(6):1070–1080
Yao S, Norton J, Wise GE (2004) Stability of cultured dental follicle cells. Cell Prolif 37(3):247–254
Yen AH-H, Sharpe PT (2008) Stem cells and tooth tissue engineering. Cell Tissue Res 331(1):359–372
Yin S, Zhang W, Zhang Z, Jiang X (2019) Recent advances in scaffold design and material for vascularized tissue-engineered bone regeneration. Adv Healthc Mater 8(10):e1801433
Young CS, Terada S, Vacanti JP, Honda M, Bartlett JD, Yelick PC (2002) Tissue engineering of complex tooth structures on biodegradable polymer scaffolds. J Dent Res 81(10):695–700
Yuan B, Zhou SY, Chen XS (2017) Rapid prototyping technology and its application in bone tissue engineering. J Zhejiang Univ Sci B 18(4):303–315
Yuan H, Xing K, Hsu HY (2018) Trinity of three-dimensional (3D) scaffold, vibration, and 3D printing on cell culture application: a systematic review and indicating future direction. Bioengineering (Basel) 5(3):57
Zbańska J, Herman K, Kuropka P, Dobrzyński M (2021) Regenerative endodontics as the future treatment of immature permanent teeth. Appl Sci 11(13):6211
Zhai Q, Dong Z, Wang W, Li B, Jin Y (2019) Dental stem cell and dental tissue regeneration. Front Med 13(2):152–159
Zhang Y, Chen Y (2014) Bioengineering of a human whole tooth: progress and challenge. Cell Regen 3(1):8
Zhang W, Walboomers XF, van Kuppevelt TH, Daamen WF, Bian Z, Jansen JA (2006) The performance of human dental pulp stem cells on different three-dimensional scaffold materials. Biomaterials 27(33):5658–5668
Zhang W, Walboomers XF, van Osch GJ, van den Dolder J, Jansen JA (2008) Hard tissue formation in a porous HA/TCP ceramic scaffold loaded with stromal cells derived from dental pulp and bone marrow. Tissue Eng Part A 14(2):285–294
Zhang L, Morsi Y, Wang Y, Li Y, Ramakrishna S (2013) Review scaffold design and stem cells for tooth regeneration. Jpn Dent Sci Rev 49(1):14–26
Zhang F, Song J, Zhang H, Huang E, Song D, Tollemar V et al (2016) Wnt and BMP signaling crosstalk in regulating dental stem cells: implications in dental tissue engineering. Genes Dis 3(4):263–276
Zhao M, Jin Q, Berry JE, Nociti FH Jr, Giannobile WV, Somerman MJ (2004) Cementoblast delivery for periodontal tissue engineering. J Periodontol 75(1):154–161
Zhu B, Liu Y, Li D, Jin Y (2013) Somatic stem cell biology and periodontal regeneration. Int J Oral Maxillofac Implants 28(6):e494–e502
Zi Z (2019) Molecular engineering of the TGF-β signaling pathway. J Mol Biol 431(15):2644–2654
Acknowledgments
The authors would like to acknowledge Dr. Mohsen khorshidi and Mrs. Shokouh Salimi for their kind support.
Funding
None.
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Tayanloo-Beik, A. et al. (2022). Application of Biocompatible Scaffolds in Stem-Cell-Based Dental Tissue Engineering. In: Turksen, K. (eds) Cell Biology and Translational Medicine, Volume 18. Advances in Experimental Medicine and Biology(), vol 1409. Springer, Cham. https://doi.org/10.1007/5584_2022_734
Download citation
DOI: https://doi.org/10.1007/5584_2022_734
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-28423-6
Online ISBN: 978-3-031-28424-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)