Abstract
Biomedical engineering breakthroughs and increased patient expectations and requests for more comprehensive care are propelling the field of regenerative dentistry forward at a fast pace. Stem cells (SCs), bioactive compounds, and scaffolds are the mainstays of tissue engineering, the backbone of regenerative dentistry. Repairing damaged teeth and gums is a significant scientific problem at present. Novel therapeutic approaches for tooth and periodontal healing have been inspired by tissue engineering based on mesenchymal stem cells (MSCs). Furthermore, as a component of the MSC secretome, extracellular vesicles (EVs) have been shown to contribute to periodontal tissue repair and regeneration. The scaffold, made of an artificial extracellular matrix (ECM), acts as a supporting structure for new cell development and tissue formation. To effectively promote cell development, a scaffold must be non-toxic, biodegradable, biologically compatible, low in immunogenicity, and safe. Due to its promising biological characteristics for cell regeneration, dental tissue engineering has recently received much attention for its use of natural or synthetic polymer scaffolds with excellent mechanical properties, such as small pore size and a high surface-to-volume ratio, as a matrix. Moreover, as a bioactive material for carrying MSC-EVs, the combined application of scaffolds and MSC-EVs has a better regenerative effect on dental diseases. In this paper, we discuss how MSCs and MSC-derived EV treatment may be used to regenerate damaged teeth, and we highlight the role of various scaffolds in this process.
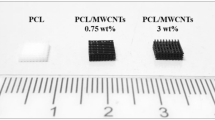
Graphical Abstract
The potential of utilizing mesenchymal stem cells (MSCs) and their derivatives (MSC-EVs) inserted into the scaffold to regenerate dental diseases is illustrated in this figure. Synthetic and natural scaffolds transport these cells to facilitate their safe and targeted delivery to the intended tissue.








Similar content being viewed by others
Data Availability
Not applicable.
References
Ortiz, G. G. R., et al. (2023). A state-of-the-art review on the MicroRNAs roles in hematopoietic stem cell aging and longevity. Cell Communication and Signaling, 21(1), 1–16.
Faghihkhorasani, A., et al. (2023). The role of oncolytic virotherapy and viral oncogenes in the cancer stem cells: A review of virus in cancer stem cells. Cancer Cell International, 23(1), 250.
Mahjoor, M., et al. (2021). MicroRNA-30c delivered by bone marrow-mesenchymal stem cells induced apoptosis and diminished cell invasion in U-251 glioblastoma cell line. Life Sciences, 279, 119643.
Andalib, E., et al. (2023). Application of hypoxia-mesenchymal stem cells in treatment of anaerobic bacterial wound infection: Wound healing and infection recovery. Frontiers in Microbiology, 14, 1251956.
Yasamineh, S., et al. (2022). Spotlight on therapeutic efficiency of mesenchymal stem cells in viral infections with a focus on COVID-19. Stem Cell Research & Therapy, 13(1), 257.
Oveili, E., et al. (2023). The potential use of mesenchymal stem cells-derived exosomes as microRNAs delivery systems in different diseases. Cell Communication and Signaling, 21(1), 1–26.
Squillaro, T., Peluso, G., & Galderisi, U. (2016). Clinical trials with mesenchymal stem cells: An update. Cell Transplantation, 25(5), 829–848.
Nasiri, K., et al. (2023). Spotlight on the impact of viral infections on Hematopoietic Stem Cells (HSCs) with a focus on COVID-19 effects. Cell Communication and Signaling, 21(1), 1–15.
Chalisserry, E. P., et al. (2017). Therapeutic potential of dental stem cells. Journal of Tissue Engineering, 8, 2041731417702531.
Egusa, H., et al. (2012). Stem cells in dentistry–part I: Stem cell sources. Journal of Prosthodontic Research, 56(3), 151–165.
Lotfy, A., AboQuella, N. M., & Wang, H. (2023). Mesenchymal stromal/stem cell (MSC)-derived exosomes in clinical trials. Stem Cell Research & Therapy, 14(1), 1–18.
Estrela, C., et al. (2011). Mesenchymal stem cells in the dental tissues: Perspectives for tissue regeneration. Brazilian Dental Journal, 22, 91–98.
Potdar, P. D., & Jethmalani, Y. D. (2015). Human dental pulp stem cells: Applications in future regenerative medicine. World Journal of Stem Cells, 7(5), 839.
Andrukhov, O., Blufstein, A., & Behm, C. (2021). A review of antimicrobial activity of dental mesenchymal stromal cells: Is there any potential? Front Oral Health, 2, 832976.
Mirshekar, M., et al. (2023). Potential antibacterial activity and healing effect of topical administration of bone marrow and adipose mesenchymal stem cells encapsulated in collagen-fibrin hydrogel scaffold on full-thickness burn wound infection caused by Pseudomonas aeruginosa. Burns. https://pubmed.ncbi.nlm.nih.gov/38042618/
Hosseini-Asl, S.-K., Mehrabani, D., & Karimi-Busheri, F. (2020). Therapeutic effect of mesenchymal stem cells in ulcerative colitis: A review on achievements and challenges. Journal of Clinical Medicine, 9(12), 3922.
Mehrabani, D., et al. (2022). The ameliorating effect of adipose tissue stem cells on liver function in experimental rats with liver fibrosis. International Journal of Nutrition Sciences, 7(4), 225–232.
Rodríguez-Lozano, F.-J., et al. (2012). Mesenchymal dental stem cells in regenerative dentistry. Medicina Oral, Patologia Oral y Cirugia Bucal, 17(6), e1062.
Jalli, R., et al. (2023). Cell proliferation, viability, differentiation, and apoptosis of iron oxide labeled stem cells transfected with lipofectamine assessed by MRI. Journal of Clinical Medicine, 12(6), 2395.
Théry, C., et al. (2018). Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. Journal of Extracellular Vesicles, 7(1), 1535750.
Wang, M., et al. (2019). Efficient angiogenesis-based diabetic wound healing/skin reconstruction through bioactive antibacterial adhesive ultraviolet shielding nanodressing with exosome release. ACS Nano, 13(9), 10279–10293.
Yamashita, T., Takahashi, Y., & Takakura, Y. (2018). Possibility of exosome-based therapeutics and challenges in production of exosomes eligible for therapeutic application. Biological and Pharmaceutical Bulletin, 41(6), 835–842.
Casado-Díaz, A., Quesada-Gómez, J. M., & Dorado, G. (2020). Extracellular vesicles derived from mesenchymal stem cells (MSC) in regenerative medicine: Applications in skin wound healing. Frontiers in Bioengineering and Biotechnology, 8, 146.
Tatullo, M., et al. (2023). Unlocking the potential of dental-derived mesenchymal stem cells in regenerative medicine. 3804. (MDPI). https://pubmed.ncbi.nlm.nih.gov/37297998/
Stamnitz, S., & Klimczak, A. (2021). Mesenchymal stem cells, bioactive factors, and scaffolds in bone repair: From research perspectives to clinical practice. Cells, 10(8), 1925.
Shaikh, F., et al. (2023). Mesenchymal stem cells and tissue engineering in dentistry. https://www.intechopen.com/online-first/1149780
Liu, Z., et al. (2022). Extracellular vesicles: A potential future strategy for dental and maxillofacial tissue repair and regeneration. Frontiers in Physiology, 13, 1012241.
Wu, X., et al. (2020). Mesenchymal stromal cell therapies: Immunomodulatory properties and clinical progress. Stem Cell Research & Therapy, 11(1), 1–16.
Miceli, V., et al. (2021). Therapeutic properties of mesenchymal stromal/stem cells: The need of cell priming for cell-free therapies in regenerative medicine. International Journal of Molecular Sciences, 22(2), 763.
Slots, J. (2017). Periodontitis: Facts, fallacies and the future. Periodontology 2000, 75(1), 7–23.
Galler, K. (2016). Clinical procedures for revitalization: Current knowledge and considerations. International Endodontic Journal, 49(10), 926–936.
Lin, L., et al. (2021). Clinical cell-based versus cell-free regenerative endodontics: Clarification of concept and term. International Endodontic Journal, 54(6), 887–901.
Nasiri, K., et al. (2023). MicroRNAs function in dental stem cells as a promising biomarker and therapeutic target for dental diseases. Molecular Diagnosis & Therapy, 1–20. https://pubmed.ncbi.nlm.nih.gov/37773247/
Lovelace, T. W., et al. (2011). Evaluation of the delivery of mesenchymal stem cells into the root canal space of necrotic immature teeth after clinical regenerative endodontic procedure. Journal of Endodontics, 37(2), 133–138.
Wang, L.-H., et al. (2022). An up-to-date overview of dental tissue regeneration using dental origin mesenchymal stem cells: Challenges and road ahead. Frontiers in Bioengineering and Biotechnology, 10, 855396.
da Silva, G. S., et al. (2020). Current evidence of tissue engineering for dentine regeneration in animal models: A systematic review. Regenerative Medicine, 15(2), 1345–1360.
Nasiri, K., et al. (2023). Recent advances in metal nanoparticles to treat periodontitis. Journal of Nanobiotechnology, 21(1), 283.
Gan, L., et al. (2020). Dental tissue-derived human mesenchymal stem cells and their potential in therapeutic application. Stem Cells International, 2020. https://pubmed.ncbi.nlm.nih.gov/32952572/
Shi, S., et al. (2005). The efficacy of mesenchymal stem cells to regenerate and repair dental structures. Orthodontics & Craniofacial Research, 8(3), 191–199.
Mashimo, T., et al. (2019). Bone marrow-derived mesenchymal stem cells enhance bone marrow regeneration in dental extraction sockets. Journal of Oral Science, 61(2), 284–293.
Ng, R., et al. (2012). Three-dimensional fibrous scaffolds with microstructures and nanotextures for tissue engineering. RSC Advances, 2(27), 10110–10124.
Raghav, P. K., et al. (2022). Mesenchymal stem cell-based nanoparticles and scaffolds in regenerative medicine. European Journal of Pharmacology, 918, 174657.
Chan, B. P., & Leong, K. W. (2008). Scaffolding in tissue engineering: General approaches and tissue-specific considerations. European Spine Journal, 17 Suppl 4(Suppl 4), 467–79.
Hosseinkhani, M., et al. (2014). Tissue engineered scaffolds in regenerative medicine. World Journal of Plastic Surgery, 3(1), 3–7.
Sarkhosh-Inanlou, R., et al. (2021). Applications of scaffold-based advanced materials in biomedical sensing. TrAC Trends in Analytical Chemistry, 143, 116342.
Willerth, S. M., & Sakiyama-Elbert, S. E. (2019). Combining stem cells and biomaterial scaffolds for constructing tissues and cell delivery. StemJournal, 1(1), 1–25.
Sakai, S., et al. (2009). An injectable, in situ enzymatically gellable, gelatin derivative for drug delivery and tissue engineering. Biomaterials, 30(20), 3371–3377.
Ahmed, E. M. (2015). Hydrogel: Preparation, characterization, and applications: A review. Journal of Advanced Research, 6(2), 105–121.
Singh, M. R., Patel, S., & Singh, D. (2016). Natural polymer-based hydrogels as scaffolds for tissue engineering. Nanobiomaterials in soft tissue engineering (pp. 231–260). Elsevier.
Samiei, M., et al. (2021). Bioactive hydrogel-based scaffolds for the regeneration of dental pulp tissue. Journal of Drug Delivery Science and Technology, 64, 102600.
Singh, H., et al. (2021). Pulp regeneration in an immature maxillary central incisor using hyaluronic acid hydrogel. Contemporary Clinical Dentistry, 12(1), 94.
Xiong, X., et al. (2021). Enhanced proliferation and angiogenic phenotype of endothelial cells via negatively-charged alginate and chondroitin sulfate microsphere hydrogels. Biomedical Materials, 16(2), 025012.
Fu, Y., et al. (2021). Poly ethylene glycol (PEG)-Related controllable and sustainable antidiabetic drug delivery systems. European Journal of Medicinal Chemistry, 217, 113372.
Chen, A., et al. (2023). Hydrogels for oral tissue engineering: Challenges and opportunities. Molecules, 28(9), 3946.
Pillay, V., et al. (2013). A review of the effect of processing variables on the fabrication of electrospun nanofibers for drug delivery applications. Journal of Nanomaterials, 2013. https://www.hindawi.com/journals/jnm/2013/789289/
Mirjalili, M., & Zohoori, S. (2016). Review for application of electrospinning and electrospun nanofibers technology in textile industry. Journal of Nanostructure in Chemistry, 6, 207–213.
Zafar, M., et al. (2016). Potential of electrospun nanofibers for biomedical and dental applications. Materials, 9(2), 73.
Wu, S., et al. (2014). Biomimetic porous scaffolds for bone tissue engineering. Materials Science and Engineering: R: Reports, 80, 1–36.
Chaudhari, A. A., et al. (2016). Future prospects for scaffolding methods and biomaterials in skin tissue engineering: A review. International Journal of Molecular Sciences, 17(12), 1974.
Jun, I., et al. (2018). Electrospun fibrous scaffolds for tissue engineering: Viewpoints on architecture and fabrication. International Journal of Molecular Sciences, 19(3), 745.
Budai-Szűcs, M., et al. (2021). Electrospun scaffolds in periodontal wound healing. Polymers, 13(2), 307.
Wu, J., & Hong, Y. (2016). Enhancing cell infiltration of electrospun fibrous scaffolds in tissue regeneration. Bioactive Materials, 1(1), 56–64.
Zhu, W., et al. (2015). Cold atmospheric plasma modified electrospun scaffolds with embedded microspheres for improved cartilage regeneration. PLoS ONE, 10(7), e0134729.
Abbaszadeh, H., et al. (2022). Chronic obstructive pulmonary disease and asthma: Mesenchymal stem cells and their extracellular vesicles as potential therapeutic tools. Stem Cell Research & Therapy, 13(1), 1–15.
Bellas, E., Marra, K. G., & Kaplan, D. L. (2013). Sustainable three-dimensional tissue model of human adipose tissue. Tissue Engineering Part C: Methods, 19(10), 745–754.
Bellas, E., et al. (2013). Sustained volume retention in vivo with adipocyte and lipoaspirate seeded silk scaffolds. Biomaterials, 34(12), 2960–2968.
Wu, I., & Elisseeff, J. (2014). Biomaterials and tissue engineering for soft tissue reconstruction. Natural and synthetic biomedical polymers (pp. 235–241). Elsevier.
Yanat, M., & Schroën, K. (2021). Preparation methods and applications of chitosan nanoparticles; with an outlook toward reinforcement of biodegradable packaging. Reactive and Functional Polymers, 161, 104849.
Yang, B., et al. (2010). Preparation and characterization of a novel chitosan scaffold. Carbohydrate Polymers, 80(3), 860–865.
Wieckiewicz, M., et al. (2017). Clinical application of chitosan in dental specialities. Mini Reviews in Medicinal Chemistry, 17(5), 401–409.
Li, F., et al. (2014). Porous chitosan bilayer membrane containing TGF-β1 loaded microspheres for pulp capping and reparative dentin formation in a dog model. Dental Materials, 30(2), 172–181.
Sukpaita, T., et al. (2021). Chitosan-based scaffold for mineralized tissues regeneration. Marine Drugs, 19(10), 551.
Farzin, A., et al. (2020). Scaffolds in dental tissue engineering: A review. Archives of Neuroscience, 7(1). https://brieflands.com/articles/ans-97014
Gathani, K. M., & Raghavendra, S. S. (2016). Scaffolds in regenerative endodontics: A review. Dental Research Journal, 13(5), 379.
Galli, M., et al. (2021). Current and future trends in periodontal tissue engineering and bone regeneration. Plastic and Aesthetic Research, 8. https://pubmed.ncbi.nlm.nih.gov/35765666/
Yasamineh, S., et al. (2023). Future prospects of natural polymer-based drug delivery systems in combating lung diseases. Natural polymeric materials based drug delivery systems in lung diseases (pp. 465–482). Springer.
Li, R., et al. (2011). Human treated dentin matrix as a natural scaffold for complete human dentin tissue regeneration. Biomaterials, 32(20), 4525–4538.
Moonesi Rad, R., et al. (2019). In vitro performance of a nanobiocomposite scaffold containing boron-modified bioactive glass nanoparticles for dentin regeneration. Journal of Biomaterials Applications, 33(6), 834–853.
Machla, F., et al. (2023). Tissue engineering at the dentin-pulp interface using human treated dentin scaffolds conditioned with DMP1 or BMP2 plasmid DNA-carrying calcium phosphate nanoparticles. Acta Biomaterialia, 159, 156–172.
Zhu, X., et al. (2018). A miniature swine model for stem cell-based de novo regeneration of dental pulp and dentin-like tissue. Tissue Engineering Part C: Methods, 24(2), 108–120.
Hasani-Sadrabadi, M. M., et al. (2020). An engineered cell-laden adhesive hydrogel promotes craniofacial bone tissue regeneration in rats. Science Translational Medicine, 12(534), eaay6853.
Sugiaman, V. K., & Jeffrey. (2023). Polymeric scaffolds used in dental pulp regeneration by tissue engineering approach. 15(5). https://pubmed.ncbi.nlm.nih.gov/36904323/
Bakhtiar, H., et al. (2018). The role of stem cell therapy in regeneration of dentine-pulp complex: A systematic review. Progress in Biomaterials, 7, 249–268.
Badylak, S. F., Freytes, D. O., & Gilbert, T. W. (2009). Extracellular matrix as a biological scaffold material: Structure and function. Acta Biomaterialia, 5(1), 1–13.
Badylak, S. F. (2007). The extracellular matrix as a biologic scaffold material. Biomaterials, 28(25), 3587–3593.
Ma, P. X. (2004). Scaffolds for tissue fabrication. Materials Today, 7(5), 30–40.
Wu, D. T., & Munguia-Lopez, J. G. (2021). Polymeric scaffolds for dental, oral, and craniofacial regenerative medicine. 26(22). https://pubmed.ncbi.nlm.nih.gov/34834134/
Li, W.-J., et al. (2005). Multilineage differentiation of human mesenchymal stem cells in a three-dimensional nanofibrous scaffold. Biomaterials, 26(25), 5158–5166.
Koh, B., et al. (2021). Mesenchymal stem cells: A comprehensive methods for odontoblastic induction. 23(1), 18. https://biologicalproceduresonline.biomedcentral.com/articles/10.1186/s12575-021-00155-7
Luo, S., et al. (2017). Bone marrow mesenchymal stem cells combine with Treated dentin matrix to build biological root. Science and Reports, 7, 44635.
Moshaverinia, A., et al. (2013). Encapsulated dental-derived mesenchymal stem cells in an injectable and biodegradable scaffold for applications in bone tissue engineering. Journal of Biomedical Materials Research Part A, 101(11), 3285–3294.
Lau, C. S., et al. (2022). A porcine model using adipose stem cell-loaded scaffolds for alveolar ridge augmentation. Tissue Engineering Part C: Methods, 28(5), 228–237.
Tan, W. L., et al. (2012). A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clinical Oral Implants Research, 23, 1–21.
Kulakov, A., et al. (2017). Modern approaches to dental implants placement in deficient alveolar bone. Stomatologiia, 96(1), 43–45.
Almansoori, A. A., et al. (2021). Mesenchymal stem cells and platelet-rich plasma-impregnated polycaprolactone-β tricalcium phosphate bio-scaffold enhanced bone regeneration around dental implants. International Journal of Implant Dentistry, 7(1), 1–8.
Vakhrushev, I., et al. (2012). Design of tissue engineering implants for bone tissue regeneration of the basis of new generation polylactoglycolide scaffolds and multipotent mesenchymal stem cells from human exfoliated deciduous teeth (SHED cells). Bulletin of Experimental Biology and Medicine, 153, 143–147.
Marei, M. K., & El Backly, R. M. (2018). Dental mesenchymal stem cell-based translational regenerative dentistry: From artificial to biological replacement. Frontiers in Bioengineering and Biotechnology, 6, 49.
Durmuslar, M. C., et al. (2016). Histological evaluation of the effect of concentrated growth factor on bone healing. Journal of Craniofacial Surgery, 27(6), 1494–1497.
Kämmerer, P. W., et al. (2017). Influence of platelet-derived growth factor on osseous remodeling properties of a variable-thread tapered dental implant in vivo. Clinical Oral Implants Research, 28(2), 201–206.
Kämmerer, P. W., et al. (2017). Guided bone regeneration using collagen scaffolds, growth factors, and periodontal ligament stem cells for treatment of peri-implant bone defects in vivo. Stem Cells International, 2017. https://pubmed.ncbi.nlm.nih.gov/28951742/
Ding, L., et al. (2019). Bone regeneration of canine peri-implant defects using cell sheets of adipose-derived mesenchymal stem cells and platelet-rich fibrin membranes. Journal of Oral and Maxillofacial Surgery, 77(3), 499–514.
Diniz, I. M., et al. (2016). Gingival mesenchymal stem cell (GMSC) Delivery system based on RGD-coupled alginate hydrogel with antimicrobial properties: A novel treatment modality for peri-implantitis. Journal of Prosthodontics, 25(2), 105–115.
Chen, M., et al. (2022). Constructions of ROS-responsive titanium-hydroxyapatite implant for mesenchymal stem cell recruitment in peri-implant space and bone formation in osteoporosis microenvironment. Bioactive Materials, 18, 56–71.
Ivica, A., Zehnder, M., & Weber, F. (2021). Therapeutic potential of mesenchymal stem cell-derived extracellular vesicles in regenerative endodontics. European Cells and Materials (ECM), 41, 233–244.
Amato, M., et al. (2022). Impact of oral mesenchymal stem cells applications as a promising therapeutic target in the therapy of periodontal disease. International Journal of Molecular Sciences, 23(21), 13419.
Yamada, Y., et al. (2015). Papilla regeneration by injectable stem cell therapy with regenerative medicine: Long-term clinical prognosis. Journal of Tissue Engineering and Regenerative Medicine, 9(3), 305–309.
Kiarashi, M., et al. (2024). Spotlight on therapeutic efficiency of green synthesis metals and their oxide nanoparticles in periodontitis. Journal of Nanobiotechnology, 22(1), 1–37.
Liu, J., et al. (2019). Periodontal bone-ligament-cementum regeneration via scaffolds and stem cells. Cells, 8(6), 537.
Cui, D., et al. (2018). The origin and identification of mesenchymal stem cells in teeth: From odontogenic to non-odontogenic. Current Stem Cell Research & Therapy, 13(1), 39–45.
Leite, YKd. C., et al. (2023). Novel scaffold based on chitosan hydrogels/phthalated cashew gum for supporting human dental pulp stem cells. Pharmaceuticals, 16(2), 266.
Yan, N., et al. (2022). Stem cell Janus patch for periodontal regeneration. Nano Today, 42, 101336.
Tahlawi, A., & Klontzas M. E. (2019). RGD-functionalized polyurethane scaffolds promote umbilical cord blood mesenchymal stem cell expansion and osteogenic differentiation. 13(2), 232–243. https://pubmed.ncbi.nlm.nih.gov/30537385/
Ouchi, T., & Nakagawa, T. (2020). Mesenchymal stem cell-based tissue regeneration therapies for periodontitis. Regenerative Therapy, 14, 72–78.
Wang, F., Du, L., & Ge, S. (2016). PTH/SDF-1α cotherapy induces CD90+ CD34− stromal cells migration and promotes tissue regeneration in a rat periodontal defect model. Scientific Reports, 6(1), 30403.
Liang, Q., et al. (2021). Stromal cell-derived factor-1/Exendin-4 cotherapy facilitates the proliferation, migration and osteogenic differentiation of human periodontal ligament stem cells in vitro and promotes periodontal bone regeneration in vivo. Cell Proliferation, 54(3), e12997.
Meng, L., et al. (2022). Stem cell homing in periodontal tissue regeneration. Frontiers in Bioengineering and Biotechnology, 10, 1017613.
Jung, Y.-H., et al. (2023). Regenerative potential of bone morphogenetic protein 7-engineered mesenchymal stem cells in ligature-induced periodontitis. Tissue Engineering Part A, 29(7–8), 200–210.
Wang, W., et al. (2023). Potential of an aligned porous hydrogel scaffold combined with periodontal ligament stem cells or gingival mesenchymal stem cells to promote tissue regeneration in rat periodontal defects. ACS Biomaterials Science & Engineering, 9(4), 1961–1975.
Moshaverinia, A., et al. (2014). Bone regeneration potential of stem cells derived from periodontal ligament or gingival tissue sources encapsulated in RGD-modified alginate scaffold. Tissue Engineering Part A, 20(3–4), 611–621.
Malekahmadi, B., et al. (2022). In vitro study of the recruitment and expansion of mesenchymal stem cells at the interface of a Cu-doped PCL-bioglass scaffold. Biomimetics, 7(1), 19.
Sone, H., et al. (2022). Clumps of mesenchymal stem cells/extracellular matrix complexes directly reconstruct the functional periodontal tissue in a rat periodontal defect model. Journal of Tissue Engineering and Regenerative Medicine, 16(10), 945–955.
Lombardo, G., et al. (2018). IL-3R-alpha blockade inhibits tumor endothelial cell-derived extracellular vesicle (EV)-mediated vessel formation by targeting the β-catenin pathway. Oncogene, 37(9), 1175–1191.
Adamo, A., et al. (2019). Extracellular vesicles mediate mesenchymal stromal cell-dependent regulation of B cell PI3K-AKT signaling pathway and actin cytoskeleton. Frontiers in Immunology, 10, 446.
Maggio, S., et al. (2019). Signal exchange through extracellular vesicles in neuromuscular junction establishment and maintenance: From physiology to pathology. International Journal of Molecular Sciences, 20(11), 2804.
Han, M., et al. (2020). Neuroprotective effect of mesenchymal stromal cell-derived extracellular vesicles against cerebral ischemia-reperfusion-induced neural functional injury: A pivotal role for AMPK and JAK2/STAT3/NF-κB signaling pathway modulation. Drug Design, Development and Therapy, 2865–2876. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7381771/
Lu, Y., et al. (2022). Biomaterials constructed for MSC-derived extracellular vesicle loading and delivery—a promising method for tissue regeneration. Frontiers in Cell and Developmental Biology, 10, 898394.
Tsiapalis, D., & O’Driscoll, L. (2020). Mesenchymal stem cell derived extracellular vesicles for tissue engineering and regenerative medicine applications. Cells, 9(4), 991.
Liang, X., et al. (2014). Paracrine mechanisms of mesenchymal stem cell-based therapy: Current status and perspectives. Cell Transplantation, 23(9), 1045–1059.
Jafarinia, M., et al. (2020). Mesenchymal stem cell-derived extracellular vesicles: A novel cell-free therapy. Immunological Investigations, 49(7), 758–780.
Keshtkar, S., Azarpira, N., & Ghahremani, M. H. (2018). Mesenchymal stem cell-derived extracellular vesicles: Novel frontiers in regenerative medicine. Stem Cell Research & Therapy, 9, 1–9.
Lei, F., et al. (2022). Treatment of inflammatory bone loss in periodontitis by stem cell-derived exosomes. Acta Biomaterialia, 141, 333–343.
Zhao, Y., et al. (2022). The experimental study of periodontal ligament stem cells derived exosomes with hydrogel accelerating bone regeneration on alveolar bone defect. Pharmaceutics, 14(10), 2189.
Faghihkhorasani, A., et al. (2023). The potential use of bacteria and bacterial derivatives as drug delivery systems for viral infection. Virology Journal, 20(1), 222.
Jeske, R., et al. (2023). Upscaling human mesenchymal stromal cell production in a novel vertical-wheel bioreactor enhances extracellular vesicle secretion and cargo profile. Bioactive Materials, 25, 732–747.
Henne, W. M., Buchkovich, N. J., & Emr, S. D. (2011). The ESCRT pathway. Developmental Cell, 21(1), 77–91.
Lui, P. P. Y. (2021). Mesenchymal stem cell-derived extracellular vesicles for the promotion of tendon repair-an update of literature. Stem Cell Reviews and Reports, 17, 379–389.
Li, W., et al. (2018). Tissue-engineered bone immobilized with human adipose stem cells-derived exosomes promotes bone regeneration. ACS Applied Materials & Interfaces, 10(6), 5240–5254.
Zhou, H., et al. (2023). Mesenchymal stem cell-derived extracellular vesicles for treatment of bone loss within periodontitis in pre-clinical animal models: A meta-analysis. BMC Oral Health, 23(1), 701.
Liu, L., et al. (2021). Bone marrow mesenchymal stem cell-derived small extracellular vesicles promote periodontal regeneration. Tissue Engineering Part A, 27(13–14), 962–976.
Shi, W., et al. (2020). Small extracellular vesicles from lipopolysaccharide-preconditioned dental follicle cells promote periodontal regeneration in an inflammatory microenvironment. ACS Biomaterials Science & Engineering, 6(10), 5797–5810.
Diomede, F., Fonticoli, L., & Marconi, G. D. (2022). Decellularized dental pulp, extracellular vesicles, and 5-azacytidine: A new tool for endodontic regeneration. 10(2). https://pubmed.ncbi.nlm.nih.gov/35203612/
Bernardo, M., Pagliara, D., & Locatelli, F. (2012). Mesenchymal stromal cell therapy: A revolution in regenerative medicine? Bone Marrow Transplantation, 47(2), 164–171.
Andrukhov, O., et al. (2019). Immunomodulatory properties of dental tissue-derived mesenchymal stem cells: Implication in disease and tissue regeneration. World Journal of Stem Cells, 11(9), 604.
Sundelacruz, S., & Kaplan, D. L. (2009). Stem cell- and scaffold-based tissue engineering approaches to osteochondral regenerative medicine. Seminars in Cell & Developmental Biology, 20(6), 646–655.
Zhou, T., et al. (2021). Challenges and advances in clinical applications of mesenchymal stromal cells. Journal of Hematology & Oncology, 14(1), 1–24.
Adamo, A., et al. (2019). Role of mesenchymal stromal cell-derived extracellular vesicles in tumour microenvironment. Biochimica et Biophysica Acta (BBA)-Reviews on Cancer, 1871(1), 192–198.
Kou, M., et al. (2022). Mesenchymal stem cell-derived extracellular vesicles for immunomodulation and regeneration: A next generation therapeutic tool? Cell Death & Disease, 13(7), 580.
Blando, S., et al. (2022). Can a scaffold enriched with mesenchymal stem cells be a good treatment for spinal cord injury?. 23(14). https://pubmed.ncbi.nlm.nih.gov/35886890/
Brown, C., et al. (2019). Mesenchymal stem cells: Cell therapy and regeneration potential. Journal of Tissue Engineering and Regenerative Medicine, 13(9), 1738–1755.
De Luca, M., et al. (2019). Advances in stem cell research and therapeutic development. Nature Cell Biology, 21(7), 801–811.
Yu, Y., et al. (2016). Directing immunomodulation using biomaterials for endogenous regeneration. Journal of Materials Chemistry B, 4(4), 569–584.
Leach, D. G., Young, S., & Hartgerink, J. D. (2019). Advances in immunotherapy delivery from implantable and injectable biomaterials. Acta Biomaterialia, 88, 15–31.
Granz, C. L., & Gorji, A. (2020). Dental stem cells: The role of biomaterials and scaffolds in developing novel therapeutic strategies. World Journal of Stem Cells, 12(9), 897–921.
Acknowledgements
Special thanks to all the scientists and researchers who are concerned about relieving the pain of patients.
Funding
None.
Author information
Authors and Affiliations
Contributions
S.Y., S.S., M.M., K.N., and M.E: Writing – original draft and Conceptualization, Supervision, M.K., H.B., E.E., N.A., Writing – review & editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
All of author are consent for publication.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kiarashi, M., Bayat, H., Shahrtash, S.A. et al. Mesenchymal Stem Cell-based Scaffolds in Regenerative Medicine of Dental Diseases. Stem Cell Rev and Rep 20, 688–721 (2024). https://doi.org/10.1007/s12015-024-10687-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-024-10687-6