Abstract
3D printing, or additive manufacturing, is a transformative technology platform impacting various disciplines, including biomaterials and biomedical devices. We present scientists, engineers, and medical professionals' perspectives about 3D printing of biomaterials and biomedical devices in this special issue. This issue is geared towards understanding the structure–process–property relationships involving different materials in vitro, in vivo, and in silico environments. The focus issue covers polymer, ceramic, glass, metallic and composite biomaterials involving various 3D-printing processes such as fused deposition, powder bed fusion, Bioprinting, directed energy deposition, and binder jetting; addressing research topics including tissue engineering, drug delivery, porous metal implants, bioink development, cell–materials interactions, wear degradation, nano-bio materials, and challenges in point-of-care delivery. Such diversity of research topics is an accurate representation of what is happening in this field globally. This article presents some of the success stories, challenges, and future directions in the 3D printing of biomaterials and devices.
Graphic abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biomaterials are natural or synthetic materials used to repair damaged body parts while interacting with living systems. During the last century, metallic, ceramic, and polymeric biomaterials have drawn innovators to develop unique biomedical devices to improve the quality of human life. These materials cannot be toxic and should be friendly to body tissues to be effective. Figure 1 broadly outlines different synthetic biomaterials as a function of biocompatibility and elastic modulus. While biocompatibility is viewed as the primary marker for the biological response of a biomaterial, the elastic modulus is viewed the same way for mechanical performance. Metals are typically bioinert, while ceramics, glasses and polymers can be either bioinert or bioactive. Although many polymeric and ceramic materials are currently being used in commercial biomedical devices, only a few selected groups are mentioned in Fig. 1. For metals, however, only a few compositions are used in all biomedical devices, such as Ti6Al4V for load-bearing hip, knee implants, stainless steel 316L for fracture management devices, and CoCr alloys for articulating surfaces. For biopolymers, ultra-high molecular weight polyethylene (UHMWPE) or poly-ether ether ketone (PEEK) are used in weight-bearing structural applications such as hip, knee, and spinal implants. Polylactic glycolic acid (PLGA) or polycaprolactone (PCL) biopolymers are used in sutures and drug delivery applications where biodegradability is more critical than mechanical performance. Similarly, alumina, zirconia, or silicon nitride ceramics are used in load-bearing applications. Calcium phosphate ceramics and bioactive glasses are used in bone tissue engineering and drug delivery due to their inherent bioactivity coupled with partial or total biodegradability. Figure 2 shows different synthetic degradable biomaterials as a function of their degradation rates and initial strength. Although initial strength is essential, the degradation rates will determine the actual application of biomaterials. Ideally, degradable biomaterials should maintain their strength until the defect site heals, and only after that time, the selected biomaterial should show significant degradation. For example, a biomaterial used for defect repair in dentistry may require a different degradation rate than in a spinal fusion application. As for degradable materials, ceramics and polymers are commonly used with varying degradation kinetics for bone, muscle, or nerve regeneration applications. Among metals, Mg alloys are the most common and used mainly in cardiovascular devices such as stents or small fasteners.
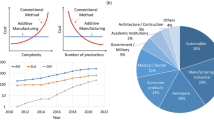
Most biomedical devices consist of multiple components made from different biomaterials or having varying structural features such as porous and dense areas in the same component, which are not easy to manufacture using a single conventional manufacturing operation. While it is essential to innovate new biomaterials with unique properties, it is also critical to establish reliable manufacturing practices to produce different biomedical devices. During the past decade, additive manufacturing (AM) or 3D printing has transformed biomedical device manufacturing—from porous scaffolds to surgical tools to patient-matched implants to innovative orthopedic, dental, and cardiovascular devices, to name a few [1]. The unique advantages of 3D printing, a layer-by-layer process, allows manufacturing complex structures on demand without using any part-specific tooling. The American Society for Testing and Materials (ASTM) has classified different 3D-printing technologies into seven broad categories, summarized in Table 1. Many of these seven processes are regularly used to make commercial biomedical devices. Vat photopolymerization is the first commercial process, commonly referred to as ‘stereolithography (SLA).’ A photopolymer resin is cured on a build plate using ultraviolet (UV) light to process parts using SLA. Since the printed part is fully immersed in the monomer liquid, the surface finish of SLA processed parts is smooth. Generally, polymer parts are produced by SLA; however, ceramic parts can also be formed via SLA using ceramic-filled monomers as a stock material [1,2,3]. Materials extrusion is another commonly used 3DP technique for biomedical devices, and a popular example is fused deposition modeling (FDM). In this approach, a neat thermoplastic filament is fed through a heated nozzle using counter-rotating rollers to extrude the build material along the x–y plane. The nozzle dimension controls the extruded size and shape. Once one layer is done, the next layer is deposited on top of the previous layer. Apart from making neat polymer parts, metal or ceramic powder-filled thermoplastic polymers can also be used as a feedstock material to make 3D-printed green metal or ceramic components after post-processing steps such as binder removal and sintering [1,2,3]. Binder jetting is another technique used for biomedical devices. In this process, polymer, metal, glass, or ceramic powder materials are used. A roller spreads the powder from a powder bed onto a build plate to form a thin uniform layer on which water-soluble or organic binder is deposited based on the tool path of the part file. The binder acts as a glue to bind the powders, and the surrounding loose powders act as support material. Because of this inherent support structure, parts with fine features can be made using this approach. Once the 3D printing is done, heating in an oven is necessary to cure the binder to strengthen the part for mechanical handling. Further heat treatment is necessary for metal and ceramic parts to sinter the parts for densification [1,2,3,4]. Powder bed fusion (PBF) is similar to binder jetting; however, the powder is heated using a laser or an electron beam for partial or complete densification during part fabrication. If the heat source is a laser and partial densification or sintering is achieved, then the process is called selective laser sintering or SLS, while the same for complete densification via melting is called selective laser melting or SLM. Similar to binder jetting, the unused powder acts as support material during the build process. In this approach, the total input energy is crucial for powder densification or melting that is controlled by factors such as laser power, scan speed, and layer thickness. SLM has become the leading 3D-printing technology for manufacturing metallic implants and devices [1, 2, 5]. E-beam is also used in manufacturing titanium-based implants. Another metal additive manufacturing process is directed energy deposition (DED), where a high-energy heat source melts free-flowing powders at the focal point on the build plate. The molten material is used to build a single layer. Unlike the powder bed process, different powders can be used in DED, which is ideal for manufacturing bimetallic and multi-material structures [6]. Moreover, less powder is sufficient to manufacture parts using DED as no powder bed is necessary. However, the DED yields poorer resolution compared to the powder bed fusion process. DED-based hybrid machines are becoming popular to improve part resolution where additive and subtractive processes are combined. DED is also widely used in the repair of expensive parts [1, 2]. Material jetting is another process similar to the DED, where thermoplastic or thermoset polymers are jetted on a substrate. Polymeric parts having vibrant colors can be printed using this approach, used for 3D-printed surgical models [2]. The last process is sheet lamination, which is used for paper-based and sheet metal-based products. However, very few biomaterials are manufactured using this process; however, multi-color surgical models can be printed [2].
Besides different biomaterials and 3D-printing processes, the applications are also another dimension of 3D printing of biomaterials and devices. Figure 3 summarizes all three key aspects—materials, processes, and applications. Among different applications, perhaps load-bearing orthopedic metal implants, low load-bearing dental implants, polymer-based surgical models, surgical tools, and patient-matched implants are the most advanced, where a large number of patients are already benefiting from advances in 3D-printing technologies worldwide. There is also significant research exploring the use of Bioprinting for organ tissue engineering, cardiovascular devices, as well as nerve and muscle regeneration [7]. Overall, the impact of 3D printing on biomedical devices will only continue to grow in the coming days.
3D printing of polymers for biomedical devices
The preliminary criteria for a polymer to qualify for tissue engineering are high bioresorbable or biodegradable properties, good mechanical strength, and enhanced cell attachment ability [8]. One of the significant hurdles in material selection is achieving desired pore size in the range of 300 to 600 microns and pore volume typically between 30 and 70% for tissue engineering scaffolds, which can be overcome using 3D-printing technology. Polylactic acid (PLA) and Polycaprolactone (PCL) are aliphatic polyesters widely used in first-generation tissue engineering. PLA and PCL are synthesized via ring-opening polymerization technique and have similar chemical compositions with different pendant groups. Such minute differences can contribute to a more significant effect on the physical properties of the polymer in terms of crystallinity and molecular weight, which would ultimately affect the degradation profiles [8]. Research has been carried out to evaluate the potential of 3D-printed PCL as drug-eluting implants. It was observed from the experimental readings that PCL biomaterial demonstrated a sustained drug release mechanism validated by the Korsmeyer-Peppas model that is mainly attributed to its slower degradation kinetics [9]. Similar observations on the functionalization of the 3D-printed silicone implants with gelatin hydrogel ensured the smooth release of the loaded biochemical mediators into the desired area [10]. Thus, a combination of 3D printing and proper biomaterial selection can generate patient-specific tissue constructs with desired mechanical strength and allow sustained release of specific drug molecules at the defect region to accelerate the healing process. PLA is one such polymeric material widely explored in bone tissue engineering. PLA scaffolds with an average pore size of 350 microns and 30% porosity were fabricated using an extrusion-based 3D-printing process and tested using osteosarcoma cells. Cells showed a high proliferation rate in 50% and 30% porous scaffolds while exhibiting necessary mechanical properties to support load-bearing bone growth [11].
Natural polymeric materials like alginate and silk fibroin are also widely explored for tissue regeneration and tissue remodeling applications. Extracted from the cell wall of algae or bacteria, Alginate is chemically composed of mannuronic acid and guluronic acid [12, 13]. Alginate hydrogels are characterized by high biocompatibility, solubility, and porosity, making them suitable for tissue engineering applications. Challenges about easy degradation, poor mechanical strength, and the absence of cell attachment restricted the use of standalone alginate hydrogel in biomimetic applications [12,13,14]. A blend of alginate and gelatin biomaterial was tested to assess the printability and cytocompatibility of the dual crosslinked scaffold in soft tissue engineering applications. High cytocompatibility with hemocompatibility has been observed in osteoblast cells along with apatite formation. The physicochemical characterization of the respective scaffold depicted a high printability making it a suitable biomaterial for 3D printing [15]. Other research groups have made similar attempts to combine alginate with silk [16], nanocellulose with hyaluronic acid [17] to impart enhanced cytocompatibility with superior rheological properties and mechanical strength for Bioprinting and tissue engineering applications.
Silk is another biomaterial for tissue engineering applications exploiting the chemical composition and amphiphilic nature added with advantages of tunable rheological and mechanical properties, making it an ideal 3D-printable biomaterial [18]. The viscosity of standalone silk fibroin protein is not satisfactory for the smooth extrusion process, whereas the addition of gelatin imparts shear thinning property to the ink and also affixes the arginine-glycine-aspartate (RGD) motifs for increased cell attachment [18]. Silk fibroin-gelatin (SF-G) and the Direct-Write (DW) technique have been used to fabricate a myriad of human tissue constructs and in vitro disease models. Silk fibroin serves as an appropriate niche to the growing cells and plays a crucial role in upregulating the Wnt/Beta-catenin pathway, a significant player in developmental biology-inspired chondrogenesis [19]. SF-G bioink has been pursued in fabricating full-thickness skin tissue [20] and in vitro 3D models for a wide range of disease conditions like osteoarthritis [21], hypertrophic scar [22], corneal scar [23] as well as liver organoids [24] for animal-free drug screening applications. Attempts have also been made using platelet-rich plasma (PRP)-gelatin methacrylate hydrogel scaffold prepared using SLM platform. The presence of PRP in the scaffold plays an integral role in osteogenic differentiation of cultured bone marrow-derived mesenchymal stem cells (BMSCs) as evaluated in vivo in the rabbit model [25]. These examples highlight the capabilities of 3D-printing technologies to process complex tissue constructs with pre-defined porosity and surface properties to enable successful tissue reconstruction.
3D printing of ceramics for biomedical devices
Bioceramics have been used in dentistry and orthopedics for many decades now. Since bioceramic materials are brittle, these are used in low load-bearing applications, bone void fillers as granules, or as coatings. Bioceramics are classified as (1) bioinert ceramics such as alumina and zirconia, and (2) bioactive and sometimes bioresorbable ceramics such as calcium phosphates. While bioinert ceramics are used in dentistry and articulating surfaces of load-bearing implants such as hip prostheses, bioactive ceramics are used in bone tissue engineering and drug delivery [26]. Traditionally, these ceramic structures are processed using casting or pressing, followed by binder removal and high-temperature densification or sintering. Using those processing approaches, making complex shapes and porous structures is always difficult. The advent of 3D-printing processes helped manufacture complex bioceramic parts reliably having dense and porous multifunctional structures [27]. Although binder jetting and stereolithography are the two most commonly used 3D-printing processes for bioceramics, other processes such as fused deposition of ceramics, robocasting, or direct-write technique, directed energy deposition, and selective laser sintering have also been used [28,29,30,31,32,33,34,35]. In most cases, ceramic structures are processed using a 3D-printing process, followed by post-processing steps to make high-density parts for final use. However, 3D-printing processes have also been used indirectly where a mold is made using 3D printing followed by slurry casting and heat treatment [36, 37]. For drug delivery applications, porous ceramic scaffolds are first made, followed by drug loading to avoid any degradation of drugs due to high-temperature processing. For the past two decades, there has been extensive research on processing, mechanical property measurements, and biocompatibility evaluations in vitro and in vivo of various calcium phosphate ceramic scaffolds [28,29,30,31,32,33,34,35,36,37]. To further enhance biocompatibility, induce osteoinductivity, and anti-microbial resistance, various dopants were added to calcium phosphate ceramics such as magnesium, zinc, strontium, and silver and processed via 3D printing [38,39,40,41]. Such doped calcium phosphate ceramics showed varied degradation kinetics, anti-microbial resistance, and early-stage osseointegration as well as angiogenesis [41,42,43]. Figure 4 shows 3D-printed ceramic scaffolds and bone tissue integration through the scaffolds [33, 35]. Both conventional and microwave heating has been used for post-processing 3D-printed ceramic scaffolds where microwave sintering clearly showed an advantage towards higher sintering kinetics [44]. Bioinert alumina and zirconia ceramics have also been processed using stereolithography-based photopolymerization and have shown good properties [45,46,47].
3D-printing processes have also been used to make ceramic–polymer composites where the polymer component is added to improve the processibility and flexibility of the part. Typically, PCL, PLA, or Poly lactide glycolic acid (PLGA) are used with calcium phosphate ceramics [42, 48, 49]. Ceramic–polymer paste has also been extruded with calcium phosphate, PCL, and starch to make porous scaffolds for drug delivery applications [50]. Similarly, polymer coatings have also been used with porous ceramic scaffolds to improve mechanical properties where the polymer layer reduces the inherent brittleness of the ceramic structure [36].
3D printing of bioactive glasses
Various 3D-printing techniques have been applied in the last decade to fabricate scaffolds and implants using bioactive glasses (BGs), glass–ceramics, and biopolymer–bioactive glass composites. The literature analysis indicates that most studies have considered bioactive glass of the 45S5 composition (45 SiO2, 24.5 CaO, 24.5 Na2O, and 6 P2O5—in wt%) due to its broad availability. However, other melt-derived bioactive glass formulations and sol–gel-derived BGs are also being investigated for 3D printing of biomedical devices, specially scaffolds for bone tissue engineering. As the geometrical accuracy and mechanical properties of the fabricated parts vary among the different 3D-printing technologies, in-depth knowledge of the detailed capabilities of each technique should provide information about their relative advantages and disadvantages when applied to bioactive glasses.
It is well known that lithography-based 3D printing provides accurate control of 3D morphology and pore architecture, offering an excellent alternative to existing bone implant and scaffold fabrication methods. The first study showing bioactive glass 45S5 BG processing by stereolithographic ceramic manufacturing (SLCM) was published in 2012 [51]. However, those early scaffolds suffered low mechanical strength, ascribed to a non-optimized sintering process [52]. SLCM has also been applied to obtain dense parts of crystallized 45S5 BG with adequate biaxial bending strength [53], achieving values similar to cortical bone. Such high mechanical strength was due to eliminating structural defects and high density (> 90%) achieved after sintering as more homogeneous glass powders were used [53]. Considering that SLCM can lead to load-bearing scaffolds, an expansion of applications of BGs is expected in the orthopedic field for low load-bearing parts, where BG scaffolds fabricated using other methods, e.g., foam replica, are not suitable due to their low mechanical strength [52]. Recent research has also shown the fabrication of 45S5 BG-based scaffolds using SLCM [54]. It was reported that the scaffolds' linear shrinkage and compressive strength could be improved by increasing the BG content. In addition to 45S5 BG, there is increasing interest in other BG compositions incorporating biologically active ions, which can be more effective from the osteogenic, angiogenic, and antibacterial points of view than 45S5 BG.
Binder Jet Printing has mainly been used to develop glass/ceramic composite scaffolds, while the fabrication of amorphous glass structures has been less investigated. For example, hydroxyapatite (HA)/apatite–wollastonite (A/W) glass–ceramic composites were fabricated from A/W glass powder and HA powder, which were previously mixed in a suspension with maltodextrin as an additional binder. After drying and grinding, a homogeneous powder with a particle size distribution having a mean diameter ~ 70 µm was achieved [55]. In a related study, a mixture of calcium phosphate ceramic and 45S5 BG was 3D-printed, employing a cementing reaction during the printing process [56]. Dicalcium hydrogen phosphate (DCPD) and dicalcium pyrophosphate (DCPP) formed during the cementing reaction. Recently, tricalcium phosphate (TCP)- 45S5 BG composite scaffolds were developed by binder jetting-based 3D-printing technique following the hypothesis that BG's addition would enhance densification via liquid phase sintering and improve mechanical properties [57]. HA/19–93 BG (composition: 53 SiO2-6 Na2O-12 K2O-5 MgO-20 CaO-4 P2O5—wt%) mixtures have also been used to prepare 3D-printed composites [58]. An aqueous slurry containing 6wt% dextrin binder and polyacrylic acid as lubricator were used. With increasing HA content, the interaction of HA particles influenced the sintering process, and higher sintering temperatures were required. Indeed sintering was facilitated by the presence of a glassy phase in such composites. Monolithic parts of 13–93 BG have been developed by 3D printing [59]. In this case, viscous flow sintering at relatively low temperatures of 742 °C and 795 °C led to fully dense structures without crystallization. The size and shape of the powder have been considered critical parameters in all studies, and in fact, such parameters also affect the surface quality of the printed structures.
Selective Laser Sintering (SLS) has been demonstrated for manufacturing 45S5 BG scaffolds [60]. One crucial aspect to consider is the possible crystallization of 45S5 BG, which usually occurs during the SLS's heating and cooling processes. Indirect SLS has also been used to develop 3D glass structures, for example, for fabricating 13–93 BG scaffolds [61, 62], in which a CO2 laser with a laser beam diameter of 0.46 mm was used. Using 13–93 BG, dense and macroporous samples were fabricated and sintered at 700 °C, below the onset of glass crystallization.
Robocasting or fused deposition modeling (FDM) has received particular attention to produce BG and polymer-BG composite scaffolds. For example, Eqtesadi et al. showed the fabrication of 45S5 BG scaffolds with 60–80% porosity using this method [63]. Moreover, sol–gel-derived mesoporous bioactive glasses combined with poly vinyl alcohol (PVA) have been used to fabricate scaffolds by robocasting [64]. Indeed, multiscale porosity in the struts of scaffolds can be achieved using mesoporous BG particles and a porogen in combination with 3D-printed biodegradable polymers [65]. In similar research, the application of 3D printing to develop composite scaffolds incorporating sol–gel-derived Cu-doped bioactive glass particles has recently been shown [66]. In this study, gelatin/silk fibroin scaffolds incorporating 1 wt% of Cu-doped BG particles were processed for bone defect repair applications. In addition, incorporation of BG micro- and nanoparticles in hydrogels, natural and synthetic biopolymers for 3D printing of bioactive scaffolds has been reported by several authors [67,68,69,70,71,72,73,74]. Solvent-based and hydrogel extrusion processes have high potential also for Bioprinting (Biofabrication). In this context, Bioprinting of cell-laden hydrogels incorporating BG particles as bioreactive fillers is an area of increasing interest in the biofabrication field [75, 76]. Finally, different 3D-printing techniques have been applied successfully for obtaining polymer-BG composites using PCL [77], PLA [78], silk [79], and poly(3-hydroxybutyrate-co-3-hydroxyvalerate) (commonly known as PHBV) [80]. Recently, Marsh et al. have shown the 3D printing of glass–ceramic scaffolds using fused filament fabrication technique, called fused deposition of ceramics [81]. Those filaments consisted of sol–gel-derived micro-sized Ag-doped BG particles and polyolefin binders [82].
3D printing of metals and alloys for biomedical devices
PBF is the most common process used in the 3D printing of metals and alloys, and Ti6Al4V is the most common alloy used for hip, knee, and spinal devices. The first-generation 3D-printed metallic implants focused on dense-porous structures where the porosity is added to reduce the effective stiffness and pathways for biological fixation [83,84,85,86,87,88]. The PBF, DED, and binder jetting processes were used to show that uniform or gradient porosity metallic structures can reduce the stiffness and help in early-stage osseointegration [2, 88]. It is established that a pore size range of 300 to 600 μm helps in osseointegration. It is also established that increasing the volume fraction porosity decreases the mechanical strength [87, 88]. For porous coatings, different lattice structures have also been developed with various porosities. Apart from Ti alloys, Ta has also been processed using 3D printing, and Ta has shown exceptional biocompatibility and is used in the porous coating on Ti6Al4V implants. Since the melting point of Ta is higher than 3000 °C, it is challenging to process Ta using conventional manufacturing operations. However, both bulk and porous Ta structures were processed easily using laser-based 3D-printing processes [89,90,91]. Biodegradable porous magnesium and iron alloys have also been processed using metal 3D printing and tested in vivo. It has been shown that 3D-printed structures are stable, biocompatible, and biodegradable in vivo, where the biodegradation kinetics varied as a function of porosity [92, 93]. Shape memory alloy nickel-titanium has also been processed via metal-based 3D-printing processes and shown to possess its shape-memory effects and biocompatibility [94,95,96,97]. Figure 5a, b show patient-matched 3D-printed metallic implants [98, 99].
(a) 3D-printed porous metal implants—design and powder bed-printed model [98]. (b) 3D-printed patient-matched spinal cage of Ti6Al4V [99]. (c) In vivo biological response at 5 weeks from porous titanium and tantalum parts fabricated using direct energy deposition (DED)-based 3D printing showing early-stage osseointegration as a function of designed porosities and extended new bone formation [90]. Used with permission from Springer and Elsevier.
For metallic biomaterials, apart from offering to manufacture complex shapes with dense and porous materials, the 3D-printing technologies also enable the design of new alloys instead of using legacy alloys such as Ti6Al4V borrowed from the aerospace and automotive industries. Recently, it has been shown that the in vivo biocompatibility of 3D-printed Ti-Ta alloys with 10 and 25 weight% Ta is similar to 100% Ta [100]. Figure 5c shows in vivo osseointegration in different Ti and Ta implants [90]. Such alloy design concepts are expected to innovate new alloys for various unmet needs in orthopedic and dental applications. 3D printing has also shown that hard or biocompatible ceramics can be coated on metal surfaces to increase wear resistance or biocompatibility of a metal such as Ti6Al4V [101,102,103]. This approach is also expected to innovate novel multi-materials biomedical devices for treating bone disorders using 3D printing.
Current challenges and future directions
3D printing has come a long way to process biomaterials for traditional and innovative devices during the past decade. 3D-printed patient-matched implants are no longer one of a kind unique cases; over 100,000 mass-produced metallic implants are being 3D Printed every year in the US alone for human use; 3D-printed surgical models are used regularly in various hospital worldwide and manufacturing surgical tools via 3D printing has become a routine operation. Yet, regulatory approval for 3D-Printed devices is still slow because of various challenges in the 3D-printing operations that are significantly different from traditional approaches. For example, for metal implants, metal powders are the starting materials for powder bed fusion technologies. It is still debatable how long metal powders can be reused and what characterization techniques should be used to assure the robustness of the process. Different vendors have developed their tools, but standardization is still lacking. Similarly, how do we assure that loose powders will not come out and go into the bloodstream after porous implants are placed in the body? What are the heat treatments that are needed for different 3D-printed devices? Although results so far are encouraging, standardization of many such operations will ease the regulatory burden worldwide. Another area of significant importance is alloy design? Using the 3D-printing routes, can we develop new alloys designed for 3D-printing processes? Legacy alloys such as Ti6Al4V were not developed, keeping fast cooling approaches that is natural to 3D printing. However, the same composition is used in 3D printing operations, although the kinetics of the manufacturing process is very different. It is anticipated that new alloys will be designed for 3D-printing-based processes and used for biomedical devices. Like metallic devices, Bioprinted products currently lack regulatory guidelines as those processes are still in developmental stages. More fundamental data on Bioprinted products and a better understanding of the process-property relationship will help develop regulatory guidelines in the coming years [104,105,106]. For ceramics and glasses, reliability of 3D-printed products is needed, along with reproducible manufacturing practices. Binder jetting-based 3D printing method can be ideal for manufacturing drug delivery devices with resorbable polymers and ceramics. Especially this method allows for printing parts with high resolution and complex features. There are significant prospects of using binder jetting method to make ceramics or glass scaffolds, for generic or patient-matched or defect specific, for small-scale bone defects. Controlled drug doses can also be programmed easily during binder jetting-based 3D printing, which can be used commercially for the mass production of such devices. It is expected that with better design flexibility and materials choices in 3D Printing, various innovative biomedical devices will be available to aid long-standing challenges in human health. We hope that the current excitement will continue to grow and more scientists, engineers, and clinicians will join the innovative world of 3D printing of biomaterials and biomedical devices, and enjoy the journey as the authors of this article did.
Data availability
All raw data for this study have been presented in this manuscript.
References
A. Bandyopadhyay, S. Bose, Additive Manufacturing, 2nd edn. (CRC Press, Boca Raton, 2019)
S. Bose, D. Ke, H. Sahasrabudhe, A. Bandyopadhyay, Additive manufacturing of biomaterials. Prog. Mater Sci. 93, 45–111 (2018)
A. Bandyopadhyay, I. Mitra, S. Bose, 3D printing for bone regeneration. Curr Osteoporos Rep 18(5), 505–514 (2020)
J.A. Gonzalez, J. Mireles, Y. Lin, R.B. Wicker, Characterization of ceramic components fabricated using binder jetting additive manufacturing technology. Ceram. Int. 42, 10559–10564 (2016)
M.S. Hossain, J.A. Gonzalez, R.M. Hernandez, M.A.I. Shuvo, J. Mireles, A. Choudhuri et al., Fabrication of smart parts using powder bed fusion additive manufacturing technology. Addit. Manuf. 10, 58–66 (2016)
A. Bandyopadhyay, B. Heer, Additive manufacturing of multi-material structures. Mater. Sci. Eng. Rep. 129, 1–16 (2018)
S.V. Murphy, A. Atala, 3D bioprinting of tissues and organs. Nat. Biotechnol. 32, 773 (2014)
M.I. Sabir, X. Xu, L. Li, A review on biodegradable polymeric materials for bone tissue engineering applications. J. Mater. Sci. 44(21), 5713–5724 (2009)
A. Liaskoni, R.D. Wildman, C.J. Roberts, 3D printed polymeric drug-eluting implants. Int. J. Pharm. 597, 120330 (2021)
J. Barthes, P. Lagarrigue, V. Riabov, G. Lutzweiler, J. Kirsch, C. Muller et al., Biofunctionalization of 3D-printed silicone implants with immunomodulatory hydrogels for controlling the innate immune response: An in vivo model of tracheal defect repair. Biomaterials 268, 120549 (2021)
A. Gregor, E. Filová, M. Novák, J. Kronek, H. Chlup, M. Buzgo et al., Designing of PLA scaffolds for bone tissue replacement fabricated by ordinary commercial 3D printer. J. Biol. Eng. 11(1), 31 (2017)
J. Sun, H. Tan, Alginate-based biomaterials for regenerative medicine applications. Materials (Basel, Switzerland) 6(4), 1285–1309 (2013)
P. Rastogi, B. Kandasubramanian, Review of alginate-based hydrogel bioprinting for application in tissue engineering. Biofabrication 11(4), 42001 (2019)
M. Farokhi, F. Jonidi Shariatzadeh, A. Solouk, H. Mirzadeh, Alginate based scaffolds for cartilage tissue engineering: A review. Int. J. Polym. Mater. Polym. Biomater. 69(4), 230–247 (2020)
D. Chawla, T. Kaur, A. Joshi, N. Singh, 3D bioprinted alginate-gelatin based scaffolds for soft tissue engineering. Int J Biol Macromol. 144, 560–567 (2020)
E. Kim, J.M. Seok, S. Bae, S.A. Park, W.H. Park, Silk fibroin enhances cytocompatibilty and dimensional stability of alginate hydrogels for light-based three-dimensional bioprinting. Biomacromol 22(5), 1921–1931 (2021)
M. Lafuente-Merchan, S. Ruiz-Alonso, A. Espona-Noguera, P. Galvez-Martin, E. López-Ruiz, J.A. Marchal et al., Development, characterization and sterilisation of Nanocellulose-alginate-(hyaluronic acid)-bioinks and 3D bioprinted scaffolds for tissue engineering. Mater. Sci. Eng. C 126, 112160 (2021)
S. Chawla, S. Midha, A. Sharma, S. Ghosh, Silk-based bioinks for 3D bioprinting. Adv. Healthc. Mater. 7(8), 1701204 (2018)
S. Chawla, A. Sharma, A. Bandyopadhyay, S. Ghosh, Developmental biology-inspired strategies to engineer 3D bioprinted bone construct. ACS Biomater. Sci. Eng. 4(10), 3545–3560 (2018)
P. Admane, A.C. Gupta, P. Jois, S. Roy, C.C. Lakshmanan, G. Kalsi et al., Direct 3D bioprinted full-thickness skin constructs recapitulate regulatory signaling pathways and physiology of human skin. Bioprinting. 15, e00051 (2019)
S. Chawla, M.H.M. Berkelaar, B. Dasen, C. Halleux, S. Guth-Gundel, I. Kramer et al., Blockage of bone morphogenetic protein signalling counteracts hypertrophy in a human osteoarthritic micro-cartilage model. J. Cell Sci. 133(23), 249094 (2020)
S. Chawla, S. Ghosh, Regulation of fibrotic changes by the synergistic effects of cytokines, dimensionality and matrix: Towards the development of an in vitro human dermal hypertrophic scar model. Acta Biomater. 69, 131–145 (2018)
S. Chawla, S. Ghosh, Establishment of in vitro model of corneal scar pathophysiology. J. Cell Physiol. 233(5), 3817–3830 (2018)
A. Sharma, P. Rawal, D.M. Tripathi, D. Alodiya, S.K. Sarin, S. Kaur et al., Upgrading hepatic differentiation and functions on 3D printed silk–decellularized liver hybrid scaffolds. ACS Biomater. Sci. Eng. 7, 3861 (2021)
G. Jiang, S. Li, K. Yu, B. He, J. Hong, T. Xu et al., A 3D-printed PRP-GelMA hydrogel promotes osteochondral regeneration through M2 macrophage polarization in a rabbit model. Acta Biomater. 128, 150–162 (2021)
S. Bose, M. Roy, A. Bandyopadhyay, Recent advances in bone tissue engineering scaffolds. Trends Biotechnol. 30(10), 546–554 (2012)
S. Bose, K.D. Traxel, A.A. Vu, A. Bandyopadhyay, Clinical significance of three-dimensional printed biomaterials and biomedical devices. MRS Bull. 44, 494–504 (2019)
R. Trombetta, J.A. Inzana, E.M. Schwarz, S.L. Kates, H.A. Awad, 3D printing of calcium phosphate ceramics for bone tissue engineering and drug delivery. Ann. Biomed. Eng. 45, 23–44 (2017)
R. Comesaña, F. Lusquiños, J. DelVal, F. Quintero, A. Riveiro, M. Boutinguiza et al., Toward smart implant synthesis: bonding bioceramics of different resorbability to match bone growth rates. Sci. Rep. 5, 1–13 (2015)
C. Bergemann, M. Cornelsen, A. Quade, T. Laube, M. Schnabelrauch, H. Rebl et al., Continuous cellularization of calcium phosphate hybrid scaffolds induced by plasma polymer activation. Mater. Sci. Eng. C 59, 514–523 (2016)
Y. Zhang, L. Xia, D. Zhai, M. Shi, Y. Luo, C. Feng et al., Mesoporous bioactive glass nanolayer-functionalized 3D-printed scaffolds for accelerating osteogenesis and angiogenesis. Nanoscale 7, 19207–19221 (2015)
L. Sweet, Y. Kang, C. Czisch, L. Witek, Y. Shi, J. Smay et al., Geometrical versus random beta-TCP scaffolds: exploring the effects on schwann cell growth and behavior. PLoS ONE 10, e0139820 (2015)
S. Bose, S. Tarafder, A. Bandyopadhyay, Effect of chemistry on osteogenesis and angiogenesis towards bone tissue engineering using 3D printed scaffolds. Ann. Biomed. Eng. 45, 261–272 (2017)
S. Bose, D. Banerjee, S. Robertson, S. Vahabzadeh, Enhanced in vivo bone and blood vessel formation by iron oxide and silica doped 3D printed tricalcium phosphate scaffolds. Ann. Biomed. Eng. 46, 1241–1253 (2018)
S. Bose, S. Vahabzadeh, A. Bandyopadhyay, Bone tissue engineering using 3D printing. Mater. Today 16, 496–504 (2013)
S. Bose, S. Sugiura, A. Bandyopadhyay, Processing of controlled porosity ceramic structures via fused deposition process. Scripta Mater. 41(9), 1009–1014 (1999)
J. Darsell, S. Bose, H. Hosick, A. Bandyopadhyay, From CT scans to ceramic bone grafts. J. Am. Ceram. Soc. 86(7), 1076–1080 (2003)
A. Bandyopadhyay, S. Bernard, W. Xue, S. Bose, Feature article: calcium phosphate based resorbable ceramics: influence of MgO, ZnO and SiO2 dopants. J. Am. Ceram. Soc. 89(9), 2675–2688 (2006)
S.S. Banerjee, S. Tarafder, N.M. Davies, A. Bandyopadhyay, S. Bose, Understanding the influence of MgO and SrO binary doping on the mechanical and biological properties of β-TCP ceramics. Acta Biomater. 6, 4167–4174 (2010)
G. Fielding, A. Bandyopadhyay, S. Bose, Effects of SiO2 and ZnO doping on mechanical and biological properties of 3D printed TCP scaffolds. Dent. Mater. 28, 113–122 (2012)
S. Hoover, S. Tarafder, A. Bandyopadhyay, S. Bose, Silver doped resorbable tricalcium phosphate scaffolds for bone graft applications. Mater. Sci. Eng. C 79, 763–769 (2017)
S. Bose, N. Sarkar, S. Vahabzadeh, Sustained release of vitamin C from PCL coated TCP induces proliferation and differentiation of osteoblast cells and suppresses osteosarcoma cell growth. Mater. Sci. Eng. C 105, 110096 (2019)
N. Sarkar, S. Bose, Liposome-encapsulated curcumin-loaded 3D Printed scaffold for bone tissue engineering. ACS Appl. Mater. Interfaces 11, 17184–17192 (2019)
S. Tarafder, V.K. Balla, N.M. Davies, A. Bandyopadhyay, S. Bose, Microwave sintered 3D printed tricalcium phosphate scaffolds for bone tissue engineering. J. Tissue Eng. Regen. Med. 7(8), 631–641 (2013)
M. Dehurtevent, L. Robberecht, J.C. Hornez, A. Thuault, E. Deveaux, P. Béhin, Stereolithography: A new method for processing dental ceramics by additive computer-aided manufacturing. Dental Mater. 33, 477 (2017)
H. Wu, Y. Cheng, W. Liu, R. He, M. Zhou, S. Wu et al., Effect of the particle size and the debinding process on the density of alumina ceramics fabricated by 3D printing based on stereolithography. Ceram. Int. 15, 17290–17294 (2016)
N. Travitzky, A. Bonet, B. Dermeik, T. Fey, I. Filbert-Demut, L. Schlier et al., Additive manufacturing of ceramic-based materials. Adv. Eng. Mater. 16, 729–754 (2014)
J.K. Placone, A.J. Engler, Recent advances in extrusion-based 3D printing for biomedical applications. Adv. Healthcare Mater. 7, 1701161 (2019)
E. Nyberg, A. Rindone, A. Dorafshar, W.L. Grayson, Comparison of 3D-printed poly-ɛ-caprolactone scaffolds functionalized with tricalcium phosphate, hydroxyapatite, bio-oss, or decellularized bone matrix. Tissue Eng. Part A 23, 503–514 (2017)
C. Koski, B. Onuike, A. Bandyopadhyay, S. Bose, Starch-hydroxyapatite composite bone scaffold fabrication utilizing a slurry extrusion-based solid freeform fabricator. Addit. Manuf. 24, 47–59 (2018)
P. Tesavibul, R. Felzmann, S. Gruber, R. Liska, I. Thompson, A.R. Boccaccini, J. Stampfl, Processing of 45S5 Bioglass® by lithography-based additive manufacturing. Mater. Lett. 74, 81–84 (2012)
Q.Z. Chen, I.D. Thompson, A.R. Boccaccini, 45S5 Bioglass®-derived glass–ceramic scaffolds for bone tissue engineering. Biomaterials 27(11), 2414–2425 (2006)
R. Gmeiner, G. Mitteramskogler, J. Stampfl, A.R. Boccaccini, Stereolithographic ceramic manufacturing of high strength bioactive glass. Int. J. Appl. Ceram. Technol. 12, 38–45 (2015)
Z. Ma, J. Xie, High solid content 45S5 Bioglass®-based scaffolds using stereolithographic ceramic manufacturing: Process, structural and mechanical properties. J. Mech. Sci. Technol. Korean Soc. Mech. Eng. (2021). https://doi.org/10.1007/s12206-021-0144-9
J. Suwanprateeb, R. Sanngam, W. Suvannapruk, T. Panyathanmaporn, Mechanical and in vitro performance of apatite-wollastonite glass-ceramic reinforced hydroxyapatite composite fabricated by 3D-printing. J. Mater. Sci. Mater. Med. 20, 1281–1289 (2009)
C. Bergmann, M. Lindner, W. Zhang, K. Koczur, A. Kirsten, R. Telle, H. Fischer, 3D printing of bone substitute implants using calcium phosphate and bioactive glasses. J. Eur. Ceram. Soc. 30, 2563–2567 (2010)
S. Bose et al., Influence of random and designed porosities on 3D printed tricalcium phosphate-bioactive glass scaffolds. Additive Manuf. 40, 101895 (2021)
A. Winkel, R. Meszaros, S. Reinsch, R. Müller, N. Travitzky, T. Fey, P. Greil, L. Wondraczek, Sintering of 3D-printed Glass/HAp composites. J. Am. Ceram. Soc. 95(11), 3387–3393 (2012)
R. Meszaros, R. Zhao, N. Travitzky, T. Fey, P. Greil, L. Wondraczek, Three-dimensional Printing of a bioactive glass. Glass Technol. Part A 52(4), 111–116 (2011)
J. Liu, H. Hu, P. Li, C. Shuai, S. Peng, Fabrication and characterization of porous 45S5 glass scaffolds via direct selective laser sintering. Mater. Manuf. Process. 28(6), 610–615 (2013)
K.C.R. Kolan, M.C. Leu, G.E. Hilmas, M. Velez, Effect of material, process parameters, and simulated body fluids on mechanical properties of 13–93 bioactive glass porous constructs made by selective laser sintering. J. Mech. Behav. Biomed. Mater. 13, 14–24 (2012)
K.C.R. Kolan, M.C. Leu, G.E. Hilmas, R.F. Brown, M. Velez, Fabrication of 13–93 bioactive glass scaffolds for bone tissue engineering using indirect selective laser sintering. Biofabrication 3(2), 025004 (2011)
S. Eqtesadi, A. Motealleh, P. Miranda, A. Pajares, A. Lemos, J.M.F. Ferreira, Robocasting of 45S5 bioactive glass scaffolds for bone tissue engineering. J. Eur. Ceram. Soc. 34(1), 107–118 (2014)
C. Wu, Y. Luo, G. Cuniberti, Y. Xiao, M. Gelinsky, Three-dimensional printing of hierarchical and tough mesoporous bioactive glass scaffolds with a controllable pore architecture, excellent mechanical strength and mineralization ability. Acta Biomater. 7(6), 2644–2650 (2011)
M.N. Gómez-Cerezo, J. Peña, S. Ivanovski, D. Arcos, M. Vallet-Regí, C. Vaquette, Multiscale porosity in mesoporous bioglass 3D-printed scaffolds for bone regeneration. Mater. Sci. Eng. C 120, 111706 (2021)
Q. Dai et al., 3D printing of Cu-doped bioactive glass composite scaffolds promotes bone regeneration through activating the HIF-1α and TNF-α pathway of hUVECs. Biomater. Sci. 9, 5519–5532 (2021). https://doi.org/10.1039/D1BM00870F
K. Kolan, Y. Liu, J. Baldridge, C. Murphy, J. Semon, D. Day, M. Leu, Solvent based 3D printing of biopolymer/bioactive glass composite and hydrogel for tissue engineering applications. Procedia CIRP 65, 38–43 (2017). https://doi.org/10.1016/j.procir.2017.04.022
Du. Xiaoyu, D. Wei, Li. Huang, M. Zhu, Y. Zhang, Y. Zhu, 3D printing of mesoporous bioactive glass/silk fibroin composite scaffolds for bone tissue engineering. Mater. Sci. Eng. C 103, 109731 (2019). https://doi.org/10.1016/j.msec.2019.05.016
N.S. Kajave, T. Schmitt, T.-U. Nguyen, A.K. Gaharwar, V. Kishore, Bioglass incorporated methacrylated collagen bioactive ink for 3D printing of bone tissue. Biomed. Mater. 16, 035003 (2021)
J. Wu, G. Miao, Z. Zheng, Z. Li, W. Ren, C. Wu, Y. Li, Z. Huang, L. Yang, L. Guo, 3D printing mesoporous bioactive glass/sodium alginate/gelatin sustained release scaffolds for bone repair. J. Biomater. Appl. 33(6), 755–765 (2019). https://doi.org/10.1177/0885328218810269
G. Luo, Xu. Yufei Ma, L.J. Cui, Wu. Mingming, Hu. Yang, Y. Luo, H. Pan, C. Ruan, 13-93 bioactive glass/alginate composite scaffolds 3D printed under mild conditions for bone regeneration. RSC Adv. 7, 11880–11889 (2017). https://doi.org/10.1039/C6RA27669E
J. Zhang, S. Zhao, Y. Zhu, Y. Huang, M. Zhu, C. Tao, C. Zhang, Three-dimensional printing of strontium-containing mesoporous bioactive glass scaffolds for bone regeneration. Acta Biomater. 10(5), 2269–2281 (2014). https://doi.org/10.1016/j.actbio.2014.01.001
M. Petretta, A. Gambardella, M. Boi, M. Berni, C. Cavallo, G. Marchiori, M.C. Maltarello, D. Bellucci, M. Fini, N. Baldini, B. Grigolo, Composite scaffolds for bone tissue regeneration based on PCL and Mg-containing bioactive glasses. Biology 10(5), 398 (2021). https://doi.org/10.3390/biology10050398
M. Monavari, S. Homaeigohar, M. Fuentes-Chandía, Q. Nawaz, M. Monavari, A. Venkatraman, A.R. Boccaccini, 3D printing of alginate dialdehyde-gelatin (ADA-GEL) hydrogels incorporating phytotherapeutic icariin loaded mesoporous SiO2-CaO nanoparticles for bone tissue engineering. Mater. Sci. Eng. C 112470 (2021). https://doi.org/10.1016/j.msec.2021.112470
Á.J. Leite, B. Sarker, T. Zehnder, R. Silva, J.F. Mano, A.R. Boccaccini, Bioplotting of a bioactive alginate dialdehyde-gelatin composite hydrogel containing bioactive glass nanoparticles. Biofabrication 8, 1–8 (2016)
V. Guduric et al., Tailorable zinc-substituted mesoporous bioactive glass/alginate-methylcellulose composite bioinks. Materials 14, 1225 (2021)
C. Murphy, K.C.R. Kolan, M. Long, W. Li, M.C. Leu, J.A. Semon, and D. E. Day, 3D printing of a polymer bioactive glass composite for bone repair, in: solid freeform fabrication 2016: Proceedings of the 26th Annual International Solid Freeform Fabrication Symposium – An Additive Manufacturing Conference (2016) pp. 1718–1731.
T. Distler et al., Polymer-bioactive glass composite filaments for 3D scaffold manufacturing by fused deposition modeling: Fabrication and characterization. Front. Bioeng. Biotechnol. 8, 552 (2020). https://doi.org/10.3389/fbioe.2020.00552
S. Midha, S. Kumar, A. Sharma, K. Kaur, X. Shi, P. Naruphontjirakul, J. Jones, S. Ghosh, Silk fibroin-bioactive glass-based advanced biomaterials: Towards patient-specific bone grafts. Biomed. Mater. 13, 055012 (2018)
B. Aráoz, E. Karakaya, A. González Wusener et al., 3D printed poly(hydroxybutyrate-co-hydroxyvalerate)—45S5 bioactive glass composite resorbable scaffolds suitable for bone regeneration. J. Mater. Res. (2021). https://doi.org/10.1557/s43578-021-00272-9
M.K. Agarwala, A. Bandyopadhyay, R. van Weeren, P. Whalen, A. Safari, S.C. Danforth, Fused deposition of ceramics: Rapid fabrication of structural ceramic components. Ceram. Bull. 11, 60–65 (1996)
A.C. Marsh, Y. Zhang, L. Poli, N. Hammer, A. Roch, M. Crimp, X. Chatzistavrou, 3D printed bioactive and antibacterial silicate glass-ceramic scaffold by fused filament fabrication. Mater. Sci. Eng. C 118, 111516 (2021)
M. Dumas, P. Terriault, V. Brailovski, Modelling and characterization of a porosity graded lattice structure for additively manufactured biomaterials. Mater. Des. 121, 383–392 (2017)
E. Sheydaeian, Z. Fishman, M. Vlasea, E. Toyserkani, On the effect of throughout layer thickness variation on properties of additively manufactured cellular titanium structures. Addit. Manuf. 18, 40–47 (2017)
T.-Y. Kuo, W.-H. Chin, C.-S. Chien, Y.-H. Hsieh, Mechanical and biological properties of graded porous tantalum coatings deposited on titanium alloy implants by vacuum plasma spraying. Surf. Coat. Technol. 372, 399–409 (2019)
L.C. Campanelli, C.C. Bortolan, P.S.C.P. da Silva, C. Bolfarini, N.T.C. Oliveira, Effect of an amorphous titania nanotubes coating on the fatigue and corrosion behaviors of the biomedical Ti–6Al–4V and Ti–6Al–7Nb alloys. J. Mech. Behav. Biomed. Mater. 100, 542–551 (2017)
V.K. Balla, S. Bose, A. Bandyopadhyay, Low stiffness porous Ti structures for load bearing implants. Acta Biomater. 3(6), 997–1006 (2007)
W. Xue, V.K. Balla, A. Bandyopadhyay, S. Bose, Processing and biocompatibility evaluation of laser processed porous titanium. Acta Biomater. 3(6), 1007–1018 (2007)
V.K. Balla, S. Bose, N.M. Davies, A. Bandyopadhyay, Tantalum—A bioactive metal for implants. JOM. 62, 61–64 (2010)
A. Bandyopadhyay, I. Mitra, A. Shivaram, N. Dasgupta, S. Bose, Direct comparison of additively manufactured porous titanium and tantalum implants towards in vivo osseointegration. Addit. Manuf. 28, 259–266 (2019)
V.K. Balla, S. Banerjee, S. Bose, A. Bandyopadhyay, Direct laser processing of a tantalum coating on titanium for bone replacement structures. Acta Biomater. 6, 2329–2334 (2010)
M.P. Staiger, A.M. Pietak, J. Huadmai, G. Dias, Magnesium and its alloys as orthopedic biomaterials: A review. Biomaterials 9, 1728–1734 (2006)
Y. Li, J. Zhou, P. Pavanram, M.A. Leeflang, L.I. Fockaert, B. Pouran et al., Additively manufactured biodegradable porous magnesium. Acta Biomater. 67, 378–392 (2018)
V.K. Balla, S. Bose, A. Bandyopadhyay, Laser processing of net-shape NiTi shape memory alloy. Metall. Mater. Trans. A 38A, 1096–1103 (2007)
S. Bernard, V.K. Balla, N. Davies, S. Bose, A. Bandyopadhyay, Bone cell–materials interactions and Ni ion release of anodized equiatomic NiTi alloy. Acta Biomater. 7, 1902–1912 (2011)
H. Ibrahim, A. Jahadakbar, A. Dehghan, N.S. Moghaddam, A. Amerinatanzi, M. Elahinia, In vitro corrosion assessment of additively manufactured porous NiTi structures for bone fixation applications. Metals 8, 164 (2018)
Z. Gorgin Karaji, M. Speirs, S. Dadbakhsh, J.-P. Kruth, H. Weinans, A.A. Zadpoor et al., Additively manufactured and surface biofunctionalized porous nitinol. ACS Appl. Mater. Interfaces. 9, 1293–1304 (2017)
M. Rana, S.K. Karmakar, B. Pal et al., Design and manufacturing of biomimetic porous metal implants. J. Mater. Res. (2021). https://doi.org/10.1557/s43578-021-00307-1
L.E. Murr, Metallurgy principles applied to powder bed fusion 3D printing/additive manufacturing of personalized and optimized metal and alloy biomedical implants: An overview. J. Market. Res. 9(1), 1087–1103 (2020)
I. Mitra, S. Bose, W. Dernell, N. Dasgupta, C. Eckstrand, J. Herrick, M.J. Yaszemski, S.B. Goodman, A. Bandyopadhyay, 3D printing in alloy design to improve biocompatibility in metallic implants. Mater. Today 45, 20–34 (2021)
J.D. Avila, K. Stenberg, S. Bose, A. Bandyopadhyay, Hydroxyapatite reinforced Ti6Al4V composites for load-bearing implants. Acta Biomater. 123, 379–392 (2021)
A. Bandyopadhyay, A. Shivaram, M. Isik, J.D. Avila, W.S. Dernell, S. Bose, Additively manufactured calcium phosphate reinforced CoCrMo alloy: Bio-tribological and biocompatibility evaluation for load-bearing implants. Addit. Manuf. 28, 312–324 (2019)
M. Roy, V.K. Balla, A. Bandyopadhyay, S. Bose, Laser processing of bioactive tricalcium phosphate coating on titanium for load-bearing implants. Acta Biomater. 4(2), 324–333 (2008)
D. Trucco, A. Sharma, C. Manferdini, E. Gabusi, M. Petretta, G. Desando, L. Ricotti, J. Chakraborty, S. Ghosh, G. Lisignoli, Modeling and fabrication of silk fibroin-gelatin-based scaffolds using extrusion-based 3D bioprinting. ACS Biomater. Sci. Eng. 7(7), 3306–3320 (2021)
J. Chakraborty, I. Banerjee, R. Vaishya, S. Ghosh, Bioengineered in vitro tissue models to study SARS-CoV-2 pathogenesis and therapeutic validation. ACS Biomater. Sci. Eng. 6(12), 6540–6555 (2020)
J. Chakraborty, S. Ghosh, Cellular proliferation, self-assembly and modulation of signaling pathways in Silk fibroin-gelatin based 3D Bioprinted constructs. ACS Appl. Bio Mater. 3(12), 8309–8320 (2020)
Acknowledgments
We would like to acknowledge financial support from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Nos. R01 DE 029204 and R01 AR067306. The content is solely the authors' responsibility and does not necessarily represent the official views of the National Institutes of Health. ARB acknowledges financial support from the ‘Deutsche Forschungsgemeinschaft’ (DFG, German Research Foundation); Collaborative Research Center SFB/TRR225 (subproject B03).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
A. Bandyopadhyay and S. Bose are permanent members of the editorial board; S. Ghosh and A. Boccaccini are guest editors of this journal during the review and decision stage. For the JMR policy on review and publication of manuscripts authored by editors, please refer to http://www.mrs.org/editor-manuscripts/.
Rights and permissions
About this article
Cite this article
Bandyopadhyay, A., Ghosh, S., Boccaccini, A.R. et al. 3D printing of biomedical materials and devices. Journal of Materials Research 36, 3713–3724 (2021). https://doi.org/10.1557/s43578-021-00407-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1557/s43578-021-00407-y