Abstract
Background
Weaning-induced pulmonary edema (WIPO) is one of the commonest causes of weaning failure in critical care. As ultrasound machine is an easy and available tool in critical care units that help to diagnose interstitial lung syndrome by detecting B lines, it can be a handy method for diagnosis of WIPO.
Aim
We aimed to detect the threshold of increase in B lines (ΔB lines) that can accurately diagnose WIPO.
Methods
This is a prospective observational study carried on 52 mechanically ventilated patients who were eligible for weaning. Lung ultrasound was done before and after spontaneous breathing trial (SBT) to detect the increase in B lines (ΔB lines).
Results
Among the first 52 SBT, 25 trials were failed. Twelve patients developed WIPO (23% of all SBT and 48% of failing SBT). The best diagnostic accuracy for WIPO was a ΔB lines ≥ 6. In these cases, a ΔB line ≥ 6 has a sensitivity of 83.3%, a specificity of 82.5%, a positive predictive value of 58.8%, and a negative predictive value of 94.3% (area under the curve = 0.824, p < 0.001). Low body mass index (BMI) and increased number of ΔB lines were independent predictors of WIPO.
Conclusion
A ΔB lines ≥ 6 has the best diagnostic accuracy for diagnosis of WIPO during SBT.
Trial registration
NCT04463303.
Similar content being viewed by others
Introduction
Failure of weaning after mechanical ventilation occurred in about 40% of patients due to many factors leading to prolonged hospital stay and poor prognosis [1]. Transition from a positive pressure to a negative pressure ventilation increases preload and afterload and induces myocardial ischemia leading to pulmonary edema. Weaning-induced pulmonary edema (WIPO) is a common cause of weaning failure that can be treated if detected early [2].
Elevation in pulmonary artery wedge pressure through pulmonary artery catheter after a SBT remains the standard diagnostic criterion for detection of WIPO [3]. This technique is invasive and associated with complications such as arrhythmias, pulmonary infarction, and others. Therefore, less invasive alternative methods for the diagnosis of WIPO are being suggested. Other alternative biological markers that have been used during SBT are as follows: (1) the increase in the B-type natriuretic peptide or the N-terminal B-type and natriuretic peptide [4, 5], (2) hemoconcentration that is induced during pulmonary edema by the filtration of a significant volume of plasma throughout the pulmonary alveolo-capillary barrier, and (3) the increase of plasma protein concentration greater than 6% [6]. However, these biological markers lack the ability to quantify the elevation LV filling pressure and to identify the unrelated mechanisms. Lung ultrasound can replace the pulmonary artery occlusion pressure measurement as a less invasive method for diagnosis of pulmonary edema in critically ill patients. It detects B lines that allow the diagnosis of interstitial lung syndrome which is the early stage of hemodynamic pulmonary edema [7, 8]. B lines have been correlated with NT-proBNP in breathless patients and with extravascular lung water accumulation [4]. To the investigators’ knowledge, very few studies investigated the diagnostic accuracy of B lines for diagnosis of WIPO. We aimed to detect the threshold of increase in B lines (ΔB lines) that can accurately diagnose WIPO and to investigate the factors contributed to WIPO during SBT.
Methods
This is a prospective observational study that was conducted in the critical care unit of a university-affiliated hospital during the period between May 2021 and May 2022.
Inclusion criteria
Adult patients ≥ 18 years on invasive mechanical ventilation who met criteria for weaning and underwent a planned SBT for 30–120 min were enrolled. The criteria for weaning according to the recommendations are as follows: (1) improvement or partial improvement of the underlying causes of acute respiratory failure, (2) patient is conscious enough to protect airways, (3) the needed inspired oxygen fraction is below 0.5, (4) the needed positive end-expiratory pressure (PEEP) is below 5-cm H2O, the (5) absence or the need of the lowest dose of vasopressor and/or inotropic drugs, and (6) a rapid shallow breathing index ≤ 105 (supplementary data 1) [3]. The patients were grouped into two groups according to development of WIPO.
Exclusion criteria
Patients with poor lung ultrasound and/or echocardiographic window were excluded from the study.
Data of the patients
Data collected before SBT includes patient demographics, smoking history, medical comorbidities (diabetes mellitus, hypertension, ischemic heart disease, obesity, or chronic kidney disease), indication for MV, mode of MV, and duration of MV, patient’s outcome, and duration of hospital stay.
Physical examination includes vital signs, and body mass index (BMI) was recorded. Rapid shallow breathing index (respiratory rate/tidal volume) was calculated at time of SBT. Laboratory investigations include basal metabolic profile, and arterial blood gases (ABG) were recorded.
Volume state was assessed by urine input and output chart, central venous pressure measurement, and point-of-care ultrasound (POCUS).
Echocardiography data
Echocardiography was done using the Philips HD5 ultrasound (USA, 2013). The echocardiographic data includes the left ventricular ejection fraction (EF) which was assessed by M-mode. The left ventricular diastolic function was assessed by measuring velocities of the mitral E and A waves and the e′ wave of the external mitral annulus and by calculating the E/e′ ratio. Echocardiography was done before and after an hour of the SBT.
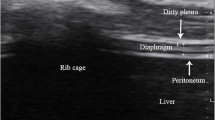
Lung ultrasound data
Lung ultrasound was done using SonoScape E2 with 2- to 4-MHz convex probe, (China) according to the BLUE protocol [3]. The number of B lines was counted in the anterior chest between two ribs at the four standardized BLUE points. The probe was applied at the same point after SBT. Images were recorded, and the change in the number of B lines (ΔB lines) was calculated. Lung ultrasound was done before and after an hour of the SBT.
Spontaneous breathing trial
SBT was performed with PS mode. The maximum duration for an SBT was set at 2 h. The failure of SBT was defined as the development of dyspnea, an oxygen desaturation, hypercapnia, respiratory rate > 35 bpm, heart rate ≥ 140 bpm, systolic arterial pressure < 90 or ≥ 180 mmHg, significant change of mental state, and/or signs of increase work of breathing [9]. Cases with failure of SBT were reconnected to the ventilator. The patients who passed the SBT safely were extubated.
Diagnosis of weaning-induced pulmonary oedema (WIPO)
The diagnosis of WIPO was made by an expert intensivist on criteria of increase of plasma proteins: hematocrit/A ratio and E/e′ ratio. The intensivist was not informed about the results of the study to prevent bias.
Statistical analysis
Data was coded and entered using the statistical package SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) version 22. Data was summarized using mean and standard deviation in quantitative data and using frequency (count) and relative frequency (percentage) for categorical data. Comparisons between WIPO cases versus cases without WIPO were assessed by a two-tailed Student’s t-test, a χ2 test, or a Mann–Whitney U-test, depending on the data distribution. Comparisons between patients’ data before versus at the end of SBT were assessed by a paired Student’s t-test or a Wilcoxon signed rank-sum test depending on the data distribution. Comparisons between quantitative variables were made using the nonparametric Mann–Whitney tests. For comparison of serial measurements within each patient in each group, the nonparametric Wilcoxon signed-rank test was used. For comparing categorical data, chi-square test was performed. Exact test was used instead when the expected frequency is less than 5. A receiver operating characteristic (ROC curve) was constructed with the area under curve analysis performed to detect the best cut-off value of ΔB lines for diagnosis of WIPO. Logistic regression analysis was used to determine the predictors for WIPO. p-values less than 0.05 were considered as statistically significant.
Ethical consideration
The study was approved by the faculty’s ethics committee, and permission was obtained from the ethics committee who assured that confidentiality would be maintained and ethical principles would be followed. Patients who met the eligibility criteria were informed about the study, and their consents were obtained before the start of the study.
Results
Patients’ demographics and clinical characteristics
We recruited 52 mechanically ventilated patients who were eligible for weaning. They were divided into 2 groups: group 1 included 12 patients who were diagnosed as WIPO, while the second group included 40 patients without WIPO. The demographic and clinical characteristics of patients in both groups were described in Table 1.
Most of our patients were males: 32 (80.0%) in patients without WIPO and 6 (50.0%) in patients with WIPO with statistically significant difference (p = 0.05). There were no significant differences between the groups regarding age, smoking, and associated co-morbidities. Thirty-seven patients (71.2%) were obese with significantly higher BMI in patient without WIPO (p = 0.037).
Data of MV
COPD exacerbation was the most common cause of mechanical ventilation in both groups (25%, 40%, respectively). COPD was the cause of ventilation in 44% of patients with failure of weaning. ARDS was the second cause of mechanical ventilation in patients with WIPO with significant difference (25%, p = 0.01). The most common mode of ventilation in WIPO patients was AC (volume): 83.3% (p = 0.01).
Incidence of WIPO
Among the 52 SBT, 25 trials failed. Twelve WIPO occurred, i.e., the incidence of WIPO was 23% of all SBT and 48% of failing SBT as shown in Fig. 1.
All cases of WIPO led to SBT failure. Respiratory exhaustion was the cause of weaning failure in the other patients.Twenty-nine patients without WIPO (72.5%) had simple weaning, while the rest of patients had respiratory weakness that prolonged their weaning.
Data during SBT
Heart rate showed significant increase following SBT in both groups with statistically significant difference between both groups (p = 0.0001). The mean arterial BP decreased in both groups with no statistically significant difference (p = 0.609, 0.481, respectively).
The mean of respiratory rate increased significantly from (16.17 ± 4.63) to (22.0 ± 4.41) in patients with WIPO and from (14.925 ± 2.291) to (15.225 ± 2.833) in patients without WIPO with statistically significant difference between the 2 groups (p = 0.0001).
As regard the changes in arterial blood gases in patients with WIPO following SBT, there was a significant decrease in PH from 7.36 ± 0.043 to 6.99 ± 1.15. Oxygen saturation and PO2 also showed a marked decrease (p = 0.002). Carbon dioxide showed an insignificant increase following failure of SBT (p = 0.157). There were statistically significant differences between the two groups regarding PH, O2 saturation, and PO2 (p = 0.002, 0.0001, and 0.001, respectively) as shown in Table 2. Hemoglobin, hematocrit, and plasma proteins increased in WIPO significantly (p = 0.0001, 0.002) in comparison with group without WIPO.
Characteristics of echocardiography at the end of SBT
There were insignificant changes in the LV systolic function, while 58.3% of patients with WIPO had diastolic dysfunction. The E/e′ ratio increased during SBT significantly in cases of WIPO (p = 0.003).
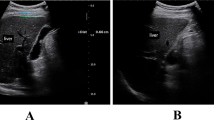
Characteristics of lung ultrasound during SBT
Before the SBT, the average number of total B lines was 5 ± 3 in cases with WIPO and 3 ± 2in cases without WIPO (p = 0.0001). The mean of B lines increased significantly to 11 ± 4 in patients with WIPO during SBT (p = 0.005) (Fig. 2).
ROC curve to detect the optimum cut-off values of ΔB lines for diagnosis of WIPO (Table 3)
ROC curve was analyzed to detect optimal cut-off values of delta B lines for diagnosis of WIPO. Area under the curve (AUC) of delta B lines was 0.824. The best accuracy for diagnosis of WIPO was reached when the delta B lines were ≥ 6. In these cases, a delta B lines ≥ 6 allowed the diagnosis of WIPO with a sensitivity of 83.3%, a specificity of 82.5%, and a positive predictive value of 58.8% and a negative predictive value of 94.3%. Among the 12 cases with WIPO, a delta B lines ≥ occurred in 9 cases (75% of cases). Among the 12 cases with SBT failure but without WIPO, a delta B lines ≥ 6 occurred in three cases (25%). While in the 27 cases with SBT success, it occurred in two cases (2.4%).
ROC curves to detect the optimum cut-off values of ΔB lines to predict failure of weaning (Fig. 3)
When the analysis by ROC was performed by considering the success or failure of weaning, a cut-off value for the increase in B lines after SBT was ≥ 6 with a p-value of 0.003, AUC = 0.741, sensitivity = 68%%, and specificity = 85.2%.
Identification of independent predictors of WIPO
By logistic regression, mode of ventilation, duration of ventilation, and COPD were not independent predictors of WIPO (Table 4). The logistic regression analysis showed that the obesity and ΔB lines ≥ 6 were independent predictors of WIPO.
Discussion
The main findings of the current study are as follows: (1) the incidence of WIPO was 23% of all SBT by lung ultrasound findings; (2) 58.3% of patients with WIPO had diastolic dysfunction; (3) the E/e′ ratio increased during SBT significantly in cases of WIPO (p = 0.003); (4) increase in B lines after SBT was ≥ 6 with a p-value of 0.003, AUC = 0.741, sensitivity = 68%, and specificity = 85.2%; and (5) low body mass index and ΔB lines ≥ 6 were independent predictors of WIPO.
WIPO is a well-known cause of weaning failure in mechanically ventilated patients, but its incidence varied in literature from 20 to 40% [2, 6, 9]. Early prediction and diagnosis of WIPO will decrease the incidence of weaning failure.
In the current study, WIPO was responsible for about half cases of weaning failure (48%) and occurred in 23% of all SBT. This finding coincides with the results of the previous studies [5, 10,11,12]. The results of our previous studies confirmed that WIPO is a recognizable cause of weaning failure. Intensivists should carefully look for it when they encounter a patient who fails SBT by using simple informative method as lung ultrasound.
Echocardiography represents a quantitative method of pulmonary artery occlusion pressure (PAOP). Lateral E/E′ value ≤ 8 is consistent with a PAOP ≤ 18 mmHg [13]. Higher E/e′ ratios have been documented in patients with WIPO [14, 15] which is in agreement with the current results. In addition, echocardiography can detect the possible mechanisms of WIPO, such as SBT-induced mitral regurgitation, and identify associated cardiac disease that may increase LV filling pressures during SBT. In spite of all these values, it requires specific training and is affected by the quality of image. In addition, the cut-off values of diastolic dysfunction for diagnosis are still debatable [16].
Benefits of lung ultrasound in critical care have been documented by many studies [17,18,19]; however, only few studies investigated its role in diagnosis of WIPO [20]. Lung ultrasound represents a promising method in diagnosis of WIPO as it can detect the early stage of hemodynamic pulmonary edema before clinical and laboratory tests. The interstitial lung syndrome is diffuse so it can be detected easily at the anterior chest wall points without need to examine posterolateral areas where B lines may present due to other causes in critically ill patients or in normal subjects [20, 21].
It well known that one B line is normal, while three B lines (or more) indicate hemodynamic pulmonary edema [22]. Frere et al. made the hypothesis that pre-lung rockets (the pattern of two B lines) may be an early stage of pulmonary edema [20]. Also, he suggested that detection of B lines during a SBT had no differential diagnosis other than WIPO [20]. On the other side, another study claimed that since several B lines could move quickly with lung sliding signs because of tachypnea, it might cause large variation in the number of B lines, as per operator [23]. All these points raise the question about the diagnostic accuracy of B lines in detecting WIPO. As we agree that the increase in B lines during SBT is explained only with WIPO, we evaluated the change in B lines (delta B lines) not the absolute B line after the SBT.
The threshold providing the best diagnosis accuracy was an increase of six B lines, i.e., 1 or 2 lines per BLUE point. These finding are concordant with the result of other studies [20, 23, 24].
Decreasing thoracoabdominal compliance and abnormal diaphragmatic position as a complication of obesity could lead to increasing the work of breathing and difficulty in weaning from ventilatory support. Also, obesity reduces functional residual capacity and expiratory flows and increases airway resistance that may lead to weaning-induced pulmonary edema [25]. The impact of obesity on weaning failure has been debatable. One of the study concluded that obesity does not affect weaning or survival outcomes in patients with ventilator-dependent respiratory failure [26]. In contrast to another study which showed that obesity was independent risk factor of WIPO [14], our study showed that the majority of patients (66.7%) with WIPO were not obese and logistic regression showed inverse relation between body mass index and weaning induced pulmonary oedema. This can be attributed to the small sample size and the impact of other factors on weaning and its complications.
The incidence of myocardial ischemia as a cause of weaning failure was very different among previous publications ranging from 6 to 50% [27,28,29]. In our cohort, 25% of WIPO patients had a history of ischemic heart disease; however, we did not report any significant changes in ECG either before or during SBT. Myocardial ischemia was reported as the main mechanism of cardiac failure during weaning but usually with no significant ECG changes [29] and without any increases in troponin 1 [12]. This may highlight that ECG and troponin are insensitive tools to detect ischemia during SBT. The diastolic dysfunction that is usually associated with ischemic insults is detected easily by echocardiography. In our cohort, 58.3% of patients with WIPO had diastolic dysfunction, and the E/e′ ratio increased during SBT significantly in cases of WIPO. This supports that WIPO could be an oxygen-work mismatch that leads to weaning failure.
COPD was the commonest cause of mechanical ventilation in our patients. One-fourth of our patients with WIPO had COPD. However, our results did not show COPD as a predictor for WIPO. Indeed, few previous studies investigated the association between COPD as a risk factor and the development of weaning-induced pulmonary edema [2, 12, 27]. COPD causes negative swing in intrathoracic pressure during SBT increasing possibility of cardiac dysfunction and WIPO [2, 27]. Also, the chronic right ventricular failure of these patients may aggravate biventricular interdependence [30, 31].
It could be predictable that WIPO is preload independent [11], and fluid removal could decrease the incidence of WIPO [12]. It was shown that fluid removal, changing the passive leg-raising test from negative to positive in cases of WIPO, achieved the success of the next SBT. While when the passive leg-raising test remained negative, most of the patients failed the next SBT. However, another study did not demonstrate any correlation between higher fluid balance and WIPO [32]; this could be related to the cohort characteristic of that study. Most of our patients were euvolemic, and WIPO occurred in overloaded patients. However, logistic regression failed to show that fluid balance as an independent predictor of SBT failure which is supported by other studies [33, 34].
In conclusion, our study confirmed the important role of lung ultrasound in diagnosis of WIPO by detecting the increase of B lines of more than 6 lines. However, the interpreter reliability of the technique still needs further investigation. This study is not without flaws. Limitations include the following: it was a single-center study that included medical patients with certain indications for mechanical ventilation. The impact of obesity should be clarified with larger sample size.
Availability of data and materials
The data analyzed during the current study are available from the corresponding author on request.
References
Boles JM, Bion J, Connors A, Herridge M, Marsh B, Melot C, Welte T (2007) Weaning from mechanical ventilation. Eur Respir J 29(5):1033–1056
Teboul J-L (2014) Weaning-induced cardiac dysfunction: where are we today? Intensive Care Med 40(8):1069–1079
Lichtenstein DA, Meziere GA (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure*: the BLUE protocol. Chest 134(1):117–125
Zein H, Baratloo A, Negida A, Safari S (2016) Ventilator weaning and spontaneous breathing trials; an educational review. Emergency 4(2):65
Grasso S, Leone A, De Michele M, Anaclerio R, Cafarelli A, Ancona G, Stripoli T, Bruno F, Pugliese P, Dambrosio M et al (2007) Use of N-terminal pro-brain natriuretic peptide to detect acute cardiac dysfunction during weaning failure in difficult-to-wean patients with chronic obstructive pulmonary disease. Crit Care Med 35(1):96–105
Anguel N, Monnet X, Osman D, Castelain V, Richard C, Teboul JL (2008) Increase in plasma protein concentration for diagnosing weaning-induced pulmonary oedema. Intensive Care Med 34(7):1231–1238
Zieleskiewicz L, Contargyris C, Brun C, Touret M, Vellin A, Antonini F, Leone M (2014) Lung ultrasound predicts interstitial syndrome and hemodynamic profile in parturients with severe preeclampsia. Anesthesiology 120(4):906–914
Enghard P, Rademacher S, Nee J, Hasper D, Engert U, Jörres A, Kruse JM (2015) Simplified lung ultrasound protocol shows excellent prediction of extravascular lung water in ventilated intensive care patients. Crit Care 19(1):1–8
Stawicki SP (2017) Mechanical ventilation: weaning and extubation. Int J Acad Med 3(3):67
Caille V, Amiel JB, Charron C, Belliard G, Vieillard-Baron A, Vignon P (2014) Echocardiography: a help in the weaning process. Crit Care 14(3):R120
Dres M, Teboul JL, Anguel N, Guerin L, Richard C, Monnet X (2015) Passive leg raising performed before a spontaneous breathing trial predicts weaning-induced cardiac dysfunction. Intensive Care Med 41(3):487–494
Liu J, Shen F, Teboul JL, Anguel N, Beurton A, Bezaz N et al (2016) Cardiac dysfunction induced by weaning from mechanical ventilation: incidence, risk factors, and effects of fluid removal. Crit Care 20(1):1–14
Vignon P (2008) Echocardiographic assessment of pulmonary artery occlusion pressure in ventilated patients: a transesophageal study. Crit Care 12:R18
Caille V, Amiel JB, Charron C, Belliard G, Vieillard-Baron A, Vignon P (2010) Echocardiography: a help in the weaning process. Crit Care 14(3):1–7
Papaioannou VE, Stakos DA, Dragoumanis CK, Pneumatikos IA (2010) Relation of tricuspid annular displacement and tissue Doppler imaging velocities with duration of weaning in mechanically ventilated patients with acute pulmonary edema. BMC Cardiovasc Disord 10(1):1–7
de Meirelles Almeida CA, Nedel WL, Morais VD, Boniatti MM, de Almeida-Filho OC (2016) Diastolic dysfunction as a predictor of weaning failure: a systematic review and meta-analysis. J Crit Care 34:135–141
Soummer A, Perbet S, Brisson H et al (2012) Ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextu bation distress. Crit Care Med 40:2064–2072
Silva S, Ait Aissa D, Cocquet P et al (2017) Combined thoracic ultrasound assessment during a successful weaning trial predicts postextubation distress. Anesthesiology 127:666–674
Smit JM, Haaksma ME, Winkler MH, Heldeweg ML, Arts L, Lust EJ, Tuinman PR (2021) Lung ultrasound in a tertiary intensive care unit population: a diagnostic accuracy study. Critical Care 25(1):1–9
Ferré A et al (2019) Lung ultrasound allows the diagnosis of weaning-induced pulmonary oedema. Intensive Care Med 45(5):601–608
Yamaga S, Ohshimo S, Shime N (2019) Is lung ultrasonography really useful for diagnosing weaning-induced pulmonary oedema? Intensive Care Med 45(9):1329–1330
Rasheed G, Shad ZS, Mehreen T, Kharadi N, Ramzan M, Abdullah A, Abbas K (2021) The ideal profile (increase in B-lines/delta B-lines) on lung ultrasound for diagnosing weaning induced pulmonary edema in ventilated patients. PAFMJ 71(6):2220–2223
Bouhemad B, Mojoli F, Nowobilski N, Hussain A, Rouquette I, Guinot PG et al (2020) Use of combined cardiac and lung ultrasound to predict weaning failure in elderly, high-risk cardiac patients: a pilot study. Intensive Care Med 46(3):475–484
Lichtenstein D (2017) Novel approaches to ultrasonography of the lung and pleural space: where are we now? Breathe 13(2):100–111
Salome CM, King GG, Berend N (2010) Physiology of obesity and effects on lung function. J Appl Physiol (1985) 108(1):206–211
Datta D, Scalise P (2004) The effect of body mass index on survival and weaning outcomes in patients with ventilator-dependent respiratory failure. Chest 126(4):868S
Chatila W et al (1996) Cardiac ischemia during weaning from mechanical ventilation. Chest 109(6):1577–1583
Chatila W, Ani S, Guaglianone D, Jacob B, Amoateng-Adjepong Y, Manthous CA (1996) Cardiac ischemia during weaning from mechanical ventilation. Chest 109(6):1577–1583. https://doi.org/10.1378/chest.109.6.1577
Carrié C et al (2011) Myocardial ischaemia and weaning failure: is angioplasty the heart of the problem? Intensive Care Med 37(7):1223–1224
Moschietto S et al (2012) Transthoracic echocardiography with Doppler tissue imaging predicts weaning failure from mechanical ventilation: evolution of the left ventricle relaxation rate during a spontaneous breathing trial is the key factor in weaning outcome. Crit Care 16(3):1–10
Mancebo J (2010) Physiological comparison of three spontaneous breathing trials in difficult-to-wean patients. Intensive Care Med 36(7):1171–1179
Routsi C et al (2019) Weaning failure of cardiovascular origin: how to suspect, detect and treat—a review of the literature. Ann Intensive Care 9(1):1–17
El Hadidy S et al (2019) Coinciding changes in B lines patterns, haemoglobin and hematocrit values can predict outcomes of weaning from mechanical ventilation. Open access Macedonian J Med Sci 7(23):4010
Lichtenstein DA, Meziere GA (2011) The BLUE-points: three standardized points used in the BLUE-protocol for ultrasound assessment of the lung in acute respiratory failure. Crit Ultrasound J 3(2):109–110
Acknowledgements
We thank the patients and their families for their participation in this study.
Funding
No funding was required.
Author information
Authors and Affiliations
Contributions
Dina A. Hamad; Acquisition of data and investigations including echocardiography and lung ultrasound, analysis and interpretation of data and writing of the research. Alaa Eldin Abdel-Moniem and Ahmad B. Abdelrehim; Conception, design and Supervision. Marwan N. Mohamed; did the lung ultrasound. Taghreed S. Meshref; did the echocardiography. Shimaa A. Elghazally; Statistical analysis. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
“The Committee of Medical Ethics” of Faculty of Medicine, Assiut University, had approved the study, with reference no. 17300611. Written consents were obtained from all patients.
Consent for publication
Not applicable. Neither identifying images nor personal data were included in the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hamad, D.A., Abdel-Moniem, A.E., Meshref, T.S. et al. Diagnostic accuracy of lung ultrasound in detecting weaning-induced pulmonary edema. Egypt J Bronchol 17, 22 (2023). https://doi.org/10.1186/s43168-023-00197-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-023-00197-3