Abstract
Background
The hematopoietic malignancy acute myeloid leukemia is a fatal disease with poor clinical prognoses. Long non-coding RNA taurine-upregulated gene1 (lncRNA TUG1) and zinc finger E-box binding homeobox 2 antisense RNA1 (lncRNA ZEB2-AS1) are reported to participate in the development and progression of different types of malignancies. The goal of the current study was to evaluate the prognostic value of the lncRNAs TUG1 and ZEB2-AS1 as well as their various expression patterns in newly diagnosed Egyptian adult acute myeloid leukemia patients.
Methods
We assessed the expression levels of both lncRNA TUG1 and lncRNA ZEB2-AS1 using the quantitative real-time reverse transcription polymerase chain reaction technique (qRT-PCR) in 80 newly diagnosed AML patients and 20 healthy subjects.
Results
lncRNA TUG1 expression was significantly higher in the AML cases compared to the controls (P < 0.001), whereas lncRNA ZEB2-AS1 expression was considerably lower in the AML cases in comparison with the controls (P < 0.001). The expression levels of the lncRNAs ZEB2-AS1 and TUG1 exhibited a significantly positive association in the AML group (P < 0.001). There was no difference in overall survival (OS) and disease-free survival (DFS) between the groups with low and high lncRNA TUG1 expression (P = 0.139 and 0.918, respectively). Furthermore, the AML cases with higher lncRNA ZEB2-AS1 expression levels had shorter DFS than patients with lower lncRNA ZEB2-AS1 expression levels (P = 0.014), while OS did not significantly differ between the studied cases with lower and higher lncRNA ZEB2-AS1 expression (P = 0.589).
Conclusion
Overexpression of lncRNA TUG1 could serve as a diagnostic biomarker for Egyptian adult AML cases, while lncRNA ZEB2-AS1 high expression could be regarded as an indicator of poor outcome in Egyptian adult AML studied cases.
Similar content being viewed by others
Background
The hematological malignancy known as acute myeloid leukemia (AML) is distinguished by the aberrant proliferation of primitive myeloid cells in the bone marrow and peripheral blood, along with severe inhibition of normal hematopoiesis [1]. Previous studies have shown that genetic aberrations are crucial to the development and spread of AML [2]. Increasing data suggest that AML is caused by epigenetic dysregulations including acetylation, DNA methylation, and noncoding RNAs [3].
A family of non-protein coding transcripts known as long non-coding RNAs (lncRNA) are > 200 nucleotides and less than 100 kb long. They cannot be translated into proteins because they lack open reading frames [4]. The main mechanisms of lncRNA action include their involvement in the process of histone modification [5, 6], their direct interaction with proteins to change their function or localization, or their use as scaffolds to encourage protein binding to other proteins (or DNA) [7]. By serving as a "sponge," they compete for miRNAs, bind to them, and subsequently control the expression of the target genes [8, 9].
The 7.1-kb lncRNA taurine-upregulated gene 1 is found on chromosome 22q12. Aberrant expression of lncRNA TUG1 may have an impact on a number of biological events, including cell proliferation, differentiation, apoptosis, invasion, drug resistance, blood tumor barrier permeability regulation, and epithelial-mesenchymal transition (EMT) [10, 11]. According to several studies, lncRNA TUG1 is an oncogene that contributes to the development and progression of several cancers, including adult Philadelphia-negative acute lymphoblastic leukemia, breast cancer, colon cancer, renal cell carcinoma, and multiple myeloma [12,13,14,15].
Long non-coding RNA zinc finger E-box-binding homeobox 2 antisense RNA 1 (lncRNA ZEB2-AS1) is located on chromosome 2q22.3 that is overlapping and antisense to the ZEB2 gene, which has been identified as an essential component in the process of epithelial-mesenchymal transition (EMT). lncRNA ZEB2-AS1 had the ability to activate ZEB2 expression [16]. Also, it has been described to affect cell proliferation, migration, invasion, and cell cycle regulation [17]. Additionally, it has been demonstrated to play a role in the development of a number of cancers, including lung and stomach cancers [18, 19].
Unfortunately, the lncRNAs ZEB2-AS1 and TUG1 prognostic implications in AML are poorly understood, and it is still unclear how those lncRNAs operate in leukemogenesis [20, 21]. Therefore, our aim was to investigate various expression patterns and the prognostic significance of the lncRNAs TUG1 and ZEB2-AS1 in newly diagnosed Egyptian adult acute myeloid leukemia patients.
Methods
This study included 80 Egyptian patients newly diagnosed with AML with a mean age of 48 ± 14 years at diagnosis (49 males and 31 females). Additionally, 20 healthy donors of BM transplantation were included as a control group with a mean age of 50 ± 15 years (13 males and 7 females).
The study was conducted at Clinical Pathology Department, National Cancer Institute, Cairo, Egypt, from 2019 to 2022 and was performed according to the Helsinki declaration guidelines and approved by Benha University ethical scientific committee.
The included cases in this study were Adult cases ≥ eighteen years old newly diagnosed with AML. The following were the exclusion criteria: patients who began therapy, those under the age of 18, patients with secondary AML, patients with AML with myelodysplasia-related changes, or with other malignancies.
Patients were subjected to full history taking, complete clinical examination, and laboratory investigations including complete blood picture, bone marrow aspiration, immunophenotyping, and cytogenetic. Also, molecular genetic analysis was carried out for detection of chromosomal abnormalities, NPM1 and FLT3-ITD mutations by reverse transcriptase PCR and real-time PCR, respectively. Real-time reverse transcription polymerase chain reaction (qRT-PCR) was carried out for all participants in the study to quantitatively estimate the expression of the long noncoding RNAs ZEB2-AS1 and TUG1.
AML diagnosis and classification were performed according to French-American-British [22] and World Health Organization criteria [23]. Genetic risk stratification of the AML cases was performed based on 2017 European Leukemia Net (ELN) recommendations [24].
The AML studied cases received induction chemotherapy in the form of standard 3 + 7 regimens (Doxorubicin 30 mg/m2 on days 1–3; Cytarabine 100 mg/m2 on days 1–7). Patients with PML/RAR-alpha gene expression acute promyelocytic leukemia received induction cycle in the form of tretinoin 22.5 mg/m2 and arsenic trioxide 0.15 mg/kg therapy.
The presence of complete remission (CR)—defined as bone marrow with at least twenty percent cellularity and BM blasts below five percent, without need for transfusions, an absolute neutrophil count greater than 1 × 109/l, and a platelet count greater than 100 × 109/l—was evaluated after induction chemotherapy was completed. In the present study, long-term prognosis evaluations were conducted using disease-free survival (DFS) and overall survival (OS). DFS was defined as the period from the start of treatment to the time of recurrence, progression, or death, while OS is the period from the time of diagnosis until death or the last follow-up [25].
Quantitative reverse transcriptase-PCR for lncRNA TUG1 and incRNA ZEB2-AS1
RNA extraction and cDNA synthesis
One milliliter of bone marrow aspiration was obtained from both the AML studied cases and the controls and then evacuated into tubes containing ethylene diamine tetra-acetic acid (1.2 mg/mL).
Following the manufacturer's instructions, total RNA was extracted from bone marrow cells using the QIAamp RNA Blood Mini Kit for total RNA purification (QIAGEN® Austin, Texas, USA catalog no. 52304). The concentration and purity of the extracted RNA were measured using a Spectrophotometer (Nano-Drop, Q-500, Scribner, USA) and then stored at − 80 °C until use. Thermo Fisher Scientific's High-Capacity cDNA Reverse Transcription Kit (USA; catalog number 4374966) was used to reverse transcribe RNA into complementary DNA, which was then stored at − 20 °C until its use in quantitative real-time PCR.
Gene expression analysis
Quantitative real-time PCR was carried out to measure the expression levels of lncRNA TUG1 and lncRNA ZEB2-AS1. Real-time PCRs were performed in twenty μL volume using TaqMan® Universal PCR Master Mix II (Catalog no.: 4440043, Thermo Fisher Scientific, Applied Biosystems, USA) and TaqMan primer probes for lncRNA TUG1 (Hs00215501_m1; Thermo Fisher Scientific, USA, Catalog number: 4448892), lncRNA ZEB2-AS1 (Hs04274848_g1; Thermo Fisher Scientific, USA, Catalog number: 4426961) and B-actin as a reference gene (Hs03929097_g1; Thermo Fisher Scientific, USA, Catalog no: 4331182). These were the primer sequences that were used: lncRNA ZEB2 AS1 forward, 5′-GGCTGG ATAGCAAAGGAC-3′ and reverse, 5′-ACACTCTTGGCGAGG-3′; lncRNA TUG1forward, 5′-TAGGAGTGGATGTGTTCTGTAGCA-3′ and reverse, 5′-TGGTCGTGGAATATGGTCAATGAG-3′; B-actin forward, 5′-ATGTTTGAGACCTTCAACACC-3′ and reverse, 5′-GCCATCTCCTGCTCGAAGTCT-3′. The thermal reaction conditions were as follows: polymerase activation at 95 °C for ten minutes followed by forty cycles of 95 °C for 15 s (denaturation), and 60 °C for one min (annealing and extension). Applied Biosystems' Step One plus™ Real-Time PCR System was used to measure the resulting fluorescence. lncRNAs TUG1 and ZEB2-AS1 relative expression was assessed using Schmittgen and Livak's comparative Ct method (2-∆∆Ct) [26].
Statistical methods
Statistical analysis and data management were carried out using SPSS version 28 (IBM, Armonk, New York, USA). To check for normalcy in quantitative data, the Kolmogorov–Smirnov test, the Shapiro–Wilk test, and direct data visualization approaches were used. Means, standard deviations, medians, and ranges were used to summarize quantitative data in a manner consistent with normality. Numbers and percentages were used for displaying categorical collections of data. Independent t-tests or Mann–Whitney U tests were employed to compare the data among the study groups based on gene expression, depending on whether or not the quantitative data had been normally distributed. If necessary, Fisher's exact test or Chi-square test was used to compare the categorical data. Correlation analyses were carried out using Spearman’s correlation. ROC analyses were carried out to evaluate the role of the studied lncRNAs in AML diagnosis. Areas under the curve, best cutoff points, and diagnostic indices were calculated. To evaluate the overall and disease-free survival of the cases under study, Kaplan–Meier analyses were carried out. The log-rank test compared the overall and the disease-free survival according to lncRNAs expression. There was a two-sided design for each statistical test. P values under 0.05 were considered significant.
The results
Demographic, clinical, and laboratory features of the AML cases are presented in Table 1.
Relative expression of the lncRNAs TUG1 and ZEB2-AS1 in AML patients and controls
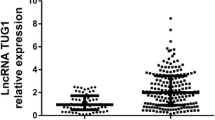
The studied AML patients showed significantly higher lncRNA TUG1 expression levels compared to controls (6.78 vs. 0.84, P < 0.001). On the other hand, they showed lower lncRNA ZEB2-AS1 expression compared to controls (0.16 vs. 0.88, P < 0.001) (Table 2; Figs. 1 and 2).
ROC analysis for lncRNA TUG1 and lncRNA ZEB2-AS1 (Fig. 3)
ROC analysis was carried out to compare the expressions of the lncRNAs ZEB2-AS1 and TUG1 in AML patients to those in the control group. It verified that the lncRNA TUG1 revealed significant AUC of 0.970 (P < 0.001), with ninety-five percent confidence interval ranging from 0.953 to 1. The best cutoff value was > 2.72, at which the sensitivity, specificity, positive predictive value, and negative predictive value were 88.6%, 100%, 100%, and 67.9%, respectively. Additionally, for lncRNA ZEB2-AS1, the Roc curve analysis showed significant AUC of 0.820 (P < 0.001), with ninety-five percent confidence interval ranging from 0.732 to 0.908. The best cutoff was ≤ 0.26, at which the sensitivity, specificity, PPV, and NPV were 60.9%, 100%, 100%, and 38.6%, respectively.
Relationship between lncRNAs ZEB2-AS1 and TUG1 expression in AML cases
The lncRNAs ZEB2-AS1 and TUG1 had a highly significant positive correlation in the studied AML cases (P < 0.001) (Fig. 4).
Correlation of lncRNA TUG1 and lncRNA ZEB2-AS1 expression with initial blast count
lncRNA TUG1 expression showed a significant positive correlation with the initial PB blast (P = 0.018) and initial BMA blast (P = 0.002) (Fig. 5b, c). Additionally, lncRNA ZEB2-AS1 expression showed a significant positive correlation with the initial BMA blast (P = 0.027) (Fig. 5a).
Correlation analysis between the expression of lncRNAs TUG1, ZEB2-AS1, and clinicopathological features of AML studied patients (Tables 3 and 4)
Patients were classified into high and low expression groups according to lncRNA TUG1 and lncRNA ZEB2-AS1 cutoff. For lncRNA TUG1 cases with a cut-off > 2.72 were considered high expression while for lncRNA ZEB2-AS1 cases with cutoff more than 0.26 were deemed high expression.
The results of this study demonstrated that 70 from 80 patients showed high lncRNA TUG1 gene expression, while only 27 patients showed high lncRNA ZEB2-AS1 expression.
There were no significant differences between the high and low lncRNA TUG1 and lncRNA ZEB2-AS1 expression groups regarding clinical findings, initial (TLC, hemoglobin, platelets, PB blasts, and cellularity), FAB subtypes, cytogenetics, and cytogenetic risk stratification (ELN 2017). Patients with higher levels of lncRNA TUG1 expression (n = 70) displayed more positive CD13 (88.6%) than patients with lower levels (55.6%) (P = 0.009). Additionally, patients with high lncRNA TUG1 expression had median initial BMA blasts that were considerably greater (76%) than those of patients with low lncRNA TUG1 expression (64%) (P = 0.034), while patients with high levels of lncRNA ZEB2-AS1 expression (n = 27) showed significantly higher CD14 than patients with low levels of lncRNA ZEB2-AS1 expression (P = 0.029). However, there was not a significant difference in initial blast count between the groups with high and low lncRNA ZEB2-AS1 expression.
Overall survival and disease-free survival assessment (Fig. 6)
To evaluate the overall and disease-free survival of the cases under study, Kaplan–Meier analysis was used. The estimated overall survival rate was 26.7% at 6 months and 21.6% at 12 and 24 months. The median survival time was 0.9 month, with a ninety five percent confidence interval ranging from 0.543 to 1.257. The estimated disease-free survival rate was 46% at six months, 21.9% at twelve months, and 16.4% at twenty-four months. The median disease-free survival time was 3.567 months, with ninety-five percent confidence interval ranging from 0 to 9.526.
OS and DFS in relation to lncRNA TUG1 and lncRNA ZEB2-AS1 expression groups
No significant association was observed between the OS and DFS rates regarding the lncRNA TUG1 expression groups (P = 0.139 and 0.918, respectively) (Fig. 7a, b). However, a lower level of lncRNA ZEB2-AS1 expression has been associated with a better DFS than a higher level of expression (P = 0.014). Between groups with high and low lncRNA ZEB2-AS1 expression, OS did not significantly differ (P = 0.589) (Fig. 8a, b).
Multivariate comparison for DFS on lncRNA ZEB2-AS1 expression and other prognostic factors
Multivariate cox regression analysis was carried out to predict disease-free survival. The model was built clinically, including all factors that may affect prognosis, including age, initial TLC, initial hemoglobin, initial platelets, initial blasts, ELN genetic risk, t(8;21), t(9;22), t(16;16), PML/RARA, and high expression of lncRNA ZEB2-AS1. Stepwise cox regression analysis was conducted, and the only significant variable that remained in the model was high lncRNA ZEB-AS1 expression (HR 3.107, 95% CI 1.193–8.094, P = 0.02).
Discussion
Acute myeloid leukemia is characterized by a wide variety of prognosis and multiple pathogenic pathways [27]. The clinical outcomes of AML remain dismal despite the breakthroughs in therapeutic approaches, such as intense chemotherapy and hematopoietic stem cell transplantation, especially in older patients (> 60 old). In order to find effective treatment options for AML, it is crucial to look at the molecular mechanisms behind its development and progression [28].
LncRNAs had previously been thought to be transcription waste products. Nevertheless, it is now well defined that lncRNAs have a role in cell proliferation and differentiation as well as pathophysiology of many illnesses, including cancer [29].lncRNA TUG1 is a rising star among all cancer-related lncRNAs [30]. Increasing evidence has found that the lncRNA TUG1 is implicated in the pathogenesis of different cancers, such as osteosarcoma, bladder cancer, and glioma [31]. Also, lncRNA ZEB2-AS1 upregulation was observed in human cancers like pancreatic cancer [32] and bladder cancer [33]. Unfortunately, the functional importance and underlying mechanisms of the lncRNAs TUG1 and ZEB2-AS1 in AML are poorly understood [20, 21]. So, we aimed in this study to assess the expression levels of lncRNA TUG1 and lncRNA ZEB2-AS1 in newly diagnosed AML Egyptian patients (Fig. 5).
Our results demonstrated that the AML patient group had considerably greater levels of lncRNA TUG1 expression than the control group (P 0.001), which suggests its role in AML pathogenesis. The results of our study are consistent with previously published studies that detected lncRNA TUG1 upregulation in AML patients by using SYBR Green RT-qPCR [20, 34,35,36]. These reported results were supported by studies suggesting that the overexpression of the lncRNA TUG1 in AML was associated with increased cell proliferation, migration, and invasion, while knockdown of TUG1 might suppress AML development [34, 37].lncRNA ZEB2-AS1 is an oncogene that was known to be associated with human cancers such as lung cancer and hepatocellular carcinoma [32, 38], but there are limited research studies about its role in AML. Guan et al. [39] detected that lncRNA ZEB2-AS1 was upregulated in bone marrow bulk cells from AML cases compared to control by using SYBR Green RT-qPCR and also reported that lncRNA ZEB2 AS1 overexpression has been correlated with a reduced survival rate in AML cases. Additionally, AML cells' growth was also inhibited, and their rate of apoptosis was enhanced when the lncRNA ZEB2 AS1 was silenced. Similarly, Shi et al. [21] demonstrated that lncRNA ZEB2-AS1 expression was higher in bone marrow bulk cells from AML cases than in the control group (P < 0.001), as high lncRNA ZEB2-AS1expression was detected only in 13 patients out of sixty-two patients.
Contrary to studies that support the oncogenic role of the lncRNA ZEB2-AS1, the current study demonstrated significantly lower lncRNA ZEB2-AS1 expression in acute myeloid leukemia cases than in the normal control group (P < 0.001). However, the lncRNA ZEB2-AS1 expression and the initial BMA blast revealed a significant positive association (P = 0.027). The discrepancy between our results and the results of other studies may be due to ethnic differences, a difference in sample sizes, or different techniques. Also, the precise mechanism of lncRNA ZEB2-AS1 upregulation in AML cases and its role in the pathophysiology of the illness are still unclear.
This study revealed a significant positive relationship among lncRNA ZEB2-As1 and lncRNA TUG expression levels in AML cases (P < 0.001), as cases with high ZEB2-AS1 also showed increased expression of TUG1.
The present study revealed a significant difference among high and low lncRNA TUG1 expression groups regarding age (P = 0.053), but no significant variation had been reported regarding gender (P = 0.301). A study performed by Wang et al. [20] revealed non-significant differences between high and low lncRNA TUG1 expression groups regarding age and gender. Furthermore, no variations were observed among low and high lncRNA ZEB2-AS1 expression groups regarding age (P = 0.581) and gender (P = 0.862). Similar findings were reported by Shi et al. [21].
Regarding laboratory findings, our results demonstrated a significantly higher median initial BMA blast (76%) in studied cases with high lnc RNA TUG1 expression than patients with low expression (64%) (P = 0.034). While there were no significant differences observed regarding initial (TLC, hemoglobin, platelets, and PB blasts), FAB subtypes (P = 0.529), FLT-ITD and NPM mutation. Li and Wang [35] also reported no relationship among high and low lncRNA TUG1 expression groups and total leukocytic count, hemoglobin level, platelet count, FAB subtypes, FLT-ITD, and NPM mutation. However, Wang et al. [20], found that the patients with higher lncRNA TUG1 expression showed a high white blood cell count.
This study revealed no significant differences between low and high lncRNA ZEB2-AS1 expression groups regarding initial (TLC, hemoglobin, platelets, PB blasts, BM blasts, and cellularity), FAB subtypes (P = 0.778), FLT-ITD and NPM mutation. Contrary to our results, Shi et al. [21] detected significant differences among high and low lncRNA ZEB2-AS1 expression groups regarding initial TLC (P = 0.046), initial platelets (P = 0.044), and FAB subtypes (P = 0.006).
As a predictor of treatment response, we analyzed the percentage of bone marrow aspirate blast at days 14 and 28 after chemotherapy in relation to low and high lncRNA TUG1and lncRNA ZEB2-AS1 expression groups. Our results demonstrated no statistically significant difference between both groups. In contrast with our finding, Wang et al. [20] reported that LncRNA TUG1 high expression was associated with a reduced chance of achieving CR (P = 0.001). Also, Shi et al. [21] observed that the CR rate was lower in the studied AML cases with high lncRNA ZEB2 AS1 expression compared to low expression subgroup (P = 0.031).
Regarding the association between lncRNA TUG1 expression levels and AML outcomes, there was no significant difference between the lncRNA TUG1 high and low expression groups and the OS and DFS. On the other hand, Li and Wang [35] found that the median DFS and OS in the AML studied cases with high lncRNA TUG1 expression were shorter than in cases with low lncRNA TUG1 expression (P < 0.001, P = 0.002, respectively). This discrepancy in the results may be attributed to different treatment protocols.
According to our findings, DFS was considerably better in AML cases with lower lncRNA ZEB2-AS1 expression than it was in those with higher expression (P = 0.014), while OS did not significantly differ between high and low lncRNA ZEB2-AS1 expression groups (P = 0.589). However, Shi et al. [21] demonstrated that AML patients with high lncRNA ZEB2-AS1 expression had shorter OS (P = 0.036) and lower DFS rates (P = 0.039) compared to those with low expression.
Conclusion
In conclusion, for Egyptian adult AML patients, lncRNA TUG1 overexpression may serve as a diagnostic biomarker, while high levels of the lncRNA ZEB2-AS1 are associated with lower survival rates and an increased risk of relapse. Further research is recommended on a larger number of cases with different ethnic groups for accurate assessment of the diagnostic and prognostic value of lncRNA TUG1 and lncRNA ZEB2-AS1 expression and to understand the molecular pathways linking these long non-coding RNAs to leukemia progression in order to target them for therapeutic benefit. Finally, a longer follow-up duration is recommended for better assessment of OS and DFS.
Availability of data and materials
Data analyzed in the current work are available from the corresponding author upon a reasonable request.
Abbreviations
- AML:
-
Acute myeloid leukemia
- TUG1:
-
Taurine-upregulated gene1
- ZEB2-AS1:
-
Zinc finger E-box binding homeobox 2 antisense RNA1
- Ct:
-
Cycle threshold
- DFS:
-
Disease-free survival
- OS:
-
Overall survival
- RQ:
-
Relative quantitation
- AUC:
-
Area under the curve
- BM:
-
Bone marrow
- EMT:
-
Epithelial–mesenchymal transition
References
Thomas D, Majeti R (2017) Biology and relevance of human acute myeloid leukemia stem cells. Blood 129:1577–1585
Bullinger L, Dohner K, Dohner H (2017) Genomics of acute myeloid leukemia diagnosis and pathways. J Clin Oncol 35:934–946
Zhang X, Tao W (2019) Long noncoding RNA LINC00152 facilitates the leukemogenesis of acute myeloid leukemia by promoting CDK9 through miR-193a. DNA Cell Biol 38:236–242
Bohmdorfer G, Wierzbicki AT (2015) Control of chromatin structure by long noncoding RNA. Trends Cell Biol 25:623–632
Sun X, Haider Ali MSS, Moran M (2017) The role of interactions of long non-coding RNAs and heterogeneous nuclear ribonucleoproteins in regulating cellular functions. Biochem J 474:2925–2935
Zhu Y, You J, Wei W (2021) Downregulated lncRNA RCPCD promotes differentiation of embryonic stem cells into cardiac pacemaker-like cells by suppressing HCN4 promoter methylation. Cell Death Dis 12:667
Xu Y, Wu W, Han Q (2019) New insights into the interplay between non-coding RNAs and RNA-binding protein HnRNPK in regulating cellular functions. Cells 8:62
Guo H-L, Wang X, Yang G-Y (2020) LINC00472 promotes osteogenic differentiation and alleviates osteoporosis by sponging miR-300 to upregulate the expression of FGFR2. Eur Rev Med Pharm Sci 24:4652–4664
Guo K, Qian K, Shi A (2021) LncRNA-MIAT promotes thyroid cancer progression and function as ceRNA to target EZH2 by sponging miR-150-5p. Cell Death Dis 12:1097
Niland CN, Merry CR, Khalil AM (2012) Emerging roles for long non-coding RNAs in cancer and neurological disorders. Front Genet 3:25
Chiu HS, Somvanshi S, Patel E (2018) Pan-cancer analysis of lncRNA regulation supports their targeting of cancer genes in each tumor context. Cell Rep 23:297-312.e12
Zeng P, Chai Y, You C (2021) Correlation analysis of long non-coding RNA TUG1 with disease risk, clinical characteristics, treatment response, and survival profiles of adult Ph− acute lymphoblastic leukemia. J Clin Lab Anal 35:e23583
Qingqing Y, Xianjuan S, Xiaopeng C (2019) Elevated serum lncRNA TUG1 levels are a potential diagnostic biomarker of multiple myeloma. Exp Hematol 79:47–55
Cai H, Xue Y, Wang P (2015) The long noncoding RNA TUG1 regulates blood-tumor barrier permeability by targeting miR-144. On-cotarget 6:19759–19779
Wang PQ, Wu YX, Zhong XD (2017) Prognostic significance of overexpressed long non-coding RNATUG1 in patients with clear cell renal cell carcinoma. Eur Rev Med Pharmacol Sci 21(1):82–86
Beltran M, Puig I, Peña C (2008) A natural antisense transcript regulates Zeb2/Sip1 gene expression during Snail1-induced epithelial-mesenchymal transition. Genes Dev 22(6):756–766
Li T, Xie J, Shen C (2016) Upregulation of long non-coding RNA zeb1-as1 promotes tumor metastasis and predicts poor prognosis in hepatocellular carcinoma. Oncogene 35:1575–1584
Guo Y, Hu Y, Hu M (2018) Long non-coding RNA ZEB2-AS1 promotes proliferation and inhibits apoptosis in human lung cancer cells. Oncol Lett 15(4):5220–5226
Wu FX, Gao HY, Liu KG (2019) The IncRNA ZEB2-AS1 is upregulated in gastric cancer and affects cell proliferation and invasion via miR-143-5p/HIF-1 alpha axis. Onco Targets Ther 12:657–667
Wang X, Lina Z, Fan Z (2018) Long non-coding RNA taurine-upregulated gene 1 correlates with poor prognosis, induces cell proliferation, and represses cell apoptosis via targeting aurora kinase A in adult acute myeloid leukemia. Ann Hematol 97:1375–1389
Shi X, Jiao L, Liang MA (2019) Overexpression of ZEB2-AS1 lncRNA is associated with poor clinical outcomes in acute myeloid leukemia. Oncol Lett 17:4935–4947
Bennett JM, Catovsky D, Daniel MT (1976) Proposals for the classification of the acute leukaemias. French–American–British (FAB) co-operative group. Br J Haematol 33(4):451–458
Arber DA, Brunning RD, Le Beau MM (2017) Acute myeloid leukaemia and related precursor neoplasms. In: Swerdlow SH, Campo E, Harris NL et al (eds) WHO classification of tumours of haematopoietic and lymphoid tissues. Revised 4th ed. IARC Press, Lyon, pp 130–71
Dohner H, Estey E, Grimwade D (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129:424–447
Hartmut D, Elihu E, David G (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129:4
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 25(4):402–408
Mohammed O, Walaa A, Johne A (2022) Clinical outcomes for patients with acute myeloid leukemia harboring IDH1 mutation after intensive chemotherapy. Egypt J Hosp Med 88:3089–3093
Tawfik B, Pardee TS, Isom S (2016) Comorbidity, age, and mortality among adults treated intensively for acute myeloid leukemia (AML). J Geriatr Oncol 7:24–31
Hu G, Niu F, Humburg BA (2018) Molecular mechanisms of long noncoding RNAs and their role in disease pathogenesis. Oncotarget 9:18648–18663
Yin DD, Zhang EB, You LH (2015) Downregulation of lncRNA TUG1 affects apoptosis and insulin secretion in mouse pancreatic beta cells. Cell Physiol Biochem 35:1892–1904
Huang MD, Chen WM, Qi FZ (2015) Long non-coding RNA TUG1 is up-regulated in hepatocellular carcinoma and promotes cell growth and apoptosis by epigenetically silencing of KLF2. Mol Cancer 14:165
Gao H, Gong N, Ma Z (2018) LncRNA ZEB2-AS1 promotes pancreatic cancer cell growth and invasion through regulating the miR-204/HMGB1 axis. Int J Biol Macromol 116:545–551
Wu XQ, Yan TZ, Wang ZW (2017) LncRNA ZEB2-AS1 promotes bladder cancer cell proliferation and inhibits apoptosis by regulating miR-27b. Biomed Pharmacother 96:299–304
Gang L, Peiming Z, Huiling W (2019) Long non-coding RNA TUG1 modulates proliferation, migration, and invasion of acute myeloid leukemia cells via regulating miR-370-3p/MAPK1/ERK. Onco Targets Ther 12:10375–10388
Li Q, Wang J (2020) LncRNA TUG1 regulates cell viability and death by regulating miR-193a-5p/Rab10 axis in acute myeloid leukemia. OncoTargets Ther 13:1289–1301
Li Qun, Wei S, Jianmin W (2019) TUG1 confers Adriamycin resistance in acute myeloid leukemia by epigenetically suppressing miR-34a expression via EZH2. Biomed Pharmacother 109:1793–1801
Weide Z, Yuhua L, Jing Z (2020) Long non-coding RNA taurine upregulated gene 1 targets miR-185 to regulate cell proliferation and glycolysis in acute myeloid leukemia cells in vitro. Onco Targets Ther 13:7887–7896
Wu SM, Chen J, Liang Y (2022) Long non-coding RNA ZEB2-AS1 promotes hepatocellular carcinoma progression byregulating the miR-582-5p/FOXC1 axis. Cell J 24(6):285–293
Guan J, Ping L, Aixia W (2020) Long non-coding RNA ZEB2-AS1 affects cell proliferation and apoptosis via the miR-1225p/PLK1 axis in acute myeloid leukemia. Int J Mol Med 46:1490–1500
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
AMA, SMD, HMK, and RN put the idea, study design, and supervised the work. RN shared in the molecular work and data collection. MNA collected the data, performed the molecular work, and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Benha University research ethics committee, and the included patients gave the consent to participate.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelrahman, A.M.N., Diab, S.M., Shabaan, H.M.K. et al. The study of long noncoding RNA TUG 1 and ZEB2-AS1 expression in newly diagnosed Egyptian adult acute myeloid leukemia patients. Egypt J Med Hum Genet 24, 46 (2023). https://doi.org/10.1186/s43042-023-00423-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43042-023-00423-z