Abstract
Background
Despite international guideline recommendations, low back pain (LBP) imaging rates have been increasing over the last 20 years. Previous systematic reviews report limited effectiveness of implementation interventions aimed at reducing unnecessary LBP imaging. No previous reviews have analysed these implementation interventions to ascertain what behaviour change techniques (BCTs) have been used in this field. Understanding what techniques have been implemented in this field is an essential first step before exploring intervention effectiveness.
Methods
We searched EMBASE, Ovid (Medline), CINAHL and Cochrane CENTRAL from inception to February 1, 2021, as well as and hand-searched 6 relevant systematic reviews and conducted citation tracking of included studies. Two authors independently screened titles, abstracts, and full texts for eligibility and extracted data on study and intervention characteristics. Study interventions were qualitatively analysed by three coders to identify BCTs, which were mapped to mechanisms of action from the theoretical domains framework (TDF) using the Theory and Techniques Tool.
Results
We identified 36 eligible studies from 1984 citations in our electronic search and a further 2 studies from hand-searching resulting in 38 studies that targeted physician behaviour to reduce unnecessary LBP imaging. The studies were conducted in 6 countries in primary (n = 31) or emergency care (n = 7) settings. Thirty-four studies were included in our BCT synthesis which found the most frequently used BCTs were ‘4.1 instruction on how to perform the behaviour’ (e.g. Active/passive guideline dissemination and/or educational seminars/workshops), followed by ‘9.1 credible source’, ‘2.2 feedback on behaviour’ (e.g. electronic feedback reports on physicians’ image ordering) and 7.1 prompts and cues (electronic decision support or hard-copy posters/booklets for the office). This review highlighted that the majority of studies used education and/or feedback on behaviour to target the domains of knowledge and in some cases also skills and beliefs about capabilities to bring about a change in LBP imaging behaviour. Additionally, we found there to be a growing use of electronic or hard copy reminders to target the domains of memory and environmental context and resources.
Conclusions
This is the first study to identify what BCTs have been used to target a reduction in physician image ordering behaviour. The majority of included studies lacked the use of theory to inform their intervention design and failed to target known physician-reported barriers to following LBP imaging guidelines.
Protocol Registation
PROSPERO CRD42017072518
Similar content being viewed by others
Introduction
Despite international guidelines and campaigns calling to reduce diagnostic imaging in low back pain (LBP) [1,2,3], recent evidence suggests that imaging has increased over the last 20 years [4]. Liberal use of LBP imaging results in avoidable costs to both healthcare systems and individual patients [5]. In addition to subjecting patients to unnecessary exposure to radiation, systematic reviews have shown that patients who received imaging without a clear clinical indication had longer recovery times, reported lower quality of life, and were more delayed in their return to work than those who were not imaged [6]. This has led to an increasing number of studies evaluating interventions that aim to change physician behaviour to reduce unnecessary imaging in LBP. For example, four relevant systematic reviews have evaluated interventions to change physician image-ordering behaviour for patients with LBP [7,8,9,10] (most of which included the same studies). Due to the heterogeneity of the interventions, none of these reviews included a meta-analysis. Narrative synthesis of the interventions, however, indicated variable effectiveness and all reviews concluded that there was insufficient evidence to identify which interventions were effective for reducing imaging rates for LBP.
While these interventions have attempted to change physician behaviour, most have not based their interventions on behaviour change theory. At least part of the reason why we see this variable effectiveness is likely due to their lack of theoretical underpinnings. Behaviour change theories such as the theoretical domains framework (TDF) can be used to identify barriers and help select intervention strategies (or behaviour change techniques (BCTs) to address those barriers. Indeed, a host of national health and research organisations including the National Institutes for Clinical Excellence (NICE) and the Medical Research Framework (MRC) [11, 12] suggest that behaviour change interventions should be rooted in theory—specifically, in a theoretical model of behaviour change. By using a theoretical framework, we can improve our understanding of the behaviour we want to change, understand the mechanism by which the behaviour can be changed and, thus, choose BCTs that are most suitable for the target behaviour and context [13].
In this context, understanding why physicians fail to change their ordering practices may provide helpful insights into how we can best intervene to support that change. To this end, our team conducted a systematic review synthesising 11 qualitative studies that asked physicians about the factors that might influence their ordering behaviour. We used the TDF to guide our analysis. Originally developed by Michie et al. to identify factors influencing health professional’s practice behaviour, the TDF is a synthesis of over 128 key theoretical constructs from 36 behaviour change theories into overarching domains presented in a single framework [14,15,16,17]. Depending on the behaviour in question and contextual factors, some domains are likely to be more important than others. Across all studies, conducted worldwide, we found high-level evidence that 3 TDF domains influenced LBP imaging behaviour: (i) Social influence (patient demand), (ii) Beliefs about consequences (lack of ability to explain why an image is not needed) and (iii) Environmental context and resources (lack of time) [18].
While previous reviews have attempted to examine the effectiveness of the interventions to reduce inappropriate imaging, none have described what behaviour change techniques were used to change physicians’ imaging behaviour. This limits our understanding of whether any of those interventions were designed to target the known barriers to changing physician ordering practices that were identified in our review. However, it is possible to re-analyse intervention descriptions according to a behaviour change framework to deduce what BCTs were reported as being included in the interventions [19]. This information can provide valuable guidance in the design and evaluation of future implementation interventions that aim to reduce LBP imaging rates. This, combined with the recent attention that unnecessary LBP imaging has received [13], provides a good rationale to conduct a new review that includes more recent studies and to better describe and analyse the interventions of included studies to ascertain what BCTs have been used and in what setting.
Therefore, we aim to produce the first comprehensive review of BCTs used to change physician behaviour to reduce unnecessary LBP imaging and assess whether they are appropriate to target the known barriers identified in our previous qualitative review. While our review will not assess the effectiveness of the interventions, our findings can be used to inform how effectiveness can be evaluated in future systematic reviews.
Research questions
-
1.
What BCTs (listed in the BCTv1 taxonomy) have been used in interventions designed to change physician behaviour to align with evidence-based guidelines to reduce unnecessary imaging for LBP in both primary care and emergency department settings?
-
2.
Do the identified interventions target known barriers to change?
Methods
We designed and report the review protocol based on the PRISMA statement [20]. The protocol was registered with PROSPERO (CRD42017072518). Since registering our protocol on PROSPERO, to improve specificity, we decided to only include studies that specifically targeted imaging for LBP rather than studies that targeted improvement of any LBP guideline-based recommendation.
Data sources and inclusion criteria
Our research librarian (MS) developed a search strategy using a broad range of terms from a previous search strategy [8] related to back pain, diagnostic imaging and relative interventions combined with additional terms for primary and emergency care settings (Additional file 1). Using this strategy, we searched EMBASE, Ovid (Medline), CINAHL and Cochrane CENTRAL from inception to February 1, 2021. We hand-searched references from six relevant systematic reviews [7,8,9,10, 21, 22], conducted forward and backward citation tracking of all included studies in our review, and emailed several content experts in the field of imaging and LBP to identify any additional studies our electronic and hand searches may have missed.
Studies were eligible if they were published in English and met the inclusion criteria detailed in Table 1. We excluded studies that targeted patients or the public directly (e.g., mass media campaigns) and interventions that were designed to improve adherence to other aspects of LBP guidelines without targeting imaging.
Study selection
All titles identified by the search were combined in Endnote (https://endnote.com) and duplicates removed. Two reviewers (DT, RL) screened the initial set of titles and abstracts, excluding irrelevant studies. Two reviewers (AH, AP, HR) then screened the full texts for eligibility. In cases of disagreement, a third reviewer (HE, JP or AP) was consulted.
Data extraction
Two reviewers (AH and HR, JT or RL) independently extracted study characteristics including year, country, design, setting, target provider and intervention information using an adapted version of the Template for Intervention Description and Replication (TIDieR) checklist [23]. One reviewer (RL) assessed and extracted data on the use of a theoretical rationale for designing/developing the intervention using the Painter criteria [24], which distinguishes the use of theory into the following categories: (i) informed by theory, (ii) applied theory, (iii) testing theory or (iv) building or creating theory.
Data synthesis and analysis
To achieve objective 1 (to describe what BCTs have been used in interventions designed to change physician’s imaging behaviour) the content of the intervention and control groups was extracted from the descriptions provided in the source paper or from referenced protocols or intervention development papers where appropriate. We coded published intervention descriptions according to the BCT Taxonomy v1 developed by Michie et al. [25]. This comprehensive taxonomy was based on a synthesis of behaviour change literature and includes 93 individual BCTs. Where studies targeted multiple behaviours (beyond reducing LBP imaging), we used the following assumptions to guide whether the study was included in the qualitative BCT intervention synthesis:
-
Studies were included if they targeted multiple behaviours and explicitly stated which strategies were used for imaging (explicitly defined) OR they targeted multiple behaviours and included one or more strategies for all target behaviours (implied).
-
Studies were excluded if they targeted multiple behaviours and did not specifically state which strategies were used for imaging.
A coding manual was created based on the BCT taxonomy v1 [25]. The BCT coding framework was piloted by all coders experienced with the BCT Taxonomy (CA, JT, AP, AH) on two studies. During this process, clarifications and examples added to the coding manual by the coders to reflect any assumptions made. Using this first version of the coding manual, interventions were coded independently by two coders. Coding was compared across coders for discrepancies and was resolved by consensus and/or discussed with experts on the team (JM, HE and AMP). There were several instances in which discrepancies were discussed with the experts on the team and further rules were added to the codebook for consistency and clarity. These instances largely related to situations in which there was a lack of explicit information to allow for coding a BCT without making assumptions. The team agreed to apply a conservative coding approach in most instances and added exception rules where applicable (see Additional file 2). Using the final version of the codebook, BCT use across studies, along with their associated taxonomy hierarchies, were tabulated by setting (primary care or emergency department).
Following this, to achieve objective 2 (to assess whether the identified interventions target known barriers to change), we used the Theory and Techniques Tool (available at: https://theoryandtechniquetool.humanbehaviourchange.org/tool) to map BCTs to their corresponding mechanisms of action in the theoretical domains framework (TDF) [26, 27]. The Theory and Techniques Tool maps 74 BCTs to 26 mechanisms of action (including the 14 TDF domains) and depicts the strength of association (link) with colour, with stronger links represented in green, and weaker links represented in orange. The strength of a link was determined by combining data from a literature synthesis [26] and an expert consensus study [27]. Where BCTs mapped to more than one TDF domain, we only recorded the domain where there was strong evidence of a link between the BCT and that domain. In cases where there was no strong association between a BCT and any of the TDF domains, we recorded a domain with a weak association to the BCT. Finally, using this information we identified which intervention addressed the three TDF domains that were implicated in our 2019 review of physician reported barriers to implement LBP guidelines [18].
Results
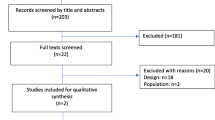
The electronic search (inception to January 2021) identified a total of 2995 citations, 1984 citations after duplicates were removed. From the unique citations, we screened 71 full texts of which 36 were eligible. Hand-searching of five relevant systematic reviews and citation tracking of included studies identified a further 2 studies. Thus, we identified a total of 38 studies that targeted physician behaviour to reduce unnecessary LBP imaging [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65]. A description of the study identification and selection process is outlined in the PRISMA flow diagram (Fig. 1).
Description of studies
Nineteen (50%) of the studies were conducted in the last 5 years (between 2015-present) in both primary care (82%) [30,31,32,33,34,35,36,37,38, 40,41,42, 44,45,46,47,48, 50, 52,53,54,55,56,57,58,59,60, 62,63,64] and emergency settings (18%) [28, 29, 39, 43, 49, 51, 61, 65] in the US (n = 17) [28, 30, 33, 35, 38, 39, 41,42,43, 46, 47, 54, 56, 59, 62, 64], the UK (n = 8) [31, 32, 40, 45, 50, 53, 55, 61], Australia (n = 6) [7, 44, 48, 49, 52, 58], Canada (n = 3) [29, 34, 51], the Netherlands (n = 2) [60, 63], Finland (n = 1) [57] and Germany (n = 1) [65]. Study designs included RCTs/Cluster RCTs (n = 12) [31,32,33, 36, 45, 48, 53, 55, 56, 63,64,65], Step-wedged RCTs (n = 3) [43, 47, 49], interrupted time series (ITS) (n = 8) [28, 34, 38, 40,41,42, 50, 52], controlled before-after studies (CBA) (n = 2) [35, 60], uncontrolled before and after studies (UBA) (n = 10) [29, 30, 37, 39, 46, 51, 58, 59, 61, 62] and three non-experimental studies (describing either the development (n = 2) [44, 57] or post-implementation (n = 1) [54] of an eligible intervention). Four of the 38 studies met the Painter criteria for use of theory, with three studies classified as being informed by theor y[44, 48, 49] and one study classified as testing theory [36]. All studies are described in Table 2.
Description of interventions
Of the 38 studies, we excluded 4 studies [31, 39, 49, 56] from our BCT qualitative synthesis since they targeted multiple aspects of LBP guideline-recommended behaviours and it was not possible to isolate which BCTs were targeting imaging only. The remaining 34 studies either i) solely targeted a reduction in imaging, ii) used the same intervention strategy for all of its target behaviours or iii) specified which BCTs targeted LBP imaging behaviour. We identified 18 BCTs across the 34 studies (see Table 3); the most common techniques were ‘4.1 instruction on how to perform the behaviour’ (n = 31 interventions; 26 studies) [29, 32, 33, 35, 36, 40,41,42, 44,45,46,47,48, 50, 52, 53, 55, 57,58,59,60,61,62,63,64,65], defined as ‘advise or agree on how to perform the behaviour’, and ‘9.1 credible source’ (n = 21 interventions; 18 studies) [29, 30, 32, 35, 36, 40,41,42, 45, 46, 48, 50, 53, 55, 58, 59, 62, 63], defined as ‘present verbal or visual communication from a credible source in favour of or against the behaviour’, ‘7.1 prompts/cues’ (n = 14 interventions; 14 studies) [29, 30, 32, 35, 41, 42, 44, 46, 53, 54, 57, 59, 61, 64] defined as ‘introduce or define environmental or social stimulus with the purpose of prompting or cuing the behaviour’, and ‘2.2 feedback on behaviour’ (n = 13 interventions; 12 studies) [30, 32, 33, 35, 41, 45, 48, 52, 55, 61, 63, 64], defined as ‘monitor and provide informative or evaluative feedback on performance of the behaviour’, and ‘12.5 adding objects to the environment’ (n = 11 interventions, 11 studies) [30, 35, 36, 44, 47, 48, 51, 52, 54, 57, 59] defined as ‘adding objects to the environment in order to facilitate the behaviour’. In these studies, 4.1 commonly referred to education based around a guideline or the provision of a guideline either delivered via post or in person or virtually via webinar, 9.1 commonly referred to the guideline being produced by a reputable/credible institution (not a society) or the guideline was verbally endorsed via video or in person by a reputable peer, 7.1 commonly referred to an automated decision support tool (implemented within a computer pop-up window) or as a hard copy summary of the guidelines/decision aid on when to image (implemented as a poster, laminated document or education booklet), 2.2 commonly referred to the use of audit and feedback in which a feedback report was delivered via email or post to physicians providing them with data on their imaging use and 12.5 commonly referred to decision support tools or education booklets that could be given to patients to help them understand their diagnosis and why imaging was not necessary. The highest number of BCTs included in a single study was 8 [36], while 5 interventions (4 studies) [34, 38, 55, 60] included only a single BCT.
Greater than 50% of studies used a BCT that targeted one of the following TDF domains Knowledge (n = 34 interventions; 27 studies) [29, 32, 33, 35,36,37, 40,41,42,43,44,45,46,47,48, 50, 52, 53, 55, 57,58,59,60,61,62,63,64,65], Skills (n = 32 interventions; 27 studies) [29, 31,32,33, 35, 36, 40,41,42, 44,45,46,47,48, 50, 52, 53, 55, 57,58,59,60,61,62,63,64,65] and Beliefs about capabilities (n = 32; 27 studies) [29, 31,32,33, 35, 36, 40,41,42, 44,45,46,47,48, 50, 52, 53, 55, 57,58,59,60,61,62,63,64,65]. Following these, the domains of environmental context and resources (n = 22 interventions; 21 studies) [28,29,30, 32, 34,35,36, 38, 41, 44, 47, 48, 51,52,53,54,55, 57, 59, 61, 64], social/professional role/identity (n = 22; 18 studies) [29, 30, 32, 35, 36, 40,41,42, 45, 46, 48, 50, 53, 55, 58, 59, 62, 63], reinforcement (n = 16; 13 studies) [29, 32, 33, 41, 45, 47, 48, 52, 53, 55, 61, 63, 64], memory (n = 14; 13 studies) [29, 30, 32, 35, 41, 44, 47, 53, 54, 57, 59, 61, 64], social influence (n = 10; 8 studies) [28, 32, 35, 41, 52, 54, 55, 64] were often targeted. The only domain that was not targeted by interventions in the included studies was optimism. Table 4 provides a detailed mapping of interventions BCTs to TDF domains.
Description of how studies targeted the TDF domains through the use of BCTs (see Additional file 3)
Many of the identified BCTs target more than one TDF domain according to Michie et al.’s guide (the Theory and Techniques Tool, https://theoryandtechniquetool.humanbehaviourchange.org/tool, [26, 27]). For example, 4.1 instruction on how to perform the behaviour maps to three TDF domains (knowledge, skills and beliefs about capabilities) meaning that using the BCT of 4.1 may help to overcome barriers at one or all three of these domains. Thus, where applicable, according to the Theory and Techniques tool, TDF domains that were frequently targeted together have been described together below. As stated in the methods, for this section of the synthesis, we have only reported a link between a BCT and mechanism of action where it has strong evidence. In cases where there were no links with strong evidence, we have reported that and cited the links with weak evidence (see the Theory and Techniques tool).
Knowledge, skills and beliefs about capabilities
Of the studies targeting the domains of knowledge, skills and beliefs about capabilities, 31 interventions (26 studies) used the BCT 4.1 ‘instruction on how to perform the behaviour’ by providing education on imaging guidelines either via active (face-to-face education sessions or webinars) or passive dissemination (email or postal delivery of the guideline). Nine of these interventions (6 studies) also provided education on topics related to imaging such as indicators for imaging, consequences of inappropriate imaging (BCT 5.1 ‘information about health consequences’) and alternatives to imaging, while 3 interventions (3 studies) provided education that was not specific to a guideline (such as communication skills training). Five studies explicitly used the BCT 8.1 ‘behavioural practice/rehearsal’ through interactive practice (n = 2), role play (n = 2), and skill rehearsal (n = 1). Six studies used additional strategies to specifically target beliefs about capabilities which included the use of patient scenarios (n = 2) (BCT 8.1) and demonstration of desired behaviours (BCT 6.1 ‘demonstration of the behaviour’) including how to use new clinical tools (such as decision support tools) in a consultation or how to prescribe an activity programme instead of ordering an image (n = 4).
Social/professional role and identity
There is weak evidence that 21 interventions targeted this domain (18 studies) with the BCT 9.1 ‘credible source’. The majority implemented this BCT by using guidelines produced by a recognised body/credible source (n = 17 interventions, 14 studies). The remaining studies implemented this BCT through accreditation of their training with a professional body (n = 1) or by using experts to deliver education/training (n = 4 interventions, 4 studies).
Beliefs about consequences; intentions
Five studies targeted the domains beliefs about consequences and intentions through the BCT 5.1 ‘information about health consequences’ by focusing on the negative consequences of imaging (n = 3) and providing education on radiation exposure (n = 2). One additional study targeted ‘intentions’, along with the domain of goals, through goal setting (BCT 1.1 ‘goal setting (behaviour)’).
Reinforcement
There is weak evidence that 17 interventions (14 studies) targeted this domain. Eleven of these interventions (10 studies) used feedback from an audit or assessment (BCT 2.2 ‘feedback on behaviour’) and 3 studies combined feedback with use of reminders (BCT 7.1 ‘prompts/cues’). 6 interventions (5 studies) used reminders only and one of these combined reminders with pre-commitment (BCT 7.1).
Environmental context and resources; memory, attention and decision processes
Seventeen interventions (16 studies) targeted environmental context and resources through either a single or multiple BCTs. 13 interventions (12 studies) used the BCT 7.1 ‘prompts/cues’ through decision tools (n = 6 interventions/studies) and reminders (n = 7 interventions, 6 studies). 5 interventions (5 studies) used the BCT 12.5 ‘adding objects to the environment’ with patient materials, 1 intervention (1 study) used the BCT 12.1 ‘restructuring the physical environment’ through restricted reimbursement, and 5 interventions (5 studies) used the BCT 12.2 ‘restructuring the social environment’ by implementing soft, medium or hard stops to the image ordering process. A soft stop included changes to the ordering process to require additional details, a medium stop included a peer to peer conversation as part of the ordering process, and a hard stop included either sign off from a consultant to order an image or an inability to order an image without the presence of red flags. The studies described above that used reminders and/or decision tools (BCT 7.1 ‘prompts/cues’) will have also targeted the domain of memory, attention and decision processes (n = 9 interventions, 8 studies).
Social influences
Eight interventions (6 studies) targeted social influences though the BCT 6.2 ‘social comparison’, namely through peer comparison, feeding back information on how an individual’s or practices’ behaviour compared to those of their peers or a specialist in the field (n = 7 interventions, 5 studies).
Behavioural regulation and emotion
One study targeted these domains with the BCT 2.3 ‘self-monitoring of own behaviour’. There is weak evidence that one study targeted the domain Behavioural regulation with the BCT 1.1 ‘goal setting (behaviour)’. There is weak evidence that one study targeted the domain Emotion with the BCT 13.2 ‘framing/reframing’.
Discussion
Summary
Searching up to February 1, 2021, we found 38 studies evaluating interventions designed to reduce unnecessary LBP imaging. Unlike previous reviews in this field, this review did not explore intervention effectiveness and instead, focused solely on developing an understanding of these implementation interventions designed to reduce LBP imaging. Thus, this review identifies what BCTs have been used to reduce LBP imaging for the first time and, through mapping these BCTs to corresponding TDF domains, provides unique insight into the interventions’ mechanisms of action.
This review highlights that the majority of studies in this field have used education to target the domains of knowledge, skills and beliefs about capabilities to bring about a change in LBP imaging behaviour. Just over half of the studies used reminders, decision tools or changes to the image ordering process to target the domain environmental context and resources. Lastly, for just over half of the studies, inconclusive evidence from the Theory and Techniques Tool suggests that by using feedback and reminders, studies will have targeted the domain of reinforcement, and through using materials from a credible source, will have targeted the domain of social/professional role and identity.
Strengths
We utilised a comprehensive search strategy across a range of databases and included hand searching references from relevant articles to identify studies. Our primary analysis was guided by the validated and widely used BCT taxonomy, enabling readers to easily draw comparisons to other studies and build on the current work. Our secondary analysis was informed by the Theory and Techniques Tool, developed by international leaders in the field of behaviour change. We iteratively developed a BCT code book, detailing all coding assumptions and rules, to ensure consistency between coders and to provide transparency to readers. Lastly, we used at least two reviewers to code BCTs and TDF domains, utilising a third reviewer where needed to resolve any ambiguity or discrepancies.
Limitations
While the search strategy we used was comprehensive and we did identify additional studies from hand-searching the references of other relevant systematic reviews, it is still possible that some studies were missed. Further, our conservative coding may have resulted in missing BCTs that more liberal coders may have included; better reporting of study interventions would have allowed us to more accurately capture all BCTs.
Implications for research
This review highlighted that nearly all study interventions were poorly designed, failing to use theory to inform intervention development and preventing assessments of fidelity and process outcomes. Despite international recognition that behaviour change interventions should be underpinned by theory, only 6 (21%) of our included studies could be classified as having utilised some element of theory to inform their intervention design. This finding is in line with a large systematic review that explored the use of theory in the design of guideline dissemination and implementation strategies [66]. Davies et al. found that only 22.5% of studies (n = 235) utilised theory in some way and noted there was inadequate justification for intervention choice [66]. A lack of theory in behaviour change intervention design has been reported in other fields, for example, a systematic review of interventions designed to improve self-management of LBP and arthritis found that only 12% of studies utilised theory [67]. These findings suggest that BCTs are frequently selected based on availability/ease of delivery/cost, as opposed to being actively selected to target known barriers to the behaviour. A recent systematic review synthesised 14 qualitative studies with physicians worldwide and found high-level evidence that 3 TDF domains influenced LBP imaging behaviour: (i) Social influence (patient demand), (ii) Beliefs about consequences (lack of ability to explain why an image is not needed) and (iii) Environmental context and resources (lack of time) [18]. However, we found less than a quarter of our included studies targeted Social influence and even fewer targeted Beliefs about consequences. Thus, highlighting the need to use more robust methods, guided by theory, to select BCTs that target LBP image ordering behaviour.
Conclusions
This is the first systematic review to synthesise interventions designed to reduce physician LBP image ordering behaviour to identify intervention BCTs. We found the most frequently used BCTs were ‘instruction on how to perform the behaviour’ (most commonly through education based on imaging guidelines), ‘feedback on behaviour’ (most commonly through audit and feedback), ‘prompts and cues’ (most commonly through automated decision support pop-ups or hard-copy guideline-based reminders/decision aids on when to image) and ‘credible source’ (guidelines produced from a credible source or endorsed by a reputable peer). Consequently, the most frequently targeted TDF domains were knowledge, skills and beliefs about capabilities. Importantly, this review identified a lack of theory and rationale in the selection of intervention BCTs with the majority of studies failing to include BCTs to target known physician-reported barriers. Future work should utilise theory to develop interventions specifically targeting known barriers to reducing LBP image ordering.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- BCT:
-
Behaviour change techniques
- ITS:
-
Interrupted time series
- LBP:
-
Low back pain
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- RCT:
-
Randomised controlled trial
- TDF:
-
Theoretical domains framework
- UBA:
-
Uncontrolled before and after studies
References
Canada CW. Imaging tests for lower back pain: when you need them and when you don’t. Secondary Imaging Tests for Lower Back Pain: When you need them and when you don’t 2017-05-30T20:33:00+00:00 2017.
NE OC, Cook CE, Wand BM, Ward SP. Clinical guidelines for low back pain: A critical review of consensus and inconsistencies across three major guidelines. Best Pract Res Clin Rheumatol. 2016;30(6):968–80. https://doi.org/10.1016/j.berh.2017.05.001 [published Online First: Epub Date].
UK CW. Royal College of Radiology Recommendations. Secondary Royal College of Radiology Recommendations Updated 2020. https://www.choosingwisely.co.uk/i-am-a-clinician/recommendations/#1476656358304-3b84e1d4-043d.
Downie A, Hancock M, Jenkins H, et al. How common is imaging for low back pain in primary and emergency care? Systematic review and meta-analysis of over 4 million imaging requests across 21 years. Br J Sports Med. 2020;54(11):642–51. https://doi.org/10.1136/bjsports-2018-100087 [published Online First: Epub Date].
Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–47. https://doi.org/10.1016/S0140-6736(16)30970-9 [published Online First: Epub Date].
Lemmers GPG, van Lankveld W, Westert GP, van der Wees PJ, Staal JB. Imaging versus no imaging for low back pain: a systematic review, measuring costs, healthcare utilization and absence from work. Eur Spine J. 2019;28(5):937–50. https://doi.org/10.1007/s00586-019-05918-1 [published Online First: Epub Date].
French SD, Green S, Buchbinder R, Barnes H. Interventions for improving the appropriate use of imaging in people with musculoskeletal conditions. Cochrane Database Syst Rev. 2010. https://doi.org/10.1002/14651858.CD006094.pub2 [published Online First: Epub Date].
Jenkins HJ, Hancock MJ, French SD, Maher CG, Engel RM, Magnussen JS. Effectiveness of interventions designed to reduce the use of imaging for low-back pain: a systematic review. Can Med Assoc J. 2015;187(6):401–8. https://doi.org/10.1503/cmaj.141183 [published Online First: Epub Date].
Liu C, Desai S, Krebs LD, et al. Effectiveness of Interventions to decrease image ordering for low back pain presentations in the emergency department: a systematic review. Acad Emerg Med. 2018;25(6):614–26. https://doi.org/10.1111/acem.13376 [published Online First: Epub Date].
Mesner SA, Foster NE, French SD. Implementation interventions to improve the management of non-specific low back pain: a systematic review. BMC Musculoskeletal Disord. 2016;17(1):258. https://doi.org/10.1186/s12891-016-1110-z [published Online First: Epub Date].
Craig P, Petticrew M. Developing and evaluating complex interventions: reflections on the 2008 MRC guidance. Int J Nurs Stud. 2013;50(5):585–7. https://doi.org/10.1016/j.ijnurstu.2012.09.009 [published Online First: Epub Date].
NICE. Overview | Behaviour change: general approaches | Guidance | NICE. Secondary Overview | Behaviour change: general approaches | Guidance | NICE. 2007.
Michie S, Atkins L, West R. The behaviour change wheel book - a guide to designing interventions. Great Britain: Silverback Publishing; 2014.
Atkins L, Francis J, Islam R, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implementation Sci. 2017;12(1):77. https://doi.org/10.1186/s13012-017-0605-9 [published Online First: Epub Date].
Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Sci. 2012;7(1):37. https://doi.org/10.1186/1748-5908-7-37 [published Online First: Epub Date].
Michie S, Francis J, Hardeman W, Eccles M. From Theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol. 2008;57(4):660–80. https://doi.org/10.1111/j.1464-0597.2008.00341.x.
Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14(1):26–33. https://doi.org/10.1136/qshc.2004.011155 [published Online First: Epub Date].
Hall AM, Scurrey SR, Pike AE, et al. Physician-reported barriers to using evidence-based recommendations for low back pain in clinical practice: a systematic review and synthesis of qualitative studies using the Theoretical Domains Framework. Implementation Sci. 2019;14(1):49. https://doi.org/10.1186/s13012-019-0884-4 [published Online First: Epub Date].
Willett M, Duda J, Fenton S, Gautrey C, Greig C, Rushton A. Effectiveness of behaviour change techniques in physiotherapy interventions to promote physical activity adherence in lower limb osteoarthritis patients: A systematic review. PLoS One. 2019;14(7):e0219482. https://doi.org/10.1371/journal.pone.0219482 [published Online First: Epub Date].
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(jul21 1):b2700–b00. https://doi.org/10.1136/bmj.b2700 [published Online First: Epub Date].
FM ALZ, Menon A, Mayo NE, Bussières AE. The effectiveness of interventions designed to increase the uptake of clinical practice guidelines and best practices among musculoskeletal professionals: a systematic review. BMC Health Serv Res. 2018;18(1):435. https://doi.org/10.1186/s12913-018-3253-0 [published Online First: Epub Date].
Tzortziou Brown V, Underwood M, Mohamed N, Westwood O, Morrissey D. Professional interventions for general practitioners on the management of musculoskeletal conditions. Cochrane Database Syst Rev. 2016. https://doi.org/10.1002/14651858.CD007495.pub2 [published Online First: Epub Date].
Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348(mar07 3):g1687–g87. https://doi.org/10.1136/bmj.g1687 [published Online First: Epub Date].
Painter JE, Borba CPC, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med. 2008;35(3):358–62. https://doi.org/10.1007/s12160-008-9042-y [published Online First: Epub Date].
Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. https://doi.org/10.1007/s12160-013-9486-6 [published Online First: Epub Date].
Carey RN, Connell LE, Johnston M, et al. Behavior change techniques and their mechanisms of action: a synthesis of links described in published intervention literature. Ann Behav Med. 2019;53(8):693–707. https://doi.org/10.1093/abm/kay078 [published Online First: Epub Date].
Connell LE, Carey RN, de Bruin M, Rothman AJ, Johnston M, Kelly MP, Michie S. Links Between Behavior Change Techniques and Mechanisms of Action: An Expert Consensus Study. Ann Behav Med. 2019;53(8):708-20. https://doi.org/10.1093/abm/kay082.
Baker RA, Lantos G, Gallagher E. The effect of restricting the indications for lumbosacral spine radiography in patients with acute back symptoms. Am J Roentgenol. 1987;149(3):535–8. https://doi.org/10.2214/ajr.149.3.535 [published Online First: Epub Date].
Chandra K, Atkinson PR, Fraser J, Chatur H, Adams C. MP31: The contrarian effect: how does a Choosing Wisely focused knowledge translation initiative affect emergency physician practice in a high awareness-low investigation environment? CJEM. 2017;19(S1):S75–6. https://doi.org/10.1017/cem.2017.197 [published Online First: Epub Date].
Chen D, Bhambhvani HP, Hom J, et al. Effect of electronic clinical decision support on imaging for the evaluation of acute low back pain in the ambulatory care setting. World Neurosurg. 2020;134:e874–e77. https://doi.org/10.1016/j.wneu.2019.11.031 [published Online First: Epub Date].
Dey P, Simpson CWR, Collins SI, et al. Implementation of RCGP guidelines for acute low back pain: a cluster randomised controlled trial. Br J Gen Pract. 2004;5:33-37.
Eccles M, Steen N, Grimshaw J, et al. Effect of audit and feedback, and reminder messages on primary-care radiology referrals: a randomised trial. Lancet. 2001;357(9266):1406–9. https://doi.org/10.1016/S0140-6736(00)04564-5 [published Online First: Epub Date].
Fenton JJ, Kravitz RL, Jerant A, et al. Promoting patient-centered counseling to reduce use of low-value diagnostic tests: a randomized clinical trial. JAMA Intern Med. 2016;176(2):191. https://doi.org/10.1001/jamainternmed.2015.6840 [published Online First: Epub Date].
Fine B, Schultz SE, White L, Henry D. Impact of restricting diagnostic imaging reimbursement for uncomplicated low back pain in Ontario: a population-based interrupted time series analysis. CMAJ Open. 2017;5(4):E760–E67. https://doi.org/10.9778/cmajo.20160151 [published Online First: Epub Date].
Freeborn DK, Shye D, Mullooly JP, Eraker S, Romeo J. Primary care physiciansʼ use of lumbar spine imaging tests: effects of guidelines and practice pattern feedback. J Gen Intern Med. 1997;12(10):619–25. https://doi.org/10.1046/j.1525-1497.1997.07122.x [published Online First: Epub Date].
French SD, McKenzie JE, O'Connor DA, et al. Evaluation of a theory-informed implementation intervention for the management of acute low back pain in general medical practice: the IMPLEMENT cluster randomised trial. PLoS One. 2013;8(6):e65471. https://doi.org/10.1371/journal.pone.0065471 [published Online First: Epub Date].
Fried JG, Andrew AS, Ring NY, Pastel DA. Changes in primary care health care utilization after inclusion of epidemiologic data in lumbar spine MR imaging reports for uncomplicated low back pain. Radiology. 2018;287(2):563–9. https://doi.org/10.1148/radiol.2017170722 [published Online First: Epub Date].
Graves JM, Fulton-Kehoe D, Jarvik JG, Franklin GM. Impact of an advanced imaging utilization review program on downstream health care utilization and costs for low back pain. Med Care. 2018;56(6):520–8. https://doi.org/10.1097/MLR.0000000000000917 [published Online First: Epub Date].
Haig A, Uren B, Loar S, et al. The impact of a complex consulting process with physiatry on emergency department management of back pain. J Int Soc Phys Rehabil Med. 2019;2(2):77. https://doi.org/10.4103/jisprm.jisprm_1_19 [published Online First: Epub Date].
Hollingworth W, Todd CJ, King H, et al. Primary care referrals for lumbar spine radiography: diagnostic yield and clinical guidelines. Br J Gen Pract. 2002;6:475-80.
Ip IK, Gershanik EF, Schneider LI, et al. Impact of IT-enabled Intervention on MRI use for back pain. Am J Med. 2014;127(6):512–18.e1. https://doi.org/10.1016/j.amjmed.2014.01.024 [published Online First: Epub Date].
Jackson JL, Browning R. Impact of national low back pain guidelines on clinical practice. Southern Med J. 2005;98(2):139–43. https://doi.org/10.1097/01.SMJ.0000136261.21711.85 [published Online First: Epub Date].
Jarvik JG, Comstock BA, James KT, et al. Lumbar Imaging With Reporting Of Epidemiology (LIRE)—protocol for a pragmatic cluster randomized trial. Contemp Clin Trials. 2015;45:157–63. https://doi.org/10.1016/j.cct.2015.10.003 [published Online First: Epub Date].
Jenkins HJ, Moloney NA, French SD, et al. Using behaviour change theory and preliminary testing to develop an implementation intervention to reduce imaging for low back pain. BMC Health Serv Res. 2018;18(1):734. https://doi.org/10.1186/s12913-018-3526-7 [published Online First: Epub Date].
Kerry S, Oakeshott P, Dundas D, Williams J. Influence of postal distribution of The Royal College of Radiologistsʼ guidelines, together with feedback on radiological referral rates, on X-ray referrals from general practice: a randomized controlled trial. Fam Pract. 2000;17(1):46–52. https://doi.org/10.1093/fampra/17.1.46 [published Online First: Epub Date].
Klein BJ, Radecki RT, Foris MP, Feil EI, Hickey ME. Bridging the gap between science and practice in managing low back pain. A comprehensive spine care system in a health maintenance organization setting. Spine. 2000;25(6):738–40. https://doi.org/10.1097/00007632-200003150-00015 [published Online First: Epub Date].
Kullgren JT, Krupka E, Schachter A, et al. Precommitting to choose wisely about low-value services: a stepped wedge cluster randomised trial. BMJ Qual Saf. 2018;27(5):355–64. https://doi.org/10.1136/bmjqs-2017-006699 [published Online First: Epub Date].
Lin IB, Coffin J, O’Sullivan PB. Using theory to improve low back pain care in Australian Aboriginal primary care: a mixed method single cohort pilot study. BMC Fam Pract. 2016;17(1):44. https://doi.org/10.1186/s12875-016-0441-z [published Online First: Epub Date].
Machado GC, Richards B, Needs C, et al. Implementation of an evidence-based model of care for low back pain in emergency departments: protocol for the Sydney Health Partners Emergency Department (SHaPED) trial. BMJ Open. 2018;8(4):e019052. https://doi.org/10.1136/bmjopen-2017-019052 [published Online First: Epub Date].
Matowe L, Ramsay CR, Grimshaw JM, Gilbert FJ, Macleod M-J, Needham G. Effects of mailed dissemination of the Royal College of Radiologistsʼ guidelines on general practitioner referrals for radiography: a time series analysis. Clin Radiol. 2002;57(7):575–8. https://doi.org/10.1053/crad.2001.0894 [published Online First: Epub Date].
Min A, Chan VWY, Aristizabal R, et al. Clinical decision support decreases volume of imaging for low back pain in an urban emergency department. J Am Coll Radiol. 2017;14(7):889–99. https://doi.org/10.1016/j.jacr.2017.03.005 [published Online First: Epub Date].
Morgan T, Wu J, Ovchinikova L, Lindner R, Blogg S, Moorin R. A national intervention to reduce imaging for low back pain by general practitioners: a retrospective economic program evaluation using Medicare Benefits Schedule data. BMC Health Serv Res. 2019;19(1):983. https://doi.org/10.1186/s12913-019-4773-y [published Online First: Epub Date].
Oakeshott P, Kerry SM, Williams JE. Randomized controlled trial of the effect of the Royal College of Radiologistsʼ guidelines on general practitionersʼ referrals for radiographic examination. Br J Gen Pract. 1994;4:197-200.
Powell AC, Lugo CT, Wang Y, et al. Modification and reinitiation of lower back imaging orders after evidence-based collaborative consultation. Acad Radiol. 2019;26(11):1450–6. https://doi.org/10.1016/j.acra.2018.12.001 [published Online First: Epub Date].
Robling MR, Houston HLA, Kinnersley P, et al. General practitionersʼ use of magnetic resonance imaging: an open randomized trial comparing telephone and written requests and an open randomized controlled trial of different methods of local guideline dissemination. Clin Radiol. 2002;57(5):402–7. https://doi.org/10.1053/crad.2001.0864 [published Online First: Epub Date].
Schectman JM, Schroth WS, Verme D, Voss JD. Randomized controlled trial of education and feedback for implementation of guidelines for acute low back pain. J Gen Int Med. 2003;18(10):773–80. https://doi.org/10.1046/j.1525-1497.2003.10205.x [published Online First: Epub Date].
Simula AS, Jenkins HJ, Holopainen R, et al. Transcultural adaption and preliminary evaluation of "understanding low back pain" patient education booklet. BMC Health Serv Res. 2019;19(1):1010. https://doi.org/10.1186/s12913-019-4854-y [published Online First: Epub Date].
Slater H, Briggs AM, Smith AJ, Bunzli S, Davies SJ, Quintner JL. Implementing evidence-informed policy into practice for health care professionals managing people with low back pain in Australian rural settings: a preliminary prospective single-cohort study. Pain Med. 2014;15(10):1657–68. https://doi.org/10.1111/pme.12351 [published Online First: Epub Date].
Solberg LI, Wei F, Butler JC, Palattao KJ, Vinz CA, Marshall MA. Effects of electronic decision support on high-tech diagnostic imaging orders and patients. Am J Manag Care. 2010;16(2):102–6.
Suman A, Schaafsma FG, van de Ven PM, et al. Effectiveness of a multifaceted implementation strategy compared to usual care on low back pain guideline adherence among general practitioners. BMC Health Serv Res. 2018;18(1):358. https://doi.org/10.1186/s12913-018-3166-y [published Online First: Epub Date].
Tracey NG, Martin JB, McKinstry CS, Mathew BM. Guidelines for lumbar spine radiography in acute low back pain: effect of implementation in an accident and emergency department. The Ulster Medical Journal. 1994;63(1):6.
Wang KY, Chong I, Consul N, Lincoln CM. To Sustain or not to sustain: Varying educational sessions on advanced imaging of low back pain and R-SCAN. Curr Probl Diagn Radiol. 2020. https://doi.org/10.1067/j.cpradiol.2020.10.017 [published Online First: Epub Date].
Winkens RAG, Pop P, Bugter-Maessen AMA, et al. Randomised controlled trial of routine individual feedback to improve rationality and reduce numbers of test requests. Lancet. 1995;345(8948):498–502. https://doi.org/10.1016/S0140-6736(95)90588-X [published Online First: Epub Date].
Zafar HM, Ip IK, Mills AM, Raja AS, Langlotz CP, Khorasani R. Effect of Clinical decision support–generated report cards versus real-time alerts on primary care provider guideline adherence for low back pain outpatient lumbar spine MRI orders. Am J Roentgenol. 2019;212(2):386–94. https://doi.org/10.2214/AJR.18.19780 [published Online First: Epub Date].
Burggraf L, Stark S, Schedlbauer A, Kühlein T, Roos M. 10 Ideas, concerns and expectations (ICE) in general practice consultations – report of a mixed methods study. BMJ Evid Based Med. 2019;24(Suppl 2):A11. https://doi.org/10.1136/bmjebm-2019-POD.24 [published Online First: Epub Date].
Davies P, Walker AE, Grimshaw JM. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implementation Sci. 2010;5(1):14. https://doi.org/10.1186/1748-5908-5-14 [published Online First: Epub Date].
Keogh A, Tully MA, Matthews J, Hurley DA. A review of behaviour change theories and techniques used in group based self-management programmes for chronic low back pain and arthritis. Man Ther. 2015;20(6):727–35. https://doi.org/10.1016/j.math.2015.03.014 [published Online First: Epub Date].
Acknowledgements
We would like to acknowledge Daphne To for providing assistance with the title/abstract screening process.
Author information
Authors and Affiliations
Contributions
AH conceived the project, designed the review, synthesised the data, drafted and refined the paper. AH, HR, CA, and JT extracted and coded data, contributed to the writing, and critically revised the manuscript. AP and RL extracted data and with HR contributed to data synthesis. JM, JH, HE, and AP assisted with the methodology, data coding and critically revised the manuscript. MS re-designed original search strategy, contributed to writing the response to reviews and the “Methods” section, and critically reviewed the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Consent for publication is not required as no individual person’s data in any form is presented in the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hall, A., Richmond, H., Pike, A. et al. What behaviour change techniques have been used to improve adherence to evidence-based low back pain imaging?. Implementation Sci 16, 68 (2021). https://doi.org/10.1186/s13012-021-01136-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13012-021-01136-w