Abstract
Purpose
Imaging (X-ray, CT and MRI) provides no health benefits for low back pain (LBP) patients and is not recommended in clinical practice guidelines. Whether imaging leads to increased costs, healthcare utilization or absence from work is unclear. Therefore, this study systematically reviews if imaging in patients with LBP leads to an increase in these outcomes.
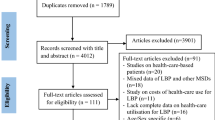
Methods
We searched PubMed, CINAHL, EMBASE, Cochrane Library and Web of Science until October 2017 for randomized controlled trials (RCTs) and observational studies (OSs), comparing imaging versus no imaging on targeted outcomes. Data extraction and risk of bias assessment was performed independently by two reviewers. The quality of the body of evidence was determined using GRADE methodology.
Results
Moderate-quality evidence (1 RCT; n = 421) supports that direct costs increase for patients undergoing X-ray. Low-quality evidence (3 OSs; n = 9535) supports that early MRI may lead to an increase in costs. There is moderate-quality evidence (1 RCT, 2 OSs; n = 3897) that performing MRI or imaging (MRI or CT) is associated with an increase in healthcare utilization (e.g., future injections, surgery, medication, etc.). There is low-quality evidence (5 OSs; n = 15,493) that performing X-ray or MRI is associated with an increase in healthcare utilization. Moderate-quality evidence (2 RCTs; n = 667) showed no significant differences between X-ray or MRI groups compared with non-imaging groups on absence from work. However, low-quality evidence (2 Oss; n = 7765) did show significantly greater mean absence from work in the MRI groups in comparison with the non-imaging groups.
Conclusions
Imaging in LBP may be associated with higher medical costs, increased healthcare utilization and more absence from work.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.


Similar content being viewed by others
References
Becker A, Held H, Redaelli M et al (2010) Low back pain in primary care. Spine (Phila Pa 1976) 35:1714–1720. https://doi.org/10.1097/BRS.0b013e3181cd656f
Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WDCT (2009) The rising prevalence of chronic low back pain. Med Arch Intern 169:8–9. https://doi.org/10.1001/archinternmed.2008.543.The
Manchikanti L, Benyamin RM, Falco FJE, Hirsch JA (2013) Recommendations of the Medicare Payment Advisory Commission (MEDPAC) on the health care delivery system: the impact on interventional pain management in 2014 and beyond. Pain Physician 16:419–440
Vos T, Flaxman AD, Naghavi M et al (2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2163–2196. https://doi.org/10.1016/S0140-6736(12)61729-2
Dagenais S, Caro J, Haldeman S (2008) A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 8:8–20. https://doi.org/10.1016/j.spinee.2007.10.005
Lin C-WC, Li Q, Williams CM et al (2018) The economic burden of guideline-recommended first line care for acute low back pain. Eur Spine J 27(1):109–116. https://doi.org/10.1007/s00586-016-4781-0
Ma VY, Chan L, Carruthers K (2015) The incidence, prevalence, costs and impact on disability of common conditions requiring rehabilitation in the US: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back. Pain 95:986–995. https://doi.org/10.1016/j.apmr.2013.10.032.The
Martin BI, Deyo RA, Mirza SK et al (2008) Expenditures and health status among adults with back and neck problems. JAMA 299:656–664. https://doi.org/10.1001/jama.299.6.656
Lambeek LC, Van Tulder MW, Swinkels ICS et al (2011) The trend in total cost of back pain in the netherlands in the period 2002 to 2007. Spine (Phila Pa 1976) 36:1050–1058. https://doi.org/10.1097/BRS.0b013e3181e70488
Hartvigsen J, Hancock MJ, Kongsted A et al (2018) What low back pain is and why we need to pay attention. Lancet 391(10137):2356–2367. https://doi.org/10.1016/S0140-6736(18)30480-X
Dagenais SHS (2012) Evidence-based management of low back pain. In: Dagenais S, Haldeman S (eds) Evidence-based management of low back pain. Mosby, St Louis, pp 1–12
Foster N, Anema J, Cherkin D et al (2018) Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 391(10137):2368–2383. https://doi.org/10.1016/S0140-6736(18)30489-6
Stochkendahl MJ, Kjaer P, Hartvigsen J et al (2018) National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J 27:60–75. https://doi.org/10.1007/s00586-017-5099-2
Koes BW, van Tulder MW, Ostelo R et al (2001) Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine (Phila Pa 1976) 26:2504
Verhagen AP, Downie A, Maher CG, Koes BW (2017) Most red flags for malignancy in low back pain guidelines lack empirical support: a systematic review. Pain 158(10):1860–1868. https://doi.org/10.1097/j.pain.0000000000000998
Hanney WJ, Masaracchio M, Liu X, Kolber MJ (2016) The influence of physical therapy guideline adherence on healthcare utilization and costs among patients with low back pain: a systematic review of the literature. PLoS ONE 11:1–18. https://doi.org/10.1371/journal.pone.0156799
Jenniskens K, de Groot JAH, Reitsma JB et al (2017) Overdiagnosis across medical disciplines: a scoping review. BMJ Open 7:e018448. https://doi.org/10.1136/bmjopen-2017-018448
Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS (1994) Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 14;331(2):69–73
Boden SD, Davis DO, Dina TS et al (1990) Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am 72:403–408
Van Tulder MW, Assendelft WJJ, Koes BW, Bouter LM (1997) Spinal radiographic findings and nonspecific low back pain: a systematic review of observational studies. Spine (Phila Pa 1976) 22:427–434
Brinjikji W, Luetmer PH, Comstock B et al (2015) Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol 36(4):811–816. https://doi.org/10.3174/ajnr.A4173
Jarvik JG, Deyo RA (2002) Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med 137:586–597
Steffens D, Hancock MJ, Maher CG et al (2014) Does magnetic resonance imaging predict future low back pain? A systematic review. Eur J Pain 18:755–765. https://doi.org/10.1002/j.1532-2149.2013.00427.x
Pham HH, Landon BE, Reschovsky JD et al (2009) Rapidity and modality of imaging for acute low back pain in elderly patients. Arch Intern Med 169:972–981. https://doi.org/10.1001/archinternmed.2009.78
Webster BS, Cifuentes M (2010) Relationship of early magnetic resonance imaging for work-related acute low back pain with disability and medical utilization outcomes. J Occup Environ Med 52:900–907. https://doi.org/10.1097/JOM.0b013e3181ef7e53
Dagenais S, Galloway EK, Roffey DM (2014) A systematic review of diagnostic imaging use for low back pain in the United States. Spine J 14:1036–1048. https://doi.org/10.1016/j.spinee.2013.10.031
Mafi J, McCarthy EP, Davis RB, Landon BE (2013) Worsening trends in the management and treatment of back pain. JAMA 173:1573–1581. https://doi.org/10.1001/jamainternmed.2013.8992
Lurie JD, Birkmeyer NJ, Weinstein JN (2003) Rates of advanced spinal imaging and spine surgery. Spine (Phila Pa 1976) 28:616–620. https://doi.org/10.1097/01.BRS.0000049927.37696.DC
Chou R, Fu R, Carrino JA, Deyo RA (2009) Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet 373:463–472. https://doi.org/10.1016/S0140-6736(09)60172-0
Jarvik JG, Gold LS, Comstock BA et al (2015) Association of early imaging for back pain with clinical outcomes in older adults. JAMA 313:1143–1153. https://doi.org/10.1001/jama.2015.1871
Sox HCJ, Margulies I, Sox CH (1981) Psychologically mediated effects of diagnostic tests. Ann Intern Med 95:680–685
Verbeek J, Sengers M-J, Riemens L, Haafkens J (2004) Patient expectations of treatment for back pain: a systematic review of qualitative and quantitative studies. Spine (Phila Pa 1976) 29:2309–2318
Wilson IB, Dukes K, Greenfield S et al (2001) Patients’ role in the use of radiology testing for common office practice complaints. Arch Intern Med 161:256–263
Blank L, Baxter S, Woods HB et al (2014) Referral interventions from primary to specialist care: a systematic review of international evidence. Br J Gen Pract 64:e765–e774. https://doi.org/10.3399/bjgp14X682837
Blank L, Baxter S, Woods HB et al (2015) What is the evidence on interventions to manage referral from primary to specialist non-emergency care? A systematic review and logic model synthesis. Health Serv Deliv Res 3:1–430. https://doi.org/10.3310/hsdr03240
Itz CJ, Ramaekers BL, van Kleef M, Dirksen CD (2017) Medical specialists care and hospital costs for low back pain in the Netherlands. Eur J Pain (United Kingdom) 21:705–715. https://doi.org/10.1002/ejp.974
Karel YHJM, Verkerk K, Endenburg S et al (2015) Effect of routine diagnostic imaging for patients with musculoskeletal disorders: a meta-analysis. Eur J Intern Med 26:585–595. https://doi.org/10.1016/j.ejim.2015.06.018
Vrabel M (2015) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Oncol Nurs Forum 42:552–554. https://doi.org/10.1188/15.ONF.552-554
Higgins J (2008) Cochrane handbook for systematic reviews of interventions version 5.0.0. Cochrane Collaboration
Institute. NHL and B (2014) Quality assessment tool for observational cohort and cross-sectional studies—NHLBI, NIH. National Institutes of Health, Bethesda, MD
Canfield SE, Dahm P (2011) Rating the quality of evidence and the strength of recommendations using GRADE. World J Urol 29:311–317. https://doi.org/10.1007/s00345-011-0667-2
Baker A, Young K, Potter J, Madan I (2010) A review of grading systems for evidence-based guidelines produced by medical specialties. Clin Med 10:358–363. https://doi.org/10.7861/clinmedicine.10-4-358
Djulbegovic B, Trikalinos TA, Roback J et al (2009) Impact of quality of evidence on the strength of recommendations: an empirical study. BMC Health Serv Res 9:120. https://doi.org/10.1186/1472-6963-9-120
Schünemann H, Brożek J, Guyatt G, Oxman A E (2013) GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group
Guyatt GH, Oxman AD, Vist GE et al (2009) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926. https://doi.org/10.1136/bmj.39489.470347.AD
Huguet A, Hayden JA, Stinson J et al (2013) Judging the quality of evidence in reviews of prognostic factor research: adapting the GRADE framework. Syst Rev 2:71. https://doi.org/10.1186/2046-4053-2-71
Shamliyan TA, Staal JB (2014) Epidural steroid injections for radicular lumbosacral pain: a systematic review. Phys Med Rehabil Clin N Am 25:471–489
Ryan R, Santesso N, Hill S (2016) Preparing Summary of Findings (SoF) tables. Cochrane Consumers and Communication Group, available at http://cccrg.cochrane.org/author-resources. Version 2.0 December 2016
Glenton C, Santesso N, Rosenbaum S et al (2010) Presenting the results of cochrane systematic reviews to a consumer audience: a qualitative study. Med Decis Making 30:566–577. https://doi.org/10.1177/0272989X10375853
Cohen SP, Gupta A, Strassels SA, Christo PJ, Erdek MA, Griffith SR, Kurihara C, Buckenmaier CC III, Cornblath D, Vu T-N (2012) Effect of MRI on treatment results or decision making in patients with lumbosacral radiculopathy referred for epidural steroid injections. Arch Intern Med 172:134. https://doi.org/10.1001/archinternmed.2011.593
Ash LM, Modic MT, Obuchowski NA et al (2008) Effects of diagnostic information, per se, on patient outcomes in acute radiculopathy and low back pain. AJNR Am J Neuroradiol 29:1098–1103. https://doi.org/10.3174/ajnr.A0999
Miller P, Kendrick D, Bentley E, Fielding K (2002) Cost-effectiveness of lumbar spine radiography in primary care patients with low back pain. Spine (Phila Pa 1976) 27:2291–2297. https://doi.org/10.1097/01.BRS.0000029264.83803.74
Kendrick D, Fielding K, Bentley E et al (2001) Radiography of the lumbar spine in primary care patients with low back pain: randomised controlled trial. BMJ 322:400–405. https://doi.org/10.1136/bmj.322.7283.400
Kerry S, Hilton S, Dundas D et al (2002) Radiography for low back pain: a randomised controlled trial and observational study in primary care. Br J Gen Pract 52:469–474
Gilbert FJ, Grant AM, Gillan MG et al (2004) Does early imaging influence management and improve outcome in patients with low back pain? A pragmatic randomised controlled trial. Health Technol Assess 8:iii, 1–131
Graves JM, Fulton-Kehoe D, Jarvik JG, Franklin GM (2014) Health care utilization and costs associated with adherence to clinical practice guidelines for early magnetic resonance imaging among workers with acute occupational low back pain. Health Serv Res 49:645–665. https://doi.org/10.1111/1475-6773.12098
Webster BS, Bauer AZ, Choi Y et al (2013) Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain. Spine (Phila Pa 1976) 38:1939–1946. https://doi.org/10.1097/BRS.0b013e3182a42eb6
Webster BS, Choi Y, Bauer AZ et al (2014) The cascade of medical services and associated longitudinal costs due to nonadherent magnetic resonance imaging for low back pain. Spine (Phila Pa 1976) 39:1433–1440. https://doi.org/10.1097/BRS.0000000000000408
Aaronson EL, Yun BJ, Mort E et al (2017) Association of magnetic resonance imaging for back pain on seven-day return visit to the emergency department. Emerg Med J. https://doi.org/10.1136/emermed-2016-206250
Fritz JM, Brennan GP, Hunter SJ (2015) Physical therapy or advanced imaging as first management strategy following a new consultation for low back pain in primary care: associations with future health care utilization and charges. Health Serv Res 50:1927–1940. https://doi.org/10.1111/1475-6773.12301
Carey M, Turon H, Goergen S et al (2015) Patients’ experiences of the management of lower back pain in general practice: use of diagnostic imaging, medication and provision of self-management advice. Aust J Prim Health 21:342–346. https://doi.org/10.1071/PY14057
Oliveira CB, Maher CG, Pinto RZ et al (2018) Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J 27:1–13. https://doi.org/10.1007/s00586-018-5673-2
Doniselli FM, Zanardo M, Manfrè L et al (2018) A critical appraisal of the quality of low back pain practice guidelines using the AGREE II tool and comparison with previous evaluations: a EuroAIM initiative. Eur Spine J 27:2781–2790. https://doi.org/10.1007/s00586-018-5763-1
Jenkins HJ, Downie AS, Maher CG et al (2018) Imaging for low back pain: is clinical use consistent with guidelines? A systematic review and meta-analysis. Spine J 18:2266–2277. https://doi.org/10.1016/j.spinee.2018.05.004
Wong JJ, Cote P, Sutton DA et al (2017) Clinical practice guidelines for the noninvasive management of low back pain: a systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur J Pain 21:201–216. https://doi.org/10.1002/ejp.931
Bernstein IA, Malik Q, Carville S, Ward S (2017) Low back pain and sciatica: summary of NICE guidance. BMJ 356:i6748. https://doi.org/10.1136/bmj.i6748
Qaseem A, Wilt TJ, McLean RM, Forciea MA (2017) Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med 166:514–530. https://doi.org/10.7326/M16-2367
Rizzardo A, Miceli L, Bednarova R et al (2016) Low-back pain at the emergency department: still not being managed? Ther Clin Risk Manag 12:183–187. https://doi.org/10.2147/TCRM.S91898
Rosenberg A, Agiro A, Gottlieb M et al (2015) Early trends among seven recommendations from the Choosing Wisely Campaign. JAMA Intern Med 175:1913–1920. https://doi.org/10.1001/jamainternmed.2015.5441
Werner EL, Ihlebaek C (2012) Primary care doctors’ management of low back pain patients-ten years after. Tidsskr Nor Laegeforen 132:2388–2390. https://doi.org/10.4045/tidsskr.12.0395
Baker SR, Rabin A, Lantos G, Gallagher EJ (1987) The effect of restricting the indications for lumbosacral spine radiography in patients with acute back symptoms. Am J Roentgenol 149:535–538. https://doi.org/10.2214/ajr.149.3.535
Eccles M, Steen N, Grimshaw J et al (2001) Effect of audit and feedback, and reminder messages on primary-care radiology referrals: a randomised trial. Lancet (London, England) 357:1406–1409. https://doi.org/10.1016/S0140-6736(00)04564-5
Riis A, Jensen CE, Bro F et al (2016) A multifaceted implementation strategy versus passive implementation of low back pain guidelines in general practice: a cluster randomised controlled trial. Implement Sci 11:1–10. https://doi.org/10.1186/s13012-016-0509-0
Jensen CE, Riis A, Petersen KD et al (2017) Economic evaluation of an implementation strategy for the management of low back pain in general practice. Pain 158:891–899. https://doi.org/10.1097/j.pain.0000000000000851
Suman A, Dikkers MF, Schaafsma FG et al (2016) Effectiveness of multifaceted implementation strategies for the implementation of back and neck pain guidelines in health care: a systematic review. Implement Sci 11:126. https://doi.org/10.1186/s13012-016-0482-7
Graves JM, Fulton-kehoe D, Jarvik JG, Franklin GM (2018) Impact of an advanced imaging utilization review program on downstream health care utilization and costs for low back pain. Med Care 56:520–528. https://doi.org/10.1097/MLR.0000000000000917
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix: search strategy
Appendix: search strategy
-
#1
((“Low Back pain”[mesh] OR “Diskectomy”[mesh] OR “Spinal diseases”[mesh] OR “back injuries”[mesh] OR “spinal fusion”[mesh] OR “sciatica”[mesh] OR “Sciatic Neuropathy”[mesh] OR backpain*[tiab] OR lumbar pain*[tiab] OR lumbar back pain*[tiab] OR lumbar backach*[tiab] OR lumbar spine pain*[tiab] OR lbp[tiab] OR sacral pain*[tiab] OR dorsalgia[tiab] OR backach*[tiab] OR back ach*[tiab] OR back pain*[tiab] OR radicular pain*[tiab] OR herniated dis*[tiab] OR slipped dis*[tiab] OR Lumbago*[tiab] OR back disorder*[tiab] OR back injur*[tiab] OR spinal fusion*[tiab] OR postlaminectomy*[tiab] OR post laminectomy*[tiab] OR arachnoiditis[tiab] OR failed back*[tiab] OR spondylit*[tiab] OR spondylosis[tiab] OR sciatic*[tiab] OR discitis[tiab] OR Radicular syndrom*[tiab] OR Radicular pain*[tiab] OR Spondylolisthes*[tiab] OR scoliosis[tiab] OR spinal stenosis[tiab] OR root stenosis[tiab] OR spine stenosis[tiab] OR degeneration dis*[tiab] OR degenerative dis*[tiab] OR displaced dis*[tiab] OR Disc problem*[tiab] OR disk problem*[tiab] OR back disab*[tiab] OR Piriformis Syndrome[tiab]) OR ((“pain”[mesh] OR “Pain Measurement”[Mesh] OR “Hernia”[mesh] OR pain[tiab] or ache*[tiab] OR aching*[tiab] OR Physical Suffering*[tiab] OR hernia*[tiab] OR Analges*[tiab] OR Nociception*[tiab]) AND (“Spine”[mesh] OR “back”[mesh] OR “spinal nerves”[mesh] OR “Intervertebral Disc”[mesh] OR spine*[tiab] OR spinal[tiab] OR Intervertebral Disk*[tiab] OR Lumbar Vertebra*[tiab] OR sacrum*[tiab] OR Cauda Equina*[tiab] OR facet joint*[tiab] OR coccyx[tiab] OR coccydynia[tiab] OR Ventral Root*[tiab] OR Dorsal Root*[tiab] OR anterior root*[tiab] OR posterior root*[tiab])))
-
#2
(“Magnetic Resonance Imaging”[mh] OR “magnetic resonance spectroscopy”[mh] OR magnetic resonance[tiab] OR NMR[tiab] OR MR[tiab] OR MRI[tiab] OR MRIs[tiab] OR mrs[tiab] OR MRSI[tiab] OR fMRI[tiab] OR fMRIs[tiab] OR fcmri[tiab] OR cmr[tiab] OR MRA[tiab] OR diffusion weighted[tiab] OR perfusion weighted[tiab] OR diffusion tensor[tiab] OR tractography[tiab] OR magnetization transfer*[tiab] OR zeugmatograph*[tiab] OR echo-planar[tiab] OR echoplanar[tiab] OR proton spin tomograph*[tiab] OR 1H-MR*[tiab] OR 1HMR*[tiab] OR H-MR*[tiab] OR HMR*[tiab] OR tesla[tiab] OR DWI[tiab] OR DTI[tiab] OR arterial spin labelling[tiab] OR arterial spin labeling[tiab] OR current density imag*[tiab] OR MP-RAGE[tiab] OR MPRAGE[tiab] OR turbo spin echo*[tiab] OR T1weighted[tiab] OR T2weighted[tiab] OR T1-weighted[tiab] OR T2-weighted[tiab] OR t2 star[tiab] OR t2-map*[tiab] OR t2-value*[tiab] OR t2-relax*[tiab] OR t1-map*[tiab] OR t1-value*[tiab] OR t1-relax*[tiab] OR dgemric[tiab] OR ASL[tiab] OR imaging[tiab] OR “Radiography”[Mesh] OR radiograph*[tiab] OR Roentgenograph*[tiab] OR Tomography[mesh] OR tomograph*[tiab] OR “Diagnostic Imaging”[Mesh:NoExp] OR “Diagnostic Imaging”[SH] OR “Tomography, X-Ray Computed”[Mesh] OR ct[tiab] OR cts[tiab] OR cat scan*[tiab] OR catscan*[tiab] OR x ray*[tiab] OR xray*[tiab] OR scan*[tiab] OR photograph*[tiab] OR photo[tiab] OR photos[tiab] OR radiolog*[tiab] OR ACR[tiab])
-
#3
(“costs and cost analysis”[mesh] OR “cost of illness”[mesh] OR “Health Care Costs”[Mesh] OR “Insurance”[Mesh] OR “Referral and Consultation”[Mesh] OR Budget control*[tiab] OR Budget saving*[tiab] OR Care budget*[tiab] OR care expen*[tiab] OR Care expen*[tiab] OR Care fund*[tiab] OR Care spend*[tiab] OR champus[tiab] OR Claim analysis[tiab] OR Claim review*[tiab] OR Claims Analysis[tiab] OR Claims Review*[tiab] OR Coinsurance*[tiab] OR Competitive Health Plan*[tiab] OR Competitive Medical Plan*[tiab] OR control cost*[tiab] OR Cost allocat*[tiab] OR Cost analy*[tiab] OR Cost apportionment*[tiab] OR Cost benefit*[tiab] OR Cost compar*[tiab] OR Cost contain*[tiab] OR Cost control*[tiab] OR Cost effective*[tiab] OR Cost Efficien*[tiab] OR Cost evaluat*[tiab] OR Cost increase*[tiab] OR Cost manag*[tiab] OR Cost minimi*[tiab] OR Cost reduc*[tiab] OR Cost reduction[tiab] OR Cost saving*[tiab] OR Cost sharing[tiab] OR Cost shifting*[tiab] OR Costeffect*[tiab] OR Cost minimisation[tiab] OR Cost minimization[tiab] OR Deductible*[tiab] OR direct cost*[tiab] OR Economic evaluat*[tiab] OR Health Benefit Plan*[tiab] OR Health budget*[tiab] OR health care cost*[tiab] OR Health care saving*[tiab] OR health care spending[tiab] OR health care system*[tiab] OR health cost*[tiab] OR health expen*[tiab] OR health expenditure*[tiab] OR Health fund*[tiab] OR Health spend*[tiab] OR health spending*[tiab] OR Healthcare budget*[tiab] OR Healthcare cost*[tiab] OR healthcare expen*[tiab] OR Healthcare fund*[tiab] OR Healthcare savings[tiab] OR Healthcare spend*[tiab] OR healthcare spending*[tiab] OR healthcare system*[tiab] OR High cost*[tiab] OR High spend*[tiab] OR Increasing cost*[tiab] OR insuran*[tiab] OR Low cost*[tiab] OR managed car*[tiab] OR Medical budget*[tiab] OR Medical Care Cost*[tiab] OR medical cost*[tiab] OR Medical expen*[tiab] OR Medical fund*[tiab] OR medical saving*[tiab] OR Medical saving*[tiab] OR Medical spend*[tiab] OR medicare[tiab] OR Preferred provider*[tiab] OR Reducing cost*[tiab] OR Reimburs*[tiab] OR Rising cost*[tiab] OR Saving cost*[tiab] OR societal cost*[tiab] OR Third-Party Pay*[tiab] OR Treatment Cost*[tiab] OR Usage reduction*[tiab] OR Value Based Purchas*[tiab] OR Worker Compensation*[tiab] OR Worker s compensation*[tiab] OR Workers compensation*[tiab])
-
#4
(“Health Services Misuse”[Mesh] OR appropriateness criteria[tiab] OR overus*[tiab] OR over us*[tiab] OR overutili*[tiab] OR over utili*[tiab] OR misuse*[tiab] OR mis use[tiab] OR Unnecessary Surgery[tiab] OR Unnecessary procedur*[tiab] OR Unnecessary treat*[tiab] OR Unnecessary medic*[tiab] OR Overdiagno*[tiab] OR Over diagno*[tiab] OR Overmedication*[tiab] OR Over medication*[tiab] OR Misdiagnosi*[tiab] OR Mis diagnosi*[tiab] OR Unwanted Medical Car*[tiab] OR Overtreat*[tiab] OR over treat*[tiab] OR inappropriate[tiab] OR Justif*[tiab])
-
#5
(“absenteeism”[mesh] OR “Sick leave”[mesh] OR “Return to work”[mesh] OR work absen*[tiab] OR work disabilit* OR absenteeism[tiab] OR sick leav*[tiab] OR sick day*[tiab] OR sickness absen*[tiab] OR disability leav*[tiab] OR Illness Day*[tiab] OR absenteeism[tiab] OR absentism[tiab] or return to work[tiab] OR returning to work[tiab] OR absence from work*[tiab] OR away from work[tiab] OR employee performance[tiab] OR job performance[tiab] OR lost work day*[tiab] OR lost work*[tiab] OR missed work*[tiab] OR missing work[tiab] OR presenteeism[tiab] OR work ability[tiab] OR work attend*[tiab] OR work day*[tiab] OR work impairment*[tiab] OR workday*[tiab] OR work performance*[tiab] OR work productivity*[tiab] OR work loss*[tiab])
-
#6
#3 OR #4 OR #5
-
#7
#1 AND #2 AND #6
-
#8
Routine diagnostic imaging[tiab] OR Unnecessary scan*[tiab] OR Unnecessary mri*[tiab] OR Unnecessary radiograph*[tiab] OR Unnecessary imag*[tiab] OR Unnecessary x ray* OR acr appropriateness criteria*[tiab] OR choosing wisely[tiab] OR Mri utiliz*[tiab] OR MRI use[tiab] OR MRI usage[tiab] OR CT utiliz*[tiab] OR CT use[tiab] OR CT usage[tiab] OR image utiliz*[tiab] OR image use[tiab] OR scan utiliz*[tiab] OR scan use[tiab] OR scan usage[tiab] OR x ray utiliz*[tiab] OR x ray use[tiab] OR x ray usage[tiab] OR radiography use[tiab] OR radiography utiliz*[tiab] OR Early mri*[tiab] OR early x ray*[tiab] OR early imag*[tiab] OR early radiograph*[tiab]
-
#9
#1 AND #8
-
#10
#7 OR #9
Rights and permissions
About this article
Cite this article
Lemmers, G.P.G., van Lankveld, W., Westert, G.P. et al. Imaging versus no imaging for low back pain: a systematic review, measuring costs, healthcare utilization and absence from work. Eur Spine J 28, 937–950 (2019). https://doi.org/10.1007/s00586-019-05918-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-05918-1