Abstract
Traumatic brain injury (TBI) is a chronic and debilitating disease, associated with a high risk of psychiatric and neurodegenerative diseases. Despite significant advancements in improving outcomes, the lack of effective treatments underscore the urgent need for innovative therapeutic strategies. The brain-gut axis has emerged as a crucial bidirectional pathway connecting the brain and the gastrointestinal (GI) system through an intricate network of neuronal, hormonal, and immunological pathways. Four main pathways are primarily implicated in this crosstalk, including the systemic immune system, autonomic and enteric nervous systems, neuroendocrine system, and microbiome. TBI induces profound changes in the gut, initiating an unrestrained vicious cycle that exacerbates brain injury through the brain-gut axis. Alterations in the gut include mucosal damage associated with the malabsorption of nutrients/electrolytes, disintegration of the intestinal barrier, increased infiltration of systemic immune cells, dysmotility, dysbiosis, enteroendocrine cell (EEC) dysfunction and disruption in the enteric nervous system (ENS) and autonomic nervous system (ANS). Collectively, these changes further contribute to brain neuroinflammation and neurodegeneration via the gut-brain axis. In this review article, we elucidate the roles of various anti-inflammatory pharmacotherapies capable of attenuating the dysregulated inflammatory response along the brain-gut axis in TBI. These agents include hormones such as serotonin, ghrelin, and progesterone, ANS regulators such as beta-blockers, lipid-lowering drugs like statins, and intestinal flora modulators such as probiotics and antibiotics. They attenuate neuroinflammation by targeting distinct inflammatory pathways in both the brain and the gut post-TBI. These therapeutic agents exhibit promising potential in mitigating inflammation along the brain-gut axis and enhancing neurocognitive outcomes for TBI patients.
Similar content being viewed by others
Background
TBI is a public health concern in the United States, with approximately 190 Americans dying each day from TBI-related injuries [1]. Despite its well established clinical course, the underlying mechanisms are yet to be fully elucidated [2]. TBI significantly increases the risk of morbidity and mortality, contributing to various neurodegenerative and psychiatric disorders, including Alzheimer’s, Parkinson’s, chronic traumatic encephalopathy, depression and epilepsy [3]. Recently, the gut has emerged as a crucial player in the pathogenesis of TBI, where TBI has been shown to induce detrimental changes along the GI tract. These changes ultimately worsen brain inflammation and cognitive outcomes via the gut-brain axis [4]. In this review, we will explore the mechanisms of brain-gut axis dysfunction post-TBI, with a specific focus on the role of various anti-inflammatory pharmacotherapies capable of breaking this dysregulated cycle between the brain and the gut.
Impact of TBI on brain neuroinflammation
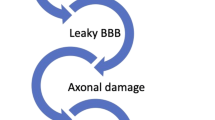
TBI is a form of acquired brain injury resulting from any external mechanical insult disrupting its structural integrity. TBI is primarily categorized into primary and secondary injuries. The irreversible primary injury results from blunt or penetrating trauma such as falls, motor vehicle accidents and gunshot wounds, followed by a secondary dysregulated inflammatory response that exacerbates tissue damage and neuronal injury [5]. TBI leads to a wide spectrum of consequences, ranging from immediate clinical deterioration to more severe cognitive outcomes. Clinical manifestations involve focal and diffuse brain swelling, vasospasm [6], hemodynamic perturbations (hypotension [7], hypoxia [8, 9]), metabolic derangements (hypoglycemia/hyperglycemia) [10], increased intracranial pressures (ICP) and coagulopathy disorders [11]. Moreover, TBI induces acute and chronic cognitive disorders, characterized by attention-deficits, memory problems and executive dysfunction [12]. At the cellular level, the rapid release of damage-associated molecular patterns (DAMPs) shortly after TBI initiates a dysregulated neuroinflammatory response. This involves the activation of resident brain cells (microglia, astrocytes, oligodendrocytes, neurons) and the recruitment of various immune cells into the injury site (monocytes, neutrophils, B and T-cells). DAMPs bind to “pattern recognition receptors”, such as nucleotide-binding oligomerization domain-like receptors and toll-like receptors, leading to an increase in inflammatory chemokines, cytokines and reactive oxygen species (ROS). This triggers a positive feedback loop that intensifies the inflammatory response by recruiting additional immune cells to the injury site [13, 14]. The hallmark features of TBI include neuronal injury, axonal damage, mitochondrial dysfunction, excitotoxicity, oxidative stress, and blood–brain-barrier (BBB) disruption [15, 16]. BBB breakdown occurs due to endothelial cell death, degradation of tight junction proteins, basement membrane damage, redistribution of aquaporin 4 (AQP4) channels, and swelling of astrocytic endfeet, leading to brain edema and increased ICP [17]. Excitotoxicity involves the heightened release of glutamate into the extracellular space, followed by the entry of calcium (Ca2+) into the cells, initiating a programmed cell death [18]. Additionally, the imbalance between increased metabolic demands and decreased mitochondrial adenosine triphosphate (ATP) production further aggravates the inflammatory response. Mitochondrial dysfunction results from a combination of increased ROS, Ca2+ overload and excitotoxicity, in addition to alterations in the expression of caspases, B-cell lymphoma 2 (Bcl-2) family proteins and apoptosis inducing factors [19]. TBI has also been shown to increase levels of polyunsaturated fatty acids within the brain, cerebrospinal fluid and serum in both preclinical and clinical models [20, 21]. These fatty acids activate the arachidonic acid metabolic pathways, leading to the release of prostaglandins and leukotrienes, further contributing to brain injury [22].
Astrocytes and microglia are key cells in the CNS that can initiate the inflammatory response post-TBI [13]. These cells have the ability to acquire proinflammatory or anti-inflammatory phenotypes and can secrete various chemokines, cytokines and growth factors [23, 24]. These changes influence the local tissue microenvironment and modulate secondary cellular damage or tissue repair [25]. Astrocytes undergo a process called reactive astrogliosis, which involves molecular, structural and functional changes [26]. They regulate the neuroinflammatory responses, scar formation, blood–brain barrier permeability and synapse remodeling [27]. At the same time, activated microglia can migrate toward the lesion site to phagocytose debris and modulate the inflammatory profile by secreting various cytokines and chemokines [28]. Microglia can have distinct roles in neurodegeneration and tissue repair depending on their activation state (pro/anti-inflammatory) [29]. Proinflammatory microglia favor the production of cytokines that exacerbate neural injury, while the anti-inflammatory microglia acquire a phagocytic role and promote repair by releasing neurotrophic factors [30, 31]. Recently, their role has expanded to show that changes in the gut microbiome after TBI can also alter microglial phenotypes in the brain and ultimately influence TBI outcomes [32]. The chronic activation of both astrocytes and microglia leads to increased peripheral immune cell infiltration through the permeable BBB, further exacerbating cognitive outcomes and increasing risk of morbidity and mortality [33].
Brain-gut axis disruption following TBI
TBI is a systemic disease that impacts various peripheral organs, including the lungs, GI tract, liver and kidneys [34,35,36,37]. TBI survivors have an increased risk of death from septicemia [38], pneumonia [39] and digestive diseases [40] compared to their healthy counterparts. Furthermore, TBI induces gastroparesis and intestinal dysmotility, resulting in feeding intolerance, where 50% of patients with severe TBI experience feeding intolerance within the first week after injury [41]. A single-center observational study conducted by McConnochie et al. demonstrated that around 52% of TBI patients often experience delayed bowel defecation, which was associated with longer intensive care unit (ICU) stays and higher gastric residual volumes [42]. A retrospective study also revealed that patients with TBI are 2.5 times more likely to die from digestive disease-related conditions and 12 times more likely to die from septicemia compared to the general population [43]. Another retrospective study demonstrated rates of fecal incontinence up to 70% in patients with acquired brain injury admitted to rehabilitation centers [44]. Fecal incontinence also significantly correlated with the presence of frontal lobe lesions and hemodynamic instability [45]. Furthermore, abdominal pain, distention and constipation were also common symptoms in patients even two years after their initial brain injury [46]. Therefore, current guidelines recommend initiating enteral nutrition within 24–48 h to attenuate TBI-induced intestinal dysfunction and improve patient prognosis [47]. Various distinct and overlapping pathways are also involved in TBI-induced intestinal dysfunction, including systemic immune dysregulation, ANS dysfunction, intestinal flora dysbiosis and neuroendocrine system disruption (Fig. 1).
Bidirectional cross-talk between the brain and gut in TBI. TBI induces tissue and cellular disruption, leading to the release of various inflammatory cytokines, chemokines, complement factors and damage-associated patterns (DAMPs), which promote diverse cellular responses: a Microglia, the resident immune cells of the brain, become activated and migrate towards the injury site to phagocytose debris and release proinflammatory cytokines. b Astrocytes contribute to the inflammatory response and undergo reactive gliosis, leading to the formation of a protective glial scar to limit injury spread. c Increased production of reactive oxygen species (ROS), excessive release of excitatory glutamate, and reduced blood flow to the brain promotes neuronal apoptosis and neurodegeneration. d Blood–brain barrier breakdown leads to the infiltration of various immune cells, such as neutrophils, monocytes and T-cells, into the brain parenchyma to aid in debris clearance. However, excessive infiltration can exacerbate tissue damage and worsen neurologic outcomes. I TBI affects the gut through several pathways, including the activation of the hypothalamic–pituitary–adrenal (HPA) axis, which releases cortisol, and sympathetic arm of the autonomic nervous system (ANS), which releases catecholamines, leading to gut intestinal barrier disintegration. e This allows the translocation of pathogenic bacteria from the gut lumen into the intestinal parenchyma, exacerbating microbial dysbiosis. f The enteric nervous system (ENS) becomes dysfunctional, with reactive gliosis in enteric glial cells, leading to dysmotility. g These changes also result in decreased expression of enteroendocrine cells (EECs), reducing their secretion of anti-inflammatory hormones such as serotonin. h Inflammatory immune cells, including T-cells and monocytes, infiltrate the intestinal epithelium and further increase gut inflammation. The gut sends signal back to the brain through various pathways: (II) Decreased release of microbial metabolites such as short-chain fatty acids (SCFAs) and bile acids, as well as reduced anti-inflammatory hormone secretion from EECs, worsen this detrimental cycle. Furthermore, the impairment of afferent and efferent vagus nerve pathways disrupts brain-gut homeostasis and exacerbate the neuroinflammatory response in the injured brain. These overlapping and interrelated pathways offer potential therapeutic targets for mitigating TBI-induced neuroinflammation and improving neurologic outcomes. Created with www.Biorender
Systemic immune dysregulation
TBI detrimentally affects the GI tract through systemic pathways by modulating the peripheral immune system [48]. TBI triggers the activation of the hypothalamic–pituitary–adrenal (HPA) axis and sympathetic nervous system, resulting in elevated levels of glucocorticoids/cortisol and catecholamines, respectively [49]. This surge in cortisol can ultimately lead to a leaky gut by increasing the intestinal barrier permeability [50, 51]. Subsequently, the translocation of luminal pathogenic bacteria across the disintegrated barrier can induce a systemic inflammatory response syndrome (SIRS) and further aggravate systemic inflammation by releasing numerous cytokines and chemokines into the systemic circulation [52]. TBI leads to an acute increase in proinflammatory mediators such as TNF-α, IL-1β and IL-6, which have been associated with worse cognitive outcomes [53]. Elevated levels of IL-1β were linked to impaired working memory in the acute phase, while increased levels of chemokine ligand 2 (CCL2) correlated with greater severity of post-concussive symptoms [54]. Further studies demonstrate that an increase in cytokine score load shortly after injury correlates with unfavorable Glasgow Coma Scale (GCS) scores at six and twelve months post-TBI [55]. Moreover, elevated blood cortisol levels can elevate the risk of infections by inducing peripheral immunosuppression [56]. TBI results in increased levels of circulating neutrophils and a decrease in circulating monocytes, T-cell lymphocytes and natural killer (NK) cells, accompanied by defective phagocytosis [57, 58]. This is characterized by impairments in respiratory burst and phagocytosis in neutrophils and monocytes, as well as decrease in percentage of perforin-positive NK cells [59, 60]. Additionally, TBI induces thymic involution, leading to chronic T-cell lymphopenia [59]. These alterations result in a shift in systemic immunity towards an anti-inflammatory state, which could explain the increased risk of nosocomial infections in hospitalized patients following TBI [61]. While these changes may be necessary to combat TBI effects acutely, the chronic stress response leads to a prolonged hyperinflammatory state that can trigger multi-organ dysfunction and, ultimately, lead to death [62, 63]. Interestingly, TBI has also been shown to increase age-related microglial phenotypes, as depicted by lipid accumulation in microglia for up to one year after injury [64]. All these acute, subacute and chronic changes in the neuroimmune responses exacerbate inflammation and accelerate immune aging and neurodegeneration [65].
To assess the impact of the systemic immune system on gut inflammation following TBI, our group have demonstrated that knocking out peripheral inflammatory C–C chemokine receptor type 2 (Ccr2)-dependent monocytes reduce levels of intestinal tumor necrosis factor alpha (TNF-α), interleukin-1β (IL-1β) and lipocalin-2. Additionally, TBI induces a significant increase in the expression of intestinal toll-like receptor 4 (TLR4) shortly after injury, which could explain aggravated intestinal inflammation. Notably, Ccr2ko mice showed decreased levels of intestinal TLR4 on days 1 and 3 post-injury [66]. These findings suggest a critical role for the systemic innate immune system in modulating the bidirectional communication between the brain and the gut post-TBI. In addition to the innate immune system, adaptive immunity, especially T-cells, has been shown to modulate the neuroinflammatory response along the brain-gut axis [67]. T-cells infiltrate the brain as early as 5 days post-TBI [68], and granzyme+ CD8+ T-cells have also been detected 8 months after TBI [69]. Daglas et al. demonstrated that pharmacologic and genetic depletion of CD8+ T-cells improves neurologic outcomes and produces a neuroprotective Th2/Th17 immunologic shift [69]. Recent studies have also shown that the gut microbiota modulate the trafficking of effector T-cells from the gut to the leptomeninges, impacting injury outcomes in both stroke and TBI models [70]. T-cell trafficking is thought to be modulated by changes in the microbiome following CNS injury, which ultimately regulates microglial functions in the brain [71]. Further research is warranted to understand the role of intestinal innate and adaptive immunity, particularly macrophages/monocytes and T-cells, in modulating neurocognitive outcomes post-TBI.
Autonomic and enteric nervous system dysfunction
In addition to the HPA-axis, the CNS exerts its effects on the gut through branches of the ANS. All divisions of the ANS innervate the GI tract, including the parasympathetic nervous system, sympathetic nervous system as well as the intrinsic ENS [72]. The bidirectional brain-gut axis serves as a conduit through which ANS exerts its influence on the ENS. TBI is associated with sympathetic hyperactivity, resulting in a surge of circulating catecholamine levels that significantly impact various peripheral organs, particularly the GI tract [73]. Increased catecholamine levels persist for weeks after injury and play a critical role in inducing systemic immunosuppression, exacerbating clinical outcomes, and increasing morbidity and mortality rates [74]. TBI induces a sympathetic storm of systemic epinephrine, which redirects blood away from the GI tract, resulting in gut dysmotility and gastroparesis [75]. Elevated catecholamine levels in the gut also disrupt ENS homeostasis, which is primarily cholinergic in nature [76]. A study by Ma et al. demonstrated ENS dysregulation four weeks post-TBI, depicted by an increased activation of enteric glial cells (EGCs) in the colon. This process, known as reactive gliosis, may further contribute to intestinal dysmotility [77]. As for the parasympathetic nervous system, the vagus nerve is the major regulator of bidirectional neuroimmune interactions between the brain and the gut [78]. The vagus nerve sends signals from the brain to the gut through postganglionic efferent neurons that regulate the secretomotor function of the gut by secreting Acetylcholine (Ach), thereby promoting gut motility [79]. Furthermore, Ach also binds to the α7 subtype of the nicotinic acetylcholine receptor (α7nAChR) located on intestinal macrophages and decreases the production of inflammatory cytokines [80]. Recent findings have also highlighted that extracellular choline acetyltransferase (ChAT), the rate limiting enzyme in Ach biosynthesis, reduces systemic inflammation and inhibits the release of proinflammatory cytokines. This effect was observed following vagus nerve stimulation or administration of a bioactive recombinant form of ChAT, as evidenced by reduced levels of serum proinflammatory markers TNF-α and IL-6 in a DSS colitis model in mice, two weeks post-injury [81]. In turn, the vagus nerve carries information from the gut to the brain through its afferent neurons which regulate brain neuroinflammatory outcomes. Visceral afferents respond to various mechanical and chemical stimuli [82], including changes in microbiome diversity [83], neuropeptides and hormones secreted by enteroendocrine cells (EECs) [84], as well as sensitization to inflammatory mediators. The importance of vagus nerve function is highlighted in vagus nerve stimulation (VNS) preclinical trials, which demonstrated improvements in cognitive outcomes following TBI when compared to placebo [85]. Therefore, dysautonomia plays a crucial role in mediating TBI outcomes post injury, and therapies should be targeted at attenuating the sympathetic storm with the potential use of beta-blockers. Additionally, there should be a greater focus on stimulating the parasympathetic vagus arm and studying its impact on immune cellular responses in the brain and gut, in addition to functional outcomes including intestinal permeability, gut motility and neurobehavioral outcomes.
Intestinal flora dysbiosis
The impact of the gut microbiota on behavioral outcomes and cognition is a rapidly expanding field of research, suggesting that alterations in the gut play a crucial role in the pathophysiology of TBI [86]. The impact of TBI on microbiome diversity and richness has been extensively studied in the preclinical [87, 88] and clinical settings [89, 90]. TBI leads to an increase in pathogenic bacteria and a decrease in protective populations [91]. These changes have been shown to manifest as early as 2 h post-TBI [92] and can persist for years [89] after the initial injury. Various factors could contribute to microbial dysbiosis, including changes in intestinal motility and alterations in paneth cells expression. Reduced gut peristalsis shifts microbial composition into a pathogenic state, and this in turn can worsen gut motility, triggering a detrimental cycle between dysmotility and dysbiosis [93]. Additionally, Paneth cells are another type of epithelial cells found the in the intestinal crypts that secrete various antimicrobial peptides, including lysozyme and α-defensins [94]. They have been also shown to regulate the composition of bacterial microbiome in various intestinal diseases such as inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS) [95]. In the setting of TBI, Yang et al. demonstrated a significant correlation between decreased expression of lysozyme antimicrobial peptides and increased translocation of pathogenic microbiome across the disintegrated epithelial barrier [96]. These changes suggest a critical role for paneth cells in modulating the microbiota-gut-brain axis following TBI.
The influence of gut microbiota on the brain is mediated mainly through vascular, neural and immune pathways. TBI results in mucosal damage and increased epithelial barrier permeability which facilitates the translocation of luminal pathogenic bacteria into the intestinal parenchyma [96]. The intestinal microbiota also transforms dietary components into various metabolites including short-chain fatty acids (SCFAs), tryptophan metabolites, and bile acid metabolites [97]. These microbial metabolites can either influence the brain directly by binding to receptors on vagal afferents, or indirectly by entering the systemic circulation and modulating cell–cell interactions between gut microbes and cells in the central nervous system (CNS), primarily astrocytes, microglia and neurons [98, 99]. In a study Xiong et al., it was demonstrated that administrating SCFAs such as butyrate and acetate for six months following TBI reduced microglial activation and promoted an anti-inflammatory microglial phenotype, while also attenuating T-cell activation and cytotoxic-related pathways [100]. Similarly, the administration of antibiotics, specifically amoxicillin-clavulanic acid, was linked to decreased infiltration of T-cells into the brain two days after TBI [70]. The interactions of various microbiome metabolites and brain immune cells such as microglia and T-cells, may ultimately impact cognition and neurobehavioral outcomes. Therefore, therapies targeted towards promoting a healthy microbiome are essential in ameliorating the hyperinflammatory response along the brain-gut axis and improving cognitive outcomes following TBI.
Neuroendocrine system disruption
Previous research focused on investigating brain-gut bidirectional communication following TBI, emphasizing the role of the HPA-axis, ANS, cellular immune responses and the microbiome axis. However, a thorough examination of the neuroendocrine axis is warranted, given the gut’s capacity to release a diverse array of hormones that can ultimately influence cognitive outcomes [101]. EECs are specialized cells lining the intestinal epithelium which form the largest endocrine system in the body. They play a pivotal role orchestrating the crosstalk between the brain and the gut by releasing various hormones and peptides including 90% of the body’s serotonin, ghrelin and glucagon-like peptide 1 (GLP-1), neuropeptide Y and cholecystokinin [101, 102]. EECs can also influence the brain directly through excitatory synaptic connections with the vagus nerve [103] and/or indirectly by releasing various hormones into the systemic circulation [104], thereby forming an interface between the brain and the gut. Our group was the first to show substantial reductions in the expression of EECs three days following TBI as demonstrated by a significant downregulation in the expression of chromogranin A (ChgA), which is the main marker of EECs (Fig. 2A–C). We have also shown reduction in the transcription factors implicated in the differentiation of Leucine-rich repeat-containing G-protein coupled receptor 5 (Lgr5+) intestinal stem cells into mature ChgA+ cells, including notch receptor 1 (Notch1), atonal bHLH transcription factor 1 (Atoh1), and neurogenin 3 (Neurog3) (Fig. 2D, E). The involvement of EECs in brain-gut communication has been also studied in various neurologic and psychiatric disorders such as Parkinson’s disease and schizophrenia [105, 106]. In Parkinson’s, EECs have been shown to express the α-synuclein misfolded proteins which directly connect to α-synuclein–containing nerves, forming a neural circuit between the gut and the nervous system [106]. More research is expected down the line to study the impact of EEC changes during acute and chronic timepoints post-TBI, alongside the various hormones they produce especially serotonin, ghrelin and GLP-1 which are primarily characterized as anti-inflammatory agents.
TBI induces enteroendocrine cell loss and decreases EEC differentiation. male C57BL/6 mice were used at the age of 4–6 weeks to induce moderate-severe TBI as previously described [66]. Mice were sacrificed three days later, and the ileum was harvested to investigate the expression of EECs. Intestinal tissues were fixed overnight with 4% paraformaldehyde and processed for paraffin embedding. Subsequently, 5-μm tissue sections were cut from paraffin blocks using a CUT 6062 microtome (SLEE Medical GmbH, D-55129 Mainz, Germany) and stained for DAPI (blue) and chromogranin A (ChgA) (green). ChgA+ cells were counted using ImageJ2 software. Scale bars, 50-μm. A–C Representative confocal images showing decreased intestinal ChgA expression in TBI mice when compared to sham on post-injury day (PID) 3. D An illustration of EEC differentiation pathway in the intestine. TBI reduces the expression of key transcription factors implicated in the differentiation of Lgr5+ intestinal stem cells into ChgA+ mature EECs, including E Notch1, F Atoh1, and G Nuerog3, as measured by quantitative reverse transcription polymerase chain reaction (qRT-PCR). The mRNA levels are expressed as relative to housekeeping gene Rplp0 expression. Statistical significance was determined by student’s t-test using GraphPad Prism 10 software. Each dot on the graph represents a different mouse. Error bars indicate the mean ± SEM. *p < 0.05, **p < 0.01, ***p < 0.001
In summary, the bidirectional communication between the brain and gut occurs through systemic immune pathways, neural networks, endocrine hormones, and the microbiota axis, thereby inducing detrimental changes along the GI tract post-TBI. These changes further exacerbate brain injury, as illustrated in Fig. 3. Strong evidence supports the role of diverse therapeutic agents in breaking this deleterious cycle and reducing inflammation through distinct mechanisms in the brain and the gut. In this comprehensive review, we highlight the anti-inflammatory role of various therapeutic modalities, including hormones such as (1) serotonin; (2) ghrelin; (3) progesterone; ANS modulators such as (4) beta-blockers; lipid-lowering agents such as (5) statins; and intestinal flora modulators such as (6) probiotics/antibiotics. We describe how these therapeutic interventions attenuate the hyperinflammatory response along the brain-gut axis following TBI.
TBI induces gut dysfunction via the brain-gut axis. This illustration depicts the intricate pathways through which TBI disrupts gut function via the brain-gut axis. Four main pathways contribute to the cross-talk between the brain and gut, including the systemic immune system, autonomic and enteric nervous systems, neuroendocrine system, and microbiota axis. In a healthy gut (left), (i) a balanced microbial flora transforms dietary components into various metabolites, including short-chain fatty acids (SCFAs), tryptophan metabolites, and bile acids. SCFAs, particularly acetate, propionate and butyrate exert various beneficial effects on brain function by acting as energy substrates for neurons and microglia. They have the ability to directly influence the brain by entering the systemic circulation and crossing the blood–brain-barrier or indirectly by binding to receptors on vagus nerve endings; (ii) Additionally, enteroendocrine cells (EECs), the largest endocrine system in the body, regulate digestive processes by secreting various hormones, such as like serotonin, ghrelin and glucagon-like peptide 1 (GLP-1), in response to luminal stimuli. These cells communicate bidirectionally with the CNS by sending hormonal signals to the brain via the blood stream or and neural signals through vagal afferent pathways; (iii) An intact vagus nerve also releases acetylcholine (Ach), which binds to the α7-subtype of the nicotinic acetylcholine receptor (α7nAChR) located on intestinal macrophages and decreases the production of inflammatory cytokines. Ach also binds to muscarinic receptors located on smooth muscle cells in the GI tract facilitating peristalsis and Ach also stimulate excitatory motor neurons in the ENS which further enhances gut motility; (iv) In normal homeostasis, immune cell activation is balanced, cortisol secretion follows diurnal rhythms and catecholamine levels remain within physiologic ranges, collectively maintaining a stable circulation and tissue perfusion. However, TBI-induced intestinal dysfunction triggers a cascade of changes (right). (I) The microbiome shifts towards a pathogenic state, with bacteria translocating into the intestinal parenchyma through the compromised intestinal barrier; (II) EECs become dysfunctional, reducing their expression, differentiation and secretion of anti-inflammatory hormones; (III) Concurrently, vagus nerve dysfunction occurs, resulting in decreased Ach, which can polarize macrophages into a proinflammatory state and heighten inflammation; and (IV) The activation of hypothalamic–pituitary–adrenal (HPA) axis during TBI increased circulating catecholamines and cortisol, leading to a leaky gut and mucosal damage. Furthermore, systemic monocytes and T-cells infiltrate the gut and exacerbate inflammation by upregulating proinflammatory cytokines. In addition, reactive gliosis in enteric glial cells (EGCs) results in intestinal dysmotility. Finally, Paneth cells reduce their secretion of antimicrobial peptides, further exacerbating microbiome dysbiosis. These intricate changes collectively aggravate brain inflammation and neurodegeneration through the gut-brain axis. Created with www.Biorender
Therapies attenuating brain-gut axis disruption following TBI
Serotonin
In the brain, serotonin is produced by neurons originating in the raphe nucleus located in the brainstem. Serotonin works as a neurotransmitter known for its role in regulating mood; however, it has also been shown to be involved in other processes such as neurogenesis and plasticity [107,108,109], cognition [110, 111], memory [112], inflammation [113], and gut motility [114, 115]. Serotonin and kynurenine, which are upregulated in inflammatory states, are both synthesized from tryptophan and compete for its availability. Most of the tryptophan in the body is used for the synthesis of kynurenine, and only a minority is used for serotonin. Tryptophan hydroxylase (TPH) is the rate-limiting enzyme of 5-HT (serotonin) synthesis and is present both in the CNS and the peripheral organs. Serotonin cannot cross the BBB, and as such, it is synthesized via TPH1 in the EEC of the gut, which are responsible for the synthesis of 90% of the serotonin in the body and via TPH2 in the CNS [107, 112, 113, 115]. There are a total of 14 known serotonin receptors that are divided into 7 classes, 5-HT1 to 5-HT7. The receptor that 5-HT activates, its location in the body, and the concentration it activates it with, determine the effect it exerts [107, 112, 113, 115].
Altered serotonin levels have been observed in TBI patients, which could be explained by alterations in tryptophan metabolism [109]. Zhang et al. showed that a rabbit subjected to controlled cortical impact had increased inflammation and upregulation of the enzyme responsible for kynurenine synthesis, shifting tryptophan away from serotonin synthesis. Although serotonin levels were not significantly decreased, there was a significant decrease in the serotonin/tryptophan ratio, with a decrease in the mean and total length of serotonin fibers compared to sham [109]. These alterations in 5-HT levels could contribute to brain dysfunction, as cognitive impairment was demonstrated to be mediated by 5-HT in the hippocampus in a tryptophan depletion clinical trial [112]. Considering such evidence, the role of serotonin in treating or altering the outcomes of TBI is under study [66, 116, 117]. Data about the efficacy of selective serotonin reuptake inhibitors (SSRIs) in treating TBI patients comes from preclinical models. Weaver et al. showed that mice subjected to severe controlled cortical impact, followed directly by a single injection of intraperitoneal (IP) fluoxetine (5 mg/kg), had decreased colonic permeability and improved motor coordination starting day 4 post-TBI compared to those treated with placebo [117]. Craine et al. studied the role of chronic IP milnacipran treatment (30 mg/kg/day), a serotonin-norepinephrine reuptake inhibitor (SNRI), in improving cognition in male rats subjected to frontal lobe injury. After TBI, rats treated with milnacipran performed significantly better in attentional set-shifting tasks compared to those treated with placebo, and their performance was comparable to that seen in sham rats [111]. In humans, a systematic review conducted by Yue et al. demonstrated that the administration of SSRIs was associated with improvements in depressive symptoms following TBI [118, 119]. In addition to TBI, many CNS disorders have been associated with altered levels of 5-HT. For example, patients with Alzheimer’s disease (AD) were found to have decreased total levels of 5-HT and 5-HT receptors [120,121,122], and a decrease in 5-HT along with an increase in kynurenine was associated with increased cognitive dysfunction and inflammation [123]. Similarly, in Parkinson’s patients, 5-HT depletion was associated with worse cognitive functioning [124,125,126]. In healthy individuals, acute serotonin depletion achieved through tryptophan depletion has been associated with impaired verbal memory and emotional processing [127, 128]. This evidence is further supported by the impact of SSRIs in alleviating some of these conditions. Preclinical studies showed that treatment with SSRIs decreased amyloid-beta plaques in female mice with AD, which was associated with improved cognitive function, learning and memory [129]. There is also evidence that longer treatment duration with SSRIs is protective against dementia [130, 131]. The mechanism of how serotonin can improve these conditions is not fully understood, as preclinical models show that agonism of different 5-HT receptors can result in either a positive or negative impact on memory and cognition [132, 133].
Since the gut is the main source of 5-HT in the body, it is not surprising the serotonin levels are altered in TBI patients. Mercado et al. show that male mouse models subjected to moderate TBI have a significant decrease in TPH1 in the duodenum and colon by 0.9-fold and 0.5-fold, respectively. Additionally, there was a reduction in serotonin expression in the colon on immunofluorescent staining accompanied by a significant increase in colonic serotonin reuptake transporters (Sert) compared to sham. This was reflected as an overall significant decrease in 5-HT level in the peripheral circulation [116]. Furthermore, our group was the first to demonstrate a significant downregulation in the expression of EECs along the intestinal epithelium, particularly the ileum, following severe unilateral TBI in male mice. This results in decreased levels of serotonin synthesis genes, especially dopa decarboxylase, another essential enzyme responsible for serotonin synthesis [66]. The long-term gut dysbiosis that occurs because of inflammation and impaired motility in TBI is another factor that explains the changes in 5-HT levels [4, 134]. Studies involving alterations in gut microbiota whether in induced or in disease states such as IBS have been correlated with changes in 5-HT levels and in behavior [135,136,137]. Similarly, people who suffer from schizophrenia [138] or depression [139] harbor pathogenic microbiota and reduced 5-HT levels [140, 141] than controls highlighting the bidirectional interaction.
In the GI system, serotonin has been shown to play a role in regulating motility through 5-HT3 and 5-HT4, and peristalsis through its action on 5-HT2B on the interstitial cells of Cajal (ICC), which are the cells responsible for initiating rhythmic contraction [112,113,114,115]. In addition to TBI and other neurological diseases, alterations in 5-HT levels have been extensively described in intestinal diseases such as IBDs [142, 143], celiac disease [144, 145], colitis [146], and diverticulitis [147]. Serotonin has been shown to improve esophageal motility in cases of dysfunction [148], increase stool frequency and improve its consistency in patients with inflammatory bowel syndrome associated with constipation [149]. Interestingly, chronic treatment with SSRIs has been associated with decreased gut motility and delayed transit both in mouse and human studies [150, 151], highlighting the complexity of serotonin signaling. 5-HT has been also shown to regulate inflammation in the gut by exerting both pro-inflammatory and anti-inflammatory effects through various receptors found on immune cells [152]. Given that intestinal epithelial cells express the serotonin reuptake transporter (Sert) on their apical membranes [153] and considering that TBI increases the expression of these receptors in the intestinal epithelium of colonic villi [116], administering SSRIs such as fluoxetine presents a promising avenue to explore the impact of intestinal serotonin on gut-brain axis interactions and neurobehavioral outcomes following TBI.
Ghrelin
First characterized in 1999, ghrelin is an orexigenic peptide hormone mainly produced by P/D1 cells in the stomach with small amounts also released by the small intestine, pancreas and brain. Ghrelin is well known for its effects on pituitary regulation, hunger, and satiety [154,155,156]. More recently, its anti-inflammatory properties have become better understood [157, 158]. Investigation into the role of exogenous ghrelin in models of brain injury has uncovered several mechanisms through which ghrelin can simultaneously ameliorate GI dysfunction and exert various neuroprotective effects. The neuroprotective effects of ghrelin have been linked to BBB preservation, reduction in oxidative damage, as well as other neuroprotective mechanisms. In a weight drop (WD) model of TBI, IP administration of ghrelin (20 μg total) in male mice was found to reduce neuronal degeneration and decrease vascular permeability and perivascular expression of AQP-4 [159]. Increased AQP-4 has been shown to be linked to cellular edema following TBI [160] which contributes to TBI-induced neuronal damage. In this study, S100B -a neurobiochemical marker of brain damage- was also found to be reduced in the serum of mice that receive ghrelin alongside TBI [159, 161], adding evidence that ghrelin prevents neuronal damage and apoptosis following trauma through preservation of the BBB. The protective role of ghrelin in TBI was linked to fibroblast growth factor (FGF) where a study by Shao et al. found that both FGF-binding protein (FGF-BP) and basic FGF (bFGF) were downregulated in the ipsilateral hemisphere following treatment with IV ghrelin (20 μg/kg) in a TBI rat model. The group proposed that ghrelin attenuates brain injury by competitively inhibiting bFGF/FGF-BP-induced neovascularization. However, it remains to be investigated whether this discovered relationship between ghrelin and both bFGF and FGF-BP is causative or competitive [162]. An alternative mechanism has been identified in relation to ghrelin's protective role against brain injury during sepsis. Sun et al. found that PI3K/Akt signaling activation mediates ghrelin’s ability to attenuate brain edema, neuronal apoptosis and enhanced BBB integrity [163]. Phosphoinositide 3-kinases (PI3K) activation results in the production of phosphatidylinositol 3,4,5 trisphosphate (PIP3) and phosphatidylinositol 3,4 bisphosphate (PIP2), leading to the activation of Protein kinase B (Pkb/Akt). Akt promotes cell survival by phosphorylating both glycogen synthase kinase 3beta (GSK-3beta) and the Bcl-2 family [164, 165]. These two molecules are tied closely to neuronal survival, highlighting a potential mechanism through which ghrelin exerts its neuroprotective effects during sepsis. Lastly, ghrelin has been shown to be exhibit neuroprotective properties in cerebral models of ischemia–reperfusion injury (IRI) [166]. When compared to IRI controls, treatment with un-acylated ghrelin in rat and mice models of cerebral IRI resulted in decreased injury, apoptosis, inflammation and BBB disruption through the reduction of oxidative damage [167, 168]. Ghrelin has also been found to reduce neutrophil infiltration following spinal cord injury (SCI), resulting in less lipid peroxidation and DNA damage following the insult [169, 170]. However, despite these potential protective roles, investigation into ghrelin has not yielded universally positive findings. For example, Ersahin et al. found that IP ghrelin (10 μg/kg/day) did not reduce neurological deterioration following SCI in rats [169]. This divergence in available data emphasizes the need for further investigation into the potential role of ghrelin as a protective agent that acts on and through the brain-gut axis.
Ghrelin’s ability to reduce GI dysfunction following CNS injury has been attributed to several mechanisms, including a link with the vagus nerve, preservation of the intestinal barrier, and activation of the mammalian target of rapamycin (mTOR) pathway following ischemic injury. Evidence supports the role of ghrelin in mediating protective responses of the gut-brain axis following TBI. Bansal et al. showed that the administration of 2 doses of IP ghrelin (20 μg/kg total) right before and after severe WD TBI preserved intestinal barrier integrity, restored villous architecture and reduced ileal levels of TNF-α [171].They also demonstrated that the beneficial effects of vagus nerve stimulation (VNS) following TBI may be mediated through ghrelin [172, 173]. VNS was shown to both increase serum ghrelin levels and decrease serum inflammatory cytokines following TBI. Exogenous ghrelin was found to mimic the response seen to VNS by decreasing circulating TNF-α. Importantly, the protective effects of VNS were abolished when a ghrelin receptor antagonist was administered alongside VNS, highlighting a potential ghrelin-dependent mechanism through which VNS works during TBI. The localization of ghrelin receptors to the dorsal motor nucleus of the vagus in the brain supports this link [174]. Furthermore, the administration of 1 dose of intravenous ghrelin (20 μg/kg) 30 min following severe TBI in male rats improved intestinal motility and preserved ileal mucosal architecture [175]. Aside from its important and well-established anti-inflammatory role, ghrelin has been shown to attenuate intestinal barrier dysfunction following intracerebral hemorrhage (ICH) in mice [176]. In a male mouse model of ICH, 2 doses of IP ghrelin (20 μg total) markedly reduced ileal mucosal injury at both histological and ultrastructural levels. Ghrelin also reduced the increase in intestinal permeability commonly seen following ICH by upregulating intestinal tight junction-related proteins Zonula occludens-1 (ZO-1) and claudin-5 [176]. The activation of the mTOR has also been implicated in the gastro-protective mechanisms of ghrelin. Zhang et al. found that ghrelin increased the phosphorylation of mTOR following superior mesenteric artery (SMA) occlusion [177]. This finding did not occur when the specific ghrelin antagonist, growth hormone-releasing peptide 6, was co-administered. Ghrelin’s ability to activate mTOR was ultimately correlated with findings of attenuated organ injury and increased survival in mice that received ghrelin treatment alongside SMA occlusion [177]. There are several mechanisms through which ghrelin can ameliorate both brain and gut injury following an insult. The lack of a consistent mechanism throughout the highlighted papers supports the hypothesis that ghrelin’s pleiotropy contributes to its beneficial impact.
Progesterone
Progesterone is a steroid hormone primarily produced by the gonads and the adrenal cortex that regulates uterine function and female reproduction [178]. However, research suggests that progesterone plays a role beyond the female reproductive tract, including the CNS, where it is secreted by neurons and glial cells. Its effects include promoting neurogenesis and myelination and improving learning and memory [179]. The role of progesterone has been extensively described in multiple CNS diseases including TBI, Parkinson’s disease and AD, where it has been labeled as neuroprotective due to its anti-inflammatory properties [180]. The therapeutic benefits of progesterone were explored in TBI [181], stroke [182] and neurodegenerative diseases’ animal models [183], where progesterone receptors are expressed in various CNS cells such as neurons, astrocytes and oligodendrocytes, in addition to Schwann cells in the peripheral nervous system [184]. Studies have shown that early administration of progesterone post-TBI reduces the expression of proinflammatory cytokines [185], repairs BBB [186], promotes myelin and axonal regeneration [187], attenuates oxidative damage of mitochondria [188], and improves cognitive and motor outcomes [189]. Progesterone also stimulates synaptogenesis and neurogenesis by increasing the expression of nerve growth factor and brain-derived neurotrophic factor (BDNF) [190].
Guo et al. demonstrated that subcutaneous (SQ) administration of progesterone (16 mg/kg) decreased brain edema 3 days following TBI in male rats by increasing the expression of AQP4 water channels near the lesion site [186]. Other studies also revealed that progesterone attenuates the neuroinflammatory response following TBI by lowering the activation of the transcription factor NF-κB and the expression of the proinflammatory cytokines TNF-α and IL-1β [185, 191]. Ultimately, this leads to a reduction in the activation of cFos, a transcription factor known to promote apoptosis and inflammation [192, 193]. Consistent with these results, Yao et al. demonstrated that progesterone administration following moderate lateral fluid percussion injury (FPI) in male rats decreased the proapoptotic genes Bad and Bax’s expression and increased the anti-apoptotic gene Bcl-2 [194]. Furthermore, progesterone increases circulating endothelial progenitor cells (CD31 and CD34) which facilitates neural regeneration and vascular remodeling, leading to improved cognitive outcomes [187]. An alternative mechanism by which progesterone exerts its therapeutic effects involves the activation of complement decay-accelerating factor (CD55), a potent inhibitor of the neuroinflammatory cascade [195].
One systematic review found that progesterone administration immediately after experimental brain injury reduced the lesion volume [196], but a more recent systematic review showed that it did not reduce mortality or adverse outcomes after TBI [197]. Due to the promising results of numerous preclinical studies, researchers conducted phase II clinical trials to study the efficacy of progesterone in human subjects following acute TBI. In the first phase II trial in Atlanta, GA named ProTECT, progesterone was shown to decrease mortality on post-injury day 30 [198]. Afterward, a more extended clinical trial was conducted in Hangzhou, China, which demonstrated improved functional outcomes and recovery at 3 months post-injury [199]. Ultimately, two phase III clinical trials (ProTECT III and SyNAPSe) failed to confirm the previous promising pro-regenerative results. Nonetheless, research critics attributed its failure to the reliance on subjective measures and the lack of objective measures to accurately evaluate the outcomes. Issues with medication dosage and the tendency to overvalue false positive results in preclinical trials were also identified [200]. However, a notable oversight in launching the trials was the failure to understand how progesterone affects gut motility [201] and the subsequent temporal changes in the gut’s immune profile [66, 202], which could potentially influence neurological outcomes. Even though Phase III clinical trials were disappointing, progesterone may still be regarded as a crucial targeted pharmacological therapy, especially in the absence of any FDA-approved drug for treating TBIs.
Progesterone’s neuroprotective quality has led researchers to study its role in TBI-related intestinal dysfunction. Chen et al. showed that SQ progesterone (16 mg/kg) administration for 5 days helped preserve ileal mucosal integrity and decrease inflammation following TBI by lowering the proinflammatory cytokines IL-1β and TNF-α, as well as reducing cellular apoptosis [203]. Then, they also discovered that progesterone decreased the activation of transcription factor NF-κB, which was thought to be responsible for its therapeutic effects [204]. Subsequent investigations revealed that the antioxidant transcription factor nuclear factor erythroid 2-related factor 2 (Nrf2) also alleviates intestinal inflammation following TBI by decreasing the activation of NF-κB [205], leading to the possibility that progesterone decreases NF-κB activation by modulating the Nrf2 pathway. In addition, Jin et al. observed an elevation in intestinal permeability following TBI in Nrf2-deficient mice, which consequently led to increased levels of plasma endotoxins. This, in turn, resulted in decreased levels of antioxidant and detoxifying enzymes [206]. Furthermore, it is worth mentioning that Nrf2-deficient mice exhibited increased levels of intercellular adhesion molecule-1 (ICAM-1) expression, while progesterone therapy successfully decreased ICAM-1 expression following TBI [204, 205]. These studies demonstrate the restorative synergistic effects of progesterone and the Nrf2 pathway in preserving mucosal integrity. More studies are necessary to fully elucidate the precise mechanisms underlying the effects of progesterone on the Nrf2 pathway via progesterone receptors. Later, Zhou et al. conducted in vitro experiments which demonstrated that progesterone effectively reduced gut permeability by upregulating the expression of the tight junction occludin [207]. In addition, gut dysfunction is observed in brain disorders like subarachnoid hemorrhage (SAH) and Parkinson’s disease, and the use of progesterone has been shown to alleviate intestinal inflammation, suggesting its protective role in brain-gut axis dysfunction. In a male rat model of SAH, IP administration of progesterone (16 mg/kg) for 5 days reduced the expression of proinflammatory cytokines IL-1β, TNF-α and IL-6 and restored mucosal integrity in the ileum [208]. In a mouse model of Parkinson’s disease, the use of progesterone also demonstrated anti-inflammatory effects in the ileal tissues [209]. In conclusion, these studies demonstrate the synergistic role of progesterone in mitigating brain and intestinal inflammation following TBI.
ANS modulators
Beta-blockers
Catecholamines, namely norepinephrine (NE), exert their effects through the activation of beta-receptors: beta1-3 and alpha-receptors: alpha1-2 [210, 211]. Beta1-3 receptors are found in various organs in the body, where they lead to increased cardiac contractility, increased heart rate, vasodilation, and bronchodilation. They also play a role in regulating lipolysis in white adipose tissue, thermogenesis in brown adipose tissue and mobilization of hematopoietic progenitor cells [212]. It has been shown that TBI patients experience sympathetic hyperactivity, causing a catecholamine surge [213,214,215,216,217,218]. This surge causes secondary insults, which manifest as posttraumatic hyperthermia [216, 218], increased inflammation and leukocyte migration [219, 220], impaired cerebral homeostasis and perfusion [217], and cardiovascular dysfunction [216], and has been associated with increased mortality [221]. In light of such evidence, the use of beta-blockers to alleviate secondary damage caused by TBI gained interest. Beta-blockers can be selective to one type of receptor, such as metoprolol (beta-1 receptor blocker), or act non-selectively on all beta-receptors, such as propranolol. Some, like labetalol (beta-1 and 2 receptor blocker), can also act on alpha-1 receptors, thereby altering the expected outcome [212].
A study by Lopez et al. subjected male mice to severe TBI via controlled cortical impact and tested the effects of treating them with the non-selective beta-blocker propranolol for two [219] and fourteen days [220]. Propranolol treatment led to decreased penumbral leukocyte migration in a dose-dependent manner and improved weight recovery at both timelines and decreased cerebral edema and albumin leakage at two days. Other preclinical trials revealed decreased p-tau accumulation [222], improved cerebral oxygenation and perfusion [212], restoration of cerebral autoregulation [217], decreased hippocampal necrosis [217], higher neurologic scores [212, 219] and improved behavioral [222], cognitive and memory [223] performances with beta-blocker treatment. Beta-blockers are hypothesized to act by (a) providing a neuroprotective environment by increasing protective proteins, such as heat shock protein 70 (HSP-70) and downregulating ubiquitin carboxyl-terminal hydrolase L1 (UCHL-1), which is involved in oxidative damage [223]; (b) decreasing calcium entry into the cell, which decreases apoptosis [223]; (c) modulating microglial function and synaptic plasticity [224]; and (d) inhibiting pro-inflammatory IL-6 signaling [217].
The success seen with beta-blocker treatment in preclinical trials translated well into clinical studies. Observational studies showed a significant decrease in mortality in TBI patients treated with beta-blockers, particularly propranolol, compared to those administered placebo [225] and better long-term neurologic functioning [215]. Results were associated with increased length of hospital stay with inconsistent results on length of ICU stay [214, 216, 225]. The adverse effects of using beta-blockers included a longer time on the ventilator and increased infection rates [214, 216]; however, both beta-blocker and placebo groups experienced similar rates of cardiopulmonary adverse events such as hypotension, bradycardia, heart blocks, arrest, and bronchospasms [215]. Asmar et al. demonstrated that beta-blockers, particularly propranolol, play a role in alleviating the dysregulation in body temperature after TBI by significantly decreasing the number of hyperthermic episodes, lowering the median temperature, and spacing out the episodes. The results were more pronounced in patients with severe head injury, and these patients further showed decreased lengths of ICU stay and higher Glasgow Coma Scale scores at discharge [218]. In a prospective randomized controlled trial, Khalili et al. showed that treating patients with severe isolated TBI with propranolol resulted in decreased mortality and improved functional outcomes at 6 months compared to placebo (Level II evidence) [226]. The Eastern Association for the Surgery of Trauma (EAST) recommends the use of beta-blockers in adult TBI patients with no contraindications and only in an ICU setting where cardiovascular side effects, primarily hypotension, and bradycardia, can be monitored and treated promptly [213].
Evidence shows that TBI is associated with increased intestinal permeability, which correlates with increased mortality, that is significantly reduced with beta-blocker treatment [221, 227]. Lang et al. also showed that male rats subjected to TBI had increased epinephrine levels, higher intestinal TNF-a levels, decreased ZO-1 protein expression, which forms tight junction in the intestine, and worse mucosal damage on ileum histopathology compared to sham rats. All these changes were reversed significantly when the rats were treated with 1 dose of IP labetalol (beta-1 and 2 receptor blocker) right after TBI [227]. Gut dysfunction seen in TBI can also induce changes in the brain via NE signaling that can further exacerbate gut dysfunction as NE plays a bidirectional role in the brain-gut axis. For instance, rat models show that gastric distension induces a signification increase in NE in the ventral bed nucleus of the stria terminalis (vBNST), which is known to be involved in response to stress. In turn agonism of beta-receptors in the vBNST leads to a significant decrease in gastric emptying and small intestinal transit, which is reversed with the administration of beta-blockers [228].
Alpha-agonists/antagonists
In the setting of the brain-gut axis, alpha-adrenergic receptor modulation remains relatively unstudied. Despite the lack of bi-directional data on the therapeutic action of alpha receptor modulators, their action on the brain following TBI is of significant interest in both translational and clinical research settings [229, 230]. In male rats, the alpha-2 adrenergic agonist mafedine promotes the restoration of interhemispheric connectivity in remote brain regions and intrahemispheric connection within the unaffected hemisphere post-TBI day 7 [231]. The authors also found that mafedine improved cortical response to photic and somatosensory stimulation [231]. Alongside alpha-2 agonists, the role of alpha-1 antagonists is also being actively explored in the setting of TBI. Kobori et al. have shown that IP administration of the alpha-1 antagonist (2-[b-(4-Hydroxyphenyl)ethyl]aminomethyl-1-tetralone hydrochloride (HEAT)) (0.1 mg/kg) improved working memory in male Sprague Dawley rats post-TBI day 14 [232]. Such studies suggest that modulation of alpha adrenoceptors and, by extension, norepinephrine signaling may benefit TBI patients. These findings add to existing clinical data from the COMA-TBI study showing that elevated catecholamines are associated with unfavorable outcomes following isolated moderate to severe TBI [73, 233]. Importantly the COMA-TBI study highlights the differences in the predictive use of both epinephrine (Epi) and norepinephrine (NE), with admission levels Epi associated with higher rates of unfavorable outcomes and mortality and changes in NE associated with higher mortality risks. The differences in the predictive value of each of these catecholamines may well be due to their affinities for adrenoceptor sub-types.
In the clinical setting, the role of alpha-2 agonists has been investigated extensively in the setting of severe TBI with the hopes that these agents may attenuate sympathetic hyperactivity following brain injury [234]. Clonidine (alpha-2 agonist), in combination with propranolol, has been studied in patients with severe TBI as it reduces levels of circulating catecholamines and decreases levels of cerebral vasoconstriction without altering cerebral blood flow [235]. To date, several studies, including the “DASH After TBI Study” [236] and the Nordness et al. [237] pilot study have found that while adrenergic blockade with propranolol and clonidine is safe and feasible, the drugs do not alter ventilator-free day numbers in patients with severe TBI.
Statins
Since their discovery in the early 1970s, statins have become the mainstay treatment for patients with high cholesterol levels [238]. As research advanced, the use of statins expanded due to their anti-inflammatory properties where they have been shown to be effective in the management of coronary artery disease [239], arthritis [240], brain injuries [241] and intestinal inflammation [242]. The protective role of statins in the CNS following brain injuries has been widely described [243,244,245]. Statins have been shown to attenuate neurodegeneration by decreasing neuronal death, apoptosis, microglial activation and astrogliosis [246]. Statins also promote neurogenesis, synaptogenesis and angiogenesis in the brain, particularly in the boundary zone of the lesion and the hippocampus [247]. Studies have shown that statin use after TBI is associated with decreased risk of death and improved function and capacity at 12 months post-injury [248]. In a randomized double-blind clinical trial, statins improved functional recovery at 3 months post injury, although they had no effect on brain contusion volume [249]. Rat animal models also showed enhanced spatial memory function with atorvastatin treatment following TBI [250, 251]. A systematic review by Sultan et al. suggested that statins display a neuroprotective role, particularly in improving cognitive outcomes and reducing the risk of dementia [243]. Statins were also shown to reduce beta-amyloid peptide levels post TBI, which may play a role in the improvement in cognitive outcomes and decreasing the risk of AD in TBI patients [252].
The anti-inflammatory effects of statins are numerous, such as reduction in the expression of proinflammatory markers TNFα and IL-1β, as well as a decrease in the activation of microglia and astrocytes, as evidenced by a decrease in the expression of cluster of differentiation 68 (CD68) and glial fibrillary acidic protein (GFAP), respectively [253, 254]. Statins reduce astrogliosis by modulating caveolin-1 expression and epidermal growth factor receptor in astrocyte lipid rafts [255]. Statins also upregulate the expression of vascular endothelial growth factor (VEGF) and BDNF in the dentate gyrus of the hippocampus through Akt-dependent signaling pathways, upregulating the expression of GSK-3beta and cAMP response element-binding proteins, ultimately increasing cellular proliferation and enhancing neurogenesis [256]. In addition, daily oral simvastatin administration (1 mg/kg/day) reduces neuronal apoptosis following TBI in male rats through increased Akt phosphorylation and activation of its downstream targets, such as Forkhead transcription factor 1, inhibitory-kappaB, and endothelial nitric oxide synthase, while attenuating the activation of caspase-3. All these effects lead to improved neuronal survival and function [257]. Furthermore, statins decrease brain edema following injury by reducing BBB permeability due to a decrease in ICAM-1 and neutrophil infiltration [258]. Taken together, these findings suggest that statins play a beneficial role in attenuating the neuroinflammatory response post-TBI and improving outcomes.
The protective role of statins along the brain-gut axis is emerging. First, it is significant to note that cluster of differentiation 40 (CD40), a transmembrane receptor of the tumor necrosis factor receptor family, is strongly implicated in intestinal inflammation in various diseases such as TBI, IRI and IBD [259]. In a rat model of TBI, Hu et al. demonstrated that the expression of CD40 increases in the jejunum which is positively correlated with an increase in the activity of NF-κB and levels of TNF-α, vascular cell adhesion molecule-1 (VCAM-1) and ICAM-1 [260]. Ultimately, studies revealed that one dose of IP (30 mg/kg) rosuvastatin right after TBI attenuated jejunal injury by reducing the expression of TNF-α and IL-1β and blocking the CD40/NF-κB pathway. Statins also alleviated TBI-induced intestinal morphometric alterations by preserving normal mucosal architecture and maintaining villous integrity [261]. Furthermore, in vivo (experimental murine colitis model) and in vitro (intestinal epithelial cells) studies both reconfirmed the anti-inflammatory properties of statins by blocking the activity of NF-κB, inhibiting the phosphorylation of IκB and eventually lowering the expression of TNF-α [262]. Statins have also been shown to decrease CD40 expression in human vascular cells [263]. In addition, Ozacmac et al. revealed that daily PO atorvastatin (10 mg/kg) 3 days before IRI promoted gut motility and ileal contractility possibly due to a decrease in oxidative stress, neutrophil accumulation and tissue malondialdehyde expression, as well as an increase in reduced glutathione levels [264]. An alternative mechanism in which statins exert their protective effects in the gut is by modulating the gut microbiome. A growing body of evidence suggests that TBI alters the composition of the gut microbiome and promotes pathogenic bacteria over commensal bacteria mainly due to intestinal dysmotility and increased paracellular permeability, therefore, aggravating disease progression [4]. In turn, the vagus nerve can reciprocally affect the CNS by sensing the microbial products through its afferent fibers [99]. This leads to a deleterious cycle between the injured brain and the dysbiotic gut. One possible way to halt this inflammatory cycle is through the use of statin therapy. Statins have been shown to promote healthy gut flora and ameliorate gut dysbiosis [265]. Studies have also shown that statins demonstrate anti-inflammatory effects in IBD and are linked to a decreased requirement of steroids [242, 266]. The potential use of these drugs is promising and interesting. More studies are encouraged to better elucidate how statin therapy regulates the brain-gut axis in the context of TBI.
Microbiome modulators
Antibiotics
Recent investigations indicate that gut microbial dysbiosis impacts intestinal function not only in diseases like IBS and IBD but also in neurologic conditions such as TBI and strokes [267, 268]. TBI promotes the presence of pathogenic bacteria over commensal bacteria, leading to heightened intestinal inflammation, increased barrier permeability and dysmotility [93, 268]. To gain a better understanding of alterations in the microbiome and their implications on brain inflammation after TBI, studies have utilized various antibiotic combinations to deplete the microbiome, in addition to the administration of beneficial probiotic strains to promote a healthy intestinal flora. Many animal studies initially utilized germ-free (GF) mice to elucidate relation between microbial dysbiosis and the host’s physiologic response [71, 269]. A study by Simon et al. demonstrated that administering a combination of antibiotics (1 g/L of ampicillin, metronidazole, neomycin and vancomycin) two weeks before TBI in male mice improved intestinal barrier permeability, as evidenced by increased ZO-1 staining along the cecum epithelium. This resulted in decreased microglial activation, increased hippocampal neuronal density, reduced lesion volume, and improved learning outcomes [269]. Conversely, another study by Celorrio et al., using the same antibiotic regimen for two weeks before injury, showed worsened neuronal loss in the hippocampus, triggering a more pronounced fear response in adult male mice [202]. The opposing outcomes may be attributed to various factors, including differences in mice intestinal flora in distinct animal facilities, variations in diet impacting the host microbiome, and differences in injury severity and time points of behavioral analysis [270, 271]. Celorrio et al.’s study also revealed the intricate interplay between the gut microbiome and the immune system. Antibiotic administration for 1 week after TBI reduced the infiltration of peripheral monocytes and T-lymphocytes into the brain while increasing microglial inflammatory markers 3 days after injury. The heightened expression of proinflammatory surface markers (TLR4 and MHCII) by microglia, along with alterations in their morphology toward an amoeboid shape, correlated with decreased neurogenesis in the dentate gyrus and increased neuronal degeneration in the CA3 region of the hippocampus [71, 202]. Benakis et al. also demonstrated that alterations in the intestinal flora of male mice induced by a two-week course of amoxicillin-clavulanic acid (1 g/L) resulted in reduced ischemic brain injury. This reduction was attributed to an increase in intestinal regulatory T-cells and a decrease in the infiltration of IL-17 + γδ T cells into the brain, observed 16 h post-injury [70]. Targeting the gut-microbiota-immune axis offers a promising approach to improve recovery following TBI.
Probiotics
In an effort to better understand microbiome changes, the administration of probiotics has been widely experimented in TBI models. Probiotics regulate microbial populations in the gut lumen by favoring the colonization of beneficial bacteria and reducing pathogenic populations [272]. They enhance epithelial cell differentiation and proliferation and maintains epithelial barrier integrity, thereby limiting the translocation of harmful bacteria into the intestinal parenchyma [273]. A study by Ma et al. showed that the supplementation of probiotics, specifically LA for 7 days after weight-drop TBI, has protective effects on the ileum after TBI. This was revealed by improvements in intestinal barrier function and the gut’s absorptive capacity for nutrients and electrolytes [274, 275]. The effects of LA also included improvements in ileal villous architecture and enhanced ileal motility through the restoration of the gut’s pacemaker cells, known as the interstitial cells of Cajal (ICC), by increasing levels of myosin light chain kinase protein and promoting smooth muscle contraction [276]. Lactobacillus reuteri was also utilized in clinical trials involving military veterans with mild TBI. Results demonstrated significant reductions in serum inflammatory C-reactive protein levels in patients taking Lactobacillus reuteri daily for 8 weeks compared to the placebo group [277]. Furthermore, a systemic review and meta-analysis conducted by Du et al. showed that early enteral nutrition with probiotics after TBI reduced mortality and decreased GI complications such as constipation, abdominal distention, reflux and stress ulcers [278].
Probiotics also stimulate the release of SCFAs, such as acetate, butyrate, and propionate, into the peripheral circulation which can ultimately cross the BBB and ameliorate brain inflammation by decreasing the expression of proinflammatory cytokines and promoting neurogenesis [279,280,281]. A study by Li et al. demonstrated the neuroprotective effects of Clostridium butyricum (Cb), a butyrate-producing probiotic, after TBI via the brain-gut axis by increasing the levels of GLP-1 and glucagon-like peptide 1 receptor in the colon. Intragastric Cb supplementation (109 CFU/ml), once daily for 2 weeks pre and post-TBI, improved neurological outcomes in male mice by attenuating neurodegeneration, decreasing apoptosis and enhancing BBB integrity [282]. In parallel, the administration of the probiotic Lactobacillus acidophilus (LA) (1 × 1010 CFU) for 7 days after weight-drop TBI shifts the microbiome towards a healthier profile in male mice. LA improved neurological outcomes by decreasing the activation of astrocytes and microglia, and reduced brain edema by preserving the BBB integrity. LA supplementation also decreased the expression of gram negative bacteria receptors in the brain, mainly TLR4 [275]. Last, a randomized clinical trial showed that the daily administration of a combination of probiotics (Bifidobacterium longum, Lactobacillus bulgaricus, Streptococcus thermophilus) for 21 days after severe TBI attenuated systemic inflammation by lowering the levels of IL-4 and IL-10 and reducing the risk of nosocomial infections [283].These studies emphasize the link between the host gut microbiome and immune responses in the brain following TBI. The utilization of antibiotics/probiotics holds substantial therapeutic potential in TBI management, with further studies warranted to better elucidate their effects on brain inflammation and behavioral outcomes.
Microbial metabolites
Studies have also revealed that TBI induces alterations in gut microbial metabolites, including SCFAs and bile acids. Among these metabolites, SCFAs such as butyrate, propionate and acetate play a crucial role [284]. They serve as alternative energy sources for the injured brain and help regulate mitochondrial homeostasis [285]. A study by Opeyemi et al. demonstrated a significant decrease in fecal SCFAs concentrations 24 h and 28 days post-TBI in adult male mice. This decrease correlated with worse learning outcomes, while the administration of SCFAs improved spatial learning in these mice [286]. Furthermore, the role of bile acids has been studied in various neurological diseases, such as intracranial hemorrhage and ischemic stroke [287, 288]. The administration of tauroursodeoxycholic acid has been shown to improve neurologic function and decrease infarct size two and seven days after reperfusion [289]. In the context of TBI, You et al. demonstrated decreased levels of bile acids in serum and fecal samples one day after TBI in adult male mice [268]. Moreover, Zhu et al. conducted a prospective study which showed decreased levels of plasma bile acids in TBI patients [290]. Therefore, supplementation of microbial metabolites byproducts such as bile acids and SCFAs present promising therapies for mitigating neuroinflammation post-TBI.
Mycobiome
In addition to the dominant bacterial microbiome, the gut mycobiome (fungal microbiome) emerges as another crucial therapeutic target, regulating brain-gut homeostasis. Imbalances in the mycobiome have been observed in various intestinal diseases including IBS [291], IBD [292] and colorectal cancers [293]. Visceral hypersensitivity in IBS has been associated with increased fungal dysbiosis [294]. While their role is still understudied in traumatic brain injury, a recent prospective observational cohort study conducted by Park et al. revealed dysregulated mycobiome balance in critically ill trauma and sepsis for up to two to three weeks after intensive care unit hospitalizations. Dominance in Candida spp population and reduction in commensal fungal species correlated with heightened vulnerability to infections [295]. Interestingly, another study by Hunag et al. demonstrated that changes in gut mycobial abundance in mice three days post-TBI were linked to dysfunctional regulation of N6-methyadensoine (m6A), which is crucial in posttranscriptional modification of eukaryotic mRNA [296]. Given the intricate relationship between bacterial and fungal microbiomes, more studies are warranted to better understand the role of fungemia, particularly, candidemia, in TBI patients, and how modulating the mycobiome can modulate neurologic outcomes.
Current limitations
Human and animal studies are pivotal in investigating microbiome alterations and their impact on neurological outcomes following TBI [297, 298]. Various methodologies are utilized to detect these changes, including the administration of antibiotics [299], probiotics [283], SCFAs [300], and the use of fecal microbiome transplant [301]. Studies on the impact of antibiotics are particularly crucial, given that some patients with open head injuries and polytrauma necessitate antibiotic administration [302, 303], yet the neurological consequences of such interventions remain poorly understood. Very few clinical studies have examined the impact of antibiotics on TBI outcomes and there are currently no general guidelines on the administration of antibiotics [299]. In the context of TBI-induced gut microbial dysbiosis, there is a need to develop well-controlled clinical trials to explore the effects of antibiotic administration on changes in infection rates and neurological outcomes over the long-term.
A primary challenge in microbiota research in TBI originates from the widespread variability in sample collection and processing methods, including targeted sequencing and metagenomic sequencing [304]. Moreover, the heterogeneity in individual’s dietary patterns and pre-existing microbiome diversity present additional challenges in detecting microbiome variations [305]. Although preclinical animal models offer controlled experimental conditions such as standardized environments, their findings pose challenges in translational efforts [306]. Another significant aspect is the time required for probiotics to exert their effects on neurocognitive outcomes, potentially spanning years [307]. Thus, well-designed long-term clinical trials are necessary to fully comprehend the impact of microbiome in TBI. Addressing these limitations is essential for developing effective therapeutic interventions.
Tables 1 and 2 present a summary of various anti-inflammatory agents that attenuate brain and gut inflammation following TBI.
Brain-gut axis dysfunction in military veterans
Military veterans provide a unique human model for studying the impact of traumatic brain injuries on the gut in a realistic environment [308]. Following military occupational training involving blast exposure, a significant increase in intestinal permeability and evidence of gut bacterial translocation into the circulation were observed 1 to 16 h later, accompanied by a stepwise increase in alpha microbial diversity and elevated levels of intestinal permeability protein biomarkers such as zonulin and occludin-3 [309]. Additionally, another study involving 26 male Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn (OEF/OEI/OND) veterans revealed that differences in gut microbial composition, specifically Verrucomicrobiota, correlated with psychiatric and cognitive symptoms, including fatigue, depressive symptoms, and PTSD severity, as well as difficulties with attention, executive function, learning and memory [310]. These findings emphasize the intricate relationship between gut microbiota and mental health in veterans. Furthermore, research on Gulf War veterans indicated that a higher abundance of phyla Bacteroidetes, Actinobacteria, Euryarchaeota, and Proteobacteria, as well as higher abundances of the families Bacteroidaceae, Erysipelotrichaceae, and Bifidobacteriaceae, correlated with increased GI symptoms severity and higher levels of the inflammatory cytokine TNF-α, alongside reports of chronic pain, fatigue and sleep difficulties [311]. The Veterans in the US Veteran Microbiome Project (US-VMP) demonstrated a significant association between microbiome composition, episodes of gastroenteritis and symptoms of severe depression [312]. Additionally, an RCT conducted on OEF/OEI/OND veterans revealed that daily administration of Lactobacilli Reuteri for 8 weeks resulted in a decrease in plasma CRP levels compared to untreated groups, indicating the potential of microbiome-targeted interventions in mitigating post-TBI inflammation [277]. Conversely, some studies on US military veterans and US Marines did not find significant differences in gut microbial diversity and permeability after moderate/severe TBI [313, 314]. These conflicting findings underscore the complexity of studying the microbiome in real-world settings. Numerous limitations exist in such studies due to challenges in identifying true control participants, variations in the timing of stool collection, and differences in diet regimens and medications, which significantly impact the microbiome [313]. Efforts to address these limitations and refine study methodologies are crucial for advancing our understanding of the brain-gut axis in the context of TBI in military populations.
Why do TBI treatments keep failing?
Despite extensive TBI research and significant investment in various therapies, there remains a lack of effective treatments to attenuate disease progression [315]. Many clinical trials have failed to replicate the anti-inflammatory effects observed in preclinical animal models due to several challenges [316]. First, TBI is inherently heterogenous and triggers complex pathogenic pathways, rendering it a highly intricate disease to manage [317]. In basic science, most of the research is focused on specific cellular processes in the brain, often missing the broader picture of the disease [316]. Additionally, each model utilizes different injury paradigms and anatomical locations to induce injury. It is essential to recognize that focal contusion, concussion, and blast injuries elicit distinct inflammatory pathways in response to injury [318]. The tendency to extrapolate inflammatory models from focal contusion to concussion and blasts presents a significant issue due to each injury type’s unique inflammatory profiles [319, 320].
Another key challenge in TBI research is the overrepresentation of males in both clinical trials and preclinical models [321]. Sex differences in TBI responses are evident, with males showing better recovery in clinical trials and females exhibiting superior outcomes in preclinical studies [322]. Emerging evidence suggests the crucial role of sex in brain-gut homeostasis by modulating the gut microbiota and immune system activation [323, 324]. Animal studies reveal notable differences in gut microbiome composition between males and females, with females demonstrating greater diversity [325, 326]. Although the impact of sex on the microbiome in TBI is underexplored, studies in other diseases suggest that females are more susceptible to autoimmune diseases due to microbial alterations [327, 328]. Similarly, the higher prevalence of IBS in women may be linked to microbiome changes driven by estrogen-mediated responses or compromised gut barrier function [329]. To comprehensively understand the sex’s impact on brain-gut axis, clinical trials and animal models with more female representation are warranted.
The complexity of immune response post-TBI presents another challenge [330]. The evolution of immune cell activation over time involves both beneficial and detrimental components, making attempts to target specific immune pathways often unsuccessful [331]. Furthermore, the existing classification of M1/M2 microglia based on in vitro cell culturing excludes the diverse array of cytokines and cellular signals encountered by these cells in vivo, particularly in a complex disease like TBI [332]. A shift away from M1 and M2 classification towards incorporating transcriptomic and proteomic profiling for better analysis is needed [333]. Additionally, inflammation in TBI is not confined to the CNS; there is also global systemic immune dysfunction that remains understudied [57]. The gut, which harbors the largest immune reservoir, exhibits significant alterations in macrophage and T-cell immune profile, necessitating a better understanding of interactions between intestinal immunity and brain immune cells [4, 66].
Most drugs lose efficacy with increasing intervals between injury time and initiation of treatment [334]. Moreover, certain treatments, such as probiotics, require prolonged administration periods, potentially spanning years before cognitive improvements are observed [307]. The therapeutic time window in treatment of TBI remains a significant focus of investigation to advance the development of TBI therapies and successfully translate from preclinical to clinical settings [335]. While animal models often receive therapy immediately after injury, clinical trials at specialized trauma centers typically enroll patients 4–7 h after moderate to severe TBI [336]. Additionally, individuals with mild injuries may delay treatment until they are symptomatic, which may occur years after injury [337, 338]. The significance of the therapeutic time window was underscored by the failure of progesterone treatment in phase III clinical trials PROTECT and SYNAPSE [339]. Both trials recruited patients within 4 and 7 h after TBI, respectively, failing to replicate the benefits observed in preclinical animal models where progesterone was administered within an hour of injury [340]. These clinical trial failures highlight the importance of therapeutic window in initiating treatment. Preclinical models are encouraged to investigate drug efficacy with progressively delayed dosing post-injury to simulate real-life settings.
In addition to treatment timing, understanding the optimal duration of treatment is essential for elucidating long-term outcomes [341]. While some drugs, such as beta-blockers, have demonstrated significant improvements with short-term administration, even as brief as two days or two weeks, others, like probiotics, may require prolonged treatment periods to exert neuroprotective effects, especially for chronic conditions like TBI [219, 220, 277, 342]. A comprehensive understanding of the temporal and spatial dynamics of immune, hormonal and neural pathways within the brain-gut axis is imperative for evaluating the effects of chronic treatment regimens post-TBI [343]. Current animal studies predominantly focus on acute changes, missing potential chronic alterations that may influence drug efficacy and subsequent neurologic outcomes [15]. Persistent microbiome alterations observed for years post-TBI emphasize the potential necessity for extended treatment durations to mitigate brain injury consequences [89]. Studying the therapeutic window for treatment, the duration of treatments, and their impact on brain-gut homeostasis is crucial for the development of successful TBI therapies [334].
In clinical trials, numerous challenges are encountered, including the nonuniform population of patients with comorbid diseases and ethical considerations for randomization [344]. Additionally, the classification of mild-moderate-severe TBI is overly broad and fails to account for radiological and clinical findings, making it subjective [345]. Improved classifications systems are necessary to address this issue. The recent FDA approval for Abbott’s i-STAT TBI cartridge, designed to identify blood biomarkers such as GFAP and UCH-L1 within just 15 min at the patient’s bedside, promises more objective results to stratify injury severity and tailor management away from the conventional mild-moderate-severe classification [346]. Last, the reliance on monotherapy to treat such a complicated disease compound the challenges [347]. There should be greater emphasis on targeting various pathways in the brain and gut at the same time to effectively manage this complex disease.
Conclusion
In conclusion, we present the first comprehensive review of various pharmacotherapies targeting inflammation along the brain-gut axis in TBI, which include hormones such as serotonin, ghrelin, and progesterone, alongside ANS modulators like beta-blockers and alpha-adrenergic agonists, antilipidemic agents such as statins, and intestinal flora modulators such as probiotics and antibiotics (summarized in Tables 1 and 2). They enhance gut function by mitigating inflammation, preserving intestinal barrier integrity, promoting motility and favoring a healthy microbiome. Importantly, these pharmacotherapies also impact neurological outcomes directly by crossing the BBB or indirectly by modulating immune, hormonal and neural pathways.
With the gut serving as the largest immune reservoir, housing the body’s second “little brain”-the ENS [348], and hosting a diverse microbiome, it emerges as a focal point in understanding TBI pathogenesis. Deciphering the complex interplay between microbial dysbiosis, ENS disruption, EEC dysfunction, ANS dysregulation and intestinal immune cell activation is crucial to develop successful TBI therapies, which have been elusive for decades. This entails understanding the temporal changes in immune system activation across the brain and the gut, as well as elucidating the effects of gut microbial metabolites and hormones, and the role of autonomic nervous system and systemic inflammation in the pathophysiological process of acute and chronic TBI.
Availability of data and materials
Not applicable.
Abbreviations
- TBI:
-
Traumatic brain injury
- GI:
-
Gastrointestinal system
- ENS:
-
Enteric nervous system
- ANS:
-
Autonomic nervous system
- ICP:
-
Intracranial pressure
- DAMP:
-
Damage-associated molecular pattern
- ROS:
-
Reactive oxygen species
- BBB:
-
Blood–brain-barrier
- AQP4:
-
Aquaporin 4
- ATP:
-
Adenosine triphosphate
- Bcl-2:
-
B-cell lymphoma 2
- ICU:
-
Intensive care unit
- HPA:
-
Hypothalamic–pituitary–adrenal
- Ccr2:
-
C–C chemokine receptor type 2
- TNF-α:
-
Tumor necrosis factor alpha
- IL-1β:
-
Interleukin-1 beta
- TLR4:
-
Toll-like receptor 4
- EGC:
-
Enteric glial cell
- Ach:
-
Acetylcholine
- α7nAChR:
-
α7 Subtype of the nicotinic acetylcholine receptor
- EEC:
-
Enteroendocrine cell
- VNS:
-
Vagus/Vagal nerve stimulation
- IBD:
-
Inflammatory bowel disease
- IBS:
-
Irritable bowel syndrome
- CNS:
-
Central nervous system
- GLP-1:
-
Glucagon-like peptide 1
- ChgA:
-
Chromogranin A
- Lgr5:
-
Leucine-rich repeat-containing G-protein coupled receptor 5
- Notch1:
-
Notch receptor 1
- Atoh1:
-
Atonal bHLH transcription factor 1
- Neurog3:
-
Neurogenin 3
- TPH:
-
Tryptophan hydroxylase
- SSRI:
-
Selective serotonin reuptake inhibitor
- SNRI:
-
Serotonin-norepinephrine reuptake inhibitor
- ICC:
-
Interstitial cells of Cajal
- IP:
-
Intraperitoneal
- FGF:
-
Fibroblast growth factor
- FGF-BP:
-
FGF-binding protein
- bFGF:
-
Basic FGF
- PI3K:
-
Phosphoinositide 3-kinase
- PIP3:
-
Phosphatidylinositol 3,4,5 trisphosphate
- PIP2:
-
Phosphatidylinositol 3,4 bisphosphate
- Pkb/Akt:
-
Protein kinase B
- IRI:
-
Ischemia–reperfusion injury
- SCI:
-
Spinal cord injury
- mTOR:
-
Mammalian target of rapamycin
- WD:
-
Weight drop
- ICH:
-
Intracerebral hemorrhage
- SMA:
-
Superior mesenteric artery
- BDNF:
-
Brain-derived neurotrophic factor
- CD55:
-
Complement decay-accelerating factor
- Nrf2:
-
Nuclear factor erythroid 2-related factor 2
- ICAM-1:
-
Intercellular adhesion molecule-1
- SAH:
-
Subarachnoid hemorrhage
- NE:
-
Norepinephrine
- HSP-70:
-
Heat shock protein 70
- UCHL-1:
-
Ubiquitin carboxyl-terminal hydrolase L1
- ZO-1:
-
Zonula Occludens-1
- vBNST:
-
Ventral bed nucleus of the stria terminalis
- AD:
-
Alzheimer’s disease
- CD68:
-
Cluster of differentiation 68
- GFAP:
-
Glial fibrillary acidic protein
- VEGF:
-
Vascular endothelial growth factor
- GSK-3beta:
-
Glycogen synthase kinase-3beta
- CD40:
-
Cluster of differentiation 40
- VCAM-1:
-
Vascular cell adhesion molecule-1
- SCFA:
-
Short-chain fatty acid
- Cb:
-
Clostridium butyricum
- LA:
-
Lactobacillus acidophilus
References
Centers for disease control and prevention (CDC). Traumatic brain injury and concussion. Atlanta: Centers for disease control and prevention; https://www.cdc.gov/traumaticbraininjury/index.html. Accessed 15 Feb 2024.
Simon DW, McGeachy MJ, Bayır H, Clark RSB, Loane DJ, Kochanek PM. The far-reaching scope of neuroinflammation after traumatic brain injury. Nat Rev Neurol. 2017;13(3):171–91.
Brett BL, Gardner RC, Godbout J, Dams-O’Connor K, Keene CD. Traumatic brain injury and risk of neurodegenerative disorder. Biol Psychiatry. 2022;91(5):498–507.
Hanscom M, Loane DJ, Shea-Donohue T. Brain-gut axis dysfunction in the pathogenesis of traumatic brain injury. J Clin Investig. 2021;131(12): e143777.
Nasr IW, Chun Y, Kannan S. Neuroimmune responses in the developing brain following traumatic brain injury. Exp Neurol. 2019;320: 112957.
Unterberg AW, Stover J, Kress B, Kiening KL. Edema and brain trauma. Neuroscience. 2004;129(4):1021–9.
Chesnut RM, Gautille T, Blunt BA, Klauber MR, Marshall LF. Neurogenic hypotension in patients with severe head injuries. J Trauma. 1998;44(6):958–63 (discussion 63-4).
Parikh U, Williams M, Jacobs A, Pineda JA, Brody DL, Friess SH. Delayed hypoxemia following traumatic brain injury exacerbates white matter injury. J Neuropathol Exp Neurol. 2016;75(8):731–47.
Davies M, Jacobs A, Brody DL, Friess SH. Delayed hypoxemia after traumatic brain injury exacerbates long-term behavioral deficits. J Neurotrauma. 2018;35(5):790–801.
Hermanides J, Hong YT, Trivedi M, Outtrim J, Aigbirhio F, Nestor PJ, et al. Metabolic derangements are associated with impaired glucose delivery following traumatic brain injury. Brain. 2021;144(11):3492–504.
Haddad SH, Arabi YM. Critical care management of severe traumatic brain injury in adults. Scand J Trauma Resusc Emerg Med. 2012;20:12.
Lozano D, Gonzales-Portillo GS, Acosta S, de la Pena I, Tajiri N, Kaneko Y, Borlongan CV. Neuroinflammatory responses to traumatic brain injury: etiology, clinical consequences, and therapeutic opportunities. Neuropsychiatr Dis Treat. 2015;11:97–106.
Karve IP, Taylor JM, Crack PJ. The contribution of astrocytes and microglia to traumatic brain injury. Br J Pharmacol. 2016;173(4):692–702.
El Baassiri MG, Rahal SS, Fulton WB, Sodhi CP, Hackam DJ, Nasr IW. Pharmacologic Toll-like receptor 4 inhibition skews toward a favorable A1/A2 astrocytic ratio improving neurocognitive outcomes following traumatic brain injury. J Trauma Acute Care Surg. 2023;95(3):361–7.
Ng SY, Lee AYW. Traumatic brain injuries: pathophysiology and potential therapeutic targets. Front Cell Neurosci. 2019;13:528.
El Baassiri MG, Chun YH, Rahal SS, Fulton WB, Sodhi CP, Hackam DJ, Nasr IW. Infiltrating anti-inflammatory monocytes modulate microglial activation through toll-like receptor 4/interferon-dependent pathways following traumatic brain injury. J Trauma Acute Care Surg. 2023;95(3):368–75.
Wu Y, Wu H, Guo X, Pluimer B, Zhao Z. Blood-brain barrier dysfunction in mild traumatic brain injury: evidence from preclinical murine models. Front Physiol. 2020;11:1030.
Baracaldo-Santamaria D, Ariza-Salamanca DF, Corrales-Hernandez MG, Pachon-Londono MJ, Hernandez-Duarte I, Calderon-Ospina CA. Revisiting excitotoxicity in traumatic brain injury: from bench to bedside. Pharmaceutics. 2022;14(1):152.
Cheng G, Kong RH, Zhang LM, Zhang JN. Mitochondria in traumatic brain injury and mitochondrial-targeted multipotential therapeutic strategies. Br J Pharmacol. 2012;167(4):699–719.
Pilitsis JG, Coplin WM, O’Regan MH, Wellwood JM, Diaz FG, Fairfax MR, et al. Free fatty acids in cerebrospinal fluids from patients with traumatic brain injury. Neurosci Lett. 2003;349(2):136–8.
Sparvero LJ, Amoscato AA, Kochanek PM, Pitt BR, Kagan VE, Bayir H. Mass-spectrometry based oxidative lipidomics and lipid imaging: applications in traumatic brain injury. J Neurochem. 2010;115(6):1322–36.
Serhan CN, Haeggstrom J. Lipid mediators in acute inflammation and resolution: Eicosanoids, PAF, resolvins, and protectins. In: Serhan CN, Ward PA, Gilroy DW, Ayoub SS, editors. Fundamentals of Inflammation. Cambridge: Cambridge University Press; 2010. p. 153–74.
Michinaga S, Koyama Y. Pathophysiological responses and roles of astrocytes in traumatic brain injury. Int J Mol Sci. 2021;22(12):6418.
Loane DJ, Kumar A. Microglia in the TBI brain: the good, the bad, and the dysregulated. Exp Neurol. 2016;275:316–27.
Mira RG, Lira M, Cerpa W. Traumatic brain injury: mechanisms of glial response. Front Physiol. 2021;12: 740939.
Zhou Y, Shao A, Yao Y, Tu S, Deng Y, Zhang J. Dual roles of astrocytes in plasticity and reconstruction after traumatic brain injury. Cell Commun Signal. 2020;18(1):62.
Burda JE, Bernstein AM, Sofroniew MV. Astrocyte roles in traumatic brain injury. Exp Neurol. 2016;275:305–15.
Yu F, Wang Y, Stetler AR, Leak RK, Hu X, Chen J. Phagocytic microglia and macrophages in brain injury and repair. CNS Neurosci Ther. 2022;28(9):1279–93.
Xu H, Wang Z, Li J, Wu H, Peng Y, Fan L, et al. The polarization states of microglia in TBI: a new paradigm for pharmacological intervention. Neural Plast. 2017;2017:5405104.
Shao F, Wang X, Wu H, Wu Q, Zhang J. Microglia and neuroinflammation: crucial pathological mechanisms in traumatic brain injury-induced neurodegeneration. Front Aging Neurosci. 2022;14: 825086.
Donat CK, Scott G, Gentleman SM, Sastre M. Microglial activation in traumatic brain injury. Front Aging Neurosci. 2017;9:208.
Abdel-Haq R, Schlachetzki JCM, Glass CK, Mazmanian SK. Microbiome-microglia connections via the gut-brain axis. J Exp Med. 2019;216(1):41–59.
Alam A, Thelin EP, Tajsic T, Khan DZ, Khellaf A, Patani R, Helmy A. Cellular infiltration in traumatic brain injury. J Neuroinflammation. 2020;17(1):1.
Anthony DC, Couch Y, Losey P, Evans MC. The systemic response to brain injury and disease. Brain Behav Immun. 2012;26(4):534–40.
Sabet N, Soltani Z, Khaksari M. Multipotential and systemic effects of traumatic brain injury. J Neuroimmunol. 2021;357: 577619.
McDonald SJ, Sharkey JM, Sun M, Kaukas LM, Shultz SR, Turner RJ, et al. Beyond the brain: peripheral interactions after traumatic brain injury. J Neurotrauma. 2020;37(5):770–81.
Faden AI, Barrett JP, Stoica BA, Henry RJ. Bidirectional brain-systemic interactions and outcomes after TBI. Trends Neurosci. 2021;44(5):406–18.
Anderson D, Kutsogiannis DJ, Sligl WI. Sepsis in traumatic brain injury: epidemiology and outcomes. Can J Neurol Sci. 2020;47(2):197–201.
Hu PJ, Pittet J-F, Kerby JD, Bosarge PL, Wagener BM. Acute brain trauma, lung injury, and pneumonia: more than just altered mental status and decreased airway protection. Am J Physiol Lung Cell Mol Physiol. 2017;313(1):L1–15.
Iftikhar PM, Anwar A, Saleem S, Nasir S, Inayat A. Traumatic brain injury causing intestinal dysfunction: A review. J Clin Neurosci. 2020;79:237–40.
Norton JA, Ott LG, McClain C, Adams L, Dempsey RJ, Haack D, et al. Intolerance to enteral feeding in the brain-injured patient. J Neurosurg. 1988;68(1):62–6.
McConnochie R, O’Brien A, Parke R. A single-centre observational study of delayed defaecation in brain-injured patients in an adult intensive care unit. Aust Crit Care. 2023. https://doi.org/10.1016/j.aucc.2023.07.002.
Harrison-Felix C, Whiteneck G, Devivo MJ, Hammond FM, Jha A. Causes of death following 1 year postinjury among individuals with traumatic brain injury. J Head Trauma Rehabil. 2006;21(1):22–33.
Giraudo D, Gozzerino F, Antoniono E, Lamberti G. Anal incontinence and severe acquired brain injury: a retrospective study of 347 rehabilitation inpatients. Pelviperineology. 2017;36(1):14.
Pelizzari L, Antoniono E, Giraudo D, Ciardi G, Lamberti G. Fecal incontinence after severe brain injury: a barrier to discharge after inpatient rehabilitation? Neurol Int. 2023;15(4):1339–51.
Hidalgo JRH. Neurogenic bowel dysfunction in subjects with brain injury: prevalence, risk factors, clinical characterization and physiopathology: Universitat Pompeu Fabra; 2018.
Lee HY, Oh BM. Nutrition management in patients with traumatic brain injury: a narrative review. Brain Neurorehabil. 2022;15(1): e4.
Schwulst SJ, Trahanas DM, Saber R, Perlman H. Traumatic brain injury–induced alterations in peripheral immunity. J Trauma Acute Care Surg. 2013;75(5):780–8.
Li D, Chen J, Weng C, Huang X. Impact of the severity of brain injury on secondary adrenal insufficiency in traumatic brain injury patients and the influence of HPA axis dysfunction on prognosis. Int J Neurosci. 2023. https://doi.org/10.1080/00207454.2023.2280450.
Rodino-Janeiro BK, Alonso-Cotoner C, Pigrau M, Lobo B, Vicario M, Santos J. Role of corticotropin-releasing factor in gastrointestinal permeability. J Neurogastroenterol Motil. 2015;21(1):33–50.
La Torre D, Van Oudenhove L, Vanuytsel T, Verbeke K. Psychosocial stress-induced intestinal permeability in healthy humans: what is the evidence? Neurobiol Stress. 2023;27: 100579.
Lu J, Goh SJ, Tng PY, Deng YY, Ling EA, Moochhala S. Systemic inflammatory response following acute traumatic brain injury. Front Biosci (Landmark Ed). 2009;14(10):3795–813.
Milleville KA, Awan N, Disanto D, Kumar RG, Wagner AK. Early chronic systemic inflammation and associations with cognitive performance after moderate to severe TBI. Brain Behav Immun Health. 2021;11: 100185.
Sun Y, Bai L, Niu X, Wang Z, Yin B, Bai G, et al. Elevated serum levels of inflammation-related cytokines in mild traumatic brain injury are associated with cognitive performance. Front Neurol. 2019;10:1120.
Kumar RG, Boles JA, Wagner AK. Chronic inflammation after severe traumatic brain injury: characterization and associations with outcome at 6 and 12 months postinjury. J Head Trauma Rehabil. 2015;30(6):369–81.
Dong T, Zhi L, Bhayana B, Wu MX. Cortisol-induced immune suppression by a blockade of lymphocyte egress in traumatic brain injury. J Neuroinflammation. 2016;13(1):197.
Bouras M, Asehnoune K, Roquilly A. Immune modulation after traumatic brain injury. Front Med (Lausanne). 2022;9: 995044.
Hazeldine J, Lord JM, Belli A. Traumatic brain injury and peripheral immune suppression: primer and prospectus. Front Neurol. 2015;6:235.
Ritzel RM, Doran SJ, Barrett JP, Henry RJ, Ma EL, Faden AI, Loane DJ. Chronic alterations in systemic immune function after traumatic brain injury. J Neurotrauma. 2018;35(13):1419–36.
Sotosek Tokmadzic V, Laskarin G, Mahmutefendic H, Lucin P, Mrakovcic-Sutic I, Zupan Z, Sustic A. Expression of cytolytic protein-perforin in peripheral blood lymphocytes in severe traumatic brain injured patients. Injury. 2012;43(5):624–31.
Dziedzic T, Slowik A, Szczudlik A. Nosocomial infections and immunity: lesson from brain-injured patients. Crit Care. 2004;8(4):266–70.
Chaban V, Clarke GJB, Skandsen T, Islam R, Einarsen CE, Vik A, et al. Systemic inflammation persists the first year after mild traumatic brain injury: results from the prospective trondheim mild traumatic brain injury study. J Neurotrauma. 2020;37(19):2120–30.
Krishnamoorthy V, Komisarow JM, Laskowitz DT, Vavilala MS. Multiorgan dysfunction after severe traumatic brain injury: epidemiology, mechanisms, and clinical management. Chest. 2021;160(3):956–64.
Ritzel RM, Li Y, Jiao Y, Lei Z, Doran SJ, He J, et al. Brain injury accelerates the onset of a reversible age-related microglial phenotype associated with inflammatory neurodegeneration. Sci Adv. 2023;9(10):eadd1101.
Barker S, Paul BD, Pieper AA. Increased risk of aging-related neurodegenerative disease after traumatic brain injury. Biomedicines. 2023;11(4):1154.
El Baassiri MG, Raouf Z, Jang HS, Scheese D, Duess JW, Fulton WB, et al. Ccr2 dependent monocytes exacerbate intestinal inflammation and modulate gut serotonergic signaling following traumatic brain injury. J Trauma Acute Care Surg. 2024. https://doi.org/10.1097/TA.0000000000004246.
Needham EJ, Helmy A, Zanier ER, Jones JL, Coles AJ, Menon DK. The immunological response to traumatic brain injury. J Neuroimmunol. 2019;332:112–25.
Holmin S, Soderlund J, Biberfeld P, Mathiesen T. Intracerebral inflammation after human brain contusion. Neurosurgery. 1998;42(2):291–8 (discussion 8-9).
Daglas M, Draxler DF, Ho H, McCutcheon F, Galle A, Au AE, et al. Activated CD8(+) T cells cause long-term neurological impairment after traumatic brain injury in mice. Cell Rep. 2019;29(5):1178-91 e6.
Benakis C, Brea D, Caballero S, Faraco G, Moore J, Murphy M, et al. Commensal microbiota affects ischemic stroke outcome by regulating intestinal gammadelta T cells. Nat Med. 2016;22(5):516–23.
Celorrio M, Shumilov K, Rodgers R, Schriefer L, Li Y, Baldridge MT, Friess SH. Innate and peripheral immune alterations after traumatic brain injury are regulated in a gut microbiota-dependent manner in mice. J Neurotrauma. 2023;40(7–8):772–87.
Furness JB, Callaghan BP, Rivera LR, Cho H-J. The enteric nervous system and gastrointestinal innervation: integrated local and central control. New York: Springer; 2014. p. 39–71.
Rizoli SB, Jaja BN, Di Battista AP, Rhind SG, Neto AC, da Costa L, et al. Catecholamines as outcome markers in isolated traumatic brain injury: the COMA-TBI study. Crit Care. 2017;21(1):37.
Schroeppel TJ, Sharpe JP, Shahan CP, Clement LP, Magnotti LJ, Lee M, et al. Beta-adrenergic blockade for attenuation of catecholamine surge after traumatic brain injury: a randomized pilot trial. Trauma Surg Acute Care Open. 2019;4(1): e000307.
Montgomery LE, Tansey EA, Johnson CD, Roe SM, Quinn JG. Autonomic modification of intestinal smooth muscle contractility. Adv Physiol Educ. 2016;40(1):104–9.
Natale G, Ryskalin L, Busceti CL, Biagioni F, Fornai F. The nature of catecholamine-containing neurons in the enteric nervous system in relationship with organogenesis, normal human anatomy and neurodegeneration. Arch Ital Biol. 2017;155(3):118–30.
Ma EL, Smith AD, Desai N, Cheung L, Hanscom M, Stoica BA, et al. Bidirectional brain-gut interactions and chronic pathological changes after traumatic brain injury in mice. Brain Behav Immun. 2017;66:56–69.
Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 2018;9:44.
Chen JD. Parasympathetic control of gastrointestinal motility and cross-branch actions of parasympathetic neuromodulation. Chin Med J (Engl). 2023;136(1):53–5.
Keever KR, Cui K, Casteel JL, Singh S, Hoover DB, Williams DL, et al. Cholinergic signaling via the alpha7 nicotinic acetylcholine receptor regulates the migration of monocyte-derived macrophages during acute inflammation. J Neuroinflammation. 2024;21(1):3.
Gabalski AH, Tynan A, Tsaava T, Li JH, Lee D, Hepler TD, et al. Circulating extracellular choline acetyltransferase regulates inflammation. J Intern Med. 2024;295(3):346–56.
Ueno H, Nakazato M. Mechanistic relationship between the vagal afferent pathway, central nervous system and peripheral organs in appetite regulation. J Diabetes Investig. 2016;7(6):812–8.
Siopi E, Galerne M, Rivagorda M, Saha S, Moigneu C, Moriceau S, et al. Gut microbiota changes require vagus nerve integrity to promote depressive-like behaviors in mice. Mol Psychiatry. 2023;28(7):3002–12.
Ye L, Bae M, Cassilly CD, Jabba SV, Thorpe DW, Martin AM, et al. Enteroendocrine cells sense bacterial tryptophan catabolites to activate enteric and vagal neuronal pathways. Cell Host Microbe. 2021;29(2):179-96 e9.
Pruitt DT, Schmid AN, Kim LJ, Abe CM, Trieu JL, Choua C, et al. Vagus nerve stimulation delivered with motor training enhances recovery of function after traumatic brain injury. J Neurotrauma. 2016;33(9):871–9.
Ullah H, Arbab S, Tian Y, Liu CQ, Chen Y, Qijie L, et al. The gut microbiota-brain axis in neurological disorder. Front Neurosci. 2023;17:1225875.
Taraskina A, Ignatyeva O, Lisovaya D, Ivanov M, Ivanova L, Golovicheva V, et al. Effects of traumatic brain injury on the gut microbiota composition and serum amino acid profile in rats. Cells. 2022;11(9):1409.
Treangen TJ, Wagner J, Burns MP, Villapol S. Traumatic brain injury in mice induces acute bacterial dysbiosis within the fecal microbiome. Front Immunol. 2018;9:2757.
Urban RJ, Pyles RB, Stewart CJ, Ajami N, Randolph KM, Durham WJ, et al. Altered fecal microbiome years after traumatic brain injury. J Neurotrauma. 2020;37(8):1037–51.
Munley JA, Kirkpatrick SL, Gillies GS, Bible LE, Efron PA, Nagpal R, Mohr AM. The intestinal microbiome after traumatic injury. Microorganisms. 2023;11(8):1990.
Pyles RB, Miller AL, Urban RJ, Sheffield-Moore M, Wright TJ, Maxwell CA, et al. The altered TBI fecal microbiome is stable and functionally distinct. Front Mol Neurosci. 2024;17:1341808.
Nicholson SE, Watts LT, Burmeister DM, Merrill D, Scroggins S, Zou Y, et al. Moderate traumatic brain injury alters the gastrointestinal microbiome in a time-dependent manner. Shock. 2019;52(2):240–8.
Singh R, Zogg H, Wei L, Bartlett A, Ghoshal UC, Rajender S, Ro S. Gut microbial dysbiosis in the pathogenesis of gastrointestinal dysmotility and metabolic disorders. J Neurogastroenterol Motil. 2021;27(1):19–34.
Bel S, Pendse M, Wang Y, Li Y, Ruhn KA, Hassell B, et al. Paneth cells secrete lysozyme via secretory autophagy during bacterial infection of the intestine. Science. 2017;357(6355):1047–52.
Yang E, Shen J. The roles and functions of Paneth cells in Crohn’s disease: a critical review. Cell Prolif. 2021;54(1): e12958.
Yang W, Yuan Q, Li Z, Du Z, Wu G, Yu J, Hu J. Translocation and dissemination of gut bacteria after severe traumatic brain injury. Microorganisms. 2022;10(10):2082.
Zeng H, Umar S, Rust B, Lazarova D, Bordonaro M. Secondary bile acids and short chain fatty acids in the colon: a focus on colonic microbiome, cell proliferation, inflammation, and cancer. Int J Mol Sci. 2019;20(5):1214.
Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28(2):203–9.
Bonaz B, Bazin T, Pellissier S. The vagus nerve at the interface of the microbiota-gut-brain axis. Front Neurosci. 2018;12: 336468.
Xiong Z, Nelson B, Sneiderman C, Janesko-Feldman K, Kochanek P, Rajasundaram D, et al. Microbiota-derived SCFAs promote chronic neurogenesis and anti-inflammatory gene expression after traumatic brain injury (P1–6.008). Neurology. 2023. https://doi.org/10.1212/WNL.0000000000203108.
Rehfeld JF. The new biology of gastrointestinal hormones. Physiol Rev. 1998;78(4):1087–108.
Raouf Z, Steinway SN, Scheese D, Lopez CM, Duess JW, Tsuboi K, et al. Colitis-induced small intestinal hypomotility is dependent on enteroendocrine cell loss in mice. Cell Mol Gastroenterol Hepatol. 2024. https://doi.org/10.1016/j.jcmgh.2024.02.017.
Kaelberer MM, Buchanan KL, Klein ME, Barth BB, Montoya MM, Shen X, Bohorquez DV. A gut-brain neural circuit for nutrient sensory transduction. Science. 2018;361(6408):eaat5236.
Latorre R, Sternini C, De Giorgio R, Greenwood-Van MB. Enteroendocrine cells: a review of their role in brain-gut communication. Neurogastroenterol Motil. 2016;28(5):620–30.
Uellendahl-Werth F, Maj C, Borisov O, Juzenas S, Wacker EM, Jorgensen IF, et al. Cross-tissue transcriptome-wide association studies identify susceptibility genes shared between schizophrenia and inflammatory bowel disease. Commun Biol. 2022;5(1):80.
Chandra R, Hiniker A, Kuo YM, Nussbaum RL, Liddle RA. alpha-Synuclein in gut endocrine cells and its implications for Parkinson’s disease. JCI Insight. 2017;2(12):e92295.
Roth W, Zadeh K, Vekariya R, Ge Y, Mohamadzadeh M. Tryptophan metabolism and gut-brain homeostasis. Int J Mol Sci. 2021;22(6):2973.
Werner JK, Stevens RD. Traumatic brain injury: recent advances in plasticity and regeneration. Curr Opin Neurol. 2015;28(6):565–73.
Zhang Z, Rasmussen L, Saraswati M, Koehler RC, Robertson C, Kannan S. Traumatic injury leads to inflammation and altered tryptophan metabolism in the juvenile rabbit brain. J Neurotrauma. 2019;36(1):74–86.
Aaldijk E, Vermeiren Y. The role of serotonin within the microbiota-gut-brain axis in the development of Alzheimer’s disease: a narrative review. Ageing Res Rev. 2022;75: 101556.
Craine TJ, Race NS, Kutash LA, Iouchmanov AL, Moschonas EH, O’Neil DA, et al. Milnacipran ameliorates executive function impairments following frontal lobe traumatic brain injury in male rats: a multimodal behavioral assessment. J Neurotrauma. 2023;40(1–2):112–24.
Jenkins T, Nguyen J, Polglaze K, Bertrand P. Influence of tryptophan and serotonin on mood and cognition with a possible role of the gut-brain axis. Nutrients. 2016;8(1):56.
Mittal R, Debs LH, Patel AP, Nguyen D, Patel K, O’Connor G, et al. Neurotransmitters: the critical modulators regulating gut-brain axis. J Cell Physiol. 2017;232(9):2359–72.
Banskota S, Khan WI. Gut-derived serotonin and its emerging roles in immune function, inflammation, metabolism and the gut-brain axis. Curr Opin Endocrinol Diabetes Obes. 2022;29(2):177–82.
Acharekar MV, Guerrero Saldivia SE, Unnikrishnan S, Chavarria YY, Akindele AO, Jalkh AP, et al. A systematic review on the efficacy and safety of selective serotonin reuptake inhibitors in gastrointestinal motility disorders: more control, less risk. Cureus. 2022. https://doi.org/10.7759/cureus.27691.
Mercado NM, Zhang G, Ying Z, Gomez-Pinilla F. Traumatic brain injury alters the gut-derived serotonergic system and associated peripheral organs. Biochim Biophys Acta Mol Basis Dis. 2022;1868(11): 166491.
Weaver JL, Eliceiri B, Costantini TW. Fluoxetine reduces organ injury and improves motor function after traumatic brain injury in mice. J Trauma Acute Care Surg. 2022;93(1):38–42.
Yue JK, Burke JF, Upadhyayula PS, Winkler EA, Deng H, Robinson CK, et al. Selective serotonin reuptake inhibitors for treating neurocognitive and neuropsychiatric disorders following traumatic brain injury: an evaluation of current evidence. Brain Sci. 2017;7(8):93.
Ansari A, Jain A, Sharma A, Mittal RS, Gupta ID. Role of sertraline in posttraumatic brain injury depression and quality-of-life in TBI. Asian J Neurosurg. 2014;9(4):182–8.
Cross AJ, Crow TJ, Ferrier IN, Johnson JA, Bloom SR, Corsellis JA. Serotonin receptor changes in dementia of the Alzheimer type. J Neurochem. 1984;43(6):1574–81.
Tohgi H, Abe T, Takahashi S, Kimura M, Takahashi J, Kikuchi T. Concentrations of serotonin and its related substances in the cerebrospinal fluid in patients with Alzheimer type dementia. Neurosci Lett. 1992;141(1):9–12.
Vermeiren Y, Van Dam D, Aerts T, Engelborghs S, De Deyn PP. Brain region-specific monoaminergic correlates of neuropsychiatric symptoms in Alzheimer’s disease. J Alzheimers Dis. 2014;41(3):819–33.
Liang Y, Xie S, He Y, Xu M, Qiao X, Zhu Y, Wu W. Kynurenine pathway metabolites as biomarkers in Alzheimer’s disease. Dis Markers. 2022;2022:9484217.
Mace JL, Porter RJ, Dalrymple-Alford JC, Wesnes KA, Anderson TJ. Effects of acute tryptophan depletion on neuropsychological and motor function in Parkinson’s disease. J Psychopharmacol. 2010;24(10):1465–72.
Politis M, Loane C. Serotonergic dysfunction in Parkinson’s disease and its relevance to disability. Sci World J. 2011;11:1726–34.
Porter RJ, Lunn BS, O’Brien JT. Effects of acute tryptophan depletion on cognitive function in Alzheimer’s disease and in the healthy elderly. Psychol Med. 2003;33(1):41–9.
Feder A, Skipper J, Blair JR, Buchholz K, Mathew SJ, Schwarz M, et al. Tryptophan depletion and emotional processing in healthy volunteers at high risk for depression. Biol Psychiatry. 2011;69(8):804–7.
van der Veen FM, Evers EA, Deutz NE, Schmitt JA. Effects of acute tryptophan depletion on mood and facial emotion perception related brain activation and performance in healthy women with and without a family history of depression. Neuropsychopharmacology. 2007;32(1):216–24.
Cirrito JR, Disabato BM, Restivo JL, Verges DK, Goebel WD, Sathyan A, et al. Serotonin signaling is associated with lower amyloid-beta levels and plaques in transgenic mice and humans. Proc Natl Acad Sci USA. 2011;108(36):14968–73.
Kessing LV, Forman JL, Andersen PK. Do continued antidepressants protect against dementia in patients with severe depressive disorder? Int Clin Psychopharmacol. 2011;26(6):316–22.
Kessing LV, Sondergard L, Forman JL, Andersen PK. Antidepressants and dementia. J Affect Disord. 2009;117(1–2):24–9.
Berger M, Gray JA, Roth BL. The expanded biology of serotonin. Annu Rev Med. 2009;60:355–66.
Hoyer D, Clarke DE, Fozard JR, Hartig PR, Martin GR, Mylecharane EJ, et al. International union of pharmacology classification of receptors for 5-hydroxytryptamine (Serotonin). Pharmacol Rev. 1994;46(2):157–203.
Weaver JL. The brain-gut axis: a prime therapeutic target in traumatic brain injury. Brain Res. 2021;1753: 147225.
Gao J, Xiong T, Grabauskas G, Owyang C. Mucosal serotonin reuptake transporter expression in irritable bowel syndrome is modulated by gut microbiota via mast cell-prostaglandin E2. Gastroenterology. 2022;162(7):1962–74.
Mishima Y, Ishihara S. Enteric microbiota-mediated serotonergic signaling in pathogenesis of irritable bowel syndrome. Int J Mol Sci. 2021;22(19):10235.
Menees S, Chey W. The gut microbiome and irritable bowel syndrome. F1000 Res. 2018;7:1029.
Akhondzadeh S. Microbiome and Schizophrenia. Avicenna J Med Biotechnol. 2019;11(4):269.
Ma J, Wang R, Chen Y, Wang Z, Dong Y. 5-HT attenuates chronic stress-induced cognitive impairment in mice through intestinal flora disruption. J Neuroinflammation. 2023;20(1):23.
Yang C, Lin X, Wang X, Liu H, Huang J, Wang S. The schizophrenia and gut microbiota: a bibliometric and visual analysis. Front Psychiatry. 2022;13:1022472.
Appleton J. The gut-brain axis: influence of microbiota on mood and mental health. Integr Med (Encinitas). 2018;17(4):28–32.
Pergolizzi S, Alesci A, Centofanti A, Aragona M, Pallio S, Magaudda L, et al. Role of serotonin in the maintenance of inflammatory state in Crohn’s disease. Biomedicines. 2022;10(4):765.
Khan WI. The role of 5-HT dysregulation in inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2013;9(4):259–61.
Makhlouf S, Messelmani M, Zaouali J, Mrissa R. Cognitive impairment in celiac disease and non-celiac gluten sensitivity: review of literature on the main cognitive impairments, the imaging and the effect of gluten free diet. Acta Neurol Belg. 2018;118(1):21–7.
Coleman NS, Foley S, Dunlop SP, Wheatcroft J, Blackshaw E, Perkins AC, et al. Abnormalities of serotonin metabolism and their relation to symptoms in untreated celiac disease. Clin Gastroenterol Hepatol. 2006;4(7):874–81.
Ghia JE, Li N, Wang H, Collins M, Deng Y, El-Sharkawy RT, et al. Serotonin has a key role in pathogenesis of experimental colitis. Gastroenterology. 2009;137(5):1649–60.
Costedio MM, Coates MD, Danielson AB, Buttolph TR, Blaszyk HJ, Mawe GM, Hyman NH. Serotonin signaling in diverticular disease. J Gastrointest Surg. 2008;12(8):1439–45.
Jandee S, Geeraerts A, Geysen H, Rommel N, Tack J, Vanuytsel T. Management of ineffective esophageal hypomotility. Front Pharmacol. 2021;12: 638915.
Thomas RH, Luthin DR. Current and emerging treatments for irritable bowel syndrome with constipation and chronic idiopathic constipation: focus on prosecretory agents. Pharmacotherapy. 2015;35(6):613–30.
Coates MD, Johnson AC, Greenwood-Van Meerveld B, Mawe GM. Effects of serotonin transporter inhibition on gastrointestinal motility and colonic sensitivity in the mouse. Neurogastroenterol Motil. 2006;18(6):464–71.
Kohen R, Jarrett ME, Cain KC, Jun SE, Navaja GP, Symonds S, Heitkemper MM. The serotonin transporter polymorphism rs25531 is associated with irritable bowel syndrome. Dig Dis Sci. 2009;54(12):2663–70.
Herr N, Bode C, Duerschmied D. The effects of serotonin in immune cells. Front Cardiovasc Med. 2017;4:48.
Gill RK, Pant N, Saksena S, Singla A, Nazir TM, Vohwinkel L, et al. Function, expression, and characterization of the serotonin transporter in the native human intestine. Am J Physiol Gastrointest Liver Physiol. 2008;294(1):G254–62.
Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402(6762):656–60.
Murray CDR, Kamm MA, Bloom SR, Emmanuel AV. Ghrelin for the gastroenterologist: history and potential. Gastroenterology. 2003;125(5):1492–502.
Wu JT, Kral JG. Ghrelin: integrative neuroendocrine peptide in health and disease. Ann Surg. 2004;239(4):464–74.
Wu R, Dong W, Cui X, Zhou M, Simms HH, Ravikumar TS, Wang P. Ghrelin down-regulates proinflammatory cytokines in sepsis through activation of the vagus nerve. Ann Surg. 2007;245(3):480–6.
Waseem T, Duxbury M, Ito H, Ashley SW, Robinson MK. Exogenous ghrelin modulates release of pro-inflammatory and anti-inflammatory cytokines in LPS-stimulated macrophages through distinct signaling pathways. Surgery. 2008;143(3):334–42.
Lopez NE, Krzyzaniak MJ, Blow C, Putnam J, Ortiz-Pomales Y, Hageny A-M, et al. Ghrelin prevents disruption of the blood-brain barrier after traumatic brain injury. J Neurotrauma. 2012;29(2):385–93.
Zhang C, Chen J, Lu H. Expression of aquaporin-4 and pathological characteristics of brain injury in a rat model of traumatic brain injury. Mol Med Rep. 2015;12(5):7351–7.
Kleindienst A, Hesse F, Bullock MR, Buchfelder M. The neurotrophic protein S100B: value as a marker of brain damage and possible therapeutic implications. Prog Brain Res. 2007;161:317–25.
Shao X, Hu Q, Chen S, Wang Q, Xu P, Jiang X. Ghrelin ameliorates traumatic brain injury by down-regulating bFGF and FGF-BP. Front Neurosci. 2018;12:445.
Sun N, Wang H, Ma L, Lei P, Zhang Q. Ghrelin attenuates brain injury in septic mice via PI3K/Akt signaling activation. Brain Res Bull. 2016;124:278–85.
Chen L, Wei X, Hou Y, Liu X, Li S, Sun B, et al. Tetramethylpyrazine analogue CXC195 protects against cerebral ischemia/reperfusion-induced apoptosis through PI3K/Akt/GSK3beta pathway in rats. Neurochem Int. 2014;66:27–32.
Hong Y, Shao A, Wang J, Chen S, Wu H, McBride DW, et al. Neuroprotective effect of hydrogen-rich saline against neurologic damage and apoptosis in early brain injury following subarachnoid hemorrhage: possible role of the Akt/GSK3β signaling pathway. PLoS ONE. 2014;9(4): e96212.
Raghay K, Akki R, Bensaid D, Errami M. Ghrelin as an anti-inflammatory and protective agent in ischemia/reperfusion injury. Peptides. 2020;124: 170226.
Ku JM, Taher M, Chin KY, Barsby T, Austin V, Wong CH, et al. Protective actions of des-acylated ghrelin on brain injury and blood-brain barrier disruption after stroke in mice. Clin Sci (Lond). 2016;130(17):1545–58.
Miao Y, Xia Q, Hou Z, Zheng Y, Pan H, Zhu S. Ghrelin protects cortical neuron against focal ischemia/reperfusion in rats. Biochem Biophys Res Commun. 2007;359(3):795–800.
Ersahin M, Toklu HZ, Erzik C, Akakin D, Tetik S, Sener G, Yegen BC. Ghrelin alleviates spinal cord injury in rats via its anti-inflammatory effects. Turk Neurosurg. 2011;21(4):599–605.
Lee JY, Chung H, Yoo YS, Oh YJ, Oh TH, Park S, Yune TY. Inhibition of apoptotic cell death by ghrelin improves functional recovery after spinal cord injury. Endocrinology. 2010;151(8):3815–26.
Bansal V, Ryu SY, Blow C, Costantini T, Loomis W, Eliceiri B, et al. The hormone ghrelin prevents traumatic brain injury induced intestinal dysfunction. J Neurotrauma. 2010;27(12):2255–60.
Bansal V, Costantini T, Ryu SY, Peterson C, Loomis W, Putnam J, et al. Stimulating the central nervous system to prevent intestinal dysfunction after traumatic brain injury. J Trauma Inj Infect Criti Care. 2010;68(5):1059–64.
Bansal V, Ryu SY, Lopez N, Allexan S, Krzyzaniak M, Eliceiri B, et al. Vagal stimulation modulates inflammation through a ghrelin mediated mechanism in traumatic brain injury. Inflammation. 2012;35(1):214–20.
Zhang W, Lin TR, Hu Y, Fan Y, Zhao L, Stuenkel EL, Mulholland MW. Ghrelin stimulates neurogenesis in the dorsal motor nucleus of the vagus. J Physiol. 2004;559(3):729–37.
Shao X, Cheng S-X, Tu Y. Effect of Ghrelin on gastrointestinal motility after traumatic brain injury. Chin J Trauma. 2018;34:370–6.
Cheng Y, Wei Y, Yang W, Cai Y, Chen B, Yang G, et al. Ghrelin attenuates intestinal barrier dysfunction following intracerebral hemorrhage in mice. Int J Mol Sci. 2016;17(12):2032.
Zhang H, Cui Z, Luo G, Zhang J, Ma T, Hu N, Cui T. Ghrelin attenuates intestinal ischemia/reperfusion injury in mice by activating the mTOR signaling pathway. Int J Mol Med. 2013;32(4):851–9.
Nagy B, Szekeres-Barthó J, Kovács GL, Sulyok E, Farkas B, Várnagy Á, et al. Key to life: physiological role and clinical implications of progesterone. Int J Mol Sci. 2021;22(20):11039.
González-Orozco JC, Camacho-Arroyo I. Progesterone actions during central nervous system development. Front Neurosci. 2019;13:431027.
Fedotcheva TA, Fedotcheva NI, Shimanovsky NL. Progesterone as an anti-inflammatory drug and immunomodulator: new aspects in hormonal regulation of the inflammation. Biomolecules. 2022;12(9):1299.
Schumacher M, Mattern C, Ghoumari A, Oudinet JP, Liere P, Labombarda F, et al. Revisiting the roles of progesterone and allopregnanolone in the nervous system: resurgence of the progesterone receptors. Prog Neurobiol. 2014;113:6–39.
Gibson CL, Coomber B, Rathbone J. Is progesterone a candidate neuroprotective factor for treatment following ischemic stroke? Neuroscientist. 2009;15(4):324–32.
Irwin RW, Wang JM, Chen S, Brinton RD. Neuroregenerative mechanisms of allopregnanolone in Alzheimer’s disease. Front Endocrinol. 2012;2:117.
De Nicola AF, Labombarda F, Gonzalez Deniselle MC, Gonzalez SL, Garay L, Meyer M, et al. Progesterone neuroprotection in traumatic CNS injury and motoneuron degeneration. Front Neuroendocrinol. 2009;30(2):173–87.
He J, Evans CO, Hoffman SW, Oyesiku NM, Stein DG. Progesterone and allopregnanolone reduce inflammatory cytokines after traumatic brain injury. Exp Neurol. 2004;189(2):404–12.
Guo Q, Sayeed I, Baronne LM, Hoffman SW, Guennoun R, Stein DG. Progesterone administration modulates AQP4 expression and edema after traumatic brain injury in male rats. Exp Neurol. 2006;198(2):469–78.
Li Z, Wang B, Kan Z, Zhang B, Yang Z, Chen J, et al. Progesterone increases circulating endothelial progenitor cells and induces neural regeneration after traumatic brain injury in aged rats. J Neurotrauma. 2012;29(2):343–53.
Irwin RW, Yao J, Hamilton RT, Cadenas E, Brinton RD, Nilsen J. Progesterone and estrogen regulate oxidative metabolism in brain mitochondria. Endocrinology. 2008;149(6):3167–75.
Garcia-Ovejero D, González S, Paniagua-Torija B, Lima A, Molina-Holgado E, De Nicola AF, Labombarda F. Progesterone reduces secondary damage, preserves white matter, and improves locomotor outcome after spinal cord contusion. J Neurotrauma. 2014;31(9):857–71.
Coughlan T, Gibson C, Murphy S. Progesterone, BDNF and neuroprotection in the injured CNS. Int J Neurosci. 2009;119(10):1718–40.
Pan DS, Liu WG, Yang XF, Cao F. Inhibitory effect of progesterone on inflammatory factors after experimental traumatic brain injury. Biomed Environ Sci. 2007;20(5):432–8.
Hermann GE, Rogers RC, Bresnahan JC, Beattie MS. Tumor necrosis factor-alpha induces cFOS and strongly potentiates glutamate-mediated cell death in the rat spinal cord. Neurobiol Dis. 2001;8(4):590–9.
Cutler SM, Pettus EH, Hoffman SW, Stein DG. Tapered progesterone withdrawal enhances behavioral and molecular recovery after traumatic brain injury. Exp Neurol. 2005;195(2):423–9.
Yao X-L, Liu J, Lee E, Ling GSF, McCabe JT. Progesterone differentially regulates pro- and anti-apoptotic gene expression in cerebral cortex following traumatic brain injury in rats. J Neurotrauma. 2005;22(6):656–68.
Pettus EH, Wright DW, Stein DG, Hoffman SW. Progesterone treatment inhibits the inflammatory agents that accompany traumatic brain injury. Brain Res. 2005;1049(1):112–9.
Gibson CL, Gray LJ, Bath PMW, Murphy SP. Progesterone for the treatment of experimental brain injury; a systematic review. Brain. 2008;131(2):318–28.
Zeng Y, Zhang Y, Ma J, Xu J. Progesterone for acute traumatic brain injury: a systematic review of randomized controlled trials. PLoS ONE. 2015;10(10): e0140624.
Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC, et al. ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med. 2007;49(4):391-402 e1-2.
Xiao GM, Wei J, Wu ZH, Wang WM, Jiang QZ, Cheng J, et al. Clinical study on the therapeutic effects and mechanism of progesterone in the treatment for acute severe head injury. Zhonghua Wai Ke Za Zhi. 2007;45(2):106–8.
Stein DG. Embracing failure: what the phase III progesterone studies can teach about TBI clinical trials. Brain Inj. 2015;29(11):1259–72.
Alqudah M, Al-Shboul O, Al Dwairi A, Al UDDG, Alqudah A. Progesterone inhibitory role on gastrointestinal motility. Physiol Res. 2022;71(2):193–8.
Celorrio M, Abellanas MA, Rhodes J, Goodwin V, Moritz J, Vadivelu S, et al. Gut microbial dysbiosis after traumatic brain injury modulates the immune response and impairs neurogenesis. Acta Neuropathol Commun. 2021;9(1):1.
Chen G, Shi JX, Qi M, Wang HX, Hang CH. Effects of progesterone on intestinal inflammatory response, mucosa structure alterations, and apoptosis following traumatic brain injury in male rats. J Surg Res. 2008;147(1):92–8.
Chen G, Shi J, Ding Y, Yin H, Hang C. Progesterone prevents traumatic brain injury-induced intestinal nuclear factor kappa B activation and proinflammatory cytokines expression in male rats. Mediat Inflamm. 2007;2007:1–7.
Jin W, Wang H, Ji Y, Hu Q, Yan W, Chen G, Yin H. Increased intestinal inflammatory response and gut barrier dysfunction in Nrf2-deficient mice after traumatic brain injury. Cytokine. 2008;44(1):135–40.
Jin W, Wang HD, Hu ZG, Yan W, Chen G, Yin HX. Transcription factor Nrf2 plays a pivotal role in protection against traumatic brain injury-induced acute intestinal mucosal injury in mice. J Surg Res. 2009;157(2):251–60.
Zhou Z, Bian C, Luo Z, Guille C, Ogunrinde E, Wu J, et al. Progesterone decreases gut permeability through upregulating occludin expression in primary human gut tissues and Caco-2 cells. Sci Rep. 2019;9(1):8367.
Zhao XD, Zhou YT. Effects of progesterone on intestinal inflammatory response and mucosa structure alterations following SAH in male rats. J Surg Res. 2011;171(1):e47-53.
Jarras H, Bourque M, Poirier AA, Morissette M, Coulombe K, Di Paolo T, Soulet D. Neuroprotection and immunomodulation of progesterone in the gut of a mouse model of Parkinson’s disease. J Neuroendocrinol. 2020;32(1): e12782.
Graham RM. Adrenergic receptors: structure and function. Cleve Clin J Med. 1990;57(5):481–91.
Bylund DB, Eikenberg DC, Hieble JP, Langer SZ, Lefkowitz RJ, Minneman KP, et al. International union of pharmacology nomenclature of adrenoceptors. Pharmacol Rev. 1994;46(2):121–36.
Loftus TJ, Efron PA, Moldawer LL, Mohr AM. β-blockade use for traumatic injuries and immunomodulation. Shock. 2016;46(4):341–51.
Alali AS, Mukherjee K, McCredie VA, Golan E, Shah PS, Bardes JM, et al. Beta-blockers and traumatic brain injury. Ann Surg. 2017;266(6):952–61.
Chen Z, Tang L, Xu X, Wei X, Wen L, Xie Q. Therapeutic effect of beta-blocker in patients with traumatic brain injury: a systematic review and meta-analysis. J Crit Care. 2017;41:240–6.
Ding H, Liao L, Zheng X, Wang Q, Liu Z, Xu G, et al. beta-Blockers for traumatic brain injury: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2021;90(6):1077–85.
Zagales I, Selvakumar S, Ngatuvai M, Fanfan D, Kornblith L, Santos RG, et al. Beta-blocker therapy in patients with severe traumatic brain injury: a systematic review and meta-analysis. Am Surg. 2023;89(5):2020–9.
Armstead WM, Vavilala MS. Propranolol protects cerebral autoregulation and reduces hippocampal neuronal cell death through inhibition of interleukin-6 upregulation after traumatic brain injury in pigs. Br J Anaesth. 2019;123(5):610–7.
Asmar S, Bible L, Chehab M, Tang A, Khurrum M, Castanon L, et al. Traumatic brain injury induced temperature dysregulation: what is the role of beta blockers? J Trauma Acute Care Surg. 2021;90(1):177–84.
Lopez AJ, ElSaadani M, Jacovides CL, Georges A, Culkin MC, Ahmed S, et al. Beta blockade in TBI: Dose-dependent reductions in BBB leukocyte mobilization and permeability in vivo. J Trauma Acute Care Surg. 2022;92(5):781–91.
Lopez AJ, ElSaadani M, Culkin MC, Jacovides CL, Georges AP, Song H, et al. Persistent blunting of penumbral leukocyte mobilization by beta blockade administered for two weeks after traumatic brain injury. J Surg Res. 2022;280:196–203.
Scharenbrock AR, Katzenberger RJ, Fischer MC, Ganetzky B, Wassarman DA. Beta-blockers reduce intestinal permeability and early mortality following traumatic brain injury in Drosophila. MicroPubl Biol. 2021. https://doi.org/10.17912/micropub.biology.000461.
Singer KE, McGlone ED, Collins SM, Wallen TE, Morris MC, Schuster RM, et al. Propranolol reduces p-tau accumulation and improves behavior outcomes in a polytrauma murine model. J Surg Res. 2023;282:183–90.
Zeeshan M, Hamidi M, O’Keeffe T, Bae EH, Hanna K, Friese RS, et al. Propranolol attenuates cognitive, learning, and memory deficits in a murine model of traumatic brain injury. J Trauma Acute Care Surg. 2019;87(5):1140–7.
Stowell RD, Sipe GO, Dawes RP, Batchelor HN, Lordy KA, Whitelaw BS, et al. Noradrenergic signaling in the wakeful state inhibits microglial surveillance and synaptic plasticity in the mouse visual cortex. Nat Neurosci. 2019;22(11):1782–92.
Ley EJ, Leonard SD, Barmparas G, Dhillon NK, Inaba K, Salim A, et al. Beta blockers in critically ill patients with traumatic brain injury: results from a multicenter, prospective, observational American Association for the Surgery of Trauma study. J Trauma Acute Care Surg. 2018;84(2):234–44.
Khalili H, Ahl R, Paydar S, Sjolin G, Cao Y, Abdolrahimzadeh Fard H, et al. Beta-blocker therapy in severe traumatic brain injury: a prospective randomized controlled trial. World J Surg. 2020;44(6):1844–53.
Lang Y, Fu F, Sun D, Xi C, Chen F. Labetalol prevents intestinal dysfunction induced by traumatic brain injury. PLoS ONE. 2015;10(7): e0133215.
Ide S, Yamamoto R, Takeda H, Minami M. Bidirectional brain-gut interactions: involvement of noradrenergic transmission within the ventral part of the bed nucleus of the stria terminalis. Neuropsychopharmacol Rep. 2018;38(1):37–43.
Dunn-Meynell AA, Yarlagadda Y, Levin BE. Alpha 1-adrenoceptor blockade increases behavioral deficits in traumatic brain injury. J Neurotrauma. 1997;14(1):43–52.
Zimering MB. Repeated traumatic brain injury is associated with neurotoxic plasma autoantibodies directed against the serotonin 2A and alpha 1 adrenergic receptors. Endocrinol Diabetes Metab J. 2023;7(2):1–12.
Sysoev YI, Prikhodko VA, Chernyakov RT, Idiyatullin RD, Musienko PE, Okovityi SV. Effects of alpha-2 adrenergic agonist mafedine on brain electrical activity in rats after traumatic brain injury. Brain Sci. 2021;11(8):981.
Kobori N, Hu B, Dash PK. Altered adrenergic receptor signaling following traumatic brain injury contributes to working memory dysfunction. Neuroscience. 2011;172:293–302.
Singh A, Prajapati HP, Kumar R, Singh NP, Kumar A. Prognostic role of catecholamine in moderate-to-severe traumatic brain injury: a prospective observational cohort study. Asian J Neurosurg. 2022;17(3):435–41.
Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–8.
Asgeirsson B, Grande PO, Nordstrom CH, Berntman L, Messeter K, Ryding E. Effects of hypotensive treatment with alpha 2-agonist and beta 1-antagonist on cerebral haemodynamics in severely head injured patients. Acta Anaesthesiol Scand. 1995;39(3):347–51.
Patel MB, McKenna JW, Alvarez JM, Sugiura A, Jenkins JM, Guillamondegui OD, Pandharipande PP. Decreasing adrenergic or sympathetic hyperactivity after severe traumatic brain injury using propranolol and clonidine (DASH After TBI Study): study protocol for a randomized controlled trial. Trials. 2012;13:177.
Nordness MF, Maiga AW, Wilson LD, Koyama T, Rivera EL, Rakhit S, et al. Effect of propranolol and clonidine after severe traumatic brain injury: a pilot randomized clinical trial. Crit Care. 2023;27(1):228.
Endo A. The discovery and development of HMG-CoA reductase inhibitors. J Lipid Res. 1992;33(11):1569–82.
Diamantis E, Kyriakos G, Quiles-Sanchez LV, Farmaki P, Troupis T. The anti-inflammatory effects of statins on coronary artery disease: an updated review of the literature. Curr Cardiol Rev. 2017;13(3):1.
Heidari B, Babaei M, Yosefghahri B. Prevention of osteoarthritis progression by statins, targeting metabolic and inflammatory aspects: a review. Mediterr J Rheumatol. 2021;32(3):227–36.
Fracassi A, Marangoni M, Rosso P, Pallottini V, Fioramonti M, Siteni S, Segatto M. Statins and the brain: more than lipid lowering agents? Curr Neuropharmacol. 2018;17(1):59–83.
Côté-Daigneault J, Mehandru S, Ungaro R, Atreja A, Colombel J-F. Potential immunomodulatory effects of statins in inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(3):724–32.
Sultan W, Sapkota A, Khurshid H, Qureshi IA, Jahan N, Went TR, et al. Statins’ effect on cognitive outcome after traumatic brain injury. Cureus. 2021. https://doi.org/10.7759/cureus.16953.
Susanto M, Pangihutan Siahaan AM, Wirjomartani BA, Setiawan H, Aryanti C, Michael. The neuroprotective effect of statin in traumatic brain injury: a systematic review. World Neurosurg X. 2023;19:100211.
Wible EF, Laskowitz DT. Statins in traumatic brain injury. Neurotherapeutics. 2010;7(1):62–73.
Lerouet D, Marchand-Leroux C, Besson VC. Neuropharmacology in traumatic brain injury: from preclinical to clinical neuroprotection? Fundam Clin Pharmacol. 2021;35(3):524–38.
Lu D, Goussev A, Chen J, Pannu P, Li Y, Mahmood A, Chopp M. Atorvastatin reduces neurological deficit and increases synaptogenesis, angiogenesis, and neuronal survival in rats subjected to traumatic brain injury. J Neurotrauma. 2004;21(1):21–32.
Schneider EB, Efron DT, MacKenzie EJ, Rivara FP, Nathens AB, Jurkovich GJ. Premorbid statin use is associated with improved survival and functional outcomes in older head-injured individuals. J Trauma. 2011;71(4):815–9.
Farzanegan GR, Derakhshan N, Khalili H, Ghaffarpasand F, Paydar S. Effects of atorvastatin on brain contusion volume and functional outcome of patients with moderate and severe traumatic brain injury; a randomized double-blind placebo-controlled clinical trial. J Clin Neurosci. 2017;44:143–7.
Lu D, Mahmood A, Goussev A, Schallert T, Qu C, Zhang ZG, et al. Atorvastatin reduction of intravascular thrombosis, increase in cerebral microvascular patency and integrity, and enhancement of spatial learning in rats subjected to traumatic brain injury. J Neurosurg. 2004;101(5):813–21.
Qu C, Lu D, Goussev A, Schallert T, Mahmood A, Chopp M. Effect of atorvastatin on spatial memory, neuronal survival, and vascular density in female rats after traumatic brain injury. J Neurosurg. 2005;103(4):695–701.
Abrahamson EE, Ikonomovic MD, Dixon CE, Dekosky ST. Simvastatin therapy prevents brain trauma-induced increases in β-amyloid peptide levels. Ann Neurol. 2009;66(3):407–14.
Li B, Mahmood A, Lu D, Wu H, Xiong Y, Qu C, Chopp M. Simvastatin attenuates microglial cells and astrocyte activation and decreases interleukin-1b level after traumatic brain injury. Neurosurgery. 2009;65(1):179–86.
Sanchez-Aguilar M, Tapia-Perez JH, Sanchez-Rodriguez JJ, Vinas-Rios JM, Martinez-Perez P, de la Cruz-Mendoza E, et al. Effect of rosuvastatin on cytokines after traumatic head injury. J Neurosurg. 2013;118(3):669–75.
Wu H, Mahmood A, Lu D, Jiang H, Xiong Y, Zhou D, Chopp M. Attenuation of astrogliosis and modulation of endothelial growth factor receptor in lipid rafts by simvastatin after traumatic brain injury. J Neurosurg. 2010;113(3):591–7.
Wu H, Lu D, Jiang H, Xiong Y, Qu C, Li B, et al. Simvastatin-mediated upregulation of VEGF and BDNF, activation of the PI3K/Akt pathway, and increase of neurogenesis are associated with therapeutic improvement after traumatic brain injury. J Neurotrauma. 2008;25(2):130–9.
Wu H, Lu D, Jiang H, Xiong Y, Qu C, Li B, et al. Increase in phosphorylation of Akt and its downstream signaling targets and suppression of apoptosis by simvastatin after traumatic brain injury. J Neurosurg. 2008;109(4):691–8.
Beziaud T, Ru Chen X, El Shafey N, Frechou M, Teng F, Palmier B, et al. Simvastatin in traumatic brain injury: effect on brain edema mechanisms. Crit Care Med. 2011;39(10):2300–7.
Senhaji N, Kojok K, Darif Y, Fadainia C, Zaid Y. The contribution of CD40/CD40L axis in inflammatory bowel disease: an update. Front Immunol. 2015;6:164586.
Hu YC, Wang F, Zhang DD, Sun Q, Li W, Dai YX, et al. Expression of intestinal CD40 after experimental traumatic brain injury in rats. J Surg Res. 2013;184(2):1022–7.
Hu Y, Wang X, Ye L, Li C, Chen W, Cheng H. Rosuvastatin alleviates intestinal injury by down-regulating the CD40 pathway in the intestines of rats following traumatic brain injury. Front Neurol. 2020;11:816.
Lee JY, Kim JS, Kim JM, Kim N, Jung HC, Song IS. Simvastatin inhibits NF-kappaB signaling in intestinal epithelial cells and ameliorates acute murine colitis. Int Immunopharmacol. 2007;7(2):241–8.
Mulhaupt F. Statins (HMG-CoA reductase inhibitors) reduce CD40 expression in human vascular cells. Cardiovasc Res. 2003;59(3):755–66.
Ozacmak VH, Sayan H, Igdem AA, Cetin A, Ozacmak ID. Attenuation of contractile dysfunction by atorvastatin after intestinal ischemia reperfusion injury in rats. Eur J Pharmacol. 2007;562(1–2):138–47.
Vieira-Silva S, Falony G, Belda E, Nielsen T, Aron-Wisnewsky J, Chakaroun R, et al. Statin therapy is associated with lower prevalence of gut microbiota dysbiosis. Nature. 2020;581(7808):310–5.
Crockett SD, Hansen RA, Stürmer T, Schectman R, Darter J, Sandler RS, Kappelman MD. Statins are associated with reduced use of steroids in inflammatory bowel disease: a retrospective cohort study*. Inflamm Bowel Dis. 2012;18(6):1048–56.
Santana PT, Rosas SLB, Ribeiro BE, Marinho Y, De Souza HSP. Dysbiosis in inflammatory bowel disease: pathogenic role and potential therapeutic targets. Int J Mol Sci. 2022;23(7):3464.
You W, Zhu Y, Wei A, Du J, Wang Y, Zheng P, et al. Traumatic brain injury induces gastrointestinal dysfunction and dysbiosis of gut microbiota accompanied by alterations of bile acid profile. J Neurotrauma. 2022;39(1–2):227–37.
Simon DW, Rogers MB, Gao Y, Vincent G, Firek BA, Janesko-Feldman K, et al. Depletion of gut microbiota is associated with improved neurologic outcome following traumatic brain injury. Brain Res. 2020;1747: 147056.
McKenzie VJ, Song SJ, Delsuc F, Prest TL, Oliverio AM, Korpita TM, et al. The effects of captivity on the mammalian gut microbiome. Integr Comp Biol. 2017;57(4):690–704.
Horn J, Mayer DE, Chen S, Mayer EA. Role of diet and its effects on the gut microbiome in the pathophysiology of mental disorders. Transl Psychiatry. 2022;12(1):164.
George AK, Behera J, Homme RP, Tyagi N, Tyagi SC, Singh M. Rebuilding microbiome for mitigating traumatic brain injury: importance of restructuring the gut-microbiome-brain axis. Mol Neurobiol. 2021;58(8):3614–27.
Gou H-Z, Zhang Y-L, Ren L-F, Li Z-J, Zhang L. How do intestinal probiotics restore the intestinal barrier? Front Microbiol. 2022;13:929346.
Yu XY, Yin HH, Zhu JC. Increased gut absorptive capacity in rats with severe head injury after feeding with probiotics. Nutrition. 2011;27(1):100–7.
Ma Y, Liu T, Fu J, Fu S, Hu C, Sun B, et al. Lactobacillus acidophilus exerts neuroprotective effects in mice with traumatic brain injury. J Nutr. 2019;149(9):1543–52.
Sun B, Hu C, Fang H, Zhu L, Gao N, Zhu J. The effects of Lactobacillus acidophilus on the intestinal smooth muscle contraction through PKC/MLCK/MLC signaling pathway in TBI mouse model. PLoS ONE. 2015;10(6): e0128214.
Brenner LA, Forster JE, Stearns-Yoder KA, Stamper CE, Hoisington AJ, Brostow DP, et al. Evaluation of an immunomodulatory probiotic intervention for veterans with co-occurring mild traumatic brain injury and posttraumatic stress disorder: a pilot study. Front Neurol. 2020;11:546517.
Du T, Jing X, Song S, Lu S, Xu L, Tong X, Yan H. Therapeutic effect of enteral nutrition supplemented with probiotics in the treatment of severe craniocerebral injury: a systematic review and meta-analysis. World Neurosurg. 2020;139:e553–71.
Silva YP, Bernardi A, Frozza RL. The role of short-chain fatty acids from gut microbiota in gut-brain communication. Front Endocrinol. 2020;11:508738.
O’Riordan KJ, Collins MK, Moloney GM, Knox EG, Aburto MR, Fulling C, et al. Short chain fatty acids: microbial metabolites for gut-brain axis signalling. Mol Cell Endocrinol. 2022;546: 111572.
Cheng Y, Liu J, Ling Z. Short-chain fatty acids-producing probiotics: a novel source of psychobiotics. Crit Rev Food Sci Nutr. 2022;62(28):7929–59.
Li H, Sun J, Du J, Wang F, Fang R, Yu C, et al. Clostridium butyricum exerts a neuroprotective effect in a mouse model of traumatic brain injury via the gut-brain axis. Neurogastroenterol Motil. 2018;30(5): e13260.
Tan M, Zhu J-C, Du J, Zhang L-M, Yin H-H. Effects of probiotics on serum levels of Th1/Th2 cytokine and clinical outcomes in severe traumatic brain-injured patients: a prospective randomized pilot study. Crit Care. 2011;15(6):R290.
Liu J, Tan Y, Cheng H, Zhang D, Feng W, Peng C. Functions of gut microbiota metabolites, current status and future perspectives. Aging Dis. 2022;13(4):1106–26.
Cavaleri F, Bashar E. Potential synergies of beta-hydroxybutyrate and butyrate on the modulation of metabolism, inflammation, cognition, and general health. J Nutr Metab. 2018;2018:7195760.
Opeyemi OM, Rogers MB, Firek BA, Janesko-Feldman K, Vagni V, Mullett SJ, et al. Sustained dysbiosis and decreased fecal short-chain fatty acids after traumatic brain injury and impact on neurologic outcome. J Neurotrauma. 2021;38(18):2610–21.
Grant SM, DeMorrow S. Bile acid signaling in neurodegenerative and neurological disorders. Int J Mol Sci. 2020;21(17):5982.
Wu H, Yu N, Wang X, Yang Y, Liang H. Tauroursodeoxycholic acid attenuates neuronal apoptosis via the TGR5/ SIRT3 pathway after subarachnoid hemorrhage in rats. Biol Res. 2020;53(1):56.
Rodrigues CM, Spellman SR, Sola S, Grande AW, Linehan-Stieers C, Low WC, Steer CJ. Neuroprotection by a bile acid in an acute stroke model in the rat. J Cereb Blood Flow Metab. 2002;22(4):463–71.
Zhu Y, Zheng P, Lin Y, Wang J, You W, Wang Y, et al. The alteration of serum bile acid profile among traumatic brain injury patients: a small-scale prospective study. J Clin Biochem Nutr. 2023;73(1):97–102.
Das A, O’Herlihy E, Shanahan F, O’Toole PW, Jeffery IB. The fecal mycobiome in patients with Irritable Bowel syndrome. Sci Rep. 2021;11(1):124.
Hoarau G, Mukherjee PK, Gower-Rousseau C, Hager C, Chandra J, Retuerto MA, et al. Bacteriome and mycobiome interactions underscore microbial dysbiosis in familial Crohn’s disease. MBio. 2016;7(5):10.
Coker OO, Nakatsu G, Dai RZ, Wu WKK, Wong SH, Ng SC, et al. Enteric fungal microbiota dysbiosis and ecological alterations in colorectal cancer. Gut. 2019;68(4):654–62.
Botschuijver S, Roeselers G, Levin E, Jonkers DM, Welting O, Heinsbroek SEM, et al. Intestinal fungal dysbiosis is associated with visceral hypersensitivity in patients with irritable bowel syndrome and rats. Gastroenterology. 2017;153(4):1026–39.
Park G, Munley JA, Kelly LS, Kannan KB, Mankowski RT, Sharma A, et al. Gut mycobiome dysbiosis after sepsis and trauma. Crit Care. 2024;28(1):18.
Huang P, Liu M, Zhang J, Zhong X, Zhong C. YTHDF1 attenuates TBI-induced brain-gut axis dysfunction in mice. Int J Mol Sci. 2023;24(4):4240.
Mahajan C, Khurana S, Kapoor I, Sokhal S, Kumar S, Prabhakar H, et al. Characteristics of gut microbiome after traumatic brain injury. J Neurosurg Anesthesiol. 2023;35(1):86–90.
Pathare N, Sushilkumar S, Haley L, Jain S, Osier NN. The impact of traumatic brain injury on microbiome composition: a systematic review. Biol Res Nurs. 2020;22(4):495–505.
Ritter K, Somnuke P, Hu L, Griemert EV, Schafer MKE. Current state of neuroprotective therapy using antibiotics in human traumatic brain injury and animal models. BMC Neurosci. 2024;25(1):10.
Yanckello LM, Fanelli B, McCulloch S, Xing X, Sun M, Hammond TC, et al. Inulin supplementation mitigates gut dysbiosis and brain impairment induced by mild traumatic brain injury during chronic phase. J Cell Immunol. 2022;4(2):50–64.
Davis BT, Chen Z, Islam M, Timken ME, Procissi D, Schwulst SJ. Fecal microbiota transfer attenuates gut dysbiosis and functional deficits after traumatic brain injury. Shock. 2022;57(6):251–9.
Marut D, Shammassian B, McKenzie C, Adamski J, Traeger J. Evaluation of prophylactic antibiotics in penetrating brain injuries at an academic level 1 trauma center. Clin Neurol Neurosurg. 2020;193: 105777.
Flanagan CD, Vallier HA. The polytraumatized patient. In: Flanagan CD, editor. Textbook of musculoskeletal disorders. Rome: Springer; 2023. p. 26–72.
Kim D, Hofstaedter CE, Zhao C, Mattei L, Tanes C, Clarke E, et al. Optimizing methods and dodging pitfalls in microbiome research. Microbiome. 2017;5(1):52.
Singh RK, Chang HW, Yan D, Lee KM, Ucmak D, Wong K, et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017;15(1):73.
Knight R, Vrbanac A, Taylor BC, Aksenov A, Callewaert C, Debelius J, et al. Best practices for analysing microbiomes. Nat Rev Microbiol. 2018;16(7):410–22.
Zhu S, Jiang Y, Xu K, Cui M, Ye W, Zhao G, et al. The progress of gut microbiome research related to brain disorders. J Neuroinflammation. 2020;17(1):25.
Armistead-Jehle P, Soble JR, Cooper DB, Belanger HG. Unique aspects of traumatic brain injury in military and veteran populations. Phys Med Rehabil Clin N Am. 2017;28(2):323–37.
Liu Q, Wang Z, Sun S, Nemes J, Brenner LA, Hoisington A, et al. Association of blast exposure in military breaching with intestinal permeability blood biomarkers associated with leaky gut. Int J Mol Sci. 2024;25(6):3549.
Li Y, Pagulayan K, Rau H, Hendrickson R, Schindler A. Association between gut microbiome composition and symptom self-report in trauma exposed OEF/OIF/OND Veterans. medRxiv. 2023. https://doi.org/10.1101/2023.11.01.23297931.
Janulewicz PA, Seth RK, Carlson JM, Ajama J, Quinn E, Heeren T, et al. The gut-microbiome in gulf war veterans: a preliminary report. Int J Environ Res Public Health. 2019;16(19):3751.
Stanislawski MA, Stamper CE, Stearns-Yoder KA, Hoisington AJ, Brostow DP, Forster JE, et al. Characterization of the gut microbiota among Veterans with unique military-related exposures and high prevalence of chronic health conditions: a United States-Veteran Microbiome Project (US-VMP) study. Brain Behav Immun Health. 2021;18: 100346.
Brenner LA, Stamper CE, Hoisington AJ, Stearns-Yoder KA, Stanislawksi MA, Brostow DP, et al. Microbial diversity and community structures among those with moderate to severe TBI: a United States-Veteran microbiome project study. J Head Trauma Rehabil. 2020;35(5):332–41.
Varanoske AN, McClung HL, Sepowitz JJ, Halagarda CJ, Farina EK, Berryman CE, et al. Stress and the gut-brain axis: cognitive performance, mood state, and biomarkers of blood-brain barrier and intestinal permeability following severe physical and psychological stress. Brain Behav Immun. 2022;101:383–93.
El-Swaify ST, Refaat MA, Ali SH, Abdelrazek AEM, Beshay PW, Kamel M, et al. Controversies and evidence gaps in the early management of severe traumatic brain injury: back to the ABCs. Trauma Surg Acute Care Open. 2022;7(1): e000859.
Alves JL, Rato J, Silva V. Why does brain trauma research fail? World Neurosurg. 2019;130:115–21.
Thapa K, Khan H, Singh TG, Kaur A. Traumatic brain injury: mechanistic insight on pathophysiology and potential therapeutic targets. J Mol Neurosci. 2021;71(9):1725–42.
Zhao Q, Zhang J, Li H, Li H, Xie F. Models of traumatic brain injury-highlights and drawbacks. Front Neurol. 2023;14:1151660.
Mendez MF, Owens EM, Reza Berenji G, Peppers DC, Liang LJ, Licht EA. Mild traumatic brain injury from primary blast vs. blunt forces: post-concussion consequences and functional neuroimaging. NeuroRehabilitation. 2013;32(2):397–407.
Sussman ES, Pendharkar AV, Ho AL, Ghajar J. Mild traumatic brain injury and concussion: terminology and classification. Handb Clin Neurol. 2018;158:21–4.
Gupte R, Brooks W, Vukas R, Pierce J, Harris J. Sex differences in traumatic brain injury: what we know and what we should know. J Neurotrauma. 2019;36(22):3063–91.
Rubin TG, Lipton ML. Sex differences in animal models of traumatic brain injury. J Exp Neurosci. 2019;13:1179069519844020.
Shobeiri P, Kalantari A, Teixeira AL, Rezaei N. Shedding light on biological sex differences and microbiota-gut-brain axis: a comprehensive review of its roles in neuropsychiatric disorders. Biol Sex Differ. 2022;13(1):12.
Jasarevic E, Morrison KE, Bale TL. Sex differences in the gut microbiome-brain axis across the lifespan. Philos Trans R Soc Lond B Biol Sci. 2016;371(1688):20150122.
Haro C, Rangel-Zuniga OA, Alcala-Diaz JF, Gomez-Delgado F, Perez-Martinez P, Delgado-Lista J, et al. Intestinal microbiota is influenced by gender and body mass index. PLoS ONE. 2016;11(5): e0154090.
Mueller S, Saunier K, Hanisch C, Norin E, Alm L, Midtvedt T, et al. Differences in fecal microbiota in different European study populations in relation to age, gender, and country: a cross-sectional study. Appl Environ Microbiol. 2006;72(2):1027–33.
Markle JG, Frank DN, Mortin-Toth S, Robertson CE, Feazel LM, Rolle-Kampczyk U, et al. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science. 2013;339(6123):1084–8.
Yurkovetskiy L, Burrows M, Khan AA, Graham L, Volchkov P, Becker L, et al. Gender bias in autoimmunity is influenced by microbiota. Immunity. 2013;39(2):400–12.
Meleine M, Matricon J. Gender-related differences in irritable bowel syndrome: potential mechanisms of sex hormones. World J Gastroenterol. 2014;20(22):6725–43.
Das M, Mohapatra S, Mohapatra SS. New perspectives on central and peripheral immune responses to acute traumatic brain injury. J Neuroinflammation. 2012;9:236.
McKee CA, Lukens JR. Emerging roles for the immune system in traumatic brain injury. Front Immunol. 2016;7:556.
Jassam YN, Izzy S, Whalen M, McGavern DB, El Khoury J. Neuroimmunology of traumatic brain injury: time for a paradigm shift. Neuron. 2017;95(6):1246–65.
Wu J, Vodovotz Y, Abdelhamid S, Guyette FX, Yaffe MB, Gruen DS, et al. Multi-omic analysis in injured humans: patterns align with outcomes and treatment responses. Cell Rep Med. 2021;2(12): 100478.
Mohamadpour M, Whitney K, Bergold PJ. The importance of therapeutic time window in the treatment of traumatic brain injury. Front Neurosci. 2019;13:07.
Sullivan PG, Sebastian AH, Hall ED. Therapeutic window analysis of the neuroprotective effects of cyclosporine A after traumatic brain injury. J Neurotrauma. 2011;28(2):311–8.
Sosin DM, Sniezek JE, Thurman DJ. Incidence of mild and moderate brain injury in the United States, 1991. Brain Inj. 1996;10(1):47–54.
Tanielian TL. Invisible wounds of war psychological and cognitive injuries, their consequences, and services to assist recovery. Santa Monica: Rand Corporation; 2008.
Demakis GJ, Rimland CA. Untreated mild traumatic brain injury in a young adult population. Arch Clin Neuropsychol. 2010;25(3):191–6.
Schumacher M, Denier C, Oudinet JP, Adams D, Guennoun R. Progesterone neuroprotection: the background of clinical trial failure. J Steroid Biochem Mol Biol. 2016;160:53–66.
Stein DG, Howard RB, Sayeed I. Why did the phase III clinical trials for progesterone in TBI fail? An analysis of three potentially critical factors. In: Stein DG, editor. New therapeutics for traumatic brain injury. Amsterdam: Elsevier; 2017. p. 3–18.
Galgano M, Toshkezi G, Qiu X, Russell T, Chin L, Zhao LR. Traumatic brain injury: current treatment strategies and future endeavors. Cell Transpl. 2017;26(7):1118–30.
Dale HF, Rasmussen SH, Asiller OO, Lied GA. Probiotics in irritable bowel syndrome: an up-to-date systematic review. Nutrients. 2019;11(9):2048.
Rogers MB, Simon D, Firek B, Silfies L, Fabio A, Bell MJ, et al. Temporal and spatial changes in the microbiome following pediatric severe traumatic brain injury. Pediatr Crit Care Med. 2022;23(6):425–34.
Giacino JT, Whyte J, Bagiella E, Kalmar K, Childs N, Khademi A, et al. Placebo-controlled trial of amantadine for severe traumatic brain injury. N Engl J Med. 2012;366(9):819–26.
Bonds B, Dhanda A, Wade C, Diaz C, Massetti J, Stein DM. Prognostication of mortality and long-term functional outcomes following traumatic brain injury: can we do better? J Neurotrauma. 2021;38(8):1168–76.
Abbott receives FDA clearance for whole blood rapid test to help with assessment of concussion at the patient’s bedside. Abbott MediaRoom. 2024. https://abbott.mediaroom.com/2024-04-01-Abbott-Receives-FDA-Clearance-for-Whole-Blood-Rapid-Test-to-Help-with-Assessment-of-Concussion-at-the-Patients-Bedside. Accessed 11 Apr 2024.
Edwards P, Arango M, Balica L, Cottingham R, El-Sayed H, Farrell B, et al. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injury-outcomes at 6 months. Lancet. 2005;365(9475):1957–9.
Annahazi A, Schemann M. The enteric nervous system: “A little brain in the gut.” Neuroforum. 2020;26(1):31–42.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
M.G. El Baassiri and I.W. Nasr conceptualized the review and prepared the manuscript. Z. Raouf, S. Badin and A. Escobosa assisted in preparing the manuscript. M.G. El Baassiri, C.P. Sodhi and I.W. Nasr made critical suggestions, reviewed, and prepared the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Animal Care and Use Committee (IACUC) approved animal protocol (Protocol # MO22M233), and experiments have been carried out in strict adherence to the National Institutes of Health Guidelines for the Use of Laboratory Animals.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
El Baassiri, M.G., Raouf, Z., Badin, S. et al. Dysregulated brain-gut axis in the setting of traumatic brain injury: review of mechanisms and anti-inflammatory pharmacotherapies. J Neuroinflammation 21, 124 (2024). https://doi.org/10.1186/s12974-024-03118-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-024-03118-3