Abstract
Traumatic brain injury is common, and often results in debilitating consequences. Even mild traumatic brain injury leaves approximately 20% of patients with symptoms that persist for months. Despite great clinical need there are currently no approved pharmaceutical interventions that improve outcomes after traumatic brain injury. Increased understanding of the endocannabinoid system in health and disease has accompanied growing evidence for therapeutic benefits of Cannabis sativa. This has driven research of Cannabis’ active chemical constituents (phytocannabinoids), alongside endogenous and synthetic counterparts, collectively known as cannabinoids. Also of therapeutic interest are other Cannabis constituents, such as terpenes. Cannabinoids interact with neurons, microglia, and astrocytes, and exert anti-inflammatory and neuroprotective effects which are highly desirable for the management of traumatic brain injury. In this review, we comprehensively appraised the relevant scientific literature, where major and minor phytocannabinoids, terpenes, synthetic cannabinoids, and endogenous cannabinoids were assessed in TBI, or other neurological conditions with pathology and symptomology relevant to TBI, as well as recent studies in preclinical TBI models and clinical TBI populations.
Similar content being viewed by others
Traumatic brain injury
Traumatic brain injury (TBI) is a common event associated with motor vehicle accidents, sports, assaults, and intimate partner violence [1,2,3]. TBI is caused by an impact and/or rotational force applied to the head which may cause alteration in consciousness alongside a range of symptoms in physical, cognitive, emotional or sleep-related domains [4,5,6]. TBI occurs on a severity spectrum of mild to severe injury. Those at the severe end of this spectrum often experience substantial impairment which may impede ability to work or study; reduce quality of life; and incur significant financial burden [7,8,9]. While the majority of TBIs are mild (mTBI, also known as concussion), 10–20% of mTBI patients experience persistent neurological deficits for months or years in a clinical presentation called persisting post-concussive symptoms [10,11,12]. The long-term outcomes of repeated mTBI, such as may occur over an athletic career, have been reported to include risk of cognitive impairment, depression, and motor deficits persisting years to decades post-injury [12,13,14,15,16], although the quality of evidence is such that further work is needed. Repeated mTBI is also associated with chronic traumatic encephalopathy, a neurodegenerative disorder which relies on post-mortem diagnosis but may share clinical signs and symptoms with Alzheimer’s and Parkinson’s diseases [17]. These clinical findings have also been observed in animal studies, with repeated mTBI associated with worse outcomes in a variety of preclinical models [18,19,20,21,22,23]. Despite concerted efforts, the only treatment options for TBI include symptom management and cognitive therapies [24]. There are currently no effective pharmaceutical treatment options to improve outcomes for TBI of any severity despite great clinical need.
The field of cannabinoid research has developed rapidly, and the rationale for use of cannabinoids in the management of neurological conditions such as TBI is increasingly recognized. This review provides a brief overview of the endocannabinoid system in the central nervous system (CNS); introduces cannabinoids; and summarizes the putative benefits of endogenous, plant-derived, and synthetic compounds in TBI models, or models with pathology relevant to TBI. Finally, clinical studies on phytocannabinoids and synthetic cannabinoids in TBI are reviewed.
The endocannabinoid system
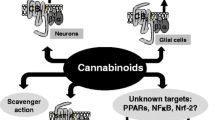
The major constituents of the endocannabinoid system are endogenous neurotransmitters collectively known as endocannabinoids, and two key cannabinoid receptors. The two most well-characterized endocannabinoids are N-arachidonylethanolamine (also known as anandamide; AEA) and 2-arachydonoyl glycerol (2-AG) [25], although the endocannabinoid system continues to expand as research progresses [26]. The two key endocannabinoid receptors are cannabinoid receptor 1 (CB1R) and cannabinoid receptor 2 (CB2R) [27, 28]. Both CB1R and CB2R are G-protein coupled receptors that, when activated, inhibit voltage-gated N-type and P/Q-type Ca2+ channels [29]. In the CNS, CB1R is expressed on neurons at the presynaptic terminal and on astrocytes, while CB2R is expressed on microglia, the resident macrophage/monocyte immune cells of the brain [28, 30]. In addition to these two major cannabinoid receptors (CB1R and CB2R), other receptors are involved in the endocannabinoid system, with the extent and significance of their roles still emerging (recently reviewed by Cristino and colleagues) [26]. The most notable of these additional receptors are: transient receptor potential vanilloid-1 (TRPV1), various G-protein-coupled receptors (GPR55, GPR13, GPR6, GPR12, GPR18), peroxisome proliferator-activated receptor-γ (PPARγ), serotonin receptors (5-HT1A), and adenosine receptors (A2A) [26, 28]. Of these, TRPV1 and PPARγ are most likely of relevance to TBI treatment due to the known roles of TRPV1 in pain management, and PPARγ in inflammation and neurodegeneration [31, 32].
A well-established role of the endocannabinoid system in the CNS is the suppression of both excitatory and inhibitory signaling in an activity-dependent manner, an effect mediated by AEA and 2-AG binding to CB1R in neurons [33,34,35,36]. The production of AEA and 2-AG is initiated by increased cellular firing rates and the associated elevation of intracellular Ca2+ levels within the postsynaptic neuron [34, 36]. AEA and 2-AG are then released from the postsynaptic cell membrane to bind CB1R on the presynaptic membrane, subsequently blocking Ca2+ channels to inhibit further neurotransmitter release. This is known as inhibitory retrograde neuromodulation [26, 36]. The ‘on-demand’ production of endocannabinoids allows them to act as a negative feedback mechanism in response to high levels of neural activity, a phenomenon known as depolarization-induced suppression of excitation, or depolarization-induced suppression of inhibition, depending on whether the presynaptic neuron is excitatory or inhibitory, respectively [33]. This is relevant to TBI, where increased cellular firing and excitotoxicity are prominent pathological events, and suppression of these effects may be neuroprotective [37].
Another important role of the endocannabinoid system in the CNS relates to participation in an endogenous injury response system mediated by CB2R located on microglia [38]. This is evidenced by increased upregulation of the CB2R in injured brain parenchyma in the hours and days following injury [38]. Endocannabinoid concentrations are also elevated after injury, with increased 2-AG hypothesized to protect the blood–brain barrier (BBB) and inhibit the expression of pro-inflammatory cytokines, regulating the inflammatory response [39, 40]. As a whole, emerging evidence supports the role of the endocannabinoid system as a compensatory, neuroprotective, injury-response system after TBI. Manipulation of this system through administration of exogenous compounds or modulation of endogenous factors is emerging as an attractive therapeutic strategy for TBI.
Cannabinoids and related compounds
In addition to the endogenous neurotransmitters produced in the mammalian nervous system (AEA and 2-AG, described above), exogenous compounds also influence the endocannabinoid system. Collectively, these are known as cannabinoids and they may be endogenous (endocannabinoids), derived from the Cannabis plant (phytocannabinoids), or synthetic (synthetic cannabinoids).
Phytocannabinoids and terpenes
Phytocannabinoids are naturally occurring compounds isolated from the Cannabis sativa plant with biological activity within the endocannabinoid system [41]. The major phytocannabinoids are ∆9-tetrahydrocannabinol (THC) and cannabidiol (CBD).
THC is the most well-known phytocannabinoid and the main psychoactive constituent of the cannabis plant [35]. The pharmacological activity of THC is similar to that of endocannabinoid AEA, whereby it acts as a partial agonist at CB1R and CB2R [29, 35, 42]. In addition, similar to AEA, THC administration suppresses neuronal firing at the presynaptic level [43, 44]. Notably, two synthetic THC compounds are approved by the FDA for medical use in the United States: nabilone (marketed as Cesamet, a synthetic THC derivative) and dronabinol (marketed as Marinol, synthetic THC). Both are indicated for chemotherapy-induced nausea and vomiting, with dronabinol also used to treat anorexia in patients with AIDS [29, 45,46,47]. Although it is possible that THC could limit nausea and vomiting within the context of acute TBI, THC has also been directly studied in models of TBI pathology and indirectly in some clinical TBI populations with encouraging results for therapeutic potential beyond the context of nausea (refer to Tables 2 and 4).
The other major cannabis constituent, CBD, possesses complex pharmacology which continues to be the focus of emerging research. CBD is generally regarded as an antagonist of CB1R and an inverse agonist of CB2R [35, 48], although other reports describe CBD as a negative allosteric modulator of CB1R [49, 50]. CBD also potentiates the effects of endocannabinoid AEA by inhibiting fatty acid amide hydrolase (FAAH), the enzyme responsible for AEA degradation [29]. This is relevant to TBI, because FAAH inhibitors restore BBB integrity and improve motor, cognitive and mood-related outcomes in models of TBI [51,52,53]. In addition, a variety of other receptor–ligand interactions within the extended endocannabinoid system have been characterized [29]. CBD is a direct agonist at serotonin 5-HT1A receptors (with implications for mood and anxiety-like effects), a weak agonist at TRPV1 receptors (with implications for pain and synaptic plasticity), a PPARγ agonist (with implications for neurodegeneration and inflammation), and an indirect agonist at adenosine (A2A) receptors [28, 42]. The effects of CBD at these receptors may confer benefits in TBI, particularly PPARγ activation which reduces neurodegeneration and inflammation [31].
While THC and CBD are the most abundant and well-studied phytocannabinoids, Cannabis sativa contains over 140 minor phytocannabinoids and other pharmacologically active compounds [29, 42]. These minor phytocannabinoids are naturally present in the Cannabis plant, and understanding their effects is integral to realizing the therapeutic potential of Cannabis, as well as to guide the utilization of full spectrum, plant-derived treatments, or design compound blends for medicinal purposes. While research on minor cannabinoids has increased, there is still very little known regarding their effects in normal physiology and disease, including TBI.
In addition to phytocannabinoids, the cannabis plant contains compounds known as terpenes, some of which also possess biological activity with potential therapeutic benefits [54,55,56]. Terpenes are naturally occurring, potent hydrocarbons found in a variety of botanical sources, including Cannabis. They are responsible for the odors and flavors associated with Cannabis and various terpenes are used as food additives that are generally recognized as safe by the US Food and Drug Administration [54]. Terpenes commonly associated with Cannabis include β-caryophyllene, myrcene, limonene, linalool, terpineol, γ-terpinene, α-pinene, β-pinene, nerolidol, phytol, and citral, although this is not an exhaustive list [54,55,56]. The role that terpenes play in the medicinal effects of cannabis, and how these interact with other biologically active plant constituents is of interest for optimizing their therapeutic potential [56].
Cannabis plant-derived extracts have proven attractive options for therapeutic development, with two botanically derived cannabis products approved for medical use by the Federal Drug Administration in the United States. These are Sativex®, a blend of high THC and high CBD plant extracts in a 1:1 ratio for the treatment of pain and spasticity in Multiple Sclerosis, and Epidiolex®, a pure CBD extract for severe forms of epilepsy [33]. The clinical success of Epidiolex and Sativex are encouraging for future application of cannabis extracts in other conditions, such as TBI.
Synthetic cannabinoids
In addition to endogenous and plant derived compounds, synthetic cannabinoids are not naturally occurring, but rather produced through lab-based synthesis. Synthetic cannabinoids may be derived from naturally occurring cannabinoids; interact with endogenous cannabinoid receptors; or otherwise resemble endocannabinoids and phytocannabinoids [41]. Synthetic cannabinoids may differ from their endogenous and plant-derived counterparts by affecting distinct receptors, or by achieving different levels of potency or binding specificity than naturally occurring cannabinoids [57, 58]. To summarize, cannabinoids are a diverse class of molecules produced through natural and synthetic means which possess biological activity within the endocannabinoid system.
Preclinical research of cannabinoids in tbi and related models
Several endogenous, plant-derived, and synthetic cannabinoids have been explored in a variety of preclinical TBI and TBI-related models, such as spinal cord injury and stroke, and these are reviewed below. Additional compounds that have not been assessed directly in TBI, but have displayed promising effects in TBI-relevant pathologies are also reviewed.
Endocannabinoids in TBI and related conditions
The neuroprotective role of endocannabinoids and the endocannabinoid system in TBI is supported by emerging preclinical research in a variety of TBI models (Table 1). For example, in a mouse model of closed-head TBI, synthetic 2-AG administration reduced edema and infarct volume; mitigated cell death in the hippocampus; and improved functional recovery. These effects were CB1R-dependent, supporting a protective role for the endocannabinoid system in response to injury [39]. These neuroprotective effects were further demonstrated in a study which potentiated 2-AG effects through inhibition of its degrading enzyme monoacylglycerol lipase (MAGL) in the controlled cortical impact (CCI) model [59]. In this study, administration of the MAGL inhibitor MJN110 in CCI mice after injury reduced inflammatory markers; attenuated cell death; restored glutamate and GABA receptors changes; and improved cognitive and locomotor behaviors [59]. In a repeated mTBI mouse model, knockout of astrocyte-specific MAGL reduced neuroinflammation; attenuated TBI-induced gene expression changes; and prevented neurodegenerative pathology and cognitive impairment, among other injury-induced effects. Again, these benefits were mediated by CB1R [60]. Similarly, administration of FAAH inhibitor URB597 was neuroprotective in an oxygen–glucose deprivation model of injury, with anti-oxidant, anti-inflammatory, and anti-apoptotic effects [61]. Finally, in a model of kainic acid-induced excitotoxicity, AEA rapidly increased in the hippocampus, conferring neuroprotection in a CB1R-dependent manner [34, 40]. These findings support the neuroprotective effects of the endocannabinoid system in response to injury, and demonstrate that endocannabinoid augmentation or supplementation may have therapeutic benefits in TBI.
Major phytocannabinoids in TBI models
Few preclinical studies have directly assessed the major constituent phytocannabinoids in models of TBI, although the available data are encouraging (Table 2). In a weight-drop mTBI mouse model, injury resulted in impaired sociability, heightened aggression, and tactile allodynia 14 days later, all of which were improved by daily oral treatment with 10% CBD oil for either 14 days, or from days 50–60 post-injury [62]. In this same study, mTBI increased levels of D-aspartate, glutamate and GABA in the medial prefrontal cortex, and CBD treatment ameliorated these changes [62]. In a rat weight-drop with craniotomy model of TBI (modified Feeney’s model), CBD (10 mg/kg) was administered both 30 min before injury and 6 h post-injury [63]. The authors demonstrated beneficial effects on BBB integrity, whereby CBD treatment reduced aquaporin-4 expression and increased expression of claudin-5 and occludin, with BBB leakage directly observed using Evan’s Blue assay. CBD treatment was also found to decrease GFAP expression, and reduced concentrations of the proinflammatory mediators TNF-α and IL-1β compared to control [63]. In rats with moderate TBI (CCI model), Friedman and colleagues [64] applied several high CBD, low THC botanical preparations directly to the open skull, over the dura above the injury site via a gelfoam matrix after injury. Additional groups received the cannabinoid gelfoam matrix as well as systemic administration of CBD 10 min after injury, and on 14 non-consecutive days thereafter [64]. The combination of gelfoam and systemic injection was more effective than gelfoam or systemic administration alone, with decreased defecation scores (an anxiety-like measure), smaller lesion volumes, reduced hippocampal neuron loss and neural pathology [64]. This combination treatment also had anti-inflammatory effects, indicated by reduced GFAP immunoreactivity, with concomitant improvements in motor and cognitive function [64]. While the gelfoam preparation may not be suitable for all types of TBI, it may be a useful strategy in the context of penetrating head wounds [64]. In conclusion, these studies demonstrate increasing evidence that CBD treatment is multifunctional, with beneficial effects on inflammation, cognition, neurobehavioral deficits, lesion volumes and BBB breach after TBI.
The available data on THC treatment in TBI models are more nuanced than that of CBD, with sex and timing emerging as important variables. In a repeated injury weight-drop model in rats, THC (1.25 mg/kg, i.p.) was administered as six intermittent pre-injury treatments or 12 consecutive post-injury treatments. The post-injury THC treatment improved anxiety-like behavior in the elevated plus maze, but not in the open field task [65]. Depression-like behavior in the forced swim task was also improved in male rats treated post-injury with THC, although a more severe depression-like phenotype was seen in females [65]. In the same study, THC treatment post-injury also prevented telomere shortening after repeated mTBI [65]. Consistent with prior studies [22, 66], the authors found that repeated mTBI increased microglial activation. However, they did not observe an effect of THC treatment on microglial activation in limbic system structures (the hippocampus and nucleus accumbens). Rather, THC increased IBA1 immunoreactivity in the prefrontal cortex, implying THC may not have a therapeutic effect on this measure of neuroinflammation [65]. In a similar rat model with a single weight-drop mTBI, a single injection of THC (1 mg/kg, i.p.) did not improve TBI-induced deficits in motor function, and treatment impaired motor function in sham-injured controls, though this was only seen in males [67]. Other sex-specific effects of THC included increased levels of cytokine interleukin-6 after TBI in males only, while female TBI rats that received THC had a reduced density of CB1R compared to those that received THC, but no injury [67]. This indicates that THC effects are sex-specific in both uninjured and TBI conditions, with variable effects on behavior outcomes, inflammatory responses, and alterations to the endocannabinoid system [67]. In contrast, in a mouse CCI model of TBI that assessed males only, THC treatment (3 mg/kg, i.p., daily for 3 days) improved motor function in the RotaRod test, although this difference may be due to dose and treatment frequency as both were greater than the previously mentioned study in rats. This improved motor performance was accompanied by upregulated brain-derived neurotrophic factor and glial-derived neurotrophic factor, which are associated with neuronal and glial repair, respectively, in different brain regions [68]. THC treatment was also associated with increased 2-AG levels in the brain and improved short term working memory in the spontaneous alternation Y-maze test [69]. These studies are encouraging for the potential application of THC in the management of TBI, though further research is necessary to investigate appropriate dosing regimens and determine sex-specific effects, particularly with regard to neuroinflammation.
Major phytocannabinoids in TBI-related conditions
In addition to the limited studies that directly assessed TBI models, models of CNS injury with related pathology such as spinal cord injury (SCI) and stroke further support the therapeutic potential of phytocannabinoid treatment in neurotrauma. In a spinal cord contusion model, CBD treatment (1.5 mg/kg; i.p.) was administered repeatedly post-injury 1 h, 24 h, and 3 days later, then continued twice per week until the end of the experiment [70]. This treatment reduced expression of inflammatory cell markers in the spinal cord, and improved thermal sensitivity after SCI. However, locomotor and bladder function were not affected by CBD treatment [70]. CBD has also been assessed in stroke models, such as the carotid artery occlusion model. CBD (10 mg/kg) administered 30 min before, and three, 24 and 48 h post-stroke, ameliorated anxiety-like behavior, depression-like behavior, and cognitive impairment observed in this model, as well as prevented neurodegeneration in the hippocampus and white matter loss in the corpus callosum. CBD treatment also prevented artery occlusion-induced microglial activation in several areas of the hippocampus (CA1, CA2/3, but not CA4) [71]. These studies offer additional support for phytocannabinoids as treatments for CNS injury.
Minor phytocannabinoids in TBI-related conditions
The pharmacology of minor cannabinoids and their potential therapeutic effects is an area of active research. While much of this research is ongoing, notable minor cannabinoids with potential neuroprotective properties have been recently reviewed (see Stone et al. [88]). Notably, no studies of minor constituent cannabinoids in TBI models have been conducted to date, though effects on neurodegeneration and inflammation are relevant to TBI and in vivo studies are briefly summarized here.
∆9-Tetrahydrocannabivarin (THCV) is generally considered to have minor effects as a CB1 antagonist in vivo, and has high-affinity for CB2R, where it acts as a partial agonist, though it has recently been described as an agonist at both CB1R and CB2R [42, 72]. With this pharmacological profile, THCV could have similar effects as THC and CBD in TBI, though direct studies are required for confirmation. THCV also acts through 5-HT1A receptors and shows promise as an antipsychotic and anticonvulsant [35, 54, 73]. ∆9-Tetrahydrocannabinolic acid (THCA) was beneficial in a mouse model of Huntington’s disease with effects through PPARγ activation which resulted in reduced microgliosis, astrogliosis, and dampening of pro-inflammatory markers alongside improved motor deficits [74, 75]. THCA also had anti-nociceptive, anxiolytic, and hyperlocomotive properties mediated by CB1R and CB2R agonist activity, as well as PPARγ [42].
Minor cannabinoid cannabichromene (CBC) has not been extensively tested in models of neurological disease. In vitro studies suggested CBC had pharmacological activity as a CB1R and CB2R partial agonist with greater selectivity and potency at CB2R, and also as a TRPV1 desensitizing agonist. These are promising actions for CB2R-mediated neuroprotection in conditions like TBI, as well as analgesia [42, 76, 77]. In rodents, CBC had topical and peripheral (i.e., non-CNS) anti-inflammatory effects [78,79,80] as well as antidepressant-like effects [81].
Cannabidiolic acid (CBDA) appears to be a partial CB2R agonist with anticonvulsant properties. Comparable effects to CBD were found in a rat maximal electroshock seizure model and a Scn1aRX/+ mouse model of Dravet syndrome hyperthermia, where treatment increased the temperature threshold required to induce tonic–clonic seizures [82, 83]. Another minor cannabinoid, cannabidivarin (CBDV) also reduced seizure activity in multiple in vivo models of epilepsy, and improved neurobehavioral abnormalities in mouse models of Rett syndrome [84, 85] Cannabinol (CBN) treatment delayed the progression of motor abnormalities in a model of amyotrophic lateral sclerosis [86].
Minor phytocannabinoid cannabigerol (CBG) is an activator of PPARγ and partial agonist of CB1R and CB2R [42]. Although CBG has not been studied in TBI models, non-cannabis derived PPARγ activator pioglitazone was neuroprotective in a rat model of TBI [87]. Pioglitazone exerted neuroprotective effects by downregulation of inflammatory NF-κB and IL-6 pathways, supporting the potential for PPARγ activators such as CBG to dampen neuroinflammation associated with TBI [87]. Despite no direct studies in TBI, CBG and its derivatives, VCE-003 and VCE-003.2, have been studied in several in vivo models of neurodegeneration and inflammation [42, 88]. In a model of Huntington’s disease, CBG derivatives improved motor performance in the RotaRod test; reduced neuron loss; enhanced neurogenesis; suppressed microglial activation and astrogliosis; mitigated the release of inflammatory enzymes and cytokines and downregulated Huntington’s disease-associated genes [89,90,91].
CBG derivatives have been further assessed in rodent models of multiple sclerosis, where beneficial effects on myelin and oligodendrocyte health are relevant to TBI [92,93,94]. CBG derivatives suppressed activation of microglia and macrophages as well as reduced levels of inflammatory mediators; preserved myelination quantity and integrity; reduced axonal damage; and improved motor outcomes [93, 94]. In the lipopolysaccharide-induced Parkinson’s disease model, CBG derivatives were neuroprotective and anti-inflammatory [95, 96]. Treatment resulted in dampened elevation of inducible nitric oxide synthase (a key mediator of inflammation); prevented elevation of pro-inflammatory cytokines TNF-α and IL-1β; reduced microgliosis; and preserved dopaminergic nigrostriatal neurons [95, 96]. Exploratory locomotor behavior was also partially improved in the cylinder rearing test [95]. In addition, in a genetic mouse model of amyotrophic lateral sclerosis, administration of a CBG derivative delayed disease progression, reduced the number of pathological signs present; and improved the clinical score while preventing weight loss [97].
The current literature on the medicinal benefits of minor cannabinoids in neurological diseases are encouraging, and further research will continue to elucidate their effects. At present, studies that directly assess minor cannabinoids in models of TBI are lacking, although the effects on overlapping pathological mechanisms described above may extend to TBI pathology. In particular, the myelin-preserving effects of CBG (and derivatives) in MS models, and reduction of microglia and astrocyte activation are candidate effects that may be relevant to TBI treatment and should be studied directly. The anti-inflammatory effects of THCV and the CB2R agonist activity of CBC are also promising and warrant further investigation.
Terpenes in TBI-related conditions
At present, terpenes have not been directly assessed in models of TBI, though studies in other disease models with relevant pathologies can be used to infer potential benefits. A recent extensive review of terpenes by Gonçalves and colleagues [55] included discussion of their antimicrobial and anti-tumor properties, and beneficial effects in the treatment of gastrointestinal diseases, though these are largely beyond the scope of this review. Effects of terpenes on pathology with relevance to TBI (such as inflammation, oxidative stress, neurodegeneration, and pain) are summarized below.
The terpene most widely investigated in neurological conditions is β-caryophyllene (BCP) [55]. Relevant benefits of BCP included analgesic effects in mouse models of neuropathic pain and peripheral neuropathy which were blocked by co-administration of a CB2R antagonist, which suggested that these effects were mediated via the CB2R receptor [98, 99]. BCP has alsoreduced DNA oxidation and GFAP expression in a d-galactose model of aging in mice, although it failed to restore cognitive (spatial memory) deficits at the dose examined [100]. In a stroke model of bilateral common carotid artery occlusion with reperfusion, BCP modulated the response of the endocannabinoid system and prevented increased levels of lipoperoxidases, which indicated protection from oxidative damage [101]. BCP also had beneficial effects for white matter preservation, with reduced axonal demyelination and improved motor function in the experimental autoimmune encephalitis model of multiple sclerosis in mice. These effects were associated with an improved neuroinflammatory state characterized by inhibition of microglia, CD4+ and CD8+ T lymphocytes, and modulation of Th1/Treg immune balance [102]. All of these effects were CB2R-dependent, and suggest neuroprotective potential. Additional studies have been conducted in non-CNS disease models, such as cancer and inflammatory bowel disease [103,104,105,106,107]. While beyond the scope of this review, it is notable that a mouse model of inflammatory bowel disease probed the mechanism of BCP’s anti-inflammatory effects and found that PPARγ, as well as CB2R, were required for the observed immune modulation [103]. This links BCP into the wider endocannabinoid system beyond CB2R, although further research is required to understand whether these findings translate to the CNS. Overall, numerous studies support the anti-inflammatory and analgesic effects of BCP and its pharmacological activity as an agonist at CB2R, which suggests that BCP is a worthy candidate for future research in TBI [55, 108].
An in vitro cell culture study examined the activity of ten terpenes commonly found in medical cannabis cultivars and found that the majority of the observed TRPV1-dependent Ca2+ response could be attributed to the terpene myrcene [109]. The effect of myrcene on TRPV1 Ca2+ flux was variable depending on intracellular Ca2+ levels, implying sensitivity to the intracellular environment [109]. Therefore, myrcene may have differential effects in health and disease states. Additional research will be needed to determine if myrcene in a high Ca2+ environment serves to regulate or potentiate intracellular Ca2+ levels. In addition, pre-application of myrcene in a cell culture model modulated CBD binding at TRPV1, suggesting myrcene may either compete with CBD, or act as an allosteric modulator [109]. These data suggest myrcene interacts with other cannabinoids and may uniquely modulate TRPV1, though further research is required to understand myrcene’s potential role in pain management [109].
Limonene is found in Cannabis as well as various citrus oils [55]. While mainly studied in terms of antifungal or antibacterial properties, limonene has also been examined in pain models, where it inhibited nociceptive behaviors [110, 111]. A high limonene content oil (not sourced from Cannabis but rather from citrus lumina) prevented downstream effects of oxidative stress such as cell death, production of reactive oxygen species (ROS), and inflammation in a drosophila model of Alzheimer’s disease [112]. Linalool had potent effects on ROS and lipid peroxidation, where it slowed cell death and improved mitochondrial morphology [113], while terpineol displayed anti-nociceptive and neuroprotective properties, as well as suppressed inflammatory cell production [55, 114]. Similarly, γ-terpinene reduced edema and inflammatory cell infiltration in mouse models of inflammation [115].
α-Pinene has various neuroprotective effects relevant to TBI. Of these, anti-oxidant activity may be most beneficial acutely after injury, with evidence that it reduced DNA damage and ROS production in skin cells after UVA light exposure [116]. Similarly, in a model of ischemic stroke, α-pinene prevented oxidative damage and inflammation, and rescued behavior deficits [117]. Nerolidol appears to have similar effects, with evidence that it prevented DNA damage through upregulation of nitric oxide levels [118]. Although these were studied in the context of parasitic infection (mice infected with Trypanosoma evansi), these mechanisms have potential relevance to TBI. Finally, citral, found in Cannabis as well as lemongrass, had anti-inflammatory properties, including inhibition of various inflammatory pathways which was partially dependent on PPARγ [119]. Citral may also affect downstream signaling from CB2R [120] and regulate cellular antioxidant defenses, such as glutathione enzymes and superoxide dismutase [121]. These findings imply citral may be beneficial in some aspects of TBI pathology.
In summary, there is a large body of evidence supporting potential therapeutic properties of terpenes, including anti-inflammatory, anti-nociceptive, and neuroprotective effects [55]. No studies have directly assessed terpenes in models of TBI, but current evidence suggests they should be considered as an integral part of the complex polypharmacy of the Cannabis plant and may contribute to the therapeutic potential of Cannabis plant extracts.
Phytocannabinoid polypharmacy
The ‘entourage’ effect is the supposed benefit that occurs when phytocannabinoids are used in combination [54]. These benefits range from reducing or counteracting adverse effects to possible synergistic benefits. The ability to modulate potential adverse effects while maintaining or enhancing medicinal benefits would be of great value for the application of phytocannabinoids as therapeutics. The existence of the ‘entourage’ effect remains controversial, and is an area of active research, yet the potential for a tailored therapeutic benefit from cannabinoid polypharmacy presents a unique advantage that plant-based extracts may offer over isolates or synthetic compounds.
The two plant-derived pharmaceuticals with current FDA approval are Epidiolex (CDB extract) and Sativex (1:1 THC/CBD combination). While the active ingredient of Epidiolex is purified CBD [122], Sativex is a roughly 1:1 combination of a high THC and high CBD whole plant extracts, which includes minor cannabinoids [123]. The benefits of combining CBD with THC have been acknowledged in the case of Sativex, combining evidence from numerous studies in animals and humans from throughout the twentieth century, as comprehensively reviewed by Russo and Guy [124] and McPartland and colliagues [43]. Briefly, higher doses of THC are tolerated when administered with CBD, and CBD reduced adverse effects of THC, such as tachycardia, intoxication, and sedation, without reducing the beneficial effect of reduced muscle spasticity [29, 124, 125]. In addition, THC alone had a moderate and long-lasting analgesic effect that was potentiated when CBC was co-administered in an electroshock seizure model, although this synergistic effect did not extend to neurobehavioral effects (motility), anti-seizure effects, or conditioned avoidance responses [126]. The minor cannabinoid CBC has also been studied in combination with THC. DeLong and colleagues [79] demonstrated that CBC potentiated the effects of THC in the behavior tetrad (a behavior battery associated with CB1R stimulation which examines analgesia, catalepsy, locomotion, and hypothermia [127]), by achieving these effects at a lower dose than when THC was administered alone [79]. The anti-inflammatory effects of CBC were also augmented when CBC and THC were administered together [79].
Some minor phytocannabinoids appear to modulate the effects of THC. For example, a number of minor cannabinoids appear to have weak or partial agonist activity at CB1R and CB2R which, when administered alongside higher concentrations of THC, may act as functional antagonists [42]. In addition, CBD and minor constituents may modulate the effects of CB1R and CB2R activity through other ligands, though the mechanisms are not fully understood [42]. This emerging evidence supports further investigation of the interactions of cannabinoids in vivo, and the effects of full-spectrum Cannabis extracts, where the combination of various major and minor constituents may result in distinct effects compared to isolate preparations.
The terpene profile of a cannabis cultivar may also contribute to its effects, including entourage effects, although consequences of interaction with other phytocannabinoids remain largely unknown. While some studies report no effect of various terpenes on CB1R or CB2R-mediated effects [128, 129], one study demonstrated a weak association between BCP and CB2R, aligning with a previous finding that BCP is a CB2R selective agonist [99]. Despite a lack of understanding of the mechanisms by which terpenes may contribute to an entourage effect, synergy between terpenes and cannabinoids have been reported, as reviewed by Russo [54]. The functional outcomes of interactions between terpenes and cannabinoids remains an area of active research and debate, but is an important consideration in the therapeutic application of full-spectrum cannabis extracts.
Synthetic cannabinoids in TBI
Synthetic cannabinoids have been relatively well studied in TBI models (summarized in Table 3), particularly regarding CB2R-mediated effects. In a weight-drop model in mice and rats, a single 10 mg/kg dose of CB2R agonist HU-914 or 5 mg/kg HU-910 administered 1 h after injury improved the neurological severity score compared to vehicle or lower treatment doses [130]. This benefit was completely blocked by co-administration of CB2R antagonist/inverse agonist SR144528, and absent in CB2R knockout mice, which indicated these effects are CB2R-dependent [130].
Synthetic CB2R agonists preserved BBB integrity in models of TBI and other neuroinflammatory states. The CB2R agonists JWH-133 (1 mg/kg) and 0–1966 (5 mg/kg) and CB2R antagonist (SR144528; 5 mg/kg) were used by Amenta and colleagues [131] to assess the role of CB2R in the neurovascular inflammatory response and BBB changes [131]. Wild-type or CB2R-knockout mice were subjected to the CCI model of TBI, and the CB2R agonists and antagonists were administered 2 or 18 h post-CCI [131]. Injury resulted in increased levels of TNF-α, and this was exacerbated in both CB2R-knockout mice, and in mice treated with the CB2R blocker SR144528 [131]. However, the CB2R agonist JWH-133 did not significantly reduce the heightened TNF-α levels [131]. When BBB permeability was assessed using sodium fluorescein, JWH-133 treatment significantly reduced uptake following CCI, indicating JWH-133 prevented the BBB breach typically observed after injury [131]. This benefit was not observed in CB2R knockout mice, indicating that the beneficial effect of JWH-133 on the BBB was mediated through CB2R-dependent mechanisms [131]. Additional research in the CCI model found that administration of the CB2R agonist 0-1966 reduced Fluoro-Jade C labelling, indicating reduced neurodegeneration after injury [132]. This CB2R agonist had also been found to attenuate CCI-induced edema and substance P elevation (a peptide associated with pain and inflammation) [133].
White matter, including myelin, axons, and oligodendrocytes, is an important therapeutic target for management of TBI symptoms [92]. The vulnerability of white matter to TBI pathology is well established, and dysmyelination and loss of white matter tract integrity likely underlies persistent symptoms after TBI [134]. Therapeutic strategies that protect oligodendrocytes, preserve axonal structure and promote myelination are needed [92]. In a CCI rat model, the CB2R agonist JWH-133 improved multiple measures of white matter pathology. Specifically, injury-induced loss of myelin basic protein and neurofilament-200 were abolished with JWH-133 treatment, with specific effects observed in the corpus callosum, external capsule, cortex, and striatum, to levels comparable to sham-injured rats [135]. Numbers of oligodendrocytes and oligodendrocyte precursor cells were likewise preserved [135], suggesting CB2R signalling supports white matter integrity when faced with injury [135]. Other injury-induced disruptions to white matter included thinner myelin relative to axon diameter and decreased fractional anisotropy (suggested reduced structural integrity), and both of these injury effects were ameliorated with JWH-113 treatment and blocked by CB2R antagonist SR144528 [135]. Treatment with JWH-133 was also associated with a bias towards the protective M2 phenotype of microglia/macrophages, with a ramified appearance and reduced phosphorylated PERK. JWH-133 also reduced clustering of microglia around myelinated fibers and reduced microglia in contact with myelin [135]. Further CB2R-dependent benefits of JWH-133 treatment after CCI injury included improved cerebral blood flow; reduced anxiety-like behavior; and mitigated spatial memory deficits in the Morris Water Maze [135]. Several of these effects, including CB2R-mediated polarization of macrophages to the M2 phenotype; enhanced cerebral blood flow; and improved behavior outcomes, were replicated with administration of another CB2R agonist, GP1a [136].
Interestingly, CB2R inverse agonists have also been assessed in models of blast TBI using raloxifene (also a selective estrogen receptor modulator) and SMM-189, and both treatments were effective in reversing a number of TBI pathologies. Briefly, SMM-189 restored electrophysiological abnormalities after injury and both SMM-189 and raloxifene restored visual acuity, visual contrast sensitivity, and reduced injury pathologies in the retina and optic nerve [137,138,139,140]. Overall, these findings support potential therapeutic benefits of CB2R modulation in models of TBI.
While there has been less focus on CB1R alone compared to CB2R, CB1R activation through a synthetic agonist arachidonyl-2′-chloroethylamide (ACEA) administered once daily for 7 days prevented cognitive impairment in the CCI model in both the Morris Water Maze task and Novel Object Recognition task, although treatment did not affect lesion size [141]. In addition to these emerging data, the beneficial effects of endocannabinoids after TBI described previously (see Table 1) are largely dependent on CB1R signaling, suggesting this is a promising target for therapeutic development. In conclusion, exogenous modulation of the endocannabinoid system with phyto- and synthetic cannabinoids is a promising therapeutic strategy, and these data can guide the application of cannabinoids in the treatment of TBI.
Synthetic cannabinoids in TBI-related conditions
In addition to the previously described research in TBI models, synthetic cannabinoids have also been examined in related neuropathologies, such as stroke and neuronal injury models. In the middle cerebral artery occlusion model, CB1R agonist ACEA treatment reduced infarct volume, neuron apoptosis, and mitochondrial fission [142]. These effects were blocked by the CB1R antagonist AM251, as well as by upregulated dynamin-related protein 1 [142]. The CB1R and CB2R agonist WIN55,212-2 was investigated in a neuron injury model in rats, relevant to HIV and HIV-associated neurocognitive dysfunction caused by the production of neurotoxic and inflammatory proteins, such as GP120 [143]. GP120 toxicity shares characteristics with TBI including glutamate excitotoxicity, elevated intracellular Ca2+, oxidative stress, and cell death. The neuronal injury model was produced by injection of GP120 into the hippocampus, and WIN55,212-2 (3 mg/kg) was administered prior to injury and for the following three consecutive days [143]. WIN55,212-2 treatment improved GP120-induced deficits in spatial memory; reduced the number of apoptotic cells; and reduced expression of p38 and JNK mRNA. Treatment also reduced inflammatory mediators and oxidative stress while increasing SOD antioxidant activity. While WIN55,212-2 has activity at both CB1R and CB2R, the beneficial effects were blocked with CB2R inverse agonist AM630, suggesting CB2R was responsible for these effects [143]. To conclude, these studies provide additional support for both CB1R and CB2R-mediated benefits in TBI-relevant pathologies.
Clinical research of cannabinoids in TBI
Phytocannabinoids in clinical populations
At present, studies on the effects of cannabinoids in clinical TBI populations are sparse, and no published randomized controlled clinical trials on phytocannabinoids in TBI were located for this review. However, there are a small number of studies on TBI patient populations and cannabis use (Table 4). In one report, 307 patients with physician diagnosed concussions (mTBI) were recruited within 1 week of their injury and followed during recovery via weekly assessments for at least 4 weeks [144]. Participants were surveyed regarding voluntary use of alcohol, cigarettes, and Cannabis before and after injury, and physicians assessed recovery ofcognitive and physical activities. 24.4% of the participants reported using Cannabis regularly prior to their injury, while 14.0% used Cannabis regularly during recovery. None of the substances were associated with improved rate of recovery; however, Cannabis use was associated with a lower symptom severity score in weeks 3 and 4 in unrecovered patients [144]. The increasing ease of access to Cannabis has also permitted the use of toxicology screens to associate the presence or absence of THC in trauma patients upon presentation to hospital with clinical outcomes. Retrospectively, cases that screened positive for THC had a lower mortality rate after TBI [145]. Of the 446 cases included, the overall mortality rate was 9.9%. Overall, 18.4% of the toxicology screens were positive for THC, and a positive screen was associated with a mortality rate of 2.4% compared to 11.5% for THC-negative patients [145]. A similar study found trauma patients that were THC-positive upon presenting to hospital had a shorter median length of stay in hospital and shorter length of stay in intensive care units, although mortality was not affected. In the subset of trauma patients with TBI, THC-positive screening was associated with a shorter hospital stay and fewer ventilator days [146]. In addition, patients with severe TBI who returned a THC-positive screen upon hospital admittance had a lower risk of hemorrhagic stroke compared to those that were THC-negative, though no other differences including thromboembolic outcomes, mortality, or length of hospital stay were found [147]. In United States Military Veterans with a history of mTBI, cannabis use is reported at higher rates compared to the general public and other military veteran populations. The self-reported reasons for cannabis use included management of mTBI-associated symptoms, such as disturbed sleep, pain, and neuropsychiatric symptoms, though cannabis use alone was not sufficient for symptom relief [148]. These are encouraging findings regarding the potential benefits of phytocannabinoids for patients with TBI, though randomized, double-blind, placebo-controlled trials are necessary to confirm these results.
Synthetic cannabinoids in clinical populations
Dexanabinol is a synthetic cannabinoid that has been tested in phase II and phase III clinical trials in TBI patients (Table 4). Dexanabinol is non-psychoactive and is an antagonist at NMDA receptors with anti-oxidant and anti-inflammatory properties [149]. In a phase II study of patients with severe TBI as determined by a score of 4–8 on the Glasgow Coma Scale (and lacking any penetrating head wound, SCI, or major visceral injuries, among other restrictions), a single intravenous injection of Dexanabinol was administered at a dose of 48 mg or 150 mg within 6 h of injury. Treatment was associated with lower intracranial pressure and reduction in the number of hypotensive episodes, suggesting beneficial effects on cerebral edema. This single administration also improved cranial perfusion pressure and was associated with improved recovery 1 month post-injury. Overall, Dexanabinol was found to be safe and well tolerated in patients with severe TBI at the doses examined; yet, despite the benefits seen, the study was not powered to test efficacy and a subsequent phase III trial was required [149]. The phase III clinical trial for Dexanabinol recruited 861 patients across 85 centers and 15 countries [150]. Similar to the phase II study, patients received a single injection of 150 mg of Dexanabinol within 6 h of injury. As with phase II, Dexanabinol was found to be safe and well tolerated, although the benefits observed in the phase II trial were not replicated [150]. The authors noted a limitation of the clinical trial was a lack of data collection regarding the plasma concentration of Dexanabinol, as this may have been altered due to the required administration of fluids during acute care. This could have reduced plasma concentrations and thus altered the efficacy. At present, the data surrounding the therapeutic benefits of cannabinoids in human TBI patient populations remain inconclusive. Further studies are warranted to continue to guide the pursuit of cannabis-based medicine for neurological conditions, such as TBI.
Conclusions
The endocannabinoid system is increasingly recognized for its physiological role in regulating cellular activity in the brain and endogenous response to adverse events, such as TBI. The ability to modulate this system with endogenous, plant-derived, or synthetic cannabinoids is promising for the development of therapeutic strategies for TBI. Presently, the strongest evidence for neuroprotective properties is seen for compounds containing CBD, or those targeting CB2R, and the effects of THC treatment are less consistent. CBG (and its derivatives) is the most studied minor phytocannabinoid in neurological disease models, while the most evidence for therapeutic benefit from terpenes relates to BCP, although studies are limited overall. The evidence for a modulating, or even synergistic ‘entourage’ effect when cannabinoids are used in combination is still emerging, but full-spectrum plant extracts with a variety of phytocannabinoids may improve the safety and therapeutic profile of cannabinoid medicine.
While the number of studies in preclinical models of TBI has increased with generally positive results, data from clinical populations remain limited. The only cannabinoid-based synthetic pharmaceutical to undergo randomized controlled trials in TBI was Dexanabinol, and it was found not effective; however, the growing literature of cannabinoids in TBI remains promising and further research is warranted. Diseases with complex, multifaceted pathology, such as TBI, may require treatment that is multi-mechanistic, such as whole plant cannabis extracts.
Availability of data and materials
Not applicable (review article).
Abbreviations
- 2-AG:
-
2-Arachydonoyl glycerol
- ACEA:
-
Arachidonyl-2′-chloroethylamide
- AEA:
-
N-arachidonylethanolamine (also known as anandamide)
- BBB:
-
Blood–brain barrier
- BCCAO:
-
Bilateral common carotid artery occlusion
- BCP:
-
β-Caryophyllene
- Ca2+:
-
Calcium ion
- CCI:
-
Controlled cortical impact
- CB1R:
-
Cannabinoid receptor 1
- CB2R:
-
Cannabinoid receptor 2
- CBC:
-
Cannabichromene
- CBD:
-
Cannabidiol
- CBDA:
-
Cannabidiolic acid
- CBDV:
-
Cannabidivarin
- CBG:
-
Cannabigerol
- CBN:
-
Cannabinol
- CNS:
-
Central nervous system
- DNA:
-
Deoxyribonucleic acid
- EAE:
-
Experimental autoimmune encephalitis
- FAAH:
-
Fatty acid amide hydrolase
- GABA:
-
Gamma aminobutyric acid
- GFAP:
-
Glial fibrillary acid protein
- IBA1:
-
Ionized calcium binding adaptor molecule 1
- IL-1β:
-
Interleukin 1 beta
- MCAO:
-
Middle cerebral artery occlusion
- MAGL:
-
Monoacylglycerol lipase
- mTBI:
-
Mild traumatic brain injury
- NSS:
-
Neurological severity score
- PPARγ:
-
Peroxisome proliferator-activated receptor gamma
- ROS:
-
Reactive oxygen species
- SCI:
-
Spinal cord injury
- TBI:
-
Traumatic brain injury
- THC:
-
∆9-Tetrahydrocannabinol
- THCV:
-
∆9-Tetrahydrocannabivarin
- THCA:
-
∆9-Tetrahydrocannabinolic acid
- TNF-α:
-
Tumor necrosis factor alpha
- TRPV1:
-
Transient receptor potential vanilloid-1
- WT:
-
Wild type
References
Corrigan JD, Selassie AW, Orman JA. The epidemiology of traumatic brain injury. J Head Trauma Rehabil. 2010;25(2):72–80.
Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–8.
Baxter K, Hellewell SC. Traumatic brain injury within domestic relationships: complications, consequences and contributing factors. J Aggress Maltreatment Trauma. 2019;28(6):660–76. https://doi.org/10.1080/10926771.2019.1602089.
Meaney DF, Smith DH. Biomechanics of concussion. Clin Sports Med. 2011;30(1):19.
Menon DK, Schwab K, Wright DW, Maas AI. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91(11):1637–40.
Kontos AP, Elbin RJ, Schatz P, Covassin T, Henry L, Pardini J, et al. A revised factor structure for the post-concussion symptom scale: baseline and postconcussion factors. Am J Sports Med. 2012;40(10):2375–84.
Saltychev M, Eskola M, Tenovuo O, Laimi K. Return to work after traumatic brain injury: systematic review. Brain Inj. 2013;27(13–14):1516–27. https://doi.org/10.3109/02699052.2013.831131.
Wood RL, Liossi C, Wood L. The impact of head injury neurobehavioural sequelae on personal relationships: preliminary findings. Brain Inj. 2009;19(10):845–51. https://doi.org/10.1080/02699050500058778.
Humphreys I, Wood RL, Phillips CJ, Macey S. The costs of traumatic brain injury: a literature review. Clin Outcomes Res. 2013;5(1):281–7.
Sterr A, Herron KA, Hayward C, Montaldi D. Are mild head injuries as mild as we think? Neurobehavioral concomitants of chronic post-concussion syndrome. BMC Neurol. 2006;6:7.
Marin JR, Weaver MD, Yealy DM, Mannix RC. Trends in visits for traumatic brain injury to emergency departments in the United States. J Am Med Assoc. 2014;311(18):1917–9.
De Beaumont L, Thoret H, Mongeon D, Messier J, Leclerc S, Tremblay S, et al. Brain function decline in healthy retired athletes who sustained their last sports concussion in early adulthood. Brain. 2009;132(3):695–708.
Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Cantu RC, Randolph C, et al. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005. 57(4). https://pubmed.ncbi.nlm.nih.gov/16239884/. Accessed 14 May 2022.
Guskiewicz KM, Marshall SW, Bailes J, Mccrea M, Harding HP, Matthews A, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39(6):903–9.
Manley G, Gardner AJ, Schneider KJ, Guskiewicz KM, Bailes J, Cantu RC, et al. A systematic review of potential long-term effects of sport-related concussion. Br J Sports Med. 2017;51(12):969–77.
Hellewell SC, Beaton CS, Welton T, Grieve SM. Characterizing the risk of depression following mild traumatic brain injury: a meta-analysis of the literature comparing chronic mTBI to non-mTBI populations. Front Neurol. 2020;19(11):1–14.
Turner RC, Lucke-Wold BP, Robson MJ, Lee JM, Bailes JE. Alzheimer’s disease and chronic traumatic encephalopathy: distinct but possibly overlapping disease entities. Brain Inj. 2016;30(11):1279–92. https://doi.org/10.1080/02699052.2016.1193631.
Mouzon B, Chaytow H, Crynen G, Bachmeier C, Stewart J, Mullan M, et al. Repetitive mild traumatic brain injury in a mouse model produces learning and memory deficits accompanied by histological changes. J Neurotrauma. 2012;29(18):2761–73. https://doi.org/10.1089/neu.2012.2498.
Kane MJ, Angoa-Pérez M, Briggs DI, Viano DC, Kreipke CW, Kuhn DM. A mouse model of human repetitive mild traumatic brain injury. J Neurosci Methods. 2012;203(1):41–9.
Prins ML, Hales A, Reger M, Giza CC, Hovda DA. Repeat traumatic brain injury in the juvenile rat is associated with increased axonal injury and cognitive impairments. Dev Neurosci. 2010;32(5–6):510–8.
Shultz SR, Bao F, Omana V, Chiu C, Brown A, Cain DP. Repeated mild lateral fluid percussion brain injury in the rat causes cumulative long-term behavioral impairments, neuroinflammation, and cortical loss in an animal model of repeated concussion. J Neurotrauma. 2012;29(2):281–94. https://doi.org/10.1089/neu.2011.2123.
Fehily B, Bartlett CA, Lydiard S, Archer M, Milbourn H, Majimbi M, et al. Differential responses to increasing numbers of mild traumatic brain injury in a rodent closed-head injury model. J Neurochem. 2019;149(5):660–78.
Yates NJ, Lydiard S, Fehily B, Weir G, Chin A, Bartlett CA, et al. Repeated mild traumatic brain injury in female rats increases lipid peroxidation in neurons. Exp Brain Res. 2017;235(7):2133–49.
Cooper DB, Bunner AE, Kennedy JE, Balldin V, Tate DF, Eapen BC, et al. Treatment of persistent post-concussive symptoms after mild traumatic brain injury: a systematic review of cognitive rehabilitation and behavioral health interventions in military service members and veterans. Brain Imaging Behav. 2015;9(3):403–20.
Lu HC, MacKie K. An introduction to the endogenous cannabinoid system. Biol Psychiatry. 2016;79:516–25.
Cristino L, Bisogno T, Di Marzo V. Cannabinoids and the expanded endocannabinoid system in neurological disorders. Nat Rev Neurol. 2020;16(1):9–29. https://doi.org/10.1038/s41582-019-0284-z.
Mackie K. Cannabinoid receptors: where they are and what they do. J Neuroendocrinol. 2008;10–4. https://pubmed.ncbi.nlm.nih.gov/18426493/. Accessed 24 Aug 2020.
Singh J, Neary JP. Neuroprotection following concussion: the potential role for cannabidiol. Can J Neurol Sci. 2020. https://doi.org/10.1017/cjn.2020.23.
Boggs DL, Nguyen JD, Morgenson D, Taffe MA, Ranganathan M. Clinical and preclinical evidence for functional interactions of cannabidiol and Î " 9-tetrahydrocannabinol. Neuropsychopharmacology. 2018;43:142–54.
Cabral GA, Raborn ES, Griffin L, Dennis J, Marciano-Cabral F. CB 2 receptors in the brain: role in central immune function. Br J Pharmacol. 2008;153:240–51.
Villapol S. Roles of peroxisome proliferator-activated receptor gamma on brain and peripheral inflammation. Cell Mol Neurobiol. 2018;38(1):121–32.
Louis-Gray K, Tupal S, Premkumar LS. TRPV1: a common denominator mediating antinociceptive and antiemetic effects of cannabinoids. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms231710016.
Diana MA, Marty A. Endocannabinoid-mediated short-term synaptic plasticity: depolarization-induced suppression of inhibition (DSI) and depolarization-induced suppression of excitation (DSE). Br J Pharmacol. 2004;142:9–19.
Marsicano G, Goodenough S, Monory K, Hermann H, Eder M, Cannich A, et al. CB1 cannabinoid receptors and on-demand defense against excitotoxicity. Science. 2003;302(5642):84–8.
Pertwee RG. The diverse CB 1 and CB 2 receptor pharmacology of three plant cannabinoids: Δ 9-tetrahydrocannabinol, cannabidiol and Δ 9-tetrahydrocannabivarin. Br J Pharmacol. 2008;153(2):199–215.
Wilson RI, Nicoll RA. Endogenous cannabinoids mediate retrograde signalling at hippocampal synapses. Nature. 2001;410(6828):588–92.
Mechoulam R, Panikashvili D, Shohami E. Cannabinoids and brain injury: therapeutic implications. Trends Mol Med. 2002;8(2):58–61.
Chen JW, Wang PF, Zhang MZ, Zhang ZD, Cheng H, Sun YF, et al. Relationship between expression changes of CB2R and wound age of brain contusion in mice. J Forensic Med. 2019;35(2):136–42.
Panikashvili D, Simeonidou C, Ben-Shabat S, Hanuš L, Breuer A, Mechoulam R, et al. An endogenous cannabinoid (2-AG) is neuroprotective after brain injury. Nature. 2001;413(6855):527–31.
Panikashvili D, Shein NA, Mechoulam R, Trembovler V, Kohen R, Alexandrovich A, et al. The endocannabinoid 2-AG protects the blood–brain barrier after closed head injury and inhibits mRNA expression of proinflammatory cytokines. Neurobiol Dis. 2006;22(2):257–64.
Calina D, Buga AM, Mitroi M, Buha A, Caruntu C, Scheau C, et al. The treatment of cognitive, behavioural and motor impairments from brain injury and neurodegenerative diseases through cannabinoid system modulation—evidence from in vivo studies. J Clin Med. 2020;9(8):2395.
Zagzoog A, Mohamed KA, Kim HJJ, Kim ED, Frank CS, Black T, et al. In vitro and in vivo pharmacological activity of minor cannabinoids isolated from Cannabis sativa. Sci Rep. 2020;10(1):1–13.
McPartland JM, Duncan M, Di Marzo V, Pertwee RG. Are cannabidiol and Δ9-tetrahydrocannabivarin negative modulators of the endocannabinoid system? A systematic review. Br J Pharmacol. 2015;172:737–53.
Mechoulam R, Fride E, Di Marzo V. Endocannabinoids. Eur J Pharmacol. 1998;359:1–18.
Badowski ME. A review of oral cannabinoids and medical marijuana for the treatment of chemotherapy-induced nausea and vomiting: a focus on pharmacokinetic variability and pharmacodynamics. Cancer Chemother Pharmacol. 2017;80:441–9.
Ward A, Holmes B. Nabilone: a preliminary review of its pharmacological properties and therapeutic use. Drugs. 1985;30(2):127–44.
Ahmedzai S, Carlyle DL, Calder IT, Moran F. Anti-emetic efficacy and toxicity of nabilone, a synthetic cannabinoid, in lung cancer chemotherapy. Br J Cancer. 1983;48(5):657–63.
Thomas A, Baillie GL, Phillips AM, Razdan RK, Ross RA, Pertwee RG. Cannabidiol displays unexpectedly high potency as an antagonist of CB 1 and CB 2 receptor agonists in vitro. Br J Pharmacol. 2007;150(5):613–23. https://doi.org/10.1038/sj.bjp.0707133.
Laprairie RB, Bagher AM, Kelly MEM, Denovan-Wright EM. Cannabidiol is a negative allosteric modulator of the cannabinoid CB1 receptor. Br J Pharmacol. 2015;172(20):4790–805.
Tham M, Yilmaz O, Alaverdashvili M, Kelly MEM, Denovan-Wright EM, Laprairie RB. Allosteric and orthosteric pharmacology of cannabidiol and cannabidiol-dimethylheptyl at the type 1 and type 2 cannabinoid receptors. Br J Pharmacol. 2019;176(10):1455–69.
Tchantchou F, Tucker LB, Fu AH, Bluett RJ, McCabe JT, Patel S, et al. The fatty acid amide hydrolase inhibitor PF-3845 promotes neuronal survival, attenuates inflammation and improves functional recovery in mice with traumatic brain injury. Neuropharmacology. 2014;85:427–39.
Tchantchou F, Zhang Y. Selective inhibition of alpha/beta-hydrolase domain 6 attenuates neurodegeneration, alleviates blood brain barrier breakdown, and improves functional recovery in a mouse model of traumatic brain injury. J Neurotrauma. 2013;30(7):565–79.
Katz PS, Sulzer JK, Impastato RA, Teng SX, Rogers EK, Molina PE. Endocannabinoid degradation inhibition improves neurobehavioral function, blood–brain barrier integrity, and neuroinflammation following mild traumatic brain injury. J Neurotrauma. 2015;32(5):297–306.
Russo EB. Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. Br J Pharmacol. 2011;163:1344–64.
Gonçalves ECD, Baldasso GM, Bicca MA, Paes RS, Capasso R, Dutra RC. Terpenoids, cannabimimetic ligands, beyond the cannabis plant. Molecules. 2020;25:1567.
Weston-Green K, Clunas H, Jimenez NC. A review of the potential use of pinene and linalool as terpene-based medicines for brain health: discovering novel therapeutics in the flavours and fragrances of cannabis. Front Psych. 2021. https://doi.org/10.3389/fpsyt.2021.583211.
Zagzoog A, Brandt AL, Black T, Kim ED, Burkart R, Patel M, et al. Assessment of select synthetic cannabinoid receptor agonist bias and selectivity between the type 1 and type 2 cannabinoid receptor. Sci Rep. 2021;11(1):10611.
Pertwee RG. Ligands that target cannabinoid receptors in the brain: from THC to anandamide and beyond. Addict Biol. 2008;13(2):147–59. https://doi.org/10.1111/j.1369-1600.2008.00108.x.
Selvaraj P, Tanaka M, Wen J, Zhang Y. The Novel monoacylglycerol lipase inhibitor MJN110 suppresses neuroinflammation, normalizes synaptic composition and improves behavioral performance in the repetitive traumatic brain injury mouse model. Cells. 2021. 10(12). https://pubmed.ncbi.nlm.nih.gov/34943962/. Accessed 13 May 2022.
Hu M, Zhu D, Zhang J, Gao F, Hashem J, Kingsley P, et al. Enhancing endocannabinoid signalling in astrocytes promotes recovery from traumatic brain injury. Brain. 2022;145(1):179–93.
Wang DP, Jin KY, Zhao P, Lin Q, Kang K, Hai J. Neuroprotective effects of VEGF-A nanofiber membrane and FAAH Inhibitor URB597 against oxygen–glucose deprivation-induced ischemic neuronal injury. Int J Nanomedicine. 2021;16:3661–78.
Belardo C, Iannotta M, Boccella S, Rubino RC, Ricciardi F, Infantino R, et al. Oral cannabidiol prevents allodynia and neurological dysfunctions in a mouse model of mild traumatic brain injury. Front Pharmacol. 2019;10(MAR):352. https://doi.org/10.3389/fphar.2019.00352/full.
Jiang H, Li H, Cao Y, Zhang R, Zhou L, Zhou Y, et al. Effects of cannabinoid (CBD) on blood brain barrier permeability after brain injury in rats. Brain Res. 2021;1768. https://pubmed.ncbi.nlm.nih.gov/34289379/. Accessed 13 May 2022.
Friedman LK, Peng H, Zeman RJ. Cannabidiol reduces lesion volume and restores vestibulomotor and cognitive function following moderately severe traumatic brain injury. Exp Neurol. 2021;346. https://pubmed.ncbi.nlm.nih.gov/34428457/. Accessed 13 May 2022.
Bhatt D, Hazari A, Yamakawa GR, Salberg S, Sgro M, Shultz SR, et al. Investigating the cumulative effects of D9-tetrahydrocannabinol and repetitive mild traumatic brain injury on adolescent rats. Brain Commun. 2020. 2(1). https://academic.oup.com/braincomms/article-abstract/2/1/fcaa042/5819138. Accessed 31 Jul 2020.
Madathil SK, Wilfred BS, Urankar SE, Yang W, Leung LY, Gilsdorf JS, et al. Early microglial activation following closed-head concussive injury is dominated by pro-inflammatory M-1 type. Front Neurol. 2018;9(NOV):964. https://doi.org/10.3389/fneur.2018.00964/full.
Black T, Zagoog A, Roebuck AJ, Greba Q, Neary JP, Howland JG, et al. Sex-specific differences in rotarod performance and type 1 cannabinoid receptor levels in a rat model of traumatic brain injury treated with Δ9-tetrahydrocannabinol. bioRxiv. 2022;2022.04.11.487790. http://biorxiv.org/content/early/2022/04/12/2022.04.11.487790.abstract.
Song S, Kong X, Wang B, Sanchez-Ramos J. Recovery from traumatic brain injury following treatment with Δ9-tetrahydrocannabinol is associated with increased expression of granulocyte-colony stimulating factor and other neurotrophic factors. Cannabis Cannabinoid Res. 2021. https://pubmed.ncbi.nlm.nih.gov/33998887/. Accessed 13 May 2022.
Song S, Kong X, Wang B, Sanchez-Ramos J. Administration of Δ 9-tetrahydrocannabinol following controlled cortical impact restores hippocampal-dependent working memory and locomotor function. Cannabis cannabinoid Res. 2021. https://pubmed.ncbi.nlm.nih.gov/34747647/. Accessed 13 May 2022.
Li H, Kong W, Chambers CR, Yu D, Ganea D, Tuma RF, et al. The non-psychoactive phytocannabinoid cannabidiol (CBD) attenuates pro-inflammatory mediators, T cell infiltration, and thermal sensitivity following spinal cord injury in mice. Cell Immunol. 2018;329:1–9.
Mori MA, Meyer E, Soares LM, Milani H, Guimarães FS, de Oliveira RMW. Cannabidiol reduces neuroinflammation and promotes neuroplasticity and functional recovery after brain ischemia. Prog Neuro-Psychopharmacol Biol Psychiatry. 2017;75:94–105.
McPartland JM, Duncan M, Di Marzo V, Pertwee RG. Are cannabidiol and Δ9-tetrahydrocannabivarin negative modulators of the endocannabinoid system? A systematic review. Br J Pharmacol. 2015;172(3):737–53.
Hill TDM, Cascio MG, Romano B, Duncan M, Pertwee RG, Williams CM, et al. Cannabidivarin-rich cannabis extracts are anticonvulsant in mouse and rat via a CB1 receptor-independent mechanism. Br J Pharmacol. 2013;170(3):679–92.
Nadal X, del Río C, Casano S, Palomares B, Ferreiro-Vera C, Navarrete C, et al. Tetrahydrocannabinolic acid is a potent PPARγ agonist with neuroprotective activity. Br J Pharmacol. 2017;174(23):4263–76.
Franco R, Rivas-Santisteban R, Reyes-Resina I, Casanovas M, Pérez-Olives C, Ferreiro-Vera C, et al. Pharmacological potential of varinic-, minor-, and acidic phytocannabinoids. Pharmacol Res. 2020. https://doi.org/10.1016/j.phrs.2020.104801.
Udoh M, Santiago M, Devenish S, McGregor IS, Connor M. Cannabichromene is a cannabinoid CB2 receptor agonist. Br J Pharmacol. 2019;176(23):4537–47.
De Petrocellis L, Ligresti A, Moriello AS, Allarà M, Bisogno T, Petrosino S, et al. Effects of cannabinoids and cannabinoid-enriched Cannabis extracts on TRP channels and endocannabinoid metabolic enzymes. Br J Pharmacol. 2011;163(7):1479–94.
Turner CE, Elsohly MA. Biological activity of cannabichromene, its homologs and isomers. J Clin Pharmacol. 1981;21(8–9 Suppl). https://pubmed.ncbi.nlm.nih.gov/7298870/. Accessed 7 Sep 2020.
DeLong GT, Wolf CE, Poklis A, Lichtman AH. Pharmacological evaluation of the natural constituent of Cannabis sativa, cannabichromene and its modulation by Δ9-tetrahydrocannabinol. Drug Alcohol Depend. 2010;112(1–2):126–33.
Tubaro A, Giangaspero A, Sosa S, Negri R, Grassi G, Casano S, et al. Comparative topical anti-inflammatory activity of cannabinoids and cannabivarins. Fitoterapia. 2010;81(7):816–9.
El-Alfy AT, Ivey K, Robinson K, Ahmed S, Radwan M, Slade D, et al. Antidepressant-like effect of Δ9-tetrahydrocannabinol and other cannabinoids isolated from Cannabis sativa L. Pharmacol Biochem Behav. 2010;95(4):434.
Anderson LL, Low IK, Banister SD, McGregor IS, Arnold JC. Pharmacokinetics of phytocannabinoid acids and anticonvulsant effect of cannabidiolic acid in a mouse model of dravet syndrome. J Nat Prod. 2019;82(11):3047–55.
Goerl B, Watkins S, Metcalf C, Smith M, Beenhakker M. Cannabidiolic acid exhibits entourage-like improvements of anticonvulsant activity in an acute rat model of seizures. Epilepsy Res. 2021;169: 106525.
Vigli D, Cosentino L, Raggi C, Laviola G, Woolley-Roberts M, De Filippis B. Chronic treatment with the phytocannabinoid Cannabidivarin (CBDV) rescues behavioural alterations and brain atrophy in a mouse model of Rett syndrome. Neuropharmacology. 2018;140:121–9.
Zamberletti E, Gabaglio M, Piscitelli F, Brodie JS, Woolley-Roberts M, Barbiero I, et al. Cannabidivarin completely rescues cognitive deficits and delays neurological and motor defects in male Mecp2 mutant mice. J Psychopharmacol. 2019;33(7):894–907.
Weydt P, Hong S, Witting A, Möller T, Stella N, Kliot M. Cannabinol delays symptom onset in SOD1 (G93A) transgenic mice without affecting survival. Amyotroph Lateral Scler Other Motor Neuron Disord. 2005;6(3):182–4.
Deng Y, Jiang X, Deng X, Chen H, Xu J, Zhang Z, et al. Pioglitazone ameliorates neuronal damage after traumatic brain injury via the PPARγ/NF-κB/IL-6 signaling pathway. Genes Dis. 2020;7(2):253–65.
Stone NL, Murphy AJ, England TJ, O’Sullivan SE. A systematic review of minor phytocannabinoids with promising neuroprotective potential. Br J Pharmacol. 2020. https://doi.org/10.1111/bph.15185.
Díaz-Alonso J, Paraíso-Luna J, Navarrete C, Del Río C, Cantarero I, Palomares B, et al. VCE-003.2, a novel cannabigerol derivative, enhances neuronal progenitor cell survival and alleviates symptomatology in murine models of Huntington’s disease. Sci Rep. 2016;6. https://pubmed.ncbi.nlm.nih.gov/27430371/. Accessed 7 Sep 2020.
Aguareles J, Paraíso-Luna J, Palomares B, Bajo-Grañeras R, Navarrete C, Ruiz-Calvo A, et al. Oral administration of the cannabigerol derivative VCE-003.2 promotes subventricular zone neurogenesis and protects against mutant huntingtin-induced neurodegeneration. Transl Neurodegener. 2019;8(1):9.
Valdeolivas S, Navarrete C, Cantarero I, Bellido ML, Muñoz E, Sagredo O. Neuroprotective properties of cannabigerol in Huntington’s disease: studies in R6/2 mice and 3-nitropropionate-lesioned mice. Neurotherapeutics. 2015;12(1):185–99.
Warnock A, Toomey LM, Wright AJ, Fisher K, Won Y, Anyaegbu C, et al. Damage mechanisms to oligodendrocytes and white matter in central nervous system injury: the australian context. J Neurotrauma. 2020;37(5):739–69. https://doi.org/10.1089/neu.2019.6890.
Carrillo-Salinas FJ, Navarrete C, Mecha M, Feliú A, Collado JA, Cantarero I, et al. A cannabigerol derivative suppresses immune responses and protects mice from experimental autoimmune encephalomyelitis. PLoS ONE. 2014;9(4). https://pubmed.ncbi.nlm.nih.gov/24727978/. Accessed 7 Sep 2020.
Granja AG, Carrillo-Salinas F, Pagani A, Gómez-Cañas M, Negri R, Navarrete C, et al. A cannabigerol quinone alleviates neuroinflammation in a chronic model of multiple sclerosis. J Neuroimmune Pharmacol. 2012;7(4):1002–16.
Burgaz S, García C, Gómez-Cañas M, Muñoz E, Fernández-Ruiz J. Development of an oral treatment with the PPAR-γ-acting cannabinoid VCE-003.2 against the inflammation-driven neuronal deterioration in experimental Parkinson’s disease. Molecules. 2019. https://doi.org/10.3390/molecules24152702.
García C, Gómez-Cañas M, Burgaz S, Palomares B, Gómez-Gálvez Y, Palomo-Garo C, et al. Benefits of VCE-003.2, a cannabigerol quinone derivative, against inflammation-driven neuronal deterioration in experimental Parkinson’s disease: Possible involvement of different binding sites at the PPARγ receptor. J Neuroinflammation. 2018. https://doi.org/10.1186/s12974-018-1060-5.
Rodríguez-Cueto C, Santos-García I, García-Toscano L, Espejo-Porras F, Bellido ML, Fernández-Ruiz J, et al. Neuroprotective effects of the cannabigerol quinone derivative VCE-003.2 in SOD1G93A transgenic mice, an experimental model of amyotrophic lateral sclerosis. Biochem Pharmacol. 2018;157:217–26.
Segat GC, Manjavachi MN, Matias DO, Passos GF, Freitas CS, Costa R, et al. Antiallodynic effect of β-caryophyllene on paclitaxel-induced peripheral neuropathy in mice. Neuropharmacology. 2017;125:207–19.
Aly E, Khajah MA, Masocha W. β-caryophyllene, a CB2-receptor-selective phytocannabinoid, suppresses mechanical allodynia in a mouse model of antiretroviral-induced neuropathic pain. Molecules. 2020;25(1). https://pubmed.ncbi.nlm.nih.gov/31892132/. Accessed 11 Aug 2020.
Chávez-Hurtado P, González-Castañeda RE, Beas-Zarate C, Flores-Soto ME, Viveros-Paredes JM. β-Caryophyllene reduces DNA oxidation and the overexpression of glial fibrillary acidic protein in the prefrontal cortex and hippocampus of d-galactose-induced aged BALB/c mice. J Med Food. 2020;23(5):515–22.
Poddighe L, Carta G, Serra MP, Melis T, Boi M, Lisai S, et al. Acute administration of beta-caryophyllene prevents endocannabinoid system activation during transient common carotid artery occlusion and reperfusion. Lipids Health Dis. 2018;17(1). https://pubmed.ncbi.nlm.nih.gov/29402275/. Accessed 25 Aug 2020.
Alberti TB, Barbosa WLR, Vieira JLF, Raposo NRB, Dutra RC. (−)-β-caryophyllene, a CB2 receptor-selective phytocannabinoid, suppresses motor paralysis and neuroinflammation in a murine model of multiple sclerosis. Int J Mol Sci. 2017;18(4). https://pubmed.ncbi.nlm.nih.gov/28368293/. Accessed 25 Aug 2020.
Bento AF, Marcon R, Dutra RC, Claudino RF, Cola M, Leite DFP, et al. β-caryophyllene inhibits dextran sulfate sodium-induced colitis in mice through CB2 receptor activation and PPARγ pathway. Am J Pathol. 2011;178(3):1153–66.
Jung JI, Kim EJ, Kwon GT, Jung YJ, Park T, Kim Y, et al. β-Caryophyllene potently inhibits solid tumor growth and lymph node metastasis of B16F10 melanoma cells in high-fat diet-induced obese C57BL/6N mice. Carcinogenesis. 2015;36(9):1028–39.
Ambrož M, Boušová I, Skarka A, Hanušová V, Králová V, Matoušková P, et al. The influence of sesquiterpenes from Myrica rubra on the antiproliferative and pro-oxidative effects of doxorubicin and its accumulation in cancer cells. Molecules. 2015;20(8):15343–58.
Amiel E, Ofir R, Dudai N, Soloway E, Rabinsky T, Rachmilevitch S. β-Caryophyllene, a compound isolated from the biblical balm of gilead (Commiphora gileadensis), is a selective apoptosis inducer for tumor cell lines. Evid Based Complement Alternat Med. 2012. https://pubmed.ncbi.nlm.nih.gov/22567036/. Accessed 28 Jun 2022.
Dahham SS, Tabana YM, Iqbal MA, Ahamed MBK, Ezzat MO, Majid ASA, et al. The anticancer, antioxidant and antimicrobial properties of the sesquiterpene β-caryophyllene from the essential oil of Aquilaria crassna. Molecules. 2015;20(7):11808–29.
Gertsch J, Leonti M, Raduner S, Racz I, Chen JZ, Xie XQ, et al. Beta-caryophyllene is a dietary cannabinoid. Proc Natl Acad Sci USA. 2008;105(26):9099–104.
Jansen C, Shimoda LMN, Kawakami JK, Ang L, Bacani AJ, Baker JD, et al. Myrcene and terpene regulation of TRPV1. Channels. 2019;13(1):344–66.
Araújo-Filho HG, Pereira EWM, Rezende MM, Menezes PP, Araújo AAS, Barreto RSS, et al. D-limonene exhibits superior antihyperalgesic effects in a β-cyclodextrin-complexed form in chronic musculoskeletal pain reducing Fos protein expression on spinal cord in mice. Neuroscience. 2017;358:158–69.
do Amaral JF, Silva MIG, de Aquino Neto MRA, Neto PFT, Moura BA, de Melo CTV, et al. Antinociceptive Effect of the monoterpene R-(+)-limonene in mice. Biol Pharm Bull. 2007;30(7):1217–20.
Shin M, Liu QF, Choi B, Shin C, Lee B, Yuan C, et al. Neuroprotective effects of limonene (+) against Aβ42-induced neurotoxicity in a Drosophila model of Alzheimer’s disease. Biol Pharm Bull. 2020;43(3):409–17.
Sabogal-Guáqueta AM, Hobbie F, Keerthi A, Oun A, Kortholt A, Boddeke E, et al. Linalool attenuates oxidative stress and mitochondrial dysfunction mediated by glutamate and NMDA toxicity. Biomed Pharmacother. 2019;118: 109295.
Nogueira MNM, Aquino SG, Rossa C, Spolidorio DMP. Terpinen-4-ol and alpha-terpineol (tea tree oil components) inhibit the production of IL-1β, IL-6 and IL-10 on human macrophages. Inflamm Res. 2014;63(9):769–78. https://doi.org/10.1007/s00011-014-0749-x.
Ramalho TRDO, De Oliveira MTP, Lima ALDA, Bezerra-Santos CR, Piuvezam MR. Gamma-terpinene modulates acute inflammatory response in mice. Planta Med. 2015;81(14):1248–54. https://doi.org/10.1055/s-0035-1546169.
Karthikeyan R, Kanimozhi G, Prasad NR, Agilan B, Ganesan M, Srithar G. Alpha pinene modulates UVA-induced oxidative stress, DNA damage and apoptosis in human skin epidermal keratinocytes. Life Sci. 2018;212:150–8.
Khoshnazar M, Bigdeli MR, Parvardeh S, Pouriran R. Attenuating effect of α-pinene on neurobehavioural deficit, oxidative damage and inflammatory response following focal ischaemic stroke in rat. J Pharm Pharmacol. 2019;71(11):1725–33. https://doi.org/10.1111/jphp.13164.
Baldissera MD, Souza CF, Riéffel RC, Velho MC, Ramos AP, Nascimento K, et al. Protective effect of nerolidol-loaded in nanospheres against cerebral damage caused by Trypanosoma evansi. Naunyn Schmiedebergs Arch Pharmacol. 2018;391(7):753–9. https://doi.org/10.1007/s00210-018-1504-6.
Katsukawa M, Nakata R, Takizawa Y, Hori K, Takahashi S, Inoue H. Citral, a component of lemongrass oil, activates PPAR α and γ and suppresses COX-2 expression. Biochim Biophys Acta Mol Cell Biol Lipids. 2010;1801(11):1214–20.
Gonçalves ECD, Assis PM, Junqueira LA, Cola M, Santos ARS, Raposo NRB, et al. Citral inhibits the inflammatory response and hyperalgesia in mice: the role of TLR4, TLR2/Dectin-1, and CB2 cannabinoid receptor/ATP-sensitive K+ channel pathways. ACS Appl Mater Interfaces. 2020. https://doi.org/10.1021/acs.jnatprod.9b01134.
Bouzenna H, Hfaiedh N, Giroux-Metges MA, Elfeki A, Talarmin H. Biological properties of citral and its potential protective effects against cytotoxicity caused by aspirin in the IEC-6 cells. Biomed Pharmacother. 2017;87:653–60.
Abu-Sawwa R, Stehling C. Epidiolex (cannabidiol) primer: frequently asked questions for patients and caregivers. J Pediatr Pharmacol Ther. 2020;25:75–7.
Sativex® | GW Pharmaceuticals, plc. https://www.gwpharm.com/healthcare-professionals/sativex#. Accessed 9 Sep 2020.
Russo E, Guy GW. A tale of two cannabinoids: the therapeutic rationale for combining tetrahydrocannabinol and cannabidiol. Med Hypotheses. 2006;66(2):234–46.
Vermersch P. Sativex ® (tetrahydrocannabinol + cannabidiol), an endocannabinoid system modulator: basic features and main clinical data. Expert Rev Neurother. 2011;11(sup4):15–9. https://doi.org/10.1586/ern.11.27.
Davis WM, Hatoum NS. Neurobehavioral actions of cannabichromene and interactions with Δ9-tetrahydrocannabinol. Gen Pharmacol. 1983;14(2):247–52.
Grim TW, Samano KL, Ignatowska-Jankowska B, Tao Q, Sim-Selly LJ, Selley DE, et al. Pharmacological characterization of repeated administration of the first generation abused synthetic cannabinoid CP47,497. J Basic Clin Physiol Pharmacol. 2016;27(3):217–28.
Santiago M, Sachdev S, Arnold JC, Mcgregor IS, Connor M. Absence of entourage: terpenoids commonly found in Cannabis sativa do not modulate the functional activity of Δ9-THC at human CB1 and CB2 receptors. Cannabis Cannabinoid Res. 2019;4(3):165–76.
Finlay DB, Sircombe KJ, Nimick M, Jones C, Glass M. Terpenoids from cannabis do not mediate an entourage effect by acting at cannabinoid receptors. Front Pharmacol. 2020;11:359. https://doi.org/10.3389/fphar.2020.00359/full.
Magid L, Heymann S, Elgali M, Avram L, Cohen Y, Liraz-Zaltsman S, et al. Role of CB2 receptor in the recovery of mice after traumatic brain injury. J Neurotrauma. 2019;36(11):1836–46.
Amenta PS, Jallo JI, Tuma RF, Craig Hooper D, Elliott MB. Cannabinoid receptor type-2 stimulation, blockade, and deletion alter the vascular inflammatory responses to traumatic brain injury. J Neuroinflammation. 2014;11(1). https://pubmed.ncbi.nlm.nih.gov/25416141/. Accessed 3 Sep 2020.
Amenta PS, Jallo JI, Tuma RF, Elliott MB. A cannabinoid type 2 receptor agonist attenuates blood–brain barrier damage and neurodegeneration in a murine model of traumatic brain injury. J Neurosci Res. 2012;90(12):2293–305.
Elliott MB, Tuma RF, Amenta PS, Barbe MF, Jallo JI. Acute effects of a selective cannabinoid-2 receptor agonist on neuroinflammation in a model of traumatic brain injury. J Neurotrauma. 2011;28(6):973–81.
Kraus MF, Susmaras T, Caughlin BP, Walker CJ, Sweeney JA, Little DM. White matter integrity and cognition in chronic traumatic brain injury: a diffusion tensor imaging study. Brain. 2007;130(10):2508–19.
Li L, Luo Q, Shang B, Yang X, Zhang Y, Pan Q, et al. Selective activation of cannabinoid receptor-2 reduces white matter injury via PERK signaling in a rat model of traumatic brain injury. Exp Neurol. 2022;347. https://pubmed.ncbi.nlm.nih.gov/34678230/. Accessed 13 May 2022.
Braun M, Khan ZT, Khan MB, Kumar M, Ward A, Achyut BR, et al. Selective activation of cannabinoid receptor-2 reduces neuroinflammation after traumatic brain injury via alternative macrophage polarization. Brain Behav Immun. 2018;68:224–37.
Honig MG, Del Mar NA, Henderson DL, Ragsdale TD, Doty JB, Driver JH, et al. Amelioration of visual deficits and visual system pathology after mild TBI via the cannabinoid type-2 receptor inverse agonism of raloxifene. Exp Neurol. 2019;322. https://pubmed.ncbi.nlm.nih.gov/31518568/. Accessed 1 Sep 2020.
Honig MG, Del Mar NA, Henderson DL, O’Neal D, Yammanur M, Cox R, et al. Raloxifene, a cannabinoid type-2 receptor inverse agonist, mitigates visual deficits and pathology and modulates microglia after ocular blast. Exp Eye Res. 2022;218. https://pubmed.ncbi.nlm.nih.gov/35143834/. Accessed 13 May 2022.
Liu Y, McAfee SS, Guley NM, Mar N Del, Bu W, Heldt SA, et al. Abnormalities in dynamic brain activity caused by mild traumatic brain injury are partially rescued by the cannabinoid type-2 receptor inverse agonist SMM-189. eNeuro. 2017;4(4). https://pubmed.ncbi.nlm.nih.gov/28828401/. Accessed 13 May 2022.
Guley NM, Del Mar NA, Ragsdale T, Li C, Perry AM, Moore BM, et al. Amelioration of visual deficits and visual system pathology after mild TBI with the cannabinoid type-2 receptor inverse agonist SMM-189. Exp Eye Res. 2019;182:109–24.
Arain M, Khan M, Craig L, Nakanishi ST. Cannabinoid agonist rescues learning and memory after a traumatic brain injury. Ann Clin Transl Neurol. 2015;2(3):289–94.
Yang S, Hu B, Wang Z, Zhang C, Jiao H, Mao Z, et al. Cannabinoid CB1 receptor agonist ACEA alleviates brain ischemia/reperfusion injury via CB1-Drp1 pathway. Cell Death Discov. 2020;6(1). https://pubmed.ncbi.nlm.nih.gov/33083022/. Accessed 13 May 2022.
Wang L, Zeng Y, Zhou Y, Yu J, Liang M, Qin L, et al. Win 55,212-2 improves neural injury induced by HIV-1 glycoprotein 120 in rats by exciting CB2R. Brain Res Bull. 2022;182:67–79.
Lawrence DW, Foster E, Comper P, Langer L, Hutchison MG, Chandra T, et al. Cannabis, alcohol and cigarette use during the acute post-concussion period. Brain Inj. 2020;34(1):42–51.
Nguyen BM, Kim D, Bricker S, Bongard F, Neville A, Putnam B, et al. Effect of marijuana use on outcomes in traumatic brain injury. Am Surg. 2014;80(10):979–83.
Taghavi S, Ramirez S, Duchesne J, Tatum D. Preinjury use of marijuana and outcomes in trauma patients. J Surg Res. 2021;257:42–9.
Ali A, Tatum D, Olubowale OO, McGrew PR, Duchesne J, Taghavi S. Thromboembolic outcomes in tetrahydrocannabinol-positive trauma patients with traumatic brain injury. J Surg Res. 2022;275:194–202.
Utter B, Anderson CA, Filley CM, Kelly JP, Johnston-Brooks C, Arciniegas DB. Cannabis use in a cohort of healthcare-seeking united states military veterans with persisting symptoms after mild traumatic brain injury: preliminary observations. Mil Med. 2022. https://pubmed.ncbi.nlm.nih.gov/35064271/. Accessed 13 May 2022.
Knoller N, Levi L, Shoshan I, Reichenthal E, Razon N, Rappaport ZH, et al. Dexanabinol (HU-211) in the treatment of severe closed head injury: a randomized, placebo-controlled, phase II clinical trial. Crit Care Med. 2002;30(3):548–54.
Maas AIR, Murray G, Henney H, Kassem N, Legrand V, Mangelus M, et al. Efficacy and safety of dexanabinol in severe traumatic brain injury: results of a phase III randomised, placebo-controlled, clinical trial. Lancet Neurol. 2006;5(1):38–45.
Acknowledgements
Not applicable.
Funding
Funding for this project was provided by MediCann Health Aust Pty Ltd.
Author information
Authors and Affiliations
Contributions
BRL researched, drafted, and edited the manuscript. CCA and SCH drafted and edited the manuscript, MP, TM, and LDP edited the manuscript. MS funded the research, initiated the project, and approved the manuscript, MF supervised the research and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
This was an industry-sponsored project. Funding from MediCann Health Aust Pty Ltd included salary support for BRL during the tenure of this project. MS is the CEO of MediCann Health Aust Pty Ltd. LDP is a Director of MediCann Health Aust Pty Ltd. MF is the CEO of Connectivity Traumatic Brain Injury Australia. All other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lins, B.R., Anyaegbu, C.C., Hellewell, S.C. et al. Cannabinoids in traumatic brain injury and related neuropathologies: preclinical and clinical research on endogenous, plant-derived, and synthetic compounds. J Neuroinflammation 20, 77 (2023). https://doi.org/10.1186/s12974-023-02734-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-023-02734-9