Abstract
Ophthalmic epidemiology is concerned with the prevalence, distribution and other factors relating to human eye disease. While observational studies cannot avoid confounding factors from interventions, human eye composition and structure are unique, thus, eye disease pathogenesis, which greatly impairs quality of life and visual health, remains to be fully explored. Notwithstanding, inheritance has had a vital role in ophthalmic disease. Mendelian randomization (MR) is an emerging method that uses genetic variations as instrumental variables (IVs) to avoid confounders and reverse causality issues; it reveals causal relationships between exposure and a range of eyes disorders. Thus far, many MR studies have identified potentially causal associations between lifestyles or biological exposures and eye diseases, thus providing opportunities for further mechanistic research, and interventional development. However, MR results/data must be interpreted based on comprehensive evidence, whereas MR applications in ophthalmic epidemiology have some limitations worth exploring. Here, we review key principles, assumptions and MR methods, summarise contemporary evidence from MR studies on eye disease and provide new ideas uncovering aetiology in ophthalmology.
Similar content being viewed by others
Introduction
Causal inference plays a central role in both epidemiological and clinical investigations. Understanding the underlying aetiology is implicit for identifying disease prevention and treatment opportunities. Conventionally, observational ophthalmic epidemiology or clinical studies have identified causal inferences between exposures (lifestyle or biomarkers) and outcomes (ocular disorders) of interest. However, due to different challenges such as unmeasured and residual confounders, where preclinical or disease status influences exposure rather than vice versa, study findings are often controversial [1]. The prospective ophthalmic cohort model is the most reliable causal test assessing the impact of exposures on outcomes. Furthermore, randomised controlled trials (RCTs) also offer high level evidence for causality. Nevertheless, cohort studies or RCTs that elucidate disease outcomes are often unfeasible due to strict quality control, comprehensive design, long-term follow-up, pleiotropic effects of the intervention, ethical issues and a lack of compliance.
Recently, Mendelian randomization (MR) analysis has gradually entered the field of researchers with its new perspective to infer the causal relationship between exposures and outcomes. Based on observational epidemiology, it mainly uses natural variable genes that are not affected by acquired confounding factors as instrumental variables (IVs) for analysis to achieve random assignment to infer potential environmental factors that can lead to disease [2]. Observational studies develop 'Berkson's bias' when investigating associations between exposures and outcomes, resulting in spurious directions of associations by excluding people who were exposed and at lower risk (outcomes) [2]. MR is a term that refers to the fusion of gametes, following Mendel's law of inheritance" parental alleles are randomly assigned to the offspring", genetic variation is unaffected by traditional confounding factors, such as environmental exposure, socioeconomic status, behavioural factors or biomarkers [3]. In diploid organisms, two copies of each allele are normally inherited from the parents, and their associations with disease are chronologically rational. Compared to traditional observational study, MR can overcome confounding issues and reverse causality[4]. With the development of particular research technologies (e.g., large genome-wide association studies (GWAS), epigenetics and metabolomics), MR analysis has been widely used for causal inference; it not only verifies conclusive causality (e.g., glucose levels in normo-glycaemic and higher ranges exerting genetic causal effects on the risk of micro- and macro-vascular disease [5]), but also provides more reliable conclusions for long-standing controversial causal association issues (e.g., some metabolic marker levels are not associated with choroidal neovascularisation [6]). MR combines observational study designs with RCT designs (Fig. 1). The similarities with RCT designs are reflected by randomised subgroups in simulated RCTs which reflect different genetic variation to exposure factors (e.g., vitamin D supplements may increase the risk of Behçet's disease (BD) [7]). Moreover, MR research leverages exposure and outcome data from observational research, which greatly reduces costs. Specifically, MR approaches assess the long-term consequences of an exposure, such as lifestyle or a biomarker, whereas cohort and RCTs typically focus on short-term assessments due to high costs.
The parallel relationship between the design flow charts of the three studies. A Mendelian randomization (MR): It uses randomly assigned the genetic variant to be equivalent to the subgroups of randomized controlled trial (RCT). B RCT: It also divides the population into different subgroups according to the way of random distribution, so that the intervention between groups is different. C Prospective cohort study: It is an observational research method that divides a group of cohorts into exposure group and non-exposure group according to whether they are exposed to a certain research factor to judge whether there is a correlation between the exposure factor and disease
In the last decade, MR analysis has become a popular tool for estimating the causality of an exposure on an ocular outcome. Here, we review the contemporary, state-of-the-art evidence for MR and its associated analytic approaches, further summarise evidence from MR-oriented ophthalmology studies and evaluate potential challenges and prospects for this novel approach.
The MR framework
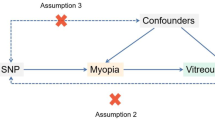
Epidemiologists have long sought an "ideal" method providing clear causality and ignoring potential confounding factors. Over the last three decades, this ideal has turned into reality when IVs were identified [8]. Initially, IV-based techniques were used in econometrics, such as the simultaneous regression equations, structural equations and two-stage least squares (2SLS) [9]. The earliest application of IVs, in modern medicine as we know it, was by Permutt and Hebel in 1989 who studied the relationship between maternal smoking and low birth weight incidences in infants [10]. After this, Greenland [11] comprehensively described the IV methods and its development. MR is advantageous in that it obtains the estimation of causal effect (X–Y) by using genetic IVs (Z) to avoids confounder interference (U). The following three assumptions are the basic assumptions that need to be met for IVs (Additional file 1: Fig. S1):
-
i.
IV Z is robustly associated with exposure, X
-
ii.
The variable Z is independent of an unmeasured confounding factor, U;
-
iii.
The IV Z has an effect on outcome Y mediated solely through exposure X.
But, not all genetic variations can be selected to assess the causal association between the exposure and the outcome. The primary and critical task in MR research has always been to find suitable IVs. The potential limitations required to ensure compliance with the three assumptions are as follows: (1) If genetic variant used as IV is in linkage disequilibrium (non-random correlation between alleles at different loci), another genetic variant in linkage disequilibrium may be associated with confounders, a mediator between IV and exposure (equivalent to vertical pleiotropy), or directly related to the outcome, therefore leading to a violation of the assumptions ii or iii. In this case, the correlation between known confounding factors and IVs should be examined carefully to avoid it. (2) The IVs satisfy hypothesis i, but have weak correlation with exposure, should be investigated in large sample research [12]. (3) The selected sample population must be homogeneous to avoid the confounding of population differences. (4) Pleiotropy is the phenomenon in which one gene locus affects multiple phenotypes, including horizontal and vertical [13].The horizontal pleiotropy refers to genes directly affect multiple phenotypes, and vertical pleiotropy means genes use one phenotype as an intermediary to influence another phenotype. Of note, the horizontal pleiotropy violates the basic hypothesis of MR and might conclude misleading causal estimation. Subsequent sensitivity analysis (e.g. gene pleiotropy test, heterogeneity test and leave-one-out method) can be used to evaluate the robustness of the results and correct for bias.
The design of MR
The early basic MR design can only solve whether there is a causal relationship between exposure and outcome, stay at the logical level, and cannot get the estimation of X causal effect. With the continuous improvement of MR design, two common MR research strategies are formed: one-sample MR and two-sample MR, also known as standard MR. Standard MR optimises the basic MR concept by constructing a quadratic regression model and calculating the estimated value of the effect of X–Y (Additional file 1: Fig. S2). There are also differences in the way of causal estimation in these two MR methods. One-sample MR relies on 2SLS to evaluate causal estimates, using the X value predicted by IV as the independent variable, and performing least squares regression with the outcome Y as the dependent variable. The magnitude of the predicted X value depends on the closeness between the IVs and the exposure, and weak instrumental bias can easily affect the causal estimate. However, the two-sample MR can calculate the causal effect value through two independent GWAS databases, not through the regression of X–Y, but according to the ratio of the regression coefficient of G- Y and G-X. As can be seen from the definition names assigned, the biggest difference between the two is that the subjects of one-sample MR are from a single population; the subjects of two-sample MR are from two independent samples of the same population. Research development of large-scale GWAS has made two samples MR data acquisition becomes more convenient, in-depth study of field and more widely. To adequately explore causality, MR methods are continuously developing (Additional file 1: Fig. S3). Two-step MR and bidirectional MR need to be analyzed twice in two samples. Two-step MR involves mediators which identify potential pathogenesis in the causal relationship between exposure and outcome, while bidirectional MR clarifies the direction of the causal correlation. Similarly, pleiotropic genetic variations are associated with homogeneous multi-classification exposure factors, thus a multivariable MR approach is appropriate.
MR theory
The fundamental reason for the widespread popularity of MR stems from the steady stream of sharable genetic data provided by large-scale GWAS studies conducted among collaborating groups around the world. In addition, the continuous improvement of MR design strategy can also make causal inference using multi-IVs. Several MR analyses based on summary data using multi-IVs are commonly used (Table 1).
The inverse variance weighted (IVW) method
The IVW method was proposed by Burgess et al. and is used in multi-instrumental variable MR analysis [14, 15]. Herein, we define \(G = \left\{ {G_{1} ,\,G_{2} ,G_{3} ...G_{J} } \right\}\) as IVs, X as an exposure factor and Y as an outcome. We assume the j-th VI (\(G_{j}\)) has an impact on exposure factor and outcome, as \(\widehat{\beta }xG_{j}\) and \(\widehat{\beta }yG_{j}\), respectively. Furthermore, their standard errors are \(\sigma_{{\widehat{\beta }xG_{j} }}\) and \(\sigma_{{\widehat{\beta }yG_{j} }}\), respectively. The corresponding causal effect value is obtained by the ratio method: \(\widehat{\beta }xy_{j} = \widehat{\beta }xG_{j} /\widehat{\beta }yG_{j}\)
After this, we calculate the causal effect value between exposure factor and outcome:
The asymptotic variance of this IV estimator is given by the formula:
where \({\sigma }_{{\widehat{\beta }}_{Y{G}_{J}}}^{-2}\), is defined as a weight, and weighted linear regression is used to force the intercept term of linear regression to be 0, whereas:
Then, the correspondence causal effect is:
MR Egger regression
MR Egger regression is an update version of the IVW method where multi-effects exist between IVs. The formula is:
Generalised summary data based MR (GSMR)
GSMR is based on summary data based MR (SMR). The estimated effect of IV is \({\widehat{\beta }}_{\mathrm{XY}}=\left\{{\widehat{\beta }}_{X{Y}_{1}} , {\widehat{\beta }}_{X{Y}_{2}} , \cdot \cdot \cdot {\widehat{\beta }}_{X{Y}_{\mathrm{j}}}\right\}\) and the variance–covariance matrix is:
MR ophthalmology studies
Many studies have explored, confirmed and quantified causal relationships between potential exposures and the risk of eye disease. To investigate the application of MR to eye disease, we systemically searched PubMed, EMBASE and Web of Science databases for studies using the search keywords, “Mendelian randomization” with any outcomes related to “eye OR ocular OR ophthalmology”. Database were searched from inception to 1st May 2021.
Inclusion criteria: (a) the exposure of interest was a lifestyle or biological factor related to eye disease, (b) the outcome was any eye disease and (c) genetic variants or genetic risk scores (GRS) were proposed as IVs to analyse the effects of exposures on outcomes. We excluded articles that did not use MR to explore causal associations in ophthalmology. Also, we excluded studies where ophthalmic conditions were identified as exposures rather than outcomes. Finally, 66 studies were included and independently reviewed by two co-authors (JXL & LL); any disagreements were resolved by discussion. These studies provided information on factors associated with eye disease aetiology (Table 2). Due to rapid developments in ophthalmology genetics research, we envisage MR will become widely used and help identify both modifiable and non-modifiable causes of disease.
Age-related cataracts and obesity
Age-related cataracts are defined by opacity of the lens due to lost optical clarity concomitant with ageing, and are common causes of vision loss worldwide [16]. Energy and nutrient intake are involved in cataract formation and progression [17]. Several epidemiological studies have also identified a link between obesity and cataracts [18, 19]. An Asian population study used MR analysis to identify causal associations between fat mass, the obesity-associated gene (FTO) and various types of senile cataracts [20]. Accordingly, no causal associations were identified between obesity and cortical or posterior subcapsular (PSC) cataracts, whereas FTO was putatively involved in nuclear cataract pathogenesis. However, this study did not test the three key aforementioned MR assumptions. It is noteworthy that genetic variations at the FTO locus are associated with lipid metabolism pathways. Thus, further studies are warranted to investigate if lipid metabolism has a potential role in cataract pathogenesis. In another study, a two-stage MR approach was used to process Blue Mountains Eye Study data, and identified the single nucleotide polymorphism (SNP), rs9939609 as strongly related to exposure (obesity); the SNP was used as an IV to analyse the causal relationship between obesity and age-related cataracts [21]. Furthermore, different regression models were applied to verify the MR hypothesis (assumption i and ii). Interactions between the FTO SNP and protein intake were shown to increase the risk of PSC cataracts in individuals with dyslipidemia. However, these studies reflected a common issue with MR: no method has yet been identified to verify the existence of horizontal pleiotropy.
Age-related macular degeneration (AMD) and related risk factors
Globally, AMD is a leading cause of blindness in the elderly. Several studies have proposed that particular genes are involved in AMD pathogenesis and may participate in inflammatory and complement pathways [22,23,24]. The Y402H SNP in the complement factor H gene, CFH is associated with AMD [25,26,27]. Increased CFH expression was observed in vitro in cultured (dedifferentiated) human retinal pigment epithelium (RPE) cells by immunohistochemistry [27]. CFH variations may lead to the improper control of the local complement system which triggers drusen formation [25]. Based on this evidence, a North Indian population-based study used MR on CFH rs1061170 as an IV to demonstrate the polymorphism affected AMD occurrence or progression by modulating serum CFH levels [28]. From their findings, CFH (rs1061170) C allele carriers had an increased risk of AMD due to decreasing serum CFH levels. Proteomic analyses subsequently confirmed that some major proteins (e.g., C-reactive protein, (CRP)) occur in drusen as hallmark lipid and proteinaceous deposits [29]. Furthermore, to assess the causal relationship between circulating CRP levels and AMD, Han et al. selected SNPs associated with serum CRP levels as IVs for two-sample MR analysis [30]. They performed IVW analysis, then multivariable MR analysis which regressed several potential AMD factors based on univariate analysis. Combined, these authors showed that inflammatory pathways were involved in AMD pathogenesis, and that CRP was causally related to AMD. Unfortunately, this study did not use the non-linear IV hypothesis to test non-linear relationships between circulating CRP levels and AMD. Thus, further investigations are required to manage non-linearity in similar MR analyses.
In clinical epidemiology, AMD is commonly classified into early, intermediate and late stages. Late-AMD stages often lead to visual impairment and even irreversible loss of central vision [31, 32], and its treatment modality is different to other AMD stages. In early and intermediate AMD stages, pigmentary abnormalities and extracellular aggregate (drusen) accumulation occurs in the macular region [24, 33]. Moreover, lipid is a structural component of drusen [34]. Several observational studies explored relationships between lipid profiles and AMD risk and concluded that high levels of high-density lipoprotein cholesterol (HDL-C) increased disease risk [35,36,37,38]. However, owing to different study designs and sample sizes, potential confounding factors and reverse causality cannot be excluded, thus conclusions remain largely inconsistent [39, 40].
Importantly, GWAS have been instrumental in identifying associations between AMD and some genetic variants, such as hepatic lipase (LIPC) [41], cholesterol ester transfer protein (CETP) [42] and apolipoprotein E (APOE) [43]. Subsequently, several studies have exploited these genes to explore causal effects in different lipid pathways in AMD [44,45,46]. A previous two-sample MR study conducted in European ancestry individuals from the International Age-Related Macular Degeneration Genomics Consortium, involving 185 lipid-related genetic variants as IVs, identified a causal relationship between HDL-C and AMD, with an odds ratio (OR) of 1.22 [47]. In fact, some of the lipid deposition associated with AMD comes from the induction of the retina. Thus far, no validated IVs have been identified for retina lipids. Additionally, a multi-ethnic genetic study using three different MR models showed that HDL-C was a causal factor for advanced AMD [48]. Both studies used multivariable MR analyses which advantageously adjusted pleiotropy caused by incomplete independence between genetic variations and tested exposure variables.
Due to the huge variety of lipids and different AMD stages, specific research on relationships between lipid subcomponents and early and intermediate AMD stages is lacking. Recently, a large-scale study using a two-sample MR approach investigated the causal effects of eight major serum lipid biomarkers toward different AMD subtypes [6].Using a multivariable MR method based on Bayesian model averaging applied to exposure factors, the study identified lipid metabolism (apolipoprotein A1 and apolipoprotein B) functions in drusen formation, in particular at early and intermediate AMD development stages. MR approach based on Bayesian model averaging (MR-BMA) is a new modality for multivariate MR that incorporates more lipid particles using high-throughput experiments. Verena Zuber et al. used this method to prioritize risk factors by marginal inclusion probability (MIP), and then repeated analysis by modifying a posteriori probability, finally verified the strong causal effect of HDL on AMD, and also found the causal relationship between large and extra-large HDL particles and AMD [49]. The verification idea of MR-MBA is also superior to the IVW method of biased estimation of risk factors. It believes that the risk factors that really play a causal role themselves are a minority of a large number of risk factors, and more risk causal factors can be found through screening and sorting.
Apart from lipid profiles, a previous systematic review summarised several other potential risk factors for AMD [50] and showed inconsistent associations between refractive error (RE) and disease [51, 52]. Wood et al. conducted a two-sample MR study with IVW, and selected 126 genetic variants associated with RE as IVs to verify if RE was a risk factor for AMD in individuals of European descent [53]. Their analysis showed that hyperopia had a minimally positive causality with AMD, with an OR = 1.08. In addition, their sensitivity analyses, after excluding 31 variants closely related to non-RE traits, generated similar results (OR = 1.069). These inconsistent associations between RE and AMD may be due to non-causal factors such as parametric variations, stochastic fluctuations, potential confounders or selection bias.
RE and related factors
RE is associated with many eye abnormalities and is one of the most common causes of visual dysfunction [54] For example, the pathological consequences of myopia, including exudative myopic macular degeneration and rhegmatogenous retinal detachment (RRD), are common causes of irreversible blindness [55]. Conventionally, observational epidemiological studies have postulated associations between some lifestyle exposures and myopia. For instance, education level was commonly regarded as a social factor leading to myopia onset, however, it is unclear if the relationship is causal [56]. Therefore, Cuellar-Partida et al. used GWAS education polygenic risk scores/data from the Social Science Genetic Association Consortium as IVs, and used a two-stage least squares approach to explore causal relationships [57]. Their analyses suggested a causal relationship existed between education and myopia, with estimated effect sizes higher than observational study estimates. Above findings have advantages in terms of strengthening due to the mediating variables that may confuse causality mentioned in the previous article were also excluded in the process of MR analysis [58, 59]. However, the other side of this causal relationship may be overestimated due to the existence of other education-associated markers (e.g., time spent on study). Therefore, more studies are required to investigate causal relationships between education and myopia, adjusted for more potential confounders.
To fully understand causal links between education and myopia, a bidirectional MR study based on the UK Biobank used a specific set of seven different assumptions and suggested exposure to more years in education increased myopia risk [60]. Two analyses in bidirectional MR, only one proved the causal relationship between the two variables: the longer the education, the more likely to develop myopia. This study is significant for strengthening the myopia prevention because it replaced the traditional regression analysis to detect potential pleiotropy.
Despite evidence from observational studies showing associations between myopia and vitamin D levels, the causal evidence for vitamin D associations with myopia is lacking, and are independent of outdoors activity times [61] or other related factors (e.g., time spent at work or exposure to natural light) [62, 63]. In view of this, Cuellar-Partida et al. selected effect estimates from a large RE meta-analysis from the Consortium for Refractive Error And Myopia (CREAM) and three other young cohorts to calculate causal estimates between vitamin D levels and myopia using Wald-type ratio estimators in an MR framework [64]. Valid and significant IVs identified by this study included 25-hydroxyvitamin D [25(OH)D] SNPs, as also determined by Afzal et al. [65] and Mokry et al. [66]. The meta-analysis identified no genetic causal links between 25(OH)D levels and myopia and further suggested associations were mediated by potential factors, including outdoor exercise times. Importantly, this analysis reflected a major MR benefit, i.e., unlike the temporary influence of exposure factors reflected by measured values in observational studies, MR IVs reflect the long-term exposure-induced state of the research factors.
In ophthalmologic anatomy, axial length (AL) and corneal radius of curvature (CR) are the two main physiological indicators of emmetropia. Previous studies reported that changes in children's growth trajectory could predict RE [67] and that correlations existed between birth parameters and ocular biometrics [68]. Tideman et al. conducted an MR analysis using weighted GRS as IVs and linear regression analysis to identify associations between prenatal and postnatal growth variables and AL and CR[69]. These authors showed that body growth parameters were significant predictors for a higher AL and corneal curvature (CC) by the age of six. The same genetic pathways between birth parameters and ocular biological indices were related to the study of causal associations between foetal growth, infancy, early childhood and REs.
Additionally, a low birth weight (LBW) is considered a common cause of visual impairment, and its relationship with RE has attracted considerable attention [70]. Some observational studies reported that LBW increased the risk of RE in school-age children (7–12 years) [71, 72], however, it was unclear if individuals with LBW within the normal birth weight range experienced RE in adulthood. Therefore, a one-sample MR analysis with GRS’s as IVs and a linear regression analysis was conducted, and showed that LBW within the normal range was causally associated with a more myopic RE, while the impact of causal effects was modest in UK Biobank participants [73]. In fact, race/ethnicity are factors associated with myopia; the myopia prevalence in East and South-East Asian is higher than European populations [55, 56]. Thus, future research must identify causal relationships between LBW and refractive changes, especially in Asian populations.
Currently, it is difficult to distinguish the effects of different environmental factors on RE, which are primarily due to heterogeneous exposure in the population. A causal role for particular medications in promoting RE was described long before MR research commenced [74]. For example, dorzolamide is a sulfonamide drug and was previously linked to transient myopia episodes [75, 76], whereas the same conclusion was drawn from a recent MR study by Patasova et al. [77]. Due to inevitable correlations between some medications and primary disease, Patasova et al. used SNPs associated with primary diseases as IVs and their effects over spherical equivalent (SE) for the outcome and suggested a causal effect of multisite chronic pain over hyperopic RE 74. One of the underlying causes of hyperalgesia is the lower threshold of sensory neuron firing, which may be related to genetic variations affecting proton-gated cation channels [78]. Likewise, RE is related to genetic polymorphisms in deionised cation channels [79]. Moreover, chronic pain may activate autonomic responses leading to pupillary dilation and accommodation relaxation [80]. Interestingly, this latter MR study showed that higher intraocular pressure (IOP) caused a greater myopic degree (MR-Egger P = 0.02), but without directional pleiotropy (intercept P = 0.256). Notably, this relationship was not mediated by IOP-lowering medication [81]. Furthermore, researchers observed that oral anti-diabetes drugs (metformin or gliburonide) may directly cause RE (MR-Egger P = 0.003, intercept P = 0.166). These findings suggest the effects of drugs on the ocular system must be accounted for when treating specific diseases.
RRD and IOP myopia
RRD is one of the main emergency indications in ophthalmology and is the most common retinological emergency threatening vision [82, 83]. Several studies reported that when compared with non-myopes, individuals with greater changes in SE were at a greater risk of RRD and suggesting myopia may be a risk factor for RRD [84, 85]. Surgery is one of most common treatments for RRD, however, IOP may change after this surgery [84, 85]. Han et al. conducted a two-sample MR analysis using the GWAS dataset from the UK Biobank cohort and identified a causality between myopia, IOP and the risk of RRD [86]. In the same study, the effect of mean SE on RRD was greater than IOP, whereas a weak correlation was identified between mean SE and IOP. Furthermore, in subsequent sensitivity analyses, a stable causal effect of IOP on RRD was verified by excluding SE loci from IOP genetic structures using multivariable MR analysis. Myopia and IOP were causally associated with the risk of RRD, thus, myopia prevention efforts could help prevent disease. In the future, specific measures must be evaluated to prevent myopia during RRD, such as using atropine [87] and increasing outdoor activities [88].
Glaucoma and related risk factors
Glaucoma is a common leading cause of irreversible blindness; by 2040, it is estimated that approximately 118 million people will suffer with the condition [89]. Progressive retinal ganglion cell degeneration and unique visual field-loss are the main clinical manifestations of primary open-angle glaucoma (POAG) [90]. Unfortunately, due to asymptomatic glaucoma, deriving a correct diagnosis at early disease stages in many patients is difficult [91]. The 2013 US Preventative Services Task Force recommendation statement reported that IOP was a modifiable risk factor in patients with POAG; its decrease prevented disease progression and emphasised the importance of an early diagnosis and treatment [92]. Notably, 10%–20% of POAG patients have normal or low IOP or "normal tension glaucoma" [93]. Therefore, glaucoma control measures cannot use IOP as the only indicator; in fact, many other factors are associated with glaucoma, such as hyperglycaemia. To the best of our knowledge, diabetes cannot only cause micro-vascular lesion-diabetic retinopathy, but may be associated with glaucoma [94, 95], however, epidemiological and clinical studies have not established a causal link between these conditions [96, 97]. Most studies, using MR analysis, have focussed on relationships between POAG and type 2 diabetes (T2D) [94, 95]. Previous studies screened relevant SNPs from an external GWAS database [98,99,100], calculated different genetic risk indices (overall genetic risk index and mechanism-specific genetic risk indices) as IVs, and confirmed causality between T2D and POAG using mechanism-specific genetic IV analyses. Furthermore, these authors emphasised the key role of pancreatic β-cell functions in POAG. Since T2D is a binary variable, this conclusion suggested T2D patients with metabolic disorders caused by pancreatic β-cell dysfunction would have a higher glaucoma risk. These studies also reported that the pleiotropic melatonin receptor 1B gene (MTNR1B) may have directly affected POAG via other mechanisms, independent of T2D. Accordingly, two loci (rs7708285 and rs6943153) were nominally significantly associated with POAG via fasting blood glucose, but the direction of effect was opposite. Thus, more studies on causal associations between fasting blood glucose and POAG, and the role of MTNR1B in POAG susceptibility are warranted.
Apart from diabetes, relationships between other metabolic disorders and IOP have been expounded [101, 102]. Hysi et al. reviewed the impact of different factors on IOP using metabolomics, Random Forest machine learning algorithms, and MR-IVW analyses to explore relationships between circulating metabolites and IOP [103]. From three MR models, O-methylascorbate had a significant IOP-lowering effect. Specifically, raising the levels of this metabolite reduced IOP causally, while IOP had no causal effect on O-methylascorbic levels. O-methylascorbate is a circulating metabolite of vitamin C, which is an antioxidant vitamin. In future research, it will be important to extrapolate if vitamin C alters IOP through antioxidant stress mechanisms [104].
Hyperlipidaemia is also a widely studied POAG biomarker [105, 106]. A two-sample MR analysis using GWAS summary data as IVs, involving three plasma lipid components (low density lipoprotein cholesterol [LDL-C], HDL-C and triglyceride (TG)) as exposure variables, showed no significant causal relationships between hyperlipidaemia and POAG risk [107]. However, only a causal association between routine lipid components and POAG was identified [107]. In fact, several other lipoprotein particles defined by the internal lipid content affected the biological function of lipid metabolites [108, 109]. Nusinovici et al., using a Bayesian network analysis, showed that total HDL-C was directly associated with POAG [110]. SNPs that correlated with HDL-C were then selected as IVs for MR-IVW, weighted median, mode based estimator and configuration mixture (Remix) method analyses. The findings suggested a causal and specific relationship between HDL-C and POAG. Mechanistically, small, dense HDL sub-fractions could mediate the cholesterol outflow pathway via the ATP-binding cassette 1 transporter (ABCA1) pathway [111, 112]. Also, imbalanced cholesterol levels can affect neurodegenerative disease [113]. High cholesterol-24-hydroxylase levels were identified in the retinas of glaucoma patients which may have damaged optic ganglion cells [114]. Additionally, HDL could contribute to POAG by influencing choroidal blood perfusion processes [115]. Therefore, future functional studies on different lipid particles must examine if these molecules participate in glaucoma pathological mechanisms by affecting blood perfusion.
Corneal hysteresis (CH) and corneal resistance factor (CRF) are both quantitative genetic indicators of corneal biomechanics. CH is a dynamic marker reflecting corneal structural and functional changes associated with IOP [116, 117]. CRF is calculated using a coefficient that emphasizes the first applanation. These biomechanical properties affect corneal-compensated IOP (IOPcc) measurements, which are used as estimated IOP values [118, 119]. Both indicators are genetically associated with ocular phenotypes and disease [120,121,122]. Simcoe et al. identified more than 200 loci related to corneal biomechanical properties using GWAS and the UK Biobank database, and conducted MR analysis to prove causal relationships between corneal biomechanics and IOP, and the directions of effect showed increased IOPcc reduced CH while simultaneously raising CRF [123]. This study also identified an association between genetically induced CRF and POAG, thus, future work could explore if the effects of CRF on POAG are driven by IOP.
A previous study reported that acute IOP increases could be associated with caffeine intake [124]. Although no links were identified between habitual caffeine intake and IOP changes in healthy subjects, increased caffeine consumption was associated with IOP increases in subjects with increased IOP susceptibility [125]. Similarly, consistent outcomes were identified in individuals with a family history of glaucoma [126]. Currently, causal evidence is lacking on whether reductions in long-term caffeine intake can control IOP and reduce glaucoma risks. Kim et al. conducted a two-sample MR analysis (UK Biobank database) using eight SNPs, which were significantly related to caffeine intake as IVs, to assess causal relationships between intake and IOP. Also, polygenic risk scores related to high IOP were calculated to test if genetically induced higher IOP altered associations between caffeine intake and IOP [127]. These authors observed a weak effect of long-term caffeine consumption on reducing IOP, but no causal relationship was identified. In contrast, in subjects with a strong genetic susceptibility to higher IOP, greater caffeine consumption would increase IOP and lead to higher glaucoma prevalence.
Another important corneal biomechanical indicator, central corneal thickness (CCT) shows strong heritability, with variability dependent on ethnicity [128, 129]. In a South African Eye Study, CCT in Africans was significantly lower than in other races [130]. Furthermore, a thinner CCT was identified as a risk factor for POAG [131]. Choquet et al. selected the main CCT related single nucleotide variants as IVs for a two-sample MR analysis, and showed a null causal association between thinner CCT and POAG [132]. From these results, the phenotypic effect of a single SNP may have been reduced by the data inclusion criteria, or other factors such as the environment or epigenetics may have contributed.
A SMR analysis was conducted in Asian and European populations; multiple genes, CLIC3, ILMN_1796423, PTGDS, ILMN_1664464, C9orf142 and ILMN_1761138 were identified and showed pleiotropic associations with CCT, but only in European ancestry participants [133]. Importantly, this study reflected the role of gene expression traits on outcomes in an MR framework. However, expression quantitative trait loci (eQTL) data were obtained from blood rather than eye tissue, and the same eQTL data were used in the analysis of different races. In the future, eQTL data must be sought from human eye tissue, and data analysis must be expanded to different races.
Optical coherence tomography (OCT) is an intravascular imaging technology widely used for the early diagnosis and management of ophthalmic diseases [134, 135]. Previous research showed that the thickness of the two inner retina layers, the retinal nerve fibre layer (RNFL) and ganglion cell inner plexiform layer (GCIPL), could change at different glaucoma stages, suggesting these indices could function as biomarkers for predicting glaucoma [136, 137]. A two-sample MR analysis using OCT images from 31,434 UK Biobank participants identified a relationship between morphological retinal phenotypes (RNFL and GCIPL) and POAG [138]. Because the causal relationship between IOP and POAG was clear, this study concluded the combination of time and IOP made the inner layer of retina thinner. Also, GWAS outcomes showed that three chromosomal loci, 1q42.3, 17q25.3 and 21q22.13 were related not only to eye pigmentation which caused foveal hypoplasia, but also eye colour [139]. These loci were also significantly related to visual acuity. Based on known genes, we can study associations between appropriate exposure factors related to them (such as changes in eye structure colour or the change force of skin and hair colour) and vision loss. OCT images combined with MR analyses could help unravel the biological function of different retina layers and provide insights on causal relationships between retinal morphology and eye disease.
Diabetic retinopathy (DR), plasma lipid and adiponectin (APN) correlations
Globally, DR is one of the leading causes of blindness in working-age individuals [140], therefore, identifying and modulating risk factors is essential in preventing this condition. However, the underlying causal factors remain unclear. A previous study used GWAS summary data to investigate if lipid changes causally increased DR risk, using MR-IVW methods across three subgroups comprising all ethnicities, Caucasians and Chinese [141]. No clear evidence suggested dyslipidaemia increased the risk of DR. However, an analysis of 12 pleiotropic TG-associated SNPs in the model suggested IVs could be associated with other lipid components. Three rs12678919, rs174546 and rs964184 SNPs were closely associated with the proliferator-activated receptor-α (PPAR-α) gene which is used to treat DR by reducing TG levels [142]. These observations suggested TGs may be involved in DR formation. However, as study data comprised summarised statistical data from large GWAS studies, no accurate blood lipid values were identified, therefore extrapolations to clinical settings are limited.
A correlation was previously identified between APN and DR. A previous meta-analysis showed APN levels were significantly associated with DR in patients with T2D [143]. An observational cohort study also examined if elevated APN levels accelerated retinopathy progression in patients with T2D, and suggested APN could be a biomarker for DR pathogenesis [144]. APN is an adipokine secreted by fat cells and has a variety of functions, including promoting blood vessel formation [145] and endothelial cell inflammatory responses [146]. To comprehensively ascertain if APN played an essential role in DR pathogenesis, Huang et al. performed an MR-IVW analysis on three SNP groups (GRSALL, GRSLimited and GRSAPN) which were previously differentially correlated with APN levels, by setting different thresholds and calculating the GRS of each group as an IV [147]. The reason for choosing GRS: through the calculation of F statistic, it was found that there were numerous weak IVs among APN-associated SNPs. A causal association between APN and DR was not fully proven, as only data from IVs- GRSALL suggested elevated APN levels could causally increase DR risk. Interestingly, this causal relationship between APN and DR only focused on T2D. It was previously suggested that the effects of APN on inflammatory markers in type 1 diabetes (T1D) or T2D was opposite [148, 149]. Therefore, the effects of APN on DR in T1D patients must be comprehensively examined in future studies.
Retinopathy, plasma lipid and glucose level correlations
Emanuelsson et al. used weighed allele combined scores from 11 gene variants related to LDL-C levels as IVs in a one-sample MR analysis to predict the causal impact of LDL-C on micro- and macro-vascular diseases, e.g., retinopathy [150]. Consistent with two-sample MR results, high LDL-C levels were not a causal risk factor for retinopathy and neuropathy, but a causal relationship existed between LDL-C, chronic kidney disease (CKD) and peripheral arterial disease (PAD) in the general population. The data showed LDL-C had different roles in both micro- and macro-vascular disease 147. Peripheral neuropathy is the most prevalent chronic diabetes complication and is based on sensory and autonomic nerve symptoms. Currently, treatments of peripheral neuropathy are limited to anti-diabetes drugs [151]; a previous meta-analysis reported these drugs could only improve diabetes development, with no apparent significant effects on neuropathy [152]. Therefore, it is important to ascertain if causality exists between glucose control and neuropathy. In other research, Emanuelsson et al. further explored the causal effects of glucose levels on micro- and macro-vascular disease (including retinopathy, nephropathy, CKD, neuropathy and PAD) [5]. Apart from PAD, they showed a causal relationship between glucose levels and micro- and macro-vascular disease.
BD and related risk factors
BD is a chronic, multi-system disease of unknown aetiology [153, 154]. It causes pathological damage to various organs, comprising oral and genital ulcers and ocular and cutaneous lesions [155]. Although BD pathogenesis is unclear, genetic susceptibility, infection triggers and immune abnormalities have been identified as the main pathogenic mechanisms [156]. Previous studies reported that patients with BD could be treated by vitamin D supplementation to modulate immune and inflammatory responses [157,158,159]. Zhong et al. used allele scores formed by four variants related to serum 25(OH)D levels as IVs to show that higher serum 25(OH)D levels increased BD risk [7]. However, the study conclusions contrasted with the protective effects of vitamin D on BD in observational studies [158, 159]. Therefore, potential BD development must be monitored after high-dose or long-term vitamin D intake. BD is also characterised by typical clinical features such as uveitis [160], which has a prevalence of 38–714/100000 individuals [161]. Uveitis causes serious damage to the eye tissue and leads to eye complications, including cataracts, glaucoma and ocular tuberculosis [162]. Pathophysiologically, Mycobacterium tuberculosis causes inflammatory immune response in the body [163], but no evidence based on MR analyses have been reported. However, Zhong et al. conducted MR and mycobacterium tuberculosis T cell spot test (T-SPOT.TB) analyses and showed that tuberculosis infection increased the risk of several non-infectious uveitis conditions [164].
Macular telangiectasia (MacTel) and metabolic pathways
MacTel is an uncommon ocular disorder potentially causing legal blindness, however, its pathogenesis is unclear [165]. From recent GWAS findings [166], Bonelli et al. performed an MR analysis and showed that serine depletion was the strongest causal driver of MacTel risk [167]. In addition, some MacTel-associated loci exerted protective roles toward retinal endophenotypes, suggesting similar pathogenetic pathways could exist between other eye diseases involved in retinal endophenotypes and MacTel. The study also identified a weak correlation between T2D and MacTel. Another larger-scale GWAS and MR analysis observed similar findings, with a significant causal effect of low serine levels on MacTel aetiology [168]. In addition, gene expression involving metabolic disorder in the aetiology of MacTel is more concentrated in RPE. More clinical studies must focus on how moderate serine levels could limit this condition.
Retinal vascular calibre and blood pressure (BP)
Retinal arterial narrowing is associated with higher BP and ambulatory BP monitoring [169]. However, another study observed no correlation between BP and retinal venular calibre [170], while a population-based cross-sectional study showed that systolic blood pressure (SBP) was positively correlated with retinal venular diameter [171]. Li et al. performed a traditional multi-linear regression and MR analysis to explore correlations and causalities between different BPs and retinal vascular calibre [172]. From their findings, elevated diastolic blood pressure (DBP) and mean arterial pressure (MAP) displayed weak causal roles with arteriolar lumen diameter, but no causal relationship was identified between retinal venular calibre and BP levels. Since potential factors during pleiotropic testing studies were not comprehensive, further analyses are required to determine causal associations between other factors (blood glucose and blood lipids) and retinal venular diameter to prevent the occurrence and development of related chronic diseases.
Opportunities for MR in ophthalmology
MR applies IV methods to observational data; IVs are genetic variants that provide reliable evidence inferring causal relationships between exposures and outcomes. Thus, MR has become instrumental in dissecting residual ophthalmology issues by combining genomics and other disciplines. Currently, large-scale GWAS have been used to identify gene loci related to eye traits and diseases, which have not only provided essential support for gene targeted therapies, but also identified preventable and modifiable environmental risk factors using MR. Indeed, specialised ocular trait measurement instruments are often required to identify apparent features in the eyes or physiological indices inside the eyeball. To measure eye traits that are not readily available, MR is a convenient tool as it analyses gene expression from blood tissue as IVs to identify exposure factors [133]. In addition, MR is also used to analyse the causal role of specific pathological pathways involved in common ocular diseases (e.g. how the pancreatic β-cell-pathway in T2D increases the risk of POAG [100]). These examples show how much underlying disease pathologies in ophthalmology have been clarified. With the development of technology, novel MR techniques have been applied to ophthalmology research, which can solve the directionality of causality and the interaction between phenotypes. In fact, there are three assumptions before implementing the MR method to make causal inferences between exposures and outcomes: 1. There is a causal relationship between exposures and outcomes; 2. There is no causal relationship between exposures and outcomes; 3. There is a bidirectional causal relationship between exposures and outcomes. When the basic MR method cannot fully explore these three situations, bidirectional MR becomes an auxiliary method to clarify the sequence of causality [173, 174]. A typical example in ophthalmology research is that education level is related to myopia. In a study using bidirectional MR, it is found that the causal relationship between them is unidirectional, and there is no reverse causality (the idea that myopia takes longer to learn is not valid[60]). In addition, the other advanced MR approach, multivariable MR analysis, which can be performed to identify associations between multiple categorical exposure factors with similar effects, allows genetic variants to be associated with more than one exposure in this analysis. At present, there are an increasing number of researches using multivariable MR analysis, which has played a unique advantage in the exploration of the etiology of mental illness and cardiovascular disease [175, 176]. The advantage of multivariable MR is that eliminating the exposure factors with strong causality and exploring the causality values of the exposure factors with relatively weak correlation (for example, IOP, which is weakly correlated with SE, has less influence on RRD than IOP, but IOP still has causal influence on RRD[86]).
MR challenges in ophthalmology
Because so many eye diseases exist, and the visual damage caused by lesions in different positions of the eye are rarely the same, MR analysis can be used to identify unclear risk factors in ophthalmic diseases. Glaucoma is a severe ocular pathology and its most critical risk factor is IOP, however, this still does not explain the pathogenesis of all glaucoma types. In addition, it is unclear if substandard physiological indicators at birth (including height and weight) causally increase the risk of developing eye disease, therefore these indicators should be investigated. The exploration of causal factors with indispensable roles in cataractogenesis should not remain on obesity. Importantly, significant racial and ethnic differences impact on the generation of most eye diseases. However, gene identification presents two issues during MR analyses; in two-sample MR, public summary gene data from similar ethnic groups are not readily available. No large-scale GWAS have been conducted for some eye diseases, or genetic data are lacking for eye diseases across some races and ethnicities. Furthermore, as outlined (Table 2), the UK Biobank database is predominantly used in most studies and includes mainly European populations, the impact of sample overlap should be considered when discuss these studies. From our review, other databases exist; CREAM, the International AMD Genomics Consortium (IAMDGC) and the International Glaucoma Genetics Consortium (IGGC) and specialise in specific eye diseases. In addition, genetic data may not fully identify exposure factors to generate true causal associations. Genetic induction at the cell and molecular level is also worthy of investigation. For example, in addition to circulating lipids implicated in AMD, specific retinal effects on lipid pathways also affect AMD pathological mechanisms [47]. Although MR-Egger regression intercepts, pleiotropy residual sums, outlier global tests, and PhenoScanner have been used to assess pleiotropy or horizontal pleiotropy using IVs, wide-spread horizontal pleiotropy may potentially exist, which leads an important statistical challenge on assumptions being violated and biased statistical inference. Therefore, scientists must fully consider horizontal pleiotropy among IVs when drawing conclusions. At the same time, although the advanced MR approach can solve the phenotypic relationship with complex causality, there are also some problems in practice. When there is a bidirectional causality between exposures and outcomes, the difficulty in implementing bidirectional MR lies in the selection of reasonable genetic variants, as there will inevitably be an association between genetic variants associated with exposures and outcomes. Then, in order to avoid collinearity, multivariable MR also has requirements for the number of genetic variations: its number cannot exceed the number of exposure factors.
Conclusion and future directions
In spite of the many promising applications of MR, the validity of causal findings depends on three key assumptions (i—iii) on valid IVs, which sometimes may not hold in practice. In fact, numerous open GWAS databases exist in different jurisdictions. Researchers can search for SNPs as IVs using GWAS catalogues and search for keywords related to the subjects to prove that they are not related to other traits, so as to satisfy the assumption [7]. From a methodology perspective, no clear and unified test method has yet indicated if pleiotropy IV’s exist in MR. The interpretation of MR results requires the consideration of numerous factors, including study design, appropriate IVs and biological complexity. A deep understanding of gene-environment interactions using BioBank genome-wide data on genetics, demographics, clinical factors and lifestyle habits may help triangulate with ophthalmic MR studies. Given the rapidly evolving research landscape, the replication of early MR studies using larger-scale multicentre investigations and improved genetic instruments continues to be of value.
In short, MR has improved ophthalmology research and helped researchers prevent and treat ophthalmic diseases. Equally, MR studies continue to provide strong evidence showing causal inferences between exposure factors and outcomes, which may guide future clinical trials and drug development, and provide a theoretical basis for clinical and public health decision-making.
Availability of data and materials
There is no new data generated as part of this review.
References
Cornish AJ, Tomlinson IPM, Houlston RS. Mendelian randomisation: A powerful and inexpensive method for identifying and excluding non-genetic risk factors for colorectal cancer. Mol Aspects Med. 2019;69:41–7.
Smith GD, Ebrahim S. Mendelian randomization: prospects, potentials, and limitations. Int J Epidemiol. 2004;33(1):30–42.
Lin LJ, Wei YY, Zhang RY, Chen F. Application of mendelian randomization methods in causal inference of observational study. Zhonghua Yu Fang Yi Xue Za Zhi. 2019;53(6):619–24.
Zhou W, Liu G, Hung RJ, Haycock PC, Aldrich MC, Andrew AS, et al. Causal relationships between body mass index, smoking and lung cancer: univariable and multivariable Mendelian randomization. Int J Cancer. 2021;148(5):1077–86.
Emanuelsson F, Marott S, Tybjærg-Hansen A, Nordestgaard BG, Benn M. Impact of glucose level on micro- and macrovascular disease in the general population: a mendelian randomization study. Diabetes Care. 2020;43(4):894–902.
Han X, Ong JS, Hewitt AW, Gharahkhani P, MacGregor S. The effects of eight serum lipid biomarkers on age-related macular degeneration risk: a Mendelian randomization study. Int J Epidemiol. 2021;50(1):325–36.
Zhong Z, Su G, Du L, Zhou Q, Li F, Chi W, et al. Higher 25-hydroxyvitamin D level is associated with increased risk for Behçet’s disease. Clin Nutr. 2021;40(2):518–24.
Hernán MA, Robins JM. Instruments for causal inference: an epidemiologist’s dream? Epidemiology. 2006;17(4):360–72.
Martens EP, Pestman WR, de Boer A, Belitser SV, Klungel OH. Instrumental variables: application and limitations. Epidemiology. 2006;17(3):260–7.
Permutt T, Hebel JR. Simultaneous-equation estimation in a clinical trial of the effect of smoking on birth weight. Biometrics. 1989;45(2):619–22.
Greenland S. An introduction to instrumental variables for epidemiologists. Int J Epidemiol. 2000;29(4):722–9.
Burgess S, Thompson SG. Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol. 2011;40(3):755–64.
Stearns FW. One hundred years of pleiotropy: a retrospective. Genetics. 2010;186(3):767–73.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37(7):658–65.
Burgess S, Dudbridge F, Thompson SG. Combining information on multiple instrumental variables in Mendelian randomization: comparison of allele score and summarized data methods. Stat Med. 2016;35(11):1880–906.
Asbell PA, Dualan I, Mindel J, Brocks D, Ahmad M, Epstein S. Age-related cataract. Lancet. 2005;365(9459):599–609.
Bunce GE, Kinoshita J, Horwitz J. Nutritional factors in cataract. Annu Rev Nutr. 1990;10:233–54.
Leske MC, Wu SY, Hennis A, Connell AM, Hyman L, Schachat A. Diabetes, hypertension, and central obesity as cataract risk factors in a black population. The Barbados Eye Study Ophthalmology. 1999;106(1):35–41.
Cheung N, Wong TY. Obesity and eye diseases. Surv Ophthalmol. 2007;52(2):180–95.
Lim LS, Tai ES, Aung T, Tay WT, Saw SM, Seielstad M, et al. Relation of age-related cataract with obesity and obesity genes in an Asian population. Am J Epidemiol. 2009;169(10):1267–74.
Tan AG, Kifley A, Flood VM, Holliday EG, Scott RJ, Cumming RG, et al. Evaluating the associations between obesity and age-related cataract: a Mendelian randomization study. Am J Clin Nutr. 2019;110(4):969–76.
Kauppinen A, Paterno JJ, Blasiak J, Salminen A, Kaarniranta K. Inflammation and its role in age-related macular degeneration. Cell Mol Life Sci. 2016;73(9):1765–86.
Molins B, Romero-Vázquez S, Fuentes-Prior P, Adan A, Dick AD. C-reactive protein as a therapeutic target in age-related macular degeneration. Front Immunol. 2018;9:808.
Miller JW. Age-related macular degeneration revisited–piecing the puzzle: the LXIX Edward Jackson memorial lecture. Am J Ophthalmol. 2013;155(1):1-35.e13.
Skerka C, Lauer N, Weinberger AA, Keilhauer CN, Sühnel J, Smith R, et al. Defective complement control of factor H (Y402H) and FHL-1 in age-related macular degeneration. Mol Immunol. 2007;44(13):3398–406.
Johnson PT, Betts KE, Radeke MJ, Hageman GS, Anderson DH, Johnson LV. Individuals homozygous for the age-related macular degeneration risk-conferring variant of complement factor H have elevated levels of CRP in the choroid. Proc Natl Acad Sci U S A. 2006;103(46):17456–61.
Mandal MN, Ayyagari R. Complement factor H: spatial and temporal expression and localization in the eye. Invest Ophthalmol Vis Sci. 2006;47(9):4091–7.
Sharma NK, Gupta A, Prabhakar S, Singh R, Sharma SK, Chen W, et al. Association between CFH Y402H polymorphism and age related macular degeneration in North Indian cohort. PLoS ONE. 2013;8(7): e70193.
Crabb JW, Miyagi M, Gu X, Shadrach K, West KA, Sakaguchi H, et al. Drusen proteome analysis: an approach to the etiology of age-related macular degeneration. Proc Natl Acad Sci U S A. 2002;99(23):14682–7.
Han X, Ong JS, An J, Hewitt AW, Gharahkhani P, MacGregor S. Using Mendelian randomization to evaluate the causal relationship between serum C-reactive protein levels and age-related macular degeneration. Eur J Epidemiol. 2020;35(2):139–46.
Mitchell P, Liew G, Gopinath B, Wong TY. Age-related macular degeneration. Lancet. 2018;392(10153):1147–59.
Congdon NG, Friedman DS, Lietman T. Important causes of visual impairment in the world today. JAMA. 2003;290(15):2057–60.
Swaroop A, Chew EY, Rickman CB, Abecasis GR. Unraveling a multifactorial late-onset disease: from genetic susceptibility to disease mechanisms for age-related macular degeneration. Annu Rev Genomics Hum Genet. 2009; 10(19–43.
Wang L, Clark ME, Crossman DK, Kojima K, Messinger JD, Mobley JA, et al. Abundant lipid and protein components of drusen. PLoS ONE. 2010;5(4): e10329.
Wang Y, Wang M, Zhang X, Zhang Q, Nie J, Zhang M, et al. The Association between the Lipids Levels in Blood and Risk of Age-Related Macular Degeneration. Nutrients. 2016; 8(10).
Butt AL, Lee ET, Klein R, Russell D, Ogola G, Warn A, et al. Prevalence and risks factors of age-related macular degeneration in Oklahoma Indians: the Vision Keepers Study. Ophthalmology. 2011;118(7):1380–5.
Klein R, Klein BE, Franke T. The relationship of cardiovascular disease and its risk factors to age-related maculopathy. The Beaver Dam Eye Study Ophthalmology. 1993;100(3):406–14.
van Leeuwen R, Tomany SC, Wang JJ, Klein R, Mitchell P, Hofman A, et al. Is medication use associated with the incidence of early age-related maculopathy? Pooled findings from 3 continents. Ophthalmology. 2004;111(6):1169–75.
Nowak M, Swietochowska E, Marek B, Szapska B, Wielkoszynski T, Kos-Kudla B, et al. Changes in lipid metabolism in women with age-related macular degeneration. Clin Exp Med. 2005;4(4):183–7.
Tan JS, Mitchell P, Smith W, Wang JJ. Cardiovascular risk factors and the long-term incidence of age-related macular degeneration: the Blue Mountains Eye Study. Ophthalmology. 2007;114(6):1143–50.
Neale BM, Fagerness J, Reynolds R, Sobrin L, Parker M, Raychaudhuri S, et al. Genome-wide association study of advanced age-related macular degeneration identifies a role of the hepatic lipase gene (LIPC). Proc Natl Acad Sci U S A. 2010;107(16):7395–400.
Fritsche LG, Igl W, Bailey JN, Grassmann F, Sengupta S, Bragg-Gresham JL, et al. A large genome-wide association study of age-related macular degeneration highlights contributions of rare and common variants. Nat Genet. 2016;48(2):134–43.
McKay GJ, Patterson CC, Chakravarthy U, Dasari S, Klaver CC, Vingerling JR, et al. Evidence of association of APOE with age-related macular degeneration: a pooled analysis of 15 studies. Hum Mutat. 2011;32(12):1407–16.
Emdin CA, Khera AV, Kathiresan S. Mendelian Randomization. JAMA. 2017;318(19):1925–6.
Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. Bmj. 2018; 362(k601.
Sekula P, Del Greco MF, Pattaro C, Köttgen A. Mendelian Randomization as an Approach to Assess Causality Using Observational Data. J Am Soc Nephrol. 2016;27(11):3253–65.
Burgess S, Davey SG. Mendelian Randomization Implicates High-Density Lipoprotein Cholesterol-Associated Mechanisms in Etiology of Age-Related Macular Degeneration. Ophthalmology. 2017;124(8):1165–74.
Fan Q, Maranville JC, Fritsche L, Sim X, Cheung CMG, Chen LJ, et al. HDL-cholesterol levels and risk of age-related macular degeneration: a multiethnic genetic study using Mendelian randomization. Int J Epidemiol. 2017;46(6):1891–902.
Zuber V, Colijn JM, Klaver C, Burgess S. Selecting likely causal risk factors from high-throughput experiments using multivariable Mendelian randomization. Nat Commun. 2020;11(1):29.
Chakravarthy U, Wong TY, Fletcher A, Piault E, Evans C, Zlateva G, et al. Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmol. 2010;10:31.
Pan CW, Ikram MK, Cheung CY, Choi HW, Cheung CM, Jonas JB, et al. Refractive errors and age-related macular degeneration: a systematic review and meta-analysis. Ophthalmology. 2013;120(10):2058–65.
Li Y, Wang J, Zhong X, Tian Z, Wu P, Zhao W, et al. Refractive error and risk of early or late age-related macular degeneration: a systematic review and meta-analysis. PLoS ONE. 2014;9(3): e90897.
Wood A, Guggenheim JA. Refractive error has minimal influence on the risk of age-related macular degeneration: a mendelian randomization study. Am J Ophthalmol. 2019;206:87–93.
Fan Q, Verhoeven VJ, Wojciechowski R, Barathi VA, Hysi PG, Guggenheim JA, et al. Meta-analysis of gene-environment-wide association scans accounting for education level identifies additional loci for refractive error. Nat Commun. 2016;7:11008.
Baird PN, Saw SM, Lanca C, Guggenheim JA, Smith Iii EL, Zhou X, et al. Myopia. Nat Rev Dis Primers. 2020;6(1):99.
Williams KM, Bertelsen G, Cumberland P, Wolfram C, Verhoeven VJ, Anastasopoulos E, et al. Increasing prevalence of Myopia in Europe and the impact of education. Ophthalmology. 2015;122(7):1489–97.
Cuellar-Partida G, Lu Y, Kho PF, Hewitt AW, Wichmann HE, Yazar S, et al. Assessing the genetic predisposition of education on myopia: a mendelian randomization study. Genet Epidemiol. 2016;40(1):66–72.
Roy A, Kar M, Mandal D, Ray RS, Kar C. Variation of axial ocular dimensions with age, sex, height, BMI-and their relation to refractive status. J Clin Diagn Res. 2015;9(1):Ac01-4.
Bulik-Sullivan B, Finucane HK, Anttila V, Gusev A, Day FR, Loh PR, et al. An atlas of genetic correlations across human diseases and traits. Nat Genet. 2015;47(11):1236–41.
Mountjoy E, Davies NM, Plotnikov D, Smith GD, Rodriguez S, Williams CE, et al. Education and myopia: assessing the direction of causality by mendelian randomisation. BMJ. 2018;361:k2022.
Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, Mackey DA, Foster PJ. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012;119(10):2141–51.
Huang HM, Chang DS, Wu PC. The association between near work activities and myopia in children-a systematic review and meta-analysis. PLoS ONE. 2015;10(10): e0140419.
Karouta C, Ashby RS. Correlation between light levels and the development of deprivation myopia. Invest Ophthalmol Vis Sci. 2014;56(1):299–309.
Cuellar-Partida G, Williams KM, Yazar S, Guggenheim JA, Hewitt AW, Williams C, et al. Genetically low vitamin D concentrations and myopic refractive error: a Mendelian randomization study. Int J Epidemiol. 2017;46(6):1882–90.
Afzal S, Brøndum-Jacobsen P, Bojesen SE, Nordestgaard BG. Genetically low vitamin D concentrations and increased mortality: Mendelian randomisation analysis in three large cohorts. BMJ. 2014;349:g6330.
Mokry LE, Ross S, Ahmad OS, Forgetta V, Smith GD, Goltzman D, et al. Vitamin D and risk of multiple sclerosis: a mendelian randomization study. PLoS Med. 2015;12(8): e1001866.
Northstone K, Guggenheim JA, Howe LD, Tilling K, Paternoster L, Kemp JP, et al. Body stature growth trajectories during childhood and the development of myopia. Ophthalmology. 2013;120(5):1064-73.e1.
Ojaimi E, Robaei D, Rochtchina E, Rose KA, Morgan IG, Mitchell P. Impact of birth parameters on eye size in a population-based study of 6-year-old Australian children. Am J Ophthalmol. 2005;140(3):535–7.
Tideman JWL, Polling JR, Jaddoe VWV, Vingerling JR, Klaver CCW. Growth in foetal life, infancy, and early childhood and the association with ocular biometry. Ophthalmic Physiol Opt. 2019;39(4):245–52.
Pai AS, Wang JJ, Samarawickrama C, Burlutsky G, Rose KA, Varma R, et al. Prevalence and risk factors for visual impairment in preschool children the sydney paediatric eye disease study. Ophthalmology. 2011;118(8):1495–500.
Chen TC, Tsai TH, Shih YF, Yeh PT, Yang CH, Hu FC, et al. Long-term evaluation of refractive status and optical components in eyes of children born prematurely. Invest Ophthalmol Vis Sci. 2010;51(12):6140–8.
O’Connor AR, Stephenson TJ, Johnson A, Tobin MJ, Ratib S, Fielder AR. Change of refractive state and eye size in children of birth weight less than 1701 g. Br J Ophthalmol. 2006;90(4):456–60.
Plotnikov D, Williams C, Guggenheim JA. Association between birth weight and refractive error in adulthood: a Mendelian randomisation study. Br J Ophthalmol. 2020;104(2):214–9.
Murphy RM, Bakir B, O’Brien C, Wiggs JL, Pasquale LR. Drug-induced bilateral secondary angle-closure glaucoma: a literature synthesis. J Glaucoma. 2016;25(2):e99-105.
Grinbaum A, Ashkenazi I, Gutman I, Blumenthal M. Suggested mechanism for acute transient myopia after sulfonamide treatment. Ann Ophthalmol. 1993;25(6):224–6.
Tsai JC, Chang HW. Refractive change after dorzolamide use in patients with primary open-angle glaucoma and ocular hypertension. J Ocul Pharmacol Ther. 2001;17(6):499–504.
Patasova K, Khawaja AP, Tamraz B, Williams KM, Mahroo OA, Freidin M, et al. Association between medication-taking and refractive error in a large general population-based cohort. Invest Ophthalmol Vis Sci. 2021;62(2):15.
Fillingim RB, Wallace MR, Herbstman DM, Ribeiro-Dasilva M, Staud R. Genetic contributions to pain: a review of findings in humans. Oral Dis. 2008;14(8):673–82.
Tedja MS, Wojciechowski R, Hysi PG, Eriksson N, Furlotte NA, Verhoeven VJM, et al. Genome-wide association meta-analysis highlights light-induced signaling as a driver for refractive error. Nat Genet. 2018;50(6):834–48.
Bouffard MA. The Pupil. Continuum (Minneap Minn). 2019;25(5):1194–214.
Wu Y, Byrne EM, Zheng Z, Kemper KE, Yengo L, Mallett AJ, et al. Genome-wide association study of medication-use and associated disease in the UK Biobank. Nat Commun. 2019;10(1):1891.
Kuhn F, Aylward B. Rhegmatogenous retinal detachment: a reappraisal of its pathophysiology and treatment. Ophthalmic Res. 2014;51(1):15–31.
Feltgen N, Walter P. Rhegmatogenous retinal detachment–an ophthalmologic emergency. Dtsch Arztebl Int. 2014;111(1–2):12–21.
Yamamoto K, Iwase T, Terasaki H. Long-term changes in intraocular pressure after vitrectomy for rhegmatogenous retinal detachment, epi-retinal membrane, or macular hole. PLoS ONE. 2016;11(11): e0167303.
Philip R, Balekudaru S, Vijaya L, George R. Intraocular pressure outcomes after surgery for rhegmatogenous retinal detachment in schwartz syndrome. Retina. 2020;40(12):2379–84.
Han X, Ong JS, An J, Craig JE, Gharahkhani P, Hewitt AW, et al. Association of myopia and intraocular pressure with retinal detachment in european descent participants of the UK biobank cohort: a mendelian randomization study. JAMA Ophthalmol. 2020;138(6):671–8.
Chia A, Lu QS, Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01% eyedrops. Ophthalmology. 2016;123(2):391–9.
He M, Xiang F, Zeng Y, Mai J, Chen Q, Zhang J, et al. Effect of time spent outdoors at school on the development of myopia among children in china: a randomized clinical trial. JAMA. 2015;314(11):1142–8.
Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–90.
Jonas JB, Aung T, Bourne RR, Bron AM, Ritch R, Panda-Jonas S. Glaucoma. Lancet. 2017;390(10108):2183–93.
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311(18):1901–11.
Moyer VA. Screening for glaucoma: U.S. preventive services task force recommendation statement. Ann Intern Med. 2013;159(7):484–9.
Dielemans I, Vingerling JR, Wolfs RC, Hofman A, Grobbee DE, de Jong PT. The prevalence of primary open-angle glaucoma in a population-based study in The Netherlands. The Rotterdam Study. Ophthalmology. 1994;101(11):1851–5.
Pasquale LR, Kang JH, Manson JE, Willett WC, Rosner BA, Hankinson SE. Prospective study of type 2 diabetes mellitus and risk of primary open-angle glaucoma in women. Ophthalmology. 2006;113(7):1081–6.
Chopra V, Varma R, Francis BA, Wu J, Torres M, Azen SP. Type 2 diabetes mellitus and the risk of open-angle glaucoma the Los Angeles Latino Eye Study. Ophthalmology. 2008;115(2):227-32.e1.
Wong VH, Bui BV, Vingrys AJ. Clinical and experimental links between diabetes and glaucoma. Clin Exp Optom. 2011;94(1):4–23.
Song BJ, Aiello LP, Pasquale LR. Presence and risk factors for glaucoma in patients with diabetes. Curr Diab Rep. 2016;16(12):124.
Morris AP, Voight BF, Teslovich TM, Ferreira T, Segrè AV, Steinthorsdottir V, et al. Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat Genet. 2012;44(9):981–90.
Mahajan A, Go MJ, Zhang W, Below JE, Gaulton KJ, Ferreira T, et al. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat Genet. 2014;46(3):234–44.
Shen L, Walter S, Melles RB, Glymour MM, Jorgenson E. Diabetes pathology and risk of primary open-angle glaucoma: evaluating causal mechanisms by using genetic information. Am J Epidemiol. 2016;183(2):147–55.
Son J, Koh H, Son J. The association between intraocular pressure and different combination of metabolic syndrome components. BMC Ophthalmol. 2016;16:76.
Sahinoglu-Keskek N, Keskek SO, Cevher S, Kirim S, Kayiklik A, Ortoglu G, et al. Metabolic syndrome as a risk factor for elevated intraocular pressure. Pak J Med Sci. 2014;30(3):477–82.
Hysi PG, Khawaja AP, Menni C, Tamraz B, Wareham N, Khaw KT, et al. Ascorbic acid metabolites are involved in intraocular pressure control in the general population. Redox Biol. 2019;20:349–53.
Raaz U, Toh R, Maegdefessel L, Adam M, Nakagami F, Emrich FC, et al. Hemodynamic regulation of reactive oxygen species: implications for vascular diseases. Antioxid Redox Signal. 2014;20(6):914–28.
Ko F, Boland MV, Gupta P, Gadkaree SK, Vitale S, Guallar E, et al. Diabetes, triglyceride levels, and other risk factors for glaucoma in the national health and nutrition examination survey 2005–2008. Invest Ophthalmol Vis Sci. 2016;57(4):2152–7.
Wang S, Bao X. Hyperlipidemia, blood lipid level, and the risk of glaucoma: a meta-analysis. Invest Ophthalmol Vis Sci. 2019;60(4):1028–43.
Xu M, Li S, Zhu J, Luo D, Song W, Zhou M. Plasma lipid levels and risk of primary open angle glaucoma: a genetic study using Mendelian randomization. BMC Ophthalmol. 2020;20(1):390.
Gordon SM, Deng J, Tomann AB, Shah AS, Lu LJ, Davidson WS. Multi-dimensional co-separation analysis reveals protein-protein interactions defining plasma lipoprotein subspecies. Mol Cell Proteomics. 2013;12(11):3123–34.
Woudberg NJ, Pedretti S, Lecour S, Schulz R, Vuilleumier N, James RW, et al. Pharmacological Intervention to Modulate HDL: What Do We Target? Front Pharmacol. 2017;8:989.
Nusinovici S, Li H, Thakur S, Baskaran M, Tham YC, Zhou L, et al. High-density lipoprotein 3 cholesterol and primary open-angle glaucoma: metabolomics and mendelian randomization analyses. Ophthalmology. 2021. https://doi.org/10.1016/j.ophtha.2021.09.013.
Du XM, Kim MJ, Hou L, Le Goff W, Chapman MJ, Van Eck M, et al. HDL particle size is a critical determinant of ABCA1-mediated macrophage cellular cholesterol export. Circ Res. 2015;116(7):1133–42.
Talbot CPJ, Plat J, Ritsch A, Mensink RP. Determinants of cholesterol efflux capacity in humans. Prog Lipid Res. 2018;69:21–32.
Di Paolo G, Kim TW. Linking lipids to Alzheimer’s disease: cholesterol and beyond. Nat Rev Neurosci. 2011;12(5):284–96.
Fourgeux C, Bron A, Acar N, Creuzot-Garcher C, Bretillon L. 24S-hydroxycholesterol and cholesterol-24S-hydroxylase (CYP46A1) in the retina: from cholesterol homeostasis to pathophysiology of glaucoma. Chem Phys Lipids. 2011;164(6):496–9.
Cheng W, Song Y, Lin F, Jin L, Wang Z, Jonas JB, et al. Choriocapillaris flow deficits in normal Chinese imaged by swept-source optical coherence tomographic angiography. Am J Ophthalmol. 2021. https://doi.org/10.1016/j.ajo.2021.09.018.
Deol M, Taylor DA, Radcliffe NM. Corneal hysteresis and its relevance to glaucoma. Curr Opin Ophthalmol. 2015;26(2):96–102.
Liang L, Zhang R, He LY. Corneal hysteresis and glaucoma. Int Ophthalmol. 2019;39(8):1909–16.
Medeiros FA, Weinreb RN. Evaluation of the influence of corneal biomechanical properties on intraocular pressure measurements using the ocular response analyzer. J Glaucoma. 2006;15(5):364–70.
Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg. 2005;31(1):146–55.
Khawaja AP, Rojas Lopez KE, Hardcastle AJ, Hammond CJ, Liskova P, Davidson AE, et al. Genetic variants associated with corneal biomechanical properties and potentially conferring susceptibility to keratoconus in a genome-wide association study. JAMA Ophthalmol. 2019;137(9):1005–12.
del Buey MA, Cristóbal JA, Ascaso FJ, Lavilla L, Lanchares E. Biomechanical properties of the cornea in Fuchs’ corneal dystrophy. Invest Ophthalmol Vis Sci. 2009;50(7):3199–202.
Carbonaro F, Andrew T, Mackey DA, Spector TD, Hammond CJ. The heritability of corneal hysteresis and ocular pulse amplitude: a twin study. Ophthalmology. 2008;115(9):1545–9.
Simcoe MJ, Khawaja AP, Hysi PG, Hammond CJ. Genome-wide association study of corneal biomechanical properties identifies over 200 loci providing insight into the genetic etiology of ocular diseases. Hum Mol Genet. 2020;29(18):3154–64.
Vera J, Redondo B, Molina R, Bermúdez J, Jiménez R. Effects of caffeine on intraocular pressure are subject to tolerance: a comparative study between low and high caffeine consumers. Psychopharmacology. 2019;236(2):811–9.
Chandrasekaran S, Rochtchina E, Mitchell P. Effects of caffeine on intraocular pressure: the Blue Mountains Eye Study. J Glaucoma. 2005;14(6):504–7.
Kang JH, Willett WC, Rosner BA, Hankinson SE, Pasquale LR. Caffeine consumption and the risk of primary open-angle glaucoma: a prospective cohort study. Invest Ophthalmol Vis Sci. 2008;49(5):1924–31.
Kim J, Aschard H, Kang JH, Lentjes MAH, Do R, Wiggs JL, et al. Intraocular pressure, glaucoma, and dietary caffeine consumption: a gene-diet interaction study from the UK Biobank. Ophthalmology. 2021;128(6):866–76.
Zheng Y, Ge J, Huang G, Zhang J, Liu B, Hur YM, et al. Heritability of central corneal thickness in Chinese: the Guangzhou Twin Eye Study. Invest Ophthalmol Vis Sci. 2008;49(10):4303–7.
Landers JA, Hewitt AW, Dimasi DP, Charlesworth JC, Straga T, Mills RA, et al. Heritability of central corneal thickness in nuclear families. Invest Ophthalmol Vis Sci. 2009;50(9):4087–90.
Baboolal SO, Smit DP. South African Eye Study (SAES): ethnic differences in central corneal thickness and intraocular pressure. Eye (Lond). 2018;32(4):749–56.
Dimasi DP, Burdon KP, Craig JE. The genetics of central corneal thickness. Br J Ophthalmol. 2010;94(8):971–6.
Choquet H, Melles RB, Yin J, Hoffmann TJ, Thai KK, Kvale MN, et al. A multiethnic genome-wide analysis of 44,039 individuals identifies 41 new loci associated with central corneal thickness. Commun Biol. 2020;3(1):301.
Yang Z, Yang J, Liu D, Yu W. Mendelian randomization analysis identified genes pleiotropically associated with central corneal thickness. BMC Genomics. 2021;22(1):517.
McCabe JM, Croce KJ. Optical coherence tomography. Circulation. 2012;126(17):2140–3.
Miller DT, Kurokawa K. Cellular-scale imaging of transparent retinal structures and processes using adaptive optics optical coherence tomography. Annu Rev Vis Sci. 2020;6:115–48.
Inuzuka H, Sawada A, Inuzuka M, Yamamoto T. Thinning rates of retinal nerve layer and ganglion cell-inner plexiform layer in various stages of normal tension glaucoma. Br J Ophthalmol. 2020;104(8):1131–6.
Demirtaş AA, Duru Z, Duru N, Erdoğan H. Evaluation of retina nerve fiber layer, ganglion cell-inner plexiform layer and lamina cribrosa in clinically unilateral exfoliative glaucoma. Int Ophthalmol. 2020;40(10):2691–7.
Currant H, Hysi P, Fitzgerald TW, Gharahkhani P, Bonnemaijer PWM, Senabouth A, et al. Genetic variation affects morphological retinal phenotypes extracted from UK Biobank optical coherence tomography images. PLoS Genet. 2021;17(5): e1009497.
Liu F, Wollstein A, Hysi PG, Ankra-Badu GA, Spector TD, Park D, et al. Digital quantification of human eye color highlights genetic association of three new loci. PLoS Genet. 2010;6(5): e1000934.
Tassetto M, Scialdone A, Solini A, Di Virgilio F. The P2X7 receptor: a promising pharmacological target in diabetic retinopathy. Int J Mol Sci. 2021;22:13.
Sobrin L, Chong YH, Fan Q, Gan A, Stanwyck LK, Kaidonis G, et al. Genetically determined plasma lipid levels and risk of diabetic retinopathy: a mendelian randomization study. Diabetes. 2017;66(12):3130–41.
Simó R, Roy S, Behar-Cohen F, Keech A, Mitchell P, Wong TY. Fenofibrate: a new treatment for diabetic retinopathy. Molecular mechanisms and future perspectives. Curr Med Chem. 2013;20(26):3258–66.
Fan X, Wu Q, Li Y, Hao Y, Ning N, Kang Z, et al. Association between adiponectin concentrations and diabetic retinopathy in patients with type 2 diabetes: a meta analysis. Chin Med J (Engl). 2014;127(4):765–71.
Kuo JZ, Guo X, Klein R, Klein BE, Genter P, Roll K, et al. Adiponectin, Insulin Sensitivity and Diabetic Retinopathy in Latinos With Type 2 Diabetes. J Clin Endocrinol Metab. 2015;100(9):3348–55.
Shibata R, Ouchi N, Kihara S, Sato K, Funahashi T, Walsh K. Adiponectin stimulates angiogenesis in response to tissue ischemia through stimulation of amp-activated protein kinase signaling. J Biol Chem. 2004;279(27):28670–4.
Ouchi N, Kihara S, Arita Y, Okamoto Y, Maeda K, Kuriyama H, et al. Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Circulation. 2000;102(11):1296–301.
Huang YC, Chang YW, Cheng CW, Wu CM, Liao WL, Tsai FJ. Causal relationship between adiponectin and diabetic retinopathy: a mendelian randomization study in an Asian population. Genes (Basel). 2020. https://doi.org/10.3390/genes12010017.
Hadjadj S, Aubert R, Fumeron F, Pean F, Tichet J, Roussel R, et al. Increased plasma adiponectin concentrations are associated with microangiopathy in type 1 diabetic subjects. Diabetologia. 2005;48(6):1088–92.
Ouchi N, Shibata R, Walsh K. Cardioprotection by adiponectin. Trends Cardiovasc Med. 2006;16(5):141–6.
Emanuelsson F, Nordestgaard BG, Tybjærg-Hansen A, Benn M. Impact of LDL cholesterol on microvascular versus macrovascular disease: a mendelian randomization study. J Am Coll Cardiol. 2019;74(11):1465–76.
Florez JC, Jablonski KA, Bayley N, Pollin TI, de Bakker PI, Shuldiner AR, et al. TCF7L2 polymorphisms and progression to diabetes in the Diabetes Prevention Program. N Engl J Med. 2006;355(3):241–50.
Hribal ML, Presta I, Procopio T, Marini MA, Stančáková A, Kuusisto J, et al. Glucose tolerance, insulin sensitivity and insulin release in European non-diabetic carriers of a polymorphism upstream of CDKN2A and CDKN2B. Diabetologia. 2011;54(4):795–802.
Davatchi F. Behcet’s disease. Int J Rheum Dis. 2014;17(4):355–7.
Tong B, Liu X, Xiao J, Su G. Immunopathogenesis of Behcet’s Disease. Front Immunol. 2019;10:665.
Greco A, De Virgilio A, Ralli M, Ciofalo A, Mancini P, Attanasio G, et al. Behçet’s disease: New insights into pathophysiology, clinical features and treatment options. Autoimmun Rev. 2018;17(6):567–75.
Pineton de Chambrun M, Wechsler B, Geri G, Cacoub P, Saadoun D. New insights into the pathogenesis of Behçet's disease. Autoimmun Rev. 2012; 11(10): 687–98.
Colotta F, Jansson B, Bonelli F. Modulation of inflammatory and immune responses by vitamin D. J Autoimmun. 2017;85:78–97.
Khabbazi A, Ghojazadeh M, Hajebrahimi S, Nikniaz Z. Relationship between vitamin D level and Bechcet’s disease activity: A systematic review and meta-analysis. Int J Vitam Nutr Res. 2020;90(5–6):527–34.
Can M, Gunes M, Haliloglu OA, Haklar G, Inanç N, Yavuz DG, et al. Effect of vitamin D deficiency and replacement on endothelial functions in Behçet’s disease. Clin Exp Rheumatol. 2012;30(3 Suppl 72):S57-61.
Ksiaa I, Abroug N, Kechida M, Zina S, Jelliti B, Khochtali S, et al. Eye and Behçet’s disease. J Fr Ophtalmol. 2019;42(4):e133–46.
Tsirouki T, Dastiridou A, Symeonidis C, Tounakaki O, Brazitikou I, Kalogeropoulos C, et al. A focus on the epidemiology of uveitis. Ocul Immunol Inflamm. 2018;26(1):2–16.
Tugal-Tutkun I, Onal S, Altan-Yaycioglu R, Huseyin Altunbas H, Urgancioglu M. Uveitis in Behçet disease: an analysis of 880 patients. Am J Ophthalmol. 2004;138(3):373–80.
Elkington P, Tebruegge M, Mansour S. Tuberculosis: an infection-initiated autoimmune disease? Trends Immunol. 2016;37(12):815–8.
Zhong Z, Su G, Zhou Q, Meguro A, Takeuchi M, Mizuki N, et al. Tuberculosis exposure with risk of behçet disease among patients with uveitis. JAMA Ophthalmol. 2021;139(4):415–22.
Charbel Issa P, Gillies MC, Chew EY, Bird AC, Heeren TF, Peto T, et al. Macular telangiectasia type 2. Prog Retin Eye Res. 2013;34:49–77.
Scerri TS, Quaglieri A, Cai C, Zernant J, Matsunami N, Baird L, et al. Genome-wide analyses identify common variants associated with macular telangiectasia type 2. Nat Genet. 2017;49(4):559–67.
Bonelli R, Ansell BRE, Lotta L, Scerri T, Clemons TE, Leung I, et al. Genetic disruption of serine biosynthesis is a key driver of macular telangiectasia type 2 aetiology and progression. Genome Med. 2021;13(1):39.
Bonelli R, Jackson VE, Prasad A, Munro JE, Farashi S, Heeren TFC, et al. Identification of genetic factors influencing metabolic dysregulation and retinal support for MacTel, a retinal disorder. Commun Biol. 2021;4(1):274.
Wei FF, Zhang ZY, Thijs L, Yang WY, Jacobs L, Cauwenberghs N, et al. Conventional and ambulatory blood pressure as predictors of retinal arteriolar narrowing. Hypertension. 2016;68(2):511–20.
Gepstein R, Rosman Y, Rechtman E, Koren-Morag N, Segev S, Assia E, et al. Association of retinal microvascular caliber with blood pressure levels. Blood Press. 2012;21(3):191–6.
Li LJ, Cheung CY, Liu Y, Chia A, Selvaraj P, Lin XY, et al. Influence of blood pressure on retinal vascular caliber in young children. Ophthalmology. 2011;118(7):1459–65.
Li LJ, Liao J, Cheung CY, Ikram MK, Shyong TE, Wong TY, et al. Assessing the causality between blood pressure and retinal vascular caliber through mendelian randomisation. Sci Rep. 2016;6:22031.
Park S, Lee S, Kim Y, Lee Y, Kang MW, Kim K, et al. Atrial fibrillation and kidney function: a bidirectional Mendelian randomization study. Eur Heart J. 2021;42(29):2816–23.
Perry BI, Upthegrove R, Kappelmann N, Jones PB, Burgess S, Khandaker GM. Associations of immunological proteins/traits with schizophrenia, major depression and bipolar disorder: a bi-directional two-sample mendelian randomization study. Brain Behav Immun. 2021;97:176–85.
Richardson TG, Sanderson E, Palmer TM, Ala-Korpela M, Ference BA, Davey Smith G, et al. Evaluating the relationship between circulating lipoprotein lipids and apolipoproteins with risk of coronary heart disease: A multivariable Mendelian randomisation analysis. PLoS Med. 2020;17(3): e1003062.
Rosoff DB, Smith GD, Lohoff FW. Prescription opioid use and risk for major depressive disorder and anxiety and stress-related disorders: a multivariable mendelian randomization analysis. JAMA Psychiat. 2021;78(2):151–60.
Acknowledgements
None.
Funding
This review work was supported by the Science and Technology Program of Guangzhou, China (202002020049); Project of Special Research on Cardiovascular Diseases (2020XXG007), National Natural Science Foundation of China (81870663, 82171075), Outstanding Young Talent Trainee Program of Guangdong Provincial People’s Hospital (KJ012019087), Guangdong Provincial People’s Hospital Scientific Research Funds for Leading Medical Talents and Distinguished Young Scholars in Guangdong Province (KJ012019457), Talent Introduction Fund of Guangdong Provincial People’s Hospital (Y012018145), GDPH Supporting Fund for Talent Program and Shenyang Young and Middle-aged Science and Technology Innovation Talent Support Program (RC190146).
Author information
Authors and Affiliations
Contributions
JL, CL, and LL performed literature review and drafted paper. LL and XY contributed to the design. LL, XY, YH, PG, DH, and HY read, revised and proved final draft. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
There is no new data generated as part of this review.
Consent for publication
All authors read the final version and approved it.
Competing interests
There is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The design framework of MR.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, J., Li, C., Huang, Y. et al. Mendelian randomization analyses in ocular disease: a powerful approach to causal inference with human genetic data. J Transl Med 20, 621 (2022). https://doi.org/10.1186/s12967-022-03822-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-022-03822-9