Abstract
Background
5-Fluorouracil (5FU) is a primary chemotherapeutic agent used to treat oral squamous cell carcinoma (OSCC). However, the development of drug resistance has significantly limited its clinical application. Therefore, there is an urgent need to determine the mechanisms underlying drug resistance and identify effective targets. In recent years, the Wingless and Int-1 (WNT) signaling pathway has been increasingly studied in cancer drug resistance; however, the role of WNT3, a ligand of the canonical WNT signaling pathway, in OSCC 5FU-resistance is not clear. This study delved into this potential connection.
Methods
5FU-resistant cell lines were established by gradually elevating the drug concentration in the culture medium. Differential gene expressions between parental and resistant cells underwent RNA sequencing analysis, which was then substantiated via Real-time quantitative PCR (RT-qPCR) and western blot tests. The influence of the WNT signaling on OSCC chemoresistance was ascertained through WNT3 knockdown or overexpression. The WNT inhibitor methyl 3-benzoate (MSAB) was probed for its capacity to boost 5FU efficacy.
Results
In this study, the WNT/β-catenin signaling pathway was notably activated in 5FU-resistant OSCC cell lines, which was confirmed through transcriptome sequencing analysis, RT-qPCR, and western blot verification. Additionally, the key ligand responsible for pathway activation, WNT3, was identified. By knocking down WNT3 in resistant cells or overexpressing WNT3 in parental cells, we found that WNT3 promoted 5FU-resistance in OSCC. In addition, the WNT inhibitor MSAB reversed 5FU-resistance in OSCC cells.
Conclusions
These data underscored the activation of the WNT/β-catenin signaling pathway in resistant cells and identified the promoting effect of WNT3 upregulation on 5FU-resistance in oral squamous carcinoma. This may provide a new therapeutic strategy for reversing 5FU-resistance in OSCC cells.
Similar content being viewed by others
Background
Oral squamous cell carcinoma (OSCC) is a major malignancy within the oral and maxillofacial region [1,2,3,4,5]. Depending on the disease stage, treatment modalities usually include surgical resection, potentially followed by adjuvant radiotherapy or a combination of chemotherapy and radiotherapy [6, 7]. Despite implementing comprehensive strategies, the risk of recurrence following surgery and radiotherapy remains significant, as indicated by the high mortality and recurrence rates supported by histopathological evidence [8]. Adjuvant chemotherapy is indispensable for postoperative recurrence, metastasis, or advanced OSCC and is unsuitable for surgical intervention. 5-Fluorouracil (5FU), as a first-line chemotherapeutic drug, can inhibit the growth of tumor cells by inhibiting thymidylate synthase and integrating its metabolites into RNA and DNA, thus causing DNA damage [9]. Despite the remarkable efficacy of 5FU in tumor treatment, there is growing clinical evidence that the development of drug resistance severely limits its clinical potential, ultimately leading to tumor recurrence, metastasis, and subsequent treatment failure [10, 11]. A groundbreaking meta-analysis reported a modest overall survival advantage of 4% for chemotherapy at both the 2- and 5-year marks in patients with OSCC [12], highlighting that drug resistance limits improvement in overall survival [10, 13]. Therefore, it is important to determine the complex mechanisms underlying chemotherapy resistance in order to improve treatment [14].
Although there have been many studies on the mechanism of 5FU-resistance, it still remains unclear. In recent years, the Wingless and Int-1 (WNT)/β-catenin signaling pathway has received more and more attention in the study of drug resistance [15,16,17,18,19]. The WNT/β-catenin pathway is activated by ligands such as WNT1, WNT3, WNT3A, WNT8A, WNT10A, and WNT10B, and then β-catenin enters the nucleus and binds to the transcription factor TCF/LEF, thus regulating the expression of downstream target genes such as c-Myc, cyclin D1, and AXIN2 [20,21,22]. Studies have shown that abnormal activation of the WNT signaling pathway is closely related to the proliferation [23], invasion [24], metastasis [15, 16, 25], and drug resistance [26,27,28] of OSCC [17,18,19], and is a potential therapeutic target [29]. Previous studies have highlighted the effect of β-catenin on drug resistance, however, more evidence is needed to explore the effects of WNT ligands, the “switches” for pathway activation, on drug resistance. WNT3 is a ligand of the canonical WNT pathway. Many studies have investigated WNT3 in relation to other types of cancer and their chemotherapy resistance. The overall survival rate was significantly lower in non-small cell lung cancer (NSCLC) patients with high-WNT3 tumors than in those with low-WNT3 tumors [30]. Knockdown of WNT3 in human NSCLC cells suppressed cellular proliferation, invasion and metastasis, and induced apoptosis by inhibiting the canonical WNT pathway and the upregulation of WNT3 promoted cisplatin resistance [31, 32]. WNT3 contributed to cell adhesion–mediated drug resistance (CAM-DR) of myeloma cells via the WNT/RhoA/ROCK pathway of myeloma cells in an autocrine manner [33]. However, the role of WNT3 in 5FU-resistance in OSCC is unclear.
Our study found that the expression of WNT3 and its downstream target genes in the canonical WNT signaling pathway were up-regulated in 5FU-resistant OSCC cells compared to that in parental cells. To investigate the effects of these changes on drug resistance, we knocked down WNT3 in 5FU-resistant (5FU-R) cells and found that the half-maximal inhibitory concentration (IC50) decreased accordingly. In addition, we overexpressed WNT3 in OSCC cells and found an increase in the IC50, suggesting that WNT3 promoted 5FU-resistance. At the same time, it was also observed that WNT3 enhanced 5FU-resistance and promoted the proliferation and mobility of cells. In addition, we verified that upregulation of WNT3 promoted the expression of β-catenin in the nucleus, and found that the use of β-catenin inhibitor methyl 3-benzoate (MSAB) combined with 5FU reversed drug resistance. These results suggested that 5FU-resistance in OSCC might be caused by the activation of the canonical WNT signaling pathway through the upregulation of WNT3.
Materials and methods
Cell culture
Human OSCC cell lines (CAL27, HN30, HN6) and 293T were obtained from the School of Stomatology at Fujian Medical University. High-glucose Dulbecco’s modified Eagle medium (DMEM, Hyclone, USA) supplemented with 10% fetal bovine serum (FBS, Gibco, USA) was used for cell culture in an incubator at 37℃ in a humidified atmosphere with 5% CO2.
Construction of OSCC cells with stable 5FU resistance
Parental CAL27 and HN30 cell lines were treated with increasing concentrations of 5FU (MedChemExpress (MCE), China). Over an approximate 12-month period, the 5FU-resistant cells (5FU-R) were successfully stabilized, resulting in the CAL27/5FU and HN30/5FU strains, which were then consistently nurtured in a medium supplemented with 10 µM 5FU.
CCK8 cell viability assay
To determine the IC50 values of 5FU or MSAB, cells were seeded in 96-well plates in triplicate for overnight incubation and later exposed to specified drug concentrations for 48 h. To investigate the reversal of drug resistance, MSAB (MCE, China) was introduced at 0.2 µg/mL, alongside a range of 5FU concentrations. A combination chemotherapy model across a constant-ratio concentration gradient was used to determine the in vitro interaction between 5FU and MSAB at various dosages. After drug exposure, the Cell Counting Kit-8 (CCK8, Dojindo, Japan) reagent was added, and absorbance readings were captured at 450 nm on a SpectroMax iD3 microplate reader (Molecular Devices, USA).
Dose-response curves were constructed using GraphPad Prism software (version 8.0) to determine the IC50 values. The resistance index (RI) values were deduced by comparing the IC50 values of the resistant cells to those of their parental counterparts. The combination index (CI) values were determined as antagonism (CI > 1), additive effect (CI = 1), or synergism (CI < 1) by employing the Chou-Talalay method with CompuSyn software (version 1.0) [34, 35].
Cell proliferation assay
Cells were seeded in 96-well plates and cultured for 3–5 days in the presence of the indicated drugs. Subsequently, cell viability was measured every 24 h using a CCK8 assay. Growth curves were constructed using GraphPad Prism 8.0.
Colony formation assay
The cells were seeded in 12-well plates and incubated overnight. These cells then prospered in the presence or absence of 5FU for 2 weeks. The colonies were stained with 0.5% crystal violet solution (Beyotime, China) for photographic documentation. Colony occupation was quantified using Fiji (ImageJ) software.
Flow cytometry analysis of cell apoptosis
Cells were seeded in 6-well plates overnight before 5FU exposure. Following treatment, cells were washed and suspended in binding buffer and stained with YF®488 Annexin V and propidium iodide (PI) (UElandy, China) for 15 min. Data acquisition was carried out on an Accuri™ C6 Flow Cytometer (BD Biosciences, USA), and subsequent analysis was executed using FlowJo software.
Wound-healing assay
Cells were seeded into 12-well plates. Scratches were created across the monolayered cells. Wound closure in serum-free medium with 5FU was monitored and photographed (100× magnification) over the next 1–3 days, and the healing percentages were quantified using ImageJ.
Transwell migration and invasion assay
The migration assay employed non-coated transwell® inserts with 8 μm pore size polycarbonate membranes (Corning, USA) positioned in a 24-well plate. For the invasion assay, the transwell inserts were pre-coated with Matrigel (Corning, USA) to form matrix barriers. Cell suspensions in serum-free culture medium containing 5FU were introduced into the upper chamber. The lower chamber was supplemented with 10% FBS. Following incubation at 37℃ for 48–72 h, the cells were stained using crystal violet. The lingering cells on the upper surface were removed. Stained cells were photographed (100× magnification) and quantified.
Immunofluorescent staining and confocal microscopy
Cells grown to 50% confluence on coverslips in 12-well plates were fixed with 4% paraformaldehyde solution (Biosharp, China), followed by permeabilization using 0.5% Triton X-100 (Biofroxx, German). Ensuing steps included blocking in 3% bovine serum albumin (BSA, Biofroxx, German) and overnight incubation at 4℃ with primary antibodies against β-catenin (1:200, BD Biosciences, USA). The samples were then incubated with goat anti-mouse secondary antibody conjugated to Alexa Fluor® 488 (Cell Signaling Technology (CST), USA). In another experiment, the fixed and permeabilized cells encountered YF®594-Phalloidin (UElandy, China). The nuclei were stained with 4’,6-diamidino-2-phenylindole (DAPI, Beyotime, China). The coverslips were mounted on glass slides using a protective antifade mounting medium. Samples were observed using confocal microscope (Olympus, Japan) at 600× magnification, particularly emphasizing the nuclear translocation of β-catenin, or marking the subcellular actin.
RNA sequencing analysis (RNA-seq) and bioinformatics analysis
Total RNA was isolated from CAL27 and CAL27/5FU cells using the TRIzol reagent (Invitrogen, USA). Library preparation and data analysis of high throughput sequencing were conducted by Novogene Co., Ltd (Beijing, China). The RNA-seq library preparations were sequenced on an Illumina Novaseq 6000 platform (Illumina, San Diego, CA). The dataset was available from the Gene Expression Omnibus (GEO) repository with accession number GSE248792. Genes with absolute fold-change > 2 in fragments per kilobase of exon model per million mapped fragments (FPKM) expression level and an adjusted P-value ≤ 0.05 found by DESeq2 were defined as differentially expressed genes (DEGs). The volcano plot and heat map presentation of DEGs and the Gene Ontology (GO) and Kyoto Encyclopedia Genes and Genomes (KEGG) pathway analyses were performed by using R language (version 4.2.1). The Cancer Genome Atlas (TCGA) database was analyzed for WNT ligand expression from TCGA- head and neck squamous cell carcinoma (HNSCC) RNAseq by using the Xiantao website (https://www.xiantaozi.com).
Total RNA isolation and real-time quantitative PCR (RT-qPCR)
Total RNA was isolated from cells using NucleoZol (Macherey Nagel, German). Extracted RNA was reverse-transcribed into cDNAs using PrimeScript™ RT Reagent Kit with gDNA Eraser (Takara Bio, Japan), and RT-PCR was performed using the SYBR Green Kit (Bio-Rad, USA). Amplification was performed on a Real-time PCR system (Applied Biosystems, USA). The primers (Table 1) were purchased from SunYa Company (Fuzhou, China). The relative mRNA expression was normalized to the GAPDH expression using the 2−ΔΔCt method.
Protein extraction and Western blot (WB)
Total protein was extracted from the samples using RIPA lysis buffer (Beyotime, China) containing protease inhibitors, PMSF and cocktail (Beyotime, China). Nuclear and cytosolic proteins were extracted using the Nuclear Protein Extraction Kit (Beyotime, China). Protein concentrations were quantified using BCA Protein Assay Kit (Beyotime, China). Equal amounts of the samples were separated by SDS-PAGE and transferred onto PVDF membranes. The membranes were blocked with 3% (w/v) BSA and incubated with primary antibodies (detailed in Table 2) overnight at 4℃. The subsequent step involved incubation with goat anti-rabbit or anti-mouse HRP-conjugated secondary antibodies (Boster, China). Visualization of protein bands was achieved with Pierce™ Enhanced Chemiluminescence (ECL) Western Blotting Substrate (Beyotime, China) on ChemiDoc™ XRS + Imaging System (Bio-Rad, USA). When the expected bands, estimated by the molecular weight ladder and the manufacturer’s instructions of primary antibodies, were separated enough, the blots were cut into 2 or 3 parts prior to incubation with primary antibodies to save the samples and primary antibodies. The original gels and multiple exposure images were shown in Supplementary file for the original images of Western blot.
Small interfering RNA (siRNA) transfection
The sequences of siRNAs (GenePharma, China) targeting WNT3 (siWNT3) and the negative control (siNC) are detailed in Table 3. Resistant cells were seeded in 6-well plates and transiently transfected with siRNAs using the Lipofectamine RNAiMAX Transfection Reagent (Invitrogen, USA). 48 h and 72 h after transfection, both RNA and proteins were harvested for subsequent assays. Cells for subsequent functional assays were processed on the day after transfection.
Transient plasmid transfection
The overexpression plasmid WNT3-Flag (WNT3) and its corresponding control (vector) were obtained from Dahong Biotechnology (Guangzhou, China). After seeding OSCC cells in 6-well plates, they were transiently transfected with plasmids using the Lipofectamine 2000 reagent (Invitrogen, USA) and the medium was replaced with fresh medium. Post-transfection protein analysis verified the overexpression efficiency, and the cells were subsequently used for additional experiments.
Dual-luciferase reporter assay
293T cells at 80% confluence were co-transfected with the WNT3 plasmid or its control vector with Top-flash (Addgene, USA) and Renilla plasmids (Promega, USA) using the Lipofectamine 2000. After 48 h, cell lysates were harvested. Luciferase activity was tested using the Dual Luciferase Assay System (Yeason, China), with firefly luciferase activity normalized to that of Renilla luciferase.
Statistical analysis
All data are presented as mean ± standard deviation, as determined using GraphPad Prism 8.0. Statistical analyses were performed using Student’s t-test, with P < 0.05 as statistically significant (ns = not significant, * P < 0.05, ** P < 0.01, *** P < 0.001).
Results
Establishment and characterization of 5FU‑resistant OSCC cells
Therapeutic resistance is of paramount importance in OSCC treatment. To elucidate the 5FU-resistance mechanism, we established 5FU-resistant cells. We first assessed the viability of the parental and resistant cells after 5FU exposure. The CCK8 assays emphasized a dose-dependent reduction in OSCC cell viability after 5FU. Among them, the IC50 values of 5FU in parental cells and 5FU-R cells were 4.535 µM and 555.1 µM, respectively, for the CAL27 cell line, and 3.355 µM and 165.5 µM for the HN30 cell line, respectively (Fig. 1A, B). The 5FU-R cells displayed a RI of 122.4 for CAL27 and 49.3 for HN30 cell line. Additionally, the clonogenic potential of 5FU-R cells surpassed that of the parental cells (Fig. 1C). When subjected to 5FU, the apoptosis rate at 1 µM 5FU was notably higher in parental cells compared to 5FU-R cells (Fig. 1D, H). Phalloidin staining showed that 5FU-R cells were more dispersed, with increased intercellular gaps and fewer connections compared to the parental cells (Fig. 1E). On assessing other phenotypes via wound-healing, transwell migration and invasion assays, we found enhanced migration and invasion capacities in 5FU-R cells compared to parental cells (Fig. 1F, G, I, J).
We successfully established an in vitro resistant cell model and demonstrated that 5FU-R OSCC cells possessed heightened resistance, proliferation, and metastatic capabilities.
Establishment and characterization of 5FU-resistant (5FU-R) oral squamous cell carcinoma (OSCC) cells. A, B Cell viabilities and IC50 of 5FU comparing parental and 5FU-R cells via CCK8 assay. C Colony-forming potential of parental and 5FU-R cells. D and H Apoptosis under 5FU exposure in parental and 5FU-R cells. E Cytoskeletal configurations (600×) in parental and 5FU-R cells visualized with F-actin staining by YF®594-Phalloidin (red) and nuclear staining by DAPI (blue). F and I Wound-healing (100×) in parental and 5FU-R cells. G and J Migration and invasion (100×) of parental and 5FU-R cells
Identification of WNT3 as a contributor of 5FU-resistance by activating the β-catenin signaling pathway in OSCC cells
To uncover the pivotal factors for 5FU-resistance in oral cancer, we extracted RNA and employed RNA-seq to identify key differentially expressed genes (DEGs) between the parental and 5FU-resistant cells. The volcano plot illustrated the decreased expression of 598 genes (blue dots) and increased expression of 1221 genes (red dots), with gray dots indicating negligible variation (Fig. 2A). A heatmap was generated to assess the overall gene expression across the samples (Fig. 2B). Further exploration of DEGs associated with tumor-related biological processes and signaling pathways was performed using Gene Ontology (GO) and Kyoto Encyclopedia Genes and Genomes (KEGG) enrichment analyses, focusing on the CAL27 and CAL27/5FU samples (Fig. 2C).
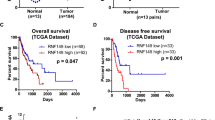
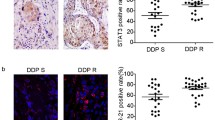
Interestingly, transcriptome sequencing highlighted abnormal activation of the WNT signaling pathway in 5FU-resistant OSCC cells. A heatmap of genes associated with the WNT signaling pathway revealed marked upregulation of several WNT ligands, transcription factors, and downstream effectors. Conversely, genes linked to the degradation complex were downregulated in CAL27/5FU cells compared with those in CAL27 cells (Fig. 2D). To validate these findings, we selected candidate genes for RT-qPCR analysis, which revealed a surge in the expression of WNT3, CCND1, CCND2, CDH2, and Vimentin (VIM) in 5FU-R cells, while CDH1 expression declined (Fig. 2E). No significant variations were observed in the remaining genes in either cell type. Moreover, the protein levels of WNT3, E-cadherin (E-Cad), N-cadherin (N-Cad), and VIM were upregulated in 5FU-R cells (Fig. 2F, G). Therefore, we speculated that the WNT3 and WNT pathway might be associated with resistance to 5FU in oral cancer.
Conventionally, the canonical WNT signaling pathway gets triggered and stabilized by β-catenin. In this scenario, non-phosphorylated β-catenin permeates the nuclei, activating the downstream target genes of the WNT/β-catenin pathway. To identify the specific WNT signaling pathway involved, we evaluated the nuclear β-catenin protein levels by western blot and verified its nuclear translocation by immunofluorescence. Elevated nuclear β-catenin expression was detected in 5FU-R cells (Fig. 2H, J). Immunofluorescence further substantiated this, showing augmented nuclear localization in 5FU-R cells due to the translocation of activated β-catenin, which predominantly resided in the cytoplasm in parental cells (Fig. 2I, K). The data from TCGA showed a predominant elevation in HNSCC genes (Fig. 2L, M, partial data). Notably, WNT3 is a ligand of WNT/β-catenin as a switch in the WNT canonical path [36] and has been generally linked to OSCC progression in previous studies [37], but no association with drug resistance has been reported. In our study, 5FU-R cells showed elevated mRNA and protein levels of WNT3 (Fig. 2E-G). Given its role as an upstream ligand of β-catenin in the WNT pathway, we hypothesized that the activation of the WNT/β-catenin pathway observed in 5FU-R cells could be attributed to amplified WNT3 expression. Consequently, under the stress of 5FU chemotherapy, OSCC cells may bolster their survival by enhancing WNT3 expression.
Therefore, in the following experiments, we manipulated WNT3 using siRNAs and WNT3 plasmids to gain further insight into the molecular complexity of how WNT3 regulated 5FU-resistance.
Transcriptomic analysis and in vitro validation for RNA-seq. A Volcano plot illustrating gene expression differences between parental and 5FU-R cells. B Segment of hierarchical clustering for parental and 5FU-R cells. C GO and KEGG enrichment analyses for DEGs between parental and 5FU-R cells. D Heat map representation of genes related to the WNT pathway. E RT-qPCR validation for changes in the expression of WNT pathway-associated genes. F, G Western blot analyses for WNT3, E-Cad, N-cad, and VIM protein levels. H and J Differential expression of β-catenin in the cytoplasm and nucleus of parental and 5FU-R cells by western blot. I and K Immunocytochemical imaging (600×) of β-catenin (green) with nuclear staining by DAPI (blue). L-M WNT3 expression in HNSCC based on the TCGA database
Downregulation of WNT3 enhances 5FU efficacy in 5FU-resistant OSCC cells
To ascertain the role of WNT3 in resistance to 5FU in OSCC cells, we suppressed the endogenous expression of WNT3 in 5FU-resistant CAL27 and HN30 cells using siRNA constructs. The knock-down effect of the two siRNA sequences (siWNT3-646 and siWNT3-1120) targeting WNT3 verified by RT-qPCR was very good in 5FU-R cells (Fig S1). According to Dharmacon™ siRNA solutions (https://horizondiscovery.com/en/gene-modulation/knockdown/sirna), pooling siRNA improves effectiveness. Therefore, in subsequent experiments, the two sequences were equally mixed as transfection mixture of siWNT3 group, and the knockdown efficiency at the mRNA and protein levels in 5FU-R cells was validated (Fig. 3A, B). Subsequent 5FU treatment of the control and WNT3-silenced cells revealed a partial reversal of 5FU-resistance with WNT3 knockdown. Notably, the IC50 values decreased from 525.0 µM to 336.9 µM for CAL27/5FU and from 160.9 µM to 66.73 µM for HN30/5FU (Fig. 3C, D). Furthermore, WNT3 knockdown enhanced the inhibitory effect of 5FU on the proliferation of resistant OSCC cells (Fig. 3E-F) and reduced the colony-forming potential of 5FU-R cells (Fig. 3G, K). After WNT3 silencing, the apoptosis rate of drug-resistant cells increased in the presence of 5FU (Fig. 3H, L). We analyzed whether changes in WNT3 affected the inhibitory effect of 5FU on the mobility of drug-resistant cells. We found that downregulation of WNT3 hindered cell migration under the action of 5FU through wound healing and transwell migration assays and inhibited cell invasion, as confirmed by the transwell invasion assay (Fig. 3I, J, M, N).
These findings suggested that WNT3 played a pivotal role in 5FU-resistance in OSCC cells. Its suppression restored drug sensitivity and inhibited growth, migration, and invasion of these cells.
Downregulation of WNT3 enhances 5FU efficacy in 5FU-resistant OSCC cells. A, B RT-qPCR and western blot evaluations of WNT3 expression post-knockdown in 5FU-R cells. C, D Decreased IC50 of 5FU in 5FU-R cells after WNT3 knockdown. E, F Inhibited proliferation under 5FU exposure in 5FU-R cells after transfection with siWNT3. G and K Reduced colony-forming potential under 5FU exposure in 5FU-R cells after transfection with siWNT3. H and L Increased apoptosis under 5FU exposure in 5FU-R cells following WNT3 knockdown. I and M Decreased wound-healing (100×) under 5FU exposure in 5FU-R cells after WNT3 knockdown. J and N Diminished migration and invasion (100×) under 5FU exposure in 5FU-R cells after WNT3 knockdown
Upregulation of WNT3 augments 5FU-resistance in OSCC cells
To verify the hypothesis that WNT3 supports chemoresistance to 5FU, we overexpressed WNT3 in parental OSCC cells by transfection with WNT3 plasmids. First of all, the expression levels of endogenous WNT3 in CAL27, HN6, and HN30 cells were detected by western blot. We found that the expression of WNT3 in HN6 and HN30 cells was lower than that in CAL27 cells (Fig S2). Considering the poor transfection results of overexpression in parental CAL27 cells in the previous preliminary experiment, overexpression in cells with low expression level would achieve better results and HN6 and HN30 cells were used in this study. Western blot analysis confirmed a notable increase in WNT3 protein levels after transfection (Fig. 4A).
After upregulation of WNT3, we detected a rise in 5FU-resistance: the IC50 value shifted from 8.892 µM to 23.59 µM in HN6 and from 3.223 µM to 11.72 µM in HN30 (Fig. 4B, C). Additionally, WNT3 overexpression promoted cell proliferation and colony formation in response to 5FU (Fig. 4D-F), indicating that high expression of WNT3 protected OSCC cells from the anti-proliferative effects of 5FU. Consistent with these observations, WNT3 overexpression conferred resistance to 5FU-induced apoptosis (Fig. 4G, N). Further investigation revealed that WNT3 also accelerated cell mobility under the action of 5FU. Wound healing and transwell assays showed that the upregulation of WNT3 expression promoted wound closure and cell invasion and migration in the presence of 5FU observed in HN6 and HN30 cells (Fig. 4H, I, O, P).
Does the effect of WNT3 on drug resistance in OSCC arise through the activation of the canonical WNT signaling pathway? We verified the activation of the canonical signaling pathway by WNT3 using nucleoplasmic isolation, immunofluorescence, and dual-luciferase reporter assays. The results showed that nuclear β-catenin levels also surged (Fig. 4J, L). Using immunofluorescence techniques, we observed the transfer of β-catenin from the cytoplasm to the nucleus following WNT3 overexpression (Fig. 4K, M), which marked the key transcriptional activation step. This was further confirmed by the enhanced luciferase activity in the dual-luciferase reporter assay after the induction of WNT3 (Fig. 4Q).
Our data emphasized that WNT3 enhanced the resistance to 5FU in OSCC through the β-catenin signaling pathway, promoted cell proliferation and mobility under 5FU action, and reduced the level of apoptosis.
Upregulation of WNT3 augments 5FU-resistance in OSCC cells. A Western blot determinations of WNT3 protein levels in OSCC cells after overexpression of WNT3. B, C Elevated IC50 of 5FU in OSCC cells post-WNT3 upregulation. D, E Enhanced proliferation under 5FU exposure in OSCC cells transfected with WNT3. F Enhanced colony-forming ability under 5FU exposure in OSCC cells after WNT3-overexpression. G and N Reduced apoptosis under 5FU exposure in OSCC cells with WNT3 overexpression. H and O Accelerated wound-healing (100×) under 5FU exposure in OSCC cells after WNT3-overexpression. I and P Elevated migration and invasion (100×) under 5FU exposure in OSCC cells after WNT3 upregulation. J and L Differential expression of β-catenin in the cytoplasm and nucleus of OSCC cells after overexpression of WNT3 by western blot. K and M Immunocytochemical imaging (600×) of β-catenin (green) with nuclear counterstaining by DAPI (blue). Q Enhanced luciferase activity in dual-luciferase reporter assay after WNT3 overexpression
WNT pathway inhibitor MSAB increases 5FU efficacy in 5FU-resistant OSCC cells
We have previously demonstrated that increased WNT3 expression amplified 5FU-resistance in OSCC cells and activated the canonical WNT signaling pathway. To ascertain whether the β-catenin pathway could alter the chemotherapy-resistant phenotype of 5FU-R cells, we treated 5FU-R cells with WNT/β-catenin signaling inhibitor MSAB [38] to investigate whether combining 5FU with a WNT-specific inhibitor would improve its efficacy.
The optimal MSAB concentration for this experiment was determined by the CCK8 test. MSAB reduced the viability of 5FU-R cells in a dose-dependent manner (Fig. 5A, B). Concurrently, the administration of MSAB resulted in a decrease in β-catenin protein levels (Fig. 5C-D). In subsequent experiments combining chemotherapy with MSAB, we observed a significant inhibition of 5FU-R cell proliferation (Fig. 5E, F). Specifically, treatment in combination with MSAB resulted in a more pronounced reduction in cell viability compared to the control cells and those receiving monotherapy. This suggested that the introduction of MSAB enhanced the growth inhibitory effect of 5FU. Co-treatment with MSAB (MSAB group) diminished 5FU-resistance in both CAL27/5FU and HN30/5FU cell lines compared with the control group, with the IC50 of 5FU dropping from 587.7 µM to 386.9 µM and from 154.6 µM to 33.70 µM, respectively (Fig. 5G, H). This underscored the notion that β-catenin suppression reduced 5FU-resistance. In a further study involving co-treatment with MSAB and 5FU, we evaluated the CI values of 5FU alongside MSAB. CI values below 1 indicated a synergistic effect of MSAB and 5FU (Fig. 5I, J). In addition, MSAB treatment increased the expression of cleaved Caspase-3, subsequently accelerating the hydrolysis of its substrate poly (ADP-ribose) polymerase (PARP) (Fig. 5K), suggesting that MSAB induced apoptosis in 5FU-R cells.
Our results suggested that disrupting the WNT pathway enhanced the sensitivity of 5FU-R cells to 5FU. The therapeutic combination of a WNT inhibitor and 5FU enhanced the treatment potency of 5FU, further emphasizing the pivotal role of β-catenin inhibition in counteracting 5FU-resistance.
MSAB increases 5FU efficacy in 5FU-resistant OSCC cells. A, B Cell viabilities and IC50 of MSAB on 5FU-R cells. C, D Decreased β-catenin protein levels after MSAB treatment. E, F Inhibited proliferation of 5FU-R cells when treated with MSAB combined with 5FU. G, H Decreased IC50 of 5FU in 5FU-R cells when combined with 0.2 µg/mL MSAB. I, J Synergistic effects as indicated by CI < 1 when combining MSAB and 5FU. K Upregulation of apoptosis-related proteins after MSAB treatment
Discussion
Chemotherapy serves as a supplementary treatment for most patients with oral cancer following surgical procedures. As a first-line therapeutic agent in both chemotherapy alone and combination chemotherapy regimens, 5FU is integral to oral cancer treatment [39]. However, the emergence of 5FU-resistance in many patients underscores the urgent need for effective countermeasures. Despite numerous molecular-targeted strategies proposed to address 5FU-resistance in OSCC, practical solutions remain elusive. A growing body of evidence highlights the activation or hyperactivation of WNT/β-catenin in the oncogenesis of various human cancers [40,41,42,43]. Previous studies have identified frequent upregulation and mutations in various WNT family members in diverse cancer types [44]. In addition, an association between the WNT signaling pathway and OSCC prognosis has been established [45,46,47,48,49,50,51,52], positioning it as an independent prognostic factor [16, 53, 54]. The role of WNT/β-catenin activation in mediating chemoresistance in other cancers has also been confirmed in the emerging literature [18, 55, 56], in which WNT/β-catenin activation supports 5FU-resistance through mechanisms such as cancer stem cell, metastasis, and enhanced transcriptional activity [19, 57,58,59].
WNT3, a ligand in the WNT signaling pathway that drives canonical WNT/β-catenin signaling through autocrine or paracrine mechanisms, plays an important role in various biological activities, and has been studied in the context of drug resistance in other cancers. For example, WNT3 silencing inhibits cell proliferation and enhances cell sensitivity to Cisplatin in NSCLC [32]. Furthermore, activation of WNT3 was observed to stimulate the WNT/β-catenin pathway and an epithelial-mesenchymal transition (EMT)-like phenotype in trastuzumab-resistant HER2-overexpressing breast cancer cells [60]. However, the effect of WNT3 on 5FU-resistance in OSCC and related mechanisms have not been reported. Our results confirm the role of WNT3 in promoting the progression of 5FU-resistant OSCC cells, providing more evidence for the role of WNT signaling pathway in chemoresistance in OSCC. In the transcriptome sequencing of 5FU-resistant cells constructed from OSCC, we found an upregulation of WNT3 expression and aberrant activation of the WNT pathway, which drew our attention to the question of whether 5FU-resistance in OSCC is related to these abnormal manifestations. We verified our hypothesis through a seriels of experiments. It is important to note that while WNT3 is a canonical ligand of the WNT pathway, it does not necessarily imply that the activation of the WNT pathway is solely attributable to WNT3. We therefore further determined the WNT3-induced activation of the canonical signal pathway in OSCC cells through the increased levels of intranuclear β-catenin protein and the translocation of β-catenin into the nucleus in immunofluorescence and luciferase reporter gene assays.
It is also possible to question whether other signaling pathways are involved in 5FU-resistance in OSCC. In fact, in the initial analysis of the sequencing results, we observed the most pronounced changes in the WNT pathway, which was selected as the research object for this study. Other signaling pathways may be involved; however, it is critical to recognize the complexity of replicating tumor cell environments in vivo and in vitro. Although this study is insightful, it has some inherent limitations. A more nuanced understanding of drug resistance mechanisms requires extensive experimentation. At present, our team is making related efforts such as constructing drug-resistant patient-derived xenograft (PDX) mouse models by mimicking the human drug-resistance process and exploring related drug-resistance mechanisms.
Notably, N-cadherin (N-Cad, encoded by the CDH2 gene), an EMT marker recognized as being critical for the diagnosis and prognosis of breast cancer [61], was upregulated in this study. Many studies have shown that cells undergoing EMT frequently exhibit amplified EMT traits during drug resistance [62], which was also reflected in our experimental results. In the PDX-resistant mouse model being constructed by our research group, proteins in the tumor tissues were extracted during the process of gradual induction, and EMT changes in the 5FU treatment group were also detected (relevant results not shown), suggesting that the mobility of tumor cells was stimulated during the development of acquired drug resistance. However, the mechanisms underlying these changes require further investigation. Current therapeutic strategies targeting WNT signaling include small-molecule inhibitors targeting β-catenin/TCF signaling activity and antibodies against WNT1 and WNT2 [63]. In vitro experiments and in mouse tumor models, MSAB, the inhibitor of WNT/β-catenin signaling pathway, showed significant selective antitumor effects by inhibiting target genes in colorectal cancer cells [38]. Our observations showed that MSAB-treated 5FU-R cells regained sensitivity to 5FU. MSAB intervention attenuated cell proliferation and increased the rate of apoptosis, as evidenced by the ensuing cascade of caspase activation. These findings underscored the critical role of the WNT/β-catenin signaling pathway in the dynamics of resistance to 5FU in OSCC. Recent studies advocate the specific targeting of WNT3, indicating its potential in countering Trastuzumab resistance, which may be of therapeutic benefit for patients with breast cancer overexpressing HER2 [60]. Therefore, the development of treatments targeting WNT3 is a promising frontier in oncology research.
Conclusions
In conclusion, by constructing 5FU-resistant OSCC cell lines, we revealed the upregulation of WNT3 expression in resistant cells, activating the WNT canonical signaling pathway, and we validated the promoting effect of WNT3 on 5FU resistance. At the same time, we further verified the reversal effect of 5FU combined with MSAB on resistance in OSCC. Our work has demonstrated the role of WNT3 in promoting 5FU resistance in OSCC, therefore, targeting WNT3 therapy may provide a promising strategy for improving 5FU sensitivity in the treatment of OSCC.
Availability of data and materials
The RNA-seq dataset was uploaded to the GEO online repository with the number GSE248792. All the data presented in this study and information supporting the results can be found in the article or in the supplementary information files and are available upon reasonable request from the corresponding authors.
Abbreviations
- 5FU:
-
5-Fluorouracil
- 5FU-R:
-
5FU-resistant cells
- BSA:
-
Bovine serum albumin
- CAM-DR:
-
Cell adhesion–mediated drug resistance
- CCK8:
-
The Cell Counting Kit-8
- CI:
-
The combination index values
- DAPI:
-
4',6-diamidino-2-phenylindole
- DEGs:
-
Differentially expressed genes
- DMEM:
-
Dulbecco's modified Eagle medium\
- ECL:
-
Enhanced Chemiluminescence
- EMT:
-
Epithelial-mesenchymal transition
- FBS:
-
Fetal bovine serum
- FPKM:
-
Fragments per kilobase of exon model per million mapped fragments
- GEO:
-
The Gene Expression Omnibus repository
- GO:
-
Gene Ontology
- HNSCC:
-
Head and neck squamous cell carcinoma
- IC50 :
-
The half-maximal inhibitory concentration
- KEGG:
-
Kyoto Encyclopedia Genes and Genomes
- MSAB:
-
Methyl 3-benzoate
- NC:
-
Negative control
- N-Cad:
-
N-cadherin
- NSCLC:
-
Non-small cell lung cancer
- OSCC:
-
Oral squamous cell carcinoma
- PARP:
-
Poly (ADP-ribose) polymerase
- PDX:
-
Patient-derived xenograft
- PI:
-
Propidium iodide
- RI:
-
The resistance index values
- RNA-seq:
-
RNA sequencing
- RT-qPCR:
-
Real-time quantitative PCR
- siRNA:
-
Small interfering RNA
- TCGA:
-
The Cancer Genome Atlas database
- VIM:
-
Vimentin
- WB:
-
Western blot
- WNT:
-
The Wingless and Int-1
References
Hysi JSH. Methods and risk of bias in molecular marker prognosis studies in oral squamous cell carcinoma. Oral Dis. 2018;24(1–2):115–9.
Ren ZH, Hu CY, He HR, Li YJ, Lyu J. Global and regional burdens of oral cancer from 1990 to 2017: results from the global burden of disease study. Cancer Commun (Lond). 2020;40(2–3):81–92.
Fan T, Wang X, Zhang S, Deng P, Jiang Y, Liang Y, Jie S, Wang Q, Li C, Tian G, et al. NUPR1 promotes the proliferation and metastasis of oral squamous cell carcinoma cells by activating TFE3-dependent autophagy. Signal Transduct Target Ther. 2022;7(1):130.
Messadi DV. Diagnostic aids for detection of oral precancerous conditions. Int J Oral Sci. 2013;5(2):59–65.
Yuan Y, Xie X, Jiang Y, Wei Z, Wang P, Chen F, Li X, Sun C, Zhao H, Zeng X, et al. LRP6 is identified as a potential prognostic marker for oral squamous cell carcinoma via MALDI-IMS. Cell Death Dis. 2017;8(9):e3035.
Mosaddad SA, Namanloo RA, Aghili SS, Maskani P, Alam M, Abbasi K, Nouri F, Tahmasebi E, Yazdanian M, Tebyaniyan H. Photodynamic therapy in oral cancer: a review of clinical studies. Med Oncol. 2023;40(3):91.
Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR. Head and neck squamous cell carcinoma. Nat Rev Dis Primers. 2020;6(1):92.
Rezazadeh F, Andisheh-Tadbir A, Malek Mansouri Z, Khademi B, Bayat P, Sedarat H, Tabesh A, Tayebi Khorami E. Evaluation of recurrence, mortality and treatment complications of oral squamous cell carcinoma in public health centers in Shiraz during 2010 to 2020. BMC Oral Health. 2023;23(1):341.
Dodevska T, Hadzhiev D, Shterev I. Recent advances in electrochemical determination of anticancer drug 5-fluorouracil. Admet DMPK. 2023;11(2):135–50.
Rueff J, Rodrigues AS. Cancer Drug Resistance: A Brief Overview from a Genetic Viewpoint. In: Cancer Drug Resistance. edn. Edited by Rueff J, Rodrigues AS. New York, NY: Springer New York; 2016. pp. 1–18.
Atashi F, Vahed N, Emamverdizadeh P, Fattahi S, Paya L. Drug resistance against 5-fluorouracil and cisplatin in the treatment of head and neck squamous cell carcinoma: a systematic review. J Dent Res Dent Clin Dent Prospects. 2021;15(3):219–25.
Pignon JP, Bourhis J, Domenge C, Designe L. Chemotherapy added to locoregional treatment for head and neck squamous-cell carcinoma: three meta-analyses of updated individual data. MACH-NC collaborative group. Meta-analysis of chemotherapy on head and neck cancer. Lancet. 2000;355(9208):949–55.
Wang X, Yang L, Yu C, Ling X, Guo C, Chen R, Li D, Liu Z. An integrated computational strategy to predict personalized cancer drug combinations by reversing drug resistance signatures. Comput Biol Med. 2023;163: 107230.
Wang J, Sheng NN, Li Y, Fan YW, Nan XR, Fu R. Ly6D facilitates chemoresistance in laryngeal squamous cell carcinoma through miR-509/beta-catenin signaling pathway. Am J cancer Res. 2023;13(5):2155–71.
Xie J, Huang L, Lu YG, Zheng DL. Roles of the wnt signaling pathway in Head and Neck squamous cell carcinoma. Front Mol Biosci. 2020;7:590912.
Xie H, Ma Y, Li J, Chen H, Xie Y, Chen M, Zhao X, Tang S, Zhao S, Zhang Y, et al. WNT7A promotes EGF-induced migration of oral squamous cell carcinoma cells by activating beta-catenin/MMP9-mediated signaling. Front Pharmacol. 2020;11:98.
Noda T, Nagano H, Takemasa I, Yoshioka S, Murakami M, Wada H, Kobayashi S, Marubashi S, Takeda Y, Dono K, et al. Activation of Wnt/beta-catenin signalling pathway induces chemoresistance to interferon-alpha/5-fluorouracil combination therapy for hepatocellular carcinoma. Br J Cancer. 2009;100(10):1647–58.
Hu J, He Q, Tian T, Chang N, Qian L. Transmission of Exosomal TPX2 promotes metastasis and resistance of NSCLC cells to docetaxel. OncoTargets Therapy. 2023;16:197–210.
Wang Y, Gao G, Wei X, Zhang Y, Yu J. UBE2T promotes temozolomide resistance of glioblastoma through regulating the Wnt/beta-catenin signaling pathway. Drug Des Devel Ther. 2023;17:1357–69.
Bai Y, Sha J. The role of carcinogenesis-related biomarkers in the wnt pathway and their effects on epithelial-mesenchymal transition (EMT) in oral squamous cell carcinoma. Cancers (Basel). 2020;12(3):555.
Mizushima T, Nakagawa H, Kamberov YG, Wilder EL, Klein PS, Rustgi AK. Wnt-1 but not epidermal growth factor induces beta-catenin/T-cell factor-dependent transcription in esophageal cancer cells. Cancer Res. 2002;62(1):277–82.
Daniels DL, Weis WI. Beta-catenin directly displaces Groucho/TLE repressors from Tcf/Lef in wnt-mediated transcription activation. Nat Struct Mol Biol. 2005;12(4):364–71.
Ji H, Song H, Wang Z, Jiao P, Xu J, Li X, Du H, Wu H, Zhong Y. FAM83A promotes proliferation and metastasis via Wnt/beta-catenin signaling in head neck squamous cell carcinoma. J Transl Med. 2021;19(1):423.
Iwai S, Yonekawa A, Harada C, Hamada M, Katagiri W, Nakazawa M, Yura Y. Involvement of the wnt-beta-catenin pathway in invasion and migration of oral squamous carcinoma cells. Int J Oncol. 2010;37(5):1095–103.
Warrier S, Bhuvanalakshmi G, Arfuso F, Rajan G, Millward M, Dharmarajan A. Cancer stem-like cells from head and neck cancers are chemosensitized by the wnt antagonist, sFRP4, by inducing apoptosis, decreasing stemness, drug resistance and epithelial to mesenchymal transition. Cancer Gene Ther. 2014;21(9):381–8.
Mohapatra P, Shriwas O, Mohanty S, et al. CMTM6 drives cisplatin resistance by regulating wnt signaling through the ENO-1/AKT/GSK3beta axis. JCI Insight. 2021;6(4):e143643.
Wang Y, Cao Z, Liu F, Ou Y. Clinical significance of activated Wnt/beta-catenin signaling in apoptosis inhibition of oral cancer. Open Life Sci. 2021;16(1):1045–52.
Li L, Liu HC, Wang C, Liu X, Hu FC, Xie N, Lu L, Chen X, Huang HZ. Overexpression of beta-Catenin induces cisplatin resistance in oral squamous cell carcinoma. Biomed Res Int. 2016;2016:5378567.
Alamoud KA. Emerging insights into Wnt/β-catenin signaling in head and neck cancer. J Dent Res Dent Clin Dent Prospects. 2018;97(6):665–73.
Nakashima N, Liu D, Huang CL, Ueno M, Zhang X, Yokomise H. Wnt3 gene expression promotes tumor progression in non-small cell lung cancer. Lung Cancer. 2012;76(2):228–34.
Xue W, Cai L, Li S, Hou Y, Wang YD, Yang D, Xia Y, Nie X. WNT ligands in non-small cell lung cancer: from pathogenesis to clinical practice. Discover Oncol. 2023;14(1):136.
Xing Z, Wang HY, Su WY, Liu YF, Wang XX, Zhan P, Lv TF, Song Y. Wnt3 knockdown sensitizes human non-small cell type lung cancer (NSCLC) cells to cisplatin via regulating the cell proliferation and apoptosis. Eur Rev Med Pharmacol Sci. 2018;22(5):1323–32.
Kobune M, Chiba H, Kato J, Kato K, Nakamura K, Kawano Y, Takada K, Takimoto R, Takayama T, Hamada H, et al. Wnt3/RhoA/ROCK signaling pathway is involved in adhesion-mediated drug resistance of multiple myeloma in an autocrine mechanism. Mol Cancer Ther. 2007;6(6):1774–84.
Chou TC. Drug combination studies and their synergy quantification using the Chou-Talalay method. Cancer Res. 2010;70(2):440–6.
Liu X, Zhao T, Shi Z, Hu C, Li Q, Sun C. Synergism antiproliferative effects of apigenin and naringenin in NSCLC cells. Molecules. 2023;28(13):4947.
Kaemmerer E, Gassler N. Wnt lipidation and modifiers in intestinal carcinogenesis and Cancer. Cancers (Basel). 2016;8(7):69.
Chung PC, Hsieh PC, Lan CC, Hsu PC, Sung MY, Lin YH, Tzeng IS, Chiu V, Cheng CF, Kuo CY. Role of chrysophanol in epithelial-mesenchymal transition in oral cancer cell lines via a Wnt-3-dependent pathway. Evid Based Complement Alternat Med. 2020;2020:8373715.
Hwang SY, Deng X, Byun S, Lee C, Lee SJ, Suh H, Zhang J, Kang Q, Zhang T, Westover KD, et al. Direct targeting of beta-catenin by a small molecule stimulates proteasomal degradation and suppresses oncogenic Wnt/beta-Catenin signaling. Cell Rep. 2016;16(1):28–36.
Rosmarin D, Palles C, Church D, Domingo E, Jones A, Johnstone E, Wang H, Love S, Julier P, Scudder C, et al. Genetic markers of toxicity from capecitabine and other fluorouracil-based regimens: investigation in the QUASAR2 study, systematic review, and meta-analysis. J Clin Oncol. 2014;32(10):1031–9.
Howe LR, Brown AM. Wnt signaling and breast cancer. Cancer Biol Ther. 2004;3(1):36–41.
Gupta S, Iljin K, Sara H, Mpindi JP, Mirtti T, Vainio P, Rantala J, Alanen K, Nees M, Kallioniemi O. FZD4 as a mediator of ERG oncogene-induced WNT signaling and epithelial-to-mesenchymal transition in human prostate cancer cells. Cancer Res. 2010;70(17):6735–45.
El Wakil A, Lalli E. The Wnt/beta-catenin pathway in adrenocortical development and cancer. Mol Cell Endocrinol. 2011;332(1–2):32–7.
MacDonald BT, Tamai K, He X. Wnt/beta-catenin signaling: components, mechanisms, and diseases. Dev Cell. 2009;17(1):9–26.
Zhang GF, Qiu L, Yang SL, Wu JC, Liu TJ. Wnt/beta-catenin signaling as an emerging potential key pharmacological target in cholangiocarcinoma. Biosci Rep. 2020;40(3):BSR20193353.
Lin X, Ding JM, Zheng XZ, Chen JG. Immunity-related long noncoding RNA WDFY3-AS2 inhibited cell proliferation and metastasis through Wnt/beta-catenin signaling in oral squamous cell carcinoma. Arch Oral Biol. 2023;147:105625.
Khan W, Haragannavar VC, Rao RS, Prasad K, Sowmya SV, Augustine D, Patil S. P-Cadherin and WNT5A expression in assessment of lymph node metastasis in oral squamous cell carcinoma. Clin Oral Investig. 2022;26(1):259–73.
Cui SH, Hu XD, Yan Y. Wnt/beta-catenin signaling pathway participates in the effect of miR-626 on oral squamous cell carcinoma by targeting RASSF4. J Oral Pathol Med. 2021;50(10):1005–17.
Shao TR, Zheng ZN, Chen YC, Wu QQ, Huang GZ, Li F, Zeng WS, Lv XZ. LncRNA AC007271.3 promotes cell proliferation, invasion, migration and inhibits cell apoptosis of OSCC via the Wnt/beta-catenin signaling pathway. Life Sci. 2019;239:117087.
Kina S, Kawabata-Iwakawa R, Miyamoto S, Arasaki A, Sunakawa H, Kinjo T. A molecular signature of well-differentiated oral squamous cell carcinoma reveals a resistance mechanism to metronomic chemotherapy and novel therapeutic candidates. J Drug Target. 2021;29(10):1118–27.
Yang J, Wei D, Wang W, Shen B, Xu S, Cao Y. TRAF4 enhances oral squamous cell carcinoma cell growth, invasion and migration by wnt-beta-catenin signaling pathway. Int J Clin Exp Pathol. 2015;8(9):11837–46.
Chen F, Qi S, Zhang X, Wu J, Yang X, Wang R. lncRNA PLAC2 activated by H3K27 acetylation promotes cell proliferation and invasion via the activation of Wnt/beta–catenin pathway in oral squamous cell carcinoma. Int J Oncol. 2019;54(4):1183–94.
Kartha VK, Alamoud KA, Sadykov K, Nguyen BC, Laroche F, Feng H, Lee J, Pai SI, Varelas X, Egloff AM, et al. Functional and genomic analyses reveal therapeutic potential of targeting beta-catenin/CBP activity in head and neck cancer. Genome Med. 2018;10(1):54.
Cierpikowski P, Lis-Nawara A, Bar J. Prognostic value of WNT1, NOTCH1, PDGFRbeta, and CXCR4 in oral squamous cell carcinoma. Anticancer Res. 2023;43(2):591–602.
Ramos-Garcia P, Gonzalez-Moles MA. Prognostic and clinicopathological significance of the aberrant expression of beta-catenin in oral squamous cell carcinoma: a systematic review and Meta-analysis. Cancers (Basel). 2022;14(3):479.
Nechay M, Wang D, Kleiner RE. Inhibition of nucleolar transcription by oxaliplatin involves ATM/ATR kinase signaling. Cell Chem Biol. 2023;30(8):906–19 (e4).
Chen Y, Fang R, Yue C, Chang G, Li P, Guo Q, Wang J, Zhou A, Zhang S, Fuller GN, et al. Wnt-Induced stabilization of KDM4C is required for Wnt/beta-Catenin target gene expression and glioblastoma tumorigenesis. Cancer Res. 2020;80(5):1049–63.
Feng WQ, Zhang YC, Gao H, Li WC, Miao YM, Xu ZF, Xu ZQ, Zhao JK, Zheng MH, Zong YP, et al. FOXD1 promotes chemotherapy resistance by enhancing cell stemness in colorectal cancer through beta–catenin nuclear localization. Oncol Rep. 2023;50(1):134.
Song Z, Liao C, Yao L, Xu X, Shen X, Tian S, Wang S, Xing F. Mir-219-5p attenuates cisplatin resistance of ovarian cancer by inactivating Wnt/beta-catenin signaling and autophagy via targeting HMGA2. Cancer Gene Ther. 2023;30(4):596–607.
Milan TM, Eskenazi APE, Oliveira LD, Silva GD, Bighetti-Trevisan RL, Freitas GP, Almeida LO. Interplay between EZH2/beta-catenin in stemness of cisplatin-resistant HNSCC and their role as therapeutic targets. Cell Signal. 2023;109:110773.
Wu Y, Ginther C, Kim J, Mosher N, Chung S, Slamon D, Vadgama JV. Expression of Wnt3 activates Wnt/beta-catenin pathway and promotes EMT-like phenotype in trastuzumab-resistant HER2-overexpressing breast cancer cells. Mol cancer Research: MCR. 2012;10(12):1597–606.
Singh M, Yelle N, Venugopal C, Singh SK. EMT: mechanisms and therapeutic implications. Pharmacol Ther. 2018;182:80–94.
Park CS, Yoshihara H, Gao Q, Qu C, Iacobucci I, Ghate PS, Connelly JP, Pruett-Miller SM, Wagner B, Robinson CG, et al. Stromal-induced epithelial-mesenchymal transition induces targetable drug resistance in acute lymphoblastic leukemia. Cell Rep. 2023;42(7): 112804.
Barker N, Clevers H. Mining the wnt pathway for cancer therapeutics. Nat Rev Drug Discovery. 2006;5(12):997–1014.
Acknowledgements
We thank all the team members who participated in the study.We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This work was supported by the National Natural Science Foundation of China (Grant number: 82272868 and 82173180), and Fujian Provincial Health Technology Project (Grant number: 2020CXA049). The funding bodies had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
D.Z. and Y.L. conceived the ideas and designed the experiments. X.Z., K.S., R.G., Y.Y. and C.Z. performed the experiments. X.Z. and K.S. were involved in data analyses and interpretation. D.Z. and Y.L. acquired the funding. K.S. and X.Z. wrote the manuscript with the feedback from all authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, X., Sun, K., Gan, R. et al. WNT3 promotes chemoresistance to 5-Fluorouracil in oral squamous cell carcinoma via activating the canonical β-catenin pathway. BMC Cancer 24, 564 (2024). https://doi.org/10.1186/s12885-024-12318-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12318-2