Abstract
Bisphenol A (BPA) is an industrial chemical used extensively to manufacture polycarbonate plastics and epoxy resins. Because of its estrogen-mimicking properties, BPA acts as an endocrine-disrupting chemical. It has gained attention due to its high chances of daily and constant human exposure, bioaccumulation, and the ability to cause cellular toxicities and diseases at extremely low doses. Several elegant studies have shown that BPA can exert cellular toxicities by interfering with the structure and function of mitochondria, leading to mitochondrial dysfunction. Exposure to BPA results in oxidative stress and alterations in mitochondrial DNA (mtDNA), mitochondrial biogenesis, bioenergetics, mitochondrial membrane potential (MMP) decline, mitophagy, and apoptosis. Accumulation of reactive oxygen species (ROS) in conjunction with oxidative damage may be responsible for causing BPA-mediated cellular toxicity. Thus, several reports have suggested using antioxidant treatment to mitigate the toxicological effects of BPA. The present literature review emphasizes the adverse effects of BPA on mitochondria, with a comprehensive note on the molecular aspects of the structural and functional alterations in mitochondria in response to BPA exposure. The review also confers the possible approaches to alleviate BPA-mediated oxidative damage and the existing knowledge gaps in this emerging area of research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
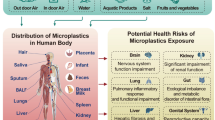
Bisphenol A or BPA [2,2-bis(4-hydroxyphenyl) propane] is a colorless solid, carbon-based synthetic monomer, and a highly used industrial chemical with widespread applications (Nachman et al. 2014; Song et al. 2015; Guo et al. 2017). It is one of the large-scale manufactured industrial chemicals (more than 2.72 × 109 kg/year) commonly used as a plasticizer, monomer, and additive in synthesizing epoxy resins, polycarbonate plastics, and polyvinyl chloride (Khan et al. 2016; Gassman 2017; Urriola-Muñoz et al. 2018). BPA is widely present in food and water containers, air, dust, dental sealants, paints, electronic equipment, toys, cosmetics, car tires, car equipment, flame retardants, inhalers, catheters, and other medical devices (Liao et al. 2012; Khan et al. 2016; Ribeiro et al. 2017; Prins et al. 2018; Shafei et al. 2018). Ingestion, inhalation, and transdermal routes are the frequent modes of BPA exposure in humans (Rubin 2011; Wang et al. 2017; Nomiri et al. 2019). The most common route of BPA’s entry into the human system is through consuming water, food, and beverages contaminated with BPA (Agarwal et al. 2016; Begum et al. 2020; Adiga et al. 2022). Thermal printed paper can also expose users to BPA transdermally (Bernier and Vandenberg 2017; Almeida et al. 2018). BPA exposure during pregnancy and lactation increased anxiety and depression-like behavior in rodent models (Xu et al. 2012).
The digestive tract primarily absorbs BPA; hence, milk, urine, serum, and fat show a plasma level of BPA ranging from 0.2 to 20 ng/mL. Routine exposure to BPA can result in its accumulation in the body tissues (Andra et al. 2016; Jalal et al. 2018) (Fig. 1). A study has shown the elevation in colonic permeability by dietary BPA (Feng et al. 2019). Dietary BPA deregulated the functions of physical and biological barriers and intestinal chemistry (Feng et al. 2019). Metabolism of BPA occurs in the liver. Once absorbed, the unconjugated BPA is bio-transformed into BPA-glucuronide and BPA-sulfate with the help of the enzymes uridine 5′-diphospho-glucuronyl transferase (UGT) and sulfotransferases (Nachman et al. 2014). BPA is excreted through the urine after detoxification and has a 2-h half-life in blood (Neri et al. 2015). Other routes of BPA elimination include sweat, feces, and bile (Genuis et al. 2012) (Fig. 1). BPA is a well-known, potent endocrine-disrupting chemical that mimics 17β-estradiol and interrupts the normal endocrine signaling processes (Ribeiro et al. 2017; Nomiri et al. 2019). It can bind to the classical nuclear estrogen receptor α (ERα) and estrogen receptor β (ERβ), membrane-associated protein receptor G protein-coupled receptor (GPR30), as well as estrogen receptor γ (ERγ), thus activating the non-classical ER pathways (Carchia et al. 2015; Seachrist et al. 2016; Valentino et al. 2016; Gassman 2017). It competes with 17β estradiol and binds to the estrogen receptor, which triggers endocrine receptor signaling pathways and disrupts normal physiological processes even at low doses (Konieczna et al. 2015; Gao et al. 2015; Gassman 2017; Khan et al. 2021).
Bisphenol A (BPA) can enter the human body as leachates from consumer products such as food and water containers, paints, dental sealants, cosmetics, toys, and medical and electronic devices. Free BPA will be bio-transformed upon absorption into BPA-glucuronide or BPA-sulfate, followed by its clearance through urine, sweat, bile, or feces. Routine exposure can accumulate BPA in body tissue, leading to oxidative stress, endocrine disruption, mitochondrial dysfunction, and altered cellular homeostasis. The present review focuses on the alterations in mitochondrial functionalities in response to BPA exposure
BPA exposure contributes to many ailments below the oral reference dose (ORD) established by the United States Environmental Protection Agency (USEPA). USEPA has set 50 µg BPA/kg body weight (kg bw) as the human reference dose (USEPA 2012). The European Food Safety Authority (EFSA) established the temporary Tolerable Daily Intake (t-TDI) of 4 μg/kg body weight/day in 2015 (EFSA 2015). BPA plays a critical role in precocious puberty, polycystic ovary syndrome, female and male infertility, cardiovascular diseases, neurological disorders, and various types of cancer due to its wide-ranging toxic effects (Rutkowska and Rachoń 2014; Inadera 2015; Chen et al. 2018; Matuszczak et al. 2019; Moon et al. 2021; Khan et al. 2021). National Center for Toxicological Research (NCTR) of the US Food and Drug Administration (FDA), the National Toxicology Program (NTP), and the National Institute for Environmental Health Sciences (NIEHS) have performed Consortium Linking Academic and Regulatory Insights on Toxicity of BPA (CLARITY-BPA) study using Sprague–Dawley rats (Heindel et al. 2015). The CLARITY-BPA study was carried out following good laboratory practice (GLP) to gain a more comprehensive understanding of the toxicological effects of BPA. Camacho and his group did not observe BPA-associated health effects in treated rats (Camacho et al. 2019). However, exposure to 25,000 μg BPA/kg bw/day was associated with a high occurrence of lesions in the male pituitary and female reproductive tract. Another CLARITY-BPA study has analyzed the effect of BPA exposure on immune cells. However, chronic BPA exposure did not induce substantial change in the composition of immune cells (Li et al. 2018). Prins and co-workers have proposed the increased risk of prostate cancer in rats exposed to BPA (Prins et al. 2018). Another study has proposed the adverse effects of BPA on organ functioning (Heindel et al. 2020). BPA-mediated epigenetic alterations were observed in the hippocampus and hypothalamus of treated rats. A consortium study has reported mammary carcinoma development and a considerable increase in the follicular cysts in female rats treated with BPA (Prins et al. 2019). Collectively, these CLARITY-BPA studies suggest the possible health effects of BPA. Similar detailed investigations are necessary to clarify the ambiguity regarding the harmful effects of BPA on human health.
BPA has gained attention due to its high chances of human exposure and its ability to predispose individuals to adverse health outcomes even at extremely low doses (Rachoń 2015). BPA has been identified as a Group 2A agent by the International Agency for Research on Cancer (IARC) due to its classification as a probable carcinogen and potential tumor-promoting characteristics (Seachrist et al. 2016). Both experimental and epidemiological findings have shown the association of BPA with different human ailments, such as developmental, metabolic, cardiovascular, neurological, respiratory, renal, and reproductive complications (Rochester 2013; Adiga et al. 2022). BPA induces genetic and epigenetic modifications, endocrine disruption, oxidative stress, and mitochondrial dysfunctions and interferes with the cellular signaling cascades (Rezg et al. 2014). Growing evidence illustrates that BPA induces oxidative stress by targeting the mitochondria’s structure, function, and signaling aspects (Marroqui et al. 2018; Wang et al. 2019b).
Mitochondria are structurally complex, versatile organelles in the cytoplasm and occupy a canonical role as the cell’s energy source (Hsu et al. 2016). Known to operate as power generators by synthesizing adenosine triphosphate (ATP), mitochondria play a central role in fuelling normal metabolic functions (Hertweck and Dasgupta 2017). In addition to its role in cellular bioenergetics, mitochondria modulate many other biological processes such as reactive oxygen species (ROS) generation, calcium (Ca2+) homeostasis, cell growth, fatty acid metabolism, amino acid metabolism, and regulation of cell death (Choudhury and Singh 2017). It uses Ca2+ for modulating cell signaling pathways associated with cell proliferation, differentiation, cell cycle progression, and apoptosis (Osellame et al. 2012). Metabolic alterations in mitochondria contribute to various chronic health disorders such as cardiovascular disorders, autism, muscular dystrophy, diabetes, and different types of cancer (Bravo-Sagua et al. 2017). Several environmental agents, including BPA, exert lethal effects by targeting mitochondria (Meyer et al. 2013; Meli et al. 2020). Owing to its ability to interfere with energy homeostasis, BPA is also considered a metabolism-disrupting chemical (MDC) (Marraudino et al. 2019).
Previous reports demonstrate the adverse effects of BPA on mitochondrial functionalities. However, to the best of our knowledge, a comprehensive review describing the impact of BPA on mitochondria is lacking. In this regard, the present review emphasizes the emerging role of BPA in altering mitochondrial functionalities, associated mechanisms, and the resulting complications (Fig. 2). Moreover, the review also provides data on in-vitro and in-vivo models, doses tested, experimental design, and toxicological impact and confers research gaps and recommendations for future investigations.
Effects of BPA Relative to Mitochondria
Accumulating evidence suggests BPA is an evolving menace to mitochondrial functions (Moon et al. 2012; Wang et al. 2019b, 2021). The subsequent sections illustrate the role of BPA in modulating oxidative stress, mitochondrial membrane potential (MMP), mitochondrial Ca2+, mitochondrial DNA (mtDNA) damage, mitochondrial biogenesis, dynamics, apoptosis, mitophagy, bioenergetics, and respiration.
Oxidative Stress
ROS are produced primarily in mitochondria as a result of electron leak from the electron transport chain (ETC) during oxidative phosphorylation (OXPHOS) (Liou and Storz 2010; Zorov et al. 2014). The cell generates ROS such as superoxide anions, hydroxyl radicals, and peroxides as a part of normal cellular metabolism. The ability of the cell to maintain the redox balance plays a crucial role in all aspects of growth, survival, and development and regulates the cell’s response to endogenous and exogenous stimuli (Ursini et al. 2016). An increase in ROS level damages mitochondrial structure and function and alters mitochondrial signaling (Bhatti et al. 2017). It also reduces MMP and alters the permeability transition of the mitochondrial membrane (Pfeifer et al. 2015). Cells have adapted to highly regulated pathways involving antioxidant defense systems to maintain a redox equilibrium and prevent the deleterious effect caused by ROS accumulation (Gassman 2017).
The BPA-mediated neurotoxic effect involves the activation of the oxidative stress pathway. A recent study using HT-22 cells showed that BPS, BPA, and BPB were toxic to hippocampal neuronal cells (Pang et al. 2019). The same study also showed that 6-h of bisphenol exposure led to a significant increase in ROS. Besides this, upon 24 and 48 h of exposure, higher apoptosis induction was observed, and 7 days of exposure inhibited cell proliferation. Thus, it is evident that long-term exposure to bisphenols may bring in cell cycle arrest and cell death. Similarly, primary hippocampal neurons exposed to bisphenols showed increased ROS and oxidative damage (Meng et al. 2021). The study also showed that hippocampal neurons isolated from males were more sensitive to bisphenols than females (Meng et al. 2021).
BPA administration is known to cause cytotoxicity in various cell and tissue types via oxidative stress and mitochondrial dysfunction (Table 1). BPA exposure affects early embryonic development in the porcine study model (Choi et al. 2016; Guo et al. 2017). Oxidative stress-induced mitochondrial damage leads to the mitochondrial release of cytochrome c (Cyt-C), while DNA damage results in the inactivation of the p53–p21 pathway (Guo et al. 2017). Several researchers have specifically investigated the ROS and antioxidant levels upon BPA exposure. Both low- and high-dose BPA exposure induced ROS generation in in-vitro cell culture systems (Ooe et al. 2005; Huc et al. 2012; Meli et al. 2020). Interestingly, the superoxides produced in response to BPA contributed to the total ROS level and lipid peroxidation in HepG2 cells (Huc et al. 2012). BPA increased the oxidative stress and inflammatory response in human endometrial stromal cells via the Mitogen-activated protein kinase/protein kinase B/nuclear factor-kappa (ERK/AKT/NF-κB) axis (Cho et al. 2018). An inverse correlation between ROS and antioxidant enzymes, such as superoxide dismutase (SOD) and catalase (CAT) was reported (Ighodaro and Akinloye 2018). This implied that BPA-mediated elevation in ROS level was due to the reduced expression of antioxidant enzymes. Reports have shown the ability of BPA to induce nitric oxide via upregulation of nitric oxide synthase (Chouhan et al. 2015; Wang et al. 2019a). In the hearts of male rats, BPA reduced catalase activity, glutathione (GSH) levels, and enhanced lipid peroxidation, thus resulting in ROS accumulation and mitochondrial dysfunction (Aboul Ezz et al. 2015). In 2019, Wang et al. investigated the effect of dietary BPA on liver and colon functions. BPA-induced oxidative stress elevated cytokine secretion and lowered antioxidant levels in mice’s liver and colon tissue (Wang et al. 2019b). These experimental evidences exemplify the influence of BPA on the antioxidant defense system and the resulting oxidative damage and cellular toxicity.
Mitochondrial Membrane Potential (MMP)
Besides taking part in mitochondrial energetics, MMP participates in several non-energetic functions, such as transporting metal ions to the interior and exporting anions to the exterior of mitochondria (Zorova et al. 2018). The regulation of molecules in and out of mitochondria by MMP is vital for maintaining mitochondrial structure, function, and metabolism. Also, MMP regulates ROS production and removal of defective mitochondria (Zorov et al. 2014). Thus, disturbance in MMP may contribute to numerous pathological conditions. In-vitro and in-vivo investigations have shown that BPA alters MMP to promote mitochondrial dysfunction (Jiang et al. 2015; Kaur et al. 2014; Shirani et al. 2019). BPA exposure below the no observed adverse effect level (NOAEL) (0.05 and 1.2 mg/kg/day for 5 days) led to compromised mitochondrial function, as evidenced by the reduction in MMP, oxygen consumption, and ATP production (Moon et al. 2012). Studies have also reported a significant reduction in the MMP of rat kidney mitochondria exposed to 1–1000 μM of BPA (Kobroob et al. 2018). The decrease in sperm motility accompanied a decrease in MMP upon BPA exposure in chicken (Singh et al. 2015b). BPA (50 μg/kg/day for 10 weeks) facilitated depolarization of MMP, impaired mitochondrial integrity, and resulted in oxidative damage in mice’s liver and colon tissues (Wang et al. 2019b). BPA (100 μM) exposure diminished the developmental capacity of mouse oocytes (Pan et al. 2021). The same study also demonstrated the abnormal distribution of mitochondria and decreased MMP upon BPA exposure. BPA-mediated MMP decline may have a decisive role in cellular toxicity. However, the exact molecular mechanism leading to MMP impairment and the consequent effect on mitochondrial function require detailed investigation.
Mitochondrial Calcium
Mitochondria uptake Ca2+ through mitochondrial Ca2+ uniporter (MCU) and Ca2+ level elevation leads to the activation of many enzymes involved in the tricarboxylic acid (TCA) cycle and ATP synthesis (Wacquier et al. 2016). Transfer of Ca2+ from the endoplasmic reticulum to mitochondria is indispensable for maintaining cellular energetics, and reduced transfer diminishes OXPHOS activity and energy production (Bustos et al. 2017). Reports have demonstrated that Ca2+ uptake by mitochondria depends on MMP, and disruption in uptake may lead to decreased mitochondrial respiration, mitochondrial DNA transcription, mitochondrial biogenesis, cell survival, and apoptosis (Choudhury and Singh 2017). The role of BPA in modulating cellular Ca2+ levels is still contentious. Few investigations have shown both the inhibitory and stimulatory effects of BPA on Ca2+ influx. A study has reported BPA as a potent Ca2+ channel inhibitor and has proposed the involvement of ERβ-dependent pathways in regulating Ca2+ entry (Villar-Pazos et al. 2017). A contrasting report has depicted that BPA elevates cytosolic Ca2+ by impeding Sarco/endoplasmic reticulum Ca2+-ATPase (SERCA) and stimulating inositol trisphosphate receptor (IP3R) (Batista-Silva et al. 2020). Using imaging techniques, Derouiche et al. revealed the augmentation of store-operated Ca2+ entry in lymph node carcinoma of the prostate (LNCaP) cells treated with BPA (Derouiche et al. 2013). However, reports showing the direct involvement of BPA in regulating mitochondrial Ca2+ levels are scarce. Investigations in this aspect may aid in a better understanding of the signaling intricacy associated with the toxicological effects of BPA.
mtDNA Damage
mtDNA damage can result from both exogenous and endogenous agents and the mtDNA repair pathways compensate for the resulting damages (Omar García-Lepe and Ma Bermúdez-Cruz 2019). mtDNA damage is one of the critical factors associated with many mitochondrial disorders (Singh et al. 2015a), including cancer and neurological ailments (Singh et al. 2015b). Oxidative stress is one of the primary causes of mtDNA damage (Cui et al. 2012; Han and Chen 2013). Several findings have depicted the potential of BPA to induce oxidative DNA damage. For instance, BPA affects genomic integrity by impairing chromosome synapsis and disturbing double-strand break repair during meiosis (Allard and Colaiacovo 2010). Gassman et al. have demonstrated the inhibitory effect of BPA on oxidized base lesion DNA repair (Gassman et al. 2015). In ERα negative mammary cells, low-dose BPA exposure resulted in DNA damage by modulating cell cycle regulatory proteins (Pfeifer et al. 2015). Another study has revealed the role of BPA in inducing chromosomal aberrations, which was evident with the presence of pulverized and fragmented chromosomes (Di Pietro et al. 2020). Collectively, these findings strongly suggest the involvement of BPA in causing oxidative DNA damage. Because there have been no reports linking BPA exposure to mtDNA damage, it can be speculated that similar to that of genomic DNA, BPA exposure may induce oxidative damage in mtDNA. Investigations in this field may shed light on the novel mechanisms of BPA-driven mitochondrial dysfunction.
mtDNA copy number is closely related to cellular health as mutation and mtDNA variations are associated with human diseases such as Parkinson’s, Alzheimer’s, Huntington’s, diabetes, and cancer (Kabekkodu et al. 2014; Li et al. 2019). Several reports have proposed the changes in mtDNA copy number as a potential disease biomarker for cancer (Hu et al. 2016). Furthermore, many environmental agents have caused mitochondrial dysfunction by altering mitochondrial copy numbers. For example, the rat granulosa cells exposed to BPA showed depletion in mtDNA (Lee et al. 2019). Jiang et al. have revealed the role of BPA in altering the mtDNA copy number. They analyzed the induction of oxidative stress, antioxidant status, cytokine levels, and apoptosis in male Wistar rats exposed to BPA. This study has demonstrated the reduced expression of mtDNA encoded genes, reduced mtDNA copy number, and the resulting mitochondrial dysfunction and kidney toxicity in the treated rats (Jiang et al. 2020). Contrastingly, BPA exposure increased mtDNA copy numbers in lymphoblast cells (Kaur et al. 2014). Although BPA affects mtDNA copy number, the exact molecular mechanism is yet to be uncovered.
Mitochondrial Biogenesis and Dynamics
Mitochondrial biogenesis is a highly regulated process in which cells augment mitochondrial mass by fusion and fission (Popov 2020). Physiological conditions such as cell division, differentiation, low temperature, exercise, oxidative stress, and caloric restriction can influence mitochondrial biogenesis (Popov 2020). Proliferator-activated receptor coactivator 1α (PGC1α), mitochondrial transcription factor A (TFAM), nuclear respiratory factor-1 and -2 (NRF1 and NRF2) also play critical roles in the regulation of mitochondrial biogenesis (Gureev et al. 2019). AMP-activated protein kinase (AMPK) signaling activates PGC1α and NRF-1/2, leading to the transcription of TFAM (Gureev et al. 2019). Following this, TFAM translocates to mitochondria, and by binding to mtDNA, it induces the transcription of genes involved in mitochondrial biogenesis (Gureev et al. 2019). BPA impairs the biogenesis of mitochondria by modifying the expression of associated genes (Lin et al. 2013; Marroqui et al. 2018). Of note, in neonatal rats, prenatal exposure to BPA (50 μg/kg/day) significantly reduced the expression of PGC1α, estrogen-related receptor α (ERRα), ERRγ, peroxisome proliferator-activated receptor α (PPARα), NRF1, and TFAM (Jiang et al. 2014a). Long-term BPA exposure (50 μg/kg/day for 48 weeks) induced hypermethylation of the PGC1α promoter and subsequent downregulation of its expression in the heart tissue of male rats (Jiang et al. 2015). The downregulated genes in response to BPA treatment included PGC1α, NRF1, NRF2, TFAM, and their validated target genes such as ATP synthase subunit epsilon (ATP5E), ATP synthase subunit O (ATP5O), cytochrome b-c1 complex subunit 2 (UQCRC2), and UQCRF1 (Jiang et al. 2015). In zebrafish, BPA exposure affected the expression of critical genes associated with mitochondrial biogenesis and oxidative phosphorylation in male gonads (Chen et al. 2015). The same study has demonstrated reduced sperm quality and count, altered sex ratio, and male-specific reproductive failure in offspring upon BPA exposure.
Both mitochondrial fission and fusion play a key role in mitochondria biogenesis and significantly impact the mitochondrial network. Genes such as dynamin-related protein 1 (DRP1), Mitofusin 1 and 2 (MFN1 and MFN2) are known for their involvement in mitochondrial fusion and fission kinetics (Agarwal et al. 2016). A balance between fission and fusion maintains mitochondrial morphology and preserves a healthy pool of mitochondria by actively controlling mitophagy (Vantaggiato et al. 2019). The imbalance in mitochondrial fission is exhibited by well-developed, elongated mitochondria, whereas disparity in mitochondrial fusion results in increased mitochondrial fragmentation (Senft and Ronai 2016). Different disease conditions showed an increase in the expression of DRP1, Optic atrophy-1 (OPA1), MFN1, and MFN2 proteins (Hall et al. 2014; Zorzano and Claret 2015; Liu et al. 2020). Impaired mitochondrial dynamics disrupt the equilibrium between fusion and fission, causing the accumulation of defective mitochondria and resulting in mitochondrial dysfunction (Agarwal et al. 2016; Wang et al. 2017). DRP1 is an extensively studied protein related to BPA exposure and mitochondrial dynamics. Peerapanyasut et al. have reported the upregulation of the active form of DRP1 in the kidney and liver of rats exposed to BPA (50 mg/kg for 5 weeks) (Peerapanyasut et al. 2019). Low-dose BPA exposure upregulated the active form of DRP1 in human embryonic stem cells derived from cardiomyocytes (Cheng et al. 2020). Chronic exposure to BPA led to the upregulation of DRP1 in hippocampal neural stem cells derived from rat embryos. Also, inhibition of DRP1 mitigated BPA-induced mitochondrial dysfunction. Thus, targeting DRP1 can be used to mitigate BPA-induced neurotoxicity and neurodegeneration (Agarwal et al. 2016). BPA exposure led to an increase in the number of fragmented mitochondria with depletion of cristae and significantly altered the structure of mitochondria from elongated and tubular to small and rounded structures (Agarwal et al. 2016). BPA exposure altered mitochondrial biogenesis by hampering the GFER-mediated mitochondrial protein import in the hippocampus of the rat brain (Goyal et al. 2021). The same study demonstrated the accompanying mitochondrial damage, distorted cristae, and reduced localization of GFER to the mitochondrial intermembrane space in the rat neurons. These observations signify that short-term and long-term exposure to BPA disturbs mitochondrial dynamics by inhibiting mitochondrial biogenesis and modifying fission and fusion kinetics.
Apoptosis
Several previous reports have shown that BPA regulates cell signaling cascades leading to ROS generation and oxidative damage (Gassman 2017). BPA induces apoptosis in various cell and tissue types by targeting the mitochondrial signaling pathways (Fig. 3). BCL2-like protein (BAX) and B cell lymphoma 2 (BCL2) regulate apoptosis by releasing Cyt-C and altering MMP levels. BCL2 and BAX inhibit and promote apoptosis, respectively (Wang et al. 2017). Inappropriate activation or suppression of apoptosis is associated with different pathological conditions, including neurodegenerative diseases, many types of cancer, and autoimmune disorders (Elmore 2007). In INS1 cells, BPA-mediated apoptosis induction involved Cyt-C release and subsequent activation of caspases. Also, these cells displayed mitochondrial toxicity, involving fragmentation of mitochondria, reduction in mitochondrial mass and MMP, and ATP depletion upon BPA exposure (Lin et al. 2013). BPA-induced germ cell apoptosis in mouse testes by activating caspase-9, BAX, caspase-8, caspase-3, and mitochondrial release of Cyt-C (Wang et al. 2010). In male rats, BPA administration increased apoptosis of testes cells and sperms via BCL2 inhibition (Othman et al. 2016). BPA exposure induced DNA fragmentation in zebrafish ovaries, activated caspase-3, caspase-8, and increased BAX/BCL2 ratio (Biswas et al. 2020). In murine macrophages, BPA-induced apoptosis via caspase-dependent and independent mechanisms. The caspase-dependent apoptosis involved activation of Cyt-C through inhibition of BCL2 and BCL-XL, activation of BAX, BID, and BAD, and induction of caspase-3 and -9, resulting in poly(ADP-ribose) polymerase 1 (PARP1) activation. The caspase-independent apoptosis induction in RAW264.7 macrophages involved nuclear translocation of apoptosis-inducing factor (AIF) (Huang et al. 2018). BPA exposure elevated the expression of Cyt-C, AIF, and caspase-3/9 and reduced the levels of BCL2 in spermatogenic cells (Wang et al. 2014). BPA triggered mitochondrial damage by impairing the levels of pro-apoptotic and anti-apoptotic proteins, resulting in increased release of Cyt-C to the cytosol (Lin et al. 2013). Besides, BPA-induced oxidative stress and inflammatory response by activating MAPK, PI3K-AKT, and NF-κB signaling (Gassman 2017; Nomiri et al. 2019). In colonic epithelial cells, treatment with BPA increased mitochondrial and cytosolic ROS, malondialdehyde, and H2O2 levels, depolarized MMP, and triggered apoptosis via MAPK and AKT signaling (Qu et al. 2018). BPA exacerbated GC-2 cell injury by activating caspase-3 and increasing mitochondrial Cyt-C release (Lee et al. 2013). Neuroblastoma cells treated with BPA showed diminished BCL2 expression with simultaneous upregulation of Cyt-C, caspase-3, BAX, and BAK1 proteins (Wang et al. 2021). BPA exposure to ARPE-19 cells decreased mitochondrial BCL-XL expression with a concomitant increase in BAX expression (Chiang et al. 2022). 4-methyl-2,4-bis(4-hydroxyphenyl)pent-1-ene is a known metabolite of BPA. Exposure of Neuro 2a cells to this metabolite elevated mitochondria-dependent apoptosis and resulted in neuronal cell death (Huang et al. 2021). Collectively, these findings insinuate the capability of BPA to induce apoptosis by altering mitochondrial signaling.
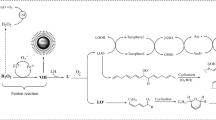
Effect of BPA-induced oxidative stress on apoptosis and mitophagy. BPA-induced ROS accumulation elevates lipid peroxidation, DNA damage, and protein carbonylation. Besides, it alters mitochondrial bioenergetics by enhancing PINK-PARKIN-mediated mitophagy. BPA exposure activates apoptotic proteins and thereby imparts its genotoxic/cytotoxic effects. BPA promotes cell death or neoplastic progression by modulating mitochondrial structure and function. The toxicological effects of BPA are mainly due to elevated oxidative stress. Treatment with antioxidant agents such as melatonin, lipoic acid, and vitamins can restore mitochondrial functionality and mitigate BPA’s toxic effects
Mitophagy
Mitophagy is the process of removal of damaged or defective mitochondria. It plays a vital role in mitochondria’s quality control and turnover to maintain normal cellular functions (Pickles et al. 2018). Additionally, it plays a crucial role in the degradation of paternal mitochondria and pathological conditions such as cancer and neurodegenerative disorders (Um and Yun 2017). In mammals, the PINK1-PARKIN signaling pathway regulates mitophagy (McWilliams and Muqit 2017). Several recent findings have shown that premature activation of mitophagy is crucial in BPA-induced mitochondrial dyshomeostasis. Studies conducted in male Wistar rats have reported the role of BPA in impairing the mitophagy pathway. Further, after BPA exposure, the induction of kidney injury and elevated levels of PINK1 and PARKIN were observed in liver tissue (Peerapanyasut et al. 2019). The hippocampus exposed to BPA showed impaired neurogenesis and mitophagy (Agarwal et al. 2016). BPA exposure resulted in aberrant expression of several nuclear-encoded genes linked with mitophagy. For instance, a systematic toxicological investigation using CRISPR screening suggested the need for UGT1A9 in BPA-induced mitochondrial dysfunction (Tian et al. 2022). In mice having wild-type UGT1A9, BPA-induced liver injury was associated with mitophagy inhibition, while silencing of UGT1A9 diminished the adverse effects of BPA. BPA exposure induced mitophagy in primary rat hepatocytes via PINK1 accumulation and PARKIN translocation to damaged mitochondria (Anand et al. 2020). BPA-related tissue injuries show mitochondrial structural and functional modifications and mitophagy (Peerapanyasut et al. 2019, 2020). Antioxidant therapy using N-Acetylcysteine reduced mitophagy and acute kidney injury caused by BPA exposure. In BHPF-treated oocytes showed mitophagy coupled with increased expression of PINK1, Beclin1 (BECN1), and microtubule-associated proteins 1A/1B light chain 3B (MAP1LC3B), and a decrease in the expression of the translocase of outer mitochondrial membrane 20 (TOMM20) and TOMM17A (Jiao et al. 2019). BPA exposure can cause mitophagy by activating autophagic flux. For example, LKB1/AMPK/mTOR axis activation has been shown to contribute to autophagy induction in rat primary hepatocytes and may participate in mitophagy induction (Anand et al. 2020).
Mitochondrial mass and mitochondrial biogenesis are interconnected. Several findings have demonstrated that alterations in mitochondrial mass can contribute to various diseases (Kobroob et al. 2018; Meli et al. 2020). Changes in mitochondrial mass could be a possible metabolic biomarker for cancer (Lamb et al. 2015). In INS1 cells, BPA treatment (0.002–2 μM for 48 h) significantly reduced mitochondrial mass and cellular ATP and resulted in MMP disruption (Lin et al. 2013). BPA-mediated mitochondrial dysfunction may involve the activation of pathways leading to mitophagy induction, thus interfering with mitochondrial mass (Fig. 3). Table 2 summarizes different findings depicting the effects of BPA on the mitochondrial structure.
Bioenergetics and Respiration
By altering cellular bioenergetics, environmental agents contributed to numerous diseases (Kasperski and Kasperska 2018). Reports have shown that BPA affects bioenergetics by disturbing mitochondrial proteins involved in modulating bioenergetics (Marroqui et al. 2018) (Table 3). For instance, exposure of pancreatic islets to BPA (25 μg/L) led to mitochondrial swelling, diminished Cyt-C oxidase activity, and ATP levels (Marroqui et al. 2018). A research group has demonstrated that exposure to an environmental dose of BPA (1 nM) significantly augmented the expression of genes linked to OXPHOS and mitochondrial function, such as ubiquinol-Cyt-C reductase binding protein (UQCRB), ATPase Na+/K+ transporting subunit β1 (ATP1B1), and isoleucyl-tRNA synthetase (IARS) (Carchia et al. 2015). Uncoupling protein 2 (UCP2) is a member of the mitochondrial anion carrier family and is vital for controlling proton flux uncoupling in mitochondria (Pierelli et al. 2017). BPA exposure activated UCP2 expression in INS1 cells (Lin et al. 2013). Also, in UCP2 overexpressing islet cells, an inverse correlation was observed between UCP2 expression and ATP levels (Lin et al. 2013). The adult rats exposed to BPA (40 μg/kg/day) showed significantly reduced mitochondrial complex activities and ATP production (Lin et al. 2013). Prenatal exposure to BPA (50 μg/kg/day) downregulated Cyt-C expression in heart tissue of neonatal rats (Marroqui et al. 2018). 3T3-L1 adipocytes treated with BPA (10 nM), nonylphenol (600 pM), and diethylstilbestrol (0.23 pM) displayed reduced respiration, ATP production and glycolytic functions (Tsou et al. 2017). BPA-induced impaired mitochondrial bioenergetics may contribute to hepatotoxicity. In Wistar rats, a high dose of BPA (500 mg/kg for 14 days) significantly affected ETC complex activities with a concomitant increase in lipid peroxidation and hepatotoxicity (Khan et al. 2016).
BPA exposure negatively affected intracellular ATP levels in mouse spermatozoa (Rahman et al. 2016). BPA lowered murine pancreatic cell viability by altering mitochondrial function. Besides, co-exposure to low concentrations of BPA (1 nM) and glucose (25 mM) depleted intracellular ATP levels suggesting impaired bioenergetics (Carchia et al. 2015). BPA diminished intracellular ATP by uncoupling OXPHOS, inhibiting respiration and thus altering mitochondrial activity (Gassman 2017). BPA affected sperm function by targeting mitochondrial and cellular ATP via activation of the kinase pathway (Rahman et al. 2016). The same study showed that BPA exposure altered the expression of genes belonging to energy metabolism, stress response, ROS metabolism, cytoskeletal/structural proteins, and fertility-related proteins (Rahman et al. 2016). Dietary intake of BPA affected the activities of mitochondrial complexes IV and V and reduced intracellular ATP levels in mouse colon and liver tissue (Wang et al. 2019b). Exposure to BPA may induce mitochondrial dysfunction to foster PCOS (Rutkowska and Rachoń 2014; Matuszczak et al. 2019). HepG2 cells treated with BPA (10 and 100 nM for 2–12 h) displayed reduced oxygen consumption rate and ATP production resulting in altered mitochondrial morphology and functionalities (Moon et al. 2012).
BPA-exposed rats showed enhanced protein oxidation, lipid peroxidation, and substantial reduction in the enzymes of mitochondrial complex I–V (150, 250, and 500 mg/kg for 14 days) (Khan et al. 2016). In mice, oral administration of BPA (10 mg/kg) for 14 days diminished mitochondrial enzyme activities, including malate dehydrogenase, NADH dehydrogenase, succinate dehydrogenase, monoamine oxidase, and isocitrate dehydrogenase (Anjum et al. 2011). Mitochondrial enzyme activity declined in BPA-treated rats (10 mg/kg of BPA for 14 days), and subsequent testicular dysfunction was observed (El-Beshbishy et al. 2013). A recent study using Caenorhabditis elegans showed that exposure to 1 mM BPA shortened life span and increased the age-related changes in neurons with a concomitant decline in oxygen consumption rate and MMP (Hyun et al. 2021). Taken together, various experimental evidence in numerous cells or tissue types emphasize the potency of BPA to impair bioenergetics, ATP levels, and mitochondrial respiration (Table 3).
Approaches to Mitigate the Toxicological Effects of BPA
BPA-induced mitochondrial dysfunction plays a crucial role in the pathogenesis of many diseases (Meli et al. 2020). Activation of the oxidative stress pathway is an effective mechanism of BPA-mediated mitochondrial dysfunction (Gassman 2017). Thus, targeting the oxidative stress pathway can help reverse the toxicological effects of BPA. In this direction, several previous investigations have demonstrated the ability of vitamins and co-factors, natural extracts, melatonin, selenium, and methyl donors to reverse the toxicological effects exerted by BPA (Anjum et al. 2011; Khalaf et al. 2019; Meli et al. 2020) (Table 4). This section describes various approaches to reverse the mitochondrial dysfunction caused by BPA. For instance, astaxanthin (ATX) treatment restored BPA-induced reduction in mitochondrial complex activity in kidney tissues (Jiang et al. 2020). Treatment with 1,25-dihydroxy vitamin D3 (1,25-D3) may help reduce the toxicity of BPA in reproductive cells. Besides, 1,25-D3 increased mtDNA content, biogenesis, ATP production, and cellular oxygen consumption rate via PI3K-AKT signaling to minimize reproductive toxicity in ovarian granulosa cells (Lee et al. 2019). BPA exposure induces apoptosis in various cell types via mitochondria-dependent and independent pathways (Wang et al. 2019b). A study showed that treatment with melatonin could control apoptosis, protect testes, and improve sperm quality against BPA (Othman et al. 2016). BPA disrupted thyroid hormone synthesis and metabolism in rats and induced pathological changes by increasing inducible nitric oxide synthase and decreasing NRF2 expression. Treatment with ginger extract protects against BPA-induced thyroid damage by targeting the oxidative pathway and restoring antioxidant balance (Mohammed et al. 2020). Another study showed that α-lipoic acid treatment reversed the neuro-behavioral toxicity induced by BPA (Khan et al. 2018). In rat liver, quercetin protects against BPA-induced mitochondrial toxicity (Mahdavinia et al. 2019). N-Acetyl Cysteine (NAC) is a powerful antioxidant extensively used to relieve oxidative stress (Kobroob et al. 2021). Male Wistar rats exposed to BPA showed mitochondrial swelling and increased ROS production in the renal tissue (Kobroob et al. 2021). NAC treatment restored mitochondrial integrity and oxidative balance by modulating the AMPK-SIRT3-SOD2 axis (Kobroob et al. 2021). Thus, NAC can be used to prevent the renal toxicities caused due to long-term exposure to BPA. Additionally, in ARPE-19 cells, BPA-induced oxidative stress and cytotoxicity were significantly reduced upon treatment with NAC (Chiang et al. 2022). Coenzyme-Q10 (CoQ10), a powerful antioxidant, has reduced apoptosis induced by BPA. The reduced incidence of apoptosis upon CoQ10 treatment involved decreased ROS levels and improved MMP (Liu et al. 2021). Selenium treatment reversed testicular oxidative stress induced by BPA exposure in mouse model (Rafiee et al. 2021). These data suggest the indispensable role of antioxidant treatment in protecting cells against BPA-induced toxicity.
Conclusion and Future Directions
Despite long-standing safety concerns, various consumer products still use BPA for their production. A plethora of experimental evidence has clearly illustrated the adverse health effects of BPA. The current review summarized the data available in published literature related to the impact of BPA on mitochondrial structure, function, and signaling. Our literature review shows that BPA-induced cellular and molecular alterations are corroborated with impaired mitochondrial structure and function. Further, the mitochondrial toxicities in in-vitro and in-vivo models depend on the dose and duration of BPA exposure. Furthermore, BPA can bring about changes to mitochondria at extremely low doses. The findings of several elegant studies have revealed the role of BPA in modulating mitochondrial biogenesis, bioenergetics, and mitochondria-mediated signaling. However, many studies have used doses higher than the concentration of BPA found in the environment. Towards this, we have highlighted some of the research gaps that require detailed investigation, such as:
-
More comprehensive, systematic, and mechanistic studies like the CLARITY-BPA study need to be undertaken using environmentally relevant doses of BPA to understand its toxicological aspects in general and mitochondrial dysfunction in particular.
-
Large-scale epidemiological analyses using organoid models are lacking to verify the toxicological effects of BPA on mitochondrial functions in humans.
-
Restoring the mitochondrial function via treatment with antioxidant agents or through mitochondria transfer or mitochondria replacement therapy could be attempted to reverse the toxic effects of BPA (Fig. 3).
-
Most studies have focused on the oxidative stress pathway upon BPA exposure. Future investigations should also examine the involvement of alternative pathways responsible for BPA-mediated mitochondrial impairments.
-
Tissue-specific exposure assessments at genomic, epigenomics, transcriptomic, and proteomic levels should be undertaken to comprehensively understand the impact of BPA exposure at the cellular level.
References
Abdel-Rahman HG, Abdelrazek HMA, Zeidan DW et al (2018) Lycopene: hepatoprotective and anti-oxidant effects toward bisphenol A-induced toxicity in female Wistar rats. Oxid Med Cell Longev 2018:1–8. https://doi.org/10.1155/2018/5167524
Aboul Ezz HS, Khadrawy YA, Mourad IM (2015) The effect of bisphenol A on some oxidative stress parameters and acetylcholinesterase activity in the heart of male albino rats. Cytotechnology. https://doi.org/10.1007/s10616-013-9672-1
Adiga D, Nadeem Khan G, Eswaran S et al (2022) Chapter 3. Bisphenol A associated signaling pathways in human diseases. In: Gassman NR (ed) Bisphenol A: a multi-modal endocrine disruptor. Royal Society of Chemistry, Cambridge, pp 42–86
Agarwal S, Yadav A, Tiwari SK et al (2016) Dynamin-related protein 1 inhibition mitigates bisphenol A-mediated alterations in mitochondrial dynamics and neural stem cell proliferation and differentiation. J Biol Chem 291:15923–15939. https://doi.org/10.1074/jbc.M115.709493
Allard P, Colaiacovo MP (2010) Bisphenol A impairs the double-strand break repair machinery in the germline and causes chromosome abnormalities. Proc Natl Acad Sci USA 107:20405–20410. https://doi.org/10.1073/pnas.1010386107
Almeida S, Raposo A, Almeida-González M, Carrascosa C (2018) Bisphenol A: food exposure and impact on human health. Compr Rev Food Sci Food Saf. https://doi.org/10.1111/1541-4337.12388
Anand SK, Sharma A, Singh N, Kakkar P (2020) Activation of autophagic flux via LKB1/AMPK/mTOR axis against xenoestrogen bisphenol-A exposure in primary rat hepatocytes. Food Chem Toxicol 141:111314. https://doi.org/10.1016/j.fct.2020.111314
Andra SS, Austin C, Yang J et al (2016) Recent advances in simultaneous analysis of bisphenol A and its conjugates in human matrices: exposure biomarker perspectives. Sci Total Environ 572:770–781. https://doi.org/10.1016/j.scitotenv.2016.07.062
Anjum S, Rahman S, Kaur M et al (2011) Melatonin ameliorates bisphenol A-induced biochemical toxicity in testicular mitochondria of mouse. Food Chem Toxicol 49:2849–2854. https://doi.org/10.1016/j.fct.2011.07.062
Aydoğan M, Korkmaz A, Barlas N, Kolankaya D (2008) The effect of vitamin C on bisphenol A, nonylphenol and octylphenol induced brain damages of male rats. Toxicology 249:35–39. https://doi.org/10.1016/j.tox.2008.04.002
Babu S, Uppu S, Claville MO, Uppu RM (2013) Prooxidant actions of bisphenol A (BPA) phenoxyl radicals: implications to BPA-related oxidative stress and toxicity. Toxicol Mech Methods 23:273–280. https://doi.org/10.3109/15376516.2012.753969
Bansal A, Rashid C, Xin F et al (2017) Sex- and dose-specific effects of maternal bisphenol a exposure on pancreatic islets of first- and second-generation adult mice offspring. Environ Health Perspect 125:097022. https://doi.org/10.1289/EHP1674
Batista-Silva H, Rodrigues K, Sousa de Moura KR et al (2020) Role of bisphenol A on calcium influx and its potential toxicity on the testis of Danio rerio. Ecotoxicol Environ Saf 202:110876. https://doi.org/10.1016/j.ecoenv.2020.110876
Begum M, Paul P, Das D, Ghosh S (2020) Endocrine-disrupting plasticizer bisphenol A (BPA) exposure causes change in behavioral attributes in Drosophila melanogaster. Toxicol Environ Health Sci 12:237–246. https://doi.org/10.1007/s13530-020-00052-8
Behmanesh MA, Najafzadehvarzi H, Poormoosavi SM (2018) Protective effect of Aloe vera extract against bisphenol A induced testicular toxicity in Wistar rats. Cell J 20:278–283. https://doi.org/10.22074/cellj.2018.5256
Bernier MR, Vandenberg LN (2017) Handling of thermal paper: implications for dermal exposure to bisphenol A and its alternatives. PLoS ONE. https://doi.org/10.1371/journal.pone.0178449
Bhatti JS, Bhatti GK, Reddy PH (2017) Mitochondrial dysfunction and oxidative stress in metabolic disorders—a step towards mitochondria based therapeutic strategies. Biochim Biophys Acta 1863:1066–1077. https://doi.org/10.1016/j.bbadis.2016.11.010
Bilgi A, Abalı R, Bilgi PT et al (2019) The apoptotic effects of bisphenol A exposure on the rat ovary: an experimental study. Environ Sci Pollut Res 26:10198–10203. https://doi.org/10.1007/s11356-019-04487-6
Bindhumol V, Chitra KC, Mathur PP (2003) Bisphenol A induces reactive oxygen species generation in the liver of male rats. Toxicology 188:117–124. https://doi.org/10.1016/S0300-483X(03)00056-8
Birla H, Keswani C, Rai SN et al (2019) Neuroprotective effects of Withania somnifera in BPA induced-cognitive dysfunction and oxidative stress in mice. Behav Brain Funct 15:9. https://doi.org/10.1186/s12993-019-0160-4
Biswas S, Ghosh S, Samanta A et al (2020) Bisphenol A impairs reproductive fitness in zebrafish ovary: potential involvement of oxidative/nitrosative stress, inflammatory and apoptotic mediators. Environ Pollut 267:115692. https://doi.org/10.1016/j.envpol.2020.115692
Bosch-Panadero E, Mas S, Civantos E et al (2018) Bisphenol A is an exogenous toxin that promotes mitochondrial injury and death in tubular cells. Environ Toxicol 33:325–332. https://doi.org/10.1002/tox.22519
Bravo-Sagua R, Parra V, López-Crisosto C et al (2017) Calcium transport and signaling in mitochondria. Comprehensive physiology. Wiley, Hoboken, pp 623–634
Bustos G, Cruz P, Lovy A, Cárdenas C (2017) Endoplasmic reticulum-mitochondria calcium communication and the regulation of mitochondrial metabolism in cancer: a novel potential target. Front Oncol. https://doi.org/10.3389/fonc.2017.00199
Camacho L, Lewis SM, Vanlandingham MM et al (2019) A two-year toxicology study of bisphenol A (BPA) in Sprague–Dawley rats: CLARITY-BPA core study results. Food Chem Toxicol 132:110728. https://doi.org/10.1016/j.fct.2019.110728
Carchia E, Porreca I, Almeida PJ et al (2015) Evaluation of low doses BPA-induced perturbation of glycemia by toxicogenomics points to a primary role of pancreatic islets and to the mechanism of toxicity. Cell Death Dis 6:e1959–e1959. https://doi.org/10.1038/cddis.2015.319
Chen J, Xiao Y, Gai Z et al (2015) Reproductive toxicity of low level bisphenol A exposures in a two-generation zebrafish assay: evidence of male-specific effects. Aquat Toxicol 169:204–214. https://doi.org/10.1016/j.aquatox.2015.10.020
Chen Y, Wang Y, Ding G et al (2018) Association between bisphenol a exposure and idiopathic central precocious puberty (ICPP) among school-aged girls in Shanghai, China. Environ Int 115:410–416. https://doi.org/10.1016/j.envint.2018.02.041
Cheng W, Yang S, Li X et al (2020) Low doses of BPA induced abnormal mitochondrial fission and hypertrophy in human embryonic stem cell-derived cardiomyocytes via the calcineurin-DRP1 signaling pathway: a comparison between XX and XY cardiomyocytes. Toxicol Appl Pharmacol 388:114850. https://doi.org/10.1016/j.taap.2019.114850
Chiang Y-W, Su C-H, Sun H-Y et al (2022) Bisphenol A induced apoptosis via oxidative stress generation involved Nrf2/HO-1 pathway and mitochondrial dependent pathways in human retinal pigment epithelium (ARPE-19) cells. Environ Toxicol 37:131–141. https://doi.org/10.1002/tox.23384
Chitra K (2003) Induction of oxidative stress by bisphenol A in the epididymal sperm of rats. Toxicology 185:119–127. https://doi.org/10.1016/S0300-483X(02)00597-8
Cho YJ, Bin PS, Park JW et al (2018) Bisphenol A modulates inflammation and proliferation pathway in human endometrial stromal cells by inducing oxidative stress. Reprod Toxicol 81:41–49. https://doi.org/10.1016/j.reprotox.2018.06.016
Choi B-I, Harvey AJ, Green MP (2016) Bisphenol A affects early bovine embryo development and metabolism that is negated by an oestrogen receptor inhibitor. Sci Rep 6:29318. https://doi.org/10.1038/srep29318
Choudhury AR, Singh KK (2017) Mitochondrial determinants of cancer health disparities. Semin Cancer Biol 47:125–146. https://doi.org/10.1016/j.semcancer.2017.05.001
Chouhan S, Yadav SK, Prakash J et al (2015) Increase in the expression of inducible nitric oxide synthase on exposure to bisphenol A: a possible cause for decline in steroidogenesis in male mice. Environ Toxicol Pharmacol 39:405–416. https://doi.org/10.1016/j.etap.2014.09.014
Cui H, Kong Y, Zhang H (2012) Oxidative stress, mitochondrial dysfunction, and aging. J Signal Transduct 2012:1–13. https://doi.org/10.1155/2012/646354
Derouiche S, Warnier M, Mariot P et al (2013) Bisphenol A stimulates human prostate cancer cell migration via remodelling of calcium signalling. SpringerPlus 2:54. https://doi.org/10.1186/2193-1801-2-54
Di Pietro P, D’Auria R, Viggiano A et al (2020) Bisphenol A induces DNA damage in cells exerting immune surveillance functions at peripheral and central level. Chemosphere 254:126819. https://doi.org/10.1016/j.chemosphere.2020.126819
Dutta M, Paul G (2019) Gallic acid protects rat liver mitochondria ex vivo from bisphenol A induced oxidative stress mediated damages. Toxicol Rep 6:578–589. https://doi.org/10.1016/j.toxrep.2019.06.011
EFSA (2015) Scientific opinion on the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs. EFSA J 13:3978. https://doi.org/10.2903/j.efsa.2015.3978
El-Beshbishy HA, Aly HAA, El-Shafey M (2013) Lipoic acid mitigates bisphenol A-induced testicular mitochondrial toxicity in rats. Toxicol Ind Health 29:875–887. https://doi.org/10.1177/0748233712446728
Elmore S (2007) Apoptosis: a review of programmed cell death. Toxicol Pathol 35:495–516. https://doi.org/10.1080/01926230701320337
Eweda S, Newairy A, Abdou H, Gaber A (2019) Bisphenol A induced oxidative damage in the hepatic and cardiac tissues of rats: the modulatory role of sesame lignans. Exp Ther Med. https://doi.org/10.3892/etm.2019.8193
Fawzy EI, El Makawy AI, El-Bamby MM, Elhamalawy HO (2018) Improved effect of pumpkin seed oil against the bisphenol-A adverse effects in male mice. Toxicol Rep 5:857–863. https://doi.org/10.1016/j.toxrep.2018.08.014
Feng L, Chen S, Zhang L et al (2019) Bisphenol A increases intestinal permeability through disrupting intestinal barrier function in mice. Environ Pollut 254:112960. https://doi.org/10.1016/j.envpol.2019.112960
Fic A, Žegura B, Sollner Dolenc M et al (2013) Mutagenicity and DNA damage of bisphenol A and its structural analogues in HepG2 cells. Arch Ind Hyg Toxicol 64:189–200. https://doi.org/10.2478/10004-1254-64-2013-2319
Gao H, Yang B-J, Li N et al (2015) Bisphenol A and hormone-associated cancers. Medicine (Baltimore) 94:e211. https://doi.org/10.1097/MD.0000000000000211
Gassman NR (2017) Induction of oxidative stress by bisphenol A and its pleiotropic effects. Environ Mol Mutagen 58:60–71. https://doi.org/10.1002/em.22072
Gassman NR, Coskun E, Stefanick DF et al (2015) Bisphenol A promotes cell survival following oxidative DNA damage in mouse fibroblasts. PLoS ONE 10:e0118819. https://doi.org/10.1371/journal.pone.0118819
Ge L-C, Chen Z-J, Liu H et al (2014) Signaling related with biphasic effects of bisphenol A (BPA) on Sertoli cell proliferation: a comparative proteomic analysis. Biochim Biophys Acta 1840:2663–2673. https://doi.org/10.1016/j.bbagen.2014.05.018
Genuis SJ, Beesoon S, Birkholz D, Lobo RA (2012) Human excretion of bisphenol A: blood, urine, and sweat (BUS) study. J Environ Public Health 2012:1–10. https://doi.org/10.1155/2012/185731
Goyal S, Tiwari S, Seth B et al (2021) Bisphenol-A inhibits mitochondrial biogenesis via impairment of GFER mediated mitochondrial protein import in the rat brain hippocampus. Neurotoxicology 85:18–32. https://doi.org/10.1016/j.neuro.2021.04.001
Gules O, Yildiz M, Naseer Z, Tatar M (2019) Effects of folic acid on testicular toxicity induced by bisphenol-A in male Wistar rats. Biotech Histochem 94:26–35. https://doi.org/10.1080/10520295.2018.1493222
Guo J, Zhao M-H, Shin K-T et al (2017) The possible molecular mechanisms of bisphenol A action on porcine early embryonic development. Sci Rep 7:8632. https://doi.org/10.1038/s41598-017-09282-2
Gureev AP, Shaforostova EA, Popov VN (2019) Regulation of mitochondrial biogenesis as a way for active longevity: interaction between the Nrf2 and PGC-1α signaling pathways. Front Genet. https://doi.org/10.3389/fgene.2019.00435
Hall AR, Burke N, Dongworth RK, Hausenloy DJ (2014) Mitochondrial fusion and fission proteins: novel therapeutic targets for combating cardiovascular disease. Br J Pharmacol 171:1890–1906. https://doi.org/10.1111/bph.12516
Han Y, Chen JZ (2013) Oxidative stress induces mitochondrial DNA damage and cytotoxicity through independent mechanisms in human cancer cells. Biomed Res Int 2013:1–8. https://doi.org/10.1155/2013/825065
Hassan ZK, Elobeid MA, Virk P et al (2012) Bisphenol A induces hepatotoxicity through oxidative stress in rat model. Oxid Med Cell Longev 2012:1–6. https://doi.org/10.1155/2012/194829
Heindel JJ, Newbold RR, Bucher JR et al (2015) NIEHS/FDA CLARITY-BPA research program update. Reprod Toxicol 58:33–44. https://doi.org/10.1016/j.reprotox.2015.07.075
Heindel JJ, Belcher S, Flaws JA et al (2020) Data integration, analysis, and interpretation of eight academic CLARITY-BPA studies. Reprod Toxicol 98:29–60. https://doi.org/10.1016/j.reprotox.2020.05.014
Hertweck KL, Dasgupta S (2017) The landscape of mtDNA modifications in cancer: a tale of two cities. Front Oncol. https://doi.org/10.3389/fonc.2017.00262
Hornos Carneiro MF, Shin N, Karthikraj R et al (2020) Antioxidant CoQ10 restores fertility by rescuing bisphenol A-induced oxidative DNA damage in the Caenorhabditis elegans germline. Genetics 214:381–395. https://doi.org/10.1534/genetics.119.302939
Hsu C-C, Tseng L-M, Lee H-C (2016) Role of mitochondrial dysfunction in cancer progression. Exp Biol Med 241:1281–1295. https://doi.org/10.1177/1535370216641787
Hu L, Yao X, Shen Y (2016) Altered mitochondrial DNA copy number contributes to human cancer risk: evidence from an updated meta-analysis. Sci Rep 6:35859. https://doi.org/10.1038/srep35859
Huang F-M, Chang Y-C, Lee S-S et al (2018) Bisphenol A exhibits cytotoxic or genotoxic potential via oxidative stress-associated mitochondrial apoptotic pathway in murine macrophages. Food Chem Toxicol 122:215–224. https://doi.org/10.1016/j.fct.2018.09.078
Huang C-F, Liu S-H, Su C-C et al (2021) Roles of ERK/Akt signals in mitochondria-dependent and endoplasmic reticulum stress-triggered neuronal cell apoptosis induced by 4-methyl-2,4-bis(4-hydroxyphenyl)pent-1-ene, a major active metabolite of bisphenol A. Toxicology 455:152764. https://doi.org/10.1016/j.tox.2021.152764
Huc L, Lemarié A, Guéraud F, Héliès-Toussaint C (2012) Low concentrations of bisphenol A induce lipid accumulation mediated by the production of reactive oxygen species in the mitochondria of HepG2 cells. Toxicol In Vitro 26:709–717. https://doi.org/10.1016/j.tiv.2012.03.017
Hyun M, Rathor L, Kim H-J et al (2021) Comparative toxicities of BPA, BPS, BPF, and TMBPF in the nematode Caenorhabditis elegans and mammalian fibroblast cells. Toxicology 461:152924. https://doi.org/10.1016/j.tox.2021.152924
Ighodaro OM, Akinloye OA (2018) First line defence antioxidants-superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GPX): their fundamental role in the entire anti-oxidant defence grid. Alex J Med 54:287–293. https://doi.org/10.1016/j.ajme.2017.09.001
Inadera H (2015) Neurological effects of bisphenol A and its analogues. Int J Med Sci 12:926–936. https://doi.org/10.7150/ijms.13267
Jain S, Mahendra Kumar CH, Suranagi UD, Mediratta PK (2011) Protective effect of N-acetylcysteine on bisphenol A-induced cognitive dysfunction and oxidative stress in rats. Food Chem Toxicol 49:1404–1409. https://doi.org/10.1016/j.fct.2011.03.032
Jalal N, Surendranath AR, Pathak JL et al (2018) Bisphenol A (BPA) the mighty and the mutagenic. Toxicol Rep 5:76–84. https://doi.org/10.1016/j.toxrep.2017.12.013
Jiang Y, Liu J, Li Y et al (2014a) Prenatal exposure to bisphenol A at the reference dose impairs mitochondria in the heart of neonatal rats. J Appl Toxicol 34:1012–1022. https://doi.org/10.1002/jat.2924
Jiang Y, Xia W, Zhu Y et al (2014b) Mitochondrial dysfunction in early life resulted from perinatal bisphenol A exposure contributes to hepatic steatosis in rat offspring. Toxicol Lett 228:85–92. https://doi.org/10.1016/j.toxlet.2014.04.013
Jiang Y, Xia W, Yang J et al (2015) BPA-induced DNA hypermethylation of the master mitochondrial gene PGC-1α contributes to cardiomyopathy in male rats. Toxicology 329:21–31. https://doi.org/10.1016/j.tox.2015.01.001
Jiang W, Zhao H, Zhang L et al (2020) Maintenance of mitochondrial function by astaxanthin protects against bisphenol A-induced kidney toxicity in rats. Biomed Pharmacother 121:109629. https://doi.org/10.1016/j.biopha.2019.109629
Jiao X-F, Liang Q-M, Wu D et al (2019) Effects of acute fluorene-9-bisphenol exposure on mouse oocyte in vitro maturation and its possible mechanisms. Environ Mol Mutagen 60:243–253. https://doi.org/10.1002/em.22258
Kabekkodu SP, Bhat S, Mascarenhas R et al (2014) Mitochondrial DNA variation analysis in cervical cancer. Mitochondrion 16:73–82. https://doi.org/10.1016/j.mito.2013.07.001
Kabuto H, Hasuike S, Minagawa N, Shishibori T (2003) Effects of bisphenol A on the metabolisms of active oxygen species in mouse tissues. Environ Res 93:31–35. https://doi.org/10.1016/S0013-9351(03)00062-8
Kabuto H, Amakawa M, Shishibori T (2004) Exposure to bisphenol A during embryonic/fetal life and infancy increases oxidative injury and causes underdevelopment of the brain and testis in mice. Life Sci 74:2931–2940. https://doi.org/10.1016/j.lfs.2003.07.060
Kalb AC, Kalb AL, Cardoso TF et al (2016) Maternal transfer of bisphenol A during nursing causes sperm impairment in male offspring. Arch Environ Contam Toxicol 70:793–801. https://doi.org/10.1007/s00244-015-0199-7
Kasperski A, Kasperska R (2018) Bioenergetics of life, disease and death phenomena. Theory Biosci 137:155–168. https://doi.org/10.1007/s12064-018-0266-5
Kaur K, Chauhan V, Gu F, Chauhan A (2014) Bisphenol A induces oxidative stress and mitochondrial dysfunction in lymphoblasts from children with autism and unaffected siblings. Free Radic Biol Med 76:25–33. https://doi.org/10.1016/j.freeradbiomed.2014.07.030
Kaur S, Saluja M, Bansal MP (2018) Bisphenol A induced oxidative stress and apoptosis in mice testes: modulation by selenium. Andrologia 50:e12834. https://doi.org/10.1111/and.12834
Kaur S, Singh G, Sadwal S, Aniqa A (2020) Alleviating impact of hydroethanolic Murraya koenigii leaves extract on bisphenol A instigated testicular lethality and apoptosis in mice. Andrologia. https://doi.org/10.1111/and.13504
Kazmi STB, Majid M, Maryam S et al (2018) Quercus dilatata Lindl. ex Royle ameliorates BPA induced hepatotoxicity in Sprague Dawley rats. Biomed Pharmacother 102:728–738. https://doi.org/10.1016/j.biopha.2018.03.097
Khalaf A, Ahmed W, Moselhy W et al (2019) Protective effects of selenium and nano-selenium on bisphenol-induced reproductive toxicity in male rats. Hum Exp Toxicol 38:398–408. https://doi.org/10.1177/0960327118816134
Khan S, Beigh S, Chaudhari BP et al (2016) Mitochondrial dysfunction induced by bisphenol A is a factor of its hepatotoxicity in rats. Environ Toxicol 31:1922–1934. https://doi.org/10.1002/tox.22193
Khan J, Salhotra S, Ahmad S et al (2018) The protective effect of α-lipoic acid against bisphenol A-induced neurobehavioral toxicity. Neurochem Int 118:166–175. https://doi.org/10.1016/j.neuint.2018.06.005
Khan NG, Correia J, Adiga D et al (2021) A comprehensive review on the carcinogenic potential of bisphenol A: clues and evidence. Environ Sci Pollut Res 28:19643–19663. https://doi.org/10.1007/s11356-021-13071-w
Khodayar MJ, Kalantari H, Mahdavinia M et al (2020) Protective effect of naringin against BPA-induced cardiotoxicity through prevention of oxidative stress in male Wistar rats. Drug Chem Toxicol 43:85–95. https://doi.org/10.1080/01480545.2018.1504958
Kobroob A, Peerapanyasut W, Chattipakorn N, Wongmekiat O (2018) Damaging effects of bisphenol A on the kidney and the protection by melatonin: emerging evidences from in vivo and in vitro studies. Oxid Med Cell Longev 2018:1–15. https://doi.org/10.1155/2018/3082438
Kobroob A, Peerapanyasut W, Kumfu S et al (2021) Effectiveness of N-acetylcysteine in the treatment of renal deterioration caused by long-term exposure to bisphenol A. Biomolecules. https://doi.org/10.3390/biom11050655
Koda T, Morita M, Imai H (2007) Retinoic acid inhibits uterotrophic activity of bisphenol A in adult ovariectomized rats. J Nutr Sci Vitaminol (Tokyo) 53:432–436. https://doi.org/10.3177/jnsv.53.432
Konieczna A, Rutkowska A, Rachoń D (2015) Health risk of exposure to bisphenol A (BPA). Rocz Panstw Zakl Hig 66:5–11
Koong LY, Watson CS (2015) Rapid, nongenomic signaling effects of several xenoestrogens involved in early- vs. late-stage prostate cancer cell proliferation. Endocr Disruptors 3:e995003. https://doi.org/10.4161/23273747.2014.995003
Lamb R, Bonuccelli G, Ozsvári B et al (2015) Mitochondrial mass, a new metabolic biomarker for stem-like cancer cells: understanding WNT/FGF-driven anabolic signaling. Oncotarget 6:30453–30471. https://doi.org/10.18632/oncotarget.5852
Lee SG, Kim JY, Chung JY et al (2013) Bisphenol A exposure during adulthood causes augmentation of follicular atresia and luteal regression by decreasing 17β-estradiol synthesis via downregulation of aromatase in rat ovary. Environ Health Perspect. https://doi.org/10.1289/ehp.1205823
Lee C-T, Wang J-Y, Chou K-Y, Hsu M-I (2019) 1,25-Dihydroxyvitamin D3 modulates the effects of sublethal BPA on mitochondrial function via activating PI3K-Akt pathway and 17β-estradiol secretion in rat granulosa cells. J Steroid Biochem Mol Biol 185:200–211. https://doi.org/10.1016/j.jsbmb.2018.09.002
Leem Y-H, Oh S, Kang H-J et al (2017) BPA-toxicity via superoxide anion overload and a deficit in β-catenin signaling in human bone mesenchymal stem cells. Environ Toxicol 32:344–352. https://doi.org/10.1002/tox.22239
Li J, Bach A, Crawford RB et al (2018) CLARITY-BPA: effects of chronic bisphenol A exposure on the immune system: part 1—quantification of the relative number and proportion of leukocyte populations in the spleen and thymus. Toxicology 396–397:46–53. https://doi.org/10.1016/j.tox.2018.01.004
Li H, Slone J, Fei L, Huang T (2019) Mitochondrial DNA variants and common diseases: a mathematical model for the diversity of age-related mtDNA mutations. Cells 8:608. https://doi.org/10.3390/cells8060608
Liao C, Liu F, Guo Y et al (2012) Occurrence of eight bisphenol analogues in indoor dust from the United States and several asian countries: implications for human exposure. Environ Sci Technol 46:9138–9145. https://doi.org/10.1021/es302004w
Lin Y, Sun X, Qiu L et al (2013) Exposure to bisphenol A induces dysfunction of insulin secretion and apoptosis through the damage of mitochondria in rat insulinoma (INS-1) cells. Cell Death Dis 4:e460–e460. https://doi.org/10.1038/cddis.2012.206
Liou G-Y, Storz P (2010) Reactive oxygen species in cancer. Free Radic Res 44:479–496. https://doi.org/10.3109/10715761003667554
Liu YJ, McIntyre RL, Janssens GE, Houtkooper RH (2020) Mitochondrial fission and fusion: a dynamic role in aging and potential target for age-related disease. Mech Ageing Dev 186:111212. https://doi.org/10.1016/j.mad.2020.111212
Liu Y, Yao Y, Tao W et al (2021) Corrigendum to “Coenzyme Q10 ameliorates BPA-induced apoptosis by regulating autophagy-related lysosomal pathways” [Ecotoxicol. Environ. Saf. 221 (2021) 112450]. Ecotoxicol Environ Saf 225:112726. https://doi.org/10.1016/j.ecoenv.2021.112726
Mahdavinia M, Alizadeh S, Raesi Vanani A et al (2019) Effects of quercetin on bisphenol A-induced mitochondrial toxicity in rat liver. Iran J Basic Med Sci 22:499–505. https://doi.org/10.22038/ijbms.2019.32486.7952
Majid M, Ijaz F, Baig MW et al (2019) Scientific validation of ethnomedicinal use of Ipomoea batatas L. Lam. as aphrodisiac and gonadoprotective agent against bisphenol A induced testicular toxicity in male Sprague Dawley rats. Biomed Res Int 2019:1–21. https://doi.org/10.1155/2019/8939854
Marraudino M, Bonaldo B, Farinetti A et al (2019) Metabolism disrupting chemicals and alteration of neuroendocrine circuits controlling food intake and energy metabolism. Front Endocrinol (Lausanne). https://doi.org/10.3389/fendo.2018.00766
Marroqui L, Tudurí E, Alonso-Magdalena P et al (2018) Mitochondria as target of endocrine-disrupting chemicals: implications for type 2 diabetes. J Endocrinol 239:R27–R45. https://doi.org/10.1530/JOE-18-0362
Matuszczak E, Komarowska MD, Debek W, Hermanowicz A (2019) The impact of bisphenol A on fertility, reproductive system, and development: a review of the literature. Int J Endocrinol 2019:1–8. https://doi.org/10.1155/2019/4068717
McWilliams TG, Muqit MM (2017) PINK1 and Parkin: emerging themes in mitochondrial homeostasis. Curr Opin Cell Biol 45:83–91. https://doi.org/10.1016/j.ceb.2017.03.013
Meli R, Monnolo A, Annunziata C et al (2020) Oxidative stress and BPA toxicity: an anti-oxidant approach for male and female reproductive dysfunction. Anti-oxidants 9:405. https://doi.org/10.3390/antiox9050405
Meng L, Liu J, Wang C et al (2021) Sex-specific oxidative damage effects induced by BPA and its analogs on primary hippocampal neurons attenuated by EGCG. Chemosphere 264:128450. https://doi.org/10.1016/j.chemosphere.2020.128450
Meyer JN, Leung MCK, Rooney JP et al (2013) Mitochondria as a target of environmental toxicants. Toxicol Sci 134:1–17. https://doi.org/10.1093/toxsci/kft102
Moghaddam HS, Samarghandian S, Farkhondeh T (2015) Effect of bisphenol A on blood glucose, lipid profile and oxidative stress indices in adult male mice. Toxicol Mech Methods 25:507–513. https://doi.org/10.3109/15376516.2015.1056395
Mohamad Zaid SS, Kassim NM, Othman S (2015) Tualang honey protects against BPA-induced morphological abnormalities and disruption of ER α, ER β, and C3 mRNA and protein expressions in the uterus of rats. Evid Based Complement Altern Med 2015:1–18. https://doi.org/10.1155/2015/202874
Mohammed ET, Hashem KS, Ahmed AE et al (2020) Ginger extract ameliorates bisphenol A (BPA)-induced disruption in thyroid hormones synthesis and metabolism: involvement of Nrf-2/HO-1 pathway. Sci Total Environ 703:134664. https://doi.org/10.1016/j.scitotenv.2019.134664
Moon MK, Kim MJ, Jung IK et al (2012) Bisphenol A impairs mitochondrial function in the liver at doses below the no observed adverse effect level. J Korean Med Sci 27:644. https://doi.org/10.3346/jkms.2012.27.6.644
Moon S, Yu SH, Lee CB et al (2021) Effects of bisphenol A on cardiovascular disease: an epidemiological study using National Health and Nutrition Examination Survey 2003–2016 and meta-analysis. Sci Total Environ 763:142941. https://doi.org/10.1016/j.scitotenv.2020.142941
Mou D, Wang J, Liu H et al (2018) Maternal methyl donor supplementation during gestation counteracts bisphenol A-induced oxidative stress in sows and offspring. Nutrition 45:76–84. https://doi.org/10.1016/j.nut.2017.03.012
Nachman RM, Hartle JC, Lees PSJ, Groopman JD (2014) Early life metabolism of bisphenol A: a systematic review of the literature. Curr Environ Health Rep 1:90–100. https://doi.org/10.1007/s40572-013-0003-7
Nakagawa Y, Tayama S (2000) Metabolism and cytotoxicity of bisphenol A and other bisphenols in isolated rat hepatocytes. Arch Toxicol 74:99–105. https://doi.org/10.1007/s002040050659
Neri M, Virzì GM, Brocca A et al (2015) In vitro cytotoxicity of bisphenol A in monocytes cell line. Blood Purif 40:180–186. https://doi.org/10.1159/000437039
Nomiri S, Hoshyar R, Ambrosino C et al (2019) A mini review of bisphenol A (BPA) effects on cancer-related cellular signaling pathways. Environ Sci Pollut Res 26:8459–8467. https://doi.org/10.1007/s11356-019-04228-9
Olchowik-Grabarek E, Makarova K, Mavlyanov S et al (2018) Comparative analysis of BPA and HQ toxic impacts on human erythrocytes, protective effect mechanism of tannins (Rhus typhina). Environ Sci Pollut Res 25:1200–1209. https://doi.org/10.1007/s11356-017-0520-2
Omar García-Lepe U, Ma Bermúdez-Cruz R (2019) Mitochondrial genome maintenance: damage and repair pathways. In: DNA repair—an update. IntechOpen, London
Ooe H, Taira T, Iguchi-Ariga SMM, Ariga H (2005) Induction of reactive oxygen species by bisphenol A and abrogation of bisphenol A-induced cell injury by DJ-1. Toxicol Sci 88:114–126. https://doi.org/10.1093/toxsci/kfi278
Osellame LD, Blacker TS, Duchen MR (2012) Cellular and molecular mechanisms of mitochondrial function. Best Pract Res Clin Endocrinol Metab 26:711–723. https://doi.org/10.1016/j.beem.2012.05.003
Othman AI, Edrees GM, El-Missiry MA et al (2016) Melatonin controlled apoptosis and protected the testes and sperm quality against bisphenol A-induced oxidative toxicity. Toxicol Ind Health 32:1537–1549. https://doi.org/10.1177/0748233714561286
Pan M-H, Wu Y-K, Liao B-Y et al (2021) Bisphenol A exposure disrupts organelle distribution and functions during mouse oocyte maturation. Front Cell Dev Biol 9:661155. https://doi.org/10.3389/fcell.2021.661155
Pang Q, Li Y, Meng L et al (2019) Neurotoxicity of BPA, BPS, and BPB for the hippocampal cell line (HT-22): an implication for the replacement of BPA in plastics. Chemosphere 226:545–552. https://doi.org/10.1016/j.chemosphere.2019.03.177
Peerapanyasut W, Kobroob A, Palee S et al (2019) N-acetylcysteine attenuates the increasing severity of distant organ liver dysfunction after acute kidney injury in rats exposed to bisphenol A. Antioxidants 8:497. https://doi.org/10.3390/antiox8100497
Peerapanyasut W, Kobroob A, Palee S et al (2020) Bisphenol A aggravates renal ischemia–reperfusion injury by disrupting mitochondrial homeostasis and N-acetylcysteine mitigates the injurious outcomes. IUBMB Life 72:758–770. https://doi.org/10.1002/iub.2175
Pfeifer D, Chung YM, Hu MC-T (2015) Effects of low-dose bisphenol A on DNA damage and proliferation of breast cells: the role of c-Myc. Environ Health Perspect 123:1271–1279. https://doi.org/10.1289/ehp.1409199
Pickles S, Vigié P, Youle RJ (2018) Mitophagy and quality control mechanisms in mitochondrial maintenance. Curr Biol 28:R170–R185. https://doi.org/10.1016/j.cub.2018.01.004
Pierelli G, Stanzione R, Forte M et al (2017) Uncoupling protein 2: a key player and a potential therapeutic target in vascular diseases. Oxid Med Cell Longev 2017:1–11. https://doi.org/10.1155/2017/7348372
Ponniah M, Billett EE, De Girolamo LA (2015) Bisphenol A increases BeWo trophoblast survival in stress-induced paradigms through regulation of oxidative stress and apoptosis. Chem Res Toxicol 28:1693–1703. https://doi.org/10.1021/acs.chemrestox.5b00093
Poormoosavi SM, Najafzadehvarzi H, Behmanesh MA, Amirgholami R (2018) Protective effects of Asparagus officinalis extract against bisphenol A-induced toxicity in Wistar rats. Toxicol Rep 5:427–433. https://doi.org/10.1016/j.toxrep.2018.02.010
Popov L (2020) Mitochondrial biogenesis: an update. J Cell Mol Med 24:4892–4899. https://doi.org/10.1111/jcmm.15194
Porreca I, Ulloa Severino L, D’Angelo F et al (2016) “Stockpile” of slight transcriptomic changes determines the indirect genotoxicity of low-dose BPA in thyroid cells. PLoS ONE 11:e0151618. https://doi.org/10.1371/journal.pone.0151618
Prins GS, Hu W-Y, Xie L et al (2018) Evaluation of bisphenol A (BPA) exposures on prostate stem cell homeostasis and prostate cancer risk in the NCTR-Sprague–Dawley rat: an NIEHS/FDA CLARITY-BPA Consortium Study. Environ Health Perspect 126:117001. https://doi.org/10.1289/EHP3953
Prins GS, Patisaul HB, Belcher SM, Vandenberg LN (2019) CLARITY-BPA academic laboratory studies identify consistent low-dose bisphenol A effects on multiple organ systems. Basic Clin Pharmacol Toxicol 125:14–31. https://doi.org/10.1111/bcpt.13125
Qu W, Zhao Z, Chen S et al (2018) Bisphenol A suppresses proliferation and induces apoptosis in colonic epithelial cells through mitochondrial and MAPK/AKT pathways. Life Sci 208:167–174. https://doi.org/10.1016/j.lfs.2018.07.040
Rachoń D (2015) Endocrine disrupting chemicals (EDCs) and female cancer: informing the patients. Rev Endocr Metab Disord 16:359–364. https://doi.org/10.1007/s11154-016-9332-9
Rafiee Z, Rezaee-Tazangi F, Zeidooni L et al (2021) Protective effects of selenium on bisphenol A-induced oxidative stress in mouse testicular mitochondria and sperm motility. JBRA Assist Reprod 25:459–465. https://doi.org/10.5935/1518-0557.20210010
Rahman MS, Kwon W-S, Yoon S-J et al (2016) A novel approach to assessing bisphenol-A hazards using an in vitro model system. BMC Genomics 17:577. https://doi.org/10.1186/s12864-016-2979-5
Rahman MS, Kang K-H, Arifuzzaman S et al (2019) Effect of anti-oxidants on BPA-induced stress on sperm function in a mouse model. Sci Rep 9:10584. https://doi.org/10.1038/s41598-019-47158-9
Rezaee-Tazangi F, Zeidooni L, Rafiee Z et al (2020) Taurine effects on bisphenol A-induced oxidative stress in the mouse testicular mitochondria and sperm motility. JBRA Assist Reprod. https://doi.org/10.5935/1518-0557.20200017
Rezg R, El-Fazaa S, Gharbi N, Mornagui B (2014) Bisphenol A and human chronic diseases: current evidences, possible mechanisms, and future perspectives. Environ Int 64:83–90. https://doi.org/10.1016/j.envint.2013.12.007
Ribeiro E, Ladeira C, Viegas S (2017) Occupational exposure to bisphenol A (BPA): a reality that still needs to be unveiled. Toxics 5:22. https://doi.org/10.3390/toxics5030022
Rochester JR (2013) Bisphenol A and human health: a review of the literature. Reprod Toxicol 42:132–155. https://doi.org/10.1016/j.reprotox.2013.08.008
Rubin BS (2011) Bisphenol A: an endocrine disruptor with widespread exposure and multiple effects. J Steroid Biochem Mol Biol 127:27–34. https://doi.org/10.1016/j.jsbmb.2011.05.002
Rutkowska A, Rachoń D (2014) Bisphenol A (BPA) and its potential role in the pathogenesis of the polycystic ovary syndrome (PCOS). Gynecol Endocrinol 30:260–265. https://doi.org/10.3109/09513590.2013.871517
Sangai NP, Patel CN, Pandya HA (2018) Ameliorative effects of quercetin against bisphenol A-caused oxidative stress in human erythrocytes: an in vitro and in silico study. Toxicol Res (Camb) 7:1091–1099. https://doi.org/10.1039/C8TX00105G
Seachrist DD, Bonk KW, Ho S-M et al (2016) A review of the carcinogenic potential of bisphenol A. Reprod Toxicol 59:167–182. https://doi.org/10.1016/j.reprotox.2015.09.006
Senft D, Ronai ZA (2016) Regulators of mitochondrial dynamics in cancer. Curr Opin Cell Biol 39:43–52. https://doi.org/10.1016/j.ceb.2016.02.001
Shafei A, Matbouly M, Mostafa E et al (2018) Stop eating plastic, molecular signaling of bisphenol A in breast cancer. Environ Sci Pollut Res 25:23624–23630. https://doi.org/10.1007/s11356-018-2540-y
Shirani M, Alizadeh S, Mahdavinia M, Dehghani MA (2019) The ameliorative effect of quercetin on bisphenol A-induced toxicity in mitochondria isolated from rats. Environ Sci Pollut Res 26:7688–7696. https://doi.org/10.1007/s11356-018-04119-5
Singh G, Pachouri UC, Khaidem DC et al (2015a) Mitochondrial DNA damage and diseases. F1000Research 4:176. https://doi.org/10.12688/f1000research.6665.1
Singh RP, Shafeeque CM, Sharma SK et al (2015b) Bisphenol A reduces fertilizing ability and motility by compromising mitochondrial function of sperm. Environ Toxicol Chem 34:1617–1622. https://doi.org/10.1002/etc.2957
Song L, Xia W, Zhou Z et al (2012) Low-level phenolic estrogen pollutants impair islet morphology and β-cell function in isolated rat islets. J Endocrinol 215:303–311. https://doi.org/10.1530/JOE-12-0219
Song H, Zhang T, Yang P et al (2015) Low doses of bisphenol A stimulate the proliferation of breast cancer cells via ERK1/2/ERRγ signals. Toxicol In Vitro 30:521–528. https://doi.org/10.1016/j.tiv.2015.09.009
Srivastava S, Gupta P (2018) Alteration in apoptotic rate of testicular cells and sperms following administration of bisphenol A (BPA) in Wistar albino rats. Environ Sci Pollut Res 25:21635–21643. https://doi.org/10.1007/s11356-018-2229-2
Suthar H, Verma RJ, Patel S, Jasrai YT (2014) Green tea potentially ameliorates bisphenol A-induced oxidative stress: an in vitro and in silico study. Biochem Res Int 2014:1–9. https://doi.org/10.1155/2014/259763
Tian M, Xia P, Gou X et al (2022) CRISPR screen identified that UGT1A9 was required for bisphenols-induced mitochondria dyshomeostasis. Environ Res 205:112427. https://doi.org/10.1016/j.envres.2021.112427
Tiwari D, Kamble J, Chilgunde S et al (2012) Clastogenic and mutagenic effects of bisphenol A: an endocrine disruptor. Mutat Res Toxicol Environ Mutagen 743:83–90. https://doi.org/10.1016/j.mrgentox.2011.12.023
Tsou T-C, Yeh S-C, Hsu J-W, Tsai F-Y (2017) Estrogenic chemicals at body burden levels attenuate energy metabolism in 3T3-L1 adipocytes. J Appl Toxicol 37:1537–1546. https://doi.org/10.1002/jat.3508
Um J-H, Yun J (2017) Emerging role of mitophagy in human diseases and physiology. BMB Rep 50:299–307. https://doi.org/10.5483/BMBRep.2017.50.6.056
Urriola-Muñoz P, Lagos-Cabré R, Patiño-García D et al (2018) Bisphenol-A and nonylphenol induce apoptosis in reproductive tract cancer cell lines by the activation of ADAM17. Int J Mol Sci 19:2238. https://doi.org/10.3390/ijms19082238
Ursini F, Maiorino M, Forman HJ (2016) Redox homeostasis: the Golden Mean of healthy living. Redox Biol 8:205–215. https://doi.org/10.1016/j.redox.2016.01.010
USEPA (2012) http://www.epa.gov/iris/index.html
Vahdati Hassani F, Mehri S, Abnous K et al (2017) Protective effect of crocin on BPA-induced liver toxicity in rats through inhibition of oxidative stress and downregulation of MAPK and MAPKAP signaling pathway and miRNA-122 expression. Food Chem Toxicol 107:395–405. https://doi.org/10.1016/j.fct.2017.07.007
Valentino R, D’Esposito V, Ariemma F et al (2016) Bisphenol A environmental exposure and the detrimental effects on human metabolic health: is it necessary to revise the risk assessment in vulnerable population? J Endocrinol Investig 39:259–263. https://doi.org/10.1007/s40618-015-0336-1
Valokola MG, Karimi G, Razavi BM et al (2019) The protective activity of nanomicelle curcumin in bisphenol A-induced cardiotoxicity following subacute exposure in rats. Environ Toxicol 34:319–329. https://doi.org/10.1002/tox.22687
Vantaggiato C, Castelli M, Giovarelli M et al (2019) The fine tuning of Drp1-dependent mitochondrial remodeling and autophagy controls neuronal differentiation. Front Cell Neurosci. https://doi.org/10.3389/fncel.2019.00120
Villar-Pazos S, Martinez-Pinna J, Castellano-Muñoz M et al (2017) Molecular mechanisms involved in the non-monotonic effect of bisphenol-a on Ca2+ entry in mouse pancreatic β-cells. Sci Rep 7:11770. https://doi.org/10.1038/s41598-017-11995-3
Wacquier B, Combettes L, Van Nhieu GT, Dupont G (2016) Interplay between intracellular Ca2+ oscillations and Ca2+-stimulated mitochondrial metabolism. Sci Rep 6:19316. https://doi.org/10.1038/srep19316
Wang Q, Zhao X-F, Ji Y-L et al (2010) Mitochondrial signaling pathway is also involved in bisphenol A induced germ cell apoptosis in testes. Toxicol Lett 199:129–135. https://doi.org/10.1016/j.toxlet.2010.08.014
Wang P, Luo C, Li Q et al (2014) Mitochondrion-mediated apoptosis is involved in reproductive damage caused by BPA in male rats. Environ Toxicol Pharmacol 38:1025–1033. https://doi.org/10.1016/j.etap.2014.10.018
Wang J, Chen C, Jiang Z et al (2016) Protective effect of Cordyceps militaris extract against bisphenol A induced reproductive damage. Syst Biol Reprod Med 62:249–257. https://doi.org/10.1080/19396368.2016.1182234
Wang Z, Liu H, Liu S (2017) Low-dose bisphenol A exposure: a seemingly instigating carcinogenic effect on breast cancer. Adv Sci 4:1600248. https://doi.org/10.1002/advs.201600248
Wang H, Chang L, Aguilar JS et al (2019a) Bisphenol-A exposure induced neurotoxicity in glutamatergic neurons derived from human embryonic stem cells. Environ Int 127:324–332. https://doi.org/10.1016/j.envint.2019.01.059
Wang K, Zhao Z, Ji W (2019b) Bisphenol A induces apoptosis, oxidative stress and inflammatory response in colon and liver of mice in a mitochondria-dependent manner. Biomed Pharmacother 117:109182. https://doi.org/10.1016/j.biopha.2019.109182
Wang C, He J, Xu T et al (2021) Bisphenol A (BPA), BPS and BPB-induced oxidative stress and apoptosis mediated by mitochondria in human neuroblastoma cell lines. Ecotoxicol Environ Saf 207:111299. https://doi.org/10.1016/j.ecoenv.2020.111299
Wei J, Lin Y, Li Y et al (2011) Perinatal exposure to bisphenol A at reference dose predisposes offspring to metabolic syndrome in adult rats on a high-fat diet. Endocrinology 152:3049–3061. https://doi.org/10.1210/en.2011-0045
Wei Y, Li S, Han C et al (2019) Cuscuta chinensis flavonoids alleviate bisphenol A-induced apoptosis of testicular cells in male mice offspring. Andrologia. https://doi.org/10.1111/and.13427
Wu H-J, Liu C, Duan W-X et al (2013) Melatonin ameliorates bisphenol A-induced DNA damage in the germ cells of adult male rats. Mutat Res Toxicol Environ Mutagen 752:57–67. https://doi.org/10.1016/j.mrgentox.2013.01.005
Xin F, Jiang L, Liu X et al (2014) Bisphenol A induces oxidative stress-associated DNA damage in INS-1 cells. Mutat Res Toxicol Environ Mutagen 769:29–33. https://doi.org/10.1016/j.mrgentox.2014.04.019
Xu X, Hong X, Xie L et al (2012) Gestational and lactational exposure to bisphenol-A affects anxiety- and depression-like behaviors in mice. Horm Behav 62:480–490. https://doi.org/10.1016/j.yhbeh.2012.08.005
Yousaf B, Amina LG et al (2016) Bisphenol A exposure and healing effects of Adiantum capillus-veneris L. plant extract (APE) in bisphenol A-induced reproductive toxicity in albino rats. Environ Sci Pollut Res 23:11645–11657. https://doi.org/10.1007/s11356-016-6330-0
Zhao Z, Qu W, Wang K et al (2019) Bisphenol A inhibits mucin 2 secretion in intestinal goblet cells through mitochondrial dysfunction and oxidative stress. Biomed Pharmacother 111:901–908. https://doi.org/10.1016/j.biopha.2019.01.007
Zorov DB, Juhaszova M, Sollott SJ (2014) Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol Rev 94:909–950. https://doi.org/10.1152/physrev.00026.2013
Zorova LD, Popkov VA, Plotnikov EY et al (2018) Mitochondrial membrane potential. Anal Biochem 552:50–59. https://doi.org/10.1016/j.ab.2017.07.009
Zorzano A, Claret M (2015) Implications of mitochondrial dynamics on neurodegeneration and on hypothalamic dysfunction. Front Aging Neurosci. https://doi.org/10.3389/fnagi.2015.00101
Acknowledgements
We thank ICMR-Senior Research fellowship (Reference ID-2019/4115/CMB/BMS), Government of India, the Directorate of Minorities Fellowship (DOM/FELLOWSHIP/CR-10/2019-20), Government of Karnataka, and Dr. TMA Pai Structured Ph.D. fellowship, Manipal Academy of Higher Education (MAHE) for financial assistance. We acknowledge the Centre for DNA repair and Genome Stability (CDRGS), MAHE, Manipal, Karnataka.
Funding
Open access funding provided by Manipal Academy of Higher Education, Manipal. No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical Approval
Not applicable.
Consent for Publication
The authors have approved the final draft of the manuscript.
Consent for Participation
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nayak, D., Adiga, D., Khan, N.G. et al. Impact of Bisphenol A on Structure and Function of Mitochondria: A Critical Review. Reviews Env.Contamination (formerly:Residue Reviews) 260, 10 (2022). https://doi.org/10.1007/s44169-022-00011-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44169-022-00011-z