Abstract
Bio-responsive nanocomposites with facile fabrication and rational design are of great importance in the diagnosis and treatment of cancer. Herein, the combination of bioimaging due to the presence of QD and controlled drug delivery via nanogel was employed for cancer treatment. To this aim, we fabricated a traceable and bioresponsive fluorescent active nanogel composite by integrating creatinine-functionalized carbon dots (QD) into a lecithin-inulin nanogel. Subsequently, PEGylation and integration of herceptin on the nanogel were carried out to improve the biofate and its ability to target HER2-positive breast cancer. The assessment of cellular uptake demonstrated that this nanogel was effectively internalized by SK-BR-3 cells and the production of reactive oxygen species was significantly boosted. Moreover, the nanogel composite led to high expression of P53 and Bax genes along with a low expression of Bcl-2 gene (as promotors of the apoptosis signaling pathway). The cellular uptake of herceptin was enhanced. It led to inhibiting the proliferation of the breast cancer cells as well as the reduction of viability of SK-BR-3 cancer cells (HER-2 positive) compared with MDA-MB-231 cells (triple-negative). The intraperitoneal injection of the developed formulation to MCF-7 breast cancer cell-bearing BALB/c mice supported the observation of tumor growth inhibition. Overall, herceptin-adorned PEGylated lecithin-inulin nanogel composite can be a promising theranostic candidate for targeting HER-2-positive breast cancer.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cancer is one of the leading causes of death worldwide with its most common types including lung, colon, prostate, and breast cancer [1,2,3,4,5]. To address this, a variety of adjuvant therapies such as hormone/radiation/chemotherapy and immunotherapy or targeted therapy have entered the medical field [10, 11]. A key part of cancer treatment is reducing the risk of relapse as well as clearing the body of cancer cells left in the body. Beyond therapy, an early cancer diagnosis is momentous to solicit the best treatment or apropos treatment to save lives [6,7,8,9].
Herceptin is a human monoclonal antibody to HER-2 (human epidermal growth factor receptor 2) and is currently used for the treatment of metastatic HER2-positive breast cancer in clinical [12,13,14]. The patients with metastatic HER2-positive breast cancer showed HER2/neu high protein overexpression and greater survival rates by receiving herceptin. Compared with those receiving chemotherapy alone, the patients receiving both chemotherapy and herceptin show a lower disease progression. Moreover, the latter has a higher response rate and a longer response time to the implemented therapy [12]. It is worth noting that the positive function of herceptin is more pronounced in cases that are in the early stages of breast cancer metastasis. The mechanism of action of herceptin remains unknown but it is associated with the cell cycle inhibition process [13]. After binding to HER-2 at the cellular level of HER2-positive breast cancer cell lines, herceptin induces apoptosis or prevents cell cycle progression. For this reason, in order to evaluate the condition of a patient with metastatic breast cancer, the HER-2 test is performed first, and in the next stage, after diagnosis of HER-2 positive breast cancer, herceptin is considered one of the common treatment options for metastatic breast cancer [15, 16].
Besides using herceptin for cancer treatment, nanoparticles and quantum dots (QDs) with sophisticated functions led to the evolution and upgrade of bio-imaging systems and diagnostic applications [17]. For this, carbon dots (CDs) have attracted significant interest as an alternative to heavy metal-based QDs because of their high biocompatibility [18,19,20]. CDs, which are also popularly known as carbon quantum dots (CQDs) or graphene quantum dots (GQDs), are zero-dimensional carbon nanomaterials that are extensively applied in biomedicine. Key advantages of the application of CDs in clinical studies are their photobleaching resistance, low toxicity, hydrophilic surface, easy passivation, good cellular compatibility, and chemical stability. Thanks to the combination of these key properties of CDs, with nanogel to fabricate nanocomposites targeted for bioimaging and responsive drug delivery to enhance the therapeutic efficacy [17]. Such nanogel composites have great potential for disease diagnosis and imaging-guided cancer therapy since fluorescent imaging not only precisely monitors the change of biosignal in vitro and in vivo, but also identifies the location of the tumor region and monitors the treatment progress [18, 19].
Current therapeutic approaches such as herceptin usually lead to excessive damage to normal cells owing to their inherent cytotoxic side effects of them. Besides, conjugated antibodies by nanoparticles can deliver the drug in a controlled manner, enhancing cancerous cell death [20]. With regard to all of the above reasons and based on the effective application of herceptin in treating HER-2-positive cancers and CDs in bioimaging, herein, we report a nano-sized, traceable, and bioresponsive lecithin-inulin-CDs nanogel composite (LI-NG-CDs) for specific bioimaging and targeted intracellular delivery of drugs to SK-BR-3 human breast cancer cells with high expression of HER-2 (Fig. 1). For the synthesis of CDs, a straightforward one-step refluxing process was performed by adjusting the acid content in the precursor solution of creatinine. Lecithin-inulin nanocomposites (LI-NG) were fabricated from creatinine-based carbon dots encapsulated with lecithin-inulin by employing a simple strategy. Subsequently, the nanocomposites were functionalized by poly (ethylene glycol) (PEG, widely used in FDA-approved biomaterials) to conjugate herceptin. The nanogel was systematically characterized by XRD, FE-SEM, TEM, DLS, Zeta potential, and EDX analysis, followed by in vivo and in vitro evaluation of the effectiveness of the fluorescent nanogel in bioimaging and treatment of HER-2-positive breast cancer.
A One-pot synthesis of amine-coated carbon dots (CDs). B Fabrication of herceptin-integrated lecithin-inulin-CDs nanogel composite (Her-LI-NG-CDs). C A schematic illustration of lecithin-inulin-CDs (LI-NG-CDs) for targeting SK-BR-3 human breast cancer cell intracellular delivery of therapeutic HER-2. PVA: polyvinyl alcohol; PEG: Poly (ethylene glycol)
2 Materials and methods
2.1 Synthesis of carbon dots
CDs were prepared by a hydrothermal refluxing method as follows. Precursor materials containing 20 mL creatinine 0.2 mol L−1 and acetic acid 2.5 mol L−1 were refluxed at 80 °C with constant vigorous stirring for 12 h. During reflux processing, the solution color converted from colorless to yellow, indicating the formation of CDs. The obtained product was cooled to room temperature and centrifuged at 10,000 rpm (~ 11,200 relative centrifugal force (RCF)) for 15 min to eliminate large-size particles. The pH value of the CDs solution was adjusted by concentrated sodium hydroxide solution and monitored by a pH meter. The optimal conditions of CDs synthesis were analyzed by experimental design as follows.
2.2 Nanogel composite preparation and PEGylation
The fabrication of inulin and CDs loaded into lecithin nanogel (LI-NG-CDs) via a modified water-in-oil (W/O) nanoemulsion technique was performed as follows. First, lecithin was selected as an oil phase and dissolved with different concentrations in a solution consisting of DMF and chloroform (7:3 ratio) while stirring at 200 rpm (~ 4 RCF) on a hot plate (50 °C). The water phase was concurrently prepared by adding 0.2 mL of pre-synthesized CDs into 0.02 g mL−1 inulin and 0.1 g mL−1 PVA while stirring at 100 rpm (~ 1 RCF) to mix homogeneously. Second, the nanogel was prepared via the addition of 20 µL of water phase into the oil phase. The whole mixture was stirred at a constant speed and temperature (100 rpm, 50 °C) for 10 min to generate the (W/O) nanoemulsion.
To prepare the PEGylated LI-NG-CDs, poly (ethylene glycol) diamine (150 µL, 10−3 gmL−1) was dropwise added by maintaining the conditions and stirring for 20 min. The nanoemulsion was centrifuged at 10,000 rpm (~ 11,200 RCF) for 10 min, and then the supernatant was removed and the resultant PEGylated LI-NG-CDs nanogel was settled down and washed with acetone to remove the superficial lecithin or unreacted reactants. The concentration of nanogel composite was obtained by a flourimetry technique, in which the sediment of PEGylated LI-NG-CDs was re-dispersed in 5 mL of PBS and the concentration was calculated by weighing the sediment sample from a certain volume of solution (200 mg mL−1).
2.3 Herceptin-integrated nanogel
To prepare herceptin-integrated nanogel (Her-LI-NG-CDs), 150 μL of glutaraldehyde was added to 1 ml of prepared nanogel in the previous step with very slow stirring, followed by a rest period of 5 min. Finally, 15 µL of herceptin (45 mg ml−1) was added to the nanogel to complete the conjugation process.
2.4 Instrument
UV–vis absorption spectra were recorded by a Jenway spectrophotometer model 6705 (UK). Fluorescence spectra were recorded by a fluorescence spectrophotometer F-2700-Hitachi (Japan) equipped with a xenon lamp source. pH adjustment was performed using a digital pH-Meter model 632 (Metrohm, Herisau, Switzerland). Transmission electron microscopy (TEM) images were taken by a transmission electron microscope (Zeiss-EM10C-80 kV, Germany). Field-emission scanning electron microscope (FE-SEM) images were taken by field emission scanning electron microscope S-4160-Hitachi. Energy-dispersive X-ray analysis (EDX, Zeiss-EM10C-80 kV, Germany) was performed using a Zeiss-EM10C-80 kV, (Germany). FTIR spectra were recorded by a Bomem 102 FT-IR spectrometer (Canada) in the frequency region of 400 to 4000 cm−1. The Olympus IX71 inverted microscope fluorescence (Japan) was used to take fluorescence microscope images, ELIZA Reader (Biorad) was used to read the results of MTT, and Eppendorf centrifuge (Germany) was used for the other assay of cell culture.
Other methodologies and experiments are provided in the supporting information.
3 Results and discussion
3.1 Fabrication and characterizations
Fabrication of the nanogel nanocomposite materials by integrating CDs into polymer matrices through intermolecular interactions or covalent bonding is a feasible pathway. Properly selected polymer matrices can play a crucial role in dispersedly anchoring CDs to effectively avoid the aggregation-induced photoluminescence self-quenching of CDs. Furthermore, the unique features of CDs can grant polymers with other potential capabilities including promoted mechanical strength, excellent fluorescence performance, ionic conductivity, bioactivity, and stimuli-responsive characteristics. On the other hand, polyethylene glycol (PEG) was approved by Food and Drug Administration (FDA) for pharmaceutical applications. It has been utilized as an adjuvant material in drug delivery for many years due to its versatility and safety. Therefore, PEGylation is a favorable choice to elevate the physiochemical characteristics and improve the biofate and ability to target HER2-positive breast cancer. In this research work, we designed a PEGylated lecithin-inulin-CDs nanogel composite as a nanocarrier for targeted Herceptin delivery and potential applications for bioimaging of breast cancer tumors.
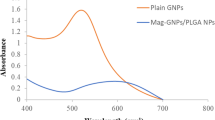
The UV − vis and fluorescence spectrum can illustrate the unique optical properties of CDs and the developed nanogel. The UV − vis absorption spectrum of CDs (Fig. 2A) indicated a characteristic peak at 390 nm, corresponding to π → π* and n → π* transitions of the interaction of C = O, C = N, and N–H. The fluorescent properties of the synthesized CDs were also investigated under different excitation wavelengths. As seen in Fig. 2B, the emission intensities decreased gradually (it was illustrated in redshift) with increasing excitation wavelength from 340 to 380 nm (excitation and emission slit widths 2.5 nm). These results reveal the excitation-dependent property of CDs (same as the prepared CDs from a natural source) and their quantum confinement effect [21, 22]. As well, the aqueous solution of CDs possesses light yellow color under daylight and bright blue luminescence color under UV light (inset of Fig. 2B).
A The UV − vis spectra of CDs and the prepared nanogel. B The emission fluorescence spectra of CDs at diverse excitation wavelengths from 340 to 380 nm along with the photo of its bright blue luminescence color under UV light (inset of Fig. 2B). C The fluorescence spectrum of lecithin-inulin-carbon dots (LI-NG-CDs) (inset of Fig. 2A: The emission spectra of synthesized CDs). D The FT-IR spectra of (a) CDs, (b) LI-NG-CDs, (c) PEGylated LI-NG-CDs, and (d) herceptin-integrated lecithin-inulin-carbon dots nanogel composite (Her-LI-NG-CDs)
In addition, the fluorescence spectrum of the synthesized CDs exhibited the strongest emission peak at 400 nm with λExi = 360 nm (Fig. 2C). FT-IR was performed to characterize the LI-NG-CDs (a), PEGylated LI-NG-CDs (b), and PEGylated LI-NG-CDs after the addition of glutaraldehyde as a mediated cross-linkinger for coupling of antibodies (c) and Her-LI-NG-CDs (d) (Fig. 2D). The peaks present in the range of 3430–3409 cm−1 are related to the stretching vibrations of the O − H and N − H groups [23, 24]. The small peaks at approximately 1240 cm−1, 1146 cm−1, and 1099 cm−1 are assigned to C–O–C stretching vibrations [23]. All spectra show almost identical peaks at nearby 1720 cm−1 and 1160 cm−1, which correspond to the C = O and C–O stretching of lecithin. The C-H stretching bending modes and symmetric and asymmetric stretching modes of C − O − C bonds were observed at 1386 cm−1, 1200 cm−1, and 1300 cm−1, respectively [25]. The phosphine oxide stretching of lecithin was also found at 1100 cm−1[26]. Two additional peaks at approximately 1649 cm−1 and 1549 cm−1 were assigned to the stretching vibration of C = O functional groups and N–H stretching of amide groups [25], which are enhanced due to the interaction of lecithin-PEG and PEG-herceptin, respectively.
The XRD patterns of all of the as-synthesized CDs, LI-NG-CDs, and PEGylated LI-NG-CDs within the range from 2θ = 5 to 80° can be seen in Fig. 3A [27]. The CDs with nitrogen precursor (such as melamine source) possess a graphitic carbon nitride phase in their XRD pattern [28]. Since the synthetic CDs in this research also have a nitrogen source (viz., creatinine), the presence of graphitic carbon nitride quantum dots phases is not unexpected, as proven by XRD. The broad diffraction peak near 25°, corresponding to the (002) crystallographic plane of graphite, indicated the graphitic structure of the carbon materials (JCPDS Card 13–0148) as also shown in the XRD pattern [29]. Moreover, several distinct peaks around 2θ = 30.4, 31.5, and 51.8° can be attributed to the graphitic carbon nitride (g-C3N4) phase [30]. Some additional new peaks that arise at 2θ = 46, 54, and 75° may be due to other intermediate products formed during the CDs preparations. The hydrothermal refluxing techniques generate carbon nuclei that convert to CDs. Hence, their characteristic d-spacing is similar to various graphene XRD patterns. Carbon-rich sources can generate highly crystalline CDs products that are parallel to the lattice plates after the anisotropic growth of carbonization [31, 32]. As a result, the CDs preparation was confirmed by XRD analysis. As shown in Fig. 3A, the XRD pattern of PEGylated LI-NG-CDs illustrates a broad peak before 2θ = 20° which demonstrates an amorphous structure.
The zeta potential of CDs, NG, PEGylated-NG, and Her-LI-NG-CDs are shown in Fig. 3B, the positive zeta potential of CDs is probably owing to imide, amine, and carbonyl functional groups existing on the CDs surface. The zeta potential of NG decreased from −6.88 mV to −33.5 mV. The PEGylating process increased the zeta potential from −33.5 mV to −19.1 mV. The higher degree of hydrophilicity of PEG-NG and lower zeta potential is responsible for decreased van der Waals interactions with cytoplasmic ingredients [33]. The zeta potential of PEGylated-NG is decreased in the presence of herceptin. The results make the conditions suitable for biological studies.
The nano-emulsification technique allowed the obtainment of a stable drug delivery system via the suitable contact between oil/water phases, preventing the coalescence of water droplets and reducing the droplet size of the nano-emulsion [34]. In this regard, it was necessary to confirm the morphology and structure of the construct, the FE-SEM images of LI-NG-CDs, and PEGylated LI-NG-CDs presented in Fig. 3C. PEG is surface conjugated to the lipoid polymer distearoyl phosphatidylethanolamine (DSPE) and also firmly attached to the lipid membrane such as Lecithin [34]. Hence, the size of the nanogel increased after PEGylating, which further confirms the PEGylation process. Moreover, to quantify and analyze the component composition of NG before and after PEGlation, the elemental distribution has been mapped using EDX (Figure S2), in which the results indicate the signals of C, O, P, and N that are uniformly spread over the whole cross-sections of nanogel. The weight and atomic percentages of elements were also specified in it.
The dynamic light scattering (DLS) of CDs, LI-NG-CDs, PEGylated LI-NG-CDs, and Her-LI-NG-CDs are illustrated in Fig. 4A. Regarding the particle size results of CDs obtained by DLS, most of the prepared CDs have a diameter of less than 10 nm, confirming TEM analysis (~ 8 nm). The TEM image of water-soluble CDs presents a uniform spherical shape and a favorable dispersion of the nanosystem (Fig. 4B). Also, TEM analysis of LI-NG-CDs illustrates well embedding of CDs into the nanogel. The hydrophobic PEG segment tends to constitute the outer shell of the nanogel, while the hydrophilic PEG segment arranges toward the core through hydrophilic interactions, which is depicted in the TEM image of PEGylated LI-NG-CDs (Fig. 4B). The TEM image shows that the PEGylated LI-NG-CDs possess a size of ~ 145 nm in diameter.
The materials’ volumes or concentration ratios used in each step of nanogel preparation may change the fine-tuned NG diameter, surface charge (and therefore the zeta potential), and fluorescence features. All of the stated parameters, especially the emission features, are of crucial importance for the biological tracing of the present research. By comparing the emission intensity of LI-NG-CDs with CDs, it was found that the fluorescence intensity of CDs encapsulated in LI-NG is higher than CDs (Fig. 5A). All stages of nanogel preparation were monitored by fluorescence signals and the optimum values were selected based on the best emission intensity responses throughout the experimental procedure. Different volumes (5–150 µL) of poly (ethylene glycol) diamine with a concentration of 10−3 g mL−1 were taken and added to the LI-NG-CDs, according to the protocol described in Section 2.3. Then, their fluorescence responses were monitored and a value (viz. 150 µL) with the least change in the fluorescence intensity of LI-NG-CDs was selected as the optimal condition (Fig. 5B). Based on the output signals of fluorescence, as evident in the recorded spectra in Fig. 5C, the values of 150 μL of glutaraldehyde and 15 µL of herceptin (45 mg ml−1) (Fig. 5D) were selected as optimal values for the synthesis of Her-LI-NG-CDs.
A Size distribution histograms carbon dots (CDs), lecithin-inulin-CDs (LI-NG-CDs), PEGylated LI-NG-CDs, and herceptin-integrated lecithin-inulin-carbon dots nanogel composite (Her-LI-NG-CDs) obtained through dynamic light scattering measurements and B corresponding TEM images of synthesized CDs, LI-NG-CDs, and PEGylated LI-NG-CDs
3.2 Cell viability assay
The morphology of cultured SK-BR-3 and MDA-MB-231 cells in a complete medium is shown in Fig. 6A. Both cell lines indicated an epithelial morphology in culture. The inhibitory effects of nanogel, free herceptin, and Her-LI-NG-CDs on SK-BR-3 and MDA-MB-231 cells were investigated. The results revealed that different concentrations of the nanogel (50, 150, 250, 350, and 450 µgmL−1) possess no toxic effect on the survival rate of SK-BR-3 and MDA-MB-231 cells. These cell lines displayed the highest cell viability after exposure to the nanogel (Fig. 6B). Similarly, different concentrations of herceptin and Her-LI-NG-CDs showed no cytotoxicity against MDA-MB-231 cells (Fig. 6C). This is due to a lack of the growth factor receptor (HER-2) in these cell lines [35]. On the opposite, Her and Her-LI-NG-CDs exhibited toxic effects against SK-BR3 cells. Among free and encapsulated herceptin, it was found that at similar concentrations (i.e., 5, 10, 15, 20, and 30 µg/mL), Her-LI-NG-CDs treated SK-BR-3 cells exhibited lower cell viability than those treated with free herceptin (Fig. 6D). Compared to herceptin-treated cells, low concentrations (5 and 10 µg/mL) of Her-LI-NG-CDs considerably reduced the viability of SK-BR3 cells due to the high levels of expression of HER2, leading to more cell death. This higher toxicity suggests that the integration of herceptin into the nanogel can effectively increase cellular targeting and uptake efficiency for receptor binding and killing SK-BR-3 cells. To further compare the toxic effects of herceptin and nanogel, the dose of 15 µgmL−1 was used in the MTT assay.
A The recorded fluorescence spectra for the synthesis of Her-LI-NG-CDs at λExi = 360 nm. B The Effect of various volumes (5–150 µL) of poly (ethylene glycol) diamine with a concentration of 10−3 g mL−1 on the fluorescence intensity of LI-NG-CDs. C The effect of different volumes (10–200 µL) of glutaraldehyde on the fluorescence intensity of LI-NG-CDs. D The effect of different volumes (5–15 µL) of herceptin (45 mg ml−1) on the synthesis of Her-LI-NG-CDs
3.3 Cellular uptake
Investigation of cellular uptake plays a key role in cancer therapy. It is due to the drug’s competency in the target cells via internalization [36]. Fluorescence microscopy was utilized to visualize the uptake of Her-LI-NG-CDs into SK-BR-3 cells. No fluorescence light was emitted in untreated and Her-treated SK-BR-3 cells. In contrast, SK-BR-3 cells treated with Her-LI-NG-CDs emitted green fluorescence due to the presence of CDs (Fig. 7). According to the merged images of DAPI-stained SK-BR-3 cells, the Her-carrying nanogel could effectively be transported into SK-BR-3 cells after 24 h of incubation. It is known that nanogel can promote the effective delivery of therapeutic agents and enhance their bioavailability in cells [37]. These results demonstrated that the nanogel effectively enhanced the cellular uptake of herceptin and may cause an increase in herceptin attachment degree to HER-2 receptors on the SK-BR-3 cells’ surface through active targeting. Furthermore, PEGylation of nanogel can contribute to the enhancement of the internalization of herceptin into the cells through receptor-mediated endocytosis. According to previous research with murine pancreatic cancer Pan 02 cells, it seems that the cellular uptake of PEGylated nanogel can be effectively increased compared to nanogel without PEGylation. In addition, PEGylation nanogel can reduce the growth of Pan 02 cells [38]. In fact, PEGylation leads to the prolonged blood circulation of conjugated nanogel [39]. PEGylation has been widely applied in nanoparticles-based systems to increase surface hydrophilicity; thereby ameliorating circulation half-life via decreasing their interactions with blood proteins and/or cells. as well, this process can envelop the surface of nanogel/nanoparticles from aggregating, and phagocytosis, hence prolonged systemic circulation time [40, 41]. Similarly, other researchers have shown that poly(ε-caprolactone)-co-poly(ethylene oxide) (PCL-PEG) micelles may enhance the ability of herceptin to bind to HER-2 receptors on the surface of SK-BR-3 cells [42]. Also, Han et al. reported that QDs enhanced herceptin-specific binding to HER-2 receptors on the SK-BR-3 cell’s surface and resulted in more cell death [43].
The morphology of cultured SK-BR-3 and MDA-MB-231 cells in a complete medium. A The right image shows SK-BR-3 cells and the left image shows MDA-MB-231 cells. B The cytotoxic effect of different concentrations of nanogel on SK-BR-3, and MDA-MB-231 cells for 24 h. The cytotoxic effect of different concentrations of herceptin (Her) and herceptin-integrated lecithin-inulin-carbon dots nanogel composite (Her-LI-NG-CDs) on MDA-MB-231 (C) and SK-BR-3 cells (D) for 24 h. The results are presented as means ± SD (n = 3). *** p < 0.001; * symbol shows compared to Her and Her-LI-NG-CDs. Scale bar: 100 µm
3.4 Colony assay
In normal conditions, every cancerous cell can grow and form a colony with at least 50 cells due to the rate of their high proliferation [44]. Therefore, a colony assay was used to evaluate whether the cytotoxic effects of herceptin and Her-LI-NG-CDs can inhibit the colony-forming of SK-BR-3 and MDA-MB-231 cells after 10 days. The results showed that colony-forming was significantly reduced in SK-BR-3 exposed to herceptin compared to the control cells. Moreover, it was found that the 15 µg/mL dosage of Her-LI-NG-CDs inhibited effectively the proliferation activity and the percentage of clonogenic survival of SK-BR-3 cells compared to herceptin-exposed SK-BR-3 cells (Fig. 8A, B). These findings suggest that the targeting of herceptin by the nanogel may trigger more long-term cytotoxic effects and eventually increase cell death. The binding of herceptin to overexpressed HER-2 receptors on the SK-BR-3 cells’ surface can inhibit cell proliferation by blocking the receipt of growth signals. In contrast, herceptin and Her-LI-NG-CDs had no impact on the colony formation of MDA-MB-231 cells (Fig. 8A, C). It was reported that integrated-herceptin into QDs resulted in a large decrease in cell viability and proliferation due to herceptin's inducing apoptotic death properties [43].
3.5 Cell migration assay
One of the most important processes for the development and metastasis of cancer is cell migration [45]. Thus, it is critical to investigate the inhibition of cell migration by anti-cancer agents. In this study, the effects of herceptin and Her-LI-NG-CDs on the migration ability of SK-BR-3 and MDA-MB-231 cells were assessed using the wound healing assay. Figure 8D, E shows the formed wounds and the progression of healing at 0 h and 24 h in SK-BR-3 and MDA-MB-231 cells, respectively. According to Fig. 8D, untreated SK-BR-3 cells completely migrated to each other 24 h after wound, while the herceptin-treated SK-BR-3 cells showed a reduction in the size and percentage of wound closure after 24 h compared to 0 h. Moreover, the obtained results showed that Her-LI-NG-CDs had a considerable inhibitory effect on the migration of SK-BR-3 cells in comparison with both the control and free herceptin after 24 h (Fig. 8F). This evidence suggests the advantageous use of the nanogel in herceptin targeting, thereby increasing the efficacy of herceptin against SK-BR-3 cells and leading to the inhibition of migration of cells.
In contrast, owing to the feature of triple-negative breast cancer and lack of response to herceptin by MDA-MB-231 cells, the treatment of MDA-MB-231 cells with herceptin and Her-LI-NG-CDs exhibited no effect on cell migration after 24 h. The percentage of wound closure in these cells was similar to the control group, as can be seen in Fig. 8G).
3.6 Cytotoxicity assay
Apoptosis is one of the key mechanisms of cell death induced by anti-cancer agents [46]. AO/EB assay was used to investigate apoptosis as a possible mechanism of growth inhibition and death of SK-BR-3 and MDA-MB-231 cells exposed to herceptin and herceptin conjugated with nanogel. In this methodology, live cells illustrate green fluorescent brilliance due to the fact that only AO can enter these cells, while EB can only enter dead cells or cells with compromised membranes and emerge with red–orange fluorescent shine.
The results demonstrated that the percentage of apoptotic cells was negligible in the control group and the SK-BR-3 cells were normal. According to merged images, green and orange-red fluorescence was detected in SK-BR-3 cells treated with herceptin, and orange fluorescence indicated a percentage of apoptotic cells of about 33%. Her-LI-NG-CDsexposed SK-BR-3 cells demonstrated a higher percentage of apoptotic death compared to free herceptin-treated SK-BR-3 cells, which indicates a significant reduction in cell viability and more cell death when using the nanogel composite (Fig. 9A, B). Furthermore, herceptin cell uptake may lead to inducing the enhancement of apoptosis. In contrast, all MDA-MB-231 cells (that served as a negative control) emitted green fluorescence and survived after 24 h in the presence of herceptin and Her-LI-NG-CDs due to MDA-MB-231 cells lacking HER2 receptor to bind to herceptin and induce cell death (Fig. 9C).
A The colony-formation ability of SK-BR-3 and MDA-MB-231 cells exposed to herceptin (Her) and herceptin-integrated lecithin-inulin-carbon dots nanogel composite (Her-LI-NG-CDs) for 10 days. Scale bar: 100 µm. The percentage of clonogenic survival in SK-BR-3 (B) and MDA-MB-231 (C) cells. The effect of herceptin and Her-LI-NG-CDs on the cell migration inhibition of SK-BR-3 and MDA-MB-231 cells by wound healing scratch assay after 24 h. D Images indicate the wounded area at 0 h and 24 h in treated-SK-BR-3 cells. The approximate edge is colored for better visualization. The uncolored images are presented in supporting information. Scale bar: 100 µm. (E) Images indicate the wounded area at 0 h and 24 h in treated-MDA-MB-231 cells. F and G show the percentage of cell migration in SK-BR-3 and MDA-MB-231 cells, respectively. The results are presented as means ± SD (n = 3). # p < 0.05 and ***, ### p < 0.001; # and * symbols show compared to control and herceptin, respectively
3.7 Real-time polymerase chain reaction (RT-PCR)
To better explore the inducing mechanism of apoptosis in Her-LI-NG-CDs-exposed SK-BR-3 cells, mRNA expression of p53, Bax, and Bcl-2 genes was investigated using RT-PCR. Treatment of SK-BR-3 cells with herceptin considerably increased Bax expression, an apoptotic gene, while the Bcl-2 expression, an anti-apoptotic gene, significantly decreased in comparison to the control. Her-LI-NG-CDs significantly increased Bax expression in SK-BR-3 cells in comparison to the control and herceptin-treated cells. No significant differences were found in P53 expression in SK-BR-3 cells exposed to Her-LI-NG-CDs compared herceptin-treated cells (Fig. 9D). It is well known that overexpression of HER-2 suppresses apoptosis in HER-2-positive cancer cells via p53 inhibition, eventually by inhibition of pro-apoptotic genes such as Bax [47]. The obtained results confirm the induction of apoptotic death in cells and display that apoptosis may be triggered in SK-BR-3 cells when treated with Her-LI-NG-CDs by increasing Bax/Bcl-2 ratio. In contrast, no change was observed in gene expression of P53, Bax, and Bcl-2 in herceptin and Her-LI-NG-CDs-treated MDA-MB-231 cells compared to the control (Fig. 9E).
3.8 Intracellular reactive oxygen species
SK-BR-3 cells exposed to Her-LI-NG-CDs produced lower levels of reROS versus non-treated and herceptin-treated cells (Fig. 9F). According to previous studies excessive ROS can cause to promote the progression and migration of tumors; therefore, cancer cells usually elevate intracellular ROS levels compared with the types of normal cells [48,49,50]. Furthermore, some evidence demonstrates that high ROS levels can inhibit apoptosis in cancer cells and lead to cancer progression [51]. Our findings displayed that the developed nanogel effectively declined the level of ROS generation in SK-BR-3 cells compared to non-treated and herceptin-treated cells and led to the induction of apoptosis. Liou and Storz reported that ROS inhibition induces apoptotic death in pancreatic cancer cells via the reduction of phosphorylated Akt levels [52]. Also, a study by Azad et al. showed that butein resulted in the death of breast cancer cells through decreased ROS generation and increased apoptotic death [53]. Moreover, the CDs that are used for prognosis may contribute to scavenging more ROS. Additionally, Sachdev and Gopinath demonstrated that CDs possess the potential for ROS scavenging in fibroblast cells [54].
3.9 In vivo studies
The effect of LI-NG-CDs on mice beard breast cancer is shown in Fig. 10A. Two cell lines of MCF-7 and SK-BR-3 were selected [55]. MCF-7 cell line shows a less complex chromosomal pattern than SK-BR-3 cells and also based on previous studies to compare the morphological changes of the cancerous tissues, MCF-7 cells with less chromosomal complexity are better in terms of their simplicity, to be used. Based on the H&E staining-derived images and compared to the literature, the morphology of the breast tissue was not changed significantly after 24 h [56,57,58,59]. The arrays remained more than > 80% intact (based on the microscopy results), and the space between the cellular arrays showed a normal behavior (compared to the control images (Fig. 10B, C). After 72 h, the space between the cellular arrays increased at a constant slope, showing that the progression of cancerous cells was inhibited. Therefore, it could be considered that the injected developed formulation had a positive effect on controlling the progression of cancerous cells. Besides, the angiogenesis of the breast cells, compared to the literature (and also compared to the control images), exhibited similar results to the normal and healthy tissues (at different distances from the cancerous sites), which could be considered promising results [60]. Based on the literature, at different stages of breast cancer progression, the angiogenesis will be disrupted; however, in this study, the microscopy results showed that the angiogenesis was not significantly disrupted. All of these results confirmed that the prepared Her-LI-NG-CDs formulation did not provoke physical aggregations to the breast tissue (based on the surface morphological comparison), and also did not exert a negative impact on the progression of cancerous cells to different cellular sites. This means that the prepared Her-LI-NG-CDs enabled the inhibition of cancerous cells, mostly by surface interactions and inhibition of the unwanted interactions. However, besides the cellular morphology of the breast tissue showed a partial deformation (Fig. 10C) compared to the control groups (Fig. 10B), those deformations are considered normal due to no significant disruption in the angiogenesis as well as the aggregation of the cellular arrays.
The cytotoxic effect of herceptin (Her) and herceptin-integrated lecithin-inulin-carbon dots nanogel composite (Her-LI-NG-CDs) on SK-BR-3 cells for 24 h. A Live and dead cells have been shown as green and red. B The percentage of apoptotic cells in SK-BR-3 cells. C The cytotoxic effect of Her and Her-LI-NG-CDs on MDA-MB-231 cells after 24 h. Her and Her-LI-NG-CDs affect the expression of P53, Bax, and Bcl-2 genes. D The expression genes in SK-BR-3 cells. E The expression genes in MDA-MB-231 cells. F The level of measured intracellular ROS by DCFH-DA in SK-BR-3 cells exposed to Her and Her-LI-NG-CDs after 24 h. The results are presented as means ± SD (n = 3). *, # p < 0.05, ## p < 0.01, and ### p < 0.001; # and * symbols show compared to control and Her. Scale bar: 100 µm
A Schematic illustration of in vivo application’s results of herceptin-integrated lecithin-inulin-carbon dots nanogel composite (Her-LI-NG-CDs) in breast cancer therapy. B Histological images of the breast tissue as control. C Histological images to different intervals of fixation time of 24 h and 72 h from different sites of the treated tissue with Her-LI-NG-CDs. The scale bars represent 200 µm
The effect of the injected Her-LI-NG-CDs formulation on the cellular arrays of the breast cells (BALB/c mice treated with MCF-7 cells) contributes to understanding the ability of new drug delivery systems to inhibit the progression of cancerous cells. In fact, different kinds of mechanisms are involved in cancerous cell advances, and those can be particularly targeted by the developed nanosystem, which contrasts with unspecific conventional therapies, including radiotherapy and chemotherapy. All of the referred mechanisms have an indirect effect on the ROS and in this study, our Her-LI-NG-CDs have the promising ability to interact with the cellular membranes via their interaction with Her-2 receptors [61, 62].
The cellular array and its effects on cellular internalizations and also bio-cellular catalytic processes are relevant to each other, and all of these factors could be able to study with the aim of measuring in vivo biocompatibility. Investigation of those effects and their interrelationships with the injected formulation could be helpful for future experiments. In fact, the physical parameters include the size of the space between the cells, the density of the packed cells, the cellular array heterogeneity/homogeneity ratio, and also the ratio of destructed cellular sites that should be identified in future works [63,64,65,66,67]. In this work, we could be able to identify some of them, especially the destructed cellular sites and the ratio of cellular array heterogeneity/homogeneity. Based on the images, the destructed cellular sites do not follow any specific pattern; however, the ratio of cellular array heterogeneity/homogeneity is very low, which is another promising result of using these types of nanocarriers; the heterogeneity/homogeneity ratio on the cellular arrays are important to show the potential negative impact of the injected sample and/or drug. To this aim, as the cellular array remains mostly intact, therefore, the in vivo biocompatibility of the nanogel composite can be concluded.
The in vivo and in vitro performance of the LI-NG-CDs nanogel composite was compared with the other reported platforms in breast cancer therapy. For example, Jia et al., PEGylated composite nanogel based on sodium alginate and carbon dot and employed it as a carrier for doxorubicin delivery for breast cancer treatment [68]. The results showed that the combination of PEGylated nanogel with carbon dot increased the doxorubicin release and penetration in the body. The cytotoxicity of the PEGylated sodium alginate/CDs nanocomposite compared to our composite nanogel (LI-NG-CDs) was higher at low concentrations (higher than 10 μg/ml) in which the cell viability percentage was reported to be close to 40% [68]. In addition, the particle size of the PEGylated sodium alginate/CDs composite was reported 365 nm, while the particle size of our composite nanogel (LI-NG-CDs) was 100 nm [68]. It is known that reducing the particle size increases cell permeability [69]. In another recently reported study, a composite nanogel based on polypropylene acrylic acid and iron oxide magnetic nanoparticles as a carrier of herceptin drug were reported [70]. The results of the cytotoxicity test and the in vivo test of the prepared nanocomposite were higher compared to LI-NG-CDs composite, and this cytotoxicity may be due to the presence of iron (II) and iron (III) salts and divinylbenzene as a cross-linking in the structure of iron oxide nanoparticles and polymer, respectively. By comparison of the proposed research with other composite-based nanogels, it was found that the carbon dots prepared by the green method play a significant role in breast cancer treatment. Additionally, the fluorescence property of the CD nanoparticles expresses the potential application of bioimaging, which boost the performance of the composite in chemotherapy and cancer cell tracking. The process of PEGylation reduces cytotoxicity and enhances biocompatibility/permeability in the body tissue.
4 Conclusions
In summary, a novel fluorescent nanogel composite (Her-LI-NG-CDs) was prepared with CDs, polyvinyl alcohol, and inulin mixture as a core, and a lecithin hydrophobic layer with herceptin receptor on the outer shell. The average diameter of the nanogel composite was 100 nm. The in vivo and in vitro evaluation of the nanogel was performed in this study. The Her-LI-NG-CDs demonstrated cytotoxic effects on SK-BR-3 cells compared to MDA-MB-231 cells. Also, it can be effectively internalized into SK-BR-3 cells via endocytosis mediated by their over-expressed HER-2 receptors. Released herceptin in the cytoplasm of SK-BR-3 cells led to the overexpression of intracellular ROS and the induction of apoptosis via upregulation of P53, Bax genes, and downregulation of Bcl-2 gene. Therefore, the prepared Her-LI-NG-CDs possess a suitable potential for application in bioimaging and treatment of HER-2-positive breast cancer cells. In vivo results showed that the prepared nanogel could be able to control and/or inhibit the progression of cancerous cells and reduce the speed. Also, the microscopy results showed that the prepared nanogel did not have any significant aggregations to the breast cells/organ, and did not change the angiogenesis considerably.
Availability of data and materials
All data are available in the supporting information and the paper.
Change history
06 July 2023
A Correction to this paper has been published: https://doi.org/10.1007/s42114-023-00705-5
References
Bigham A, Rahimkhoei V, Abasian P et al (2022) Advances in tannic acid-incorporated biomaterials: infection treatment, regenerative medicine, cancer therapy, and biosensing J Chem Eng 432:134146
Ashrafizadeh M, Aghamiri S, Tan SC et al (2022) Nanotechnological approaches in prostate cancer therapy: integration of engineering and biology. Nano Today 45:101532
Raza F, Zafar H, Khan A, Hatami K (2022) T-cell membrane-coated nanomaterials in cancer treatment. Mater Chem Horizons 1(3):199–217
Lopes J, Lopes D, Macário-Soares A, Ferreira-Faria I, Peixoto D, Motallebi M, Mohammad I, Giram P, Pires P, Raza F (2022) Cell membrane-coated biomaterials for bone cancer-targeted diagnosis and therapy: a critical update on osteosarcoma applications. Mater Chem Horizons. https://doi.org/10.22128/mch.2022.615.1032
lian Y, Wang L, Cao J et al (2021) Recent advances on the magnetic nanoparticle–based nanocomposites for magnetic induction hyperthermia of tumor: a short review. Adv Compos Hybrid Mater 4:925–937. https://doi.org/10.1007/s42114-021-00373-3
Moghaddam FD, Heidari G, Zare EN, et al (2023) Carbohydrate polymer-based nanocomposites for breast cancer treatment. Carbohydr Polym 304:120510
Tavakoli N, Divsalar A, Haertlé T et al (2021) Milk protein-based nanodelivery systems for the cancer treatment. J Nanostructure Chem 11:483–500. https://doi.org/10.1007/s40097-021-00399-5
Wang X, Qi Y, Hu Z et al (2022) Fe3O4@PVP@DOX magnetic vortex hybrid nanostructures with magnetic-responsive heating and controlled drug delivery functions for precise medicine of cancers. Adv Compos Hybrid Mater 5:1786–1798. https://doi.org/10.1007/s42114-022-00433-2
Ashrafizadeh M, Zare EN, Rossi F et al (2022) Photoactive polymers-decorated Cu-Al layered double hydroxide hexagonal architectures: a potential non-viral vector for photothermal therapy and co-delivery of DOX/pCRISPR. Chem Eng J 448:137747
Gulla S, Lomada D, Araveti PB et al (2021) Titanium dioxide nanotubes conjugated with quercetin function as an effective anticancer agent by inducing apoptosis in melanoma cells. J Nanostructure Chem 11:721–734
Stebbing J, Copson E, O’Reilly S (2000) Herceptin (trastuzamab) in advanced breast cancer. Cancer Treat Rev 26:287–290
Kute T, Lack CM, Willingham M et al (2004) Development of Herceptin resistance in breast cancer cells. Cytom Part A J Int Soc Anal Cytol 57:86–93
Sarfjoo M, Shad A, Hassanpour M et al (2022) An overview on new anticancer drugs approved by food and drug administration: Impending economic and environmental challenges. Mater Chem Horizons 1(3):189-198.
Dabbagh Moghaddam F, Romana Bertani F (2022) Application of microfluidic platforms in cancer therapy. Mater Chem Horizons 1:69–88. https://doi.org/10.22128/mch.2022.556.1007
Moammeri A, Abbaspour K, Zafarian A et al (2022) pH-responsive, adorned nanoniosomes for codelivery of cisplatin and epirubicin: synergistic treatment of breast cancer. ACS Appl bio Mater 5:675–690
Basuthakur P, Patra CR (2021) Green-synthesized nanoparticles for fluorescence bioimaging and diagnostic applications. In: Biogenic Nanoparticles for Cancer Theranostics. Elsevier, pp 153–188
Gudimella KK, Appidi T, Wu H-F et al (2021) Sand bath assisted green synthesis of carbon dots from citrus fruit peels for free radical scavenging and cell imaging. Colloids Surfaces B Biointerfaces 197:111362
Chen W, Lin H, Wu Y et al (2022) Fluorescent probe of nitrogen-doped carbon dots derived from biomass for the sensing of MnO4− in polluted water based on inner filter effect. Adv Compos Hybrid Mater 5:2378–2386
Ni J, Huang X, Bai Y et al (2022) Resistance to aggregation-caused quenching: chitosan-based solid carbon dots for white light-emitting diode and 3D printing. Adv Compos Hybrid Mater 5:1865–1875
White BE, White MK, Adhvaryu H, Makhoul I, Nima ZA, Biris AS, Ali N (2020) Nanotechnology approaches to addressing HER2-positive breast cancer. Cancer 11:12
D’souza SL, Chettiar SS, Koduru JR, Kailasa SK (2018) Synthesis of fluorescent carbon dots using Daucus carota subsp. sativus roots for mitomycin drug delivery. Optik (Stuttg) 158:893–900
Yin B, Deng J, Peng X et al (2013) Green synthesis of carbon dots with down-and up-conversion fluorescent properties for sensitive detection of hypochlorite with a dual-readout assay. Analyst 138:6551–6557
Mahmood S, Kiong KC, Tham CS et al (2020) PEGylated lipid polymeric nanoparticle–encapsulated acyclovir for in vitro controlled release and ex vivo gut sac permeation. AAPS PharmSciTech 21:1–15
Arizmendi-Cotero D, Villanueva-Carvajal A, Gómez-Espinoza RM et al (2017) Radical scavenging activity of an inulin-gallic acid graft and its prebiotic effect on Lactobacillus acidophilus in vitro growth. J Funct Foods 29:135–142
Abedi F, Davaran S, Hekmati M et al (2021) An improved method in fabrication of smart dual-responsive nanogels for controlled release of doxorubicin and curcumin in HT-29 colon cancer cells. J Nanobiotechnology 19:1–22. https://doi.org/10.1186/s12951-020-00764-6
Matson T, Gootee J, Snider C et al (2019) Electrospun PCL, gold nanoparticles, and soy lecithin composite material for tissue engineering applications. J Biomater Appl 33:979–988
Das D, Banerjee D, Pahari D et al (2017) Defect induced tuning of photoluminescence property in graphitic carbon nitride nanosheets through synthesis conditions. J Lumin 185:155–165
Guo X, Yang J, Wei Y et al (2022) Graphitic carbon nitride quantum dots in dual-mode fluorescence switching platforms for trace analysis of Ag (I) and l-Cysteine. ACS Appl Nano Mater 5:4230–4240
Zhang G, Zhu J, Zeng W et al (2014) Tin quantum dots embedded in nitrogen-doped carbon nanofibers as excellent anode for lithium-ion batteries. Nano Energy 9:61–70
Fina F, Callear SK, Carins GM, Irvine JTS (2015) Structural investigation of graphitic carbon nitride via XRD and neutron diffraction. Chem Mater 27:2612–2618
Li C-L, Huang C-C, Periasamy AP et al (2015) Synthesis of photoluminescent carbon dots for the detection of cobalt ions. Rsc Adv 5:2285–2291
Dong Y, Pang H, Bin YH et al (2013) Carbon-based dots co-doped with nitrogen and sulfur for high quantum yield and excitation-independent emission. Angew Chemie Int Ed 52:7800–7804
Suh J, Choy K-L, Lai SK et al (2007) PEGylation of nanoparticles improves their cytoplasmic transport. Int J Nanomedicine 2:735
Sahu P, Kashaw SK, Sau S, Iyer AK (2019) Polylactide-co-glycolide-based Nanogel: Concept and Functions. In: Materials for Biomedical Engineering. Elsevier, pp 399–423
Chavez KJ, Garimella SV, Lipkowitz S (2010) Triple negative breast cancer cell lines: one tool in the search for better treatment of triple negative breast cancer. Breast Dis 32:35
Makvandi P, Kirkby M, Hutton ARJ et al (2021) Engineering microneedle patches for improved penetration: analysis, skin models and factors affecting needle insertion. Nano-Micro Lett 13:93. https://doi.org/10.1007/s40820-021-00611-9
Murphy EA, Majeti BK, Mukthavaram R et al (2011) Targeted nanogels: a versatile platform for drug delivery to tumors. Mol Cancer Ther 10:972–982
Ganta C, Shi A, Battina SK et al (2008) Combination of nanogel polyethylene glycol-polyethylenimine and 6 (hydroxymethyl)-1, 4-anthracenedione as an anticancer nanomedicine. J Nanosci Nanotechnol 8:2334–2340
Mohapatra A, Uthaman S, Park I-K (2019) Polyethylene glycol nanoparticles as promising tools for anticancer therapeutics. Polym Nanoparticles as a Promis Tool Anti-cancer Ther, Elsevier 205–231
Suk JS, Xu Q, Kim N, Hanes J, Ensign LM (2016) PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv Drug Deliv Rev 99:28–51
Perry JL, Reuter KG, Kai MP, Herlihy KP, Jones SW, Luft JC, Napier M, Bear JE, DeSimone JM (2012) PEGylated PRINT nanoparticles: the impact of PEG density on protein binding, macrophage association, biodistribution, and pharmacokinetics. Nano Lett 12(10):5304–5310
Peng J, Chen J, Xie F et al (2019) Herceptin-conjugated paclitaxel loaded PCL-PEG worm-like nanocrystal micelles for the combinatorial treatment of HER2-positive breast cancer. Biomaterials 222:119420
Han S-J, Rathinaraj P, Park S-Y et al (2014) Specific intracellular uptake of herceptin-conjugated CdSe/ZnS quantum dots into breast cancer cells. Biomed Res Int 2014:954307
Franken NAP, Rodermond HM, Stap J et al (2006) Clonogenic assay of cells in vitro. Nat Protoc 1:2315–2319
Freitas JT, Jozic I, Bedogni B (2021) Wound healing assay for melanoma cell migration. In: Melanoma. Springer, pp 65–71
Pfeffer CM, Singh ATK (2018) Apoptosis: a target for anticancer therapy. Int J Mol Sci 19:448
Carpenter RL, Lo H-W (2013) Regulation of apoptosis by HER2 in breast cancer. J Carcinog Mutagen 2013:003
Zaidieh T, Smith JR, Ball KE, An Q (2019) ROS as a novel indicator to predict anticancer drug efficacy. BMC Cancer 19:1–14. https://doi.org/10.1186/s12885-019-6438-y
Perillo B, Di Donato M, Pezone A et al (2020) ROS in cancer therapy: The bright side of the moon. Exp Mol Med 52:192–203
Reczek CR, Chandel NS (2017) The two faces of reactive oxygen species in cancer. Annu Rev Cancer Biol 1:79–98
Chen J (2014) Reactive oxygen species and drug resistance in cancer chemotherapy. Austin J Clin Pathol 1:1–7
Liou G-Y, Storz P (2010) Reactive oxygen species in cancer. Free Radic Res 44:479–496
Azad N, Rojanasakul Y, Vallyathan V (2008) Inflammation and lung cancer: roles of reactive oxygen/nitrogen species. J Toxicol Environ Heal Part B 11:1–15
Sachdev A, Gopinath P (2016) Monitoring the intracellular distribution and ROS scavenging potential of carbon dot – cerium oxide nanocomposites in fibroblast cells. ChemNanoMat 2(3):226–235. https://doi.org/10.1002/cnma.201500224
Weißenborn C, Ignatov T, Ochel HJ et al (2014) GPER functions as a tumor suppressor in triple-negative breast cancer cells. J Cancer Res Clin Oncol 140:713–723. https://doi.org/10.1007/s00432-014-1620-8
Ghader A, Ardakani AA, Ghaznavi H et al (2018) Evaluation of nonlinear optical differences between breast cancer cell lines SK-BR-3 and MCF-7; an in vitro study. Photodiagnosis Photodyn Ther 23:171–175
An Y, Li R, Zhang F, He P (2020) Magneto-mediated electrochemical sensor for simultaneous analysis of breast cancer exosomal proteins. Anal Chem 92:5404–5410
Khan A, Aljarbou AN, Khan S, Khan MA (2022) Her-2-directed systemic delivery of fatty acid synthase (FASN) siRNA with novel liposomal carrier systems in the breast cancer mouse model. J Drug Target 30(6):634–645
Niu Y, Bao L, Chen Y et al (2020) HIF2-induced long noncoding RNA RAB11B-AS1 promotes hypoxia-mediated angiogenesis and breast cancer metastasis. Cancer Res 80:964–975
Mirzaei-Parsa MJ, Najafabadi MRH, Haeri A et al (2020) Preparation, characterization, and evaluation of the anticancer activity of artemether-loaded nano-niosomes against breast cancer. Breast Cancer 27:243–251. https://doi.org/10.1007/s12282-019-01014-w
Jeon H, Huynh DTN, Baek N et al (2021) Ginsenoside-Rg2 affects cell growth via regulating ROS-mediated AMPK activation and cell cycle in MCF-7 cells. Phytomedicine 85:153549
Hoang QT, Ravichandran V, Cao TGN et al (2022) Piezoelectric Au-decorated ZnO nanorods: ultrasound-triggered generation of ROS for piezocatalytic cancer therapy. Chem Eng J 435:135039
Ilina O, Gritsenko PG, Syga S et al (2020) Cell–cell adhesion and 3D matrix confinement determine jamming transitions in breast cancer invasion. Nat Cell Biol 22:1103–1115. https://doi.org/10.1038/s41556-020-0552-6
Loyez M, Hassan EM, Lobry M et al (2020) Rapid detection of circulating breast cancer cells using a multiresonant optical fiber aptasensor with plasmonic amplification. ACS sensors 5:454–463
Ghanbari R, Khorsandi D, Zarepour A et al (2022) Ionic liquid-based sensors. Mater Chem Horizons 1:123–135. https://doi.org/10.22128/mch.2022.574.1015
Yang L, George J, Wang J (2020) Deep profiling of cellular heterogeneity by emerging single-cell proteomic technologies. Proteomics 20:1900226. https://doi.org/10.1002/pmic.201900226
Tang Z, min, Liu Y yan, Ni DL et al (2020) Biodegradable nanoprodrugs: “delivering” ROS to cancer cells for molecular dynamic therapy. Adv Mater 32:1904011. https://doi.org/10.1002/adma.201904011
Jia X, Pei M, Zhao X, Tian K, Zhou T, Liu P (2016) PEGylated oxidized alginate-DOX prodrug conjugate nanoparticles cross-linked with fluorescent carbon dots for tumor theranostics. ACS Biomater Sci Eng 2(9):1641–1648. https://doi.org/10.1021/acsbiomaterials.6b00443
Zare EN, Zheng X, Makvandi P, Gheybi H, Sartorius R, Yiu CKY, Adeli M, Wu A, Zarrabi A, Varma RS, Tay FR (2021) Nonspherical metal-based nanoarchitectures: synthesis and impact of size, shape, and composition on their biological activity. Small 17:2007073. https://doi.org/10.1002/smll.202007073
Zhang X, Wei P, Wang Z, Zhao Y, Xiao W, Bian Y, Liang D, Lin Q, Song W, Jiang W, Wang H (2022) Herceptin-conjugated DOX-Fe3O4/P(NIPAM-AA-MAPEG) nanogel system for HER2-targeted breast cancer treatment and magnetic resonance imaging. ACS Appl Mater Interfaces 14:15956–15969. https://doi.org/10.1021/acsami.1c24770
Funding
Open access funding was provided by Istituto Italiano di Tecnologia.
Author information
Authors and Affiliations
Contributions
Methodology, investigation, and writing—original draft preparation, M.G., H.A., and N.R.; supervision, project administration, and writing—review and editing, E.N.Z.; review, editing, and commenting: A.S., X.C., N.P., V.M., and P.M. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All of the animal experiments were conducted with the guidelines and ethical statements at Shahid Beheshti University of Medical Sciences, Tehran, Iran (Code: 29805).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: An error in Fig. 3A has been identified. Full information regarding the corrections made can be found in the erratum/correction for this article.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ghomi, M., Zare, E.N., Alidadi, H. et al. A multifunctional bioresponsive and fluorescent active nanogel composite for breast cancer therapy and bioimaging. Adv Compos Hybrid Mater 6, 51 (2023). https://doi.org/10.1007/s42114-022-00613-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s42114-022-00613-0