Abstract
Introduction
Obstructive sleep apnea (OSA) is often observed in subjects with interstitial lung disease (ILD). It may have a negative impact on the course of ILD, but its prognostic significance in relation to other known indicators of poor outcome is unclear.
Methods
After a detailed work-up, including overnight unattended type III polygraphy, all subjects newly diagnosed with ILDs referred to our clinics were followed-up for at least 1.5 years or until death or progression of disease [> 10% decline in forced vital capacity (FVC) below baseline]. We analyzed relationships between some prespecified variables of interest, including sleeping results, to establish parameters predictive of progressive course.
Results
Our population consisted of 46 subjects (mean age 59.6 years; males 61%); 23.9% and 41% had idiopathic pulmonary fibrosis and ILD associated with systemic diseases, respectively. Mean baseline forced vital capacity and diffusion capacity of carbon monoxide were 83% and 57% of predicted, respectively. Mean (± SE) Apnea–Hypopnea Index (AHI) was 17 (± 3) events/h. AHI in the ranges 5–14.9, 15–29.9, and ≥ 30 was recorded in 14 (31%), 6 (13%), and 9 (20%) subjects, respectively. Mean distance covered in the 6-MWG walk test (6MWT) was 302 (± 19) m and 26 subjects (57%) showed exertional oxyhemoglobin desaturation. The median follow-up was about 18 months. Multivariate logistic regression analysis showed that exertional desaturation (HR 8.2; 1.8–36.5 95% CI; p = 0.006) and AHI ≥ 30, namely the threshold of severe OSA (HR 7.5; 1.8–30.6; p = 0.005), were the only independent variables related to progressive disease course.
Conclusion
We conclude that exertional desaturation and elevated AHI had independent negative prognostic significance in our ILD population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
In accordance with previous literature data we found that that OSA was common in our population with mixed interstitial lung disease (ILD). |
It is unclear whether and how much Obstructive sleep apnea (OSA) is predictive of poor outcome with respect to other known negative prognostic indicators. |
What was learned from the study? |
We showed prospectively that exertional oxyhemoglobin desaturation during the 6-minute walk test and a high Apnea-Hypopnea Index (≥ events/hour), the parameter commonly used to define severe OSA, were independently associated with progressive disease course in our mixed ILD population. |
Introduction
Interstitial lung diseases (ILDs) are a heterogeneous family of pulmonary disorders with diffuse parenchymal fibrosing lesions classified on the basis of etiological, clinical, radiological, and histopathological findings. Idiopathic pulmonary fibrosis (IPF), the most common ILD, has a rapidly progressive course associated with increasing exertional dyspnea, reduced exercise tolerance, deteriorating quality of life, and poor prognosis [1]. Although the natural history of ILDs other than IPF varies, a significant percentage of subjects with these diseases, approximately one-third, also show rapid evolution with loss of lung function and progression of disease [2, 3]. It is important to know all the factors that can have a negative influence on outcome of subjects with IPF and ILD. The factors so far associated with poor prognosis in IPF and ILD include age [2,3,4], baseline predicted forced vital capacity (FVC) [2,3,4,5], diffusion capacity of the lung for carbon monoxide (DLco) [3, 4] and their decline over time [3,4,5], as well as distance walked in the 6-minute walk test (6MWT) [6] and exertional oxyhemoglobin desaturation during 6MWT [7].
Obstructive sleep apnea (OSA) is a highly prevalent sleep-related breathing disorder characterized by repeated episodes of partial (hypopnea) and/or complete (apnea) closure of the upper airways despite ongoing respiratory effort during sleep. Sleep poligraphy is the key examination for diagnosing OSA and grading its severity in terms of the number of apneas and hypopneas per hour of sleep [Apnea–Hypopnea Index (AHI)]. Males and older persons are prevalent among those with OSA, which is often associated with sleeping hypoxemia and poor sleep quality and quantity. If not treated, it is associated with increased morbidity. Although OSA and sleep-related hypoxemia were widely believed to be relatively uncommon and to have little clinical impact in subjects with ILD [8, 9], recent studies have found that they are common among subjects with ILD [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37]. OSA is now identified as a comorbidity in the IPF guidelines [1]. It is suggested that OSA may have a unfavorable impact on the course of IPF and ILD [25], but its role with respect to other known indicators of poor outcome is unclear.
The aim of this prospective observational study was to investigate the frequency of OSA and, above all, its prognostic significance in a group of subjects with ILD.
Methods
All adults consecutively diagnosed with ILD at our regional referral Center for Sarcoidosis and other Interstitial Lung Diseases at the Respiratory Diseases and Lung Transplant Unit, Siena, Italy, from May 2016 to May 2017 were considered as eligible for this study. ILD was diagnosed by multidisciplinary evaluation according to international guidelines [1]. Subjects were enrolled if they were clinically stable for at least 1 month prior to the scheduled appointment for the sleep study, which was scheduled within 2 (± 2) weeks of their first referral to our chest clinics, and prior to any change in baseline drug treatment, which also had to be stable for at least a month. Other exclusion criteria were: estimated life expectancy less than 6 months, recent (< 12 months) chest or upper airway surgery, concomitant congestive heart failure, severe psychiatric disorder, drug or alcohol abuse, thoracic or neuromuscular disease, chronic lung diseases other than ILD, previous lung transplant, known sleep disorders other than OSA, and treatment for OSA. Subjects were enrolled if they agreed to participate and provided written informed consent.
The following parameters were recorded at baseline: age, gender, smoking history, body mass index (BMI), medical history including previous drug treatments and duration of illness since onset of symptoms. Lung function tests were performed using a Master Screen Body plethysmography (Carefusion GmbH, Hoechberg, Germany, EU) according to ATS/ERS guidelines [38,39,40]. Diffusion capacity of the lung for carbon monoxide (DLco) was measured by the single breath method. Forced vital capacity (FVC), forced expiratory volume in the first second (FEV1), DLco, and Krogh diffusion coefficient were reported as percentage of predicted values. Arterial blood gas analysis was measured at rest in a sitting position for at least 15 min, obtaining oxygen (PaO2) and carbon dioxide (PaCO2) tensions. The 6MWT was performed according to ATS guidelines [41] monitoring heart rate and oxyhemoglobin saturation immediately before and during walking with a Rad-5 MirOXI pulse oximeter (Masimo, Irvine, CA, USA) and recording the following: starting resting and nadir oxyhemoglobin saturation, starting resting and peak heart rate, distance walked in meters, starting resting and final modified Borg scores for dyspnea and lower limbs exhaustion (the latter values are not shown). We also calculated the difference between starting and final modified Borg scores for dyspnea (ΔBss), the difference between starting and trough saturation level, and the number of subjects with exertional desaturation, defined as a significant drop (at least 4%) below baseline and a trough below 90% during the 6 MWT. Five subjects on long-term oxygen therapy performed the 6MWT using ambulatory oxygen therapy at flows from 1 to 6 lpm, as prescribed for walking at home. All subjects underwent high-resolution computed tomography (HRCT) of the chest. We evaluated composite physiology index (CPI), a surrogate for disease severity, by fitting lung function to disease extent as determined by CT [42].
Sleep data was obtained using a six-channel level III system, either Embletta (Embla Systems Medcare Flaga Hs. Medical Devices, Reykjavik, Iceland) or Somnea (Compumedics Ltd., Abbottsford, Australia) by established techniques [43,44,45]. The overnight study monitored heart rate and oxyhemoglobin saturation by pulse oximeter, snoring and airflow by nasal cannula with air pressure transducer, thoracic and abdominal respiratory effort by strain gauges, and body position by actigraphy. All signals were recorded automatically and then analyzed manually by a single experienced physician blind to the subjects’ other clinical data. Average sleep time was evaluated on the basis of a standardized self-compiled diary and confirmed by actigraphy. Apnea was defined as an absence or ≥ 90% reduction in baseline airflow for at least 10 s. Hypopnea was defined as a discernible ≥ 30% drop in airflow with respect to baseline for at least 10 s, followed by a ≥ 4% drop in oxyhemoglobin. The mean number of apnea and/or hypopnea events per hour of estimated sleep was indicated by AHI. OSA was confirmed for AHI ≥ 5 events/h. OSA severity was categorized as mild (AHI = 5–14.9), moderate (AHI = 15–29.9), and severe (AHI ≥ 30). Since central respiratory events were uncommon in all subjects (< 3% of total), we decided that apneas and hypopneas were only to obstructive events. The oxygen desaturation index (ODI4) was defined as the mean number of oxyhemoglobin desaturations ≥ 4% accompanying a respiratory event (apnea or hypopnea) per hour of estimated sleep time. We also calculated the percentage of estimated sleep time with oxyhemoglobin saturation below 90% ( CT90) and mean (smSpO2) and nadir (snSpO2) sleeping oxyhemoglobin saturation values. Five subjects were on long-term oxygen therapy and were given oxygen via nasal prongs at the usual flow rates: 1 lpm (two subjects), 2 lpm (one subject), and 4 lpm (two subjects) during the sleep study.
The subjects were followed up for at least 1.5 years or until death or disease progression (defined as a > 10% drop in FVC below baseline whichever came first). This reduction in FVC is often used to assess disease progression in subjects with IPF [46]. Follow-ups were performed every 3 months on average until death or disease progression, as defined.
The study was approved by the institutional ethics board of the university hospital (CEAVSE, Tuscany, Italy, OSS_REOS no. 12908). The design, conduct, and reporting of the study complied with the ethical standards established by the 1961 Declaration of Helsinki (as revised in Hong Kong in 1989, and in Edinburgh, Scotland in 2000).
Statistical Analysis
The data is expressed as absolute number or percentage with 95% confidence interval (95% CI) for categorical variables, and as mean with standard error (SE), or median with interquartile range (IQR) for continuous variables. Some variables are always (i.e., type of ILD: IPF, yes–no; smoking status: current, former, and never smokers) or sometimes (exertional desaturation versus no exertional desaturation in the 6MWT; severe OSA versus no OSA plus mild-to-moderate OSA in the multivariate analysis) expressed as a binary or ternary outcome. A power analysis was not performed, as this work is an exploratory, observational and descriptive analytical study. We considered the following variables of known and possible prognostic significance in our analysis: sex, age, smoking status, BMI, type of ILD (IPF or otherwise), CPI, FEV1% predicted, FVC% predicted, DLco% predicted, PaO2, distance walked in meters, difference between starting and final modified Borg scores for dyspnea in 6MWT, AHI, ODI4 and CT90. Generalized linear models with Gaussian family and identity link were used to test for relationships between all prespecified variables of interest. Due to the small sample, we only performed analyses adjusted for CPI, as it seemed the best descriptor of disease severity at baseline. Progressive course, defined either as death or > 10% decline in FVC below baseline during the study period, was identified by risk factors using Cox proportional hazards regression analysis and the results were expressed as hazard ratio (HR) with 95% confidence intervals. Survival curves using the Kaplan–Meier product limit method for some predefined thresholds of disease severity are shown in Figs. 2 and 3. A p-value < 0.05 for a two-tailed distribution was considered statistically significant. All calculations were performed using Stata version 12 for Windows (College Station, TX, USA).
Results
As shown in Fig. 1, 63 subjects were eligible for the study, but the final analysis was performed on a population of 46 subjects (30 males, 16 females). Twenty-seven subjects (59%) had ILD limited to the lungs and the other 19 (41%) had lung involvement associated with a systemic disease. Other details of the population can be found in Fig. 1 and Table 1. At the time of enrollment, 21 subjects (45%) had been treated with systemic corticosteroids for a mean period of 2.4 (± 0.3) years. Seven patients were smokers, 22 were ex-smokers, and 17 never smokers. Twenty-six (57%) subjects showed exertional desaturation. Mean estimated sleep time was 7.2 h. Forty-three subjects underwent sleep poligraphy with a Somnea instrument. The number of subjects with AHI in the ranges ≥ 5–14.9, ≥ 15–29.9, and ≥ 30/h were 14 (31%, mild OSA), 6 (13%, moderate), and 9 (20%, severe), respectively. Some characteristics of subjects with severe OSA vs. no OSA plus mild-to-moderate OSA are reported in Table 2. Of the 20 subjects without exertional desaturation, 5 (25%), 10 (50%), and 5 (25%) patients had no OSA, mild-to-moderate OSA, and severe OSA, respectively. Of the 26 subjects with exertional desaturation, 12 (46%), 10 (38%), and 4 (13%) patients had no OSA, mild-to-moderate OSA, and severe OSA, respectively.
Median follow-up was 18 months (494 days, IQR 277–698 days). Six subjects died and 13 showed a ≥ 10% decline in FVC below baseline. Table 3 presents all the significant correlations detected between prespecified variables.
Using the univariate model, only age (HR 1.05; 95% CI 1.00–1.11; p = 0.038), difference between starting and trough oxyhemoglobin saturation level in the 6MWT (HR 1.15; 95% CI 1.00–1.30, p = 0.045), and AHI (HR 1.03; 95% CI 1.00–1.06; p < 0.048) were significantly associated with progressive course. Although not statistically significant (HR 1.06; 95% CI 0.95–1.16; p < 0.052), data for ODI4 was similar to that of AHI.
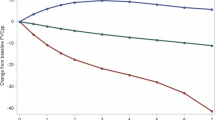
Multivariate analysis showed that only exertional desaturation (HR 8.23; 1.82–36.54 95% CI p = 0.006) and severe OSA (HR 7.53; 1.83–30.64; p = 0.005) were independently related to progressive course. Figure 2 shows Kaplan–Meier prognostic curves based on AHI dividing our sample into tertiles (A, no OSA; B, mild-to-moderate OSA; C, severe OSA). Group C showed the greatest negative impact (HR 5.50; 1.22–24.78 95% CI; p-trend = 0.025). Figure 3 shows Kaplan–Meier curves based on AHI and exertional desaturation dividing our sample into quartiles (A, AHI < 30, no exertional desaturation; B, AHI < 30 and exertional desaturation; C, AHI ≥ 30, no exertional desaturation; D, AHI ≥ 30 and exertional desaturation). Group D showed by far the worst prognosis (HR 46.52; 3.19–674.83 95% CI; p-trend = 0.005). Figure 4 shows scatter plots of CT90 versus AHI.
Kaplan–Meier disease progression curves in relation to Apnea–Hypopnea Index and exertional desaturation during walking test of 46 subjects with ILDs. Group A: no OSA, no exertional desaturation (blue line); Group B: OSA, no exertional desaturation (red line); Group C: no OSA, exertional desaturation (green line); Group D: OSA and exertional desaturation (orange line)
Discussion
Several studies have found that OSA is common in subjects with IPF and ILD [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37]. Some findings of prospective studies, including ours, on the prevalence of OSA in IPF and ILD populations are presented in Table 4 [15, 16, 18, 22,23,24,25,26,27,28, 30, 32,33,34,35,36,37]. This search was not systematic, but includes all the studies (with sample size > ten subjects) reported in a recent systematic review on the topic [47]. Differences between these studies may be due to variations in age, sex, BMI, treatment, disease severity of populations, and methods. Overall, OSA proves to be very common in subjects with IPF and ILD. However, OSA is in any case a highly prevalent disorder. For instance, in the large HypnoLaus Cohort study on a population age 35–75 years, AHI ≥ 5 and ≥ 15 (the thresholds of mild and moderate-to-severe OSA) were observed in 84% and 50% of men and 61% and 23% of women, respectively [48]. Cohorts studies have found a prevalence of OSA in subjects with chronic obstructive pulmonary disease (COPD), a chronic lung disease common in older males, similar to that in a healthy population [49, 50]. However, if untreated, the association of COPD and OSA is more detrimental to health than either condition alone [51].
The primary aim of our study was to evaluate the prognostic significance of certain sleep parameters in a population of subjects with mixed ILD with respect to other known indicators of poor outcome.
We found that exertional desaturation and AHI were independent negative predictors of disease course in our subjects. Exertional desaturation is a known negative prognostic factor in IPF and ILD populations, sometimes reported as a stronger predictor of prognosis than lung function test [7]. Exertional desaturation has been evaluated by different methods across studies. We used the 6MWT because it is a simple, safe, and inexpensive exercise test, widely used in clinical and trial settings with a standardized protocol and well-defined outcomes [41]. We defined exertional desaturation as a > 4% decrease in SpO2 below baseline and a SpO2 nadir ≤ 90%, as previously reported [52]. We observed exertional desaturation in 57% of our subjects with no significant difference between those with IPF and those with other ILDs. This result is similar to those of other studies. In an unselected cohort of IPF patients, a ≈ 50% prevalence of exertional desaturation was reported [5], while in another large group of 400 subjects with mixed ILDs, exertional desaturation was observed in 54% of cases without any significant difference between different types of ILD [53].
The impact of sleep parameters and elevated AHI on prognosis of subjects with ILD is less obvious. In one study, no association was observed between AHI > 20 and survival in 27 newly diagnosed steroid-naïve IPF subjects undergoing unattended polygraphy and monitored for 5 years [23]. In another prospective study, sleeping nadir oxyhemoglobin saturation (but not AHI) was inversely related to survival in a group of 31 IPF subjects [18]. In another mixed population of 134 ILD subjects, there was retrospective evidence that sleep hypoxemia, defined as ≥ 10% of sleep with oxyhemoglobin saturation ≤ 90%, was a predictor of progressive disease. These authors also observed that sleeping desaturation may occur in the context of mild ILD and may be disproportionate to the extent of the underlying ILD [17]. Another study found that sleep-related hypoxemia (defined as total sleep time spent with saturation ≤ 90%) was a negative prognostic predictor in a population of 92 subjects with mixed ILDs [34]. Finally, Bosi et al. [25] found that OSA and sleep-related hypoxemia were associated with disease progression in a group of 35 subjects with IPF; interestingly, they noted that the severity of OSA was an independent predictor of prognosis. We found that AHI has an independent negative effect on disease course. Of course, our results need to be confirmed in larger and more homogeneous populations.
There may be several explanations for the negative effect of AHI on the course of ILDs. Untreated OSA may predispose to or aggravate lung fibrosis through gastric reflux, oxidative stress, and cytokine-mediated inflammatory pathways activated by intermittent hypoxia-reoxygenation episodes and tractional lung injury caused by intrathoracic pressure swings. Gille et al. [22] showed that persistent intermittent hypoxemia was linked to increased oxidative stress and chronic inflammation. Repeated swings in pleural pressure associated with apneas/hypopneas episodes could result in recurrent tractional stretch on alveolar tissue, causing in turn cellular injury and inflammation. An intriguing cross-sectional study of community-dwelling adults [54] observed an association between moderate-to-severe OSA and subclinical ILDs, mainly among normal-weight adults.
Limits of the Study
Our study has several limitations. Firstly, sample size was small and there was no control group. Secondly, we excluded ILD subjects treated for OSA. Thirdly, we studied our ILD population with a portable type III monitoring device. These systems offer the opportunity to increase diagnostic capacity and are less expansive and labor intensive than polysomnography at the expense of accuracy [55]. Unlike level I devices, level III systems cannot measure the duration of sleep and sleep stages. So, sleep time is estimated rather than objectively measured, which often leads to underestimation of disease severity [45]. Level III systems also do not permit to recognize arousals. We defined hypopneas according to 2007 AASM guideline as episodes with > 30% airflow decrease for at least 10 s accompanied by ≥ 4% oxyhemoglobin desaturation [43]. The 2012 American Academy of Sleep Medicine (AASM) accepts this definition, but recommends recording hypopneas as > 30% airflow decreases for at least 10 s associated with either ≥ 3% desaturation or arousal [44]. The first method of scoring hypopneas may also underestimate the severity of OSA [55]. Finally, although most of our subjects reported bothersome nocturnal symptoms, such as coughing or dyspnea, others had trouble falling asleep, woke frequently, or had nonrestorative sleep (data not shown). We did not systematically investigate sleep-related symptoms by means of validated questionnaires.
Conclusions
OSA was common in our population of subjects with different types of ILDs. Exertional desaturation and AHI were independently associated with progressive course. Our results, if confirmed, are a further indication of the need for effective treatments of exertional desaturation and OSA.
References
Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824.
Nasser M, Larrieu S, Si-Mohamed S, et al. Progressive fibrosing interstitial lung disease: a clinical cohort (the PROGRESS® study). Eur Respir J. 2021;57(2):2002718. https://doi.org/10.1183/13993003.02718-2020. (PMID: 32943410).
Wongkarnjana A, Scallan C, Kolb MRJ. Progressive fibrosing interstitial lung disease: treatable traits and therapeutic strategies. Curr Opin Pulm Med. 2020;26(5):436–42. https://doi.org/10.1097/mcp.0000000000000712.
du Bois RM, Weycker D, Albera C, et al. Ascertainment of individual risk of mortality for patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;184(4):459–66.
Flaherty KR, Andrei AC, Murray S, et al. Idiopathic pulmonary fibrosis: prognostic value of changes in physiology and six-minute-walk test. Am J Respir Crit Care Med. 2006;174(7):803–9.
du Bois RM, Albera C, Bradford WZ, et al. 6-Minute walk distance is an independent predictor of mortality in patients with idiopathic pulmonary fibrosis. Eur Respir J. 2014;43(5):1421–8.
Lama VN, Flaherty KR, Toews GB, et al. Prognostic value of desaturation during a 6-minute walk test in idiopathic interstitial pneumonia. Am J Respir Crit Care Med. 2003;168(9):1084–90. https://doi.org/10.1164/rccm.200302-219OC. (PMID: 12917227).
McNicholas WT, Coffey M, Fitzgerald MX. Ventilation and gas exchange during sleep in patients with interstitial lung disease. Thorax. 1986;41(10):777–82. https://doi.org/10.1136/thx.41.10.77.
Midgren B. Oxygen desaturation during sleep as a function of the underlying respiratory disease. Am Rev Respir Dis. 1990;141(1):43–6. https://doi.org/10.1164/ajrccm/141.1.4.
Bye PT, Issa F, Berthon-Jones M, Sullivan CE. Studies of oxygenation during sleep in patients with interstitial lung disease. Am Rev Respir Dis. 1984;129(1):27–32. https://doi.org/10.1164/arrd.1984.129.1.27.
Perez-Padilla R, West P, Lertzman M, Kryger MH. Breathing during sleep in patients with interstitial lung disease. Am Rev Respir Dis. 1985;132:224–322.
Clark M, Cooper B, Singh S, Cooper M, Carr A, Hubbard R. A survey of nocturnal hypoxaemia and health related quality of life in patients with cryptogenic fibrosing alveolitis. Thorax. 2001;56:482–6.
Krishnan V, McCormack MC, Mathai SC, et al. Sleep quality and health-related quality of life in idiopathic pulmonary fibrosis. Chest. 2008;134(4):693–8. https://doi.org/10.1378/chest.08-0173.
Mermigkis C, Chapman J, Golish J, et al. Sleep-related breathing disorders in patients with idiopathic pulmonary fibrosis. Lung. 2007;185:173–8.
Lancaster LH, Mason WR, Parnell JA, et al. Obstructive sleep apnea is common in idiopathic pulmonary fibrosis. Chest. 2009;136:772–8.
Mermigkis C, Stagaki E, Tryfon S, et al. How common is sleep-disordered breathing in patients with idiopathic pulmonary fibrosis? Sleep Breath. 2010;14:387–90.
Corte TJ, Wort SJ, Talbot S, et al. Elevated nocturnal desaturation index predicts mortality in interstitial lung disease. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29:41–50.
Kolilekas L, Manali E, Vlami KA, et al. Sleep oxygen desaturation predicts survival in idiopathic pulmonary fibrosis. J Clin Sleep Med. 2013;9:593–601.
Mermigkis C, Bouloukaki I, Antoniou KM, et al. CPAP therapy in patients with idiopathic pulmonary fibrosis and obstructive sleep apnea: does it offer a better quality of life and sleep? Sleep Breath. 2013;17:1137–43.
Pihtili A, Bingol Z, Kiyan E, et al. Obstructive sleep apnea is common in patients with interstitial lung disease. Sleep Breath. 2013;17:1281–8.
Pitsiou G, Bagalas V, Boutou A, Stanopoulos I, Argyropoulou-Pataka P. Should we routinely screen patients with idiopathic pulmonary fibrosis for nocturnal hypoxemia? Sleep Breath. 2013;17(2):447–8. https://doi.org/10.1007/s11325-012-0716-0. (PMID: 22562264).
Mermigkis C, Bouloukaki I, Antoniou K, et al. Obstructive sleep apnea should be treated in patients with idiopathic pulmonary fibrosis. Sleep Breath. 2015;19:385–91.
Reid T, Vennelle M, McKinley M, et al. Sleep disordered breathing and idiopathic pulmonary fibrosis–is there an association? Sleep Breath. 2015;19(2):719–21.
Lee RN, Kelly E, Nolan G, et al. Disordered breathing during sleep and exercise in idiopathic pulmonary fibrosis. QJM. 2016;109(2):142.
Bosi M, Milioli G, Fanfulla F, et al. OSA and prolonged oxygen desaturation during sleep are strong predictors of poor outcome in IPF. Lung. 2017;195(5):643–51.
Gille T, Didier M, Boubaya M, et al. Obstructive sleep apnoea and related comorbidities in incident idiopathic pulmonary fibrosis. Eur Respir J. 2017. https://doi.org/10.1183/13993003.01934-2016.
Ahmed M, Awadalla NJ. Burden of sleep-related breathing disorders, air trapping, and obesity in idiopathic pulmonary fibrosis patients. Egypt J Chest Dis Tuberc. 2018;67:300–5. https://doi.org/10.4103/ejcdt.ejcdt_32_17.
Mavroudi M, Papakosta D, Kontakiotis T, et al. Sleep disorders and health-related quality of life in patients with interstitial lung disease. Sleep Breath. 2018;22(2):393–400.
Bosi M, Milioli G, Parrino L, et al. Quality of life in idiopathic pulmonary fibrosis: the impact of sleep disordered breathing. Respir Med. 2019;147:51–7. https://doi.org/10.1016/j.rmed.2018.12.018.
Canora A, Nicoletta C, Ghinassi G, et al. First description of the hyperpnea-hypopnea periodic breathing in patients with interstitial lung disease-obstructive sleep apnea: treatment implications in a real-life setting. Int J Environ Res Public Health. 2019;16(23):4712. https://doi.org/10.3390/ijerph16234712. (PMID: 31779226).
Cho JG, Teoh A, Roberts M, Wheatley J. The prevalence of poor sleep quality and its associated factors in patients with interstitial lung disease: a cross-sectional analysis. Eur Respir J Open Res. 2019;5(3):00062–2019. https://doi.org/10.1183/23120541.00062-2019.
Pereira N, Cardoso AV, Mota PC, et al. Predictive factors of obstructive sleep apnoea in patients with fibrotic lung diseases. Sleep Med. 2019;56:123–7. https://doi.org/10.1016/j.sleep.2019.01.020.
Sarac S, Kavas M, Sahin M, Aras G, Afsar GC, Tezel YB. Relation of Warrick Score and polysomnographic parameters in patients with interstitial lung disease. Med Sci Monit. 2019;25:2087–95. https://doi.org/10.12659/MSM.914905.
Troy LK, Young IH, Lau EMT, et al. Nocturnal hypoxaemia is associated with adverse outcomes in interstitial lung disease. Respirology. 2019;24(10):996–1004. https://doi.org/10.1111/resp.13549.
Tudorache V, Traila D, Marc M, et al. Impact of moderate to severe obstructive sleep apnea on the cognition in idiopathic pulmonary fibrosis. PLoS ONE. 2019;14(2):e0211455. https://doi.org/10.1371/journal.pone.0211455. (PMID: 30707735).
Zhang XL, Dai HP, Zhang H, et al. Obstructive sleep apnea in patients with fibrotic interstitial lung disease and COPD. J Clin Sleep Med. 2019;15(12):1807–15. https://doi.org/10.5664/jcsm.8090. (PMID: 31855166).
Papadogiannis G, Bouloukaki I, Mermigkis C, et al. Patients with idiopathic pulmonary fibrosis with and without obstructive sleep apnea: differences in clinical characteristics, clinical outcomes, and the effect of PAP treatment. J Clin Sleep Med. 2021;17(3):533–44. https://doi.org/10.5664/jcsm.8932. (PMID: 33108270).
Miller MR, Hankinson J, Brusasco V, on behalf of the ATS/ERS Task Force, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38.
Quanjer PH, Stanojevic S, Cole TJ, on behalf of the ERS Global Lung Function Initiative, et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–43.
Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–68. https://doi.org/10.1183/09031936.05.00035205.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–7.
Wells AU, Desai SR, Rubens MB, et al. Idiopathic pulmonary fibrosis: a composite physiologic index derived from disease extent observed by computed tomography. Am J Respir Crit Care Med. 2003;167(7):962–9.
Iber C, Ancoli-Israel S, Chesson AL Jr, Quan SF, for the American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Westchester: American Academy of Sleep Medicine; 2007.
Berry RB, Budhiraja R, Gottlieb DJ, for the American Academy of Sleep Medicine, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events—deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597–661.
El Shayeb M, Topfer LA, Stafinski T, Pawluk L, Menon D. Diagnostic accuracy of level 3 portable sleep tests versus level 1 polysomnography for sleep-disordered breathing: a systematic review and meta-analysis. CMAJ. 2014;186(1):E25-51. https://doi.org/10.1503/cmaj.130952. (PMID:24218531).
Richeldi L, Ryerson CJ, Lee JS, et al. Relative versus absolute change in forced vital capacity in idiopathic pulmonary fibrosis. Thorax. 2012;67(5):407–11.
Karuga FF, Kaczmarski P, Szmyd B, et al. The association between idiopathic pulmonary fibrosis and obstructive sleep apnea: a systematic review and meta-analysis. J Clin Med. 2022;11(17):5008. https://doi.org/10.3390/jcm11175008. (PMID: 36078938).
Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310–8.
Sanders MH, Newman AB, Haggerty CL, et al. Sleep and sleep-disordered breathing in adults with predominantly mild obstructive airway disease. Am J Respir Crit Care Med. 2003;167(1):7–14.
Bednarek M, Plywaczewski R, Jonczak L, Zielinski J. There is no relationship between chronic obstructive pulmonary disease and obstructive sleep apnea syndrome: a population study. Respiration. 2005;72(2):142–9.
Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182(3):325–33.
Jenkins S, Cecins N. Six-minute walk test: observed adverse events and oxygen desaturation in a large cohort of patients with chronic lung disease. Intern Med J. 2011;41(5):416–22.
Khor YH, Goh NSL, Glaspole I, Holland AE, McDonald CF. Exertional desaturation and prescription of ambulatory oxygen therapy in interstitial lung disease. Respir Care. 2019;64(3):299–306. https://doi.org/10.4187/respcare.06334. (PMID: 30377245).
Kim JS, Podolanczuk AJ, Borker P, et al. Obstructive sleep apnea and subclinical interstitial lung disease in the multi-ethnic study of atherosclerosis (MESA). Ann Am Thorac Soc. 2017;14(12):1786–95. https://doi.org/10.1513/AnnalsATS.201701-091OC.
Mansukhani MP, Kolla BP, Wang Z, Morgenthaler TI. Effect of varying definitions of hypopnea on the diagnosis and clinical outcomes of sleep-disordered breathing: a systematic review and meta-analysis. J Clin Sleep Med. 2019;15(5):687–96. https://doi.org/10.5664/jcsm.7750. (PMID: 31053203).
Acknowledgements
We thank collaborators who collected data and cared for the patients; we thank Helen Ampt for her language editing
Funding
No funding or sponsorship was received for this study or publication of this article.
Authors Contributions
We declare that all the authors made substantial contributions as follows: Paola Rottoli and Debora Valecchi conceived and designed the study; Debora Valecchi, Andrea Melani, Elena Bargagli, Maria Grazia Pieroni and Metella Refini acquired data; Andrea Melani reviewed polysomonographic examinations; Piersante Sestini analysed data; Piersante Sestini, Andrea Melani and Paola Rottoli interpreted data, Andrea Melani drafted the article; all authors read and critically revised the manuscript and approved the version to be submitted.
Disclosures
The authors declare that there is no disclosure/conflict of interest regarding the publication of this paper.
Compliance with Ethics Guidelines
The study was approved by the institutional ethics board of the university hospital (CEAVSE, Tuscany, Italy, OSS_REOS number 12908). The design, conduct, and reporting of this study complied with the ethical standards established by the 1961 Declaration of Helsinki (as revised in Hong Kong in 1989, and in Edinburgh, Scotland, in 2000). All participants gave their written informed consent.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Valecchi, D., Bargagli, E., Pieroni, M.G. et al. Prognostic Significance of Obstructive Sleep Apnea in a Population of Subjects with Interstitial Lung Diseases. Pulm Ther 9, 223–236 (2023). https://doi.org/10.1007/s41030-023-00215-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-023-00215-1