Abstract
Purpose
Sleep Breathing Disorders (SBD) are frequently found in idiopathic pulmonary fibrosis (IPF) and they are associated with worse quality of sleep and life and with higher mortality. The study aimed at evaluating the impact of SBD on prognosis (mortality or disease progression) in 35 patients with mild to moderate IPF.
Methods and Results
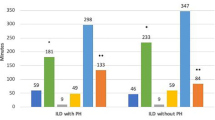
Obstructive sleep apnea (OSA) was diagnosed in 25/35 patients with IPF: 14/35 mild, 7/35 moderate, and 4/35 severe. According to the American Academy of Sleep Medicine (AASM) definition, sleep-related hypoxemia was found in 9/35 patients with IPF. According to the presence/absence of SBD, IPF patients were divided into 4 groups: NO-SBD group (Group A, 25.7%), OSA without sleep-related hypoxemia (Group B, 48.5%), OSA with sleep-related hypoxemia group (Group C, 22.8%), and only 1/35 had sleep-related hypoxemia without OSA(Group D, 2.8%). Statistical analysis was focused only on group A, B, and C. Patients with OSAS and sleep-related hypoxemia (Group C) had the worse prognosis, both in terms of mortality or clinical deterioration. SBD were the only independent risk factor (Cox Proportional Hazards Multiple Regression Analysis) for mortality (HR 7.6% IC 1.2–36.3; p = 0.029) and disease progression (HR 9.95% IC 1.8–644.9; p = 0.007).
Conclusions
SBD are associated with a worse prognosis, both in terms of mortality or clinical progression. The presence of SBD should be explored in all IPF patients.



Similar content being viewed by others
Abbreviations
- 6Mwtest:
-
6 minutes walking test
- 6MWD:
-
6 minutes walking distance
- AE:
-
Acute phase
- AHI:
-
Apnea hypopea index,
- BMI:
-
Body mass index
- Dlco:
-
Diffusion lung capacity for carbon monoxide (% or predicted)
- FEV1:
-
Forced expiratory volume in the first second
- FVC:
-
Forced vital capacity
- IPF:
-
Idiopathic pulmonary fibrosis
- ODI:
-
Oxygen desaturation index
- OSA:
-
Obstructive sleep apnea
- PaCO2 :
-
Arterial carbon dioxide partial pressure
- PaO2 :
-
Arterial oxygen partial pressure
- POD:
-
Death or the first episode of progression of disease
- RDI:
-
Respiratory disturbance index
- RERA:
-
Respiratory effort related arousal
- SaO2 :
-
Average SpO2 during sleep
- SaO2w :
-
Average SpO2 during wakefulness
- SBD:
-
Sleep Breathing Disorders
- SE:
-
Sleep efficiency
- T90:
-
% of total sleep time spent with SpO2 < 90%
- TST:
-
Total sleep time
- V/Q:
-
Ventilation/perfusion relationship
- WASO:
-
Wake time after sleep onset
References
Ley B, Ryerson CJ, Vittinghoff E, Ryu JH, Tomassetti S, Lee JS, Poletti V, Buccioli M, Elicker BM, Jones KD, King TE, Collard HR (2012) A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med 156:684–691. doi:10.7326/0003-4819-156-10-201205150-00004
Drent M, du Bois RM, Poletti V (2003) Recent advances in the diagnosis and management of nonspecific interstitial pneumonia. Curr Opin Pulm Med 9:411–417
Poletti V, Ravaglia C, Buccioli M, Tantalocco P, Piciucchi S, Dubini A, Carloni A, Chilosi M, Tomassetti S (2013) Idiopathic pulmonary fibrosis: diagnosis and prognostic evaluation. Respiration. 86:5–12. doi:10.1159/000353580
De Vries J, Kessels BL, Drent M (2001) Quality of life of idiopathic pulmonary fibrosis patients. Eur Respir J 17:954–961
Swigris JJ, Kuschner WG, Jacobs SS, Wilson SR, Gould MK (2005) Health-related quality of life in patients with idiopathic pulmonary fibrosis: a systematic review. Thorax 60:588–594. doi:10.1136/thx.2004.035220
Kreuter M, Wuyts W, Renzoni E, Koschel D, Maher TM, Kolb M, Weycker D, Spagnolo P, Kirchgaessler K-U, Herth FJF, Costabel U (2016) Antacid therapy and disease outcomes in idiopathic pulmonary fibrosis: a pooled analysis. Lancet Respir Med 4:381–389. doi:10.1016/S2213-2600(16)00067-9
De Boer K, Lee JS (2016) Under-recognised co-morbidities in idiopathic pulmonary fibrosis: a review. Respirology 21:995–1004. doi:10.1111/resp.12622
Papiris SA, Kagouridis K, Kolilekas L, Bouros D, Manali ED (2014) Idiopathic pulmonary fibrosis acute exacerbations: where are we now? Expert Rev Respir Med 8:271–273. doi:10.1586/17476348.2014.896206
Papiris SA, Kagouridis K, Kolilekas L, Papaioannou AI, Roussou A, Triantafillidou C, Baou K, Malagari K, Argentos S, Kotanidou A, Karakatsani A, Manali ED (2015) Survival in Idiopathic pulmonary fibrosis acute exacerbations: the non-steroid approach. BMC Pulm Med. doi:10.1186/s12890-015-0146-4
Jo HE, Randhawa S, Corte TJ, Moodley Y (2016) Idiopathic pulmonary fibrosis and the elderly: diagnosis and management considerations. Drugs Aging 33:321–334. doi:10.1007/s40266-016-0366-1
Antoniou KM, Tomassetti S, Tsitoura E, Vancheri C (2015) Idiopathic pulmonary fibrosis and lung cancer: a clinical and pathogenesis update. Curr Opin Pulm Med 21:626–633. doi:10.1097/MCP.0000000000000217
Mermigkis C, Stagaki E, Amfilochiou A, Polychronopoulos V, Korkonikitas P, Mermigkis D, Bregou M, Kouris N, Bouros D (2009) Sleep quality and associated daytime consequences in patients with idiopathic pulmonary fibrosis. Med Princ Pract 18:10–15. doi:10.1159/000163039
Agarwal S, Richardson B, Krishnan V, Schneider H, Collop NA, Danoff SK (2009) Interstitial lung disease and sleep: what is known? Sleep Med 10:947–951. doi:10.1016/j.sleep.2009.01.004
Perez-Padilla R, West P, Lertzman M, Kryger MH (1985) Breathing during sleep in patients with interstitial lung disease. Am Rev Respir Dis 132:224–229
Milioli G, Bosi M, Poletti V, Tomassetti S, Grassi A, Riccardi S, Terzano MG, Parrino L (2015) Sleep and respiratory sleep disorders in idiopathic pulmonary fibrosis. Sleep Med Rev 26:57–63. doi:10.1016/j.smrv.2015.03.005
Schiza S, Mermigkis C, Margaritopoulos GA, Daniil Z, Harari S, Poletti V, Renzoni EA, Torre O, Visca D, Bouloukaki I, Sourvinos G, Antoniou KM (2015) Idiopathic pulmonary fibrosis and sleep disorders: no longer strangers in the night. Eur Respir Rev 24:327–339. doi:10.1183/16000617.00009114
Ruhle K-H (2010) Commentary on how common is sleep-disordered breathing in patients with idiopathic pulmonary fibrosis? Mermigkis C. et al. Sleep Breath 14:289. doi:10.1007/s11325-010-0341-8
Mermigkis C, Stagaki E, Tryfon S, Schiza S, Amfilochiou A, Polychronopoulos V, Panagou P, Galanis N, Kallianos A, Mermigkis D, Kopanakis A, Varouchakis G, Kapsimalis F, Bouros D (2010) How common is sleep-disordered breathing in patients with idiopathic pulmonary fibrosis? Sleep Breath 14:387–390. doi:10.1007/s11325-010-0336-5
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, Colby TV, Cordier J-F, Flaherty KR, Lasky JA, Lynch DA, Ryu JH, Swigris JJ, Wells AU, Ancochea J, Bouros D, Carvalho C, Costabel U, Ebina M, Hansell DM, Johkoh T, Kim DS, King TE, Kondoh Y, Myers J, Müller NL, Nicholson AG, Richeldi L, Selman M, Dudden RF, Griss BS, Protzko SL, Schünemann HJ (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183:788–824. doi:10.1164/rccm.2009-040GL
Collard HR, Ryerson CJ, Corte TJ, Jenkins G, Kondoh Y, Lederer DJ, Lee JS, Maher TM, Wells AU, Antoniou KM, Behr J, Brown KK, Cottin V, Flaherty KR, Fukuoka J, Hansell DM, Johkoh T, Kaminski N, Kim DS, Kolb M, Lynch DA, Myers JL, Raghu G, Richeldi L, Taniguchi H, Martinez FJ (2016) Acute exacerbation of idiopathic pulmonary fibrosis. An International Working Group Report. Am J Respir Crit Care Med 194:265–275. doi:10.1164/rccm.201604-0801CI
The AASM Manual for the Scoring of Sleep and Associated Events (2014). Version 2.1, American academy of sleep medicine
American Academy of Sleep Medicine (2014). International Classification of Sleep Disorders, Third Edition., Am Acad Sleep Med
Kolilekas L, Manali E, Vlami KA, Lyberopoulos P, Triantafillidou C, Kagouridis K, Baou K, Gyftopoulos S, Vougas KN, Karakatsani A, Alchanatis M, Papiris S (2013) Sleep oxygen desaturation predicts survival in idiopathic pulmonary fibrosis. J Clin Sleep Med 9:593–601. doi:10.5664/jcsm.2758
Becker HF, Piper AJ, Flynn WE, McNamara SG, Grunstein RR, Peter JH, Sullivan CE (1999) Breathing during sleep in patients with nocturnal desaturation. Am J Respir Crit Care Med 159:112–118. doi:10.1164/ajrccm.159.1.9803037
Pitsiou G, Bagalas V, Boutou A, Stanopoulos I, Argyropoulou-Pataka P (2013) Should we routinely screen patients with idiopathic pulmonary fibrosis for nocturnal hypoxemia? Sleep Breath 17:447–448. doi:10.1007/s11325-012-0716-0
Corte TJ, Wort SJ, Talbot S, Macdonald PM, Hansel DM, Polkey M, Renzoni E, Maher TM, Nicholson AG, Wells AU (2012) Elevated nocturnal desaturation index predicts mortality in interstitial lung disease. Sarcoidosis Vasc Diffuse Lung Dis 29:41–50
Mermigkis C, Bouloukaki I, Antoniou KM, Mermigkis D, Psathakis K, Giannarakis I, Varouchakis G, Siafakas N, Schiza SE (2013) CPAP therapy in patients with idiopathic pulmonary fibrosis and obstructive sleep apnea: does it offer a better quality of life and sleep? Sleep Breath 17:1137–1143. doi:10.1007/s11325-013-0813-8
Mermigkis C, Bouloukaki I, Antoniou K, Papadogiannis G, Giannarakis I, Varouchakis G, Siafakas N, Schiza SE (2015) Obstructive sleep apnea should be treated in patients with idiopathic pulmonary fibrosis. Sleep Breath. 19:385–391. doi:10.1007/s11325-014-1033-6
Mermigkis C, Bouloukaki I, Schiza SE (2013) Obstructive sleep apnea in patients with interstitial lung diseases: past and future. Sleep Breath 17:1127–1128. doi:10.1007/s11325-013-0836-1
McNicholas WT, Coffey M, Fitzgerald MX (1986) Ventilation and gas exchange during sleep in patients with interstitial lung disease. Thorax 41:777–782
Bye PT, Issa F, Berthon-Jones M, Sullivan CE (1984) Studies of oxygenation during sleep in patients with interstitial lung disease. Am Rev Respir Dis 129:27–32
Fanfulla F, Grassi M, Taurino AE, D’Artavilla Lupo N, Trentin R (2008) The relationship of daytime hypoxemia and nocturnal hypoxia in obstructive sleep apnea syndrome. Sleep 31:249–255
Lacedonia D, Carpagnano GE, Aliani M, Sabato R, Foschino Barbaro MP, Spanevello A, Carone M, Fanfulla F (2013) Daytime PaO2 in OSAS, COPD and the combination of the two (overlap syndrome). Respir Med 107:310–316. doi:10.1016/j.rmed.2012.10.012
Author Contributions
MB, GM, FF, and LP had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. MB, GM, FF, LP, ST, JHR, SR, AM, AEV, CR, PT, AR, VP contributed substantially to the study design, data analysis and interpretation, and the writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This was not an industry supported study. Marcello Bosi, Giulia Milioli,Francesco Fanfulla, Sara Tomassetti, Jay H Ryu, Liborio Parrino, Silvia Riccardi, Andrea Melpignano, Anna Elisabetta Vaudano, Claudia Ravaglia, Paola Tantalocco, Andrea Rossi, and Venerino Poletti have indicated no financial conflict of interest.
Rights and permissions
About this article
Cite this article
Bosi, M., Milioli, G., Fanfulla, F. et al. OSA and Prolonged Oxygen Desaturation During Sleep are Strong Predictors of Poor Outcome in IPF. Lung 195, 643–651 (2017). https://doi.org/10.1007/s00408-017-0031-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-017-0031-4