Abstract
Purpose of Review
The aim of this narrative review is to summarize critical considerations for perioperative airway management and mechanical ventilation in patients undergoing neurosurgical procedures.
Recent Findings
Given the significant influence that ventilation has on intracranial pressure (ICP) and cerebral blood flow, ventilator settings need to be carefully managed. For example, high positive end-expiratory pressure (PEEP) can increase ICP, while hyperventilation can reduce it. Finding the optimal balance is the key. While evidence supporting lung-protective ventilation in neurosurgical patients is limited, preliminary data suggest that its use could be beneficial, similar to general surgical patients. This typically involves using lower tidal volumes and maintaining optimal oxygenation to prevent ventilator-associated lung injury. Airway management in neurosurgical patients must consider the risk of increased ICP during intubation and the potential for airway complications. Techniques like rapid sequence induction and the use of neuromuscular blockers may be employed to minimize these risks. The primary goal of ventilation in neurosurgical patients is to maintain adequate oxygenation and carbon dioxide removal while minimizing harm to the lungs and brain. However, there may be exceptions where specific ventilatory adjustments are needed, such as in cases of compromised gas exchange or elevated ICP.
Summary
Patients undergoing neurosurgical procedures often require invasive ventilation due to the complexities of the operation and the need to manage the airway. This creates unique challenges because ventilator settings must balance the need to protect both the lungs and the brain. Further research is needed to establish clear guidelines and optimize ventilatory care in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In acute brain injury (ABI), patients undergoing neurosurgical procedures often require sedation and invasive mechanical ventilation (MV) for airway protection and ventilatory support. However, invasive MV poses potential risks to several organ systems and, therefore, necessitates careful considerations when choosing ventilatory strategies. A balance between preventing both ventilator-induced lung injury (VILI) and brain injury requires careful consideration, with the latter requiring monitoring of hemodynamics, cerebral perfusion and intracranial pressure (ICP) [1].
Little is known about MV in neurosurgical patients and most of the data stem from perioperative surgical or intensive care unit (ICU) cohorts. Lung-protective ventilation (LPV), a strategy discussed in the MV section, is employed during various surgical procedures [2] to prevent postoperative pulmonary complications (PPCs) [3] such as VILI [4]; however, it is often avoided in patients undergoing neurosurgical anesthesia [5].
Another critical consideration is the bi-directional brain-lung crosstalk [6,7,8], which may increase the risk of secondary brain injury [9]. Brain-lung crosstalk is mediated by multiple mechanisms [10]. After brain injury, inflammatory responses, hormonal dysregulation and catecholamine surges, result in increased expression of injurious molecular patterns and affect the lymphatic system [11]. This immune activation can directly damage type II pneumocytes, increasing pulmonary vascular hydrostatic pressure and lung capillary permeability, ultimately leading to lung injury [6, 8, 12,13,14].
Given the challenges associated with neurosurgical procedures, this review summarizes the current knowledge on specific airway management, MV parameters, thresholds to avoid brain and lung injury, extubation, and the risk of PPCs in patients undergoing neurosurgical procedures.
Specific Airway Management Considerations in Neurosurgical Patients
Positioning, cervical spine stability, hemodynamics during induction and the effects of anesthesia on ICP are unique conditions that may complicate airway management in neurosurgical patients [15]. Neurosurgical approaches involving the pituitary gland, temporal lobe or occipital-cervical zone, such as the Halo position or stereotactic head frame, often require forced unnatural head positions, leading to difficult airway management or failed intubation. Prolonged unnatural head positioning can impair cerebral venous outflow, potentially causing intraoperative brain swelling, increased ICP, ischemia, and cerebral infarction [15, 16]. The risk of ischemia is augmented in patients with large vessel occlusions [17].
Acute cervical spine injuries require immobilization and a cervical collar, hindering head extension during intubation, which may complicate airway management.
In addition, fluctuations in arterial blood pressure (ABP) can affect cerebral autoregulation, leading to poor postoperative outcomes like stroke, acute kidney injury, and delirium. It is important to individualize ABP targets to preserve cerebral perfusion [18]. Recent research, conducted in patients undergoing elective neurosurgery, monitored cerebral autoregulation (CA) using the correlation between changes in mean artery pressure (MAP) and regional cerebral O2 saturation (rSO2). Although preoperative ABP value is often the target used to adjust the intraoperative ABP value, the optimal ABP (defined as the value above lower limit of CA) is lower than the ABP at the baseline. These data may suggest the need of monitoring CA intraoperatively in order to personalized ABP target preserving cerebral perfusion [18].
Prolonged ventilation due to difficulties in airway management may lead to hypercapnia, hypoxemia and increased cerebral blood flow (CBF) with the risk of intracranial hypertension. In addition, laryngoscopy and intubation maneuvers often result in increase in systolic blood pressure by a mean of 20 mmHg [19], and consequentially in a rise of MAP and possibly of ICP especially in patients with impaired CA [20]. During this phase it is important to balance and maintain cerebral hemodynamics parameters as CBF, cerebral metabolic rate of oxygen (CMRO2) and cerebrospinal fluid (CSF) dynamics by ensuring deep sedation, avoiding increased ICP and cerebral perfusion pressure (CPP) as consequence of extreme hyper- and hypotension, and the safeguarding of cerebral and spinal perfusion [21].
The optimal airway management strategy in neurosurgical patients is not yet defined and should be individualized. Generally, a focused medical history on potential difficult airway or on signs and symptoms of intracranial vascular insufficiency followed by a detailed physical examination (neck mobility, cervical cord stability etc.) and by the consultation of imaging is recommended in the preoperative period to anticipate and address eventual difficulties. In case of elective cranio-facial procedures and suspected difficult airway, a preoperative endoscopic airway examination could be considered in order to reduce the use of unnecessary awake intubation [22]. For patients with cervical spine instability, techniques minimizing head movement, maintaining head neutral position [23] with a manual in-line stabilization [24], are aimed to prevent secondary neurologic injury. A review suggests that conventional direct laryngoscopy may be inappropriate for securing the upper airway in cervical spine surgery [23]. Awake flexible fiberoptic intubation, nasal intubation, video-laryngoscopy and neck immobilization could be considered in case of unstable cervical spine patients [25]. If intraoperative intubation is necessary during awake surgery, a video-laryngoscope approach is indicated [21].
During endotracheal intubation, it is crucial to avoid hypoxia by ensuring adequate preoxygenation. Three minutes of preoxygenation with 100% of fraction inspirated of oxygen (FiO2) or a short period of high flow nasal cannula (HFNC) is highly recommended [26]. The risk of hypercapnia and hypertension can be mitigated by using an appropriate level of sedation to blunt the sympathetic response to intubation [21]. In addition, care must be taken to prevent neck rotation which can lead to jugular vein compression and increases in intrathoracic pressure and ICP [27]. Weintraub et al. suggest that a prolonged (> 12 min) neck hyperextension could predispose to perioperative stroke because of transient changes in blood flow [28]. In a swine model, rapid sequence intubation (RSI) with paralysis seems to generate three-fold increases in peak of ICP compared with sedation only [29].
Furthermore, as recommended by American Society of Anesthesiologists guidelines during the intubation phase it is fundamental to use End tidal carbon dioxide (ETCO2) monitoring as a standard of anesthetic monitoring to ensure adequate ventilation throughout the surgical procedure. This is extremely useful in neurosurgical patients, also because of the linear relation between PaCO2 and cerebral blood flow. Supporting this, in cervical spine surgery patients with change of position from supine to prone, a recent study reported that PaCO2 can decrease with no significant change in arterial to ETCO2 value, suggesting that ETCO2 can be used as a reliable guide to estimate PaCO2 also during cervical spine procedures in prone position [30].
In any case, the best strategy for airway management seems to be the one with the highest possibility of success on the first attempt considering the operator’s knowledge and with the lowest influence on patients [24]. Figure 1 summarizes issues in airway management in neurosurgical patients.
Mechanical Ventilation Strategies
LPV uses low tidal volumes (VT) (6–8 ml/kg of PBW) and moderate positive end-expiratory pressure (PEEP) [31] Although LPV has been shown to reduce PPCs in other surgical contexts [3, 32,33,34], its use in neurosurgical patients is controversial.
In this line, the use of low VT during LPV can result in hypercapnia with consequent harmful effects, such as cerebral vasodilatation and raised ICP [35,36,37]. In addition, PEEP may increase intrathoracic pressure, with a potential risk of intracranial hypertension due to diminished outflow from the jugular veins [7]. For the same reasons, a future study of permissive hypercapnia, named ‘PERMISS’ will exclude neurocritical care patients, explicitly.
Optimal MV parameters in neurosurgical anesthesia remains to be defined [38]. A post-hoc analysis of ‘Local Assessment of Ventilatory management during general anesthesia for surgery’ (LAS VEGAS) showed that neurosurgical patients were commonly ventilated with low VT (median VT 8 ml/kg PBW (IQR = 7.3– 9) and low PEEP (median PEEP = 5 cmH2O (IQR 3–5), while RMs were rarely applied (6.9% of routine RMs vs. 1.4% of unplanned RMs) [39]. In this analysis, a similar incidence in PPCs (unplanned need for oxygen therapy, respiratory failure, ARDS, pneumonia, pneumothorax) was found in both spine and the brain surgical patients, and intraoperative ventilator settings were not associated with them [39].
Tidal Volume
Specific data on VT thresholds in neurosurgical patients are limited in the perioperative setting. Knowledge about the impact of VT on brain is derived from studies conducted especially in critically ill patients with brain injury from ICU cohorts. In a recent meta-analysis conducted in 5639 ventilated patients with ABI, no differences in mortality were shown in patients ventilated with a low VT strategy (< 8 ml/kg PBW) compared to those who received high VT (≥ 8 ml/kg PBW) [OR 0.88 (95% CI 0.74 to 1.05), p = 0.16, I2 = 20%] [40], but a major risk of PPCs was shown in patients exposed to high VT (VT > 10 mL/Kg of PBW) [41].
A consequential risk of low VT is the potential hypercapnia effect which could be deleterious on cerebral hemodynamics. As known, due to the linear relation between PaCO2 and CBF [42] and because of the perivascular acidosis, cerebrovascular vasodilation and consequent intracranial hypertension can occur in case of elevated CO2. Given the lack of specific recommendations, and unless low VT might be related to hypercapnia current knowledge assess the feasibility of LPV in neurosurgical patients [43] applying low VT (6–8 ml/kg of PBW) [44,45,46,47], ideally adjusting it to lung size [43] with the aim to reduce PPCs, [9] minimizing alveolar overdistention and rupture, and lung injury associated to both systemic and alveolar inflammation and setting it to achieve normal PaCO2 levels [42, 48].
PEEP and RMs
PEEP titration can prevent alveolar de-recruitment, reduce atelectasis and intrapulmonary shunt, and thereby improve oxygenation and lung mechanics [49]. The application of recruitment maneuvers (RMs) is still controversial in neurosurgical patients because of concerns for increased ICP, especially in patients with impaired CA [50]. In fact, the risk of intracranial hypertension due to the increase in intrathoracic pressure and reduced cerebral venous outflow is traditionally considered a concern in this population [9], although recent evidence suggests that PEEP application might not compromise ICP, provided that MAP is preserved [51, 52]. In addition, a decrease in venous return and cardiac output may reduce MAP compromising cerebral perfusion pressure (CPP) with a risk of ischemia [53].
Data about PEEP in neurosurgical patients is controversial. In the past, PEEP was used to prevent and treat venous air embolism (VAE) that can occur during sitting positioning craniotomies [54] because of its effect in increasing right atrial and peripheral venous pressures impeding the entry of air into the central circulation [54]. However, more recent knowledge do not demonstrated decrease in incidence of VAE in patients ventilated with PEEP. [55] In addition, PEEP seems to be related to an increased risk of paradoxical air embolism in the specific scenario of patients with a probe patent foramen ovale. [56, 57].
Historically, clinicians have been cautious regarding PEEP titration due to concerns of increased intrathoracic pressure and ICP. At present, in neurosurgical patients, while it’s important to cautiously focus on the hemodynamic status, respiratory mechanics and lung morphology [58] and monitor ICP in those at risk, PEEP should be used with the same principles as for the general ICU population.
Similarly to PEEP, RMs increase intrathoracic pressure and lead to detrimental effects on ICP, although pressure control recruitment strategy may improve oxygenation, reducing the impairment of ICP [59, 60]. A randomized clinical trial, conducted on neurosurgical patients with the aim to understand feasibility of LPV, found a correlation between RMs and hemodynamic adverse events (i.e. hypotension) [43].
In short, high PEEP and RMs are generally avoided and used only in cases of severe hypoxemia under strict neuromonitoring control [36]. In addition, optimization of intravascular volume status before anesthesia induction should be considered to keep hemodynamics stable [61].
Plateau and Driving Pressure
Plateau pressure (Pplat), which reflects the pressure applied at the end of inspiration to small airways, and driving pressure (ΔP) defined as the difference between Pplat and PEEP, can lead to VILI [62, 63] A secondary analysis of five randomized controlled trials (RCTs) and a post hoc analysis of a large multicenter observational study conducted in acute respiratory distress syndrome (ARDS) patients found a clear correlation between Pplat on the first day of MV and mortality [64, 65]. The ARDSnet trial conducted on ARDS patients found that the risk of mortality was lower (31% vs. 39.8%) in patients treated with lower VT (6 ml/kg PBW) and lower Pplat (< 30 cmH20) compared to those treated with VT = 12 ml/kg PBW [66]. An association of ΔP with ARDS was found in brain injured subjects [67, 68].
Current guidelines recommend that protective MV should include low Pplat with a threshold value below 20 cmH20 [43] with an upper limit to 30 cmH2O in case of concomitant ARDS [2, 45,46,47] and low ΔP (< 14 cmH20), especially in case of coexistent ARDS and TBI diseases in order to prevent lung damage [68]. The potential caveats for patients with brain injury could be that the gain of a Pplat reduction is often reached by reducing VT, which may lead to hypercapnia and its potential harmful effects already described [69], therefore a balanced and tailored made approach is always recommended.
Mechanical Power
Mechanical power (MP) is the total amount of energy transmitted by the ventilator to the respiratory system during each breath cycle. Observational data suggest that MP may be a potential mediator of VILI during invasive MV in ARDS patients [70]. Strong associations between MP and outcomes have been described in various categories of invasive ventilated ICU patients [71, 72], and even short periods with high MP are associated with worse outcomes [73]. However, it is currently unclear whether these findings can be extrapolated to patients undergoing intraoperative ventilation, and whether similar associations exist in neurocritical care patients, both in the ICU and in the operating room.
Specific data about MP in neurosurgical patients are not available. A study evaluating the association between MP and PPCs in patients undergoing general anesthesia showed that the exposure to high MP values was associated with increased risks of PPCs (OR 1.34, 95% CI, 1.17 to 1.52); p < 0.001) and acute respiratory failure (OR 1.40, 95% CI, 1.21 to 1.61; P < 0.001) in the first seven postoperative days [74]. A prospective observational study assessing the MP effects in the intraoperative setting reported that high MP (12.9 ± 4.5 J/min) is a risk factor for developing PPCs suggesting a 12 J/min as a MP cut-off to prevent PPCs [75]. Specific data on neuro patients derived from ICU neurocritical population. Jiang et al. found that high MP enhances the risk of hospital mortality, prolonged ICU stay, and decreased the number of ventilator-free days [76]. Accordingly a secondary analysis of ‘extubation strategies in neuro-intensive care unit patients and associations with outcome’ (ENIO) study including 1,217 ABI patients who required MV found that the exposure to high MP is associated with poor clinical outcomes (need for reintubation, tracheostomy placement, and ARDS development) [67].
Additionally, it remains unclear whether the association between low MP and improved outcome is due to the fact that less sick patients inherently less often have injured lungs, or have less injured lungs per se. Herein, it is important to note that MP is often low in neurocritical care patients since their lungs are usually uninjured [77]. A relationship of high MP with mortality is reported both in ARDS [78] and non-ARDS patients [79], a value of MP < 17 J/min, associated with appropriate gas exchange and hemodynamics values [80], should be aimed. From the data reported in the LAS VEGAS post hoc analysis in neurosurgical patients, MP had median value of 6.2 J/min [39], suggesting a protective approach generally applied in this population.
The main and easiest way to reduce MP is by reducing VT [81] However, respiratory rate also plays a role in MP, and if reducing VT leads to a significant increase in respiratory rate, there is a chance that MP may actually increase. Furthermore, in neurocritical care, it is uncertain whether PaCO2 levels may be allowed to rise to reduce MP, or rather, what level of PaCO2 can be accepted to protect both the brain and the lungs as much as possible.
Gas Exchange
Oxygen and carbon dioxide levels modulation is a chief priority to prevent secondary brain injury [14]. Based on current knowledge, exact thresholds of gas exchange values in neurosurgical patients remain controversial but the recommended target range in traumatic brain injured patients seem to be 80–120 mmHg of PaO2 independently of ICP elevation, and 35–45 mmHg of PaCO2 in case of no ICP elevation [82]. In general, normoxemia and normocapnia should be aimed, based on the individualization of PaO2 and PaCO2 values on specific patient and disease.
Hypoxemia and hyperoxemia may both be physiologically detrimental. Current knowledge correlate hypoxemia to precipitating ischemia and risk of brain injury and hyperoxemia to the potential oxidative damage due to the activation of reactive oxygen species (ROS) [83], but data are actually mixed. A study reported that high FiO2 may be used in patients with secondary brain injury with no negative effects and without an increase in inflammatory markers and incidence of pulmonary complications [84], while other studies showed an increased risk of death in case of elevated PaO2 [85]. In this sense, oxygenation should be strictly monitored, and a peripheral oxygen saturation (SpO2) of > 94% should be the target [86, 87].
PaCO2 is a key mediator of CBF [42]. Cerebrovascular vasodilation and consequent intracranial hypertension can occur in case of elevated CO2; this effect is mediated by a reduction in the perivascular pH. Conversely, a low PaCO2 value can result in cerebral vasoconstriction via perivascular alkalosis, potentially leading to brain tissue hypoxia and cerebral hypoperfusion [88]. Hypocapnia is associated with brain neuronal damage and apoptosis [89]; extreme hypercapnia should also be prevented [88]. A randomized clinical trial of intraoperative LPV in patients undergoing neurosurgical procedures conducted in 60 patients equally divided into control treatment (treated with VT = 10 ml/kg of PBW, RR at 6–8 breaths/min, no PEEP and no RM) and LPV strategy group (treated with VT≤6 ml/kg of PBW, Respiratory rate at 16 breaths/min, PEEP at 5 cmH20, RM routinely applied after intubation) found higher values of PaCO2 during LPV (mean PaCO2 35.5 mmHg in control group vs. 37.1 mmHg in LPV group), though the difference was not clinically relevant (p = 0.002) [43]. This result should be confirmed by larger studies but suggest again that a personalized approach of MV parameters on the single patient should be recommended.
A recent secondary analysis of the ENIO study suggests that PaCO2 had a U-shaped relationship with PaCO2, where extreme values of hypocapnia (< 25 mmHg) and hypercapnia (> 45 mmHg) were both associated with in-hospital mortality in acute brain injured patients in ICU, suggesting against extreme PaCO2 values [90]. In addition, normal values of CO2 are associated with decreased mortality and could improve outcome in TBI patients [91]. Probably, because of a concern for potential increased ICP, traditionally, TBI patients were often hyperventilated [92]. This was confirmed in the post hoc analysis of the LAS VEGAS study where lower levels of ETCO2 (32 mmHg vs. 33 mmHg) were found in patients undergoing brain surgery compared to those undergoing spinal surgery [39]. Lower values of CO2 can be targeted to manage intracranial hypertension, but therapeutic hyperventilation may be considered as an option in brain herniation as a rescue therapy for brief periods (15–30 min), while definitive treatments for ICP management are arranged (e.g. urgent surgery) [93]. Current knowledge suggests to absolutely avoid PaCO2 < 25 mmHg because of the potential risk of vasoconstriction, reduced CBF and increased risk of cerebral ischemia. In absence of herniation risk, PaCO2 should be maintained between 35 and 38 mmHg or 32–35 mmHg in case of refractory intracranial hypertension [42].
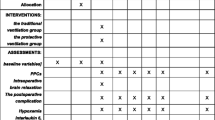
Fig. 2 summarizes the issues and MV parameters that could be used in neurosurgical patients.
Ongoing Trials of MV in Neurosurgical Patients
A recent study relating mechanical ventilation during neurosurgical patients (NCT02386683) with the purpose to explore the effectiveness of LPV during general anesthesia for neurosurgical procedures on postoperative pulmonary outcome, compared with traditional ventilation has been concluded but results are still not published. Further studies are required to understand the better intraoperative ventilation strategy to apply in neurosurgical patients.
Management of Intraoperative Conditions Impacting Mechanical Ventilation
Various conditions related to neurosurgical disease can impact MV management, including intraoperative seizures and ICP crises, VAE.
During awake surgery, in case of seizures and status epilepticus, for instance, cold water or cold artificial CSF can be used on the brain surface to terminate seizures [94]. However, in case of continuous seizures, a switch to general anesthesia with airway protection is mandatory [94].
In patients under general anesthesia, the recognition of seizures could be difficult, and tachycardia and hypertension as a result of sympathetic discharge may be the only signs. [21].
ICP rises need to be prevented and aggressively managed. Appropriate sedation and muscles relaxation are mandatory under anesthesia in order to control ICP by reducing metabolic demand, ventilator asynchrony, venous congestion, and the sympathetic responses [21].
Strict intraoperative monitoring of ICP or of indirect signs, such as pupil alterations and cardiac arrhythmias is warranted [95], aiming at the maintenance of cerebral perfusion pressure and implementation of brain protective measures to decrease CMRO2 and oxygen need. ETCO2 monitoring could help in preventing additional increases in ICP due to hypercarbia [21].
Moreover, VAE may occur during neurosurgical procedures when there is an open connection between the environment and a venous vessel with sub atmospheric pressure, especially those that require a sitting or semi-sitting position (i.e. fossa posterior craniotomies) although this risk was also identified during lumbar laminectomy in the prone position [96, 97]. Saturation, hypotension [98], dyspnea, chest pain and nausea as a sudden drop in the arterial blood pressure and in the ETCO2 value are highly representative signs of VAE, suggesting ETCO2 monitoring as a useful monitoring to prevent this condition [99].
Extubation and Postoperative Pulmonary Complications
Important considerations in determining extubation readiness after neurosurgical procedures include the potential for upper airway obstruction related to different conditions that may develop during surgery. Patients who underwent cervical spine surgery, major head and neck surgery obesity and obstructive sleep apnea syndrome (OSAS), among others, have a significantly higher risk of extubation failure [100].
Risk factors for airway obstruction include prolonged operative time (> 5 h), blood loss > 300 mL, manipulation above the C4 vertebra, myelopathy, operations with > 3 vertebral bodies involved, and use of an anterior-posterior approach [101]. In addition, pharyngeal stenosis leading to airway obstruction after extubation has been described following an anterior approach in cervical spine surgery involving C0-C2 because of the paralysis of the recurrent laryngeal nerve and overflexion during cervical fixation, causing the protrusion of C2 vertebral body into the pharyngeal wall [102,103,104]. Similarly, laryngeal edema is possible after spinal surgeries in the prone position [105].
Mainly in neurosurgical patients, during the awakening and extubation phase, it is important to avoid hypertension and coughing to reduce the risk of bleeding and CSF leak [106]. Current knowledge does not provide a right timing or a procedure for performing extubation in neurosurgical patients, but it is undeniable that early and safe extubation might reduce PPCs, diminishing the duration of MV experienced by patients.
In neurosurgery the occurrence of PPCs is closely related with neurological deficits and has a significant impact on patients’ quality of life [107,108,109]. Intraoperative MV plays an important role in the development of PPCs, such as atelectasis, pneumonia, and infections [88]. Neurosurgical procedures are recognized as high risk for the occurrence of PPCs [110].
PPCs adversely influence morbidity and mortality [111], especially within the first postoperative week [112].
In patients undergoing neurosurgical procedures, PPCs are estimated to develop in 13% of subjects, significantly affecting clinical outcomes [34, 39, 43, 113].
Neurosurgical patients who undergo craniotomy [114] as well as patients undergoing posterior fossa surgery are at higher risk of developing PPCs because of the potential for mechanical obstruction, central respiratory dysfunction, and neuromuscular dysfunction [115]. In addition, OSAS is a frequently existing condition in posterior fossa lesions [116]. A recent study analyzed the incidence of PPCs in patients underwent craniotomy for posterior fossa tumors, finding that the most important predictors of PPCs were postoperative blood transfusion, prolonged ICU stay, and tracheostomy and relating PPCs to a longer ICU and hospital stay, and increased mortality [117].
In this sense, LPV strategies including the use of a low VT, low PEEP and low Pplat seem to reduce the risk of PPCs [2], but its application in neurocritical patients is still debated. A recent randomized controlled trial (RCT) found LPV feasible for neurosurgical patients, reporting no differences in intraoperative adverse events (cerebral tension and PaCO2) between the group treated with LPV strategy and the control group [43].
A post-hoc analysis of the LAS VEGAS study focused on neurosurgical patients undergoing brain or spine surgery showed no differences in PPCs incidence in the spine and the brain surgical groups, and no association between intraoperative ventilator settings and PPCs [39].
Conclusion
Many questions regarding MV in neurosurgical patients remain unsolved and are still under debate.
Neurosurgical patients pose challenges for perioperative anesthesiologist management. The main challenges include the need to use protective ventilation to prevent lung injury while avoiding secondary brain damage.
Firstly, the airway management could be more difficult in these patients. Some may require cervical immobilization, hindering standard extension procedure during laryngoscopy. The fragile cerebral dynamics of this population could be affected by unnatural head positioning, potentially impairing cerebral venous outflow and increasing the risk of ischemia. The risk of hypercapnia, related to a delayed ventilation or a low VT LPV could lead to increased CBF with an increasing the risk of high ICP, which is dangerous for the patients’ dynamics and the risk of bleeding. LPV, generally recommended in abdominal surgical patients for its protective effect on PPCs, may be applied in neurosurgical patients with special attention. Permissive hypercapnia and higher level of PEEP could have detrimental effects in this population. Strict monitoring is needed intraoperatively to prevent eventual intraoperative conditions that can impact MV, seizures or ICP crises.
Much of the knowledge in this area is derived from neurocritical ICU trials or from studies conducted on general surgical patients. A strong statement on more evidence and specific to neurosurgical patients is needed to understand specific ventilatory threshold and risks in this population, possibly distinguishing between brain surgical and spine surgical patients. While waiting for new results, as there is currently no definitive evidence on the feasibility of utilizing LPV strategies in cranial and spinal surgery, we underscore the importance of using a protective MV strategy to reduce the risk of secondary brain injury. This involves titrating MV parameters to the specific patient’s need and disease characteristics, with strict monitoring.
Data Availability
No datasets were generated or analysed during the current study.
Abbreviations
- ABI:
-
Acute brain injury
- ABP:
-
Arterial blood pressure
- ARDS:
-
Aacute respiratory distress syndrome
- CA:
-
Cerebral autoregulation
- CBF:
-
Cerebral blood flow
- CMRO2 :
-
Cerebral metabolic rate of oxygen
- CPP:
-
Cerebral perfusion pressure
- CSF:
-
Cerebrospinal fluid
- ΔP:
-
Driving Pressure
- EEG:
-
Electroencephalogram
- ETCO2 :
-
End tidal CO2
- FiO2 :
-
Fraction inspirated of oxygen
- HFNC:
-
High flow nasal cannula
- ICP:
-
Intracranial pressure
- ICU:
-
Intensive care unit
- LPV:
-
Lung-protective ventilation
- MAP:
-
Median artery pressure
- MV:
-
Mechanical ventilation
- MP:
-
Mechanical power
- OSAS:
-
Obstructive sleep apnea syndrome
- PBW:
-
Predicted body weight
- PEEP:
-
Positive end-expiratory pressure
- PPC:
-
Postoperative pulmonary complications
- Pplat:
-
Plateau Pressure
- RCT:
-
Randomized controlled trial
- RMs:
-
Recruitment maneuvers
- ROS:
-
Reactive oxygen species
- RSI:
-
Rapid sequence intubation
- rSO2 :
-
Regional cerebral saturation of oxygen
- TBI:
-
Traumatic brain injured
- VAE:
-
Venous air embolism
- VILI:
-
Ventilator-associated lung injury
- VT :
-
Tidal volume
References
Swain A, Bhagat H, Sahni N, Salunke P. Mechanical ventilation in neurological and neurosurgical patients. Neurol India. 2016;64:485. https://doi.org/10.4103/0028-3886.181585.
Young CC, Harris EM, Vacchiano C, Bodnar S, Bukowy B, Elliott RRD, Migliarese J, Ragains C, Trethewey B, Woodward A, et al. Lung-protective ventilation for the Surgical patient: International Expert Panel-based Consensus recommendations. Br J Anaesth. 2019;123:898–913. https://doi.org/10.1016/j.bja.2019.08.017.
Futier E, Jaber S. Lung-protective ventilation in abdominal surgery. Curr Opin Crit Care. 2014;20:426–30. https://doi.org/10.1097/MCC.0000000000000121.
Slutsky AS, Ranieri VM. Ventilator-Induced Lung Injury. N Engl J Med. 2013;369:2126–36. https://doi.org/10.1056/NEJMra1208707.
Pelosi P, Ferguson ND, Frutos-Vivar F, Anzueto A, Putensen C, Raymondos K, Apezteguia C, Desmery P, Hurtado J, Abroug F, et al. Management and outcome of mechanically ventilated neurologic Patients*. Crit Care Med. 2011;39:1482–92. https://doi.org/10.1097/CCM.0b013e31821209a8.
Chacón-Aponte AA, Durán-Vargas ÉA, Arévalo-Carrillo JA, Lozada-Martínez ID, Bolaño-Romero MP, Moscote-Salazar LR, Grille P, Janjua T. Brain-Lung Interaction: a vicious cycle in traumatic brain Injury. Acute Crit Care. 2022;37:35–44. https://doi.org/10.4266/acc.2021.01193.
Robba C, Bonatti G, Battaglini D, Rocco PRM, Pelosi P. Mechanical ventilation in patients with Acute Ischaemic Stroke: from pathophysiology to clinical practice. Crit Care. 2019;23:388. https://doi.org/10.1186/s13054-019-2662-8.
Mascia L. Acute Lung Injury in patients with severe Brain Injury: a double hit Model. Neurocrit Care. 2009;11:417–26. https://doi.org/10.1007/s12028-009-9242-8.
Battaglini D, Siwicka Gieroba D, Brunetti I, Patroniti N, Bonatti G, Rocco PRM, Pelosi P, Robba C. Mechanical ventilation in Neurocritical Care setting: a clinical Approach. Best Pract Res Clin Anaesthesiol. 2021;35:207–20. https://doi.org/10.1016/j.bpa.2020.09.001.
Mrozek S, Constantin J-M, Geeraerts T. Brain-lung crosstalk: implications for Neurocritical Care patients. WJCCM. 2015;4:163. https://doi.org/10.5492/wjccm.v4.i3.163.
Lohela TJ, Lilius TO, Nedergaard M. The Glymphatic System: implications for drugs for Central Nervous System diseases. Nat Rev Drug Discov. 2022;21:763–79. https://doi.org/10.1038/s41573-022-00500-9.
Asehnoune K, Roquilly A, Cinotti R. Respiratory management in patients with severe Brain Injury. Crit Care. 2018;22:76. https://doi.org/10.1186/s13054-018-1994-0.
Koutsoukou A. Respiratory mechanics in Brain Injury: a review. WJCCM. 2016;5. https://doi.org/10.5492/wjccm.v5.i1.65.
Pelosi P, Rocco PR. The lung and the brain: a dangerous cross-talk. Crit Care. 2011;15:168. https://doi.org/10.1186/cc10259.
Murselović T. Airway Management in Neuroanesthesia. ACC 2023, https://doi.org/10.20471/acc.2023.62.s1.15
Rozet I, Vavilala MS. Risks and benefits of patient positioning during Neurosurgical Care. Anesthesiol Clin. 2007;25:631–53. https://doi.org/10.1016/j.anclin.2007.05.009.
Smith WS, Lev MH, English JD, Camargo EC, Chou M, Johnston SC, Gonzalez G, Schaefer PW, Dillon WP, Koroshetz WJ, et al. Significance of large vessel intracranial occlusion causing Acute ischemic stroke and TIA. Stroke. 2009;40:3834–40. https://doi.org/10.1161/STROKEAHA.109.561787.
Beqiri E, García-Orellana M, Politi A, Zeiler FA, Placek MM, Fàbregas N, Tas J, De Sloovere V, Czosnyka M, Aries M, et al. Cerebral autoregulation derived blood pressure targets in Elective Neurosurgery. J Clin Monit Comput. 2024. https://doi.org/10.1007/s10877-023-01115-0.
Tong JL, Ashworth DR, Smith JE. Cardiovascular responses following laryngoscope assisted, fibreoptic Orotracheal Intubation. Anaesthesia. 2005;60:754–8. https://doi.org/10.1111/j.1365-2044.2005.04238.x.
Burney RG, Winn R. Increased cerebrospinal fluid pressure during laryngoscopy and intubation for induction of Anesthesia. Anesth Analgesia. 1975;54:687–90. https://doi.org/10.1213/00000539-197509000-00028.
Rao S, Avitsian R. Anesthesia for Neurosurgical emergencies. Anesthesiol Clin. 2020;38:67–83. https://doi.org/10.1016/j.anclin.2019.10.004.
Rosenblatt W, Ianus AI, Sukhupragarn W, Fickenscher A, Sasaki C. Preoperative endoscopic airway examination (PEAE) provides Superior Airway Information and May reduce the Use of Unnecessary Awake Intubation. Anesth Analgesia. 2011;112:602–7. https://doi.org/10.1213/ANE.0b013e3181fdfc1c.
Farag E. Airway Management for cervical spine surgery. Best Pract Res Clin Anaesthesiol. 2016;30:13–25. https://doi.org/10.1016/j.bpa.2016.01.001.
Martini RP, Larson DM. Clinical evaluation and Airway Management for adults with cervical spine instability. Anesthesiol Clin. 2015;33:315–27. https://doi.org/10.1016/j.anclin.2015.02.004.
Front Matter. In Benumof and Hagberg’s Airway Management; Elsevier. 2013; pp. i–iii ISBN 978-1-4377-2764-7.
Baillard C, Fosse J-P, Sebbane M, Chanques G, Vincent F, Courouble P, Cohen Y, Eledjam J-J, Adnet F, Jaber S. Noninvasive ventilation improves Preoxygenation before Intubation of hypoxic patients. Am J Respir Crit Care Med. 2006;174:171–7. https://doi.org/10.1164/rccm.200509-1507OC.
Ng I, Lim J, Wong HB. Effects of Head posture on cerebral hemodynamics: its influences on intracranial pressure, cerebral perfusion pressure, and cerebral oxygenation. Neurosurgery. 2004;54:593–8. https://doi.org/10.1227/01.NEU.0000108639.16783.39.
Weintraub MI, Khoury A. Cerebral hemodynamic Changes Induced by simulated tracheal intubation: a possible role in Perioperative Stroke? Magnetic Resonance Angiography and Flow Analysis in 160 cases. Stroke. 1998;29:1644–9. https://doi.org/10.1161/01.STR.29.8.1644.
Bozeman WP, Idris AH. Intracranial pressure changes during Rapid sequence intubation: a swine model. J Trauma: Injury Infect Crit Care. 2005;58:278–83. https://doi.org/10.1097/01.TA.0000152536.71932.85.
Yadav M, Reddy EP, Sharma A, Kulkarni DK, Gopinath R. The effect of position on PaCO2 and PETCO2 in patients undergoing cervical spine surgery in supine and prone position. J Neurosurg Anesthesiol. 2017;29:298–303. https://doi.org/10.1097/ANA.0000000000000322.
Güldner A, Kiss T, Serpa Neto A, Hemmes SNT, Canet J, Spieth PM, Rocco PRM, Schultz MJ, Pelosi P. Gama De Abreu, M. Intraoperative Protective Mechanical Ventilation for Prevention of Postoperative Pulmonary complications: a Comprehensive Review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015;123:692–713. https://doi.org/10.1097/ALN.0000000000000754.
Futier E, Constantin J-M, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, Marret E, Beaussier M, Gutton C, Lefrant J-Y, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–37. https://doi.org/10.1056/NEJMoa1301082.
PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology, Hemmes SNT, Gama de Abreu M, Pelosi P, Schultz MJ. High versus low positive end-expiratory pressure during General Anaesthesia for Open Abdominal surgery (PROVHILO trial): a Multicentre Randomised Controlled Trial. Lancet. 2014;384:495–503. https://doi.org/10.1016/S0140-6736(14)60416-5.
Mazo V, Sabaté S, Canet J, Gallart L, De Abreu MG, Belda J, Langeron O, Hoeft A, Pelosi P. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121:219–31. https://doi.org/10.1097/ALN.0000000000000334.
Meng L, Gelb AW. Regulation of cerebral autoregulation by Carbon Dioxide. Anesthesiology. 2015;122:196–205. https://doi.org/10.1097/ALN.0000000000000506.
Della Torre V, Badenes R, Corradi F, Racca F, Lavinio A, Matta B, Bilotta F, Robba C. Acute Respiratory Distress Syndrome in Traumatic Brain Injury: how do we manage it? J Thorac Dis. 2017;9:5368–81. https://doi.org/10.21037/jtd.2017.11.03.
Komjáti K, Greenberg JH, Reivich M, Sándor P. Interactions between the endothelium-derived relaxing Factor/Nitric Oxide System and the endogenous Opiate System in the modulation of cerebral and spinal vascular CO 2 responsiveness. J Cereb Blood Flow Metab. 2001;21:937–44. https://doi.org/10.1097/00004647-200108000-00006.
Mazzeo AT, Fanelli V, Mascia L. Brain-lung crosstalk in critical care: how protective mechanical ventilation can affect the Brain Homeostasis. Minerva Anestesiol. 2013;79:299–309.
VEGAS Study, Robba C, Hemmes SNT, Serpa Neto A, Bluth T, Canet J, Hiesmayr M, Hollmann MW, Mills GH, et al. * In this post-hoc analysis of LAS VEGAS study authors analyzed intraoperative ventilator settings and their association with postoperative pulmonary complications specifically in patients undergoing neurosurgery. BMC Anesthesiol. 2020;20. https://doi.org/10.1186/s12871-020-00988-x. stratified them on the type of surgery (brain and spine). Intraoperative Ventilator Settings and Their Association with Postoperative Pulmonary Complications in Neurosurgical Patients: Post-Hoc Analysis of LAS.
Asehnoune K, Rooze P, Robba C, Bouras M, Mascia L, Cinotti R, Pelosi P, Roquilly A. Mechanical ventilation in patients with Acute Brain Injury: a systematic review with Meta-analysis. Crit Care. 2023;27:221. https://doi.org/10.1186/s13054-023-04509-3.
Neto AS, Hemmes SNT, Barbas CSV, Beiderlinden M, Fernandez-Bustamante A, Futier E, Gajic O, El-Tahan MR, Ghamdi AAA, Günay E, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for General Anaesthesia: a Meta-analysis of individual Patient Data. Lancet Respiratory Med. 2016;4:272–80. https://doi.org/10.1016/S2213-2600(16)00057-6.
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GWJ, Bell MJ, Bratton SL, Chesnut R, Harris OA, Kissoon N, et al. Guidelines for the management of severe traumatic brain Injury, Fourth Edition. NEUROSURGERY. 2017;80:6–15. https://doi.org/10.1227/NEU.0000000000001432.
Longhini F, Pasin L, Montagnini C, Konrad P, Bruni A, Garofalo E, Murabito P, Pelaia C, Rondi V, Dellapiazza F, et al. Intraoperative Protective Ventilation in patients undergoing major neurosurgical interventions: a Randomized Clinical Trial. BMC Anesthesiol. 2021;21:184. https://doi.org/10.1186/s12871-021-01404-8. * In this RCT authors studied the feasibility of intraoperative lung protective ventilation in patients undergoing major neurosurgical intervention.
Towner JE, Rahmani R, Zammit CG, Khan IR, Paul DA, Bhalla T, Roberts DE. Mechanical ventilation in Aneurysmal Subarachnoid Hemorrhage: systematic review and recommendations. Crit Care. 2020;24:575. https://doi.org/10.1186/s13054-020-03269-8.
Neto AS, Simonis FD, Barbas CSV, Biehl M, Determann RM, Elmer J, Friedman G, Gajic O, Goldstein JN, Linko R, et al. Lung-protective ventilation with low tidal volumes and the occurrence of pulmonary complications in patients without Acute Respiratory Distress Syndrome: a systematic review and Individual Patient Data Analysis*. Crit Care Med. 2015;43:2155–63. https://doi.org/10.1097/CCM.0000000000001189.
Davies JD, Senussi MH, Mireles-Cabodevila E, Should. A tidal volume of 6 mL/Kg be used in all patients? Respir Care. 2016;61:774–90. https://doi.org/10.4187/respcare.04651.
Marhong JD, Ferguson ND, Singh JM. Ventilation practices in Subarachnoid Hemorrhage: a Cohort Study exploring the Use of Lung Protective Ventilation. Neurocrit Care. 2014;21:178–85. https://doi.org/10.1007/s12028-014-0014-8.
Sterling G, Ventilation. Br J Clin Pharmacol. 1979;8:513–21. https://doi.org/10.1111/j.1365-2125.1979.tb01038.x.
Gattinoni L, Collino F, Maiolo G, Rapetti F, Romitti F, Tonetti T, Vasques F, Quintel M. Positive end-expiratory pressure: how to set it at the individual level. Ann Transl Med. 2017;5:288–288. https://doi.org/10.21037/atm.2017.06.64.
Armstead WM. Cerebral blood Flow Autoregulation and Dysautoregulation. Anesthesiol Clin. 2016;34:465–77. https://doi.org/10.1016/j.anclin.2016.04.002.
Mascia L, Grasso S, Fiore T, Bruno F, Berardino M, Ducati A. Cerebro-Pulmonary interactions during the application of low levels of positive end-expiratory pressure. Intensive Care Med. 2005;31:373–9. https://doi.org/10.1007/s00134-004-2491-2.
Robba C, Bragazzi NL, Bertuccio A, Cardim D, Donnelly J, Sekhon M, Lavinio A, Duane D, Burnstein R, Matta B, et al. Effects of Prone position and positive end-expiratory pressure on Noninvasive estimators of ICP: a pilot study. J Neurosurg Anesthesiol. 2017;29:243–50. https://doi.org/10.1097/ANA.0000000000000295.
Georgiadis D, Schwarz S, Baumgartner RW, Veltkamp R, Schwab S. Influence of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure in patients with Acute Stroke. Stroke. 2001;32:2088–92. https://doi.org/10.1161/hs0901.095406.
Zasslow MA, Pearl RG, Larson CP, Silverberg G, Shuer LF. PEEP does not affect left atrial-right atrial pressure difference in neurosurgical patients. Anesthesiology. 1988;68:760–3. https://doi.org/10.1097/00000542-198805000-00014.
Giebler R, Kollenberg B, Pohlen G, Peters J. Effect of positive end-expiratory pressure on the Incidence of Venous Air Embolism and on the Cardiovascular response to the sitting position during neurosurgery. Br J Anaesth. 1998;80:30–5. https://doi.org/10.1093/bja/80.1.30.
Perkins NA, Bedford RF. Hemodynamic consequences of PEEP in seated neurological patients–implications for Paradoxical Air Embolism. Anesth Analg. 1984;63:429–32.
Meyer P-G, Cuttaree H, Charron B, Jarreau M-M, Perie A-C, Sainte-Rose C. Prevention of venous air Embolism in Paediatric Neurosurgical procedures Performed in the sitting position by combined use of MAST suit and PEEP. Br J Anaesth. 1994;73:795–800. https://doi.org/10.1093/bja/73.6.795.
Robba C, Ball L, Nogas S, Battaglini D, Messina A, Brunetti I, Minetti G, Castellan L, Rocco PRM, Pelosi P. Effects of positive end-expiratory pressure on Lung Recruitment, respiratory mechanics, and intracranial pressure in mechanically ventilated brain-injured patients. Front Physiol. 2021;12:711273. https://doi.org/10.3389/fphys.2021.711273.
Giardina A, Cardim D, Ciliberti P, Battaglini D, Ball L, Kasprowicz M, Beqiri E, Smielewski P, Czosnyka M, Frisvold S, et al. Effects of positive end-expiratory pressure on cerebral hemodynamics in Acute Brain Injury patients. Front Physiol. 2023;14. https://doi.org/10.3389/fphys.2023.1139658.
Sanfilippo F, Uryga A, Ball L, Battaglini D, Iavarone IG, Smielewski P, Beqiri E, Czosnyka M, Patroniti N, Robba C. The Effect of Recruitment maneuvers on Cerebrovascular dynamics and right ventricular function in patients with Acute Brain Injury: a single-center prospective study. Neurocrit Care. 2024. https://doi.org/10.1007/s12028-024-01939-x.
Morakul S, Prachanpanich N, Permsakmesub P, Pinsem P, Mongkolpun W, Trongtrakul K. Prediction of Fluid responsiveness by the Effect of the lung recruitment maneuver on the Perfusion Index in mechanically ventilated patients during surgery. Front Med. 2022;9:881267. https://doi.org/10.3389/fmed.2022.881267.
Amato MBP, Meade MO, Slutsky AS, Brochard L, Costa ELV, Schoenfeld DA, Stewart TE, Briel M, Talmor D, Mercat A, et al. Driving pressure and survival in the Acute Respiratory Distress Syndrome. N Engl J Med. 2015;372:747–55. https://doi.org/10.1056/NEJMsa1410639.
International Consensus Conferences in Intensive Care Medicine: Ventilator-Associated Lung Injury in ARDS: This Official Conference Report was C osponsored by the American Thoracic Society, the European Society of Intensive Care Medicine, and the Societé de Réanimation de Langue Française, and was A pproved by the ATS B oard of D irectors, J uly 1999. Am J Respir Crit Care Med. 1999, 160, 2118–2124, https://doi.org/10.1164/ajrccm.160.6.ats16060
The LUNG SAFE Investigators and the ESICM Trials Group, Laffey JG, Bellani G, Pham T, Fan E, Madotto F, Bajwa EK, Brochard L, Clarkson K, Esteban A, et al. Potentially modifiable factors contributing to Outcome from Acute Respiratory Distress Syndrome: the LUNG SAFE study. Intensive Care Med. 2016;42:1865–76. https://doi.org/10.1007/s00134-016-4571-5.
Hager DN, Krishnan JA, Hayden DL, Brower RG. Tidal volume reduction in patients with Acute Lung Injury when Plateau pressures are not high. Am J Respir Crit Care Med. 2005;172:1241–5. https://doi.org/10.1164/rccm.200501-048CP.
Brower RG, Matthay MA, Morris A, et al. Ventilation with Lower Tidal Volumes as compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. N Engl J Med. 2000;342:1301–8. https://doi.org/10.1056/NEJM200005043421801.
Wahlster S, Sharma M, Taran S, Town JA, Stevens RD, Cinotti R, Asehnoune K, Robba C. the ENIO collaborators Associations Between Driving Pressure and Clinical Outcomes in Acute Brain Injury: A Subanalysis of ENIO. Am J Respir Crit Care Med 2024, rccm.202402-0402LE, https://doi.org/10.1164/rccm.202402-0402LE
Tejerina E, Pelosi P, Muriel A, Peñuelas O, Sutherasan Y, Frutos-Vivar F, Nin N, Davies AR, Rios F, Violi DA, et al. Association between Ventilatory settings and Development of Acute Respiratory Distress Syndrome in mechanically ventilated patients due to Brain Injury. J Crit Care. 2017;38:341–5. https://doi.org/10.1016/j.jcrc.2016.11.010.
Taran S, Cho S-M, Stevens RD. Mechanical ventilation in patients with traumatic Brain Injury: is it so different? Neurocrit Care. 2023;38:178–91. https://doi.org/10.1007/s12028-022-01593-1.
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, Protti A, Gotti M, Chiurazzi C, Carlesso E, et al. Ventilator-related causes of Lung Injury: the Mechanical Power. Intensive Care Med. 2016;42:1567–75. https://doi.org/10.1007/s00134-016-4505-2.
Sim JK, Lee S-M, Kang HK, Kim KC, Kim YS, Kim YS, Lee W-Y, Park S, Park SY, Park J-H, et al. Association between Mechanical Power and Intensive Care Unit Mortality in Korean patients under pressure-controlled ventilation. ACC. 2024;39:91–9. https://doi.org/10.4266/acc.2023.00871.
for the PROVE Network Investigators, Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, Cazati DC, Cordioli RL, Correa TD, et al. Mechanical Power of Ventilation Is Associated with Mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44:1914–22. https://doi.org/10.1007/s00134-018-5375-6.
Chen H, Chen Z-Z, Gong S-R, Yu R-G. Visualizing the dynamic Mechanical Power and Time Burden of Mechanical Ventilation Patients: an analysis of the MIMIC-IV Database. j Intensive care. 2023;11:58. https://doi.org/10.1186/s40560-023-00709-9.
Karalapillai D, Weinberg L, Neto A, Peyton S, Ellard P, Hu L, Pearce R, Tan B, Story CO, O’Donnell D. Intra-operative Ventilator Mechanical Power as a predictor of Postoperative Pulmonary complications in Surgical patients: a secondary analysis of a Randomised Clinical Trial. Eur J Anaesthesiol. 2022;39:67–74. https://doi.org/10.1097/EJA.0000000000001601.
El-Khatib M, Zeeni C, Shebbo FM, Karam C, Safi B, Toukhtarian A, Nafeh NA, Mkhayel S, Shadid CA, Chalhoub S, et al. Intraoperative Mechanical Power and Postoperative Pulmonary complications in Low-Risk Surgical patients: a prospective Observational Cohort Study. BMC Anesthesiol. 2024;24. https://doi.org/10.1186/s12871-024-02449-1.
Jiang X, Zhu Y, Zhen S, Wang L. Mechanical Power of Ventilation Is Associated with Mortality in Neurocritical patients: a Cohort Study. J Clin Monit Comput. 2022;36:1621–8. https://doi.org/10.1007/s10877-022-00805-5.
Frisvold S, Coppola S, Ehrmann S, Chiumello D, Guérin C. Respiratory challenges and Ventilatory Management in different types of Acute Brain-injured patients. Crit Care. 2023;27:247. https://doi.org/10.1186/s13054-023-04532-4.
Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, Cazati DC, Cordioli RL, Correa TD, Pollard TJ, et al. Mechanical Power of Ventilation Is Associated with Mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44:1914–22. https://doi.org/10.1007/s00134-018-5375-6.
Wu H-P, Chu C-M, Chuang L-P, Lin S-W, Leu S-W, Chang K-W, Chiu L-C, Liu P-H, Kao K-C. The Association between Mechanical Power and Mortality in patients with Pneumonia using pressure-targeted ventilation. Diagnostics. 2021;11:1862. https://doi.org/10.3390/diagnostics11101862.
Gattinoni L, Collino F, Camporota L. Mechanical power: meaning, uses and limitations. Intensive Care Med. 2023;49:465–7. https://doi.org/10.1007/s00134-023-06991-3.
Kassis EB, Hu S, Lu M, Johnson A, Bose S, Schaefer MS, Talmor D, Lehman L-WH, Shahn Z. Titration of Ventilator settings to target driving pressure and Mechanical Power. Respir Care. 2022;68:199–207. https://doi.org/10.4187/respcare.10258.
Meyfroidt G, Bouzat P, Casaer MP, Chesnut R, Hamada SR, Helbok R, Hutchinson P, Maas AIR, Manley G, Menon DK, et al. Management of moderate to severe traumatic brain Injury: an update for the Intensivist. Intensive Care Med. 2022;48:649–66. https://doi.org/10.1007/s00134-022-06702-4.
Mach WJ, Thimmesch AR, Pierce JT, Pierce JD. Consequences of Hyperoxia and the toxicity of Oxygen in the lung. Nurs Res Pract. 2011;2011:1–7. https://doi.org/10.1155/2011/260482.
Lång M, Skrifvars MB, Siironen J, Tanskanen P, Ala-Peijari M, Koivisto T, Djafarzadeh S, Bendel S. A pilot study of Hyperoxemia on Neurological Injury, inflammation and oxidative stress. Acta Anaesthesiol Scand. 2018;62:801–10. https://doi.org/10.1111/aas.13093.
Ni Y-N, Wang Y-M, Liang B-M, Liang Z-A. The Effect of Hyperoxia on Mortality in critically ill patients: a systematic review and Meta Analysis. BMC Pulm Med. 2019;19:53. https://doi.org/10.1186/s12890-019-0810-1.
Roffe C, Nevatte T, Sim J, Bishop J, Ives N, Ferdinand P, Gray R. For the Stroke Oxygen Study investigators and the Stroke OxygenStudy Collaborative Group Effect of Routine Low-Dose Oxygen supplementation on death and disability in adults with Acute Stroke: the Stroke Oxygen Study Randomized Clinical Trial. JAMA. 2017;318:1125. https://doi.org/10.1001/jama.2017.11463.
Chesnut R, Aguilera S, Buki A, Bulger E, Citerio G, Cooper DJ, Arrastia RD, Diringer M, Figaji A, Gao G, et al. A management algorithm for adult patients with both brain oxygen and intracranial pressure monitoring: the Seattle International severe traumatic brain Injury Consensus Conference (SIBICC). Intensive Care Med. 2020;46:919–29. https://doi.org/10.1007/s00134-019-05900-x.
Borsellino B, Schultz MJ, De Gama M, Robba C, Bilotta F. Mechanical ventilation in Neurocritical Care patients: a systematic literature review. Expert Rev Respir Med. 2016;10:1123–32. https://doi.org/10.1080/17476348.2017.1235976.
Deng R-M, Liu Y-C, Li J-Q, Xu J-G, Chen G. The role of Carbon Dioxide in Acute Brain Injury. Med Gas Res. 2020;10:81. https://doi.org/10.4103/2045-9912.285561.
Robba C, Battaglini D, Abbas A, Sarrió E, Cinotti R, Asehnoune K, Taccone FS, Rocco PR, Schultz MJ, Citerio G, et al. Clinical practice and effect of Carbon Dioxide on outcomes in mechanically ventilated Acute Brain-injured patients: a secondary analysis of the ENIO Study. Intensive Care Med. 2024;50:234–46. https://doi.org/10.1007/s00134-023-07305-3.
Howard MB, McCollum N, Alberto EC, Kotler H, Mottla ME, Tiusaba L, Keller S, Marsic I, Sarcevic A, Burd RS, et al. Association of Ventilation during initial trauma resuscitation for traumatic Brain Injury and post-traumatic outcomes: a systematic review. Prehosp Disaster med. 2021;36:460–5. https://doi.org/10.1017/S1049023X21000534.
Dumont TM, Visioni AJ, Rughani AI, Tranmer BI, Crookes B. Inappropriate prehospital ventilation in severe traumatic brain Injury increases In-Hospital mortality. J Neurotrauma. 2010;27:1233–41. https://doi.org/10.1089/neu.2009.1216.
Robba C, Poole D, McNett M, Asehnoune K, Bösel J, Bruder N, Chieregato A, Cinotti R, Duranteau J, Einav S, et al. Mechanical ventilation in patients with Acute Brain Injury: recommendations of the European Society of Intensive Care Medicine Consensus. Intensive Care Med. 2020;46:2397–410. https://doi.org/10.1007/s00134-020-06283-0.
Guidelines Committee of the Japan Awake Surgery Conference. Guidelines for awake surgery. Neurol Med Chir (Tokyo). 2024;64:1–27. https://doi.org/10.2176/jns-nmc.2023-0111.
Molnár C, Nemes C, Szabó S, Fülesdi B. Harvey Cushing, a Pioneer of Neuroanesthesia. J Anesth. 2008;22:483–6. https://doi.org/10.1007/s00540-008-0652-0.
Horlocker TT, Wedel DJ, Cucchiara RF. Venous air Embolism during spinal Instrumentation and Fusion in the Prone position. Anesth Analgesia. 1992;75:152. https://doi.org/10.1213/00000539-199207000-00045.
Albin MS, Ritter RR, Pruett CE, Kalff K. Venous air embolism during lumbar laminectomy in the Prone position: report of three cases. Anesth Analgesia. 1991;73:346–9. https://doi.org/10.1213/00000539-199109000-00021.
Bithal PK, Pandia MP, Dash HH, Chouhan RS, Mohanty B, Padhy N. Comparative Incidence of Venous Air Embolism and Associated Hypotension in adults and Children Operated for Neurosurgery in the sitting position. Eur J Anaesthesiol. 2004;21:517–22. https://doi.org/10.1097/00003643-200407000-00003.
Vinay B, Sriganesh K, Gopala Krishna KN. An abrupt reduction in End-Tidal Carbon-Dioxide during Neurosurgery is not always due to venous air Embolism: a Capnograph artefact. J Clin Monit Comput. 2014;28:217–9. https://doi.org/10.1007/s10877-013-9505-y.
Cavallone LF, Vannucci A. Extubation of the difficult Airway and Extubation failure. Anesth Analgesia. 2013;116:368–83. https://doi.org/10.1213/ANE.0b013e31827ab572.
Sagi HC, Beutler W, Carroll E, Connolly PJ. Airway complications Associated with surgery on the anterior cervical spine. Spine. 2002;27:949–53. https://doi.org/10.1097/00007632-200205010-00013.
Lee Y-H, Hsieh P-F, Huang H-H, Chan K-C. Upper Airway obstruction after Cervical Spine Fusion surgery: role of cervical fixation Angle. Acta Anaesthesiol Taiwan. 2008;46:134–7. https://doi.org/10.1016/S1875-4597(08)60008-9.
Tagawa T, Akeda K, Asanuma Y, Miyabe M, Arisaka H, Furuya M, Yoshida K, Sakuraba S. Upper Airway Obstruction Associated with Flexed Cervical position after posterior Occipitocervical Fusion. J Anesth. 2011;25:120–2. https://doi.org/10.1007/s00540-010-1069-0.
Yoshida M, Neo M, Fujibayashi S, Nakamura T. Upper-Airway obstruction after short posterior Occipitocervical Fusion in a Flexed position. Spine (Phila Pa 1976). 2007;32:E267–270. https://doi.org/10.1097/01.brs.0000259977.69726.6f.
Cook TM, Woodall N, Frerk C. Fourth National Audit Project Major Complications of Airway Management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: Anaesthesia. Br J Anaesth. 2011;106:617–31. https://doi.org/10.1093/bja/aer058.
Gracia I, López AM, Valero R. Airway Management in Neurosurgical Procedures (Along with Ventilation Management). In Challenging Topics in Neuroanesthesia and Neurocritical Care; Khan, Z.H., Ed.; Springer International Publishing: Cham, 2017; pp. 109–121 ISBN 978-3-319-41443-0.
Schiavolin S, Broggi M, Acerbi F, Brock S, Schiariti M, Cusin A, Visintini S, Leonardi M, Ferroli P. The impact of neurosurgical complications on patients’ Health Status: a comparison between different grades of complications. World Neurosurg. 2015;84:36–40. https://doi.org/10.1016/j.wneu.2015.02.008.
Ghimire P, Hasegawa H, Kalyal N, Hurwitz V, Ashkan K. Patient-reported outcome measures in neurosurgery: a review of the current literature. NEUROSURGERY. 2018;83:622–30. https://doi.org/10.1093/neuros/nyx547.
Schiavolin S, Ferroli P, Acerbi F, Brock S, Broggi M, Cusin A, Schiariti M, Visintini S, Quintas R, Leonardi M, et al. Disability in Italian neurosurgical patients: validity of the 12-Item World Health Organization Disability Assessment Schedule. Int J Rehabil Res. 2014;37:267–70. https://doi.org/10.1097/MRR.0000000000000064.
Qaseem A, Snow V, Fitterman N, Hornbake ER, Lawrence VA, Smetana GW, Weiss K, Owens DK. For the Clinical Efficacy Assessment Subcommittee of the American College of Physicians* Risk Assessment for and strategies to reduce Perioperative Pulmonary complications for patients undergoing noncardiothoracic surgery: a Guideline from the American College of Physicians. Ann Intern Med. 2006;144:575. https://doi.org/10.7326/0003-4819-144-8-200604180-00008.
Shander A, Fleisher LA, Barie PS, Bigatello LM, Sladen RN, Watson CB. Clinical and economic Burden of Postoperative Pulmonary complications: Patient Safety Summit on Definition, risk-reducing interventions, and preventive Strategies*. Crit Care Med. 2011;39:2163–72. https://doi.org/10.1097/CCM.0b013e31821f0522.
Brooks-Brunn JA. Predictors of postoperative pulmonary complications following abdominal surgery. Chest. 1997;111:564–71. https://doi.org/10.1378/chest.111.3.564.
Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Subramaniam B, Martinez Ruiz R, Lee J-W, Henderson WG, Moss A, Mehdiratta N, et al. Postoperative pulmonary complications, early mortality, and Hospital Stay following noncardiothoracic surgery: a Multicenter Study by the Perioperative Research Network Investigators. JAMA Surg. 2017;152:157. https://doi.org/10.1001/jamasurg.2016.4065.
Franceschini J, Sogame LC, Gazzotti MR, Vidotto MC, Jardim JR. Pulmonary function and thoraco-abdominal configuration after Elective Craniotomy. Neurosurg Q. 2008;18:22–7. https://doi.org/10.1097/WNQ.0b013e3181642714.
Howard R, Mahoney A, Thurlow AC. Respiratory obstruction after posterior Fossa surgery. Anaesthesia. 1990;45:222–4. https://doi.org/10.1111/j.1365-2044.1990.tb14689.x.
Guleria R, Madan K. Pulmonary complications in neurosurgical patients. IJNS. 2012;01:175–80. https://doi.org/10.4103/2277-9167.102299.
Hooda B, Chouhan R, Rath G, Lamsal R, Bithal P. Incidence and predictors of postoperative pulmonary complications in patients undergoing craniotomy and excision of posterior Fossa Tumor. J Anaesthesiol Clin Pharmacol. 2019;35:254. https://doi.org/10.4103/joacp.JOACP_350_17.
Funding
Open access funding provided by Università degli Studi di Genova within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
CR, PR, II and MS designed the review. II, SW ST designed the figures. All the authors drafted the manuscript; all the authors contributed in drafting and finalising the manuscript. All the authors approved the last version of the manuscript.
Corresponding author
Ethics declarations
Human and Animal Rights
All reported studies with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its institutional research committee standards, and international guidelines).
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iavarone, I.G., Rocco, P.R., Silva, P.L. et al. Perioperative Ventilation in Neurosurgical Patients: Considerations and Challenges. Curr Anesthesiol Rep (2024). https://doi.org/10.1007/s40140-024-00644-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s40140-024-00644-x